Abstract
Development of pulmonary hypertension (PH) in patients with left side heart disease (LHD) is a predictor of poor prognosis. The use of pulmonary vasodilators in PH associated with LHD (PH-LHD) is controversial. In this study, we describe the practice patterns regarding the use of pulmonary vasodilators in PH-LHD among a group of international pediatric PH specialists. A survey was distributed to the members of three pediatric PH networks: PPHNet, PVRI, and REHIPED. The survey queried participants on the rationale, indications, and contraindications of the use of pulmonary vasodilators in children with PH-LHD. Forty-seven PH specialists from 39 PH centers completed the survey. Participants included PH specialists from North America (57%), South America (15%), and Europe (19%). The majority of participants (74%) recommended the use of pulmonary vasodilators only in patients with combined pre-capillary and post-capillary pulmonary hypertension. Participants required the presence of clinical symptoms or signs of heart failure (68%) or right ventricular dysfunction by echocardiography (51%) in order to recommend pulmonary vasodilator therapy. There was no agreement regarding hemodynamic criteria used to recommend pulmonary vasodilators or the etiologies of LHD considered contraindications for using pulmonary vasodilators to manage PH-LHD. Of the available PH-targeted drugs, most participants preferred the use of phosphodiesterase-5-inhibitors for this indication. In conclusion, the practice of recommending pulmonary vasodilators in PH-LHD is highly variable among international pediatric PH specialists. Most specialists of those surveyed (57% in North America) would consider the use of pulmonary vasodilators in PH-LHD only if pre-capillary pulmonary hypertension and right ventricular dysfunction are present.
Keywords: survey, children, WHO group II pulmonary hypertension, pulmonary vascular disease
Pulmonary hypertension (PH) is a known predictor of poor prognosis in left-sided heart disease (LHD), including mitral and aortic valve disease and heart failure.1–3 PH can develop in all patients with LHD secondary to elevation of the pulmonary venous pressure resulting in passive elevation in pulmonary artery pressure (PAP; isolated post-capillary PH) to maintain the cardiac output.4 In isolated post-capillary PH, the pulmonary artery diastolic pressure is slightly higher than the left atrial pressure (difference <7 mmHg) and the pulmonary vascular resistance is normal (<3 Woods Units (WU)).5 In some patients, the pulmonary arteries, alveolar vessels, and pulmonary veins can remodel resulting in a decrease in pulmonary edema at the expense of further elevation in PAP.6 The pulmonary artery diastolic pressure in these patients is elevated out of proportion to the left atrial pressure (difference 7 mmHg) and the pulmonary vascular resistance is also elevated (3 WU; combined pre-capillary and post-capillary PH).5 The definitions of pre-capillary, post-capillary, and combined pre-capillary and post-capillary PH are shown in Table 1. Low cardiac output, systemic congestion, and right ventricular dysfunction occur in patients with combined pre-capillary and post-capillary PH as a result of increased right ventricular afterload.7 The presence of right ventricular dysfunction in patients with LHD is a poor prognostic marker.8
Table 1.
Definitions of pulmonary hypertension.26
| PH: mPAP >20 mmHg in children >3 months of age at sea level |
|---|
| Pre-capillary PH: |
| mPAP >20 mmHg |
| PAWP or LVEDP ≤15 mmHg |
| PVR index ≥3 WU m2 |
| Diastolic TPG (DPG) ≥7 mmHg (adjunct criterion) |
| Isolated post-capillary PH: |
| mPAP >20 mmHg |
| PAWP or LVEDP >15 mmHg |
| PVR index <3 WU m2 |
| Diastolic TPG (DPG) <7 mmHg (adjunct criterion) |
| Combination of pre-capillary and post-capillary PH |
| mPAP >20 mmHg |
| PAWP or LVEDP >15 mmHg |
| PVR index ≥3 WU m2 |
LVEDP: left ventricular end diastolic pressure; mPAP: mean pulmonary artery pressure; PAWP: pulmonary artery wedge pressure; PH: pulmonary hypertension; PVR: pulmonary vascular resistance; TPG: transpulmonary gradient.
The use of pulmonary vasodilators in the management of PH associated with LHD (PH-LHD) is controversial among adult PH providers.9 In a survey of adult PH referral centers in the United States, 77% of centers prescribed pulmonary vasodilators in patients with PH-LHD.10 The common use of PH-targeted therapies was especially remarkable in the face of strong guideline recommendations from major medical organizations against the use of pulmonary vasodilators in PH-LHD.11 These recommendations stem from the results of clinical trials that showed no clear benefit and possibly increased risks of administering pulmonary vasodilators in the setting of PH-LHD.12–14
The incidence and prevalence of PH in children with LHD is unknown.15Pediatric PH registries have reported 5–14% of included patients having PH-LHD.16,17 The etiologies of LHD in children are different from those in adults, with different implications regarding PH treatment and prognosis.18The effect of elevated pulmonary venous pressure on the alveolo-capillary bed and vascular remodeling are also possibly different with added factors related to lung vascular growth and development, which is absent in adults.19This makes extrapolation of results of clinical trials from adults to children very difficult and likely inappropriate. There are currently no guidelines or consensus statements on management of PH-LHD in children.18 Therefore, to study PH-LHD in pediatric patients, it is important to first establish what are the common current practice patterns in managing these patients among pediatric PH providers. This study aims at identifying the practice patterns of a cohort of international PH specialists regarding the use of pulmonary vasodilators in children with PH-LHD.
Methods
A survey in the form of multiple-choice and open-ended questions was created in Redcap (Supplementary material). The survey questions addressed the practice patterns of PH specialists regarding the use of pulmonary vasodilators in children with PH-LHD. Participants who did not recommend pulmonary vasodilators in PH-LHD did not continue the remainder of the survey. Participants who recommend the use of pulmonary vasodilators in PH-LHD were asked about their rationale for doing so, the indications and contraindications for starting pulmonary vasodilators and the class of pulmonary vasodilators used. All questions inquiring about cutoff thresholds were open-ended questions to avoid any suggestion or anchoring effect. The participants were also asked if their recommendation to treat PH-LHD changed depending on the etiology of LHD and whether the etiology of LHD was reversible.
The survey was distributed in the pediatric sessions at the Pulmonary Vascular Research Institute (PVRI) meeting held in Peru (January 2020), the Spanish PH registry meeting in Madrid (February 2020) and the International Conference of Neonatal and Pediatric Pulmonary Vascular Disease in San Francisco (March 2020). The survey was also distributed via email to the members of three pediatric PH networks: the Pediatric Pulmonary Hypertension Network (PPHNet, collaborative group of 14 pediatric PH centers in North America and Canada), the Pediatric & Congenital Heart Disease Taskforce of the PVRI, and the Spanish Registry of Pediatric Pulmonary Hypertension (REHIPED). The participants received a link to the Redcap survey or a hard copy of the survey if they preferred. The survey was conducted between January 2020 and April 2020.
Statistics
Continuous data were expressed as median and interquartile range and categorical data as frequency and percentages. The mode was calculated for certain variables to express the most common choice of the participants. To evaluate the differences in practice patterns based on the demographics of the participants, we divided the participants into two groups based on the median value of age and years of experience. We also compared the participants’ responses based on the volume of patients managed in their PH practice (<100 patients vs. >100 patients), and according to the continent where they practiced (North America, South America and Europe). Comparisons of the responses based on these demographic groups were performed using the Chi squared test. Statistical analysis was performed using Stata (version 14, College Station, TX); differences were considered significant if p value <0.05.
Results
The survey was sent to 210 potential participants out of which 49 participants attempted and 47 participants (response rate 22%) from 39 centers fully completed the survey. The characteristic demographics of the participants are shown in Table 2. The participants represented a balanced group of international PH specialists in regard to age, years of experience, and volume of patients managed by their practice. On the other hand, the majority (85%) of participants were pediatric cardiologists, practicing in North America (57%) and were involved predominantly in clinical rather than basic science research.
Table 2.
Characteristics of the study participants (n = 47).
| Median (IQR), n (%) | |
|---|---|
| Age (years) | 50 (43,56) |
| Years of experience (years) | 12 (9,20) |
| Hours/week managing PH (h) | 10 (5,20) |
| Volume of practice | |
| Less than 50 patients | 16 (34) |
| 50–100 patients | 11 (23) |
| More than 100 patients | 20 (43) |
| Specialty | |
| Cardiology | 40 (85) |
| Pulmonology | 4 (9) |
| Neonatology | 2 (4) |
| Other | 1 (2) |
| Research type | |
| Not involved in research | 5 (11) |
| Clinical research | 32 (68) |
| Basic science research | 1 (2) |
| Clinical & basic science | 9 (19) |
| Continenta | |
| North America | 27 (57%) |
| United States of America | 23 |
| Mexico | 4 |
| South America | 7 (15%) |
| Columbia | 3 |
| Argentina | 1 |
| Brazil | 1 |
| Ecuador | 1 |
| Peru | 1 |
| Europe | 9 (19%) |
| Spain | 5 |
| Holland | 1 |
| Italy | 1 |
| Sweden | 1 |
| United Kingdom | 1 |
| Asia | 1 (2%) |
| Australia | 1 (2%) |
aTwo participants did not record their location of practice.
Q1: Do you treat PH-LHD with pulmonary vasodilators?
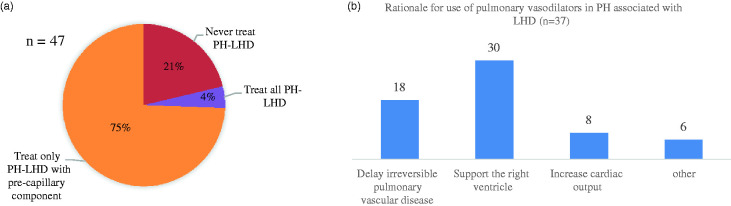
Ten (21%) participants would not recommend pulmonary vasodilators in children with PH-LHD (Fig. 1). For those participants the survey ended. The remainder of the results reflect the views of 37 (79%) of the participants who would prescribe pulmonary vasodilators in children with PH-LHD.
Fig. 1.
Participants’ views regarding the use of pulmonary vasodilators in children with PH-LHD. (a) Pie chart depicting percentage of participants recommending pulmonary vasodilators. (b) Bar chart depicting the different rationale for recommending pulmonary vasodilators.
Q2: Rationale for using pulmonary vasodilators?
The majority of the providers prescribing pulmonary vasodilators to children with PH-LHD would only do so in the presence of pre-capillary PH. The rationale for prescribing pulmonary vasodilators was predominantly to support the right ventricle (81%) and to delay the development of irreversible pulmonary vascular disease (49%). Other reasons noted were to increase cardiac output (22%), to prevent PH crisis and to improve candidacy for heart transplantation.
Q3: Assessments used to decide which patient with PH-LHD to initiate pulmonary vasodilators on?
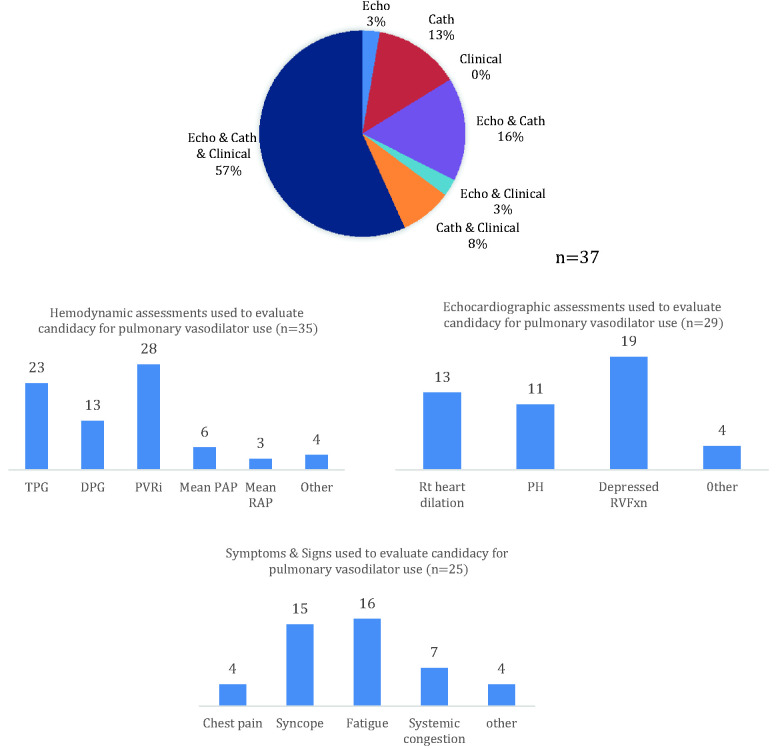
Thirty-four (94%) and 29 (79%) participants who would prescribe pulmonary vasodilators for PH-LHD used the information obtained from a cardiac catheterization or an echocardiogram respectively to decide on prescribing pulmonary vasodilators (Fig. 2). Twenty-five (68%) of participants required patients to be symptomatic prior to prescribing pulmonary vasodilators. Twenty-one (57%) of participants required patients to be symptomatic and obtain an echocardiogram and cardiac catheterization prior to prescribing pulmonary vasodilators in PH-LHD.
Fig. 2.
Assessments used by participants in children with PH-LHD to evaluate their candidacy for pulmonary vasodilators. (a) Pie chart depicting minimal assessments required by participants to recommend pulmonary vasodilators. (b) Hemodynamic criteria used to evaluate the candidacy for pulmonary vasodilators. (c) Echocardiographic criteria used to evaluate the candidacy for pulmonary vasodilators. (d) Clinical criteria used to evaluate the candidacy for pulmonary vasodilators. Cath: cardiac catheterization; DPG: diastolic pulmonary gradient; Echo: echocardiography; PAP: pulmonary artery pressure; PVRi: pulmonary vascular resistance indexed to body surface area; RAP: right atrial pressure; Rt: right; RVFxn: right ventricular function; TPG: mean transpulmonary gradient.
Q4: Hemodynamic parameters used in the decision to initiate pulmonary vasodilators in PH-LHD?
The hemodynamic variables and their cutoff thresholds used to recommend pulmonary vasodilators were not consistent among the participants. Most participants used the pulmonary vascular resistance followed by the mean transpulmonary gradient and diastolic transpulmonary gradient. The range of cutoff thresholds for these three variables was large (3–12 WU, 6–20 mmHg, 5–15 mmHg) and the mode for each variable was (3 WU, 15 mmHg and 7 mmHg), respectively. Of the participants who use cardiac catheterization results to recommend pulmonary vasodilators in PH-LHD, 13 (38%) would not prescribe pulmonary vasodilators if the left atrial mean pressure was greater than 20 mmHg and 8 (24%) would not prescribe pulmonary vasodilators if the left atrial mean pressure was greater than 15 mmHg.
Q5: Does acute vasoreactivity response affect the decision to initiate pulmonary vasodilators?
The participants were split on whether acute vasoreactivity testing was helpful in identifying patients who would benefit from a pulmonary vasodilator. Fifty-nine percent reported that the results of acute vasodilator testing during cardiac catheterization did not help identify patients who would benefit from a pulmonary vasodilator. On the other hand, 41% of participants would prescribe pulmonary vasodilators only if an acute vasodilator test was positive and the left atrial pressure did not significantly increase during the test.
Q6: Echocardiographic parameters used in the decision to initiate pulmonary vasodilators in PH-LHD?
The majority (79%) of participants required the presence of findings on echocardiography prior to recommending a pulmonary vasodilator (Fig. 2). These findings mainly reflected right ventricular function, with 19 (66%) participants requiring the presence of depressed right ventricular systolic function and 13 (45%) participants requiring the presence of right heart dilation. Other echocardiographic findings reported by the participants as important in deciding which patient might benefit from pulmonary vasodilators were; the presence of signs of PH, the gradients across the left heart structures, the left atrial dimensions, the flow direction across any cardiac defect, and the velocity of flow across an atrial communication.
Q7: Clinical symptoms and signs used in the decision to initiate pulmonary vasodilators in PH-LHD?
Most of the participants (68%) required the presence of clinical symptoms prior to recommending pulmonary vasodilators (Fig. 2). The two symptoms most commonly required were increasing fatigue (43%) and syncope (41%). While these symptoms overlap with symptoms of LHD without PH, the more specific sign of right-sided heart failure, systemic congestion, was required by only a small group of participants (19%).
Q8: Does the etiology of PH-LHD affect the decision to initiate pulmonary vasodilators in PH-LHD?
The etiology of the LHD was reported to affect the decision to recommend pulmonary vasodilators in 78% of the participants (Fig. 3). Participants were reluctant to recommend pulmonary vasodilators to patients with pulmonary vein stenosis, systolic left ventricular dysfunction, aortic valve disease, and coarctation of the aorta. The majority (62.5%) of the participants used the same clinical, echocardiographic or hemodynamic criteria to recommend pulmonary vasodilators for the different etiologies of LHD.
Fig. 3.
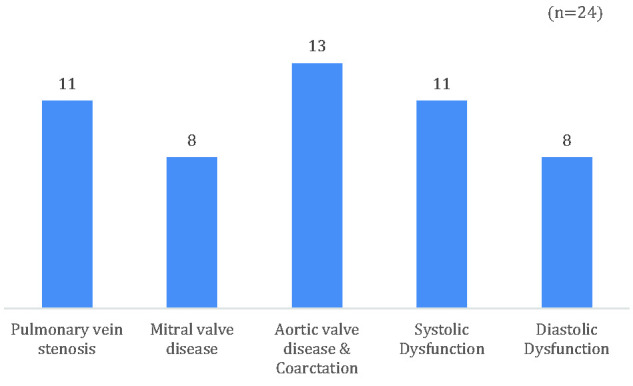
Bar chart depicting etiologies of left-sided heart disease in which participants considered pulmonary vasodilators were contraindicated.
Q9: Does the decision to initiate pulmonary vasodilators in PH-LHD differ if the cause of the PH-LHD was reversible versus irreversible?
The reversibility of the LHD was not considered an important factor in recommending pulmonary vasodilators in PH-LHD in 50% of participants. For those participants where reversibility was important (35%), half would prescribe it only if the LHD was reversible and the other half only if the LHD was irreversible. Five participants did not respond to this question.
Q10: Which class of pulmonary vasodilators is preferred in PH-LHD?
Participants preferred using phosphodiesterase-5-inhibitors (64%) and endothelin receptor antagonists (18%) for PH-LHD. Eighteen percent of participants had no preference and no participant preferred the use of prostanoids for PH-LHD.
Q11: Were the differences in responses based on the participant’s demographic information?
There were no differences between the participants regarding recommending pulmonary vasodilators for PH-LHD based on participants’ ages, years of experience or the volume of their practice (p values >0.05). There were also no differences based on the aforementioned participant characteristics regarding the rationale for recommending pulmonary vasodilators in PH-LHD, the assessments used prior to this recommendation and the preferred class of pulmonary vasodilator recommended (p values >0.05). Overall there were also no differences in the practice patterns based on location of practice (p values >0.05). The only difference found among the different groups of participants was that high-volume centers were more likely to recommend the use of pulmonary vasodilators in patients with pulmonary vein stenosis (p = 0.01). This difference was mainly driven by participants from North America, where 90% (versus 43% in the rest of the cohort) of participants who use pulmonary vasodilators in PH-LHD, would use them in patients with pulmonary vein stenosis.
Discussion
This study sheds light on the significant variation in practice among PH providers in regard to treating children with PH-LHD with pulmonary vasodilators. The survey results reflect the absence of agreement to the most fundamental question of whether to recommend pulmonary vasodilators in PH-LHD. The survey tried to clarify the underlying rationale behind prescribing pulmonary vasodilators in this group of patients, the criteria used, and the preferred class of pulmonary vasodilators recommended. The survey responses indicate that most pediatric PH providers would consider treating patients with PH-LHD with pulmonary vasodilators if they have combined pre-capillary and post-capillary PH and evidence of right ventricular dysfunction. Their rationale is mainly to support the right ventricle. There was no agreement, however, regarding the clinical, echocardiographic or hemodynamic criteria or cutoff thresholds used to recommend pulmonary vasodilators in PH-LHD. There was disagreement among the participants regarding the definition of PH-LHD. Eight participants (17%) reported recommending pulmonary vasodilators in PH-LHD but would not do so if the mean left atrial pressure was greater than 15 mmHg, which is part of the definition of PH-LHD. This suggests that some PH specialists use different definitions or cutoffs of left atrial pressure to define PH-LHD. There was also disagreement among providers regarding the etiologies of LHD that would be considered relative contraindications to the use of pulmonary vasodilators. We could not elucidate a pattern that can explain why certain etiologies were considered contraindications relative to others. For example, the most proximal and the most distal left-sided obstructions were considered contraindications with almost equal frequency. The same applies to systolic versus diastolic left ventricular dysfunction. Diastolic dysfunction was the least reported contraindication while aortic obstruction, that is commonly associated with diastolic dysfunction, was the most commonly reported contraindication.
The study results suggest fundamental differences in how the community of pediatric PH providers thinks about the role of pulmonary vasodilators in PH-LHD. Some providers think there is no role while others think the role of pulmonary vasodilators is palliative, hence only using it if the LHD is irreversible with signs of right ventricular failure. A third group of providers consider it as a method to postpone irreversible pulmonary vascular disease and hence would advocate for treatment even if the LHD was treatable and in some of these providers even prior to developing right ventricular dysfunction.
The class of pulmonary vasodilators preferred by PH specialists in PH-LHD was phosphodiesterase-5-inhibitors. This may be driven by the ease of administration, availability, and the lower side effect profile of this class of medications. However, it may also be driven by reports of improvement in pulmonary hemodynamics and exercise capacity in adult heart failure patients with reduced ejection fraction.20 However, less respondents considered diastolic dysfunction a contraindication to pulmonary vasodilators than systolic dysfunction despite the inefficacy of phosphodiesterase-5-inhibitors in adult patients with heart failure and preserved ejection fraction.12
In comparison to surveys performed in adult PH providers, the pediatric PH providers show a similar degree of disagreement in regard to the use of pulmonary vasodilators in PH-LHD. In the study by Trammell et al., 77% of adult PH providers consider the use of pulmonary vasodilators in PH-LHD, strikingly similar to the 79% in this study.10 The results of this survey and similar ones addressing the use of pulmonary vasodilators in WHO non-group I PH patients, reflect the lack of evidence based practice within the PH community.21–25 They also reflect the need for larger well designed studies to address these pressing questions.
The main limitation of our study is that the survey reflects the views of a very specialized group of providers, PH specialists attending international conferences, who probably treat an overall small percentage of children with PH-LHD. Most centers worldwide do not have PH specialists, and many do not have access to pulmonary vasodilators. This issue is reflected in the geographical distribution of the study participants. Therefore, the practice patterns reported are skewed towards practice patterns in academic centers in the United States with specialized pediatric PH teams, rather than what most children with PH-LHD experience in pediatric cardiology departments. The response rate to our survey, despite being higher than other published surveys,22,23 is still low (22% of surveyed individuals). The survey was anonymous and so the participant’s demographic information and size of their practice could not be verified. The survey tried to address the general trend towards the evaluation of PH-LHD patients and usage of PH targeted drugs in this patient population. Therefore, we did not evaluate more specific questions, e.g. the echocardiographic criteria used to diagnose RV dysfunction or if the presence of an atrial communication affects the decision to use pulmonary vasodilators in PH-LHD.
In conclusion, the practice of recommending pulmonary vasodilators in PH-LHD is highly variable among international pediatric PH specialists. Most specialists of those surveyed (57% in North America) would consider the use of pulmonary vasodilators in PH-LHD only if pre-capillary PH and right ventricular dysfunction are present. However, there is no consensus on the rationale, the criteria and the thresholds used to recommend pulmonary vasodilators in children with PH-LHD.
Supplemental Material
Supplemental material, sj-pdf-1-pul-10.1177_2045894021991446 for Practice patterns of pulmonary hypertension secondary to left heart disease among pediatric pulmonary hypertension providers by Hythem Nawaytou, Jeffrey R. Fineman, Shahin Moledina, Dunbar Ivy, Steven H. Abman and Maria J. Del Cerro in Pulmonary Circulation
Acknowledgments
We would like to thank the members of the PPHnet, the PVRI Pediatric & CHD Taskforce, and the REHIPED registry for participating in the survey.
Footnotes
Conflict of interest: The author(s) declare that there is no conflict of interest.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by NIH/NCATS Colorado CTSA Grant Number UL1 TR00253.
Ethical approval: This is a survey of providers and did not require IRB approval.
Contributorship: HN, JF, and MC designed and distributed the survey, HN analyzed the responses and wrote the manuscript, SM, DI, and SA contributed to the writing and review of the manuscript.
References
- 1.Gerges C, Gerges M, Lang MB, et al. Diastolic pulmonary vascular pressure gradient: a predictor of prognosis in “Out-of-Proportion” pulmonary hypertension. Chest 2013; 143: 758–766. [DOI] [PubMed] [Google Scholar]
- 2.Cam A, Goel SS, Agarwal S, et al. Prognostic implications of pulmonary hypertension in patients with severe aortic stenosis. J Thorac Cardiovasc Surg 2011; 142: 800–808. [DOI] [PubMed] [Google Scholar]
- 3.Fawzy ME, Osman A, Nambiar V, et al. Immediate and long-term results of mitral balloon valvuloplasty in patients with severe pulmonary hypertension. J Heart Valve Dis 2008; 17: 485–491. [PubMed] [Google Scholar]
- 4.Wood P. Pulmonary hypertension with special reference to the vasoconstrictive factor. Br Heart J 1958; 20: 557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Naeije R, D’Alto M. The diagnostic challenge of group 2 pulmonary hypertension. Prog Cardiovasc Dis 2016; 59: 22–29. [DOI] [PubMed] [Google Scholar]
- 6.Dayeh NR, Ledoux J, Dupuis J. Lung capillary stress failure and arteriolar remodelling in pulmonary hypertension associated with left heart disease (group 2 PH). Prog Cardiovasc Dis 2016; 59: 11–21. [DOI] [PubMed] [Google Scholar]
- 7.Wood P. An appreciation of mitral stenosis – I. Br Med J 1954; 1: 1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Groote P, Millaire A, Foucher-Hossein C, et al. Right ventricular ejection fraction is an independent predictor of survival in patients with moderate heart failure. J Am Coll Cardiol 1998; 32: 948–954. [DOI] [PubMed] [Google Scholar]
- 9.Maron BA, Ryan JJ. A concerning trend for patients with pulmonary hypertension in the era of evidence-based medicine. Circulation 2019; 139: 1861–1864. [DOI] [PubMed] [Google Scholar]
- 10.Trammell AW, Pugh ME, Newman JH, et al. Use of pulmonary arterial hypertension–approved therapy in the treatment of non-group 1 pulmonary hypertension at US referral centers. Pulm Circ 2014; 5: 356–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Galiè N, Humbert M, Vachiery J-L, et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J 2015; 37: 67–119. [DOI] [PubMed] [Google Scholar]
- 12.Redfield MM, Chen HH, Borlaug BA, et al. Effect of phosphodiesterase-5 inhibition on exercise capacity and clinical status in heart failure with preserved ejection fraction: a randomized clinical trial. JAMA 2013; 309: 1268–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Califf RM, Adams KF, McKenna WJ, et al. A randomized controlled trial of epoprostenol therapy for severe congestive heart failure: The Flolan International Randomized Survival Trial (FIRST). Am Heart J 1997; 134: 44–54. [DOI] [PubMed] [Google Scholar]
- 14.Koller B, Steringer-Mascherbauer R, Ebner CH, et al. Pilot Study of Endothelin Receptor Blockade in Heart Failure with Diastolic Dysfunction and Pulmonary Hypertension (BADDHY-Trial). Heart Lung Circ 2017; 26: 433–441. [DOI] [PubMed] [Google Scholar]
- 15.Rosenzweig EB, Abman SH, Adatia I, et al. Paediatric pulmonary arterial hypertension: updates on definition, classification, diagnostics and management. Eur Respir J 2019; 53: 1801916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.del Cerro Marín MJ, Rotés AS, Ogando AR, et al. Assessing pulmonary hypertensive vascular disease in childhood. Data from the Spanish Registry. Am J Respir Crit Care Med 2014; 190: 1421–1429. [DOI] [PubMed] [Google Scholar]
- 17.van Loon RLE, Roofthooft MTR, Hillege HL, et al. Pediatric pulmonary hypertension in the Netherlands: epidemiology and characterization during the period 1991 to 2005. Circulation 2011; 124: 1755–1764. [DOI] [PubMed] [Google Scholar]
- 18.Abman SH, Hansmann G, Archer SL, et al. Pediatric pulmonary hypertension. Circulation 2015; 132: 2037–2099. [DOI] [PubMed] [Google Scholar]
- 19.Endo M, Yamaki S, Ohmi M, et al. Pulmonary vascular changes induced by congenital obstruction of pulmonary venous return. Ann Thorac Surg 2000; 69: 193–197. [DOI] [PubMed] [Google Scholar]
- 20.Zhuang X-D, Long M, Li F, et al. PDE5 inhibitor sildenafil in the treatment of heart failure: a meta-analysis of randomized controlled trials. Int J Cardiol 2014; 172: 581–587. [DOI] [PubMed] [Google Scholar]
- 21.Kim D, Lee KM, Freiman MR, et al. Phosphodiesterase-5 inhibitor therapy for pulmonary hypertension in the United States. Actual versus recommended use. Ann Am Thorac Soc 2018; 15: 693–701. [DOI] [PubMed] [Google Scholar]
- 22.Minai OA, Nathan SD, Hill NS, et al. Pulmonary hypertension in lung diseases: survey of beliefs and practice patterns. Respir Med 2010; 104: 741–748. [DOI] [PubMed] [Google Scholar]
- 23.Altit G, Lee HC, Hintz S, et al. Practices surrounding pulmonary hypertension and bronchopulmonary dysplasia amongst neonatologists caring for premature infants. J Perinatol 2018; 38: 361–367. [DOI] [PubMed] [Google Scholar]
- 24.Ryan JJ, Butrous G, Maron BA. The heterogeneity of clinical practice patterns among an international cohort of pulmonary arterial hypertension experts. Pulm Circ 2014; 4: 441–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Caicedo L, Hopper R, Aguilar HG, et al. Acute vasoreactivity testing in pediatric idiopathic pulmonary arterial hypertension: an international survey on current practice. Pulm Circ 2019; 9: 2045894019857533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hansmann G, Koestenberger M, Alastalo T-P, et al. 2019 Updated Consensus Statement on the diagnosis and treatment of pediatric pulmonary hypertension. The European Pediatric Pulmonary Vascular Disease Network (EPPVDN), endorsed by AEPC, ESPR and ISHLT. J Heart Lung Transpl 2019; 38: 879–901. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-pul-10.1177_2045894021991446 for Practice patterns of pulmonary hypertension secondary to left heart disease among pediatric pulmonary hypertension providers by Hythem Nawaytou, Jeffrey R. Fineman, Shahin Moledina, Dunbar Ivy, Steven H. Abman and Maria J. Del Cerro in Pulmonary Circulation