Abstract
Since 2014, 32 states implemented Medicaid expansion by removing the categorical criteria for childless adults and by expanding income eligibility to 138% of the federal poverty level (FPL) for all non-elderly adults. Previous studies found that the Affordable Care Act (ACA) Medicaid expansion improved rates of being insured, unmet needs for care due to cost, number of physician visits, and health status among low-income adults. However, a few recent studies focused on the expansion’s effect on racial/ethnic disparities and used the National Academy of Medicine (NAM) disparity approach with a limited set of access measures. This quasi-experimental study examined the effect of Medicaid expansion on racial/ethnic disparities in access to health care for U.S. citizens aged 19 to 64 with income below 138% of the federal poverty line. The difference-in-differences model compared changes over time in 2 measures of insurance coverage and 8 measures of access to health care, using National Health Interview Survey (NHIS) data from 2010 to 2016. Analyses used the NAM definition of disparities. Medicaid expansion was associated with significant decreases in uninsured rates and increases in Medicaid coverage among all racial/ethnic groups. There were differences across racial/ethnic groups regarding which specific access measures improved. For delayed care and unmet need for care, decreases in racial/ethnic disparities were observed. After the ACA Medicaid expansion, most access outcomes improved for disadvantaged groups, but also for others, with the result that disparities were not significantly reduced.
Keywords: Medicaid expansion, access to care, racial/ethnic disparities
- What do we already know about this topic?
- The expansion of Medicaid that occurred under the Affordable Care Act increased the proportion insured among low-income populations above the existing poverty guidelines.
- How does your research contribute to the field?
- We found that there were differences across racial/ethnic groups regarding which specific access measures improved. For delayed care and unmet need for care, decreases in racial/ethnic disparities were observed.
- What are your research’s implications toward theory, practice, or policy?
- Since most disparities were not significantly reduced after the ACA Medicaid expansion, there is a need for continuous monitoring of policy impacts, as well as research into the pathways through which Medicaid expansion affects access to care and mitigates health care disparities among racial/ethnic groups.
Health disparities among racial/ethnic subgroups have been large, ubiquitous, and persistent. Blacks and Hispanics have a higher prevalence of obesity and medically diagnosed diabetes, as well as poorer self-reported health, a greater number of both mentally or physically unhealthy days, and higher rates of potentially preventable hospitalizations than non-Hispanic whites.1,2 Particularly, Blacks have higher rates than Whites for most of the 15 leading causes of death.2,3 As a consequence of such disparities, Blacks and Hispanics are expected to have higher health care needs than Whites. However, racial and ethnic minorities have been more likely than Whites to be uninsured for decades, and have experienced unequal treatment in terms of using poorer quality sources of care, having greater unmet need due to cost, and having fewer physician visits.1,4
The National Academy of Medicine (NAM), previously called Institute of Medicine (IOM), in its Unequal Treatment report, defined racial/ethnic disparities in healthcare as “racial or ethnic differences in the quality of healthcare that are not due to access-related factors or clinical needs, preference, and appropriateness of intervention.”5 According to the NAM approach, measurement of racial/ethnic disparities excludes differences in use that result from different health care needs, but includes differences that result from differential SES impact on health and discrimination.5,6 In empirical studies, disparities are commonly measured by comparing means of outcomes between racial/ethnic minorities and non-Hispanic Whites after controlling for all the individual characteristics, which was called the “residual direct effect” (RDE).7 Since RDE captures only those effects of race/ethnicity that are not mediated by SES (or other included individual characteristics), the magnitude of racial/ethnic disparities on access to health care and health outcomes using RDE tends to be underestimated compared to the NAM approach.7 Nearly all empirical studies examining the ACA coverage expansion used RDE in measuring racial/ethnic disparities.
The expansion of Medicaid that occurred under the Affordable Care Act (ACA, 2010) increased rates of insurance among low-income populations.8 Before the ACA Medicaid expansion, poor adults were ineligible if their family income exceeded their state’s Medicaid cutoffs or due to categorical ineligibility. Since 2014, in 32 states, the implementation of Medicaid amendments increased overall access by expanding income eligibility to 138% of the federal poverty level (FPL) for all non-elderly adults, while 19 states (initially 26) opted not to implement the expansion.9,i Various recent ACA studies found improvements in the insured rate and access to care among low-income and childless adults in Medicaid expansion states.8,10-14 There have been fewer studies performing rigorous econometric analyses of the impacts of ACA Medicaid expansion on racial/ethnic disparities. Analyses examining the expansion’s impact on insurance coverage have generated mixed findings. Some studies found that Hispanics experienced a greater decrease in uninsured rates relative to Whites,15-22 or Blacks experienced a greater reduction in uninsured rates than Whites.10,15,20-23 Other studies, however, found that Blacks or Hispanics experienced smaller reductions in uninsured rates than Whites.17,19,23,24
Few studies have examined the effect of the ACA Medicaid expansion on access to care among racial/ethnic subgroups. Two studies found no statistically significant increase in rates of having a usual source of care,10,23 and 1 study found Blacks had a greater increase than Whites in rates of having a usual source of care.24 Two studies found that Hispanics experienced a greater reduction than Whites in unmet need for care due to cost, but Blacks did not,20,22 while 2 other studies found that Blacks had a greater reduction than Whites in unmet need for care due to cost, but Hispanics did not.23,24 One study examined the effect on physician visits for racial/ethnic groups and found no changes in the gap between Blacks or Hispanics relative to Whites.22
There have been even fewer studies that examine the ACA’s impact using the NAM approach. One study estimated the changes in disparities controlling only for age and gender,15 and the other study estimated NAM models by controlling for health care need variables (age, gender, general health status) and marital status among adults with serious psychological distress.25
Important gaps exist in this literature regarding the ACA’s impact on racial/ethnic disparities. First, few studies have examined the effect of the ACA Medicaid expansion on access to care among racial/ethnic subgroups using the NAM approach15,25 by only controlling for health care need variables. Studies which also controlled for other economic factors found mixed results regarding disparities.10,20,22-24 Second, while a few recent studies estimated the effects of Medicaid expansion on “unmet need for care due to cost” and “physician visits,”20,22,23,26 access to specific types of care, such as specialist and mental health care were not distinguished. Since uninsured patients are less likely to be referred to diagnostic/therapeutic services,27 an increase in insured rates due to Medicaid expansion is expected to increase in rates of referral to specialty and mental health care among low-income adults.
This study will address these gaps by applying NAM health care disparities methods and by extending current racial/ethnic ACA impact studies using multiple measures of access and utilization outcomes. We will use rank-and-replace methods to adjust health need variables across race/ethnic subgroups to implement the NAM definition. We will also contribute to the existing ACA literature by adding new findings about whether Medicaid expansion has mitigated disparities in access to care and health service utilization among racial/ethnic subgroups.
Methods
Data
The primary data source for this study is the National Health Interview Survey (NHIS), a national cross-sectional in-person survey collected annually by the CDC’s National Center for Health Statistics (NCHS) for the civilian noninstitutionalized population in the United States. State identifiers are important to this research because the DD model estimates are based on classification of expansion and non-expansion states. Since geographic variables are restricted in the public-use NHIS, these geographic variables were obtained through the NCHS Research Data Center (RDC).
The Area Health Resources File (AHRF), published by the Health Resources and Services Administration (HRSA), was used for annual county unemployment rates from 2010 to 2016.
Study Sample
The study sample was restricted to U.S. citizens aged 19 to 64 with incomes below 138% of the federal poverty line (FPL), for the years 2010 to 2016. This subpopulation is the target group who were most likely to be affected by the ACA Medicaid expansion. A 138% FPL income limit was imposed because the ACA increased income eligibility for Medicaid to 138% of the FPL. Non-U.S. citizens are excluded from the sample since they are not eligible for Medicaid. Two other groups are excluded from the analysis since they were unlikely to be affected by the ACA Medicaid expansion. Specifically, Supplemental Security Income (SSI) recipients are categorically eligible for Medicaid in most states, and Social Security Disability Insurance (SSDI) recipients frequently qualify for Medicare.
Supplemental Table S1a reports the effect of exclusions and missing data on the eventual pooled sample size, which was 67 384 respondents. The final sample size ranged from 29 369 to 67 341 depending on whether respondents are in the sample NHIS adult file or the person file.
Measures
Outcome measures
Following Andersen et al,28 the access variables used in this study can be classified as measuring potential access and health care utilization (realized access). Potential access refers to enabling resources (eg, health insurance) that allow individuals to use health care services, whereas health care utilization refers to actual use of health services (eg, physician visits). Since Medicaid eligibility expansion is designed to reduce the proportion of a household’s total economic resources spent on medical care, it is expected that potential access would be directly affected. However, Medicaid expansion does not deal directly with non-financial barriers to obtaining services, implying smaller effects on health care utilization than on potential access.29
Outcome variables were selected based on previous empirical studies of Medicaid expansion.8,10,26,30-34,11-13,15,18,19,23,24 Seven potential access variables were specified (all binary): uninsured, Medicaid coverage, no usual source of care, delayed care due to cost, and unmet need for care due to cost for general care, specialty, and mental health care. “No usual source of care” was defined having no regular place of care where treatment is sought for acute and preventive care except emergency room, and was constructed using 4 related survey questions. Three health care utilization variables are specified (all binary): no visits to a physician, specialist, or mental health provider. Rates of having physician visits were expected to increase through improvement of affordability of access to care, insurance status, and having regular source of care after the Medicaid expansion. Access variables related to dental care were not included because dental care is not a mandatory Medicaid benefit. For convenience of interpretation, all the outcome variables were negatively coded except for the Medicaid coverage variable (see Supplemental Table S1b).
Treatment and control groups
States were assigned between treatment and control groups based on whether they had adopted the ACA Medicaid expansion by 2016 (treatment group: 32 states) or had not (control group: 19 states). Expansion status was coded 1 for states in the treatment group (including for observations before the expansion), and 0 for control states.
Control variables
The individual-level covariates specified in the model as control variables include age, gender, education level, marital status, employment status, family size, number of children, race/ethnicity, activity limitation, self-reported health status and urban/rural residence based on previous studies.28,29,35-37 Supplemental Table S1d shows specification and coding of these control variables.
The NAM Disparity Models
The quasi-experimental approach described above is implemented using a difference-in-differences (DD) model, which compares the pre-post change in each outcome between expansion and non-expansion states.38 The non-expansion states provide the counterfactual, suggesting what would have happened if the ACA Medicaid expansion had not been implemented.38 The DD estimator was defined based on the date of the implementation date. Twenty-five states expanded Medicaid as of January 1, 2014 and 7 states expanded their Medicaid programs later than January 2014, including Michigan (4/1/2014), New Hampshire (8/15/2014), Pennsylvania (1/1/2015), Indiana (2/1/2015), Alaska (9/1/2015), Montana (1/1/2016), and Louisiana (7/1/2016). Using the NAM definition, racial/ethnic disparities are measured by comparing the mean of access to care and health outcomes between racial/ethnic minorities and non-Hispanic Whites after controlling for selected individual characteristics (age, gender, and health status). The NAM definition is widely accepted in terms of considering the different need for health care by age, gender, and health status.15,25,39-44
Following the NAM disparity approach,6,45 disparities in access outcomes were estimated after adjusting health care need variables (Needicst) for racial/ethnic groups, but not for variables that do not reflect health care need.45 The idea is that health care need variables are the variables that affect health status and regardless of race/ethnicity, SES, or income. This approach starts by estimating initial models of the form:
| (1) |
where Yicst is the outcome for individual i in county c in state s in year-quarter t. Expansionst is the primary explanatory variable, already defined. λt is a vector of quarterly time fixed effects, which capture nationwide differences in outcomes for each year-quarter during the study period. γs is a vector of state fixed effects to capture state-level time-invariant characteristics across the full study period. Unconditional treatment and post-period dummy variables are not specified in the models because quarter and state fixed effects capture their effects. Individual-level covariates other than race/ethnicity were classified into need and non-need variables.45 Needicst is a vector of need factors for individual respondents (age, gender, self-reported general health status, activity limitation, psychological distress). Non-Needicst is a vector of non-need factors (education, income, employment status, marital status, family size, number of children, rural residence). UnempRatect is the annual county unemployment rate.
Due to the nonlinearity of the outcome measures, we used the rank-and-replace method to adjust for health care needs. The rank-and-replace method involves ranking and replacing each minority individual’s health care need variables in order to equalize the distribution of need variables across race/ethnicity.6,7,39-42,45
First, the health care need index was created from the need variables included in the model, listed above. This required estimating a fully specified model (equation (1)) for each access outcome. The health care need index for each outcome was then computed as follows. For outcomes measured using the NHIS Person file, health care need index is a summation of the predicted values of fair or poor health status, functional limitation, age, and gender (βfair/poor Fair/Poor + βlimitation Limitation + βage age + βfemale Female).6,45 For outcomes measured using the NHIS sample adults file, the K-6 scale of psychological distress is added to that list.
Next, observations within each race/ethnicity were ranked based on their values on the health care need index. The health care need index value of each Black and Hispanic individual was then replaced with that of the equivalently ranked White individual (same percentile, in distribution for Whites). The replacement created counterfactual populations of Blacks and Hispanics with the same distribution of the need index as Whites.
Finally, DD models were estimated controlling for the replaced Need Index but removing non-need variables such as education and employment status.
| (2) |
After separate DD models were estimated for each racial/ethnic group, the Stata procedure for “seemingly unrelated estimation,” suest, was used to allow the estimations from all subgroups to be pooled together.46 Then, racial/ethnic cross-equation difference in coefficients was tested using the State lincom post-estimation command. Seemingly unrelated estimation methods were used because it is likely that the errors of the stratified models will be correlated across racial/ethnic groups. This is because unobserved time-varying state-level factors may influence the outcomes among persons of racial/ethnic groups. In contrast to separate models for subgroups, the seemingly unrelated estimation method (suest) estimates the simultaneous covariance-variance matrix using the observations from all racial/ethnic groups.47,ii
Linear probability models were used in preference to logit, as this allows the coefficient on the DD parameter to be interpreted as the effect of the Medicaid expansion on outcome measures. By contrast, in non-linear models, additional steps are required to compute the interaction effect and its statistical significance.48,49 In particular, our plans to use seemingly unrelated regression models (see below) would have further complicated the interpretation of interaction effects if the models used were nonlinear.
In general, researchers using the NHIS employ survey data analysis procedures due to the complex survey design. However, given that the decisions of Medicaid expansion were made at the state-level, error terms are most likely to be correlated within states across time periods.11 Accordingly, observations were weighted using the NHIS final survey weights, and standard errors of all coefficient estimates were adjusted for clustering within states. Considering that survey strata are nested within states, this approach is more conservative than inference using the NHIS survey design variables.11 All analyses were conducted using Stata, version 15.50
The assumption that expansion and non-expansion states groups have parallel pre-ACA trends was tested and robustness checks and a falsification test were conducted. Detailed descriptions are in the supplemental materials (Sections 2 and 3).
Results
Descriptive Statistics
Descriptive statistics for control variables were reported separately in Table 1. This table presented weighted sample means for expansion and non-expansion states and for pre-and post-ACA Medicaid expansion. Regarding individual characteristics, there were moderate differences between groups prior to Medicaid expansion. Compared to those in non-expansion states, individuals in expansion states were more likely to be younger, male, more educated, to have larger family size, to reside in a rural area, but less likely to be married, employed, and to have activity limitation. In addition, prior to expansion, individuals in expansion states were more likely to be Whites (57% vs 54%) and Hispanics (17% vs 15%) and less likely to be Blacks (19% vs 28%), compared to those in non-expansion states. On average, county unemployment rates were initially higher in expansion states than non-expansion states. All these characteristics were controlled for in the DD models.
Table 1.
Descriptive Statistics and Specification of Control Variables for Low-income Whites, Blacks, and Hispanics Adults.
| Overall | Whites | Blacks | Hispanics | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Expansion states | Non–expansion states | Expansion states | Non–expansion states | Expansion states | Non–expansion states | Expansion states | Non–expansion states | |||||||||
| Before | After | Before | After | Before | After | Before | After | Before | After | Before | After | Before | After | Before | After | |
| Age, mean (SD) | 36.68 (13.57) | 37.24 (13.96) | 36.98 (13.67) | 37.33 (13.82) | 37.37 (13.87) | 38.19 (14.29) | 37.51 (13.93) | 37.72 (14.06) | 36.35* (13.11) | 36.82 (13.5) | 36.95 (13.41) | 37.7 (13.73) | 34.56* (12.79) | 34.83 (13.04) | 35.24 (13.01) | 35.3 (13.07) |
| Female | 0.54* (0.5) | 0.56 (0.50) | 0.57 (0.50) | 0.57 (0.5) | 0.53 (0.5) | 0.54 (0.5) | 0.54 (0.5) | 0.54 (0.5) | 0.6 (0.49) | 0.62 (0.49) | 0.62 (0.48) | 0.62 (0.49) | 0.55 (0.5) | 0.55 (0.5) | 0.56 (0.5) | 0.57 (0.5) |
| Elementary school | 0.04 (0.21) | 0.04 (0.19) | 0.04 (0.2) | 0.04 (0.19) | 0.03 (0.18) | 0.03 (0.16) | 0.04 (0.19) | 0.03 (0.18) | 0.02 (0.15) | 0.02 (0.14) | 0.02 (0.14) | 0.02 (0.15) | 0.11 (0.31) | 0.08 (0.28) | 0.09 (0.29) | 0.08 (0.27) |
| Middle school | 0.13* (0.33) | 0.11 (0.32) | 0.14 (0.35) | 0.13 (0.34) | 0.11* (0.31) | 0.1 (0.3) | 0.12 (0.33) | 0.12 (0.33) | 0.16 (0.36) | 0.12 (0.32) | 0.16 (0.37) | 0.14 (0.35) | 0.17 (0.37) | 0.16 (0.36) | 0.16 (0.37) | 0.15 (0.35) |
| High school | 0.73 (0.45) | 0.74 (0.44) | 0.73 (0.44) | 0.74 (0.44) | 0.74 (0.44) | 0.74 (0.44) | 0.73 (0.44) | 0.72 (0.45) | 0.76 (0.42) | 0.8 (0.4) | 0.76 (0.42) | 0.78 (0.42) | 0.67 (0.47) | 0.7 (0.46) | 0.67 (0.47) | 0.71 (0.46) |
| Bachelor/Graduate school | 0.1* (0.3) | 0.11 (0.31) | 0.09 (0.28) | 0.10 (0.3) | 0.13* (0.33) | 0.13 (0.34) | 0.11 (0.31) | 0.12 (0.33) | 0.06 (0.23) | 0.06 (0.24) | 0.05 (0.22) | 0.06 (0.24) | 0.05* (0.22) | 0.06 (0.23) | 0.07 (0.25) | 0.07 (0.25) |
| Married | 0.30* (0.46) | 0.30 (0.46) | 0.32 (0.47) | 0.31 (0.46) | 0.32* (0.47) | 0.32 (0.46) | 0.36 (0.48) | 0.34 (0.47) | 0.18* (0.38) | 0.18 (0.39) | 0.20 (0.4) | 0.20 (0.4) | 0.35* (0.48) | 0.33 (0.47) | 0.4 (0.49) | 0.37 (0.48) |
| Employed | 0.59* (0.49) | 0.59 (0.49) | 0.60 (0.49) | 0.61 (0.49) | 0.6 (0.49) | 0.59 (0.49) | 0.61 (0.49) | 0.59 (0.49) | 0.55* (0.5) | 0.58 (0.49) | 0.58 (0.49) | 0.6 (0.49) | 0.59* (0.49) | 0.61 (0.49) | 0.64 (0.48) | 0.67 (0.47) |
| Family size | 3.18* (1.98) | 3.20 (2.04) | 3.13 (1.92) | 3.08 (1.85) | 2.84 (1.83) | 2.87 (1.92) | 2.88 (1.85) | 2.8 (1.75) | 3.25 (1.92) | 3.22 (1.90) | 3.20 (1.88) | 3.17 (1.89) | 4.10* (2.08) | 3.94 (2.11) | 3.89 (2.02) | 3.77 (1.9) |
| Number of child | 1.11 (1.40) | 1.10 (1.43) | 1.10 (1.38) | 1.08 (1.38) | 0.94 (1.32) | 0.94 (1.37) | 0.95 (1.31) | 0.91 (1.28) | 1.22 (1.45) | 1.21 (1.44) | 1.16 (1.41) | 1.18 (1.45) | 1.56 (1.49) | 1.42 (1.46) | 1.5 (1.46) | 1.43 (1.49) |
| Activity limitation | 0.19* (0.40) | 0.21 (0.41) | 0.20 (0.40) | 0.21 (0.41) | 0.22* (0.41) | 0.25 (0.43) | 0.24 (0.43) | 0.24 (0.42) | 0.2 (0.4) | 0.2 (0.4) | 0.2 (0.4) | 0.22 (0.41) | 0.12 (0.33) | 0.13 (0.34) | 0.11 (0.32) | 0.13 (0.34) |
| Fair/poor Status | 0.19* (0.40) | 0.20 (0.40) | 0.21 (0.41) | 0.21 (0.41) | 0.20* (0.4) | 0.21 (0.41) | 0.22 (0.41) | 0.22 (0.41) | 0.22 (0.42) | 0.2 (0.4) | 0.23 (0.42) | 0.24 (0.43) | 0.17 (0.38) | 0.17 (0.38) | 0.17 (0.38) | 0.17 (0.37) |
| Serious psychological distress | 0.08 (0.27) | 0.09 (0.28) | 0.08 (0.27) | 0.09 (0.28) | 0.09 (0.29) | 0.1 (0.3) | 0.09 (0.29) | 0.11 (0.31) | 0.07 (0.26) | 0.07 (0.26) | 0.06 (0.24) | 0.07 (0.25) | 0.07 (0.25) | 0.07 (0.26) | 0.05 (0.22) | 0.07 (0.25) |
| Rural | 0.83* (0.38) | 0.85 (0.36) | 0.73 (0.45) | 0.76 (0.43) | 0.74 (0.44) | 0.76 (0.42) | 0.64 (0.48) | 0.66 (0.47) | 0.96* (0.19) | 0.96 (0.2) | 0.8 (0.4) | 0.84 (0.36) | 0.96* (0.2) | 0.97 (0.18) | 0.91 (0.29) | 0.9 (0.3) |
| Unemployment rate | 4.46* (1.06) | 2.93 (0.75) | 4.02 (0.99) | 2.58 (0.59) | 4.33 (1.02) | 2.81 (0.69) | 3.95 (0.99) | 2.51 (0.53) | 4.44* (0.96) | 3.02 (0.69) | 4.28 (0.95) | 2.74 (0.54) | 4.91* (1.12) | 3.16 (0.87) | 3.88 (1.03) | 2.55 (0.75) |
Note. The means were weighted by NHIS final weights. Standard deviation is in parentheses. Difference in means of pre-ACA Medicaid expansion between expansion and non-expansion states. *P < .05.
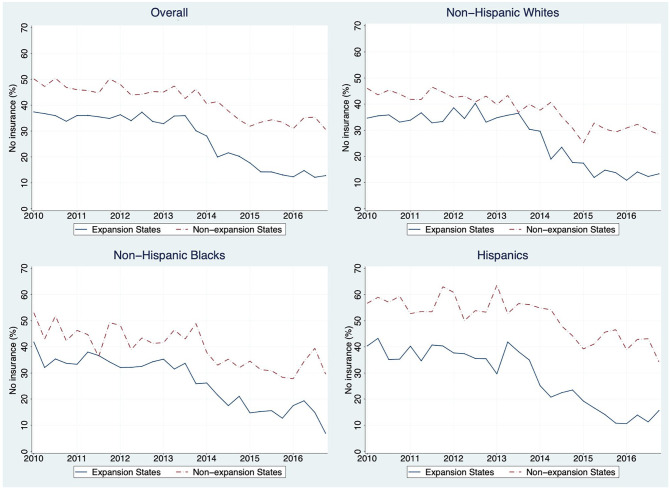
Table 2 and Figure 1 showed unadjusted sample means for the outcome measures before (2010-2013) and after (2014-2016) ACA Medicaid expansion separately for expansion and non-expansion states, for this sample of nonelderly low-income adults. As shown in columns 3 and 6 in Table 2, in both expansion and non-expansion states, sample members had better access to care after Medicaid expansion on most measures, except for visits to mental health providers and specialists. For all 3 racial/ethnic groups, there were decreases in unadjusted uninsured rates and increases in unadjusted rates of Medicaid coverage after the expansion, in both expansion and non-expansion states. Figure 1 show the quarterly trends of the unadjusted rates of the uninsured for all adults aged 19 to 64 with income below 138% of the FPL.
Table 2.
Unadjusted Differences in Outcomes before and after the ACA Medicaid Expansion for Expansion and Non-expansion states Among Non-elderly, Low-income Adults.
| All low–income adults | Low–income White adults | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Expansion states | Non-expansion states | Expansion states | Non-expansion states | |||||||||
| Before | After | Before | After | Before | After | Before | After | |||||
| Sample size† | 21 303 | 17 933 | 16 070 | 11 098 | N/A | N/A | N/A | N/A | ||||
| No insurance | 0.35 (0.48) | 0.18 (0.38) | −0.17*** | 0.46 (0.5) | 0.35 (0.48) | −0.11*** | 0.34 (0.47) | 0.17 (0.38) | −0.17*** | 0.43 (0.5) | 0.33 (0.47) | −0.10*** |
| Medicaid | 0.28 (0.45) | 0.45 (0.5) | 0.17*** | 0.16 (0.37) | 0.21 (0.41) | 0.05*** | 0.23 (0.42) | 0.4 (0.49) | 0.17*** | 0.14 (0.35) | 0.19 (0.39) | 0.05*** |
| No usual source of care | 0.21 (0.41) | 0.15 (0.36) | −0.06*** | 0.27 (0.44) | 0.21 (0.41) | −0.06*** | 0.2 (0.4) | 0.16 (0.37) | −0.04*** | 0.25 (0.43) | 0.19 (0.39) | −0.06*** |
| Delayed care due to cost | 0.21 (0.41) | 0.14 (0.35) | −0.07*** | 0.24 (0.43) | 0.19 (0.4) | −0.05*** | 0.24 (0.42) | 0.17 (0.38) | −0.07*** | 0.27 (0.45) | 0.22 (0.41) | −0.05*** |
| Unmet need for medical care | 0.18 (0.39) | 0.12 (0.32) | −0.06*** | 0.22 (0.41) | 0.18 (0.39) | −0.04*** | 0.2 (0.4) | 0.14 (0.35) | −0.06*** | 0.23 (0.42) | 0.2 (0.4) | −0.03*** |
| Unmet need for mental health care | 0.07 (0.25) | 0.04 (0.2) | −0.03*** | 0.07 (0.25) | 0.06 (0.23) | −0.01** | 0.08 (0.27) | 0.05 (0.22) | −0.03*** | 0.08 (0.27) | 0.07 (0.26) | −0.01 |
| Unmet need for specialty care | 0.12 (0.32) | 0.08 (0.27) | −0.04*** | 0.14 (0.34) | 0.11 (0.32) | −0.03*** | 0.12 (0.33) | 0.09 (0.28) | −0.03*** | 0.15 (0.36) | 0.12 (0.32) | −0.03*** |
| No visits to physician | 0.43 (0.5) | 0.37 (0.48) | −0.06*** | 0.46 (0.5) | 0.44 (0.5) | −0.02** | 0.42 (0.49) | 0.34 (0.47) | −0.08*** | 0.43 (0.5) | 0.42 (0.49) | −0.01 |
| No visits to mental health providers | 0.87 (0.33) | 0.87 (0.34) | 0.00 | 0.91 (0.29) | 0.9 (0.31) | −0.01* | 0.85 (0.36) | 0.84 (0.36) | −0.01 | 0.88 (0.32) | 0.87 (0.34) | −0.01 |
| No visits to specialists | 0.81 (0.39) | 0.79 (0.41) | −0.02** | 0.82 (0.38) | 0.83 (0.38) | 0.01 | 0.79 (0.41) | 0.76 (0.43) | −0.03*** | 0.79 (0.41) | 0.81 (0.4) | 0.02 |
| Low–income Black adults | Low–income Hispanic adults | |||||||||||
| Expansion states | Non-expansion states | Expansion states | Non-expansion states | |||||||||
| Before | After | Before | After | Before | After | Before | After | |||||
| Sample sizea | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | ||||
| No insurance | 0.35 (0.48) | 0.19 (0.39) | −0.16*** | 0.45 (0.5) | 0.33 (0.47) | −0.12*** | 0.37 (0.48) | 0.18 (0.39) | −0.19*** | 0.55 (0.5) | 0.43 (0.49) | −0.12*** |
| Medicaid | 0.37 (0.48) | 0.51 (0.5) | 0.14*** | 0.22 (0.42) | 0.28 (0.45) | 0.06*** | 0.36 (0.48) | 0.53 (0.5) | 0.17*** | 0.14 (0.34) | 0.17 (0.37) | 0.03*** |
| No usual source of care | 0.22 (0.41) | 0.14 (0.35) | −0.08*** | 0.24 (0.43) | 0.2 (0.4) | −0.04*** | 0.24 (0.43) | 0.16 (0.37) | −0.08*** | 0.38 (0.49) | 0.3 (0.46) | −0.08*** |
| Delayed care due to cost | 0.19 (0.39) | 0.12 (0.33) | −0.07*** | 0.21 (0.41) | 0.16 (0.37) | −0.05*** | 0.17 (0.38) | 0.09 (0.29) | −0.08*** | 0.19 (0.39) | 0.19 (0.39) | 0.00 |
| Unmet need for medical care | 0.18 (0.39) | 0.11 (0.31) | −0.07*** | 0.21 (0.41) | 0.17 (0.38) | −0.04*** | 0.16 (0.36) | 0.08 (0.27) | −0.08*** | 0.18 (0.38) | 0.16 (0.37) | −0.02 |
| Unmet need for mental health care | 0.05 (0.22) | 0.03 (0.18) | −0.02** | 0.06 (0.24) | 0.04 (0.2) | −0.02** | 0.06 (0.23) | 0.03 (0.18) | −0.03*** | 0.05 (0.21) | 0.04 (0.2) | −0.01 |
| Unmet need for specialty care | 0.1 (0.3) | 0.08 (0.27) | −0.02 | 0.12 (0.33) | 0.1 (0.31) | −0.02 | 0.13 (0.33) | 0.07 (0.25) | −0.06*** | 0.13 (0.33) | 0.13 (0.33) | 0.00 |
| No visits to physician | 0.42 (0.49) | 0.38 (0.49) | −0.04* | 0.48 (0.5) | 0.43 (0.49) | −0.05*** | 0.48 (0.5) | 0.41 (0.49) | −0.07*** | 0.55 (0.5) | 0.49 (0.5) | −0.06** |
| No visits to mental health providers | 0.89 (0.31) | 0.89 (0.31) | 0.00 | 0.93 (0.25) | 0.92 (0.27) | −0.01 | 0.91 (0.28) | 0.91 (0.29) | 0.00 | 0.94 (0.23) | 0.94 (0.23) | 0.00 |
| No visits to specialists | 0.82 (0.39) | 0.82 (0.39) | 0.00 | 0.85 (0.36) | 0.85 (0.35) | 0.00 | 0.85 (0.35) | 0.85 (0.36) | 0.00 | 0.86 (0.34) | 0.85 (0.35) | −0.01 |
Note. Cases were weighted by NHIS final survey weights. Standard deviations are in parentheses.
Sample size varies by outcome.
Sample size varies by outcome.
P < .01. **P < .05. *P < .1. Before and after were defined based on specific month to each state based on expansion date in the expansion states, and in non-expansion states before and after were defined using Jan 2014 as a cutoff.
Figure 1.
Trends of uninsured rate for all low-income adults.
Note. Figure 1 shows the quarterly trends of the unadjusted rates of the uninsured rates for all adults aged 19 to 64 with income below 138% of the FPL.
For White sample members, rates of having no usual source of care and unmet care need due to cost decreased in both groups of states, except for unmet need for mental health care. Among Whites, there were decreases in the proportion having no visits to each provider type examined except mental health providers, but only in expansion states. Among Blacks in both groups of states, there were decreases in the proportion having no usual source of care, unmet need for general and mental health care, and no physician visits. There were no changes in other physician visit outcomes in either group of states. Lastly, among Hispanics, having no usual source of care and having no physician visit decreased in both groups of states. Unmet need for care outcomes changed only in expansion states after Medicaid expansion. In summary, after the 2014 Medicaid expansions, all racial/ethnic groups had generally better access to care in both expansion and non-expansion states.
Multivariate Results
The multivariate DD models indicate that the proportion uninsured declined by an additional 6.5 percentage points (P < .01) in expansion states relative to non-expansion states after ACA Medicaid expansion, controlling for other variables specified in the model (Table 3). Similarly, rates of Medicaid coverage increased by an additional 11.7 percentage points (P < .01). For medical care, mental health care, and specialty health care, rates of unmet need due to cost decreased by an additional 2.6 percentage points (P < .01), 1.2 percentage points (P < .05), and 2.3 percentage points (P < .1), respectively, among sample members after Medicaid expansion in expansion states relative to non-expansion states. Rates of having no visit to a physician decreased by 3.0 percentage points (P < .1) in expansion states relative to non-expansion states.
Table 3.
Effects of the ACA Medicaid Expansion on Disparities in Outcomes Among All Low-income Adults, and for Whites, Hispanics, and Blacks.
| No insurance | Medicaid | No usual source of care | Delayed care due to cost | Unmet need for medical care due to cost | Unmet need for mental health care due to cost | Unmet need for specialty health care due to cost | No visit of physician | No visit of mental health providers | No visit of specialists | |
|---|---|---|---|---|---|---|---|---|---|---|
| Overall (1) | −0.065*** (0.017) | 0.117*** (0.023) | 0.000 (0.015) | −0.020 (0.012) | −0.026*** (0.008) | −0.012** (0.006) | −0.023* (0.012) | −0.030* (0.016) | 0.003 (0.009) | −0.012 (0.012) |
| Whites (2) | −0.060*** (0.019) | 0.111*** (0.019) | 0.014 (0.022) | −0.012 (0.011) | −0.018 (0.011) | −0.020** (0.009) | −0.019 (0.014) | −0.050** (0.021) | 0.008 (0.014) | −0.020 (0.018) |
| Blacks (3) | −0.067*** (0.020) | 0.086*** (0.021) | −0.037 (0.023) | −0.015 (0.017) | −0.027* (0.015) | −0.002 (0.009) | −0.008 (0.021) | 0.010 (0.037) | 0.015 (0.014) | −0.007 (0.018) |
| Hispanics (4) | −0.070*** (0.026) | 0.166*** (0.049) | 0.012 (0.034) | −0.074*** (0.026) | −0.064*** (0.014) | −0.001 (0.009) | −0.045 (0.028) | −0.022 (0.037) | −0.024** (0.011) | 0.000 (0.016) |
| Pre–treatment means | ||||||||||
| Overall | 0.345 (0.476) | 0.283 (0.451) | 0.211 (0.408) | 0.211 (0.408) | 0.184 (0.388) | 0.068 (0.252) | 0.117 (0.322) | 0.432 (0.495) | 0.873 (0.332) | 0.808 (0.394) |
| White | 0.337 (0.473) | 0.233 (0.423) | 0.204 (0.403) | 0.236 (0.425) | 0.197 (0.398) | 0.08 (0.271) | 0.124 (0.329) | 0.417 (0.493) | 0.85 (0.357) | 0.786 (0.41) |
| Blacks | 0.354 (0.478) | 0.372 (0.483) | 0.217 (0.412) | 0.189 (0.392) | 0.185 (0.388) | 0.053 (0.224) | 0.101 (0.302) | 0.424 (0.494) | 0.894 (0.307) | 0.818 (0.386) |
| Hispanics | 0.37 (0.483) | 0.356 (0.479) | 0.237 (0.425) | 0.174 (0.379) | 0.158 (0.365) | 0.056 (0.23) | 0.126 (0.332) | 0.482 (0.5) | 0.912 (0.283) | 0.855 (0.353) |
| Sample size (overall) | 66 404 | 66 404 | 33 346 | 67 341 | 67 323 | 33 270 | 29 369 | 33 143 | 33 177 | 33 160 |
Note. Marginal effects and standard errors are in parentheses. For overall sample, regressions control for age, gender, race, education, marital status, employment status, family size, number of child, functional limitation, fair/poor health status, K-6, rural/urban residence, unemployment rate, state-fixed effects, and quarter/year-fixed effects. For each racial/ethnic group, regressions control for unemployment rate, state-fixed effects, and quarter/year-fixed effects and the health care need index.
Pre-treatment means are the weighted mean of outcomes before the ACA Medicaid was implemented in the expansion states and standard deviations are in parentheses.
P < .01. **P < .05. *P < .1.
Similar patterns were observed when examining expansion impacts separately by racial/ethnic groups, after adjusting health care need variables for race/ethnicity. There were greater decreases in uninsured rates in expansion states than elsewhere for every race/ethnicity group: among White (−6.0 percentage points, P < .01), Black (−6.7 percentage points, P < .01), and Hispanic sample members (−7.0 percentage points, P < .01). There were increases in Medicaid coverage in expansion states among White (11.1 percentage points, P < .01), Black (8.6 percentage points, P < .01), and Hispanic sample members (16.6 percentage points, P < .01). In addition, among White sample members, expansion states saw larger decreases in rates of unmet need for mental health care due to cost (−2.0 percentage points, P < .05) and in having no visit to a physician (−5.0 percentage points, P < .05). Black adults in expansion states experienced larger decreases in unmet need for medical care (2.7 percentage points more, P < .05), compared to those in non-expansion states. Among Hispanics, those in expansion states had larger decreases in rates of delayed care due to cost (−7.4 percentage points, P < .01), unmet need for medical care due to cost (−6.4 percentage points, P < .01), and no visits to mental health providers (−2.4 percentage points, P < .05), all relative to non-expansion states. No statistically significant impacts of Medicaid expansion were found for other access outcomes among all racial/ethnic groups.
Table 4 showed unadjusted racial/ethnic disparities before and after the ACA Medicaid expansion, and unadjusted and adjusted changes in the disparities. For several outcomes there were changes in disparities that differed significantly between expansion and non-expansion states. As with the unadjusted DD results, there was modest evidence of decreases in the Hispanic-White disparities in having delayed care (by 6.2 percentage points, P < .01) and in unmet need for medical care due to cost (by 4.6 percentage points, P < .05). In addition, the Hispanic-White disparity in the proportion having no visit to a mental health provider decreased by 3.3 percentage points (P < .05), which is greater than the unadjusted DD result. The estimated results provided no evidence that Medicaid expansion reduced racial/ethnic disparities in uninsured rates through 2016, although large gains in Medicaid coverage were found for sample members of all race/ethnic groups in expansion states. The estimated change in Black-White disparities was not statistically significant for any outcome.
Table 4.
Disparities Pre- and Post-ACA Medicaid Expansion and the Effect of Medicaid Expansion on Disparities Among Non-elderly, Low-income Adults.
| Expansion states | Non-expansion states | Unadjusted DID | Adjusted DID | ||||
|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | ||||
| No insurance | B–W | 0.017* | 0.015 | 0.02** | 0.004 | 0.015 | −0.006 |
| H–W | 0.033*** | 0.011 | 0.122*** | 0.095*** | 0.004 | −0.009 | |
| Medicaid | B–W | 0.139*** | 0.112*** | 0.082*** | 0.094*** | −0.040** | −0.025 |
| H–W | 0.123*** | 0.139*** | −0.006 | −0.02 | 0.030 | 0.055 | |
| No usual source of care | B–W | 0.013 | −0.017 | −0.012 | 0.004 | −0.045 | −0.051 |
| H–W | 0.033** | 0.003 | 0.131*** | 0.104*** | −0.003 | −0.002 | |
| Delayed care due to cost | B–W | −0.047*** | −0.053*** | −0.065*** | −0.06*** | −0.012 | −0.003 |
| H–W | −0.062*** | −0.079*** | −0.081*** | −0.034*** | −0.064** | −0.062*** | |
| Unmet need for medical care | B–W | −0.012 | −0.03*** | −0.018** | −0.022** | −0.014 | −0.009 |
| H–W | −0.039*** | −0.062*** | −0.055*** | −0.032*** | −0.047** | −0.046** | |
| Unmet need for mental health care | B–W | −0.027*** | −0.019*** | −0.018** | −0.03*** | 0.020** | 0.017 |
| H–W | −0.024*** | −0.018*** | −0.032*** | −0.027** | 0.002 | 0.019 | |
| Unmet need for specialty care | B–W | −0.023** | −0.005 | −0.029** | −0.013 | 0.001 | 0.011 |
| H–W | 0.002 | −0.021** | −0.025 | 0.01 | −0.060** | −0.025 | |
| No visits to physician | B–W | 0.007 | 0.04** | 0.047*** | 0.005 | 0.075* | 0.059 |
| H–W | 0.065*** | 0.063*** | 0.118*** | 0.071*** | 0.044 | 0.027 | |
| No visits to mental health providers | B–W | 0.044*** | 0.05*** | 0.048*** | 0.052*** | 0.001 | 0.006 |
| H–W | 0.062*** | 0.065*** | 0.058*** | 0.076*** | −0.014 | −0.033** | |
| No visits to specialists | B–W | 0.032*** | 0.062*** | 0.06*** | 0.048*** | 0.042* | 0.013 |
| H–W | 0.069*** | 0.091*** | 0.074*** | 0.047** | 0.050** | 0.021 | |
Note. Cases were weighted by NHIS final survey weights. Before and after were defined based on specific month to each state based on expansion date in the expansion states, and in non-expansion states before and after were defined using Jan 2014 as a cutoff. Unadjusted DID were the changes in racial/ethnic disparities in expansion states after expansion, compared to those in non-expansion expansion states. Adjusted DID were estimated using stratified regressions by each race/ethnicity and seemingly unrelated estimation, controlling for unemployment rate, state-fixed effects, and quarter/year-fixed effects and the health care need index.
B-W denotes Black minus White. H-W denotes Hispanic minus White.
P < .01. **P < .05. *P < .1.
The estimates of racial/ethnic disparities were generally similar under the NAM definition compared with the residual direct (RDE) estimates (see Supplemental Table S5a).
Parallel Trend Assumption Test
The results of the joint statistical tests support the parallel trend assumption for all models for all low-income adults, and separately for Whites, and Blacks (Supplemental Table S2a-c). Among low-income Hispanics, with the exception of the models for uninsured rates, delayed care due to cost, and unmet mental health care due to cost, statistical tests supported the parallel trend assumption (Supplemental Table S2d).
Sensitivity Analysis
We estimated sensitivity of our results to varying definitions of treatment and control groups, by excluding (1) states that fully expanded their Medicaid program before 2014 (DE, DC, MA, NY, VT); (2) states that expanded their Medicaid program with full or partial benefit packages (AZ, CA, CT, DC, DE, HI, IA, MA, ME, MN, NY, VT, WA, WI); (3) Wisconsin; (4) states that expanded their Medicaid program after January 2014 (AK, NH, PA, IN, MO, LA), and (5) Louisiana. Although the coefficient estimates were generally larger in the sensitivity analysis, overall the empirical results were very robust to these changes (see Supplemental Appendix and Table S3a). There might be the possibility of the impact of the ACA dependent mandate provision, as of September 23, 2010, allowed young adults aged 19 to 25 to remain their parents’ insurance coverage and the possibility that the ACA subsidy has impact on insurance status for people with 100% to 138% FPL in non-expansion state. The estimated changes among low-income adults aged 26 to 64 were, on average, a little larger in absolute values for rates of uninsured, Medicaid coverage, and physician visits than for those aged 19 to 64 (Supplemental Table S3b). When the sample was limited to adults with income less than 100% of the FPL and childless adults, the estimated Medicaid effects were larger on rates of the uninsured, delayed care and unmet care needs due to cost, than the change in our full sample (adults with income less than 138% of the FPL) (Supplemental Table S3b). Low-income childless adults were more likely to experience significant insurance gain after the expansion than the overall low-income population, since low-income childless adults, as distinct from poor parents, were not generally eligible for Medicaid before the expansion regardless of their income (Supplemental Table S3b).
Discussion
This study adds to a growing literature seeking to evaluate the ACA’s impact on racial/ethnic disparities in access to health care.10,23,24 Specific contributions of this study include the use of data from the first 3 years of the 2014 ACA Medicaid expansion, examination of a wide variety of access outcomes in NHIS national survey data, and the use of quasi-experimental design and the “seemingly unrelated equations” estimation method to estimate the effect of Medicaid expansion on disparities. In addition, this study builds on the existing ACA literature by adding new findings about whether Medicaid expansion has mitigated any disparities in access to care among racial/ethnic groups and by using the NAM definition of disparities
Insurance Status
This study found evidence of reductions in the rates of uninsured and increases in Medicaid coverage for all racial/ethnic groups among nonelderly, low-income adults in expansion states, beyond what was observed in non-expansion states. The expansion is estimated to have increased rates of Medicaid coverage by 12 percentage points, with larger gains for Hispanics (17 points) than for Whites (11 points) and Blacks (9 points) but the group differences were not statistically significant. The results regarding insurance coverage for these groups are consistent with the findings of previous research. 10,11,15,18,19,23,24 This study found that the insurance gap between non-Whites and Whites remained largely unchanged after Medicaid expansion, despite the substantial gains in insurance coverage for all racial/ethnic groups. In contrast, past research on this question showed mixed findings. Similar to our findings, some studies found no statistically significant differences by racial/ethnic group in the change in insurance status over time.19,23 Other studies found that in expansion states there were greater reductions in uninsured rates among Hispanics and Blacks relative to Whites.10,15,18 Another study showed that the gap in uninsured rates between Whites and Hispanics increased after Medicaid expansion, however.24 These differences in findings might result from the shorter post-ACA periods in previous studies. In supplementary analyses estimating effects for 2014 through 2016 (see Supplemental Table S2a-d), only Whites showed decreases in uninsured rates in 2015 and 2016 relative to 2013. Accordingly, adding more recent years of data with more favorable effects on Whites’ insurance coverage may have reduced estimated post-expansion period disparities and their statistical significance.
Access to Care
This study found that Medicaid expansion has more favorable impacts on potential access than health care utilization. This is not surprising, as potential access includes financial barriers to access, which are expected to be directly affected by the coverage expansion.29,51 The expansion was associated with favorable changes in the proportion uninsured and the proportion covered by Medicaid, although not in the proportion with a usual source of care. On the one hand, rates of delayed care and unmet need for care due to cost significantly decreased, mitigating Hispanic-White disparities in those outcomes. On the other hand, this study found less favorable impacts of the Medicaid expansion on other measures of health care utilization such as having a physician visit, which did not improve after expansion. Since insurance coverage is presumably the “pathway” through which Medicaid expansion would affect access to care, it is plausible that we found more favorable impacts on potential access related to financial barriers. Previous studies found decreases in unmet need for care due to cost but no improvement in having a usual source of care,26,32,34 while other studies found favorable impacts on both outcomes.10,13,23,24 Similarly, findings on health care utilization are mixed. Some studies found that visiting physicians and having annual check-up increased after the ACA Medicaid expansion,12,23,32 while other studies did not find any improved health care utilization.13,26,33
This study found that the coverage expansion affected insurance coverage similarly across race/ethnic groups, but the effects on other access measures were different across those groups, in ways that decreased disparities. Potential access other than insurance coverage improved more for Blacks and Hispanics, but health care utilization improved more for Whites. A few prior studies have compared the ACA impact on access to care across race/ethnicity, with mixed findings. By comparison, findings on access to care were mixed in prior studies of this question. One study found that racial/ethnic differences in difficulty in access to medications decreased10 while there were no statistically significant changes in the racial/ethnic disparities in having no usual source of care and in unmet need for care due to cost.10,23,24 These different findings on ACA impacts on access to care might also come from variations among studies in the length of post-ACA period, data sources, and study sample. Overall, the magnitude and significance of effects on access outcomes is greater in 2016 than in 2014 or 2015 for all racial/ethnic groups. The effects of the ACA on health care access estimated using the NHIS are generally smaller than those using the BRFSS.52 In addition, the estimated changes in access to care were larger for adults without dependent children, presumably because this group was previously ineligible.
These differences in impact by race/ethnicity may be due to other pathways through which the Medicaid expansion could have affected access and disparities. Contextual enabling factors, such as the availability of primary care providers, residential segregation, lack of minority workforce, and policy interventions other than Medicaid, and individual predisposing and enabling factors, such as patient activation and distrust in physicians could still remain as non-financial barriers to access to care. The availability of physicians is an important determinant of physician visits. According to the federal Health Resources and Services Administration (HRSA), in 2019 79 million people lived in Primary Care Health Professional Shortage Areas, where ratios of population to primary care practitioners are greater than 2000:1.53 People living in inner-city and rural communities with large racial and ethnic minority patient populations typically face greater difficulties in visiting physicians. Moreover, the segregated neighborhoods of Blacks and Hispanics, characterized as economically and socially disadvantaged, are more likely to have the lower quality of care, clinical, logistical, and administrative challenges and lack of resources attracting health care providers.54 The under-representation of racial/ethnic minorities among health care professionals also affects the use of medical services among Hispanics and Blacks, since patient-physician racial/ethnic concordance has been associated with higher patient satisfaction.55,56
The decrease in unmet need for care that we identified could have resulted from policies other than the Medicaid expansion, such as the Mental Health Parity and Addiction Equity Act (MHPAEA). The MHPAEA prohibited financial requirements for mental health and substance use benefits greater than for medical and surgical benefits and eliminated treatment and visit limits. It was implemented starting in 2010 for most private and employer health insurance plans, and from March 2016 on for Medicaid. The Medicaid expansion under the ACA potentially interacted with the MHPAEA to increase the access to mental health care, since the adults newly eligible for Medicaid would benefit from the prohibition of higher copayments.57,58
Moreover, even after obtaining health insurance coverage, poor individuals may not have been able to reduce their unmet need for care, for example due to their income level remaining too low to obtain medical services. State Medicaid programs can impose copayments, coinsurance, and deductibles although maximum allowable out of pocket costs for Medicaid beneficiary are very low. For example, while the maximum allowable copayment for inpatient hospital care is $75 per admission for family with income below 100% of the FPL in 2013,59,iii this amount may still represent a burden for individuals and families facing severe economic hardship. Moreover, low-income residents in rural areas would face additional transportation costs, given lesser availability of physicians and hospitals in those areas.
One important implication for policy makers is that there remain racial/ethnic disparities in insurance coverage and access to care within low-income populations. Although the Medicaid expansion decreased the gap in Medicaid coverage between low-income Hispanics and Whites, Hispanics are still the most commonly uninsured (30.0%), and Blacks (28.7%) are more likely to be uninsured than Whites (27.4%). Racial/ethnic disparities in having any physician visits did not change after the expansion, while non-Hispanic Whites showed an increase in the proportion with physician visits. There should be continuous efforts and follow-up policies in addition to coverage expansion in order to mitigate health care disparities among racial/ethnic groups. Further, as these findings suggest, it may be necessary to implement different strategies for Blacks and Hispanics considering other factors such as racial/ethnic differences in health status and health behaviors.
Future research is warranted to evaluate states’ waiver programs in both expansion and non-expansion states. States can test new approaches in their Medicaid programs by applying for “Section 1115” waivers from CMS. As of March 2018, there are 36 states with approved waivers and 23 states with pending waivers.60 These approved and pending waivers contain eligibility and enrollment restrictions, work requirements, benefit restrictions, requirements of copays and healthy behaviors, and delivery system reforms.60 Any of these could interact with Medicaid expansion to affect individuals’ potential or health care utilization to care. Future studies should therefore research how these state waivers are different than the 2014 Medicaid expansion on eligibility, and whether these waivers differentially affect insurance status, access to care, and health status among racial/ethnic minorities.61
Several limitations in our difference in differences (DD) approach need to be acknowledged. First, the design of this study was quasi-experimental, since the Medicaid expansion was not randomly assigned across states. Unobserved factors such as policy changes other than Medicaid expansion could have caused confounding effects on outcomes. Second, the DD design assumes that treatment and control groups would have had a parallel trend of outcome measures in absence of the expansion. Although most of tests indicated that this parallel trend assumption was not violated, unobserved time-varying characteristics might nonetheless be different between expansion and non-expansion states.38 Third, difference-in-differences estimation could have potential bias due to serial correlation across multiple years of data, as the conventional DD approach may understate standard errors, resulting in over-rejection of the null hypothesis of no effect.62 Fourth, since available measures of insurance status and Medicaid only captures capture respondents’ coverage status at the time of the interview, the insurance status of some respondents may differ before and after the interview. Fifth, there is variation in Medicaid eligibility among states, over time, and by category such as pregnant women or individuals with disabilities. Our study only estimated the average overall effect of Medicaid expansion rather than effects by state or eligibility category, which is beyond the scope of this study. Sixth, although findings concerning the impact of Medicaid expansion on self-reported health status have been mixed, self-reported health status can be affected by Medicaid expansion,63 resulting in a potential endogeneity problem. However, we did not find a change in self-reported status after the expansion in our study sample (data not shown), suggesting that for this sample endogeneity is not a serious concern. Seventh, we acknowledge the potential concern for some Type 1 errors given the large number of statistical tests performed. However, we note that the results we highlight were often consistently significant across more than 1 specification, allaying this concern somewhat. For example, Medicaid expansion was associated with an access-improvement for 6 of 10 outcomes studied; and it was associated specifically with lower uninsured rates for all 3 race/ethnicity groups examined.
Conclusion
This study found that among low-income non-elderly adults, Medicaid expansion was associated with significant decreases in uninsured rates and increases in Medicaid coverage. This study also found that while the Medicaid expansion affected insurance coverage similarly across race/ethnic groups, the effects on other measures of access were different across racial/ethnic groups. Among Blacks and Hispanics, there were more favorable impacts on potential access measures such as unmet need for care, while among Whites there were more favorable impacts on health care utilization. In conclusion, the ACA Medicaid expansion has more favorable impacts on racial/ethnic minorities for unmet need for care due to cost but not for physician visits. However, there is limited evidence from the NHIS data and analyses that the ACA Medicaid expansion is associated with significant or widespread reductions in health disparities according to the NAM definitions. These findings suggest a need for continuous monitoring of policy impacts, as well as research into the pathways through which Medicaid expansion affects access to care and mitigates health care disparities among racial/ethnic groups.
Supplemental Material
Supplemental material, sj-pdf-1-inq-10.1177_0046958021991293 for Medicaid Expansion and Racial and Ethnic Disparities in Access to Health Care: Applying the National Academy of Medicine Definition of Health Care Disparities by Hyunjung Lee, Dominic Hodgkin, Michael P. Johnson and Frank W. Porell in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Acknowledgments
The support of the Office of Graduate Studies at UMass Boston, the Federal Statistical Research Data Center (RDC), and National Center for Health Statistics RDC Analyst are acknowledged. The authors would like to thank Dr. Jerry Cromwell, and Dr. Hefei Wen for their helpful comments on the original research proposal for this study.
A total of 19 470 127 of Medicaid enrollees are from non-expansion states, which is 29.3% of total Medicaid enrollees (66 346 562) for October 2018. Retrieved October 2018, from https://www.medicaid.gov/medicaid/program-information/medicaid-and-chip-enrollment-data/report-highlights/index.html
The standard errors from suest will be slightly smaller than those from individual model using vce (robust) option because suest uses a large number of observations to estimate the simultaneous (co) variance matrix (StataCorp, 2013).
Maximum allowable copayment of hospital inpatient care for family with income between 101%FPL and 150%FPL is 10% of the cost that the agency pays for the entire state and 20% for family with income below 150% FPL. Retrieved September, 2018, from https://www.medicaid.gov/medicaid/cost-sharing/out-of-pocket-costs/index.html
Footnotes
Authors’ Contributions: Dr. Lee conceptualized and designed the study, performed the statistical analyses, and developed all tables and graphs, and drafted and revised the manuscript. Drs. Hodgkin, Johnson, and Porell reviewed, and revised the manuscript. All authors critically reviewed the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Disclaimer: The views expressed in this publication are solely the opinions of the authors and do not necessarily reflect the official policies of ORISE, UMass Boston, or Brandeis University, nor does mention of the department or agency names imply endorsement by the U.S. Government. The research in this paper was conducted at the Federal Statistical Research Data Center (RDC).
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by the Doctoral Dissertation Research Grant Program of UMass Boston.
ORCID iD: Hyunjung Lee  https://orcid.org/0000-0003-0783-5484
https://orcid.org/0000-0003-0783-5484
Supplemental Material: Supplemental material for this article is available online.
References
- 1. CDC. CDC Health disparities and inequalities report – United States, 2013. (CDC) C for DC and P, ed. MMWR 2013;2013(62):1-189. [PubMed] [Google Scholar]
- 2. Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32(1):20-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kochanek KD, Murphy SL, Xu J, Arias E. Deaths: final data for 2017. Natl Vital Stat Rep. 2019;68(9):1-77. [PubMed] [Google Scholar]
- 4. Agency for Healthcare Research and Quality. 2018 National Healthcare Quality and Disparities Report. Agency for Healthcare Research and Quality; 2019. [Google Scholar]
- 5. Smedley BD, Stith AY, Nelson AR. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care (Full Printed Version). National Academies Press; 2002. [PubMed] [Google Scholar]
- 6. Lê Cook B, McGuire TG, Lock K, Zaslavsky AM. Comparing methods of racial and ethnic disparities measurement across different settings of mental health care. Health Serv Res. 2010;45(3):825-847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cook BL, McGuire TG, Zaslavsky AM. Measuring racial/ethnic disparities in health care: methods and practical issues. Health Serv Res. 2012;47(3 pt 2):1232-1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kominski GF, Nonzee NJ, Sorensen A. The affordable care act’s impacts on access to insurance and health care for low-income populations. Annu Rev Public Health. 2017;38:489-505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Brooks T, Miskell S, Artiga S, Cornachione E, Gates A. Medicaid and CHIP Eligibility, Enrollment, Renewal, and Cost-Sharing Policies as of January 2016: Findings from a 50-State Survey. The Henry J. Kaiser Family Foundation; 2016. Heal Care Cover Maps”(NILC, Revis Aug 13, 2018). 2016. [Google Scholar]
- 10. Sommers BD, Gunja MZ, Finegold K, Musco T. Changes in self-reported insurance coverage, access to care, and health under the Affordable Care Act. JAMA. 2015;314(4):366-374. [DOI] [PubMed] [Google Scholar]
- 11. Dworsky M, Eibner C. The Effect of the 2014 Medicaid Expansion on Insurance Coverage for Newly Eligible Childless Adults. RAND; 2016. [Google Scholar]
- 12. Wherry LR, Miller S. Early coverage, access, utilization, and health effects associated with the Affordable Care Act Medicaid expansions: a quasi-experimental study. Ann Intern Med. 2016;164(12):795-803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Simon K, Soni A, Cawley J. The impact of health insurance on preventive care and health behaviors: evidence from the first two years of the ACA Medicaid expansions. J Policy Anal Manag. 2017;36(2):390-417. [DOI] [PubMed] [Google Scholar]
- 14. Courtemanche C, Marton J, Ukert B, Yelowitz A, Zapata D, Fazlul I. The three-year impact of the Affordable Care Act on disparities in insurance coverage. Health Serv Res. 2019;54(suppl 1):307-316. doi: 10.1111/1475-6773.13077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. McMorrow S, Long SK, Kenney GM, Anderson N. Uninsurance disparities have narrowed for black and hispanic adults under the affordable care act. Health Aff. 2015;34(10):1774-1778. [DOI] [PubMed] [Google Scholar]
- 16. Sommers BD, Chua K, Kenney GM, Long SK, McMorrow S. California’s early coverage expansion under the affordable care act: a county-level analysis. Health Serv Res. 2016;51(3): 825-845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Buchmueller TC, Levinson ZM, Levy HG, Wolfe BL. Effect of the Affordable Care Act on racial and ethnic disparities in health insurance coverage. Am J Public Health. 2016;106(8): 1416-1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Courtemanche C, Marton J, Ukert B, Yelowitz A, Zapata D. Early impacts of the affordable care act on health insurance coverage in medicaid expansion and non-expansion states. J Policy Anal Manag. 2017;36(1):178-210. doi: 10.1002/pam.21961 [DOI] [PubMed] [Google Scholar]
- 19. Decker SL, Lipton BJ, Sommers BD. Medicaid expansion coverage effects grew in 2015 with continued improvements in coverage quality. Health Aff. 2017;36(5):819-825. [DOI] [PubMed] [Google Scholar]
- 20. Buchmueller TC, Levy HG. The ACA’s impact on racial and ethnic disparities in health insurance coverage and access to care: an examination of how the insurance coverage expansions of the Affordable Care Act have affected disparities related to race and ethnicity. Health Aff. 2020;39(3):395-402. [DOI] [PubMed] [Google Scholar]
- 21. Wehby GL, Lyu W. The impact of the ACA Medicaid expansions on health insurance coverage through 2015 and coverage disparities by age, race/ethnicity, and gender. Health Serv Res. 2018;53(2):1248-1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Chen J, Vargas-Bustamante A, Mortensen K, Ortega AN. Racial and ethnic disparities in health care access and utilization under the Affordable Care Act. Med Care. 2016;54(2):140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lee H, Porell FW. The effect of the affordable care act medicaid expansion on disparities in access to care and health status. Med Care Res Rev. 2020;77(5):461-473. [DOI] [PubMed] [Google Scholar]
- 24. Yue D, Rasmussen PW, Ponce NA. Racial/ethnic differential effects of medicaid expansion on health care access. Health Serv Res. 2018;53(5):3640-3656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Creedon TB, Cook BL. Access to mental health care increased but not for substance use, while disparities remain. Health Aff. 2016;35(6):1017-1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Courtemanche C, Marton J, Ukert B, Yelowitz A, Zapata D. Early effects of the Affordable Care Act on health care access, risky health behaviors, and self-assessed health. South Econ J. 2018;84(3):660-691. [Google Scholar]
- 27. Mort EA, Edwards JN, Emmons DW, Convery K, Blumenthal D. Physician response to patient insurance status in ambulatory care clinical decision-making: implications for quality of care. Med Care. 1996;34(8):783-797. [DOI] [PubMed] [Google Scholar]
- 28. Andersen RM, McCutcheon A, Aday LA, Chiu GY, Bell R. Exploring dimensions of access to medical care. Health Serv Res. 1983;18(1):49. [PMC free article] [PubMed] [Google Scholar]
- 29. Aday LA, Andersen R. A framework for the study of access to medical care. Health Serv Res. 1974;9(3):208 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1071804/pdf/hsresearch00560-0030.pdf. [PMC free article] [PubMed] [Google Scholar]
- 30. Antonisse L, Garfield R, Rudowitz R, Artiga S. The effects of Medicaid expansion under the ACA: updated findings from a literature review. 2018. Henry J. Kaiser Family Foundation (KFF). 2018 March. http://files.kff.org/attachment/Issue-Brief-The-Effects-of-Medicaid-Expansion-Under-the-ACA-Updated-Findings-from-a-Literature-Review
- 31. Kaestner R, Garrett B, Chen J, Gangopadhyaya A, Fleming C. Effects of ACA Medicaid expansions on health insurance coverage and labor supply. J Policy Anal Manag. 2017;36(3):608-642. [DOI] [PubMed] [Google Scholar]
- 32. Miller S, Wherry LR. Health and access to care during the first 2 years of the ACA Medicaid expansions. N Engl J Med. 2017;376(10):947-956. [DOI] [PubMed] [Google Scholar]
- 33. McMorrow S, Gates JA, Long SK, Kenney GM. Medicaid expansion increased coverage, improved affordability, and reduced psychological distress for low-income parents. Health Aff. 2017;36(5):808-818. [DOI] [PubMed] [Google Scholar]
- 34. Selden TM, Lipton BJ, Decker SL. Medicaid expansion and Marketplace eligibility both increased coverage, with trade-offs in access, affordability. Health Aff. 2017;36(12):2069-2077. [DOI] [PubMed] [Google Scholar]
- 35. Andersen PL, Davidson RM, Baumeister SE. Improving access to care in America. In: Changing the US Health Care System: Key Issues in Health Services Policy and Management. 3a ed. John Wiley & Sons; 2013. [Google Scholar]
- 36. Manning WG, Newhouse JP, Duan N, Keeler EB, Leibowitz A, Marquis MS. Health insurance and the demand for medical care: evidence from a randomized experiment. Am Econ Rev. 1987;77(3):251-277. [PubMed] [Google Scholar]
- 37. Hulka BS, Wheat JR. Patterns of utilization: the patient perspective. Med Care. 1985;23(5):438-460. [DOI] [PubMed] [Google Scholar]
- 38. Angrist JD, Pischke J-S. Mostly Harmless Econometrics: An Empiricist’s Companion. Princeton university press; 2008. [Google Scholar]
- 39. McGuire TG, Alegria M, Cook BL, Wells KB, Zaslavsky AM. Implementing the Institute of Medicine definition of disparities: an application to mental health care. Health Serv Res. 2006;41(5):1979-2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Lê Cook B, McGuire TG, Zuvekas SH. Measuring trends in racial/ethnic health care disparities. Med Care Res Rev. 2009; 66(1):23-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Cook BL, McGuire T, Miranda J. Measuring trends in mental health care disparities, 2000–2004. Psychiatr Serv. 2007; 58(12):1533-1540. [DOI] [PubMed] [Google Scholar]
- 42. Cook BL, McGuire TG, Meara E, Zaslavsky AM. Adjusting for health status in non-linear models of health care disparities. Heal Serv Outcomes Res Methodol. 2009;9(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Hunt JB, Eisenberg D, Lu L, Gathright M. Racial/ethnic disparities in mental health care utilization among US college students: applying the institution of medicine definition of health care disparities. Acad Psychiatry. 2015;39(5):520-526. [DOI] [PubMed] [Google Scholar]
- 44. Biener AI, Zuvekas SH. Do racial and ethnic disparities in health care use vary with health? Health Serv Res. 2019;54(1): 64-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Cook BL, Zuvekas SH, Carson N, Wayne GF, Vesper A, McGuire TG. Assessing racial/ethnic disparities in treatment across episodes of mental health care. Health Serv Res. 2014; 49(1):206-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Fiebig DG. Seemingly unrelated regression. In: Baltagi B, ed. A companion to Theoretical Econometrics. Blackwell; 2001:101-121. [Google Scholar]
- 47. StataCorp. Stata 13 Base Reference Manual. Stata Press; 2013. [Google Scholar]
- 48. Ai C, Norton EC. Interaction terms in logit and probit models. Econ Lett. 2003;80(1):123-129. [Google Scholar]
- 49. Hodgkin D, Merrick EL, Horgan CM, Garnick DW, McLaughlin TJ. Does type of gatekeeping model affect access to outpatient specialty mental health services? Health Serv Res. 2007;42(1 pt 1):104-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. StataCorp. Stata Statistical Software: Release 15. 2017. [Google Scholar]
- 51. Long SK, Coughlin TA, Kendall SJ. Access to care among disabled adults on Medicaid. Health Care Financ Rev. 2002; 23(4):159. [PMC free article] [PubMed] [Google Scholar]
- 52. Glied S, Ma S, Borja AA. Effect of the affordable care act on health care access. Issue Brief (Commonw Fund). 2017;13: 1-11. [PubMed] [Google Scholar]
- 53. Bodenheimer T, Pham HH. Primary care: current problems and proposed solutions. Health Aff. 2010;29(5):799-805. [DOI] [PubMed] [Google Scholar]
- 54. White K, Haas JS, Williams DR. Elucidating the role of place in health care disparities: the example of racial/ethnic residential segregation. Health Serv Res. 2012;47(3 pt 2):1278-1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR. Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann Intern Med. 2003;139(11):907-915. [DOI] [PubMed] [Google Scholar]
- 56. Betancourt JR, Green AR, Carrillo JE, Ananeh-Firempong O., II Defining cultural competence: a practical framework for addressing racial/ethnic disparities in health and health care. Public Health Rep. 2003;118(4):293-302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Goodell S. Enforcing Mental Health Parity. Project HOPE; 2015. [Google Scholar]
- 58. Beronio K, Glied S, Frank R. How the Affordable Care Act and Mental Health Parity and Addiction Equity Act greatly expand coverage of behavioral health care. J Behav Health Serv Res. 2014;41(4):410-428. [DOI] [PubMed] [Google Scholar]
- 59. Medicaid.gov. Cost sharing out of pocket costs. https://www.medicaid.gov/medicaid/cost-sharing/out-of-pocket-costs/index.html. Accessed September, 2018.
- 60. Musumeci M, Rudowitz R, Hinton E, Antonisse L, Hall C. Section 1115 Medicaid Demonstration Waivers: The Current Landscape of Approved and Pending Waivers. Henry J Kaiser Family Foundation; 2019; 28. [Google Scholar]
- 61. Rudowitz R, Musumeci M, Gates A. Medicaid expansion waivers: what will we learn. Kaiser Comm Medicaid Uninsured. 2016. https://www.kff.org/medicaid/issue-brief/medicaid-expansion-waivers-what-will-we-learn/. Accessed April 10, 2018.
- 62. Bertrand M, Duflo E, Mullainathan S. How much should we trust differences-in-differences estimates? Q J Econ. 2004; 119(1):249-275. [Google Scholar]
- 63. Soni A, Wherry LR, Simon KI. How have ACA insurance expansions affected health outcomes? Findings from the literature: a literature review of the Affordable Care Act’s effects on health outcomes for non-elderly adults. Health Aff. 2020;39(3):371-378. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-inq-10.1177_0046958021991293 for Medicaid Expansion and Racial and Ethnic Disparities in Access to Health Care: Applying the National Academy of Medicine Definition of Health Care Disparities by Hyunjung Lee, Dominic Hodgkin, Michael P. Johnson and Frank W. Porell in INQUIRY: The Journal of Health Care Organization, Provision, and Financing