Abstract
We report a case of posterior uveal effusion (UE) with a long-term follow-up that has occurred following cataract surgery. A 64-year-old woman presented with diminished vision of the right eye (RE) 3 weeks after an uneventful phacoemulsification and intraocular lens implantation. Complete ophthalmic examination including fluorescein angiography (FA), indocyanine green angiography (ICGA), echography and optical coherence tomography (OCT) were performed. Best corrected visual acuity (BCVA) of the RE was 20/50. Anterior segment and intraocular pressure were unremarkable. OCT revealed prominent folds of the choroid and retina, subretinal fluid and darkening of the choroid with reduced visibility of the choroidal vessels and the scleral border. The left eye (LE) was unremarkable. BCVA of the LE was: 20/20. After topical anti-inflammatory and systemic corticosteroid therapy for 5 months, no morphological change of the macula was seen. The patient was observed without any treatment. Forty-three months after the cataract surgery and 38 months after cessation of the corticosteroid therapy, OCT revealed a normal macular morphology and the BCVA improved to 20/25. Even though rare, UE at the posterior pole may occur after modern cataract surgery. OCT examination is a reliable tool in monitoring the macular morphology. Since morphological and functional improvement can be seen in long-term, observation may be considered for some cases of posterior UE with resistance to the therapy.
Keywords: Cataract surgery, Complication, Optical coherence tomography, Uveal effusion
Introduction
Uveal effusion (UE) usually presents with a complex of clinical findings caused by several triggers. Well-known frequent pathologies and risk factors leading to UE are nanophthalmus, high hyperopia, ocular trauma, intraocular inflammation, and intraocular surgery. UE syndrome is reserved for cases without known ocular diseases and thought to be due to pathological structures of the choroidea and/or sclera [1].
Characteristic clinical findings of UE are unilaterality, circular detachment of choroidea and secondary serous retinal detachment at the periphery. Optic disc swelling, dilated vortex veins, uveal folds or detachment of the ciliary body may also occur [2]. UE in the posterior pole, also called macular hypotony, is seen frequently following filtrating glaucoma operation and less frequently after cataract surgery [3].
Treatment of the UE is based on the underlying pathology, whereas the UE syndrome responds well to the corticosteroid treatment or to the scleral fenestration [4]. We report a case of UE at the posterior pole with a long-term follow-up that developed after cataract surgery.
Case Report
A 64-year-old woman presented in February 2014 with a painless loss of vision of the right eye (RE) 3 weeks after uncomplicated phacoemulsification and posterior chamber intraocular lens implantation by her local physician. Application of pilocarpine or systemic carbonic anhydrase inhibitors after the operation was not reported. No information regarding the intra- or postoperative course was available. Except for a bilateral hyperopia of 4.25 dpt, the ocular history was unremarkable. The patient reported that the vision was good and equal between two eyes before developing cataract. General history was unremarkable, too.
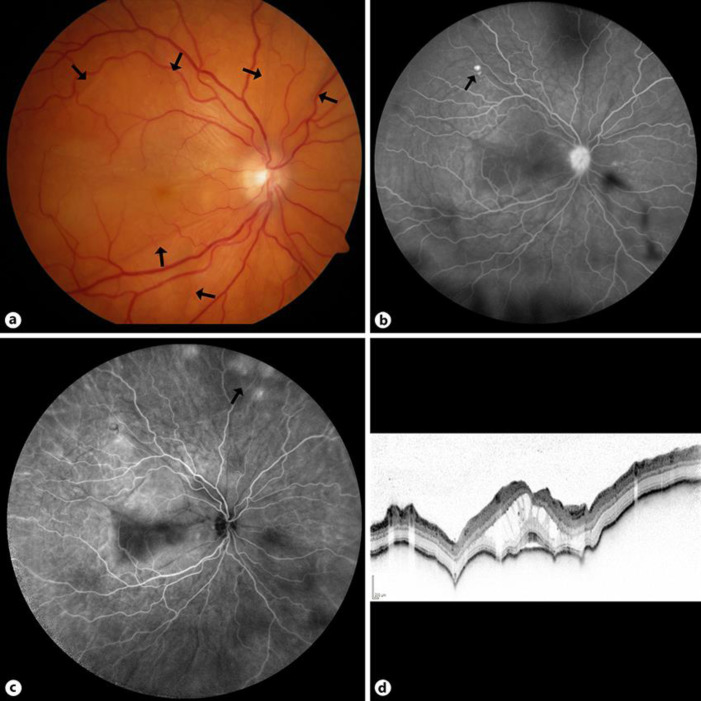
The best corrected visual acuity (BCVA) of the RE was 20/50 (−1.5sph/–1.0cyl × 90°). Intraocular pressure was 12 mm Hg. Anterior chamber depth was measured as 4.59 mm and axial length 22.39 mm. Slit lamp examination was unremarkable. Cyclodialysis was excluded on gonioscopy [5]. The intraocular lens was located endocapsular and well-centered. The posterior capsule was intact. Dilated fundoscopy revealed papillary hyperemia, macular edema and folds at the posterior pole extending to the middle periphery (Fig. 1a). Fluorescein angiography (FA) revealed staining of the optic disc on the RE and focal hyperfluorescence in the superior middle periphery (Fig. 1b). Indocyanine green angiography (ICGA) lacked signs for choroidal ischemia but showed a focal hyperfluorescence in the superior middle periphery (Fig. 1c). Optical coherence tomography (OCT) showed a cystoid macula edema, subretinal fluid in the fovea, multiple irregular elevations of the retinal pigment epithelium (RPE) and lobular swelling of the choroid (Fig. 1d). B-scan ultrasound examination revealed thickening of the uvea, but no intraocular mass or a peripheral choroidal detachment. An intraorbital or intracranial lesion was excluded by magnetic resonance tomography (MRI), but a thickening of the retina-uvea complex could be shown with staining of gadolinium. The left eye was pseudophakic and the examination was unremarkable with a BCVA of 20/20.
Fig. 1.
Baseline presentation. a Color fundus photograph of the right eye showing choroidal folds (arrows). b Late phase of the fluorescein angiogram showing staining of optic disc and subretinal focal hyperfluorescence (arrow). c Indocyanine green angiogram showing a subretinal localized hyperfluorescence in the superior middle periphery (arrow). d Optical coherence tomography: vertical scan through the fovea showing a cystoid macula edema, thickening of the fovea, subretinal fluid, irregularity of the retinal pigment epithelial band and lobular swelling of the choroid.
At the first presentation, the patient was under a local therapy with non-steroidal anti-inflammatory eye drops (Nepanfenac, qid). A systemic corticosteroid therapy (1 mg/kg) was initiated for 20 weeks and tapered in weekly intervals. Re-examination 4 weeks later showed no change of the initial findings.
Due to the temporal correlation to the cataract surgery, posterior UE was suspected to be a complication of this procedure. The local anti-inflammatory therapy was continued and systemic steroids were discontinued after a period of 2 months in absence of morphological changes.
Twenty-one months after the first presentation, the ocular findings were unchanged. Additionally, enhanced depth imaging OCT (EDI-OCT) was performed, which showed a diffuse, homogenous hypo-reflectivity of the choroid and decreased visibility of choroidal vessels and the scleral border. Another attempt of treatment by intravenous steroidal pulse therapy of 250 mg of prednisolone was done for 3 days. Three months later (24 months after the first presentation), BCVA, clinical and OCT findings did not show any improvement.
Forty-three months after the first presentation, BCVA improved to 20/25. Fundoscopy revealed a dry macula with some pigmentary changes at the RPE level. OCT showed complete resolution of the pathologies at the posterior pole.
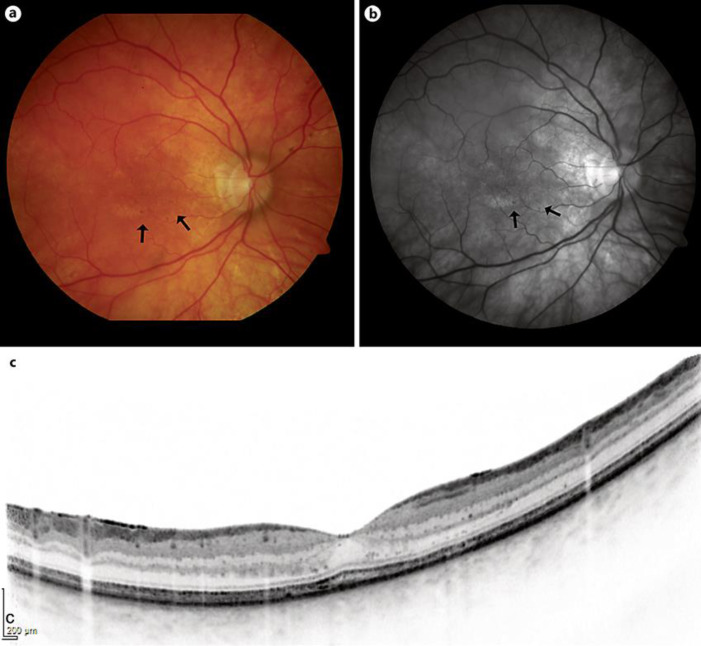
The patient was seen last in August 2018, BCVA of the RE was 20/25. Dilated fundoscopy and OCT revealed stable clinical findings (Fig. 2a–c).
Fig. 2.
Fifty-four months after the presentation. a Color and b red-free photograph of the right eye showing complete resolution of the exudation and choroidal folds at the posterior pole. Note few leopard-like subretinal hyperpigmentations inferior to the fovea (arrow) and nasal to the papilla. c Optical coherence tomography: vertical scan through the fovea showing a normal macular morphology.
Discussion and Conclusions
We report on a case of posterior UE after uncomplicated cataract surgery. Because nanophthalmus was not present, no surgical therapy was performed. Under local anti-inflammatory and systemic cortisone therapy no change of the clinical findings were seen. Forty-three months after the first presentation, clinical findings at the posterior pole improved spontaneously and BCVA increased to 20/25.
Differential diagnosis of the presented case included intraocular inflammation, such as Harada disease, choroidal ischemia, cyclodialysis and intraocular or retrobulbar mass. The FA as well as ICGA findings were not consistent with a chorioretinal inflammatory disease or choroidal ischemia. The B-scan ultrasound examination and MRI eliminated any intraocular or retrobulbar tumor and peripheral choroidal detachment. The homogenous hypo-reflectivity of the choroid shown by EDI-OCT could be explained by an accumulation of fluid in the choroidal stroma. The ocular length was within normal limits and nanophthalmus was excluded. The anterior segment of the affected eye was normal and there was no cyclodialysis on gonioscopy. A temporary intraocular hypotony could not be excluded with certainty. We assumed therefore surgery-related ocular hypotony in presence of moderate hyperopia as the cause of the posterior UE.
Severity of the exudative findings at the posterior pole as well as resistance to corticosteroid therapy of the reported case was unusual for a posterior UE or hypotonic macula. On the other hand, the presented case shows that in the long-term course of posterior UE following cataract surgery, a late spontaneous improvement of the ocular morphology and visual function can be seen.
Statement of Ethics
This case report was conducted ethically in accordance with the declarations of Helsinki.
Written informed consent for publication of this case report and any accompanying images was obtained from the patient. A copy of the consent form is available for review by the Editor of this journal.
Funding Sources
No funding was received.
Conflicts of Interest
The following authors have no financial disclosures: A.A., F.G., I.N., Ö.D.
Author Contributions
A.A. and F.G. analyzed, interpreted the data and were major contributors in writing the manuscript. A.A. has made substantial contributions to the designs of the work. F.G. has made substantial contributions to the conception. I.N. and Ö.D. have made substantial contributions to the analysis and interpretation of data. All authors read and approved the final manuscript.
References
- 1.Elagouz M, Stanescu-Segall D, Jackson TL. Uveal effusion syndrome. Surv Ophthalmol. 2010 Mar-Apr;55((2)):134–45. doi: 10.1016/j.survophthal.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 2.Besirli C, Johnson M. Uveal Effusion Syndrome and Hypotony Maculopathy. In: Ryan S, editor. Retina. 5th ed. Los Angeles, USA: Elsevier Inc; 2013. pp. pp. 1306–17. [Google Scholar]
- 3.Agarwal A. Idiopathic Uveal Effusion Syndrome. In: Agarwal A, editor. Gass' Atlas of Macular Diseases. one. 5th ed. Elsevir Inc; 2012. pp. pp. 196–202. [Google Scholar]
- 4.Shields CL, Roelofs K, Di Nicola M, Sioufi K, Mashayekhi A, Shields JA. Uveal effusion syndrome in 104 eyes: Response to corticosteroids - The 2017 Axel C. Hansen lecture. Indian J Ophthalmol. 2017 Nov;65((11)):1093–104. doi: 10.4103/ijo.IJO_752_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.González-Martín-Moro J, Contreras-Martín I, Muñoz-Negrete FJ, Gómez-Sanz F, Zarallo-Gallardo J. Cyclodialysis: an update. Int Ophthalmol. 2017 Apr;37((2)):441–57. doi: 10.1007/s10792-016-0282-8. [DOI] [PubMed] [Google Scholar]