Abstract
Introduction
Data of COVID-19 in newborns and children are limited, and clinical manifestations are nonspecific and might delay the diagnosis, which might lead to severe complications. In this clinical case, we will describe new-onset diabetes with consciousness impairment as an atypical revealing way of COVID-19.
Case
A 3-year-old child presented to the Emergency Department with loss of consciousness (without fever), lethargy, and stupor. Clinical assessment on admission found an unconscious child with a pediatric Glasgow Coma Scale of 10/15 with no localizing signs or meningeal syndrome, polypneic of 35 breaths/min, pulse oximetry of 90%, with signs of overall dehydration: skin folds, sunken eyes, tachycardia of 160 beats/minute, and recoloring time superior at 3 seconds. Laboratory findings showed hyperleukocytosis of 16000/mm3, lymphopenia of 450/mm3, glycemia of 5 g/L with a correct ionogram : corrected natremia of 139 mmol/L, serum potassium of 4.5 mmol/L, glycosuria of 3+, ketonuria of 2+, and HbA1c of 10%, and COVID-19 RT-PCR came back positive.
Conclusion
COVID-19 might be revealed with atypical symptoms including new-onset diabetes and diabetic ketoacidosis; therefore, clinicians must suspect it in children with blood glucose and HbA1c at the time of admission. This will help to manage patients with hyperglycemia early.
1. Introduction
From March 2020, Anesthesiology and Intensive Care Unit Department, Mohammed VI University Hospital Center, Oujda, Morocco, has been facing an unprecedented outbreak of coronavirus disease and spread of 2019 novel coronavirus or severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which has now become a global pandemic [1, 2]. The disease caused by SARS-CoV-2 was termed “COVID-19,” and the World Health Organization declared the COVID-19 outbreak a public health emergency of international concern and officially was declared a pandemic on March 11, 2020 [2].
Data from the early months of 2020 suggest that there is a bidirectional relationship between COVID-19 and diabetes [3]. Diabetes is associated and is continuously suggested as a risk factor that contributes to the severity and mortality of COVID-19 [1]. Multiple forms of diabetes might be observed in patients with COVID-19 including new-onset diabetes and metabolic complications such as diabetic ketoacidosis and hyperosmolarity [4]. Nonetheless, data on new-onset type 1 diabetes during the COVID-19 pandemic, particularly in children, are limited [5]. In this article, we describe a clinical case of a 3-year-old child who presented to the Emergency Department (ED) in a ketoacidosis decompensation state, a recent diagnosis with COVID-19 infection, and who was retrospectively diagnosed with new-onset diabetes.
2. Clinical Case
A 3-year-old child presented to the ED with loss of consciousness (without fever), lethargy, and stupor. Clinical assessment on admission found an unconscious child with a pediatric Glasgow Coma Scale (GCS) of 10/15 with no localizing signs or meningeal syndrome, polypneic of 35 breaths/min, pulse oximetry of 90%, with signs of overall dehydration (skin folds), sunken eyes, tachycardia of 160 beats/minute, and recoloring time superior at 3 seconds.
Laboratory findings showed hyperleukocytosis of 16000 mm3, lymphopenia of 450 mm3, glycemia of 5 g/L with a correct ionogram : corrected natremia of 139 mmol/L, serum potassium of 4.5 mmol/L, glycosuria of 3+, ketonuria of 2+, and HbA1c of 10%.
Brain computed tomography (CT) came back normal; the search for a primary infection site led us to carry out a chest X-ray showing an alveolar-interstitial syndrome (Figure 1), supplemented by a thoracic CT revealing a bilateral ground-glass opacification consistent with viral pneumopathy, with moderate impairment with a level of suspicion scored CO-RADS 4 (Figure 2). Given the epidemiological context, a COVID-19 RT-PCR came back positive.
Figure 1.
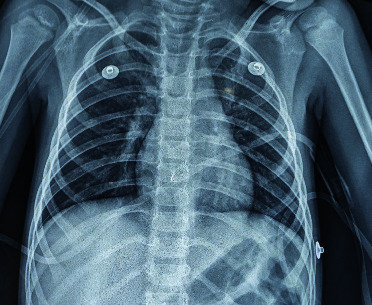
Chest X-ray showing an alveolar-interstitial syndrome.
Figure 2.
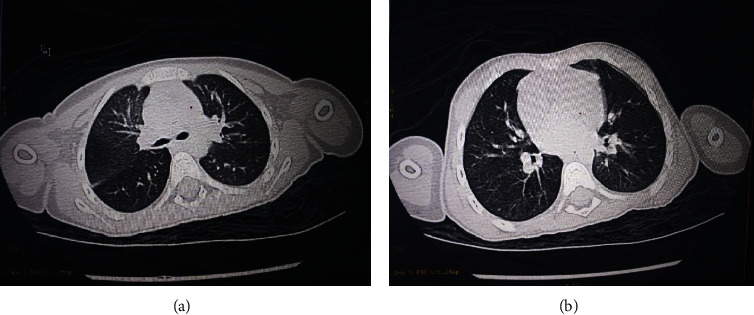
Chest CT scan showing images in favor of pneumopathy COVID-19 CO-RADS 4.
Diabetic ketoacidosis (DKA) is the most common hyperglycemic emergency and is associated with increased morbidity and mortality. In children and adolescents with type 1 diabetes, DKA accounts for the most common cause of death. DKA is characterized by hyperglycemia, ketosis, and metabolic acidosis [6].
Management of DKA consisted of rehydration with Ringer's lactate 20 ml/kg initially and physiological serum as well as insulin therapy with a dose of 0.05 IU/kg/h along with monitoring of blood sugar levels and any complications. The prognosis was favorable with neurological, respiratory, and metabolic improvement; the child was transferred to the pediatric endocrinology department for further assessment.
3. Discussion
Coronaviruses are positive-strand ribonucleic, large viruses. Only two genera of the viruses can infect humans: a and b types, and they are called human coronaviruses (HCoVs) [7].
HCoVs are used to be mild phenotypes in humans because of their inconsequential pathogenic effect. However, two epidemics emerging in the early 21st century (severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS)) with a high rate of morbidity and mortality changed the knowledge about this [8].
COVID-19 is generally more frequent among adults more than 15 years old with less confirmed cases among children [9]. However, the number of children infected has increased due to the pathogen detection campaigns and the lack of protective measures [10].
A report of a multicenter regional data from North West London of new-onset type 1 diabetes and DKA in children has estimated an increase of 80% of new type 1 diabetes cases during the COVID-19 pandemic and postulates that COVID-19 exposure contributed to the observed increase in cases by precipitating or accelerating type 1 diabetes onset [5]. A previous paper reported that children accounted for 5% of confirmed COVID-19 cases and presented with a milder disease symptom, and they have a better prognosis compared with adults, with very low mortality rate [7, 9]. But children with newly diagnosed diabetes, either it is new-onset or previously undiagnosed, tend to have increased levels of inflammatory markers and indicators of multiorgan injury leading to severe or critical illness of COVID-19 [11]. They also present severe hyperglycemic complications such as DKA and hyperosmolar hyperglycemic syndrome requiring high doses of insulin [12]. COVID-19 patients with newly diagnosed diabetes have higher mortality rate than those with known diabetes [11].
The pathophysiological mechanisms implicated with the increased frequency and severity of COVID-19 in people with diabetes are not yet elucidated, and several hypotheses have been elaborated to explain the link between COVID-19 and high rate and worst outcomes in diabetic people [2].
Diabetes is associated with an increased risk of infections, including viral ones due to defects in the innate immunity affecting phagocytosis, neutrophil chemotaxis, and cell-mediated immunity [1, 13]. Besides, diabetes and insulin resistance are associated with endothelial dysfunction and increased platelet aggregation and activation leading to the hypercoagulable prothrombotic state [13]. The latter associated with the low-grade chronic inflammation might promote the cytokine storm, a severe complication of COVID-19 characterized by excessive production of inflammatory cytokines [14]. Furthermore, COVID-19 spike protein gains entry to its target cells by using the angiotensin-converting enzyme 2 (ACE2) as the receptor, which has protective effects primarily regarding inflammation [1]. COVID-19 infection reduces ACE2 expression inducing cellular damage, hyperinflammation, and respiratory failure and can lead to a direct effect on β-cell function, which not only explains that diabetes might be a risk factor for a severe form of COVID-19 disease but also explains that infection could induce new-onset diabetes [1, 9, 15–18].
New-onset diabetes must be detected in all nondiabetic patients especially those at high risk for metabolic disease who have contracted the viral infection. Besides, most patients present multiple stresses with COVID-19 including respiratory failure and sepsis requiring intravenous infusion of insulin and fluid balance to control the glycemia levels [19]. In addition, potassium balance must be carefully considered in the context of insulin treatment, as hypokalemia is a common feature of COVID-19 and may be exacerbated after the introduction of insulin [19].
4. Conclusion
This clinical case supports the strong link between COVID-19 infection and diabetes. Therefore, physicians should consider this in all nondiabetic children and screen them at their admission with blood glucose and HbA1C for appropriate and early management.
Acknowledgments
The authors acknowledge the frontline medical staff working day and night in Morocco to rescue critical cases and protect the public health. The authors know that these great efforts are now and will be in the future crucial in overcoming COVID-19.
Data Availability
The data used to support the findings of this study are available from the corresponding author.
Ethical Approval
This study was exempt from ethical approval at our institution, as it was an observational finding in regular practice.
Consent
Written informed consent was obtained from the child holder for publication of this case report and accompanying images.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Authors' Contributions
Dr. Aabdi Mohammed contributed to conceptualization, methodology, validation, formal analysis, and visualization and wrote the original draft. Dr. Aarab Adnane contributed to formal analysis and visualization and reviewed and edited the manuscript. Dr. Es-Saad Ounci provided resources and developed software and was responsible for data curation. Dr. Malki Khalil, Pr. Housni Brahim, and Pr. Houssam Bkiyar were responsible for visualization. Pr. Houssam Bkiyar reviewed and edited the manuscript. Pr. Housni Brahim was responsible for project administration; provided resources; contributed to conceptualization, methodology, and validation; and reviewed and edited the manuscript. Dr. Aarab Adnane, Dr. Es-Saad Ounci, Dr. Malki Khalil, Pr. Housni Brahim, and Pr. Houssam Bkiyar approved the final version of the manuscript.
References
- 1.Bornstein S. R., Rubino F., Khunti K., et al. Practical recommendations for the management of diabetes in patients with COVID-19. The Lancet Diabetes & Endocrinology. 2020;8(6):546–550. doi: 10.1016/s2213-8587(20)30152-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Papadokostaki E., Tentolouris N., Liberopoulos E. COVID-19 and diabetes: what does the clinician need to know? Primary Care Diabetes. 2020;14(5):558–563. doi: 10.1016/j.pcd.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen Y., Gong X., Wang L., Guo J. Effects of hypertension, diabetes and coronary heart disease on COVID-19 diseases severity: a systematic review and meta-analysis MedRxiv. 2020. p. p. 280. [DOI]
- 4.Paul Zimmet M., George Alberti M. D., Stefan Bornstein M. D., et al. New-onset diabetes in COVID-19. The New England Journal of Medicine. 2020;383(8):787–789. doi: 10.1056/NEJMc2018688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Unsworth R., Wallace S., Oliver N. S., et al. New-onset type 1 diabetes in children during COVID-19: multicenter regional findings in the UK. Diabetes Care. 2020;43(11):e170–e171. doi: 10.2337/dc20-1551. [DOI] [PubMed] [Google Scholar]
- 6.Fayfman M., Pasquel F. J., Umpierrez G. E. Management of hyperglycemic crises. Medical Clinics of North America. 2017;101(3):587–606. doi: 10.1016/j.mcna.2016.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dong Y., Dong Y., Mo X., Hu Y., Qi X., Jiang F. Epidemiology of COVID-19 among children in China. Pediatrics. 2020;145(6) doi: 10.1542/peds.2020-0702. [DOI] [PubMed] [Google Scholar]
- 8.De Wilde A. H., Eric J., Snijder M. K., Van M. J. Assessment & Evaluation in Higher Education. New York, NY, USA: Springer International Publishing; 2012. Host factors in coronavirus replication; p. p. 435. Available from: http://books.google.com/books?id=_DDwCqx6wpcC&printsec=frontcover&dq=unwritten+rules+of+phd+research&hl=&cd=1&source=gbs_api%255Cnpapers2://publication/uuid/48967E01-55F9-4397-B941-310D9C5405FA%255Cnhttp://medcontent.metapress.com/index/A65RM03P4874243N.p. [Google Scholar]
- 9.She J., Liu L., Liu W. COVID-19 epidemic: disease characteristics in children. Journal of Medical Virology. 2020;92(7):747–754. doi: 10.1002/jmv.25807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jiehao C., Jin X., Daojiong L., et al. A case series of children with 2019 novel coronavirus infection: clinical and epidemiological features. Clinical Infectious Diseases. 2020;71(6):1547–1551. doi: 10.1093/cid/ciaa198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sathish T., Cao Y., Kapoor N. Newly diagnosed diabetes in COVID-19 patients. Primary Care Diabetes. 2020;15(1):p. 194. doi: 10.1016/j.pcd.2020.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jie Y., Jia S., Ng H., Yeoh E. Diabetic ketoacidosis precipitated by COVID-19 in a patient with newly diagnosed diabetes mellitus. Diabetes Research and Clinical Practice. 2020;164 doi: 10.1016/j.diabres.2020.108166.108166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abu-ashour W., Twells L., Valcour J., et al. The association between diabetes mellitus and incident infections : a systematic review and meta-analysis of observational studies. BMJ Open Diabetes Research and Care. 2017;5(1) doi: 10.1136/bmjdrc-2016-000336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guo W., Li M., Dong Y., et al. Diabetes is a risk factor for the progression and prognosis of COVID-19. Diabetes Metabolism Research and Reviews. 2020;36(6) doi: 10.1002/dmrr.3319.e3319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bindom S. M., Lazartigues E. The sweeter side of ACE2: physiological evidence for a role in diabetes. Molecular and Cellular Endocrinology. 2020;302(2):193–202. doi: 10.1016/j.mce.2008.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Apicella M., Campopiano M. C., Mantuano M., Mazoni L., Coppelli A., Del Prato S. COVID-19 in people with diabetes: understanding the reasons for worse outcomes. The Lancet Diabetes & Endocrinology. 2020;8(9):782–792. doi: 10.1016/s2213-8587(20)30238-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guo J.-K., Lin S.-S., Ji X.-J., Guo L.-M. Binding of SARS coronavirus to its receptor damages islets and causes acute diabetes. Acta Diabetologica. 2010;47(3):193–199. doi: 10.1007/s00592-009-0109-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fang L., Karakiulakis G., Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? The Lancet Respiratory Medicine. 2020;8(4):p. e21. doi: 10.1016/s2213-2600(20)30116-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dellinger R. P., Levy M. M., Rhodes A., et al. Surviving sepsis campaign : international guidelines for management of severe sepsis and septic shock . Critical Care Medicine. 2013;41(2):580–637. doi: 10.1097/CCM.0b013e31827e83af. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author.


