Abstract
Understanding the health-related quality of life (HrQoL) of hospitalized COVID-19 survivors is an emerging global challenge arising from the current pandemic. A qualitative study of the experiences of sixteen hospitalized COVID-19 survivors from Nanning City, China, was conducted using semi-structured telephone interviews in May 2020. These first-hand accounts were critically and empirically analysed to identify emerging health and social issues, and provide potential solutions to improve survivors’ quality of life. This in-depth, qualitative study of HrQoL for hospitalized COVID-19 survivors provides the first empirical evidence and conceptual framework with eight dimensions (physical symptoms, anxiety, trauma, economic loss, place-based identity, self-stigma, health self-interventions, and changing lifestyle) for understanding the physiological, psychological, socio-economic and health behavioral aspects of their daily lives. We argue that local and global governments should provide integrated healthcare, social and digital infrastructure to support this vulnerable group. More comparative and multi-disciplinary studies in this area are needed to generate academic standards of assessing health-related quality of life and produce good practice guidelines for promoting urban resilience in response to public health disasters.
Keywords: COVID-19, Health-related quality of life, COVID-19 survivors, Physical symptoms, Mental problems, Identity, Self-stigma, Nanning city
1. Introduction
The incidence and control of COVID-19 has varied spatially and temporally across China. With the first and highest concentration of COVID-19 patients within China, Wuhan city successfully and efficiently treated more than 40,000 patients (Health Commission of Hubei Province, 2020) by May 31, 2020. Other cities across China not only had a much smaller number of COVID-19 cases but also a higher proportion of mild cases and a lower incidence of ventilator use or admission to ICT (Immunochromatography) hospital units. However, all COVID-19 survivors might face the challenges of working, living and recovering. Previous studies on the quality of life of SARS survivors concluded that they were left with many health burdens including physical and mental health issues (Bonanno et al., 2008; Kwek et al., 2006; Lau et al., 2008). An understanding of the issues and challenges faced by COVID-19 survivors is necessary to deliver policies that can improve their health and well-being effectively. This study aims to identify the health and social issues faced by COVID-19 survivors through semi-structured interviews with a sample of sixteen hospitalized COVID-19 survivors from Nanning City, China.
The term ‘quality of life’ has been variously defined. The World Health Organization (WHO, 1958) stated that human health does not merely refer to the absence of disease, but is a status of complete physical, mental and social well-being. Quality of Life (QoL) is defined by the WHO as an ‘‘individual's perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards, and concerns'’ (1995, p. 1403). A more specific, health-related measure of quality of life (HrQoL) has been developed to appraise the impact of a disease and the effects of medical intervention on the quality of several domains of life (Arnold et al., 2004; Staquet et al., 1998). Evidence suggests different medical disorders, such as diabetes (Mielck et al., 2014) and HIV (Fleming et al., 2004), may impact HrQoL in different ways due to disease-specific factors. As such, disease-specific studies emphasize different dimensions of HrQoL. Consequently, HrQoL is a multidimensional construct that encompasses a broad range of domains, however, physical, psychological and social functioning are the most prevalent dimensions among HrQoL studies (Kalliopi, 2013).
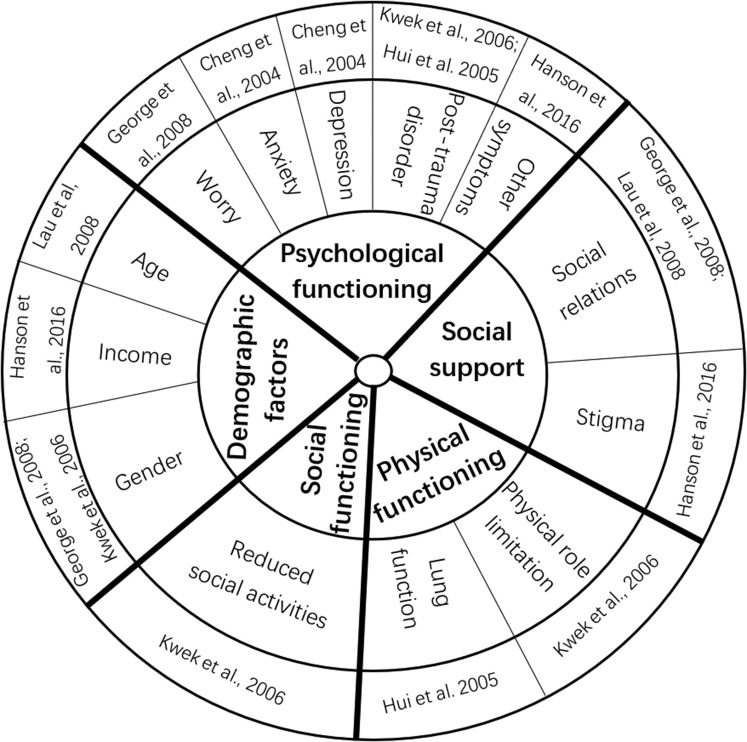
The outbreak of an infectious virus tends to cause a variety of health and social problems. Previous studies of SARS and Ebola survivors demonstrated that their HrQoL was associated with five key domains: physical functioning, psychological functioning, social support, social functioning and demographic factors (Fig. 1 ). This paper aims to explore HrQoL of hospitalized COVID-19 survivors, and its domains specific to Covid-19 pandemic.
Fig. 1.
The five domains and key measures of HrQoL of SARS and Ebola survivors (Cheng et al., 2004).
Since the COVID-19 pandemic began in December 2019 there has been an exponential growth of COVID-19 related studies. As of 24th August, 58,200 papers with COVID-19 in the title had been published according to Google scholar. Due to the largest-scale lockdown in human history, everyone's health has been affected to some extent. The health impacts of COVID-19 on different social groups, including the public (Zhang and Ma, 2020), healthcare professionals (Liu et al., 2020), people with underlying chronic diseases (Shalash et al., 2020), and people with suspected COVID-19 symptoms (Nguyen et al., 2020) have been investigated. Research into the effects of COVID-19 on physiological functions (Kowalik et al., 2020) has covered fever, coughs, shortness of breath, disturbance of smell and taste (Vaira et al., 2020; Gane et al., 2020), multiorgan failure (Bansal and Prasad, 2020), cardiovascular complications (Driggin et al., 2020), and potential post-viral sequelae such as demyelinating and neuromuscular complications (Troyer et al., 2020). Mental health studies (Zuercher et al., 2020) have found potential links between COVID-19 and anxiety and Post-Traumatic Stress Disorder (Mehrad, 2020; Cai et al., 2020), depression (Troyer et al., 2020; Cai et al., 2020), and sleep disorders (Tasnim et al., 2020).
COVID-19 survivors (>20 million as of August 24, 2020), like those of SARS (Hui et al., 2009) and Ebola (Hanson et al., 2016) will likely face difficult challenges in their daily life post COVID-19. In the first study of the quality of life of suspected COVID-19 patients, Nguyen et al. (2020), focusing on the link between health literacy and HrQoL, concluded that individuals with suspected COVID-19 symptoms had lower HrQoL than symptom-free individuals during the COVID-19 pandemic. As more and more COVID-19 patients are discharged from medical care, an increasing but still limited number of studies have focused on survivors' experiences, including their physical, psychological and social issues. For example, Zhao et al. (2020) reported radiological and physiological abnormalities in COVID-19 survivors three months after being discharged from hospital. Cai et al. (2020) showed that COVID-19 survivors had a higher incidence of psychological distress in the early recovery stage. Asare (2020) found that survivors were stigmatised by their communities. These studies explored specific domains of COVID-19 survivors' quality of life. The aim of this study is to provide a systematic, qualitative analysis of hospitalized COVID-19 survivors’ perceived health-related quality of life in the 3-month period after discharge and to provide suggestions on their future care.
2. Materials and methods
Grounded theory, a qualitative methodology that uses data to construct a theory about people's views, actions, and life experience within the context in which they live (Charmaz, 2014; Corner et al., 2019), was used in this study to explore the daily life and HrQoL of hospitalized COVID-19 survivors three months after being discharged from hospital.
2.1. Sample and recruitment
Nanning city, the capital of Guangxi Autonomous Region (a provincial unit), is situated in Southern China (Shen et al., 2020). Nanning city had reported 55 cases of COVID-19 by August 4, 2020 (Nanning Health Committee, 2020), far fewer than in Wuhan city. Study participants were recruited from a group of COVID-19 survivors discharged from the Fourth People's Hospital in Nanning city. Both purposive and snowball sampling were used to select participants for the study. Firstly, to achieve a maximum variation in gender, age, occupation, degree of infection, and duration of hospitalization, 13 participants identified by continuous screening were invited to be interviewed. Secondly, snowball sampling was used to make supplementary selections. A total of 16 individuals (Fig. 2 ) expressed interest in the study and consented to be interviewed. The interviewees were aged between 21 and 67. Fifteen interviewees had a moderate case of COVID-19 and one had a severe case. The interviewees had been hospitalized for between 10 and 28 days and were discharged from hospital between 6th February and March 2, 2020. All interviewees were required to quarantine for 14 days after being discharged.
Fig. 2.
Characteristics of the 16 invited interviewees (the codes of interviewees (1–16) followed by occupations).
2.2. Data collection
Demographic and clinical data (e.g. age, degree of infection and hospital length of stay) were collected from the interviewees' hospital case notes provided by the Fourth People's Hospital. All interviewees were anonymised to ensure their privacy. Due to ongoing lockdown, the semi-structured interviews were conducted via telephone between 6th-29th May 2020. Telephone interviews ensured the personal safety and security of the interviewer and interviewees (Chapple, 1999) and enabled data collection during lockdown. Each interview lasted between 1 and 1.5 h. The conversation started with a general question, “Do you have any problems, or anything to highlight, from your daily life experience after being discharged?”. The interview then proceeded with several open questions about multiple dimensions of quality of life, such as physical, mental, social, and cultural factors. The interviews were concluded with an open question, “What domains of life do you think our study on COVID-19 survivors should focus on?“. Participants were informed that they could answer each open question as they liked according to their personal experience and thoughts, and they were also encouraged to bring up new topics. All interviews were recorded using the telephone's recording function.
2.3. Data analysis
After being transcribed from the audio recordings, the interviews were coded and anonymised in preparation for direct quotation and critical analysis. The interview transcripts were analysed line-by-line using open coding, axial coding and selective coding (Corbin and Strauss, 2014; Khisa, 2016; Charmaz, 2014). Open coding is an initial step, in which data is repeatedly compared and contrasted until emergent themes or concepts (e.g. emotion) are identified. The second step, axial coding, involves analysing the relationships between emergent themes and combining them to form overarching groups (e.g. anxiety). The third step, selective coding, involves conducting an in-depth analysis of the links between independent groups, and identifying core dimensions (e.g. mental problems). The whole process of coding aims to generate a conceptual framework from the analysis (Corner et al., 2019).
3. Physical and mental health status
3.1. Physical symptoms
Due to the short observation period, medical complexity and individual differences among COVID-19 patients, there have not been any systematic analyses about the full array of potential side-effects post-treatment. In this study, the most commonly physical symptom reported by interviewees was fatigue, leading to diminished physical motion, as reported by Zhao et al. (2020) and Greenhalgh et al. (2020). Other symptoms and biomarkers mentioned during the interviews included hyperglycemia, hypertension, chest tightness, increased flatus, arthralgia, herpes zoster, palpitations, intercostal neuralgia, breathlessness, cough, throat pain, and irregular stools. The interviewees reported these as likely side-effects from the virus or its treatment because they did not have these health problems before. Some survivors appeared to suffer diabetes due to COVID-19, for example:
‘My friend and I were both found to have high levels of blood sugar during treatment of COVID-19 but we were both very healthy before. I am healthy now, but my friend has to take insulin now and might have to do so for the rest of his life, which is a bothersome challenge’ (Interviewee 9).
Some survivors had not visited hospital since being discharged except for the mandatory re-examinations even though they worried that their physical symptoms were indicative of potential health problems:
‘In hospital, I suffered with diarrhoea for three months during the treatment. I suspected that my liver has been damaged……Now I have a lot of farts’. (Interviewee 14).
Previous studies about other coronaviruses, like SARS and MERS, showed that there were respiratory, musculoskeletal, and neuropsychiatric sequelae (Das et al., 2017; Hosseiny et al., 2020; Hui et al., 2009; Lam et al., 2009; Moldofsky and Patcai 2011; Ngai et al., 2010). Although no clinical evidence exists to support the finding that these physical symptoms are directly related to COVID-19 or its treatment, the above symptoms indicate the high risk of physical health issues for survivors.
3.2. Mental problems
All interviewees had varying degrees of anxiety about their physical health status. This anxiety was most intense during the first month after being discharged, which concurs with Cai et al. (2020) conclusions that COVID-19 survivors had a higher incidence of psychological distress in the early recovery stage. In this period, they were particularly sensitive to and aware of their physical symptoms because they worried whether they were fully cured or would have a further positive RNA test. Some studies have reported a re-detectable positive result from a COVID-19 RNA test in some recovered patients (e.g. Qu et al., 2020). Worrying about such likelihood has increased survivors' anxieties. The uncertainties about their physical status somehow lead to self-stigma. As one interviewee explained, “I am not sure if I will infect others again after being treated in hospital. Any growth in the number of infected patients within the local neighbourhood will increase others' suspicions that I might spread the virus again. Given this, I try to stay at home as much as possible. Occasionally, I wander along the riverside at night when nobody is there” (Interviewee 9). However, some interviewees suggested their anxiety would “gradually decrease to normal levels when the results of several re-tests of COVID-19 infection are negative” (Interviewee 12).
Previous studies on SARS have indicated that survivors could develop long-term psychological disorders (Lee et al., 2007). Incidences of long-term psychological disorders following COVID-19 infection are currently unknown (e.g. more than 1 year), but some survivors in this study reported higher levels of anxiety for more than two months, which could be attributed to the following reasons. Firstly, their physical re-examinations showed some abnormal values (e.g. remaining inflammation in the lungs, or an absence of SARS-CoV-2 antibodies), which made them worry about adverse sequelae resulting from incomplete recovery. This has led to a continuous psychological burden, and even depression. Secondly, many interviewed survivors felt that was “no effective consultation service to support discharged COVID-19 survivors, such as an explanation of physical symptoms or the medical implications of re-test results (e.g. CT image), even by a phone call” (Interviewee 7).
After the National Health Commission of the People's Republic of China (2020) issued a requirement on February 19, 2020 to monitor and follow-up discharged COVID-19 patients, Nanning City's Fourth People's Hospital conducted two re-examinations and ran a four-week health monitoring programme, such as checking the temperature of survivors. However, in the absence of systematic, standardised programs and professional institutions to carry out effective follow-up monitoring of COVID-19 survivors, some interviewees reported feeling that there was currently “no tracking of our health status by professional institutions” (Interviewee 8, 13), or any opportunity to seek a professional opinion about their health. Thus, the hidden uncertainties about their future life has generated or exacerbated fear, depression, and anxiety. In addition, the interviewees tend to focus more on their physical state, due to low awareness of mental health effects, making it difficult to ease their anxiety. This is because Chinese people have a lower level of mental health awareness culturally than those in Western countries (Huang et al., 2019; Liu et al., 2011).
Furthermore, extensively exaggerated or unverified news about COVID-19 related impacts, such as reproductive impairment, have been spread via social media channels which can amplify uncertainty, fear and anxiety. Lee et al. (2007) also indicated that misinformation on the internet engendered unnecessary worries and fears amongst SARS survivors. For example, Interviewee 11 commented, “We saw the news online that the COVID-19 virus would remain in semen after treatment and infect our partner through sex, which really destroyed my whole family’. Such long-lasting anxiety occasionally caused physical symptoms, such as fever, or influenced social functions, by reducing social interaction and lowering capacity to work (Interviewee 3, 7).
Traumatic experiences primarily emerged in the period of COVID-19 suspicion and during quarantine before treatment. Loneliness as a result of separation from loved ones (Xiang et al., 2020; Cai et al., 2020), fear of death, worries about the physical health of their families (Cai et al., 2020), as well as uncertainty about the future life, generated or exacerbated anxiety and depression during pre-treatment quarantine, as Interviewee 8 recalled “I even wanted to die at that time. I was so scared that I couldn't sleep all night”, for some survivors these symptoms persisted post COVID-19 treatment (Cai et al., 2020). In addition to suffering from Covid-19, the traumatic experiences including continuous disturbance and negative reactions (e.g. blaming, gossiping) from society aggravated the survivors' psychological pressures and anxiety.
After being discharged from hospital, survivors in this study still received peculiar looks and felt they were intentionally avoided by many people. Similarly, Asare (2020) found that COVID-19 survivors have suffered stigma from members of their communities, leading to a form of ‘social death’. As shown in previous studies, survivors of SARS (Siu, 2008) and Ebola (Hanson et al., 2016) have been prone to shame and stigma. In this account, many survivors tended to internalise others' exclusionary behaviors and attitudes towards them, resulting in decreased self-esteem and feeling increased prejudice (Interviewees 4, 7, 11, 16), leading to feelings of sadness, low mood, anxiety, and difficulty sleeping.
However, our study has also found that several survivors have adapted to their new situations very quickly, without anxiety or self-stigma. They understand the societal impacts of COVID-19 so accept how other people communicate with them and are confident in their own lifestyles (Interviewee 10, 12).
4. Socio-economic impacts
4.1. Economic losses
The COVID-19 pandemic and associated lockdown measures have caused an inevitable global economic recession (Fernandes, 2020). Social distancing regulations have made it particularly difficult for small businesses, such as restaurants, coffee shops, pubs and bars, to operate normally during lockdown. It is widely acknowledged there will be job losses or reduced income (Collie et al., 2020).
The hospitalized survivors in this study are likely to face more economic challenges than healthy people. First, they reported being left out by employers or employees. As the owner of a garment shop with concerns about high rent and no business during lockdown, Interviewee 11 said that she was only able to visit her shop in June even though she had been discharged from hospital in March. Her employees had threatened to resign if she came to the shop earlier. Second, those survivors without permanent jobs (e.g. migrant workers) are likely to struggle to find a new job during the pandemic period. According to some interviewees (4, 6, 9), self-stigma and decreased physical capacity can destroy confidence and delay plans for seeking jobs.
4.2. Place-based identity of survivors
Identity is conceptualized as how a person makes sense of himself/herself, in relation to others and local places in everyday life (Hopkins and Pain, 2007). Identities are constantly re-configured over time and in different socio-spatial contexts (Meijering et al., 2016). Place and identity may facilitate social and spatial exclusion or inclusion, including divisions between different places, as well as between groups of people (Fried, 2000; Dixon and Durrheim, 2000; Brown et al., 2019). The 16 hospitalized survivors we interviewed were exposed to multiple tones of communication: emotionally positive, neutral and negative. For example, government officers were supportive and friendly during contact but communication with neighbours was relatively negative. Similarly, these survivors felt their sense of identity varied by place (home, neighbourhood, workplace, medical site and virtual space). Both their identities and the places in which they do everyday activities have been redefined as a consequence of their post-COVID-19 experiences.
At home, the survivors were perceived as people who have been cured but still needed informal care. Home is a place of refuge from the outside world, where people feel a sense of belonging (Rowles and Bernard, 2013; Meijering et al., 2016). Our interviewees had stayed in hospital and been in quarantine for 1–2 months, during which they experienced physical pain, fear and loneliness. The positive support, care and communication from their families helped relieve the psychological pressure they felt and increased their confidence to some extent (Interviewee 3, 5). The need for family support also affected the identities and homes of the interviewees' partners, and sometimes children, who often became informal caregivers. ‘Home’ functioned as a private, safe and familiar place; a shelter or sanctuary to escape from public stigma; a place providing informal care, as well as a spatial symbol of being cured and becoming a ‘normal’ person again.
By contrast, the neighbourhoods and workplaces were demarcated as sites of exclusion for COVID-19 survivors, who were perceived as a life threatening rather than a vulnerable group, and cast as “potential contaminating influences in these settings” (Laurie and Richardson, 2020, p14.). Neighbourhood is the place where the survivors reside and physically interact with other members. Several studies have shown that neighbourhood environments can impact people's well-being outcomes, including the onset of ill-health, and as such its influence is significant (Walsh and Urbaniak, 2018; Freedman et al., 2011; Marquet and Miralles-Guasch, 2015). Although the physical distance between survivors and other people in their neighbourhood was small, the psychological distance between them was much greater, due to negative attitudes to their COVID-19 infection. Almost all the interviewed survivors felt intentional, purposeful and even aggressive avoidance, blame and gossip from their neighbours, which has led to a strong fear of any physical and social contact after being discharged from hospital. The use of physical disguises (in the form of glasses, heavy coat, masks and caps/hats) has become part of their strategy of managing social stigma, with the aim of not being seen in public. The excluding reactions in the neighbourhood may be partly explained by the prevalence of shared communal areas and building entrances/lifts in residential buildings in which social distancing is difficult to implement effectively, even if face masks are worn.
In the workplace the physical distance between survivors and their colleagues was slightly greater than that between neighbours, whereas the psychological pressure from the workplace was less than that from their neighbourhood. New virtual working patterns have greatly reduced physical contact or social interaction between colleagues. The survivors were still aware of “widespread of gossip but did not feel targeted individually” (Interviewee 13).
In contrast to the above, in a medical site (hospital), the survivors were perceived as discharged patients who were cured and at low-risk for spreading the virus. Throughout the whole process from diagnosis, treatment and re-examination, doctors showed physical, mental and emotional support for patients by providing high confidence in friendly ways (Interviewees 1, 3, 13), which made the survivors feel like “normal patients” (Interviewee 13).
The virtual space is a both positive/inclusive and negative/exclusive place for COVID-19 survivors interviewed. On the one hand, survivors were perceived positively as COVID-19 victims who had ‘success stories’ of fighting the virus. A variety of groups including relatives, some neighbours, colleagues, friends and netizens, delivered caring, encouraging and supportive messages to survivors via social media (e.g. WeChat) or phone calls. The positive attitudes in virtual space or the online world, including enquiries about the provision of good quality food (Interviewees 8, 14), had a positive impact on the mental health of survivors. People wished to help survivors where there was no risk of infection. On the other hand, several government offices were required to provide details of close contacts for tracing purposes. It was found that agencies dealing with survivors' personal data did not protect it adequately. In some cases, it was possible for personal information to be combined with other information to identify a specific individual (Tao, 2019). In this account, it was not difficult to determine who had the virus according to personal information (e.g. residence location, surname) released publicly. Many interviewees felt that they were completely exposed to the public, almost everyone in their social circles knew they had been infected by the virus. At once, survivors received a great deal of disturbing calls and messages from friends, workplaces (employers and colleagues) and neighbours, even some of whom, particularly neighbours, blamed them and spread their gossips on social media platforms (Interviewees 1, 5, 7, 14).
It is clear that these survivors felt more excluded in both physical and virtual places closer to their everyday life. The lack of knowledge about this new virus (e.g. spread, infection and side-effects), and the reality that no remedy or vaccine for COVID-19 has yet been developed (Cascella et al., 2020) during the study period, increased the public perception of life-threatening health risks from COVID-19 survivors. This has lead to continuously avoiding physical contact with infected people. Moreover, the government appears more concerned about minimising infection rates during the pandemic; for example, a quickly published scheme for fighting COVID-19 (BDPC, 2020), while the quality of life of COVID-19 survivors has not been considered adequately which indicates a lack of awareness of this vulnerable group's needs.
5. Health behaviors
5.1. Health self-interventions
The hospitalized COVID-19 survivors were advised by doctors that more physical exercise would help improve their physical condition and rehabilitate their health. Several self-help strategies were recommended during the 14-day quarantine after hospital discharge including rubbing the lung area with their hands, deep breathing and chest-expanding exercises (Interviewee 2, 3, 9, 13).
After quarantine, survivors were allowed to do more physical exercise outside. Some survivors intended to increase physical exercise by walking and jogging in the residential quarter or nearby parks in late evening or at night. It was found that the majority of survivors wanted to reinstate their former good physical health by doing more physical exercise and activities (e.g. Interviewee 1), which was also reported by Greenhalgh et al. (2020). However, some were afraid of being recognized and blamed by neighbours and acquaintances, so most survivors chose to stay at home. Interviewee 13 reported that their “limited indoor space and decrease in physical fitness due to fatigue” made them give up any physical activity. On the seventh day after being discharged from hospital, Interviewee 3 could only run 200–300 m before feeling breathless and faint compared to running 10,000 m pre-infection. Faced with such changes, survivors wished to receive professional guidance on exercising.
Owing to the aforementioned physical symptoms (e.g. fatigue), some survivors were encouraged by information about the effectiveness of traditional Chinese medicine for treating COVID-19 (Zhang et al., 2020) in the mass and social media, and they decided to take traditional Chinese medicines prescribed by doctors or suggested in online government guidelines. Interviewee 8 said, “both me and my wife felt better and more relaxed after taking the medicine bought from a pharmacy”.
5.2. Changing lifestyles
During the interview the survivors were asked to consider any changes about their lifestyles compared with pre COVID-19. More physical exercise and a healthier diet were frequently identified, because they believed that a lack of physical exercise and an unhealthy diet may have reduced their immunity to COVID-19, as explained by Interviewee 9:
“I was very healthy and strong before, for example, I can take cold-water showers even in winter. But I have been travelling for business these past years so family life and exercise were very limited, and my diet was not very healthy. All these have made me more susceptible to the virus by decreasing my immunity. That is why only I got infected but my family and others working in my restaurant were all fine” (Interviewee 9).
A family cluster case is one of the typical patterns of COVID-19 infection caused by person-to-person transmission (Chan et al., 2020). When family members are simultaneously infected with COVID-19 the psychological and economic consequences are considerable. In that circumstance Interviewee 1 spoke of being able to do nothing except encourage and care for each other with great compassion during treatment, and support each other in dealing with the likely social stigma after hospital discharge. The co-experience of suffering from the disease and the anticipation of facing more challenges in the future has, to some extent, enhanced the close relationship among family members. Some survivors highlighted that they had changed their conventional views of life and were prioritising family togetherness (Interviewee 1, 2, 4, 5, 8, 13, 15). As Interviewee 13 reflected, “there has only been work all my life, never thinking about myself or my family. But my husband was severely affected by COVID-19 and nearly died, I felt that death was so close to me for the first time. After this disaster, I have realised I must separate work from living. I will look after and care about my family as much as possible” (Interviewee 13).
6. Discussion
The Interviewee accounts in this study have confirmed several negative physical, mental and social experiences that hospitalized COVID-19 survivors face (Table 1 ). As the pandemic continues, it is likely that more problems of post COVID-19 will be discovered, and that these will exhibit spatial, temporal and social heterogeneity explained by complex factors. Improving the quality of life of COVID-19 survivors is an emerging global challenge in the post-COVID-19 era.
Table 1.
The specific impacts of COVID-19 on HrQoL of hospitalized survivors.
| Results | Quotes (Interviewee Code) | Results | Quotes (Interviewee Code) |
|---|---|---|---|
| Fatigue | 1, 2, 5, 9, 15 | Anxiety | 1, 3, 4, 5, 6, 7, 8, 11, 12, 13, 14, 15, 16 |
| Hyperglycemia | 9 | ||
| Hypertension | 3 | Trauma | 5, 7, 8, 12 |
| Chest tightness | 2 | ||
| Increased flatus | 14 | Self-stigma | 4, 6, 7, 9, 16 |
| Arthralgia | 13, 14, 15 | ||
| Herpes zoster | 16 | Economic losses | 6, 9, 11, 16 |
| Palpitations | 3 | ||
| Intercostal neuralgia | 11 | Exclusive identity in some places (particularly neighbourhood) | 4, 5, 6, 7, 8, 11, 12, 13, 15 |
| Breathlessness | 1, 3, 7, 9 | Health Self-interventions (exercises and Traditional Chinese medicines) | 1, 2, 3, 7, 8, 9, 13 |
| Cough | 13 | ||
| Throat pain | 2 | More physical exercise and a healthier diet | 4, 7, 8, 9, 13 |
| Irregular stools | 4, 14 | ||
| Diabetes | 9 | Family togetherness | 1, 2, 3, 4, 5, 7, 8, 13, 15 |
6.1. Physical problems
Current communication between survivors and professional doctors is dominated by (mandatory) regular re-examinations at a designated hospital. In the case of Nanning City, hospitalized COVID-19 survivors were re-examined two times after discharge from the Fourth People's Hospital. Re-examinations include chest CT screening and other tests depending on the health status of survivors. However, minor or daily physical health issues (e.g. fatigue and breathlessness) underlay survivors' anxiety and depression, and the uncertainties about the post-COVID-19 physical dysfunction or sequela contribute to survivors' desires to be continuously monitored and treated in the future. However, Interviewee 8 reported that requests for further help were not always followed up effectively, “after being discharged from hospital, except for two mandatory re-examinations and monitoring within one month, I requested longer monitoring and treatment from the hospital for free. However, I have not received effective feedback from the doctors I contacted because of my current normal test results. This is one of my biggest concerns about COVID-19 rehabilitation.”
Greenhalgh et al. (2020) suggested that a pulse oximetry can be used for assessing and monitoring physical health of COVID-19 survivors, but its measurement is sensitive and vulnerable to many factors, for example, the finger has to be clean, dry, warm and without nail polish. On this account, virtual monitoring and diagnosis through digital infrastructure could offer feasible solutions. For example, mobile systems, together with a variety of sensors, have been extensively used for data collection (e.g. via an app) due to their diverse strengths including portability. An easy-to-use and home-based dynamic monitoring system for COVID-19 could consist of wearable sensors, a smart phone app, and a cloud platform. Such a system could collect data on many key biomarkers such as body temperature distributions, skin blood flow, sweating rates, heart rate, physiological stress, heat stress or cold stresses via a small-sized chip attached to clothing or a wearable device. A health-risk estimation model could be developed based on the time-series data captured by survivors on a regular basis (e.g. every 6 h) and a warning message on likely occurrence of high risks could be sent to a hospital doctor for further diagnosis and intervention.
6.2. Health intervention
For post-COVID-19 rehabilitation, the healthcare knowledge plays an important role. For example, Interviewee 9 was very confident of his rehabilitation because he was able to receive medical advice from his brother. “As a doctor of Chinese medicine, my brother advised me to take some traditional Chinese medicine for one week or so after the hospital discharge. He told me a lot about this disease, so I understand that COVID-19 has damaged my stomach, liver and kidney to some extent so my rehabilitation will take at least 6 months, or even a year.” Another survivor explained, “based on the medicines and prescriptions issued online by the government, I have purchased some Chinese traditional medicine from pharmacy shops. Both my wife and myself are taking the medicine together and are feeling much better now, which has relaxed our anxiety’ (Interviewee 8).
However, most survivors did not have good access to quality COVID-19 related health information, and instead relied on mis- (and dis-) information via social media or other people. Correct and timely online guidance not only helps solve short-term demand for emerging healthcare needs but also reduces long-term anxiety and depression. Moreover, it is imperative to disseminate accurate information by trusted medical organisations including hospitals, because people often trust and comply with doctors (Ruiming et al., 2015). Doctors or health professionals could provide the instruction of health self-intervention to help the rehabilitation, such as breathing control exercises suggested by Homerton University Hospital (2020).
6.3. Anxiety, trauma and self-stigma
It is imperative that the government and medical institutions provide psychological intervention and mental support for COVID-19 patients in both pre- and post-treatment periods. As interviewee 8 strongly recommends, paying more attention to the mental status of patients in the period of COVID-19 suspicion and during quarantine before treatment, because the fear and loneliness of that time “really drove people crazy”.
Except for worries about the uncertainties of their physical health, social interactions are also strongly associated with COVID-19 survivors' mental issues (i.e. anxiety, trauma, self-stigma) in this study. Unclear COVID-19 related knowledge is the parameter leading to other's negative responses to survivors. For example, Interviewee 13 said, “I think experts and governments should be more concerned about the mental health of survivors and other people's misunderstandings about us. If we have been treated successfully and will not spread the virus anymore, experts should explain this to the public through press releases. There has been unclear, or very ambiguous guidance on health management.”
Recently, virtual, augmented and mixed reality (VR/AR/MR) technologies have stimulated large-scale applications for mental health and physical rehabilitation (Alemanno et al., 2019; Park et al., 2019; Vieira et al., 2018). The strengths of VR/AR/MR technologies include complete immersion into a simulated environment using a headset such as HTC vive. The 5G technology enables reliable, robust, fast and affordable/free development and application of virtual reality techniques into health care, learning and planning. Given the high cost of VR hardware and software, it would be more cost effective to build a VR rehabilitation centre in the hospital so all survivors can access the training and use it freely or at low cost. The VR centre could help treat survivors'self-stigma if specifically designed for this purpose.
6.4. Social and economic exclusion identity
The ongoing pandemic, with its considerable health consequences, has sparked much debate about the inequities and social injustices experienced by those affected by COVID-19. COVID-19 survivors have become a vulnerable group excluded from many social and economic activities. Firstly, the leakage of personal data including name, affiliation and location has increased social stigma against this group, which also reported by Bao et al. (2020). There should be better, more regulated procedures to ensure information transparency and data protection. Secondly, as survivors felt being most excluded in neighborhoods, locally relevant solutions are relevant at the community level and for cross-sector collaborations. In the future, the resilient neighbourhood design (Jefferies et al., 2020) could take account of social innovation in response to emerging disasters. Thirdly, survivors may lose their jobs due to a decreased capacity for physical work. This raises the issue of how governments and employers will provide financial support for survivors and their families, including subsequent healthcare costs.
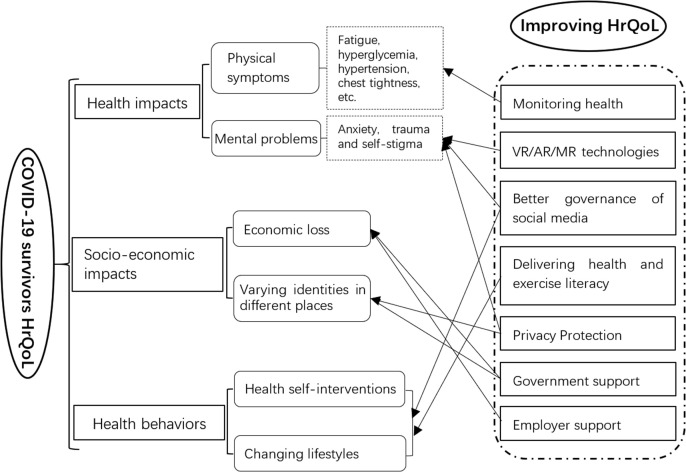
Based on the issues raised and discussed from the Nanning City case study, a framework for improving the HrQoL of COVID-19 survivors is proposed (Fig. 3 ).
Fig. 3.
A proposed framework for improving the HrQoL of hospitalized COVID-19 survivors.
7. Conclusions
Through this small-scale qualitative study, this paper has produced the first evidence of the health, social, economic and digital issues affecting hospitalized COVID-19 survivors' health-related quality of life. We identified eight dimensions affecting COVID-19 survivors’ HrQoL: physical symptoms, anxiety, trauma, economic loss, place-based identity, self-stigma, health self-interventions, and changing lifestyles. These dimensions are intertwined. Combined, these represent a conceptual model for understanding HrQoL of COVID-19 survivors, reflecting a range of physical, psychological and social-economic concerns.
First of all, the physical and mental health of COVID-19 survivors needs continuous monitoring and treatment, taking account of variations on a case-by-case basis. Secondly, the place-based identity and self-stigma have resulted in significant social and economic exclusion of COVID-19 survivors, which makes them increasingly vulnerable. Thirdly, there is a conflict between sharing patients health information and protecting their privacy. The former is crucial to combat COVID-19 but the latter creates social inequality and has an adverse impact on survivors' quality of life. Fourthly, improving survivors’ quality of life requires governmental, digital and spatial interventions to provide knowledge (e.g. self-intervention), as well as place-based (e.g. exercise), medical, social and economic support at various scales.
Self-stigma, as demonstrated among COVID-19 survivors in this study, is prejudice against oneself. This issue was rarely observed in studies about the HrQoL of patients infected by Ebola (Hanson et al., 2016), SARS (Siu, 2008), and HIV (Xu et al., 2017). Its occurrence in this study is largely caused by the uncertainties about incomplete recovery or re-infection and the public exclusive behaviors. More behavioral studies should be conducted in the future to understand not only the causes of self-stigma but also psychological solutions.
It is also interesting to see that survivors have a more positive sense of identity in places away from their daily lives in both physical and virtual spaces. This is because virus transmission is dependent on physical distance and density. Besides, it should be noted that the majority of hospitalized COVID-19 survivors determined to change their lifestyles by spending more time with family and achieving a better balance between working and living. The idea of lockdown urbanism proposed by Jefferies et al. (2020) should include such positive reflections from a vulnerable survivor group.
It is clear from this study that digital infrastructure can have a positive or negative impact on quality of life. In previous studies on SARS and Ebola survivors, digital technology was not in widespread use. However, it is now suggested that digital factors should be added as a ninth dimension of health-related quality of life. Digital applications used in fighting against COVID-19 should be critically reviewed in the post pandemic era. This could provide guidelines for digital responses to future public health disasters.
Many studies, such as Hanson et al. (2016), indicate that traumatic experiences (e.g. watching other people suffering or even deaths) during medical treatment in care units created mental problems (e.g. PTSD) of discharged patients. However, this study reported that the traumatic experiences of COVID-19 survivors are overwhelmingly caused by their social interactions, particularly with neighbours, rather than the process of medical treatment. It suggested that more research should examine how to minimize social negative impacts on COVID-19 infected people (e.g. processing personal data with desensitization) when combating COVID-19 pandemic.
There are limitations in this empirical study. The HrQoL findings in this study are subjectively formulated (Matza et al., 2004) by centering on the self-assessment of 16 hospitalized COVID-19 survivors within 3 months from discharge. Thereby, the generalized conceptual model developed from this small sample (e.g. only one severe case among the interviewees) requires further examination employing a wider range of COVID-19 survivor cases, with heterogeneous attributes of health, treatment, gender and family. In particular, those COVID-19 survivors, who were not hospitalized or treated within an ICU, should be included for comparative purposes. In addition to the self-assessment of patients, the third-party assessment from other stakeholders such as health professionals, colleagues, neighbours and communities, and networking friends, enables holistic understanding of the various impacts and solutions within different situations. Combating COVID-19 is a complicated dynamic process affected by heterogeneous political, technical, social, economic, and cultural factors. The findings from this small-scale pilot study (proof of concept), need verifying and further development by additional studies in other cities and countries across a range of contexts. In addition, the HrQoL metrics proposed here, with its multiple domains and dimensions, needs to be substantiated with additional data sets and quantitative analysis across multiple disciplines (e.g. medicine). Moreover, further works implementing the proposed working model (e.g. healthcare technology, data protection policy, governance, and economic climate) that affect long-term HrQoL of COVID-19 survivors in societies, will need continuous monitoring and assessment through larger-scale inter-disciplinary projects. For example, the advent of vaccines against the virus might significantly reduce the public's fear of COVID-19, thereby reversing negative attitudes towards the patients, which largely impacts the HrQoL of COVID-19 survivors. The follow-up interviews with survivors are planned for May 2021 (one year on from the first investigation), with aims to explore any significant changes in these issues and solutions.
Credit author statement
Chenhui Wu: Conceptualization, Methodology, Formal analysis, Investigation, Writing – original draft, Writing – review & editing, Visualization, Data curation, Jianquan Cheng: Conceptualization, Formal analysis, Writing – original draft, Writing – review & editing, Supervision, Jun Zou: Validation, Writing – review & editing, Resources, Project administration, Lian Duan: Writing – review & editing, Funding acquisition, Janis E. Campbell: Writing – review & editing
Acknowledgment
We greatly appreciate the constructive and critical comments from Professor Samantha Baron at the Open University, UK. This study was funded by Chinese Academy of Engineering (grant number: 2020-XY-61-01), National Natural Science Foundation of China (grant number: 41961062), Guangxi Natural Science Foundation (grant number: 2018JJA150089).
References
- Arnold R., Ranchor A.V., Sanderman R., et al. The relative contribution of domains of quality of life to overall quality of life for different chronic diseases. Qual. Life Res. 2004;13(5):883–896. doi: 10.1023/B:QURE.0000025599.74923.f2. [DOI] [PubMed] [Google Scholar]
- Asare N.K.O. 2020. Stigma as a Social Death for COVID‐19 Survivors in Ghana.https://www.researchgate.net/publication/341342665_Stigma_as_a_Social_Death_for_COVID-19_Survivors_in_Ghana [Google Scholar]
- Alemanno F., Houdayer E., Emedoli D., et al. Efficacy of virtual reality to reduce chronic low back pain: proof-of-concept of a non-pharmacological approach on pain, quality of life, neuropsychological and functional outcome. PloS One. 2019;14(5) doi: 10.1371/journal.pone.0216858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonanno G.A., Ho S.M.Y., Chan J.C.K., et al. Psychological resilience and dysfunction among hospitalized survivors of the SARS epidemic in Hong Kong: a latent class approach. Health Psychol. 2008;27(5):659. doi: 10.1037/0278-6133.27.5.659. [DOI] [PubMed] [Google Scholar]
- Bansal A., Prasad J.B. Liver profile in COVID-19: a meta-analysis. J. Public Health. 2020 doi: 10.1007/s10389-020-01309-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown K., Adger W.N., Devine-Wright P., et al. Empathy, place and identity interactions for sustainability. Global Environ. Change. 2019;56:11–17. [Google Scholar]
- Bureau of Disease Prevention and Control (BDPC), China . second ed. 2020. The Scheme of Fighting Covid-19.http://www.nhc.gov.cn/jkj/s3577/202001/c67cfe29ecf1470e8c7fc47d3b751e88.shtml [Google Scholar]
- Bao H., Cao B., Tang W. Digital media's role in COVID-19 pandemic (preprint) JMIR mhealth and uhealth. 2020;8(9) doi: 10.2196/20156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai X., Hu X., Ekumi I.O., et al. Psychological distress and its correlates among COVID-19 survivors during early convalescence across age groups. Am. J. Geriatr. Psychiatr. 2020;28(10):1030–1039. doi: 10.1016/j.jagp.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collie A., Sheehan L., van Vreden C., et al. medRxiv; 2020. Psychological Distress Among People Losing Work during the COVID-19 Pandemic in Australia. [Google Scholar]
- Corner E.J., Murray E.J., Brett S.J. Qualitative, grounded theory exploration of patients' experience of early mobilisation, rehabilitation and recovery after critical illness. BMJ open. 2019;9(2) doi: 10.1136/bmjopen-2018-026348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charmaz K. second ed. Sage; London: 2014. Constructing Grounded Theory. [Google Scholar]
- Corbin J., Strauss A. Sage publications; 2014. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. [Google Scholar]
- Cheng S.K.W., Wong C.W., Tsang J., et al. Psychological distress and negative appraisals in survivors of severe acute respiratory syndrome (SARS) Psychol. Med. 2004;34(7):1187. doi: 10.1017/s0033291704002272. [DOI] [PubMed] [Google Scholar]
- Chapple A. The use of telephone interviewing for qualitiative research. Nurse Res. 1999;6(3):85. through 2013. [Google Scholar]
- Cascella M., Rajnik M., Cuomo A., et al. StatPearls Publishing; 2020. Features, Evaluation and Treatment Coronavirus (COVID-19) //Statpearls [internet] [PubMed] [Google Scholar]
- Chan J.F.W., Yuan S., Kok K.H., et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Driggin E., Madhavan M.V., Bikdeli B., et al. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J. Am. Coll. Cardiol. 2020;75(18):2352–2371. doi: 10.1016/j.jacc.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das K.M., Lee E.Y., Singh R., et al. Follow-up chest radiographic findings in patients with MERS-CoV after recovery. Indian J. Radiol. Imag. 2017;27(3):342. doi: 10.4103/ijri.IJRI_469_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon J., Durrheim K. Displacing place identity: a discursive approach to locating self and other. Br. J. Soc. Psychol. 2000;39(1):27–44. doi: 10.1348/014466600164318. [DOI] [PubMed] [Google Scholar]
- Fleming C.A., Christiansen D., Nunes D., et al. Health-related quality of life of patients with HIV disease: impact of hepatitis C coinfection. Clin. Infect. Dis. 2004;38(4):572–578. doi: 10.1086/381263. [DOI] [PubMed] [Google Scholar]
- Fried M. Continuities and discontinuities of place. J. Environ. Psychol. 2000;20:193–205. [Google Scholar]
- Freedman V.A., Grafova I.B., Rogowski J. Neighborhoods and chronic disease onset in later life. Am. J. Publ. Health. 2011;101:79–86. doi: 10.2105/AJPH.2009.178640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandes N. 2020. Economic Effects of Coronavirus Outbreak (COVID-19) on the World Economy. Available at: SSRN 3557504. [Google Scholar]
- Gane S.B., Kelly C., Hopkins C. Isolated sudden onset anosmia in COVID-19 infection. A novel syndrome. Rhinology. 2020;10 doi: 10.4193/Rhin20.114. [DOI] [PubMed] [Google Scholar]
- Greenhalgh T., Knight M., Buxton M., et al. Management of post-acute covid-19 in primary care. Bmj. 2020;370 doi: 10.1136/bmj.m3026. [DOI] [PubMed] [Google Scholar]
- Health Commission of Hubei Province, China . 2020. Epidemic Situation of Covid-19 in Hubei Province on 31 May, 2020.http://wjw.wuhan.gov.cn/ztzl_28/fk/yqtb/index.shtml [Google Scholar]
- Hanson J., Decosimo A., Quinn M. Diminished quality of life among women affected by Ebola. Journal of Social, Behavioral, and Health Sciences. 2016;10(1):11. [Google Scholar]
- Hosseiny M., Kooraki S., Gholamrezanezhad A., et al. Radiology perspective of coronavirus disease 2019 (COVID-19): lessons from severe acute respiratory syndrome and Middle East respiratory syndrome. Am. J. Roentgenol. 2020;214(5):1078–1082. doi: 10.2214/AJR.20.22969. [DOI] [PubMed] [Google Scholar]
- Hui D.S., Wong K.T., Antonio G.E., et al. Long-term sequelae of SARS: physical, neuropsychiatric, and quality-of-life assessment. Hong Kong medical journal= Xianggang yi xue za zhi. 15: 21.Huang D, Yang L H, Pescosolido B A., 2019. Understanding the public's profile of mental health literacy in China: a nationwide study. BMC Psychiatr. 2009;19(1):20. [PubMed] [Google Scholar]
- Hopkins P., Pain R. Geographies of age: thinking relationally. Area. 2007;39:287–294. doi: 10.1111/j.1475-4762.2007.00750.x. [DOI] [Google Scholar]
- Homerton University Hospital . 2020. Post COVID-19 Patient Information Pack.https://www.hackneycitizen.co.uk/wp-content/uploads/Post-COVID-19-information-pack-5.pdf [Google Scholar]
- Jefferies T., Cheng J., Coucill L. Lockdown urbanism: covid-19 lifestyles and liveable futures opportunities in wuhan and manchester. Cities and Health. 2020 doi: 10.1080/23748834.2020.1788771. [DOI] [Google Scholar]
- Kwek S.K., Chew W.M., Ong K.C., et al. Quality of life and psychological status in survivors of severe acute respiratory syndrome at 3 months postdischarge. J. Psychosom. Res. 2006;60(5):513–519. doi: 10.1016/j.jpsychores.2005.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalliopi M. Quality of life in chronic disease patients. Health Psychology Research. 2013;1(3):e27. doi: 10.4081/hpr.2013.e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kowalik M.M., Trzonkowski P., Łasińska-Kowara M., et al. COVID-19—toward a comprehensive understanding of the disease. Cardiol. J. 2020;27(2):99–114. doi: 10.5603/CJ.a2020.0065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khisa A. University of Nairobi; 2016. A Grounded Theory of Regaining Normalcy: Health Seeking Behaviour and Reintegration of Patients with Obstetric Fistula in Kenya. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau A.L.D., Chi I., Cummins R.A., et al. The SARS (Severe Acute Respiratory Syndrome) pandemic in Hong Kong: effects on the subjective wellbeing of elderly and younger people. Aging Ment. Health. 2008;12(6):746–760. doi: 10.1080/13607860802380607. [DOI] [PubMed] [Google Scholar]
- Liu X., Shao L., Zhang R., et al. 2020. Perceived Social Support and its Impact on Psychological Status and Quality of Life of Medical Staffs after Outbreak of SARS-CoV-2 Pneumonia: a Cross-Sectional Study. Available at: SSRN 3541127. [Google Scholar]
- Lam M.H.B., Wing Y.K., Yu M.W.M., et al. Mental morbidities and chronic fatigue in severe acute respiratory syndrome survivors: long-term follow-up. Arch. Intern. Med. 2009;169(22):2142–2147. doi: 10.1001/archinternmed.2009.384. [DOI] [PubMed] [Google Scholar]
- Laurie N., Richardson D. Geographies of stigma: post‐trafficking experiences. Trans. Inst. Br. Geogr. 2020 [Google Scholar]
- Lee A.M., Wong J.G., McAlonan G.M., et al. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can. J. Psychiatr. 2007;52(4):233–240. doi: 10.1177/070674370705200405. [DOI] [PubMed] [Google Scholar]
- Liu J., Ma H., He Y.L., et al. Mental health system in China: history, recent service reform and future challenges. World Psychiatr. 2011;10(3):210. doi: 10.1002/j.2051-5545.2011.tb00059.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mielck A., Vogelmann M., Leidl R. Health-related quality of life and socioeconomic status: inequalities among adults with a chronic disease. Health Qual. Life Outcome. 2014;12(1):1–10. doi: 10.1186/1477-7525-12-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moldofsky H., Patcai J. Chronic widespread musculoskeletal pain, fatigue, depression and disordered sleep in chronic post-SARS syndrome; a case-controlled study. BMC Neurol. 2011;11(1):37. doi: 10.1186/1471-2377-11-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehrad A. 2020. Post-traumatic Stress Disorder (PTSD) Effect of Coronavirus (COVID-19) Pandemic and Role of Emotional Intelligence. [Google Scholar]
- Meijering L., Nanninga C.S., Lettinga A.T. Home-making after stroke. A qualitative study among Dutch stroke survivors. Health Place. 2016;37:35–42. doi: 10.1016/j.healthplace.2015.11.006. [DOI] [PubMed] [Google Scholar]
- Marquet O., Miralles-Guasch C. Neighbourhood vitality and physical activity among the elderly: the role of walkable environments on active ageing in Barcelona, Spain. Soc. Sci. Med. 2015;135:24–30. doi: 10.1016/j.socscimed.2015.04.016. [DOI] [PubMed] [Google Scholar]
- Matza L.S., Swensen A.R., Flood E.M., et al. Assessment of health-related quality of life in children: a review of conceptual, methodological, and regulatory issues. Value Health. 2004;7(1):79–92. doi: 10.1111/j.1524-4733.2004.71273.x. [DOI] [PubMed] [Google Scholar]
- Ngai J.C., Ko F.W., Ng S.S., et al. The long‐term impact of severe acute respiratory syndrome on pulmonary function, exercise capacity and health status. Respirology. 2010;15(3):543–550. doi: 10.1111/j.1440-1843.2010.01720.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nanning Health Committee, China . 2020. Epidemic Situation of Covid-19 in Nanning in August 4.http://wjw.nanning.gov.cn/gzdt/bjdt/t4384507.html 2020. [Google Scholar]
- Nguyen H.C., Nguyen M.H., Do B.N., et al. People with suspected COVID-19 symptoms were more likely depressed and had lower health-related quality of life: the potential benefit of health literacy. J. Clin. Med. 2020;9(4):965. doi: 10.3390/jcm9040965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Health Commission of the People’s Republic of China . 2020. The Notification of Doing Monitoring and Follow-Up Work of COVID19 Discharged Patients.http://www.nhc.gov.cn/xcs/zhengcwj/202002/0572eef930d5441c96181c44a1fca878.shtml [Google Scholar]
- Park M., Ko M.H., Oh S.W., et al. Effects of virtual reality-based planar motion exercises on upper extremity function, range of motion, and health-related quality of life: a multicenter, single-blinded, randomized, controlled pilot study. J. NeuroEng. Rehabil. 2019;16(1):122. doi: 10.1186/s12984-019-0595-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qu Y.M., Kang E.M., Cong H.Y. Positive result of SARS-Co-2 in sputum from a cured patient with COVID-19. Trav. Med. Infect. Dis. 2020 doi: 10.1016/j.tmaid.2020.101619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiming L., Shuangmiao W., Liquan Ch, et al. Construction of doctors' power and authority: the operation mode two of the doctor and patient rights (power) from the perspective of interaction. Chinese Hospital Management. 2015;35(10):13–15. [Google Scholar]
- Rowles G.D., Bernard M. In: Environmental Gerontology. Rowles G.D., Bernard M., editors. Springer; New York: 2013. The meaning and significance of place in old age; pp. 3–24. [Google Scholar]
- Staquet M.J., Hays R.D., Fayers P.M. Oxford University Press; New York: 1998. Quality of Life Assessment in Clinical Trials. [Google Scholar]
- Shalash A., Essam M., Fathy M., et al. Mental health, physical activity and quality of life in Parkinson's disease during COVID-19 pandemic. Mov. Disord. 2020 doi: 10.1002/mds.28134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen J., Cheng J., Huang S., Zeng F. An exploration of spatial and social inequalities of urban sports facilities in nanning city, China. Sustainability. 2020;12(11):4353. [Google Scholar]
- Siu J.Y. The SARS-associated stigma of SARS victims in the post-SARS era of Hong Kong. Qual. Health Res. 2008;18(6):729–738. doi: 10.1177/1049732308318372. [DOI] [PubMed] [Google Scholar]
- The WHOQOL Group The world health organization quality of life assessment (WHOQOL): position paper from the world health organization. Soc. Sci. Med. 1995;10:1403–1409. doi: 10.1016/0277-9536(95)00112-k. 1995. [DOI] [PubMed] [Google Scholar]
- Troyer E.A., Kohn J.N., Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain Behav. Immun. 2020;87 doi: 10.1016/j.bbi.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tasnim S., Rahman M., Pawar P., et al. Epidemiology of sleep disorders during COVID-19 pandemic: a systematic scoping review. medRxiv. 2020 doi: 10.1101/2020.05.17.20104794. [DOI] [Google Scholar]
- Tao J. The choice of “identification” of personal information in criminal law. Criminal Science. 2019;5 [Google Scholar]
- Vieira Á., Melo C., Machado J., et al. Virtual reality exercise on a home-based phase III cardiac rehabilitation program, effect on executive function, quality of life and depression, anxiety and stress: a randomized controlled trial. Disabil. Rehabil. Assist. Technol. 2018;13(2):112–123. doi: 10.1080/17483107.2017.1297858. [DOI] [PubMed] [Google Scholar]
- Vaira L.A., Hopkins C., Salzano G., et al. Olfactory and gustatory function impairment in COVID‐19 patients: Italian objective multicenter‐study. Head Neck. 2020;42 doi: 10.1002/hed.26269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organisation . World Health Organisation; Geneva: 1958. The First Ten Years. The Health Organization. [Google Scholar]
- Walsh K., Urbaniak A. The interrelationship between life-course ruptures and place in old-age social exclusion: a scoping review. Innovation in Aging. 2018 doi: 10.1093/geroni/igy023.802. 2. 218-218. [DOI] [Google Scholar]
- Xu J.F., Ming Z.Q., Zhang Y.Q., et al. Family support, discrimination, and quality of life among ART-treated HIV-infected patients: a two-year study in China. Infectious Diseases of Poverty. 2017;6(1):152. doi: 10.1186/s40249-017-0364-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiang Y.T., Yang Y., Li W., et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7(3):228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuercher S.J., Kerksieck P., Adamus C., et al. medRxiv; 2020. Prevalence of Mental Health Problems during Virus Epidemics in the General Public, Health Care Workers and Survivors: A Rapid Review of the Evidence. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang S., Zhu Q., Zhan C., et al. 2020. Acupressure Therapy and Liu-Zi-Jue Qigong for Pulmonary Function and Quality of Life in Patients with Severe Novel Coronavirus Pneumonia (COVID-19): Study Protocol for a Randomized Controlled Trial. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Ma Z.F. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in Liaoning Province, China: a cross-sectional study. Int. J. Environ. Res. Publ. Health. 2020;17(7):2381. doi: 10.3390/ijerph17072381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Y., Shang Y., Song W., et al. Follow-up study of the pulmonary function and related physiological characteristics of COVID-19 survivors three months after recovery. EClinicalMedicine. 2020;25:100463. doi: 10.1016/j.eclinm.2020.100463. [DOI] [PMC free article] [PubMed] [Google Scholar]