Abstract
Objectives
This study aimed to investigate the frequency, nature, and clinical significance of pharmacist interventions on over-the-counter (OTC) medicines with abuse potential across community pharmacies with and without virtual care.
Methods
In this prospective observational study, a trained research team observed the dispensary teams of 12 community pharmacies in the United Arab Emirates (UAE), 6 of which were operating virtual pharmacy care. A standardized data collection form was used to include information about dispensing of OTC medicines and pharmacist interventions on those with abuse/misuse potential. The clinical significance of the interventions was evaluated by a multidisciplinary committee.
Results
The frequency of pharmacist interventions on OTC medicines with abuse potential across pharmacies with and without virtual services was 83.2% versus 91.0%, respectively, whereas the frequency of pharmacist interventions on OTC medicines with misuse potential across pharmacies with and without virtual services was 79.8% versus 41.2%, respectively. The proportions of clinically significant interventions across pharmacies with and without virtual services were 19.7% versus 10.5%, respectively. Cough medicines were dispensed significantly more across pharmacies with virtual care than across pharmacies without virtual care (25.6% vs. 9.7%, respectively; P = 0.04). Asking the patient to seek the advice of an addiction specialist (adjusted odds ratio = 4.11; P = 0.001) versus refusing to sell the drug was more likely to be associated with pharmacies with virtual services than with pharmacies operating traditional pharmacy services.
Conclusion
Virtual pharmaceutical care is a potential approach to reduce the abuse/misuse of OTC medicines but needs some improvements regarding detection of these cases. The UAE is the first country in the region to implement and regulate virtual pharmacy practice.
Key Points.
Background
-
•
Abuse of OTC medicine can lead to severe adverse events.
-
•
Virtual pharmacy services have gained much more importance worldwide after the COVID-19 outbreak.
Findings
-
•
Implementation of virtual pharmacy services increased the clinical value of pharmacist interventions on abuse of OTC medicine.
-
•
Digitalization of pharmacy services allowed patients with alarming symptoms to recieve remote care while reducing the risk for spreading the virus.
Over-the-counter (OTC) medications are commonly self-administered by patients for minor ailments, without a physician order.1 , 2 These medications have been used for a broad range of conditions, including a cold, heartburn, headaches, and musculoskeletal pain.3 Despite their good safety profile, these medicines can still induce severe adverse events such as fatality and addiction.4 , 5 Lack of awareness of several risks with regard to OTC medications and an underestimation of the potential risks might have contributed to these consequences because many patients think that the easily accessible drugs are harmless.6 , 7 The global prevalence of self-medication is extremely high, and thus the risk for abuse of OTC medicines is high worldwide.8 , 9 In a United Arab Emirates (UAE) study, 51% of the participants from the general public indicated that they usually used OTC medicines without medical consultation.10 The literature has shown that analgesics are the most common medications associated with OTC misuse and cough medicines with OTC abuse.3 , 11 Community pharmacists are reachable health professionals and can play a crucial role in preventing adverse events related to the use of OTC medicines. Nevertheless, the delivery of health care to the public has been challenging after the outbreak of coronavirus disease (COVID-19).12 In this regard, virtual health care services have been increasingly recognized as an efficient approach to increase access to care and combat the pandemic because they minimize the risk of COVID-19 transmission by reducing in-person contact among individuals.13 These virtual health care services include remote pharmaceutical services, which have been used in the United States to increase access to pharmaceutical care.14 Several studies have presented information technology in health care as a potential tool to maintain asthma control,15 reduce adverse drug events,16 minimize medication dispensing errors, and improve pharmacist interventions.17 Owing to the current crisis, which has posed unprecedented difficulties in health care delivery worldwide, the roles of community pharmacists have been legally expanded in many countries to involve providing remote services such as virtual consultation, home delivery of medications, and remote optimization of dosing regimens.18 , 19 These services have been effective in reducing the burden on the health care sectors and minimizing medication dispensing errors. Despite the barriers, the UAE overcome technical barriers towards implementation of health informatics by improving the healthcare infrastructure when the health officials of Abu Dhabi implemented a sophisticated regulatory regime for telemedicine across the country.20 In 2019, Dubai Health Authority launched the “Doctor for Every Citizen Initiative” to enable health care providers in Dubai to use the latest digital technology to enhance efficiencies in care delivery.20 In light of the COVID-19 pandemic, UAE health authorities have issued circulars regulating the delivery of virtual pharmacist services during the pandemic.21 The UAE managed to strike a balance between precautionary measures and health care delivery during the pandemic by upgrading the remote health services provided by outpatient clinics, pharmacies, and hospitals using smart technology and digital communication systems. These tools include fast Web access, video conferencing software, phone calls, home delivery of medications, and social media websites. Therefore, this study aimed to evaluate if information technology can be used by pharmacists to identify potential abuse/misuse of OTC medications and if implementation of virtual services can improve the clinical effects of pharmacist interventions on OTC abuse and misuse.
Methods
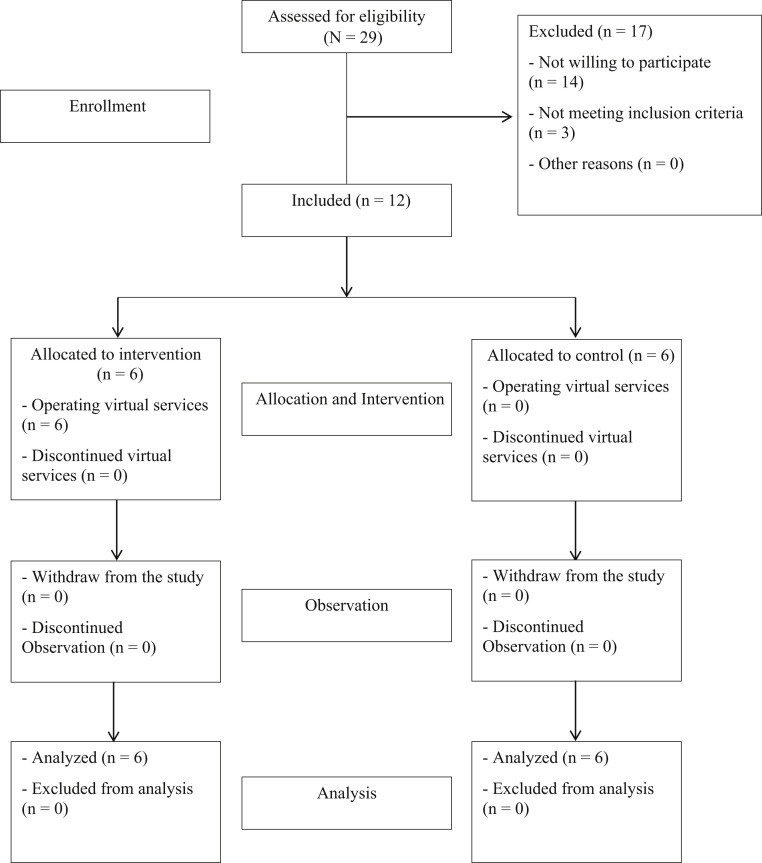
This was a prospective, observational, comparative study conducted over a period of 2 months (from August 1, 2020 to October 1, 2020) at community pharmacies operating remote services (intervention group) and community pharmacies operating traditional pharmacy services (control group) across the UAE. Trained researchers conducted a direct observation of the pharmacy dispensary team for 10 days to collect data related to the dispensing of OTC medications and the nature of pharmacist interventions. This study was approved by the ethics committee at the University of Sharjah. Using G∗Power software (Heinrich Heine University),22 and considering power = 0.8, α ≤ 0.05, and effect size = 0.8, the sample size for this study was decided as 12 community pharmacies (6 in each group). An effect size of 0.8 meant that the score of the average pharmacy in the intervention group (with virtual services) was 0.8 SDs above the average pharmacy in the control group (without virtual services) and hence exceeded the scores of 79% of the control group.
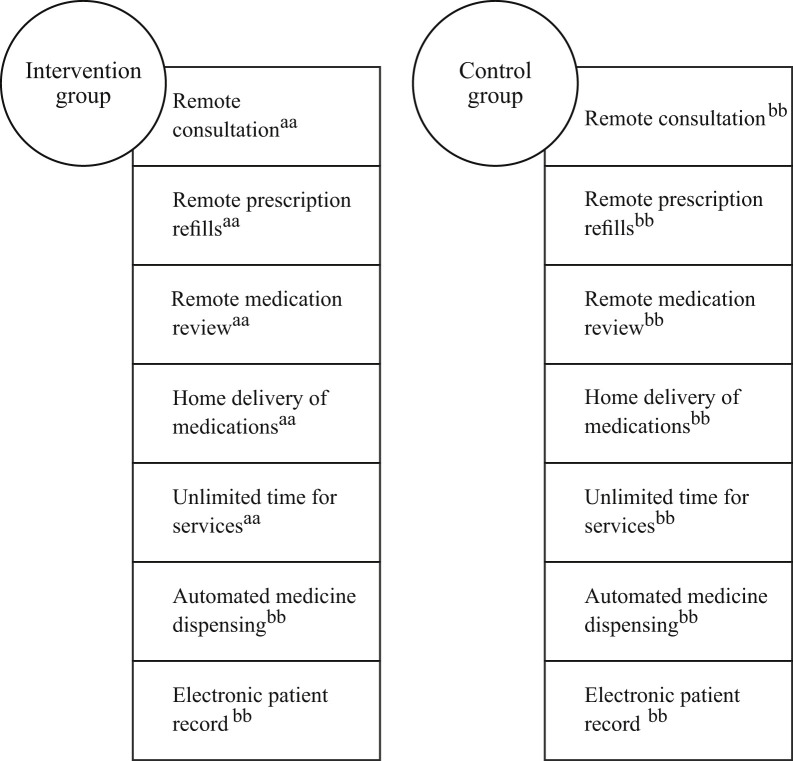
Sampling technique, allocation of pharmacies, and inclusion criteria
The total number of community pharmacies in the UAE is 2703, of which 880 (32.55%) are based in the capital region (Abu Dhabi), 775 (28.67%) in the central region (Dubai), and 1048 (38.78%) in the northern region (Ajman, Fujairah, Ras al Khaimah, Sharjah, and Umm al Quwain). Each emirate was stratified geographically into districts on the basis of the density of the pharmacies. The capital and central regions were divided into 7 and 9 areas (districts), respectively, whereas the northern region was divided into 13 areas (districts). The areas from each region were listed in decreasing order, coded with numbers, and entered into a computer software program; 3 areas from each region were then selected randomly. The pharmacies from each area were listed alphabetically and then coded with numbers. A random sample of community pharmacies was invited from each area, proportionate to the relative proportion of pharmacists in the region, that is, 4 (32.55%, 4/12) from the capital region, 3 (28.67% (3/12) from the central region, and 5 (38.78% (5/12) from the northern region. To recruit the sample (N= 12), we invited 29 pharmacies, of which 14 refused participation, and 3 were excluded. The reasons for exclusion were the very small size (< 50 m2) of the pharmacy, intermittent working days (closed > 1 day per week), incomplete implementation of virtual services, and light workload (< 35 items dispensed per day). Community pharmacies operating remote services were assigned to the intervention group, and community pharmacies with traditional pharmacy services were allocated to the control group (Figure 1 ). The allocation ratio was 1:1. Pharmacies were eligible for the intervention group allocation if they were operating virtual pharmacist services using information technology tools. These services included remote consultation, remote prescription refills, home delivery of medications, and remote medication review (Figure 2 ). Pharmacies were excluded from the intervention group if the used tools were not adequate to perform complete virtual services and if the pharmacies were not following precautionary measures23 or not following the standards of pharmacy practice as prescribed by health officials in the UAE. Pharmacies in the control group were included if they were operating traditional pharmacy services, following precautionary measures, and working on a regular basis. Among all pharmacies included in this study, electronic patient record, electronic prescribing system, and automated medication dispensing cabinets were not implemented.
Figure 1.
The flow of the study.
Figure 2.
Remote services provided across pharmacies with (intervention group) and without (control group) virtual services. aa, present; bb, absent.
Definitions and pharmacist intervention evaluation
OTC medicines were defined as medications sold without a physician order. The term “abuse of a medication” is used in our study to describe the use of drugs for nonmedical purposes, whereas “misuse of a medication” is applied to describe the use of a drug for medical purposes but in a wrong manner, for instance, use over a prolonged period or at increased dosage.3 , 24 The significance of the pharmacist interventions was categorized into significant, moderate, and minor on the basis of the seriousness of the health consequences in case no interventions were performed. A pharmacist intervention that potentially prevented serious harm and possibly death from occurring was defined as a significant intervention.25 An intervention that potentially prevented a temporary harm with no risk of hospitalization was defined as a moderate intervention, whereas an intervention that was performed on the basis of a situation involving no risk of patient harm was considered a minor intervention.26 The significance of pharmacist interventions was evaluated by a committee of experts comprising a general practitioner, a clinical pharmacist, and an internist. The research team adopted a validated method for quantifying and rating the responses of the committee.23 After completing the data collection process, the committee members were asked to rate clinical significance on a 10-point scale from 0 (no harm) to 10 (death), and the mean score across all judges was used as an index of clinical significance of pharmacist interventions. A score of less than 3 represented a minor intervention, a score between 3 and 7 a moderate intervention, and a score of more than 7 a significant intervention. The internal consistency of the committee members was tested using the kappa statistic. A kappa value of below 0.5 was considered bad reliability, between 0.5 and 0.7 moderate reliability, between 0.7 and 0.8 good reliability, and above 0.8 great reliability.
Development of the study instrument and piloting
We developed a standardized data collection form, which included information about the frequency, nature, and reasons of pharmacist interventions related to the misuse/abuse of OTC medications. Information about the pharmacy dispensary team, such as experience, education, and country of graduation, was also included. A preliminary piloting was conducted at 2 pharmacies (1 from each group) for 3 days. The purposes of the pilot study were to test the accuracy and appropriateness of the data collection form, time feasibility, the cooperation of the staff members, and the optimal approach to observation without affecting patient privacy. After piloting, we set 10 days per pharmacy as the period for data collection. The main investigator instructed the researchers to have no interaction with customers or patients. The data of the piloting test were not included in the final results.
Data collection
The data collectors were 6 licensed pharmacists with at least 2 years of experience in community settings. They were recruited and trained on the professional practice of dispensing OTC medications, health informatics, and information technology tools. Furthermore, they were given training on accurate completion of the data collection form and correct use of operational definitions on the basis of guidelines for reporting observational studies.27 Each researcher collected data for 10 days (from 8:30 AM to 4:30 PM) at a community pharmacy. Data were sent to the principal investigator at the end of each research day; a final review with reference to the inclusion criteria was then carried out before addition to the final dataset. The types of data collected during the research can be categorized as follows: (1) frequency and types of OTC medicines dispensed during the research—this was crucial to determine the incidence of abuse/misuse of OTC medicines, (2) frequency and nature of potential abuse/misuse of OTC medicines, and (3) frequency and types of pharmacist interventions. In this regard, the data collectors observed 3 major types of interventions: (1) patient education on medication use, drug category, and suggestions to seek a specialist’s advice; (2) alteration on drug dose, dosage form, and duration; and (3) refusal to sell the drug. Pharmacists determined potential misuse or abuse of drugs either through obtaining information from patients in case of misuse (medical history, concurrent medications, allergies, and symptoms) or through specific indicators in case of drug abuse, for instance, asking for too much of a product at once, or behaving suspiciously, perhaps seeming to be drunk or high. Both pharmacy managers and staff signed a consent form demonstrating their willingness to participate.
Data analysis
The data were analyzed using SPSS version 26 (IBM Corp, Armonk, NY). To explore the differences in frequencies, types, and significance of pharmacist interventions; frequency and types of OTC medicines; and number of patients who received pharmaceutical care across the intervention and control groups, chi-square or Fisher exact tests were used as appropriate.
Regression model
To assess the association of each type of pharmacist intervention and clinical importance of the intervention with community pharmacy status but with or without virtual services, a multivariable logistic regression model was constructed. The dependent variable was considered pharmacy status (with virtual services vs. without virtual services), and the independent variables were the types (all interventions vs. refusal to sell the drug) and significance (significant and moderate vs. minor) of pharmacist interventions. Refusal to sell the drug is a pharmacist intervention that was considered a reference for comparison among the types of interventions because it was a strict intervention, unlike other interventions that included giving the patients advice and giving them several choices. We decided to construct a multivariable logistic regression because the data comprised 2 sets of independent variables. Descriptive results are presented as proportions (%) with 95% CIs, whereas logistic regression results are presented as adjusted odd ratios (aORs) with 95% CIs. Statistical significance was considered at P < 0.05 (with a confidence limit set at 95%).
Results
Characteristics of pharmacies and customers
There were no significant differences in the number, educational level, and experience of pharmacy staff across pharmacies with and without virtual services (P > 0.05). Compared with the control group, pharmacies with virtual pharmaceutical services had a significantly higher frequency of customers who requested or received OTC medications (intervention group 2036 vs. control group 1163, P = 0.01). Of the customers who requested or received OTC medication using virtual pharmacy services, 20.7% were older adults (aged > 65 years), whereas most of the customers who received traditional care were aged below 45 years (Table 1 ). The findings of this study indicate that antihistamine medicines were the most common OTC medicines with abuse potential, and analgesics were the most common OTC medicines with misuse potential.
Table 1.
Characteristics of pharmacies, customers, and OTC medications
| Code | Pharmacy characteristics | Pharmacies with virtual services | Pharmacies with traditional services | P value |
|---|---|---|---|---|
| A | No. pharmacies | 6 | 6 | — |
| B | No. pharmacy staff | 18 | 21 | — |
| C | Educational level of pharmacy staff | — | — | 0.25 |
| Diploma | 1 | 3 | — | |
| Bachelor’s degree | 14 | 15 | — | |
| Master’s degree | 3 | 2 | — | |
| Doctorate | 0 | 1 | — | |
| D | Experience of pharmacy staff | — | — | 0.43 |
| < 2 y | 8 | 10 | — | |
| 2–5 y | 6 | 8 | — | |
| > 5 y | 4 | 3 | — | |
| Characteristics of customers | — | — | — | |
| E | No. customers who requested or received OTC medicines | 2036 | 1163 | 0.01a |
| F | Estimated age (y) (%) | — | — | 0.03a |
| < 18 | 21 (1.0) | 103 (8.9) | — | |
| 18–29 | 298 (14.6) | 429 (36.9) | — | |
| 30–45 | 673 (33.1) | 419 (36.0) | — | |
| 45–65 | 623 (30.6) | 203 (17.5) | — | |
| > 65 | 421 (20.7) | 9 (0.7) | — | |
| G | Patient age groups (younger/older) (y) (%) | 0.001a | ||
| > 65 y | 421 (20.7) | 9 (0.7) | ||
| < 65 y | 1615 (79.3) | 1154 (99.3) | ||
| H | Gender (%) | 0.61 | ||
| Male | 1066 (52.4) | 652 (56.1) | ||
| Female | 970 (47.6) | 511 (43.9) | ||
| OTC medication characteristics | 0.001 | |||
| J | Total no. OTC medications requested (by patient) | 4623 | 1986 | |
| K | Total no. prescribed OTC medications (by physician or pharmacist) | 1730 | 447 | |
| L | Total no. dispensed OTC medications | 5099 | 1876 | |
| M | Frequency of potential abuse | 368 | 188 | |
| N | Frequency of potential misuse | 872 | 403 | |
| O | Incidence of potential OTC abuse {O = M/(J + K) ×100} (%) | 5.8 | 7.7 | 0.1 |
| P | Incidence of potential OTC misuse {P = N/(J + K) × 100} (%) | 13.7 | 16.6 | 0.6 |
| Q | Pharmacist interventions on potential OTC abuse (%) | 306 (83.2) | 82 (91.0) | 0.09 |
| R | Pharmacist interventions on potential OTC misuse (%) | 696 (79.8) | 166 (41.2) | 0.02a |
| S | Types of OTC medications requested or prescribed with potential abuse/misuse (%) | 0.04a | ||
| Antihistamines | 1684 (26.5) | 746 (30.7) | ||
| Analgesics | 1496 (23.5) | 603 (24.8) | ||
| Cough medicines | 1626 (25.6) | 236 (9.7) | ||
| Laxatives | 203 (3.2) | 169 (6.9) | ||
| Codeine-containing products | 893 (14.1) | 421 (17.3) | ||
| Decongestants | 451 (7.1) | 258 (10.6) | ||
| Total (%) | 6353 (100.0) | 2433 (100.0) |
Abbreviation used: OTC, over the counter.
P values are considered significant.
Rates of potential OTC abuse and misuse
The rate of potential OTC abuse across pharmacies with and without virtual services was 5.8% versus 7.7%, respectively, whereas the rate of potential OTC misuse across pharmacies with and without virtual services was 13.7% versus 16.6%, respectively. There were significant differences between pharmacies with and without virtual services for types of OTC medications requested or prescribed with potential abuse/misuse (P = 0.04). For instance, the proportions of cough medicines and codeine-containing products across pharmacies with and without virtual services were 25.6% versus 9.7% and 14.1% versus 17.3%, respectively.
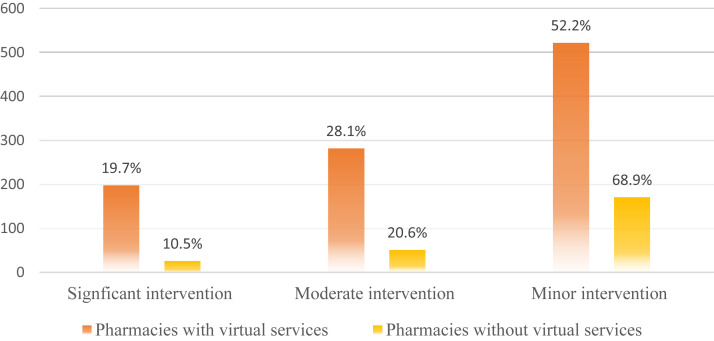
Pharmacist interventions on potential OTC abuse and misuse
The frequency of pharmacist interventions on OTC medicines with abuse potential across pharmacies with and without virtual services was 83.2% versus 91.0%, respectively, whereas the frequency of pharmacist interventions on OTC medicines with misuse potential across pharmacies with and without virtual services was 79.8% versus 41.2%, respectively. Most of the interventions on potential OTC abuse and misuse performed by pharmacists operating information technology tools involved providing the patients with instructions about the medications (39.3%), suggesting another medication (21.9%), and asking the patient to seek the advice of their general practitioner (GP) (13.3%). The intervention types (1) providing the patients with instructions about the medications (aOR = 2.69 [95% CI 1.45–5.99], P = 0.03), (2) asking the patient to seek the GP’s advice (3.66 [2.45–5.96], P = 0.01), and (3) asking the patient to seek the advice of an addiction specialist (4.11 [2.89–7.78], P = 0.001) each versus refusal to sell the drug were more likely to be associated with pharmacies with virtual services versus pharmacies operating traditional pharmacy services. Table 2 summarizes the regression model used to describe the association between independent factors (types of interventions) and the dependent variable (with vs. without virtual services). The proportions of significant and moderate interventions across pharmacies with and without virtual services were 19.7% versus 10.5% and 28.1% versus 20.6%, respectively (Figure 3 ). The internal consistency test showed that, overall, the experts’ opinions were in agreement by 73% (α = 0.73). As mentioned earlier, pharmacists in both groups were alerted to the risk of OTC abuse and misuse on the basis of many indicators, including the type of drug requested, the amount of the drug requested, the time of patient appearance, and the voice and behavior of the patient. Table 3 demonstrates several examples of potential OTC abuse/misuse, each with the pharmacist intervention, clinical significance, and type of pharmacy. Table 3 also lists cases of potential abuse/misuse of drugs and the associated pharmacist interventions.
Table 2.
Association of pharmacist intervention types and significance with pharmacy status (with vs. without virtual services)
| Independent variables |
Adjusted odds ratio | 95% confidence limits |
P value | |
|---|---|---|---|---|
| Types of interventions (type vs. reference) | Lower | Upper | ||
| Alteration of the dose vs. refusal to sell the drug | 0.82 | 0.23 | 1.68 | 0.21 |
| Provide the patients with instructions about the medications vs. refusal to sell the drug | 2.69 | 1.45 | 5.99 | 0.03 |
| Suggest another medication vs. refusal to sell the drug | 1.60 | 0.84 | 3.55 | 0.36 |
| Alteration of the duration vs. refusal to sell the drug | 0.68 | 0.23 | 1.57 | 0.19 |
| Alteration of the dosage form vs. refusal to sell the drug | 2.59 | 1.73 | 4.88 | 0.47 |
| Ask the patient to seek their GP’s advice vs. refusal to sell the drug | 3.66 | 2.45 | 5.96 | 0.01a |
| Ask the patient to seek the advice of an addiction specialist vs. refusal to sell the drug | 4.11 | 2.89 | 7.78 | 0.001a |
| Clinical significance of interventions | ||||
| Significant vs. minor | 2.51 | 1.42 | 3.94 | 0.01a |
| Moderate vs. minor | 0.89 | 0.24 | 1.27 | 0.18 |
Abbreviation used: GP, general practitioner.
P values are considered significant.
Figure 3.
Clinical significance of pharmacist interventions across pharmacies with and without virtual services.
Table 3.
Examples of pharmacist interventions on potential abuse/misuse of OTC medications
| Potential OTC abuse/misuse | Pharmacist intervention | Clinical significance of interventions | How pharmacists are alerted to the risk | Type of pharmacy |
|---|---|---|---|---|
| A male adult asked for 10 bottles of cough medicine (containing dextromethorphan) | Refused to sell | Significant | The customer asked for too much of a product at once | Operating remote services |
| A woman asked for cetirizine (syrup) to help her baby (aged < 1 y) sleep | Suggested dimethindene maleate (drops) | Moderate | The pharmacist asked the customer about the reason for requesting the medication | Operating remote services |
| A woman asked for a salbutamol inhaler for the first time | Provided the customer with instructions about the correct use of inhalers | Moderate | The customer informed the pharmacist that this was the first time she was using the inhaler | Operating remote services |
| A young man asked for 5 bottles of a codeine-containing product at almost midnight | Advised the customer to seek an addiction specialist | Significant | The customer behaved suspiciously | Operating traditional services |
| A woman asked for diclofenac sodium suppository for her 6-month-old child | Suggested paracetamol suppository | Moderate | The pharmacist asked the customer about the age of her child | Operating traditional services |
| A man asked for paracetamol 500 mg tablets | Alteration of the dose | Minor | The patient self-administered 4 tablets at once inside the pharmacy | Operating traditional services |
| A pregnant woman asked for calcium supplements to relieve constant pain in her legs and back | Suggested to the customer that she seek physician consultation | Moderate | The patient informed the pharmacist about her problem | Operating traditional services |
Abbreviation used: OTC, over the counter.
Discussion
Our findings suggest that the adoption of information technology by community pharmacies enables them to identify and intervene on the abuse and misuse of OTC medicines. Furthermore, we found that more older patients are involved in requesting OTC medicines through virtual pharmacy services than young people (aged < 30 years). The plausible explanation is that older patients may represent a specific cluster of patients with a high risk for developing COVID-19 with rapidly progressive clinical deterioration.28 Therefore, several countries have restricted the movement of older adults to reduce the risk for infection.29 However, because polypharmacy often increases with age, the population consisting of older adults may in turn develop higher risk for abuse of OTC medicines.30 , 31 We believe that this is a major challenge for virtual care. Of note, the association between age groups and the risk for OTC abuse was beyond the scope of this study owing to practical reasons. To some extent, this study has helped to shed some light on this issue, and we urge researchers to consider conducting extensive evaluation of the impact of virtual care on older patients’ medication safety during the pandemic.
There is no study in the literature investigating virtual pharmacist interventions on potential abuse of OTC medicines before the COVID-19 pandemic. Thus, it is difficult to compare between the 2 periods. However, the literature shows that the rate of adoption of remote pharmacy services has increased considerably since the beginning of the pandemic alongside the rise in demand for OTC medicines. Therefore, we expect that virtual interventions on the abuse of OTC medicines have also increased.
The rates for potential abuse and misuse of OTC medications were not significantly different across pharmacies with and without virtual services. Nevertheless, it is extremely difficult to detect potential abuse without interviewing patients or observing their behaviors. Pharmacists operating virtual care could be unsighted because physical appearance (look and behavior) is vital in discovering individuals with intention to abuse OTC medicines.8 Other behaviors such as requesting several bottles of the same drug without declaring a legitimate reason could indicate a potential abuse of OTC medicines. These behaviors are extremely difficult to observe remotely. Thus, we believe that virtual pharmacy services could increase the rate of potential abuse of OTC medicines because virtual care increases access to OTC medications.3 This emphasizes the importance of training for pharmacists, particularly those operating virtual services. Further research is necessary to report and explain the impact of information technology on the rate of abuse of OTC medicines.
The proportion of pharmacist interventions on the abuse of OTC medicines in pharmacies with virtual services was relatively less than that in pharmacies without virtual services. As mentioned previously, some practical issues blind the pharmacists operating virtual care to detect potential abuse of OTC medicines. Interestingly, pharmacist interventions on misuse of OTC medicines were significantly higher in pharmacies with virtual care. It seems that virtual care enabled pharmacists and patients to share information more efficiently than traditional care, where customers avoid the risk of COVID-19 transmission by purchasing OTC medicines and hurtling outside the pharmacy without providing adequate information to the pharmacist about why they requested the medication or how they usually use it. However, the definitions of abuse and misuse of OTC medications are not unequivocal, and in many cases abuse/misuse of OTC medicines might be unnoticeable, especially when the customers are out of sight. Thus, we recommend measures such as developing an early warning system, sharing information on OTC misuse with patients, and improving information technology tools to alert pharmacists to the misuse potential of some products.
Our findings demonstrate that there is a group of medications that seem to have a higher potential of being misused: antihistamines, analgesics, cough medicines, laxatives, and codeine-containing products. This aligns with several studies worldwide.32, 33, 34 Although no studies have assessed the possibility of an association between certain types of OTC medications with abuse potential and virtual care, we found that the proportion of cough medicines with abuse potential is higher in pharmacies with virtual care than in those operating traditional care. The UAE has made enormous efforts to reduce the risk of COVID-19 transmission by raising the awareness of the community about the importance of using remote health care services. This might have caused patients with alarming symptoms such as a cough and fever to seek virtual pharmaceutical care.
Our findings link specific types of pharmacist interventions to pharmacies with virtual services; 1 of these types is providing the patient with instructions about the medications. As noted previously, information technology enables pharmacists to share information with patients freely without any concerns regarding the risk for COVID-19 transmission. De Fátima Marin et al.35 emphasized that information technology and social media are making it easier than ever for consumers to find timely, personalized health care information. Our findings are consistent with those of the study by de Fátima Marin et al.35 because we found that interventions such as asking the patient to seek the advice of an addiction specialist or a GP are more likely to be associated with pharmacies providing virtual care. A second area of virtual care benefit comes in the form of improved trust and privacy, which enables pharmacists to have higher engagement levels in sensitive health cases, particularly in the Arab region, where the stigma is widespread.
Interestingly, the proportions of significant and moderate pharmacist interventions were higher in pharmacies with virtual care than in those operating traditional pharmacy services. This may be an indicator of the effectiveness of information technology in making pharmacists more proactive in managing OTC medication abuse by enabling them to use their clinical skills and provide oral medication information while maintaining trust and privacy with patients.
Limitations
The study has several limitations. First, it was conducted at pharmacies operating different trends of virtual services, and this variation might have affected the major outcomes of the study. Second, this is a prospective study conducted directly on the dispensary team inside the pharmacy, and although most of the pharmacist interventions were observed and reported, sometimes, as in a case of crowding or patients requesting privacy, interventions were missing. The absence of an electronic patient record and lack of time were issues because it was extremely difficult to cover every single intervention that a pharmacist performed during the course of their duties or in-between their duties. Third, the impact of missing data related to pharmacist interventions was beyond the scope of this study’s aims. Fourth, this study provides only a quantitative evidence of the number, types, and clinical significance of virtual pharmacist interventions on potential OTC medicine abuse. Neither the acceptance of patients of the virtual interventions nor the appropriateness of these interventions was assessed. Fifth, although the research team was in disguise, we have concerns regarding the impact of the Hawthorne effect on the study’s findings because it was difficult to keep the aims of the study hidden, especially in the presence of the pharmacy managers who were informed about the true purposes of the study. Sixth, the frequency of OTC medicines dispensed varied greatly between both groups. We suspect that this might have a minor impact on the findings of the study. Finally, this study was conducted on a few community pharmacies and examined only 1 component of virtual care; our findings may not reflect the habits and preferences of remote pharmacist interventions in other settings. Nevertheless, these drawbacks could be a foundation for future research.
Conclusion
The study demonstrates that the digitalization of pharmacy services improves pharmacist interventions on OTC misuse and allows patients with alarming symptoms, for example, a cough, to receive remote pharmaceutical care and reduces transmission of COVID-19. Furthermore, it enables older patients who are vulnerable to viruses to access pharmacies without the risk of contracting the infection. The development of an early warning system may further enhance the ability of remote pharmaceutical care to intervene and prevent OTC abuse.
Biographies
Nadia Al Mazrouei,PhD, Assistant Professor, Department of Pharmacy Practice and Pharmacotherapeutics, College of Pharmacy, University of Sharjah, United Arab Emirates
Rana M. Ibrahim,PharmD, Lecturer, Department of Pharmacy Practice and Pharmacotherapeutics, College of Pharmacy, University of Sharjah, United Arab Emirates
Ahmad Z. Al Meslamani,MSc Laboratory, Supervisor, College of Pharmacy, Al Ain University of Science and Technology, Abu Dhabi, United Arab Emirates
Derar H.Abdel-Qader,PhD, Senior Clinical Lecturer & Consultant Pharmacotherapist, Faculty of Pharmacy and Medical Sciences, University of Petra, Amman, Jordan
Osama Mohamed Ibrahim,PhD, Associate Professor, Department of Pharmacy Practice and Pharmacotherapeutics, College of Pharmacy, University of Sharjah, United Arab Emirates; and Associate Professor, Department of Clinical Pharmacy, Faculty of Pharmacy, Cairo University, Cairo, Egypt
Footnotes
Disclosure: The authors declare no relevant conflicts of interest or financial relationships.
References
- 1.Anderson J.G. Demographic factors affecting health services utilization: a causal model. Med Care. 1973;11(2):104–120. doi: 10.1097/00005650-197303000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Wazaify M., Shields E., Hughes C.M., McElnay J.C. Societal perspectives on over-the-counter (OTC) medicines. Fam Pract. 2005;22(2):170–176. doi: 10.1093/fampra/cmh723. [DOI] [PubMed] [Google Scholar]
- 3.Sansgiry S.S., Bhansali A.H., Bapat S.S., Xu Q. Abuse of over-the-counter medicines: a pharmacist’s perspective. Integr Pharm Res Pract. 2017;6:1–6. doi: 10.2147/IPRP.S103494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cooper R. Surveillance and uncertainty: community pharmacy responses to over the counter medicine abuse. Health Soc Care Community. 2013;21:254–262. doi: 10.1111/hsc.12012. [DOI] [PubMed] [Google Scholar]
- 5.Fingleton N.A., Watson M.C., Duncan E.M., Matheson C. Non-prescription medicine misuse, abuse and dependence: a cross-sectional survey of the UK general population [published correction appears in J Public Health (Oxf). 2017;39:876] J Public Health (Oxf) 2016;38(4):722–730. doi: 10.1093/pubmed/fdv204. [DOI] [PubMed] [Google Scholar]
- 6.Calamusa A., Di Marzio A., Cristofani R. Factors that influence Italian consumers’ understanding of over-the-counter medicines and risk perception. Patient Educ Couns. 2012;87(3):395–401. doi: 10.1016/j.pec.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 7.Cuzzolin L., Benoni G. Safety of non-prescription medicines: knowledge and attitudes of Italian pharmacy customers. Pharm World Sci. 2010;32(1):97–102. doi: 10.1007/s11096-009-9348-2. [DOI] [PubMed] [Google Scholar]
- 8.Cooper R.J. Over-the-counter medicine abuse - a review of the literature. J Subst Use. 2013;18(2):82–107. doi: 10.3109/14659891.2011.615002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shehnaz S.I., Agarwal A.K., Khan N. A systematic review of self-medication practices among adolescents. J Adolesc Health. 2014;55(4):467–483. doi: 10.1016/j.jadohealth.2014.07.001. [DOI] [PubMed] [Google Scholar]
- 10.Barakat-Haddad C., Siddiqua A. Prevalence and predictors of over-the-counter medication use among adolescents in the United Arab Emirates. East Mediterr Health. 2018;23(11):744–753. doi: 10.26719/2017.23.11.744. [DOI] [PubMed] [Google Scholar]
- 11.MacFadyen L., Eadie D., McGowan T. Community pharmacists’ experience of over-the-counter medicine misuse in Scotland. J R Soc Promot Health. 2001;121(3):185–192. doi: 10.1177/146642400112100316. [DOI] [PubMed] [Google Scholar]
- 12.Cadogan C.A., Hughes C.M. On the frontline against COVID-19: community pharmacists’ contribution during a public health crisis. Res Social Adm Pharm. 2021;17(1):2032–2035. doi: 10.1016/j.sapharm.2020.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kaplan B. Revisiting health information technology ethical, legal, and social issues and evaluation: telehealth/telemedicine and COVID-19. Int J Med Inform. 2020;143:104239. doi: 10.1016/j.ijmedinf.2020.104239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kimber M.B., Peterson G.M. Telepharmacy—enabling technology to provide quality pharmacy services in rural and remote communities. J Pharm Pract Res. 2006;36(2):128–133. [Google Scholar]
- 15.Brown W., Scott D., Friesner D., Schmitz T. Impact of telepharmacy services as a way to increase access to asthma care. J Asthma. 2017;54(9):961–967. doi: 10.1080/02770903.2017.1281292. [DOI] [PubMed] [Google Scholar]
- 16.Schneider P.J. Evaluating the impact of telepharmacy. Am J Health Syst Pharm. 2013;70(23):2130–2135. doi: 10.2146/ajhp130138. [DOI] [PubMed] [Google Scholar]
- 17.Garrelts J.C., Gagnon M., Eisenberg C., Moerer J., Carrithers J. Impact of telepharmacy in a multihospital health system. Am J Health Syst Pharm. 2010;67(17):1456–1462. doi: 10.2146/ajhp090670. [DOI] [PubMed] [Google Scholar]
- 18.Abdel Jalil M., Alsous M.M., Abu Hammour K., Saleh M.M., Mousa R., Hammad E.A. Role of pharmacists in COVID-19 disease: a Jordanian perspective. Disaster Med Public Health Prep. https://doi.org/10.1017/dmp.2020.186 accessed November 18, 2020. [DOI] [PMC free article] [PubMed]
- 19.Merks P., Jakubowska M., Drelich E. The legal extension of the role of pharmacists in light of the COVID-19 global pandemic. Res Social Adm Pharm. 2021;17(1):1807–1812. doi: 10.1016/j.sapharm.2020.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Al-Samarraie H., Ghazal S., Alzahrani A.I., Moody L. Telemedicine in Middle Eastern countries: progress, barriers, and policy recommendations. Int J Med Inform. 2020;141:104–232. doi: 10.1016/j.ijmedinf.2020.104232. [DOI] [PubMed] [Google Scholar]
- 21.Department of Health Remote healthcare platform. https://doh.gov.ae/covid-19/Remote-Healthcare-Platform Available at.
- 22.Buchner A., Erdfelder E., Faul F., Lang A. G∗Power: statistical power analyses for Windows and Mac. https://www.psychologie.hhu.de/arbeitsgruppen/allgemeine-psychologie-und-arbeitspsychologie/gpower.html Available at:
- 23.Crowe S., Cresswell K., Robertson A., Huby G., Avery A., Sheikh A. The case study approach. BMC Med Res Methodol. 2011;11:100. doi: 10.1186/1471-2288-11-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hughes G.F., McElnay J.C., Hughes C.M., McKenna P. Abuse/misuse of non-prescription drugs. Pharm World Sci. 1999;21(6):251–255. doi: 10.1023/a:1008788726842. [DOI] [PubMed] [Google Scholar]
- 25.Sartore M.E., Ehman K.M., Good C.B. The significance of pharmacy interventions: an updated review in the presence of electronic order entry. Am J Pharm Benefits. 2014;6(2):e24–e30. [Google Scholar]
- 26.Al Rahbi H.A., Al-Sabri R.M., Chitme H.R. Interventions by pharmacists in out-patient pharmaceutical care. Saudi Pharm J. 2014;22(2):101–106. doi: 10.1016/j.jsps.2013.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.von Elm E., Altman D.G., Egger M. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335(7624):806–808. doi: 10.1136/bmj.39335.541782.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Perrotta F., Corbi G., Mazzeo G. COVID-19 and the elderly: insights into pathogenesis and clinical decision-making [published correction appears in Aging Clin Exp Res. 2020;32(9):1909] Aging Clin Exp Res. 2020;32(8):1599–1608. doi: 10.1007/s40520-020-01631-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sun Z., Yang B., Zhang R., Cheng X. Influencing factors of understanding COVID-19 risks and coping behaviors among the elderly population. Int J Environ Res Public Health. 2020;17(16):5889. doi: 10.3390/ijerph17165889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Olson C.H., Dey S., Kumar V., Monsen K.A., Westra B.L. Clustering of elderly patient subgroups to identify medication-related readmission risks. Int J Med Inform. 2016;85(1):43–52. doi: 10.1016/j.ijmedinf.2015.10.004. [DOI] [PubMed] [Google Scholar]
- 31.Dagli R.J., Sharma A. Polypharmacy: a global risk factor for elderly people. J Int Oral Health. 2014;6(6):i–ii. [PMC free article] [PubMed] [Google Scholar]
- 32.Cooper R.J. I can’t be an addict. I am. Over-the-counter medicine abuse: a qualitative study. BMJ Open. 2013;3(6) doi: 10.1136/bmjopen-2013-002913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Murphy J.C. Americans make choices about self-care. Am J Health Syst Pharm. 2001;58(16):1494–1499. doi: 10.1093/ajhp/58.16.1494. [DOI] [PubMed] [Google Scholar]
- 34.McBride A.J., Pates R., Ramadan R., McGowan C. Delphi survey of experts’ opinions on strategies used by community pharmacists to reduce over-the-counter drug misuse. Addiction. 2003;98(4):487–497. doi: 10.1046/j.1360-0443.2003.00345.x. [DOI] [PubMed] [Google Scholar]
- 35.de Fátima Marin H., Delaney C. Chapter 10. Patient engagement and digital health communities. In: de Fátima Marin H., Massad E., Gutierrez M.A., Rodrigues R.J., Sigulem D., editors. Global Health Informatics. Academic Press; Cambridge, UK: 2017. pp. 218–231. [Google Scholar]