Key Points
Question
How has the incidence rate of central retinal artery occlusion changed over time in Korea?
Findings
In this cohort study of 50 million residents of Korea using data from the Korean National Health Insurance Service from 2002 to 2015, the incidence rate of central retinal artery occlusion decreased over time, especially among women, individuals younger than 65 years, and individuals born after 1930.
Meaning
This study found decreasing trends in the incidence rates of central retinal artery occlusion in Korea between 2002 and 2015; these decreases may be associated with the development of a national health care system and the general improvement in chronic disease management.
Abstract
Importance
Central retinal artery occlusion (CRAO) is associated with and shares common risk factors with cardiovascular diseases. Over the past several decades, the incidence rates of stroke and ischemic heart disease have substantially decreased in high-income industrialized countries. However, little is known regarding current trends in CRAO incidence rates.
Objective
To estimate trends in the incidence rates of CRAO in Korea.
Design, Setting, and Participants
This nationwide population-based cohort study was designed on September 7, 2017, and used data from the Korean National Health Insurance Service from January 1, 2002, to December 31, 2015. Individuals with incident CRAO between 2002 and 2015 were identified using the CRAO diagnostic code (H34.1) from the International Classification of Diseases, Tenth Revision. Unadjusted CRAO incidence rates were calculated using the number of CRAO cases identified and the corresponding midyear population, which was obtained from resident registration data. Standardized incidence rates were calculated based on the 2015 census population, and weighted mean annual incidence rates with 95% CIs were computed based on the Poisson distribution. To identify trends in incidence rates, joinpoint regression analysis was performed using standardized incidence rates, and annual percentage changes (APCs) were calculated across the 12-year study period. Data were analyzed from May 1, 2019, to April 30, 2020.
Main Outcomes and Measures
Temporal trends in CRAO incidence rates (measured as cases per 100 000 person-years) and age-standardized APCs in CRAO incidence rates using joinpoint and birth cohort analyses.
Results
Among 50 million residents of Korea, 9892 individuals (5884 men [59.5%]) with incident CRAO between 2002 and 2015 were identified. The mean age of Korean individuals diagnosed with CRAO was 62.4 years (range, 0-97 years); among men and women, the mean age was 61.5 years (range, 0-96 years) and 63.6 years (range, 0-97 years), respectively. The mean standardized incidence rate of CRAO was 2.00 cases per 100 000 person-years (95% CI, 1.97–2.04 cases per 100 000 person-years) among the entire population, 2.43 cases per 100 000 person-years (95% CI, 2.37-2.49 cases per 100 000 person-years) among men, and 1.61 cases per 100 000 person-years (95% CI, 1.57-1.66 cases per 100 000 person-years) among women. The highest incidence rate (9.85 cases per 100 000 person-years; 95% CI, 9.10-10.60 cases per 100 000 person-years) was observed among those aged 80 to 84 years (13.74 cases per 100 000 person-years [95% CI, 12.16-15.32 cases per 100 000 person-years] for men and 8.04 cases per 100 000 person-years [95% CI, 7.21-8.86 cases per 100 000 person-years] for women). The incidence rate in the overall study population decreased over time (APC, −3.46%; 95% CI, −4.3% to −2.6%), and this decreasing trend was more evident in women (APC, −4.56%; 95% CI, −5.7% to −3.4%) than in men (APC, −2.90%; 95% CI, −3.9% to −1.9%). The decrease in the incidence rate was more evident among participants younger than 65 years (APC, −6.80%; 95% CI, −8.3% to −5.2%) than among those 65 years and older (APC, −0.57%; 95% CI, −1.5% to −0.4%). Among participants born after 1930, a decrease in the CRAO incidence rate over time was observed in every age group, while the same decreasing trend was not present among those born before 1930.
Conclusions and Relevance
This study found that the CRAO incidence rate has been decreasing among residents of Korea, especially among women, individuals younger than 65 years, and individuals born after 1930. This observed decrease may be associated with the development of a national health care system and the general improvement in chronic disease management.
This cohort study uses data from the Korean National Health Insurance Service database from 2002 to 2015 to estimate temporal trends in the incidence rates of central retinal artery occlusion among residents of Korea.
Introduction
Central retinal artery occlusion (CRAO) is an ophthalmic emergency that is associated with severe acute blindness.1,2 This condition is commonly precipitated by an embolism that produces ischemia of the inner retina and permanent visual impairment. Previous studies have reported an association between CRAO and cardiovascular diseases (CVDs), particularly stroke and ischemic heart disease, as CRAO and CVDs share risk factors, etiologic factors, and incidence trends.3,4 Over the past several decades, the incidence rates of stroke and ischemic heart disease have substantially decreased in high-income industrialized countries, likely because of better control of vascular risk factors, such as hypertension, diabetes, and cigarette smoking.5,6,7,8 Similar decreases have also been observed in Korea, where the incidence rates of both coronary heart disease and stroke have decreased,9 and the awareness, treatment, and control of hypertension and diabetes have improved.10,11 However, there has been a paucity of research investigating current trends in CRAO incidence rates.12 Therefore, we aimed to investigate the trends in CRAO incidence rates and elucidate the association of age, sex, and birth cohort with these trends by analyzing the standardized incidence rates of CRAO in the entire Korean population across a 12-year period.
Methods
This retrospective cohort study was designed on September 7, 2017, and used data from the Korean National Health Insurance Service (NHIS) database from January 1, 2002, to December 31, 2015. The study was approved by the institutional review board of Seoul National Bundang Hospital and adhered to the tenets of the Declaration of Helsinki.13 Written consent was waived by the institutional review board because of the retrospective nature of the study, which was conducted using a preconstructed deidentified data set. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline for cohort studies.
The NHIS database includes records for the entire Korean population (50 million people), as a single-payer health insurance program covers every resident of Korea through either the National Health Insurance system (97% of residents) or the Medical Aid system (3% of residents).14 Thus, the NHIS database contains all medical records associated with medical insurance claims (eg, diagnoses, procedures, prescription records, demographic information, and direct medical costs) in Korea.
We identified CRAO cases registered in the NHIS database between 2002 and 2015 using the CRAO diagnostic code (H34.1) from the International Classification of Diseases, Tenth Revision (ICD-10). The date of the earliest claim associated with the ICD-10 diagnostic code for CRAO was defined as the date of an index occurrence in the NHIS database and was considered the time of disease incident. The patient was then considered to have an incident case in that particular year.4,12 To remove any potential preexisting cases of CRAO, we set a wash-out period of at least 2 years by excluding cases that had the ICD-10 diagnostic code for CRAO during the first 2 years of the study period (2002-2003).4,12,15
We then calculated unadjusted CRAO incidence rates for each year from 2004 to 2015 using the number of CRAO cases identified and the corresponding midyear population. The Korean population for each year was obtained from resident registration data in Korea,16 categorized by 5-year age groups and sex. To estimate standardized incidence rates, we used a direct standardization method for age and sex, with the 2015 census population in Korea used as the standard population.16 Using these estimated standardized incidence rates, we calculated the weighted mean annual incidence rates of CRAO from 2004 to 201517 and estimated 95% CIs for the incidence rates based on the Poisson distribution.
To identify trends in CRAO incidence rates, we performed a joinpoint regression analysis using the standardized incidence rates from 2004 to 2015. The joinpoint regression model is a segmented linear regression analysis used to investigate the trends in incidence rates and identify changes in trends over time.18 First, we estimated the annual percentage changes (APCs) of CRAO incidence and plotted CRAO incidence throughout the 12-year study period. Next, we performed a joinpoint regression analysis for each sex and age group (divided into participants younger than 65 years vs participants 65 years and older). To assess the association of birth cohort with CRAO incidence, we examined CRAO incidence rates according to sequential 5-year birth cohorts, beginning with the population born between 1910 and 1914 and ending with the population born between 2005 and 2009. Because the data available in the NHIS database allowed only 12 years of follow-up, we were able to follow up the 21 birth cohorts (from individuals born in 1910 to those born in 2010) for 10 years (2005, 2010, and 2015).
Statistical Analysis
We used Stata software, version 12.0 (StataCorp); SAS software, version 9.3 (SAS Institute); and Joinpoint Regression Program software, version 4.1.1 (National Cancer Institute). Data were analyzed from May 1, 2019, to April 30, 2020.
Results
We identified 9892 patients with incident CRAO (5884 men [59.5%]) in Korea from 2004 to 2015 (Table). The mean age of patients diagnosed with CRAO was 62.4 years (range, 0-97 years); among men and women, the mean age was 61.5 years (range, 0-96 years) and 63.6 years (range, 0-97 years), respectively. We could not identify any patients with incident CRAO who also had giant cell arteritis (which may indicate that no patients had both conditions or that diagnoses were missed or miscoded in the database).
Table. Frequencies and Incidence Rates of Central Retinal Artery Occlusion Among Resident of Korea From 2004 to 2015.
| Age group, y | Korean populationa | Total incidents | Incidents among men | Incidents among women | Male to female ratio | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total residents | Men | Women | No. | Incidence rate (95% CI)b | No. | Incidence rate (95% CI)b | No. | Incidence rate (95% CI)b | ||
| 0-4 | 2 235 397 | 1 147 126 | 1 088 271 | 11 | 0.04 (0.02 to 0.06) | 3 | 0.02 (0.00 to 0.04) | 8 | 0.06 (0.02 to 0.10) | 0.35 |
| 5-9 | 2 252 950 | 1 162 087 | 1 090 863 | 2 | 0.01 (0.00 to 0.01) | 2 | 0.01 (0.00 to 0.03) | 0 | 0.00 (0.00 to 0.00) | NA |
| 10-14 | 2 418 360 | 1 257 902 | 1 160 458 | 14 | 0.04 (0.02 to 0.06) | 9 | 0.04 (0.02 to 0.07) | 5 | 0.03 (0.00 to 0.05) | 1.62 |
| 15-19 | 3 170 545 | 1 657 722 | 1 512 823 | 50 | 0.12 (0.09 to 0.16) | 33 | 0.16 (0.10 to 0.21) | 17 | 0.09 (0.05 to 0.13) | 1.74 |
| 20-24 | 3 385 936 | 1 808 857 | 1 577 079 | 76 | 0.19 (0.14 to 0.23) | 33 | 0.15 (0.10 to 0.21) | 43 | 0.22 (0.15 to 0.29) | 0.70 |
| 25-29 | 3 027 896 | 1 581 887 | 1 446 009 | 131 | 0.30 (0.25 to 0.35) | 70 | 0.31 (0.24 to 0.38) | 61 | 0.28 (0.21 to 0.36) | 1.09 |
| 30-34 | 3 611 034 | 1 854 905 | 1 756 129 | 205 | 0.42 (0.36 to 0.48) | 130 | 0.52 (0.43 to 0.61) | 75 | 0.31 (0.24 to 0.38) | 1.66 |
| 35-39 | 3 783 589 | 1 927 388 | 1 856 201 | 283 | 0.55 (0.49 to 0.61) | 184 | 0.70 (0.60 to 0.80) | 99 | 0.39 (0.31 to 0.47) | 1.79 |
| 40-44 | 4 215 921 | 2 142 101 | 2 073 820 | 476 | 0.90 (0.82 to 0.99) | 319 | 1.19 (1.06 to 1.32) | 157 | 0.61 (0.51 to 0.70) | 1.95 |
| 45-49 | 4 266 941 | 2 151 070 | 2 115 871 | 657 | 1.30 (1.20 to 1.40) | 426 | 1.66 (1.50 to 1.81) | 231 | 0.93 (0.81 to 1.05) | 1.78 |
| 50-54 | 4 145 976 | 2 094 318 | 2 051 658 | 822 | 1.85 (1.73 to 1.98) | 507 | 2.27 (2.07 to 2.46) | 315 | 1.43 (1.27 to 1.59) | 1.58 |
| 55-59 | 3 863 095 | 1 922 796 | 1 940 299 | 933 | 2.72 (2.55 to 2.90) | 581 | 3.41 (3.13 to 3.68) | 352 | 2.04 (1.83 to 2.26) | 1.67 |
| 60-64 | 2 758 941 | 1 348 273 | 1 410 668 | 1148 | 4.33 (4.08 to 4.58) | 728 | 5.67 (5.26 to 6.09) | 420 | 3.08 (2.78 to 3.37) | 1.84 |
| 65-69 | 2 117 875 | 1 015 463 | 1 102 412 | 1462 | 6.53 (6.19 to 6.86) | 906 | 8.76 (8.19 to 9.33) | 556 | 4.61 (4.23 to 5.00) | 1.90 |
| 70-74 | 1 760 932 | 789 607 | 971 325 | 1538 | 8.61 (8.18 to 9.04) | 899 | 11.84 (11.07 to 12.61) | 639 | 6.22 (5.74 to 6.71) | 1.90 |
| 75-79 | 1 356 014 | 550 684 | 805 330 | 1137 | 9.56 (9.00 to 10.11) | 634 | 14.27 (13.16 to 15.38) | 503 | 6.75 (6.16 to 7.23) | 2.11 |
| 80-84 | 810 891 | 275 462 | 535 429 | 657 | 9.85 (9.10 to 10.60) | 291 | 13.74 (12.16 to 15.32) | 366 | 8.04 (7.21 to 8.86) | 1.71 |
| 85-89 | 371 527 | 98 367 | 273 160 | 239 | 7.94 (6.93 to 8.94) | 104 | 12.80 (10.34 to 15.26) | 135 | 6.14 (5.10 to 7.17) | 2.09 |
| 90-94 | 124 111 | 28 565 | 95 546 | 48 | 4.92 (3.53 to 6.32) | 24 | 11.06 (6.64 to 15.49) | 24 | 3.17 (1.90 to 4.43) | 3.49 |
| ≥95 | 27 732 | 5259 | 22 473 | 3 | 1.30 (−0.17 to 2.78) | 1 | 2.53 (−2.43 to 7.50) | 2 | 1.05 (−0.40 to 2.50) | 2.42 |
| Total | 49 705 663 | 24 819 839 | 24 885 824 | 9892 | 2.00 (1.97 to 2.04) | 5884 | 2.43 (2.37 to 2.49) | 4008 | 1.61 (1.57 to 1.66) | 1.51 |
Abbreviation: NA, not applicable.
Information on the Korean population was based on 2015 census data from the Korean Statistical Information Service.16
Incidence rate was measured as cases per 100 000 person-years.
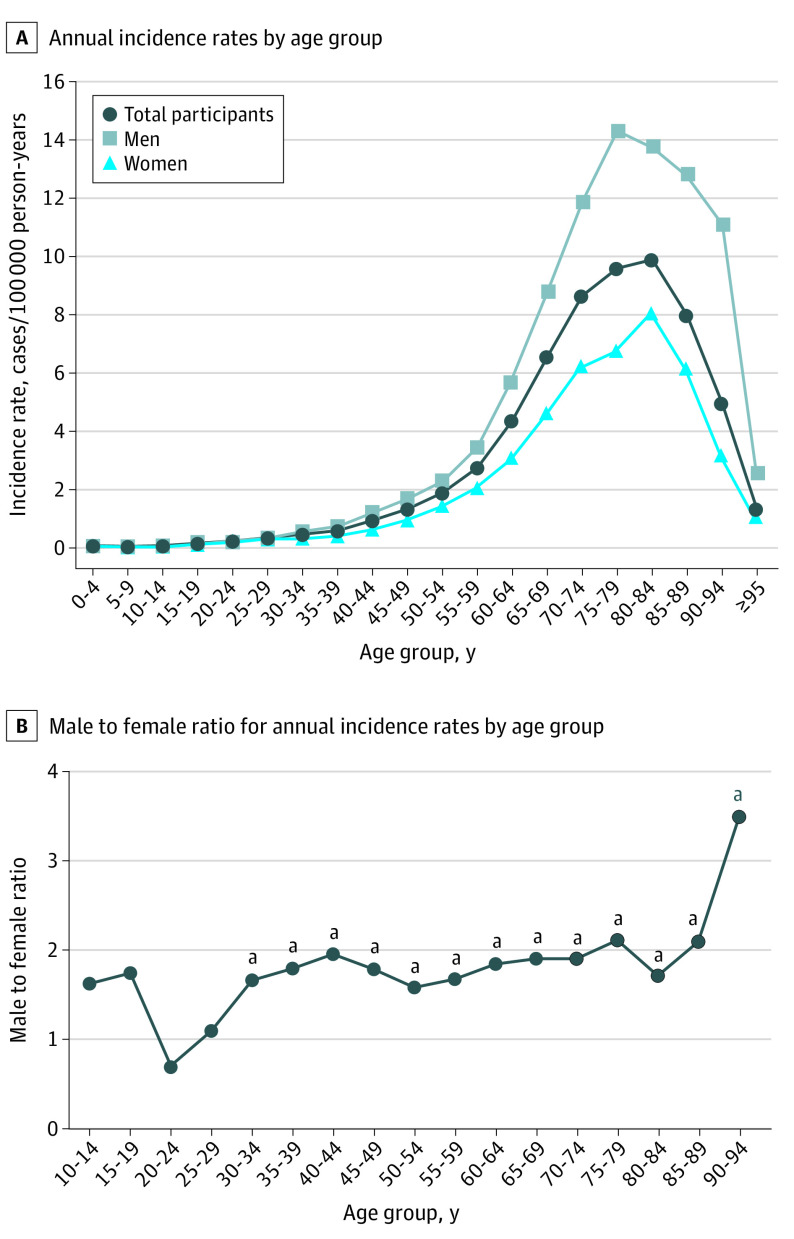
The weighted mean incidence rate of CRAO during the 12-year period was 2.00 cases per 100 000 person-years (95% CI, 1.97–2.04 cases per 100 000 person-years). Analyzed by sex, the weighted mean incidence rates of CRAO in men and women were 2.43 cases per 100 000 person-years (95% CI, 2.37-2.49 cases per 100 000 person-years) and 1.61 cases per 100 000 person-years (95% CI, 1.57-1.66 cases per 100 000 person-years), respectively. Overall, the incidence rate among men was 1.51 times higher than that of women (Table). Men also had a higher CRAO incidence rate than women in most age groups (Figure 1A), and the male to female ratio ranged from 1.58 for individuals aged 30 to 34 years to 3.49 for individuals aged 90 to 94 years (Figure 1B). The incidence rate exponentially increased with age, with the highest incidence rate of 9.85 cases per 100 000 person-years (95% CI, 9.10-10.60 cases per 100 000 person-years) observed among individuals aged 80 to 84 years, with 13.74 cases per 100 000 person-years (95% CI, 12.16-15.32 cases per 100 000 person-years) among men and 8.04 cases per 100 000 person-years (95% CI, 7.21-8.86 cases per 100 000 person-years) among women (Table). Among women, the incidence rate for those aged 80 to 84 years represented the highest rate. Among men, the highest incidence rate was observed among those aged 75 to 79 years (14.27 cases per 100 000 person-years; 95% CI, 13.16-15.38 cases per 100 000 person-years) (Table).
Figure 1. Annual Incidence Rates of Central Retinal Artery Occlusion by Age Group and Male to Female Ratio Among Residents of Korea From 2004 to 2015.
A, Annual incidence rates by age group. B, Male to female ratio for annual incidence rates by age group. Statistical analysis for male to female ratio was performed using the Wilcoxon matched-pairs test.
aP < .05.
Results from the joinpoint regression analysis indicated that the age-standardized incidence rates of CRAO decreased in both men and women throughout the study period, a trend that was more evident in women than in men. The age-standardized APC for CRAO was −3.46% (95% CI, −4.3% to −2.6%) across all patients, with the APC among men decreasing by −2.90% (95% CI, −3.9% to −1.9%), and the APC among women decreasing by −4.56% (95% CI, −5.7% to −3.4%) (Figure 2A). In addition, decreases in APC were more evident among patients younger than 65 years (APC, −6.80%; 95% CI, −8.3% to −5.2%) (Figure 2B); among patients 65 years and older, this decrease was not observed (APC, −0.57%; 95% CI, −1.5% to −0.4%) (Figure 2C). Among those 65 years and older, no change was found in men (APC, 0.02%; 95% CI, −1.2% to 1.3%) across the 12-year study period, but a decreasing trend was found in women (APC, −1.94%; 95% CI, −3.5 to −0.4%) over the study period (Figure 2C). All annual incidence rates of CRAO by age group and sex are presented in the eTable in the Supplement. Consistent with the results of the joinpoint analysis, cohorts born after 1930 indicated decreases in CRAO incidence rates over time among every age group, while this decreasing trend was less evident among those born before 1930 (Figure 3).
Figure 2. Joinpoint Regression Analysis of Annual Incidence Rates of Central Retinal Artery Occlusion by Age Group and Sex Among Residents of Korea From 2004 to 2015.
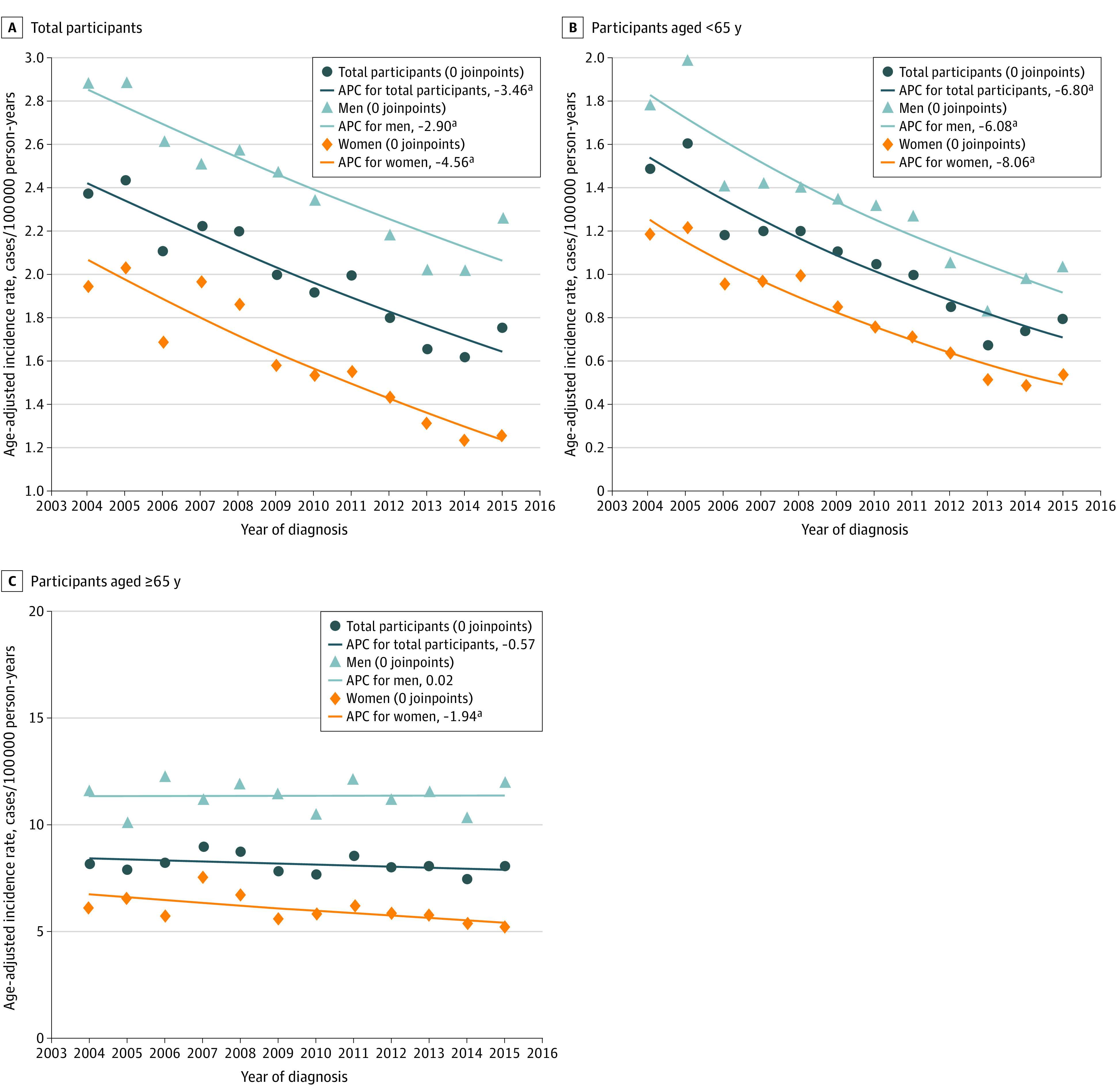
The joinpoint analysis, a segmented linear regression model used to fit trends by connecting different lines at joinpoints, was performed to identify changes in trends over time. APC indicates annual percentage change from 2004 to 2015.
aP < .05.
Figure 3. Annual Incidence Rates of Central Retinal Artery Occlusion by Birth Cohort and Sex Among Residents of Korea From 2004 to 2015.
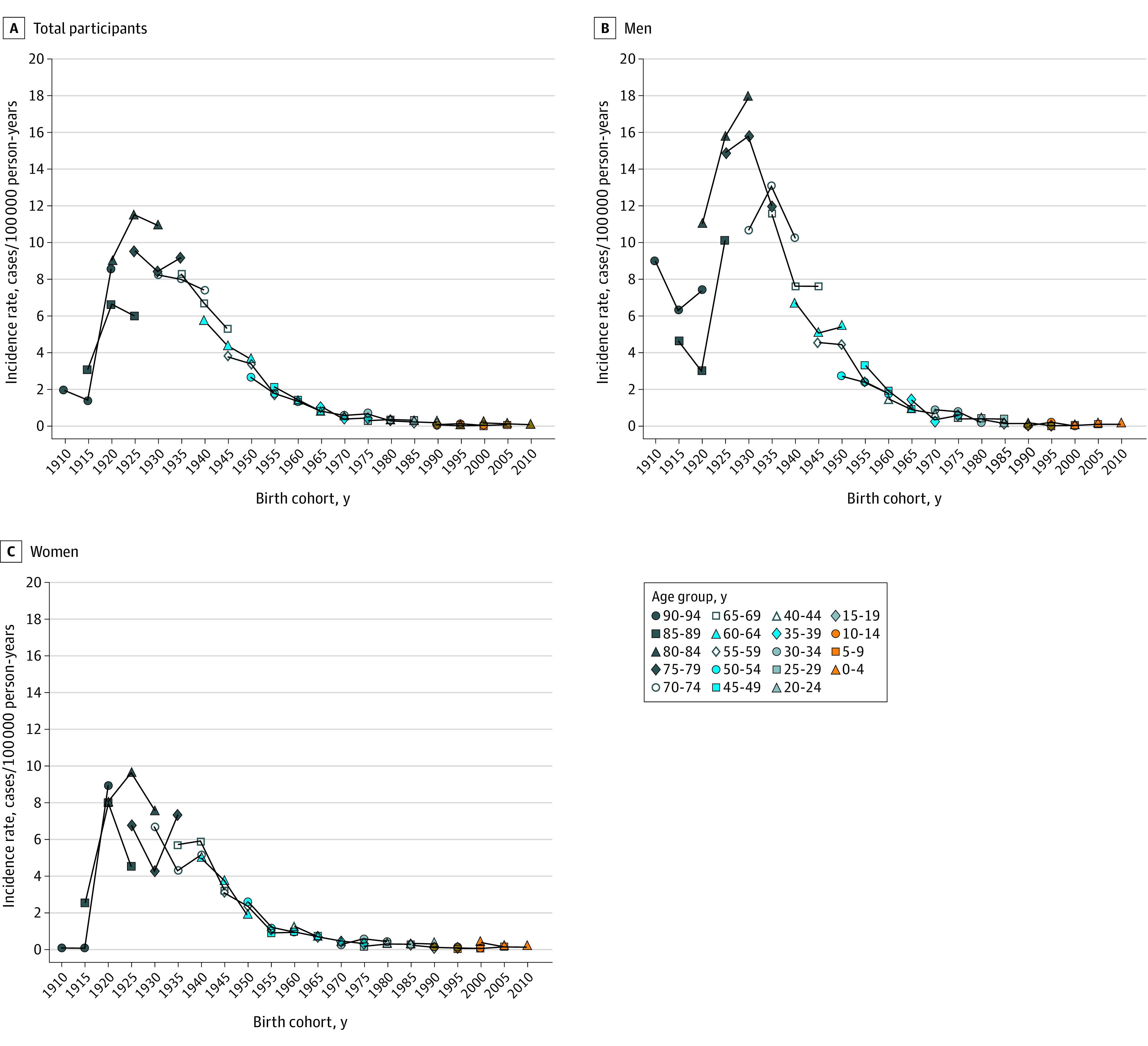
Because the National Health Insurance Service database allowed only 12 years of follow-up, the follow-up analysis of birth cohorts was limited to 10 years (in 2005, 2010, and 2015) in each age group.
Discussion
In this nationwide population-based cohort study, CRAO incidence rates decreased from 2004 to 2015 in Korea, particularly among women, individuals younger than 65 years, and individuals born after 1930. In the past several decades, the incidence rates of stroke and coronary heart disease have decreased, primarily in high-income industrialized countries.5,6,7,8 The incidence rates of both stroke and coronary heart disease also decreased in Korea from 2006 to 2010.9 In addition, awareness, treatment, and control of risk factors for CVDs, such as hypertension, diabetes, and smoking, have generally improved in Korea over the last decade.10,11,19 Because these risk factors for CVDs have also been associated with CRAO,3 the favorable trends in CRAO incidence rates may be associated with the successful control of shared risk factors. Furthermore, the present study indicated a decrease in birth cohort–specific CRAO incidence rates among younger cohorts born after 1930. Therefore, it is expected that these decreasing trends in CRAO incidence rates will gradually occur in older cohorts over time, and these trends can be expected to continue in the future.
Similar to the results of a previous study, the incidence rates of CRAO increased substantially with age (until ages 75-79 years), and the ratio of men to women with CRAO remained consistent across a wide range of age groups (30-89 years).12 However, this trend of age-associated CRAO incidence rates was somewhat different from that of coronary heart disease and stroke, in which the incidence rates have increased continuously with age.19,20 Lower incidence rates of CRAO in the oldest age group may be associated with decreased detection or reporting of symptoms, which would have produced fewer requests for medical care.12,21
Strengths and Limitations
This study has several strengths. The Korean government assigns a unique identifier, the Korean Resident Registration Number, to every resident at birth. This identifier is used in the NHIS database and population statistics (both for the midyear population in the resident registration data and the census population every 5 years). Therefore, we were able to identify patients with CRAO without omission or duplication and estimate reliable unadjusted and standardized incidence rates. In addition, because Korea is a densely populated country with a population of 50 million, we could include a sufficient number of patients with incident CRAO and use a joinpoint regression analysis to assess the temporal trends in CRAO incidence rates.
This study also has several limitations. First, the study may have underestimated the CRAO incidence rates because of ascertainment bias, such as missed diagnosis or misdiagnosis. We only included cases at the time of the first insurance claim and did not count claims after that point, which is an inherent limitation of any study using an insurance claims database. In addition, there might have been potential cases of diagnosed CRAO for which nonspecific diagnostic codes were used, such as visual disturbances (ICD-10 code H53) and visual impairment (including blindness [ICD-10 code H54]), in the database. However, CRAO is a rare disease with a specific ICD-10 diagnostic code (H34.1). Therefore, the probability of misclassification is low, and the diagnosis can be considered reliable.
Because our data are based on insurance claims, detailed clinical information, such as patients’ health status (before CRAO onset), risk factors for CRAO, symptoms, and test results, is lacking. Therefore, we are limited to analyzing the association between decreasing CRAO incidence rates and those of other systemic diseases, such as stroke and CVDs. In addition, this study focused on CRAO and did not include the other retinal arterial occlusive disorders, such as branch artery occlusion and amaurosis fugax.
Because data available in the NHIS database allowed only 12 years of follow-up, we were limited to have only 3 follow-ups in 2005, 2010, and 2015 for birth cohort analysis and could not use the age-period-cohort model,22 which would have allowed us to control for the independent associations of age, period, and cohort. We plan to perform a more comprehensive birth cohort analysis using the age-period-cohort model after obtaining data from 5 or more 5-year cohorts in the future.
Conclusions
This cohort study provided detailed CRAO incidence rates over a 12-year period and highlighted the decreasing trend in CRAO incidence rates in Korea, finding that these decreases were more evident in women, individuals younger than 65 years, and individuals born after 1930. This decreasing trend may be associated with the development of a national health care system and the general improvement in chronic disease management. The data from this study can help to assess the CRAO-associated public health burden and improve planning for ophthalmic health care policy. Further studies are warranted to evaluate the long-term changes in CRAO incidence rates and their association with vascular comorbidities among patients with CRAO.
eTable. Annual Incidence Rates of Central Retinal Artery Occlusion by Age Group and Sex Among Residents of Korea From 2004 to 2015
References
- 1.Hayreh SS, Zimmerman MB. Central retinal artery occlusion: visual outcome. Am J Ophthalmol. 2005;140(3):376-391. doi: 10.1016/j.ajo.2005.03.038 [DOI] [PubMed] [Google Scholar]
- 2.Hayreh SS. Acute retinal arterial occlusive disorders. Prog Retin Eye Res. 2011;30(5):359-394. doi: 10.1016/j.preteyeres.2011.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hayreh SS, Podhajsky PA, Zimmerman MB. Retinal artery occlusion: associated systemic and ophthalmic abnormalities. Ophthalmology. 2009;116(10):1928-1936. doi: 10.1016/j.ophtha.2009.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Park SJ, Choi N-K, Yang BR, et al. Risk and risk periods for stroke and acute myocardial infarction in patients with central retinal artery occlusion. Ophthalmology. 2015;122(11):2336-2343. doi: 10.1016/j.ophtha.2015.07.018 [DOI] [PubMed] [Google Scholar]
- 5.Benjamin EJ, Virani SS, Callaway CW, et al. ; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics—2018 update: a report from the American Heart Association. Circulation. 2018;137(12):e67-e492. doi: 10.1161/CIR.0000000000000558 [DOI] [PubMed] [Google Scholar]
- 6.Ford ES, Roger VL, Dunlay SM, Go AS, Rosamond WD. Challenges of ascertaining national trends in the incidence of coronary heart disease in the United States. J Am Heart Assoc. 2014;3(6):e001097. doi: 10.1161/JAHA.114.001097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Koton S, Schneider ALC, Rosamond WD, et al. Stroke incidence and mortality trends in US communities, 1987 to 2011. JAMA. 2014;312(3):259-268. doi: 10.1001/jama.2014.7692 [DOI] [PubMed] [Google Scholar]
- 8.Wang Y, Rudd AG, Wolfe CDA. Age and ethnic disparities in incidence of stroke over time: the South London Stroke Register. Stroke. 2013;44(12):3298-3304. doi: 10.1161/STROKEAHA.113.002604 [DOI] [PubMed] [Google Scholar]
- 9.Kim RB, Kim B-G, Kim Y-M, et al. Trends in the incidence of hospitalized acute myocardial infarction and stroke in Korea, 2006-2010. J Korean Med Sci. 2013;28(1):16-24. doi: 10.3346/jkms.2013.28.1.16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shin J-Y. Trends in the prevalence and management of diabetes in Korea: 2007-2017. Epidemiol Health. 2019;41:e2019029. doi: 10.4178/epih.e2019029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kang S-H, Kim S-H, Cho JH, et al. Prevalence, awareness, treatment, and control of hypertension in Korea. Sci Rep. 2019;9(1):10970. doi: 10.1038/s41598-019-46965-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Park SJ, Choi N-K, Seo KH, Park KH, Woo SJ. Nationwide incidence of clinically diagnosed central retinal artery occlusion in Korea, 2008 to 2011. Ophthalmology. 2014;121(10):1933-1938. doi: 10.1016/j.ophtha.2014.04.029 [DOI] [PubMed] [Google Scholar]
- 13.World Medical Association . World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191-2194. doi: 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- 14.Song SO, Jung CH, Song YD, et al. Background and data configuration process of a nationwide population-based study using the Korean national health insurance system. Diabetes Metab J. 2014;38(5):395-403. doi: 10.4093/dmj.2014.38.5.395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Park SJ, Choi N-K, Park KH, Woo SJ. Nationwide incidence of clinically diagnosed retinal vein occlusion in Korea, 2008 through 2011: preponderance of women and the impact of aging. Ophthalmology. 2014;121(6):1274-1280. doi: 10.1016/j.ophtha.2013.12.024 [DOI] [PubMed] [Google Scholar]
- 16.Korean Statistical Information Service database. Statistics Korea. Accessed October 1, 2019. https://kosis.kr/index/index.do
- 17.Cho SC, Park SJ, Byun SJ, Woo SJ, Park KH. Five-year nationwide incidence of macular hole requiring surgery in Korea. Br J Ophthalmol. 2019;103(11):1619-1623. doi: 10.1136/bjophthalmol-2018-313237 [DOI] [PubMed] [Google Scholar]
- 18.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for Joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335-351. doi: [DOI] [PubMed] [Google Scholar]
- 19.Hong K-S, Bang OY, Kang D-W, et al. Stroke statistics in Korea: part I. epidemiology and risk factors: a report from the Korean Stroke Society and Clinical Research Center for Stroke. J Stroke. 2013;15(1):2-20. doi: 10.5853/jos.2013.15.1.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hong JS, Kang HC, Lee SH, Kim J. Long-term trend in the incidence of acute myocardial infarction in Korea: 1997-2007. Korean Circ J. 2009;39(11):467-476. doi: 10.4070/kcj.2009.39.11.467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Driver JA, Djousse L, Logroscino G, Gaziano JM, Kurth T. Incidence of cardiovascular disease and cancer in advanced age: prospective cohort study. BMJ. 2008;337:a2467. doi: 10.1136/bmj.a2467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yang Y, Land KC. Age-Period-Cohort Analysis: New Models, Methods, and Empirical Applications. Morgan BJT, Van der Heijden P, Wikle CK, eds. Chapman & Hall/CRC Interdisciplinary Statistics Series. CRC Press; 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Annual Incidence Rates of Central Retinal Artery Occlusion by Age Group and Sex Among Residents of Korea From 2004 to 2015