Abstract
Proton pump inhibitors (PPIs) were widely used. Observational studies suggested increasing risk of kidney injury in patients with PPIs treatment. We gathered six PPI regimens and adverse reports of acute kidney injury (AKI) and chronic kidney disease (CKD) based on US FDA Adverse Event Reporting System (FAERS) database from 2004 to 2019. We employed reporting odds ratio (ROR) to detect signals. Finally, we identified 3187 PPIs-associated AKI cases and 3457 PPIs-associated CKD cases. We detected significant signals between PPIs and AKI as well as CKD. The signal strength was stronger for CKD (ROR = 8.80, 95% CI 8.49–9.13) than AKI (ROR = 3.95, 95% CI 3.81–4.10), while dexlansoprazole performed stronger association for CKD (ROR = 34.94, 95% CI 30.89–39.53) and AKI (ROR = 8.18, 95% CI 7.04–9.51) than the other five PPIs. The median time from PPIs use to event occurrence was 23 days for AKI and 177 days for CKD. PPIs-associated AKI resulted larger proportion of death, life-threatening, hospitalization and disability events than PPIs-associated CKD. By mining the FAERS big data, we provided more information between PPIs use and the AKI and CKD events. PPIs rational use should be repeatedly stressed.
Subject terms: Drug safety, Kidney diseases
Introduction
Proton pump inhibitors (PPIs) were widely used to treat peptic ulcer disease (PUD), gastroesophageal reflux disease (GERD), Helicobacter pylori infection, and to prevent side effects of glucocorticoids or non-steroidal anti-inflammatory drugs (NSAIDs)1. However, PPIs were overused by off label indication, excessive dosage and long-term treatment2,3.
With the widespread use of PPIs, more and more studies concerned for the safety of PPIs treatment4–7. Among which, kidney injury including acute kidney injury (AKI) and chronic kidney disease (CKD) following PPI therapy was a hot issue. However, original studies concerning PPIs-associated kidney injury were almost cohort or retrospective studies and systematic reviews based on them8–11, the only randomized controlled trial evaluated only pantoprazole and found no significant relationship between pantoprazole and CKD12.
Adverse event reporting system data was an outstanding source for post-marketing drug safety monitoring and pharmacovigilance analysis. The US food and drug administration (FDA) adverse event reporting system (FAERS) is one of the largest databases open to the public13. To the end of 2019, FAERS had collected more than ten million of cases, containing adverse drug event reports submitted by healthcare professionals, manufacturers, consumers and lawyers. These reports could be quantitatively analyzed using data mining methods to detect signals of drug-associated adverse events14,15. The objective of present study was to detect the signal of PPI-associated renal injury by systematically assessing spontaneous reports submitted to the FAERS database.
Results
Characteristics analysis
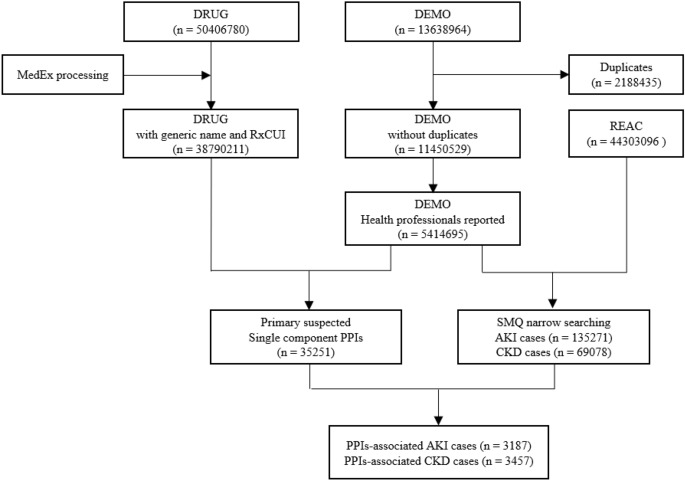
After data cleaning, we retrieved a total of 11,450,529 cases from January 2004 to December 2019 from FAERS database, 5,414,695 of which were reported by health professionals (Fig. 1). We screened 35,251 PPIs-associated ADE cases reported by health professionals, including 10,299, 8963, 6093, 1439, 7273 and 1184 cases for omeprazole, pantoprazole, lansoprazole, rabeprazole, esomeprazole and dexlansoprazole, respectively. No case was identified for dexrabeprazole (ATC code: A02BC07). We further identified 3187 and 3457 PPIs users reported by health professionals with AKI and CKD events, respectively (Table 1). 1096 (34.39%) cases reported more than one kinds of PPIs in AKI group, however, the number was 1748 (51.61%) in CKD group. The concomitant drugs and adverse events were in Supplementary Table S1 and S2, respectively.
Figure 1.
Flow chart of identifying PPI associated AKI and CKD cases from FAERS database.
Table 1.
Characteristics of PPIs associated AKI and CKD cases from FAERS database.
| Characteristics | Subgroups | AKI | CKD | ||
|---|---|---|---|---|---|
| Cases/N | Proportion/% | Cases/N | Proportion/% | ||
| Cases | All PPIs | 3187 | 100.00 | 3457 | 100.00 |
| Omeprazole | 561 | 17.60 | 166 | 4.80 | |
| Pantoprazole | 999 | 31.30 | 1196 | 34.60 | |
| Lansoprazole | 1014 | 31.80 | 1542 | 44.60 | |
| Rabeprazole | 55 | 1.70 | 28 | 0.80 | |
| Esomeprazole | 353 | 11.10 | 158 | 4.60 | |
| Dexlansoprazole | 205 | 6.40 | 367 | 10.60 | |
| PPI | One kind | 2091 | 65.61 | 1673 | 48.39 |
| Two or more kinds | 1096 | 34.39 | 1784 | 51.61 | |
| Age | < 18 years | 24 | 0.80 | 10 | 0.30 |
| 18–65 years | 752 | 23.60 | 559 | 16.20 | |
| ≥ 65 years | 882 | 27.70 | 419 | 12.10 | |
| Unknown | 1529 | 48.00 | 2469 | 71.40 | |
| Sex | Female | 1038 | 32.60 | 892 | 25.80 |
| Male | 971 | 30.50 | 695 | 20.10 | |
| Unknown | 1178 | 37.00 | 1870 | 54.10 | |
| Reporter | Physician | 665 | 20.90 | 314 | 9.10 |
| Other health professional | 2255 | 70.80 | 3082 | 89.20 | |
| Pharmacist | 267 | 8.40 | 61 | 1.80 | |
| Country (top 5) | United States | 1844 | 57.9 | 3015 | 87.20 |
| France | 526 | 16.5 | 154 | 4.50 | |
| Great Britain | 289 | 9.10 | 61 | 1.80 | |
| Japan | 84 | 2.60 | 32 | 0.90 | |
| Germany | 59 | 1.90 | 34 | 1.00 | |
| Year | 2019 | 1942 | 60.90 | 2851 | 82.50 |
| 2018 | 391 | 12.30 | 231 | 6.70 | |
| 2017 | 140 | 4.40 | 45 | 1.30 | |
| 2016 | 207 | 6.50 | 35 | 1.00 | |
| 2004 to 2015 | 507 | 15.90 | 295 | 8.40 | |
PPIs proton pump inhibitors, AKI acute kidney injury, CKD chronic kidney disease.
Among cases reported with age, the proportion of PPIs users in over-65-year group was larger than other age groups for AKI, while the proportion was larger in 18 to 65 group for CKD. Female cases were reported more than male, the female versus male ratio were 1.07 and 1.28 for the events of AKI and CKD, respectively.
Other health professional (70.80%) reported the most cases, followed by physician (20.90%) and pharmacist (8.40%). United States (57.90%) reported the most cases, followed by France (16.50%) and Great Britain (9.10%).
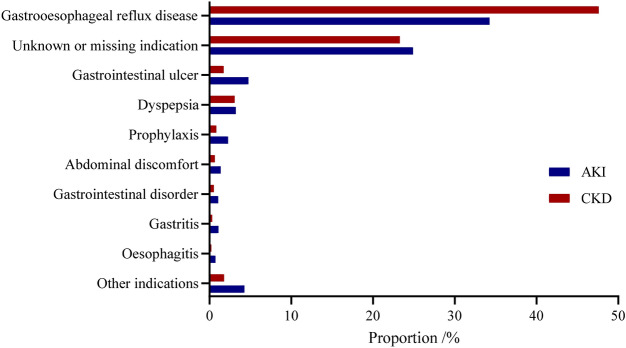
Gastroesophageal reflux disease was the most common indication, accounting for 41.21% (2738/6644) for all AKI and CKD cases. However, 24.07% (1599/6644) PPIs users were prescribed with unknown or missing indication. The other indications were shown in Fig. 2.
Figure 2.
Indications of PPIs associated AKI and CKD cases from FAERS database. PPIs proton pump inhibitors, AKI acute kidney injury, CKD chronic kidney disease.
Signal detection
We first conducted signal detection based on all PPIs, detected significant AKI and CKD signals. The strength of CKD signal (ROR = 8.80, 95% CI 8.49–9.13) was stronger than AKI (ROR = 3.95, 95% CI 3.81–4.10). Then we conducted signal detection in individual PPI, detected significant AKI and CKD signals in all the six PPIs (Table 2).
Table 2.
Signal detection for AKI and CKD of PPIs users from FAERS database.
| Renal injury | Drugs | Cases with renal injury/n | Cases with all AE/N | Proportion of renal injury cases in all AE cases/% | ROR | 95% CI |
|---|---|---|---|---|---|---|
| AKI | All PPIs | 3187 | 35,251 | 9.04 | 3.95 | 3.81–4.10 |
| Omeprazole | 561 | 10,299 | 5.45 | 2.25 | 2.07–2.45 | |
| Pantoprazole | 999 | 8963 | 11.15 | 4.92 | 4.61–5.26 | |
| Lansoprazole | 1014 | 6093 | 16.64 | 7.84 | 7.33–8.39 | |
| Rabeprazole | 55 | 1439 | 3.82 | 1.55 | 1.18–2.03 | |
| Esomeprazole | 353 | 7273 | 4.85 | 1.99 | 1.79–2.22 | |
| Dexlansoprazole | 205 | 1184 | 17.31 | 8.18 | 7.04–9.51 | |
| CKD | All PPIs | 3457 | 35,251 | 9.81 | 8.80 | 8.49–9.13 |
| Omeprazole | 166 | 10,299 | 1.61 | 1.27 | 1.09–1.48 | |
| Pantoprazole | 1196 | 8963 | 13.34 | 12.11 | 11.39–12.87 | |
| Lansoprazole | 1542 | 6093 | 25.31 | 26.80 | 25.28–28.40 | |
| Rabeprazole | 28 | 1439 | 1.95 | 1.54 | 1.06–2.23 | |
| Esomeprazole | 158 | 7273 | 2.17 | 1.72 | 1.47–2.01 | |
| Dexlansoprazole | 367 | 1184 | 31.00 | 34.94 | 30.89–39.53 |
PPIs proton pump inhibitors, AKI acute kidney injury, CKD chronic kidney disease, AE adverse event, ROR reporting odds ratio, 95% CI 95% confidence interval.
For AKI detection, dexlansoprazole detected the strongest signal (ROR = 8.18, 95% CI 7.04–9.51), followed by lansoprazole (ROR = 7.84, 95% CI 7.33–8.39), rabeprazole detected the weakest signal (ROR = 1.55, 95% CI 1.18–2.03).
For CKD detection, dexlansoprazole detected the strongest signal (ROR = 34.94, 95% CI 30.89–39.53), followed by lansoprazole (ROR = 26.80, 95% CI 25.28–28.40), omeprazole detected the weakest signal (ROR = 1.27, 95% CI 1.09–1.48).
Time interval calculation
The time interval analysis included a total of 848 cases, including 562 cases for AKI and 286 cases for CKD.
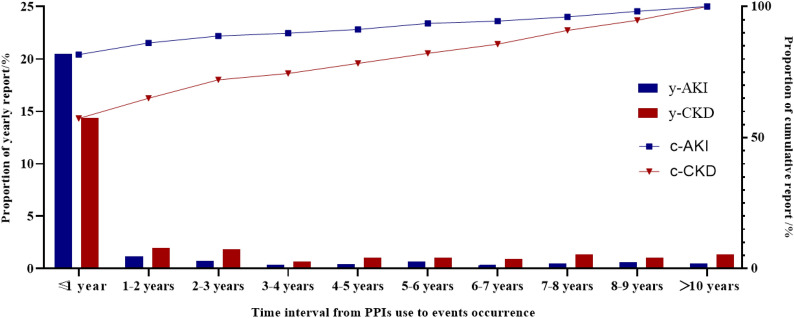
The biggest yearly reports proportion of PPIs-associated AKI and CKD events occurred in the first year (Fig. 3), accounting 81.67% (459/562) for AKI and 57.34% (164/286) CKD.
Figure 3.
Time interval from PPIs use to AKI and CKD events occurrence from FAERS database. PPIs proton pump inhibitors, AKI acute kidney injury, CKD chronic kidney disease.
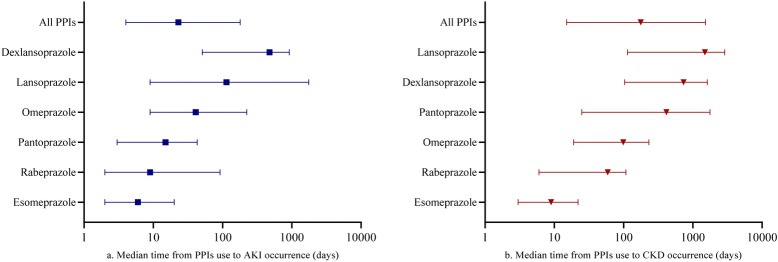
The median time from PPIs use to AKI occurrence was 23 (interquartile range (IQR) 4 to 179) days (Fig. 4a). The longest AKI occurrence median time was 476 (IQR 51 to 917) days for dexlansoprazole, while the shortest time was 6 (IQR 2 to 20) days for esomeprazole.
Figure 4.
Median time from PPIs use to events occurrence from FAERS database. PPIs proton pump inhibitors, AKI acute kidney injury, CKD chronic kidney disease.
The median time from PPIs use to CKD occurrence was 177 (IQR 15 to 1528) days (Fig. 4b). The longest CKD occurrence median time was 1495 (IQR 114 to 2883) days for lansoprazole, while the shortest time was 9 (IQR 3 to 22) days for esomeprazole.
Prognosis analysis
We analyzed outcomes of PPIs-associated AKI and CKD events. Compared with PPIs-associated CKD, PPIs-associated AKI resulted larger proportion of death, life-threatening, hospitalization and disability events. The individual PPI-associated AKI and CKD outcomes were shown in Table 3.
Table 3.
Outcomes of cases reported as AKI and CDK using PPIs from FAERS database.
| Renal injury | Drugs | Cases with renal injury/N | Death | Life-threatening | Hospitalization | Disability | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Cases/n | Proportion/% | Cases/n | Proportion/% | Cases/n | Proportion/% | Cases/n | Proportion/% | |||
| AKI | All PPIs | 3187 | 391 | 12.27 | 161 | 5.05 | 856 | 26.86 | 19 | 0.60 |
| Omeprazole | 561 | 46 | 8.20 | 69 | 1.23 | 294 | 52.41 | 8 | 1.43 | |
| Pantoprazole | 999 | 111 | 11.11 | 29 | 0.29 | 245 | 24.52 | 7 | 0.70 | |
| Lansoprazole | 1014 | 150 | 14.79 | 14 | 0.14 | 93 | 9.17 | 2 | 0.20 | |
| Rabeprazole | 55 | 6 | 10.91 | 4 | 0.73 | 24 | 43.64 | 1 | 1.82 | |
| Esomeprazole | 353 | 57 | 16.15 | 44 | 1.25 | 195 | 55.24 | 1 | 0.28 | |
| Dexlansoprazole | 205 | 21 | 10.24 | 1 | 0.05 | 5 | 2.44 | 0 | 0.00 | |
| CKD | All PPIs | 3457 | 375 | 10.85 | 65 | 0.19 | 296 | 8.56 | 16 | 0.46 |
| Omeprazole | 166 | 19 | 11.45 | 32 | 1.93 | 76 | 45.78 | 7 | 4.22 | |
| Pantoprazole | 1196 | 122 | 10.20 | 10 | 0.08 | 99 | 8.28 | 7 | 0.59 | |
| Lansoprazole | 1542 | 174 | 11.28 | 4 | 0.03 | 30 | 1.95 | 1 | 0.06 | |
| Rabeprazole | 28 | 4 | 14.29 | 1 | 0.36 | 13 | 46.43 | 0 | 0.00 | |
| Esomeprazole | 158 | 24 | 15.19 | 17 | 1.08 | 73 | 46.20 | 1 | 0.63 | |
| Dexlansoprazole | 367 | 32 | 8.72 | 1 | 0.03 | 5 | 1.36 | 0 | 0.00 | |
PPIs proton pump inhibitors, AKI acute kidney injury, CKD chronic kidney disease.
Dosage analysis
The median daily dose (60 mg, IQR 60 to 60) of dexlansoprazole was the highest, twofold of the WHO DDD, followed by esomeprazole (CKD group), 1.33-fold of the WHO DDD, however the dose ranges were within that recommended by drug label. The median daily doses of other PPIs were equal to or lower than the WHO DDD (Table 4).
Table 4.
Daily dose of PPIs from FAERS database.
| Renal injury | Drugs | Cases with renal injury /N | Renal injury cases with daily dose reported /n | WHO DDD /mg | Daily dose recommended by drug label /mg | PPI daily dose /mg | |
|---|---|---|---|---|---|---|---|
| Median | IQR | ||||||
| AKI | Omeprazole | 561 | 217 | 20 | 20–60 | 20 | 20–40 |
| Pantoprazole | 999 | 320 | 40 | 40 | 40 | 40–40 | |
| Lansoprazole | 1014 | 404 | 30 | 15–60 | 30 | 30–40 | |
| Rabeprazole | 55 | 6 | 20 | 20–60 | 20 | 10–20 | |
| Esomeprazole | 353 | 198 | 30 | 20–40 | 20 | 20–40 | |
| Dexlansoprazole | 205 | 56 | 30 | 30–60 | 60 | 60–60 | |
| CKD | Omeprazole | 166 | 42 | 20 | 20–60 | 20 | 20–40 |
| Pantoprazole | 1196 | 332 | 40 | 40 | 40 | 40–40 | |
| Lansoprazole | 1542 | 662 | 30 | 15–60 | 30 | 30–40 | |
| Rabeprazole | 28 | 3 | 20 | 20–60 | 20 | 10–20 | |
| Esomeprazole | 158 | 51 | 30 | 20–40 | 40 | 20–40 | |
| Dexlansoprazole | 367 | 107 | 30 | 30–60 | 60 | 60–60 | |
PPIs proton pump inhibitors, AKI acute kidney injury, CKD chronic kidney disease, DDD defined daily dose IQR: interquartile range.
Discussion
The present study investigated six PPIs-associated AKI and CKD, as well as indications and outcomes of reported cases, time interval to events occurrence and dosage of PPIs using. The results indicated significant association between AKI or CKD events and PPIs, including dexlansoprazole, lansoprazole, pantoprazole, omeprazole, esomeprazole and rabeprazole. The signal strength was stronger in CKD than AKI and varied across specific PPI regimens.
PPIs-associated renal injury had caught professionals’ attention, as well as the public and the media. Recently, many studies focused on PPIs associated AKI8,16,17 and CKD9,18–21. To reduce the influence of the public and the media, we had removed cases reported by consumers and lawyers. However, more than half the cases were reported in 2019, the risk of stimulated reporting could not be ruled out.
Overuse of PPIs was a worldwide problem. Our study found more than 20% PPI cases did not report clear indications. A PPI prescription survey of 45 hospitals published in 2019 indicated that between 32 and 56% of the PPI prescriptions did not have appropriate indications in China2. And an multicenter observational study in 2020 showed a range from 22 to 63% of PPIs treatment in Italian nursing homes were inappropriate3. To decrease drug related kidney injury, improper PPI use should be avoided firstly.
Omeprazole is the PPI with the longest history of clinical use and first report of PPIs-associated kidney injury22. However, the most cases reported of PPIs-associated AKI and CKD was lansoprazole, and the strongest signal of PPIs-associated AKI and CKD was dexlansoprazole from FAERS. Welch analyzed drug-associated AKI compared with all other drugs using FAERS data from 2004 to 2015, found the ROR was 2.35 (95% CI 2.19–2.53) for omeprazole23, being consistent with the result of our study. Chen detected PPIs-associated AKI based on cases reported by all reporters in FAERS from 2004 to 2019, the ROR value of each PPI was bigger than our study17, indicated over-estimation could be reduced to a certain extent by removing non-health professionals' reports.
Our study found the highest yearly proportion of PPIs-associated AKI and CKD was within the first years after PPIs treatment and the median time was 23 days for AKI and 177 days for CKD. Chen found a longer median time (446 days) for PPIs-associated AKI17. Studies revealed the risk of AKI or CKD increased with cumulative or prolonged PPIs use20,24. Unnecessary long-term PPIs use should be avoided.
Studies revealed PPIs was associated with increased risk of death25–27. Research reported the all cause death ratio of PPIs was 13.40%, 4861 deaths out of 36,282 PPIs users, and PPIs showed higher odds (OR 1.76) for mortality after logistic analysis25. Another study reported the estimated death ratio due to PPIs-induced CKD was 0.419%26. In our study, outcome analysis revealed all cause death proportion (PPIs-associated renal injury number as denominator) was 10.85% for PPIs-associated CKD and 12.27% for PPIs-associated AKI. Because the FAERS data did not include PPI users without adverse event occurrence, the incidence rate could not be calculated. However, such a high proportion of death and hospitalization could still attract our attention.
The findings of the present study and the existing evidence should arouse vigilance of PPI use. PPIs should be prescribed or sold following proven indication, low dose and short course28. PPIs users with no or unknown indication should stop PPI treatment, and those with indications should avoid long term PPI use if unnecessary26. Patients with primary kidney disease should pay more attention using PPIs. Monitoring of kidney function for long-term PPI users was necessary26.
Our study revealed significant association between AKI, CKD and PPIs treatment based on the FAERS real world big data, however, certain limitations existed. Like other spontaneous reporting system, FAERS is voluntary and opened to health professional as well as general public, so under-reporting, over-reporting, varied or missing information was inevitable29. Some calculation, especially PPIs duration and PPIs dose, just included cases with data reported. It was also difficult to perform risk factors analysis between PPIs and kidney injury for the limited information. Although non-health professionals’ reports excluded, the risk of stimulated reporting could not be eliminated.
Conclusion
The present study identified six PPIs-associated AKI and CKD signals based on the FAERS data. Significant signal strength was stronger for CKD than AKI, while dexlansoprazole performed stronger association for AKI and CKD than the other five PPIs. A high proportion of renal injury occurred after the first year of PPI treatment and the median time was longer for CKD than AKI. Besides, more than 20% PPI treatment did not have clear indications. Our findings suggest PPIs-associated AKI and CKD should be taken into account, and the importance of PPIs rational use should be reemphasized.
Methods
Data source
We downloaded 64 quarters of adverse event report datasets from the FAERS Quarterly Data Extract Files website30, covering the period from January 2004 to December 2019.
Each quarterly data was consisted of seven data tables, including the DEMO table for patient demographic and administrative information, the DRUG table for the drug information, the REAC table for adverse events information, the OUTC table for patient outcomes information, the RPSR table for report sources information, the THER table for drug therapy start and end dates information and the INDI table for the indications for drug use. We imported all data into the local FAERS database, managed by Microsoft SQL server 2017 software.
We de-duplicated cases from the original datasets following the FDA recommendations. We removed the same records from the DEMO table and kept one, then removed the earliest FDA_DT when the CASEIDs were the same and removed the lower PRIMARYID when the CASEID and FDA_DT were the same. To make the evaluation more accurately, we only included cases reported by health professionals, including physician, pharmacist and other health professional in the OCCP_COD column of the DEMO table.
PPIs identification
In the DRUG table, drugs could be documented in brand names, synonymous names or their abbreviations besides generic names in the DRUGNAME or the PROD_AI columns. We used the MedEx software (MedEx UIMA 1.3.7, Vanderbilt university, US) to transform different forms of drug name into the “generic name”, and add an identification code named RXNORM_RxCUI31,32.
We tried to identify the seven single component PPI regimens with the WHO Anatomical Therapeutic Chemical (ATC) code of A02BC from the local FAERS database. The seven PPIs included omeprazole (ATC code: A02BC01), pantoprazole (ATC code: A02BC02), lansoprazole (ATC code: A02BC03), rabeprazole (ATC code: A02BC04), esomeprazole (ATC code: A02BC05), dexlansoprazole (ATC code: A02BC06) and dexrabeprazole (ATC code: A02BC07). We restricted the drug role as primary suspected (PS) drug in the DRUG table.
Events identification
According to the Medical Dictionary for Regularly Activities (MedDRA) and Standardised MedDRA Queries (SMQs) version 23.1. We identified AKI cases using SMQ coded 20000003 narrow searching in the REAC table, including 19 Preferred Terms (PTs). We then identified CKD cases using SMQ coded 20000213 narrow searching, including 38 PTs. One case could be reported more than one PTs of the same SMQ, duplicate records was removed. For example, one case reported two records of “acute kidney injury” and “acute phosphate nephropathy”, we counted the two records as one AKI case. The PTs details could be found in Supplementary Table S3.
Data mining
We counted the characteristics of AKI and CKD cases with PPIs use, including cases attributed to different PPIs, age and sex of patient, occupation and country of reporter, year of event reported and indications for PPIs application.
We employed reporting odds ratio (ROR) to detect the signals of AKI and CKD relevant to PPIs. In current study, ROR was the degree of disproportionate reporting of AKI or CKD event for PPIs compared to the same event for all other drugs in the FAERS database. The calculation method of ROR, 95% confidence interval (95% CI) for ROR were shown in Table 5. A significant signal is detected when the report cases ≥ 3 and the lower limit of 95% CI exceed one33. Basically, the higher the ROR value, the stronger the strength of the signal13.
Table 5.
Two-by-two contingency table for reporting odds ratio analyses.
| Drugs | AKI/CKD cases | All other adverse event cases |
|---|---|---|
| PPIs | a | b |
| All other drugs | c | d |
| ROR = , 95% CI for ROR = exp (ln (ROR) ± 1.96 ) | ||
PPIs proton pump inhibitors, AKI acute kidney injury, CKD chronic kidney disease, ROR reporting odds ratio, 95% CI 95% confidence interval.
We further estimated the time interval from PPIs use to AKI and CKD events occurrence. We unified the time format as yyyy-mm-dd. The time interval was calculated using event date (EVENT_DT) in the DEMO table minus drug start date (START_DT) in the THER table. To make the calculation more accurately, we excluded cases not in the period of 2004 to 2019, cases without year, month or day data in either EVENT_DT or START_DT field, and cases with earlier event date than drug start date.
We also analyzed patient outcomes for the events, including death, life-threatening, hospitalization and disability for the PPIs associated AKI and CKD cases. If a case reported more than one outcome, we kept the worst one, for instance, one case reported both death and life-threatening, we removed the life-threatening one.
Finally, we analyzed PPIs daily dose and compared to the defined daily dose (DDD) recommended by the world health organization (WHO) or the label dose.
The statistical analyses were conducted by SPSS version 20.0 (IBM corporation, Armonk, New York, USA) and GraphPad prism version 8.0.2 (GraphPad Software, San Diego, California, USA).
Supplementary Information
Author contributions
B.W. and T.X. designed the research. B.W., D.L., T.X., M.L., Z.H. and Y.L. wrote the article. B.W. and D.L. collected the data. B.W. and M.L. performed data analysis. B.W., D.L., T.X., Z.H. and Y.L. contributed to data interpretation and intellectual content.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-83099-y.
References
- 1.Strand DS, Kim D, Peura DA. 25 years of proton pump inhibitors: A comprehensive review. Gut Liver. 2017;11:27–37. doi: 10.5009/gnl15502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ying J, Li LC, Wu CY, Yu ZW, Kan LD. The status of proton pump inhibitor use: A prescription survey of 45 hospitals in China. Rev. Esp. Enferm. Dig. 2019;111:738–743. doi: 10.17235/reed.2019.6155/2019. [DOI] [PubMed] [Google Scholar]
- 3.Pasina L, Novella A, Elli C, Nobili A, Ianes A. Overuse of proton pump inhibitors in nursing homes: An Italian multicenter observational study. Pharmacoepidemiol. Drug Saf. 2020;29:461–466. doi: 10.1002/pds.4963. [DOI] [PubMed] [Google Scholar]
- 4.Haastrup PF, Thompson W, Søndergaard J, Jarbøl DE. Side effects of long-term proton pump inhibitor use: A review. Basic Clin. Pharmacol. Toxicol. 2018;123:114–121. doi: 10.1111/bcpt.13023. [DOI] [PubMed] [Google Scholar]
- 5.Perry IE, Sonu I, Scarpignato C, Akiyama J, Hongo M, Vega KJ. Potential proton pump inhibitor-related adverse effects. Ann. N. Y. Acad. Sci. 2020 doi: 10.1111/nyas.14428. [DOI] [PubMed] [Google Scholar]
- 6.Rameau A, Andreadis K, Bayoumi A, Kaufman M, Belafsky P. Side effects of proton pump inhibitors: What are patients' concerns? J. Voice. 2020 doi: 10.1016/j.jvoice.2020.01.018. [DOI] [PubMed] [Google Scholar]
- 7.Savarino V, Marabotto E, Furnari M, Zingone F, Zentilin P, Savarino E. Latest insights into the hot question of proton pump inhibitor safety-a narrative review. Dig. Liver Dis. 2020;52:842–852. doi: 10.1016/j.dld.2020.04.020. [DOI] [PubMed] [Google Scholar]
- 8.Antoniou T, et al. Proton pump inhibitors and the risk of acute kidney injury in older patients: A population-based cohort study. CMAJ Open. 2015;3:166–171. doi: 10.9778/cmajo.20140074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hart E, Dunn TE, Feuerstein S, Jacobs DM. Proton pump inhibitors and risk of acute and chronic kidney disease: A retrospective cohort study. Pharmacotherapy. 2019;39:443–453. doi: 10.1002/phar.2235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang Y, George KC, Shang WF, Zeng R, Ge SW, Xu G. Proton-pump inhibitors use, and risk of acute kidney injury: A meta-analysis of observational studies. Drug Des. Dev. Ther. 2017;11:1291–1299. doi: 10.2147/DDDT.S130568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nochaiwong S, et al. The association between proton pump inhibitor use and the risk of adverse kidney outcomes: A systematic review and meta-analysis. Nephrol. Dial. Transplant. 2018;33:331–342. doi: 10.1093/ndt/gfw470. [DOI] [PubMed] [Google Scholar]
- 12.Moayyedi P, et al. Safety of proton pump inhibitors based on a large, multi-year, randomized trial of patients receiving rivaroxaban or aspirin. Gastroenterology. 2019;157:682–691. doi: 10.1053/j.gastro.2019.05.056. [DOI] [PubMed] [Google Scholar]
- 13.FDA. Data Mining at FDA: White Paper (2018). https://www.fda.gov/science-research/data-mining/data-mining-fda-white-paper. Accessed 1 May 2020.
- 14.Duggirala HJ, et al. Use of data mining at the Food and Drug Administration. J. Am. Med. Inform. Assoc. 2016;23:428–434. doi: 10.1093/jamia/ocv063. [DOI] [PubMed] [Google Scholar]
- 15.Evans SJ, Waller PC, Davis S. Use of proportional reporting ratios (PRRs) for signal generation from spontaneous adverse drug reaction reports. Pharmacoepidemiol. Drug Saf. 2001;10:483–486. doi: 10.1002/pds.677. [DOI] [PubMed] [Google Scholar]
- 16.Sutton SS, Magagnoli J, Cummings TH, Hardin JW. Risk of acute kidney injury in patients with HIV receiving proton pump inhibitors. J. Comp. Eff. Res. 2019;8:781–790. doi: 10.2217/cer-2019-0017. [DOI] [PubMed] [Google Scholar]
- 17.Chen G, Ning LJ, Qin Y, Zhao B, Mei D, Li XM. Acute kidney injury following the use of different proton pump inhibitor regimens: A real-world analysis of post-marketing surveillance data. J. Gastroenterol. Hepatol. 2020 doi: 10.1111/jgh.15151. [DOI] [PubMed] [Google Scholar]
- 18.Grant CH, Gillis KA, Lees JS, Traynor JP, Mark PB, Stevens KI. Proton pump inhibitor use and progression to major adverse renal events: A competing risk analysis. QJM. 2019;112:835–840. doi: 10.1093/qjmed/hcz166. [DOI] [PubMed] [Google Scholar]
- 19.Devraj R, Deshpande M. Demographic and health-related predictors of proton pump inhibitor (PPI) use and association with chronic kidney disease (CKD) stage in NHANES population. Res. Soc. Admin. Pharm. 2020;16:776–782. doi: 10.1016/j.sapharm.2019.08.032. [DOI] [PubMed] [Google Scholar]
- 20.Klatte DCF, et al. Association between proton pump inhibitor use and risk of progression of chronic kidney disease. Gastroenterology. 2017;153:702–710. doi: 10.1053/j.gastro.2017.05.046. [DOI] [PubMed] [Google Scholar]
- 21.Lazarus B, et al. Proton pump inhibitor use and the risk of chronic kidney disease. JAMA Intern. Med. 2016;176:238–246. doi: 10.1001/jamainternmed.2015.7193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Christensen PB, Albertsen KE, Jensen P. Renal failure after omeprazole. Lancet. 1993;341:55. doi: 10.1016/0140-6736(93)92531-W. [DOI] [PubMed] [Google Scholar]
- 23.Welch HK, Kellum JA, Kane-Gill SL. Drug-associated acute kidney injury identified in the united states food and drug administration adverse event reporting system database. Pharmacother. J. Hum. Pharmacol. Drug Therapy. 2018;38:785–793. doi: 10.1002/phar.2152. [DOI] [PubMed] [Google Scholar]
- 24.Xie Y, Bowe B, Li T, Xian H, Yan Y, Al-Aly Z. Long-term kidney outcomes among users of proton pump inhibitors without intervening acute kidney injury. Kidney Int. 2017;91:1482–1494. doi: 10.1016/j.kint.2016.12.021. [DOI] [PubMed] [Google Scholar]
- 25.Arora P, et al. Proton pump inhibitors are associated with increased risk of development of chronic kidney disease. BMC Nephrol. 2016 doi: 10.1186/s12882-016-0325-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Al-Aly Z, Maddukuri G, Xie Y. Proton pump inhibitors and the kidney: Implications of current evidence for clinical practice and when and how to deprescribe. Am. J. Kidney Dis. 2020;75:497–500. doi: 10.1053/j.ajkd.2019.07.012. [DOI] [PubMed] [Google Scholar]
- 27.Elias E, Targownik LE. The clinician's guide to proton pump inhibitor related adverse events. Drugs. 2019;79:715–731. doi: 10.1007/s40265-019-01110-3. [DOI] [PubMed] [Google Scholar]
- 28.Moayyedi P. How to advise patients on the risk of chronic proton pump inhibitor therapy. Curr. Opin. Gastroenterol. 2020;36:317–322. doi: 10.1097/MOG.0000000000000641. [DOI] [PubMed] [Google Scholar]
- 29.Palleria C, et al. Limitations and obstacles of the spontaneous adverse drugs reactions reporting: Two "challenging" case reports. J. Pharmacol. Pharmacother. 2013;4:S66–72. doi: 10.4103/0976-500X.120955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.FDA. FDA Adverse Event Reporting System (FAERS) Quarterly Data Extract Files (2019). https://fis.fda.gov/extensions/FPD-QDE-FAERS/FPD-QDE-FAERS.html. Accessed 10 February 2020.
- 31.Xu H, Stenner SP, Doan S, Johnson KB, Waitman LR, Denny JC. MedEx: A medication information extraction system for clinical narratives. J. Am. Med. Inform. Assoc. 2010;17:19–24. doi: 10.1197/jamia.M3378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wu B, Wu FB, Luo M, Qin Z, Xu T. Application of MedEx in FAERS drug names standardization. China J. Hosp Pharm. 2019;39:1989–1992. [Google Scholar]
- 33.van Puijenbroek EP, Bate A, Leufkens HG, Lindquist M, Orre R, Egberts AC. A comparison of measures of disproportionality for signal detection in spontaneous reporting systems for adverse drug reactions. Pharmacoepidemiol. Drug Saf. 2002;11:3–10. doi: 10.1002/pds.668. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.