Abstract
Purpose
To determine the significance of initial and residual rotator cuff tear defect size on the need for revision surgery or additional nonsurgical therapy, in a consecutive group of patients undergoing partial repair of massive rotator cuff tears.
Methods
A retrospective chart review was carried out for all arthroscopic rotator cuff repairs performed by a single surgeon between January of 2013 and December of 2016. All patients with massive rotator cuff tears (>30 cm2) who underwent partial repair were included in the study. Outcomes for the surgical procedure were measured based on the necessity for revision surgery or adjunct therapy, including steroid injections or additional physical therapy after initial release from care.
Results
In total, 1954 patients who underwent arthroscopic rotator cuff repair were identified. Thirty-eight of these met the inclusion criteria. Those patients undergoing revision surgery represented 5.2% (2/38) of the series and had an average initial/residual tear defect area of 45.0/7.0 cm2. Patients requiring adjunct therapy represented 7.9% (3/38) of the series and possessed an average initial/residual tear defect size of 40.0/16.0 cm2. The remaining 33 (86.9%) patients did not require revision surgery or adjunct therapy at a minimum follow-up of 2 years. There was no significance between initial and/or residual rotator cuff tear defect size and the need for revision surgery. However, there was a significant difference in the mean residual defect size in the patients requiring additional nonoperative treatment after initial release from care (P = .012).
Conclusions
There was no relationship between residual defect size after partial repair and the need for revision surgery. Patients who returned for additional nonoperative treatment after being released from care were noted to have a statistically larger residual defect size at the time of index surgical intervention. Only 5% of patients underwent subsequent surgery at an average of more than 4 years’ follow-up, suggesting that partial repair of massive rotator cuff tears can provide a durable, joint-preserving intervention.
Level of Evidence
Level IV, Therapeutic Case Series
Rotator cuff tears are a common problem that greatly range in severity. Massive cuff tears include full-thickness tears of 2 or more tendons or a tear defect area >30 cm2. These can be particularly challenging to deal with, as they are often associated with fatty atrophy, tendon retraction, peritendinous adhesions, and poor tissue quality.1, 2, 3 However, as we have learned more about the biomechanical properties of the rotator cuff, our repair techniques and surgical strategies have changed. Effective management of these complex patients is somewhat controversial, with treatment options ranging from open versus arthroscopic repair to reverse shoulder arthroplasty. Various procedures have evolved over the years in an attempt to address these difficult clinical situations.1 Surgical techniques such as arthroscopic debridement, capsular release,4,5 interval slides,6,7 margin convergence,8, 9, 10 and partial rotator cuff repair are commonly used during surgical intervention, with the goal of increasing rotator cuff excursion and therefore humeral head coverage, which will allow restoration of the transverse plane force couples. However, if the native tissue is too deficient or immobile even after attempts at mobilization, one may consider the supplemental use of graft augmentation11 or reconstruction options including interposition allograft,12 superior capsular reconstruction,13,14 tendon transfers,15 or even reverse shoulder arthroplasty.16 While some of these methods have allowed for increased rotator cuff tear footprint coverage, none alone have provided the surgeon with a universal solution that yields consistent functional outcomes or precludes the necessity for subsequent revision surgery for this challenging pathologic condition.17,18
In 1994, Burkhart first described the concept of a partial repair for massive, irreparable cuff tears. He coined the term “functional cuff tear,” which is the idea that while the rotator cuff may be anatomically deficient, it may remain biomechanically intact.2 He used the comparison of the rotator cable to a suspension bridge in describing how force is transferred across the rotator cuff.19,20 The goal of partial repair is to balance the anterior and posterior rotator cuff to restore the transverse plane force couple and thus stabilize the glenohumeral joint fulcrum.2 Burkhart concluded that the location of the tear may be more important than tear size when determining treatment of these massive cuff tears.
Partial repair of massive cuff tears has been reported in the literature by many authors to be a minimally invasive approach that significantly increases patient functional outcomes and decreases pain.1,3,21,22 Other authors have reported an initial improvement in functional outcomes after partial repair followed by a decline in functional outcomes and increased pain in the short-term follow-up (<2 years postoperatively), which questions the durability of these repairs.23,24
The purpose of this study was to determine the significance of initial and residual rotator cuff tear defect size on the need for revision surgery or additional nonsurgical therapy, in a consecutive group of patients undergoing partial repair of massive rotator cuff tears. The study hypothesis to be tested is that within a group of massive rotator cuff tears, the greater the area of the initial and residual tear defect, the greater the subsequent rate of revision surgery.
Methods
This study was approved by institutional review board no, IRB00110; Mississippi Sports Medicine and Orthopaedic Center Committee on Human Research, IORG 0007408. A series of consecutive shoulders undergoing arthroscopic rotator cuff repair by a single surgeon between January 1, 2013, and December 31, 2016, was identified by a database search. Shoulders that met the inclusion criteria had a rotator cuff tear with initial tear area greater than 30 cm2 and that underwent partial repair. Exclusion criteria included only those patients who had previously undergone rotator cuff repair or decompression. Potential correlations related to either the initially presenting rotator cuff tear defect size and/or the residual defect area achieved following partial repair were evaluated specifically as they related to the necessity for revision surgery or additional nonoperative treatment following release of patients from the surgeon’s care.
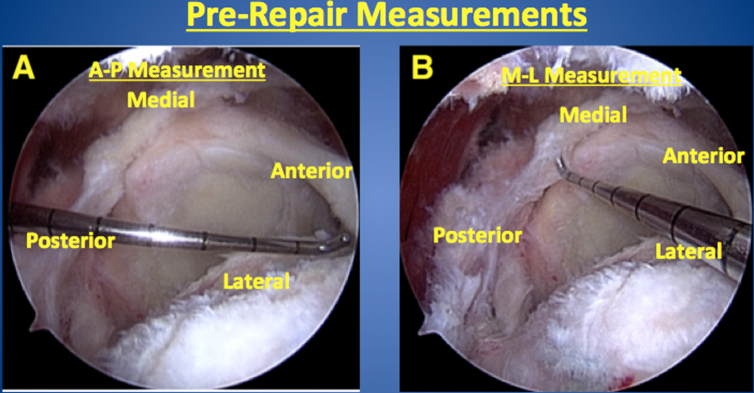
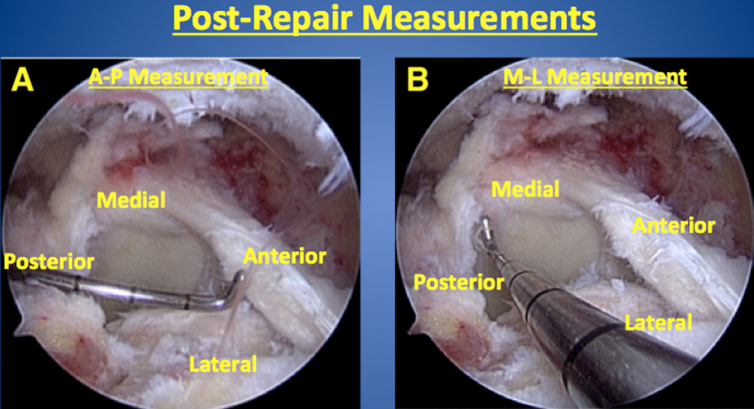
Evaluation of Rotator Cuff Tears
All patients were classified as having massive rotator cuff tears that involved 2 or more tendons with a tear defect area >30 cm2. Magnetic resonance imaging was obtained and reviewed on all patients before surgical intervention confirming rotator cuff tears in all patients. However, tear size was determined at the time of arthroscopic assessment and measured using a calibrated probe, Elite (Smith & Nephew, Inc., London, England). The borders of the tears were measured in both the anterior to posterior plane as well as medial to lateral dimension before repair as well as immediately following partial repair (Figs 1 and 2). Each set of 2 defect measurements was taken by positioning the calibrated probe at the midpoint of the anterior/posterior and medial/lateral defect boarders. The orientation of the probe was as parallel and close to the defect surface as permitted by the available arthroscopic portal access. Cross-sectional area was then calculated by multiplying the 2 measurements. The tear defect area was then measured following repair in a similar fashion to calculate the residual defect area. This allowed for an objective way to accurately and consistently measure tear defect area. The individual tendon involvement at initial presentation and after partial repair is shown in Table 1.
Fig 1.
The right shoulder rotator cuff tear is measured before repair in the anterior/posterior (A) and medial/lateral (B) orientation using a calibrated probe, as viewed arthroscopically from the lateral portal with the patient in the beach chair position.
Fig 2.
The right shoulder anterior/posterior (A) and medial/lateral (B) measurements of the residual cuff defect after partial repair is shown as viewed arthroscopically from the lateral portal with the patient in the beach chair position (same patient as in Fig 1).
Table 1.
Individual Tendon Tear Status Upon Initial Arthroscopic Presentation and Degree of Tendon Repair Achieved Postoperatively
| Supraspinatus | Infraspinatus | Subscapularis | |
|---|---|---|---|
| Initial tendon status | |||
| Intact | 0% | 0% | 57.1% |
| Partial tear | 2.6% | 18.9% | 11.4% |
| Complete tear | 97.4% | 81.1% | 31.4% |
| Repaired tendon status | |||
| Fully repaired | 11.4% | 57.1% | 84.4% |
| Partial repair | 40.0% | 40.0% | 12.5% |
| Irreparable | 48.6% | 2.9% | 3.1% |
Operative Technique
All procedures were performed by a single surgeon using a consistent setup and technique. Patients were placed in the beach chair position under general anesthesia in combination with an interscalene regional block. Three routine arthroscopic portals were created (posterior, anterior, lateral) with accessory portals as needed for anchor placement and instrumentation. After a diagnostic arthroscopy of the glenohumeral joint was performed, the arthroscope and shaver were placed in the subacromial space and a thorough bursectomy and decompression was performed as indicated to allow for optimal visualization of the rotator cuff. At this time, a calibrated probe was inserted and the cuff tear dimensions were measured as mentioned previously. A grasper was then used to evaluate tissue quality and mobility. Arthroscopic techniques employed during these cases of partial repair included capsular releases, anterior and/or posterior interval slides, and margin convergence, which were performed at the discretion of the surgeon based on intraoperative factors such as tissue retraction, relative immobility of the rotator cuff, and tear orientation with the goal of achieving a balanced, low-tension partial repair when a complete repair was not possible. Both single-row and double-row suture repair techniques were routinely employed to secure the rotator cuff tendon that could be reapproximated to the rotator cuff footprint.
Postoperative Rehabilitation
All surgical procedures were performed on an outpatient basis. Patients were immobilized in an abduction sling postoperatively and discharged home on the day of surgery. Shoulder immobilization was maintained for 2 to 6 weeks following surgical intervention at the discretion of the surgeon. A standardized physical therapy protocol was subsequently initiated and progressed on an individualized basis as physical progress deemed.
Statistical Analysis
The comparison of group means for significant differences was analyzed through use of a Student t test. A 2-tailed distribution, with homoscedastic variance was used. The threshold for significance of 0.05 was uniformly employed. Aspect found to be significant were evaluated with post-hoc power analysis for alpha of 0.05.
Results
A total of 1954 patients who underwent arthroscopic rotator cuff repair were identified. Thirty-eight of these met the inclusion criteria. The mean patient age was 66 years old (45-79 years), with a distribution of 14 female and 24 male patients included. Average postoperative follow-up was 4.5 years (2.4-6.3 years). None of the patients undergoing partial repair during the period of the study had supplemental grafts or other implants other than suture anchors used at the time of their partial repairs. Of the 38 patients who underwent partial repair of their massive cuff tear, 33 (87%) successfully progressed through their rehabilitation, were released from care, and did not require any further treatment during the study period. Three patients subsequently returned after being released from organized care (at 8, 13, and 16 months following the index procedure) with complaints of mild ipsilateral shoulder and upper arm pain. Due to their persistent pain, these 3 patients received additional nonoperative treatment and underwent either an additional 6 weeks of physical therapy (1 patient) or 6 additional weeks of physical therapy in conjunction with one subacromial space corticosteroid injection (2 patients). Two patients of the 38 shoulders that were partially repaired underwent subsequent surgery on the operative shoulder. One shoulder underwent a revision cuff repair 9 weeks after sustaining an acute retear from a low energy fall that had occurred 2 weeks postoperatively, and one shoulder was revised to a reverse total shoulder arthroplasty that was carried out 25 months following the index partial repair due to poor functional recovery and continued postoperative pain. There were no intraoperative complications, postoperative infections, thromboembolic events, or other perioperative complications that occurred in the study group.
For patients who required no additional therapeutic interventions, beyond the previously discussed standard rehabilitation protocol, an initial average tear area of 38.2 cm2 and a residual average tear area, following partial repair, of 6.8 cm2 were arthroscopically measured. For patients who required additional nonoperative treatment after initial release from care, an initial average tear area of 40.0 cm2 and a residual average tear area of 16.0 cm2 were arthroscopically measured. For patients who required revision surgery on the operative shoulder, an initial average tear area of 45.0 cm2 and a residual average tear area of 7.0 cm2 were arthroscopically measured (Table 2). When the initial tear area of each patient group was statistically evaluated for a difference against the overall patient group, no significant difference was found (no additional intervention, P = .641, additional nonoperative treatment, P = .630, revision surgery, P = .064). In addition, when the residual tear area of each patient group was statistically evaluated for a difference against the overall patient group, a larger residual tear area was seen to significantly correlate with the need for additional nonoperative therapy (no additional intervention, P = .521, additional nonoperative treatment, P = .012, revision surgery, P = .919). Post-hoc power analysis for alpha 0.05 was 91.4% for the significant difference found within the additional nonoperative treatment group.
Table 2.
Average Cuff Defect Area, Initial and Residual, for Groups Requiring Differing Levels of Postoperative Intervention
| Initial RC Defect, cm2 | Residual RC Defect, cm2 | |
|---|---|---|
| Patients requiring no additional intervention | 38.2 (P = .641) | 6.8 (P = .521) |
| Patients requiring minimal additional intervention | 40.0 (P = .630) | 16.0 (P = .012) |
| Patients requiring revision surgery | 45.0 (P = .064) | 7.0 (P = .919) |
NOTE. Student t test results are shown for each group versus the overall patient cohort.
RC, rotator cuff.
Discussion
The evidence collected within this study shows that appropriate application of a biomechanically balanced partial rotator cuff repair was associated with a low rate for subsequent revision surgery (5.2%) after an average follow-up period of greater than four years. Somewhat in contrast with the findings of Shon et al.,23 which reported relatively early deterioration of function following partial rotator cuff repair, partial repair of select massive rotator cuff patients in the current study largely remained free of the necessity for revision surgery during the follow-up period. A possible explanation for this difference is that Shon et al. measured patient-reported scoring (visual analog scale and American Shoulder and Elbow Surgeons score) up to 2 years postoperatively, in contrast to the current study’s longer period of postoperative observation (+4 years) and its more demanding outcomes measure of revision surgery. There was no statistically significant association between initial or residual tear defect size and the need for revision surgery in the current study. In fact, the only statistically significant finding was a larger residual defect size in those patients requiring additional nonoperative treatment after being released from care.
Taken together, and in light of the original biomechanical principles described by Burkhart concerning a balanced partial rotator cuff repair,2 greater presenting defect size was associated with a slight, but not statistically significant, decrease in the likelihood of achieving an adequately balanced partial repair for which revision surgery is not subsequently undertaken. Correspondingly, an increase in the residual defect following partial repair was not found to be associated with a statistical increase in the necessity to undergo a revision surgical intervention but did statistically correlate with a greater need for additional nonoperative treatment. The strengths of this study include the use of a consecutive series of arthroscopic partial rotator cuff repairs performed by a single surgeon at a single institution while using a consistent repair technique. Also, the method used to measure rotator cuff defect size was felt to be advantageous because it allowed for an easy, accurate, and reproducible objective measurement of the initial and residual defect areas in square centimeters.
Limitations
The limitations of this study are its retrospective study design and the low statistical power of the surgical revision group, due to its relatively low frequency. In addition, the defects were measured along 2 perpendicular axes and multiplied. Therefore, the resulting area calculation assumes a square, 2-dimensional tear shape, while shape variations in individual tear defect configurations exist. Still, the authors felt that the arthroscopically determined square centimeter measurements of tear size were an improvement over other methods, such as nonquantitative, unidirectional, or solely derived from magnetic resonance imaging, to describe rotator cuff tear size25, 26, 27 and allowed the authors to reproducibly define both the initial and residual rotator cuff tear defects that were present. Also, the arthroscopic measurements were taken to an accuracy of 1 cm, thus introducing a “rounding error” that contributes to inaccuracy within the tear area calculation. Also, all tear defect linear measurements were collected by a single surgeon and therefore not reproduced or validated by other observers, creating potential observer bias. Also, clinical outcome at the time of follow-up is not reported, and the outcomes reported are limited to the need for revision surgery or additional therapy. Follow-up ranges widely, and heterogeneous surgical repair techniques were performed.
Conclusions
In conclusion, there was no relationship between residual defect size after partial repair and the need for revision surgery. Patients who returned for additional nonoperative treatment after being released from care were noted to have a statistically larger residual defect size at the time of index surgical intervention. Only 5% of patients underwent subsequent surgery at an average of more than 4 years follow-up, suggesting that partial repair of massive rotator cuff tears can provide a durable, joint-preserving intervention.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: L.D.F. reports consulting income from Smith & Nephew, and research and educational support from Arthrex, Mitek, and Smith & Nephew. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
References
- 1.Iagulli N.D., Field L.D., Hobgood E.R., Ramsey J.R., Savoie F.H. Comparison of partial versus complete arthroscopic repair of massive rotator cuff tears. Am J Sports Med. 2012;40:1022–1026. doi: 10.1177/0363546512438763. [DOI] [PubMed] [Google Scholar]
- 2.Burkhart S.S., Nottage W.M., Oglivie-Harris D.J., Kohn H.S., Pachelli A. Partial repair of irreparable rotator cuff tears. Arthroscopy. 1994;10:363–370. doi: 10.1016/s0749-8063(05)80186-0. [DOI] [PubMed] [Google Scholar]
- 3.Kim S.J., Kim S.H., Lee S.K., Chun Y.M. Arthroscopic repair of massive contracted rotator cuff tears; aggressive release with anterior and posterior interval slides do not improve cuff healing and integrity. J Bone Joint Surg Am. 2013;95:1482–1488. doi: 10.2106/JBJS.L.01193. [DOI] [PubMed] [Google Scholar]
- 4.Giuseffi S., Field L.D., Giel T.V., Brislin B.T., Savoie F.H. Arthroscopic rotator cuff repair with concomitant capsular release. Arthrosc Tech. 2016;5:833–837. doi: 10.1016/j.eats.2016.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim Y.S., Lee H.J. Essential surgical techniques for arthroscopic capsular release in the treatment of shoulder stiffness. JBJS Essential Surg Tech. 2015;3:1–5. doi: 10.2106/JBJS.ST.N.00102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Corpus K.T., Taylor S.A., O’Brien S.J., Gulotta L.V. All-arthroscopic modified rotator interval slide for massive anterosuperior cuff tears using the subdeltoid space: Surgical technique and early results. HSS J. 2016;12:200–208. doi: 10.1007/s11420-016-9497-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lo I.K., Burkhart S.S. Arthroscopic repair of massive, contracted, immobile rotator cuff tears using single and double interval slides: Technique and preliminary results. Arthroscopy. 2004;20:22–33. doi: 10.1016/j.arthro.2003.11.013. [DOI] [PubMed] [Google Scholar]
- 8.Shindle M.K., Nho S.J., Nam D., et al. Technique for margin convergence in rotator cuff repair. HSS J. 2011;7:208–212. doi: 10.1007/s11420-011-9222-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim K.C., Shin H.D., Cha S.M., Kim J.H. Repair integrity and functional outcomes for arthroscopic margin convergence of rotator cuff tears. J Bone Joint Surg Am. 2013;96:536–541. doi: 10.2106/JBJS.L.00397. [DOI] [PubMed] [Google Scholar]
- 10.Burkhart S.S., Athanasiou K.A., Wirth M.A. Margin convergence: A method of reducing strain in massive rotator cuff tears. Arthroscopy. 1996;12:335–338. doi: 10.1016/s0749-8063(96)90070-5. [DOI] [PubMed] [Google Scholar]
- 11.Lewington M.R., Ferguson D.P., Smith T.D., Burks R., Coady C., Wong I.H. Graft utilization in the bridging reconstruction of irreparable rotator cuff tears: A systematic review. Am J Sports Med. 2017;45:3149–3157. doi: 10.1177/0363546517694355. [DOI] [PubMed] [Google Scholar]
- 12.Narvani A.A., Consigliere P., Polyzois I., Sarkhel T., Gupta R., Levy O. “Owl” technique for all-arthroscopic augmentation of a massive or large rotator cuff tear with extracellular matrix graft. Arthrosc Tech. 2016;5:717–724. doi: 10.1016/j.eats.2016.02.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sanchez G., Chahla J., Moatshe G., Ferrari M.B., Kennedy N.I., Provencher M.T. Superior capsular reconstruction with superimposition of rotator cuff repair for massive rotator cuff tears. Arthrosc Tech. 2017;6:1775–1779. doi: 10.1016/j.eats.2017.06.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pennington W.T., Chen S.W., Bartz B.A., Pennington J.M. Superior capsular reconstruction with arthroscopic rotator cuff repair in a “functional biologic augmentation” technique to treat massive atrophic rotator cuff tears. Arthrosc Tech. 2019;8:465–472. doi: 10.1016/j.eats.2019.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kokubu T., Mifune Y., Inui A., Kuroda R. Arthroscopic rotator cuff repair with graft augmentation of fascia lata for large and massive tears. Arthrosc Tech. 2016;5:235–238. doi: 10.1016/j.eats.2016.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ecklund K.J., Lee T.Q., Tibone J., Gupta R. Rotator cuff tear arthropathy. J Am Acad Orthop Surg. 2007;15:340–349. doi: 10.5435/00124635-200706000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Bedeir Y.H., Jimenez A.E., Grawe B.M. Recurrent tears of the rotator cuff: Effect of repair technique and management options. Orthop Rev (Pavia) 2018;10(7593):70–76. doi: 10.4081/or.2018.7593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Le B.T., Wu X.L., Lam P.H., Murrell G.A. Factors predicting rotator cuff retears: An analysis of 1000 consecutive rotator cuff repairs. Am J Sports Med. 2014;42:1134–1142. doi: 10.1177/0363546514525336. [DOI] [PubMed] [Google Scholar]
- 19.Burkhart S.S. Fluoroscopic comparison of kinematic patterns in massive rotator cuff tears: A suspension bridge model. Clin Orthop Rel Res. 1992;284:144–152. [PubMed] [Google Scholar]
- 20.Burkhart S.S., Esch J.C., Jolson R.S. The rotator crescent and rotator cable: An anatomic description of the shoulder’s “suspension bridge.”. Arthroscopy. 1993;9:611–616. doi: 10.1016/s0749-8063(05)80496-7. [DOI] [PubMed] [Google Scholar]
- 21.Duralde P.J., Bair B. Massive rotator cuff tears: The result of partial rotator cuff repair. J Shoulder Elbow Surg. 2005;14:121–127. doi: 10.1016/j.jse.2004.06.015. [DOI] [PubMed] [Google Scholar]
- 22.Kim S.J., Lee I.S., Kim S.H., Lee W.Y., Chun Y.M. Arthroscopic partial repair of irreparable large to massive rotator cuff tears. Arthroscopy. 2012;28:761–768. doi: 10.1016/j.arthro.2011.11.018. [DOI] [PubMed] [Google Scholar]
- 23.Shon M.S., Koh K.H., Lim T.K., Kim W.J., Kim K.C., Yoo J.C. Arthroscopic partial repair of irreparable rotator cuff tears: Preoperative factors associated with outcome deterioration over 2 years. Am J Sports Med. 2015;43:1965–1975. doi: 10.1177/0363546515585122. [DOI] [PubMed] [Google Scholar]
- 24.Galatz L.M., Ball C.M., Teefey S.A., Middleton W.D., Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86-A:219–224. doi: 10.2106/00004623-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 25.Mori D., Kizaki K., Funakoshi N., et al. Clinical and radiographic outcomes after arthroscopic lamina-specific double-row repair of large delaminated rotator cuff tears in active patients. Orthop J Sports Med. 2019;7:1–14. doi: 10.1177/2325967119838249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Derwin K.A., Sahoo S., Zajichek A., et al. Tear characteristics and surgeon influence repair technique and suture anchor use in repair of superior-posterior rotator cuff tendon tears. J Shoulder Elbow Surg. 2019;28:227–236. doi: 10.1016/j.jse.2018.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kuptniratsaikul V., Laohahaimongkol T., Umprai V., Yeekian C., Prasathaporn N. Pre-operative factors correlated with arthroscopic reparability of large-to-massive rotator cuff tears. BMC Musculoskelet Disord. 2019;20:111. doi: 10.1186/s12891-019-2485-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.