Abstract
Drug-law enforcement constitutes a structural determinant of health among people who inject drugs (PWID). Street encounters between police and PWID (e.g., syringe confiscation, physical assault) have been associated with health harms, but these relationships have not been systematically assessed. We conducted a systematic literature review to evaluate the contribution of policing to risk of human immunodeficiency virus (HIV) infection among PWID. We screened MEDLINE, sociological databases, and gray literature for studies published from 1981 to November 2018 that included estimates of HIV infection/risk behaviors and street policing encounters. We extracted and summarized quantitative findings from all eligible studies. We screened 8,201 abstracts, reviewed 175 full-text articles, and included 27 eligible analyses from 9 countries (Canada, China, India, Malaysia, Mexico, Russia, Thailand, Ukraine, and the United States). Heterogeneity in variable and endpoint selection precluded meta-analyses. In 5 (19%) studies, HIV infection among PWID was significantly associated with syringe confiscation, reluctance to buy/carry syringes for fear of police, rushed injection due to a police presence, fear of arrest, being arrested for planted drugs, and physical abuse. Twenty-one (78%) studies identified policing practices to be associated with HIV risk behaviors related to injection drug use (e.g., syringe-sharing, using a “shooting gallery”). In 9 (33%) studies, policing was associated with PWID avoidance of harm reduction services, including syringe exchange, methadone maintenance, and safe consumption facilities. Evidence suggests that policing shapes HIV risk among PWID, but lower-income settings are underrepresented. Curbing injection-related HIV risk necessitates additional structural interventions. Methodological harmonization could facilitate knowledge generation on the role of police as a determinant of population health.
Keywords: drug injection, HIV, people who inject drugs, police, policing, substance-related disorders, systematic reviews
Abbreviations
- CI
confidence interval
- HIV
human immunodeficiency virus
- OR
odds ratio
- PWID
people who inject drugs
INTRODUCTION
Globally, injection drug use remains a growing public health concern, as there are an estimated 10–23 million people who inject drugs (PWID) (1). Injection drug use is widely distributed among at least 179 countries or territories (2). The health consequences of injection drug use include overdose morbidity and mortality, bloodborne pathogen infection, endocarditis, and other harms (3). Sharing of injection equipment remains a substantial cause of bloodborne virus transmission, including transmission of human immunodeficiency virus (HIV) and hepatitis C virus (3). In 2013, injection drug use caused an additional 2.82 million disability-adjusted life years resulting from HIV infection (3). Although the HIV burden attributed to injection drug use is highest in low- and middle-income countries (3), PWID remain highly vulnerable to HIV infection in US and other upper-income settings (4, 5). While effective evidence-based harm reduction interventions are available for preventing and treating HIV infection among PWID, global coverage of such services remains low (6, 7). In regions experiencing notable crises of opioid dependence, such as North America and Eastern Europe/Central Asia, injection drug use is a critical problem causing substantial harm to PWID (4, 8, 9). The role of drug policy and its enforcement has been increasingly recognized as a structural force shaping HIV risk among PWID (8).
Most PWID live in countries where drug use is highly criminalized (7). Prohibitionist drug policy and the global “war on drugs” have impacted numerous societies in the form of mass incarceration, police militarization, extrajudicial killings, and other human rights abuses (10–14). Drug-law enforcement practices anchored in these policies significantly shape the HIV risk environment for PWID (15). For example, laws that criminalize possession of syringes or other drug paraphernalia have had a negative impact on HIV risk and injection-related risk behaviors (16). Thus, laws limiting syringe access and their operationalization through street-level policing of PWID run counter to evidence-based syringe distribution programs and other public health measures (e.g., syringe service programs) known to prevent HIV.
At a time when a new paradigm of “public health policing” is being heralded in response to drug and other health crises (17, 18), there has not been a systematic accounting of the harms that cascade from interactions between police and PWID. Police are responsible for the enforcement of drug-related laws, which disproportionately affect marginalized populations such as PWID. Detention, regardless of whether it is legally justified, serves as an entryway to carceral settings. As revealed in numerous large systematic reviews, incarceration is a major source of individual and public health detriment (19, 20). Often failing to provide humane conditions and adequate treatment, correctional settings expose individuals to disproportionately elevated levels of infectious disease, such as HIV, hepatitis B and C viruses, and tuberculosis, compared with the burden in the community (20). Moreover, formerly incarcerated PWID are at significantly elevated risk of acquiring bloodborne infections within the first few months after release (19).
Less attention has focused on the encounters with police that can elevate PWID disease risk above and beyond what is conferred by incarceration. Syringe confiscation, harassment outside of harm reduction sites, and extrajudicial arrest are among the many practices that shape injection-related risk behaviors among PWID (21–23). Behavioral responses to such practices include increased syringe-sharing, reduced help-seeking at syringe service programs and opioid agonist therapy clinics, use of “shooting galleries,” and rushed or other risky injection practices (24–27).
As the negative health and social consequences of drug criminalization have become recognized (28), decriminalization efforts have been implemented in some settings (29–31). Such efforts have produced scientific evidence to support a shift in priority from criminal sanctions to a public health approach (11). Notably, however, harmful policing practices can persist even when the drug policy environment is favorable to public health. For example, Mexico passed sweeping drug policy reforms in 2009 which decriminalized possession of drugs for personal use, but PWID experienced little positive impact because of continued aggressive drug-law enforcement by police (29, 32). Successful implementation of drug policy is contingent upon the extent to which police enforce the law. Therefore, drug policy reform alone is necessary but insufficient to extinguish the harms caused by drug criminalization. As such, the alignment of policing practices with public health is a relevant global research imperative that has not been adequately explored.
Our objective in this systematic review is to provide a synthesis of policing practices that can act as structural risk factors for HIV infection and injection-related risk behaviors among PWID. We build on other systematic reviews that have focused on the effect of drug criminalization on HIV infection risk and the role of police as a structural determinant of HIV risk among female sex workers (17, 33). We provide additional insight by examining how individual-level policing encounters shape the HIV risk environment for PWID. To our knowledge, this is the first systematic literature review of its kind.
METHODS
We conducted a systematic literature review in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines that has been registered with PROSPERO, the international prospective register of systematic reviews (PROSPERO registration no. CRD42018105967). We screened abstracts of articles published from September 2017 to November 2018. Search terms for the abstract review were initially implemented in the MEDLINE database (PubMed; US National Library of Medicine, Bethesda, Maryland) and were subsequently adapted for application in other research databases. Our search terms (see Web Table 1, available at https://academic.oup.com/aje) consisted of 2 distinct classes: 1) terms related to law enforcement, policing practices, and criminal justice; and 2) terms related to injection drug use. We did not include terms related to incarceration, since they are not direct policing exposures and therefore were outside of the scope of this review. We applied the search terms to the following bibliographical databases: MEDLINE, Sociological Abstracts (ProQuest LLC, Ann Arbor, Michigan), EMBASE (Excerpta Medica Database; Elsevier B.V., Amsterdam, the Netherlands), PsycINFO (American Psychological Association, Washington, DC), and SocINDEX (EBSCO Information Services, Ipswich, Massachusetts). We also searched non–peer-reviewed sources and gray literature, including reports produced by Harm Reduction International (London, United Kingdom), the National Harm Reduction Coalition (New York, New York), Human Rights Watch (New York, New York), Amnesty International (London, United Kingdom), the United Nations Office on Drugs and Crime (Vienna, Austria), the Global Fund (Washington, DC), and the Open Society Foundations (New York, New York) (see Web Table 1 for a complete list of search terms by database). All abstracts and references were managed using EndNote software, version 8.2 (Clarivate Analytics, Philadelphia, Pennsylvania); duplicate abstracts were recorded but not included in the review.
We screened abstracts from studies published in English between 1981 and May 2018 to ensure that we captured all abstracts that had been published since the emergence of HIV in the scientific literature (34). Three of the authors (L.A., C.V., and P.B.) conducted a review of the titles and abstracts. Quality assurance of the abstract review was conducted for approximately 5% of the reviewed abstracts. We assessed interreviewer reliability for each reviewer by taking a random subset of abstracts from each reviewer and having a second reviewer rescreen the abstracts and determine whether they should be included or excluded. Overall, agreement among all reviewers was high, with an interreviewer reliability greater than 90%.
We selected articles for full manuscript review if they quantitatively measured a valid association between exposures of interest (policing practices) and outcomes of interest (HIV serostatus (primary outcome) or injection-related HIV risk behaviors among PWID (secondary outcomes)). Policing practices were defined a priori as any interaction with police or law enforcement officials experienced by PWID at the individual level (e.g., confiscation of syringes, arrest, being beaten, soliciting a bribe, etc.). The primary outcome was HIV serostatus, measured by validated laboratory methods (rapid test, blood draw, and confirmatory test). We included secondary outcomes of interest, such as self-reported HIV positivity and several injection-related risk factors for HIV. We defined injection-related HIV risk behaviors as any practice exhibited by PWID that could increase their individual risk of HIV transmission through injection drug use (e.g., syringe-sharing, avoiding opioid agonist therapy due to a police presence, using a “shooting gallery”). Factors specifically related to sexual risk (e.g., condom usage, multiple sex partners) were not considered injection drug use–related HIV risk behaviors and were not included in the review.
We excluded studies that 1) reported only qualitative findings; 2) did not disaggregate between PWID and non-PWID; 3) did not make individual PWID the unit of analysis (e.g., ecological analyses); 4) consisted of only modeling, cost-effectiveness, or analyses where PWID were not empirically investigated; or 5) did not present a valid association between a policing exposure and HIV risk or an HIV-related injection risk behavior.
Abstracts screened to be potentially eligible underwent full text review by 4 of the authors (P.B., C.R., L.A., and J.C.) to determine whether they met all inclusion criteria. At least 2 reviewers abstracted relevant data from eligible studies using a standardized coding and data abstraction form that we developed (Web Appendix 1). Briefly, this form collated study-specific data, including information on study design, sampling methods, recruitment period, geographic location, study population, demographic factors, analytical sample size, and reported summary measures. When possible, we reconstructed bivariate summary measures using raw numbers and/or proportions as reported in the document (e.g., odds ratios and 95% confidence intervals) to confirm the measured value given the data provided. For each eligible article, we recorded the prevalence of policing exposure(s), the prevalence of HIV serostatus and/or HIV risk factors, univariate summary measures, and adjusted associations from multivariable models (including covariates), when available. We could not conduct a meta-analysis because of high heterogeneity of reported policing exposures and HIV-related outcomes and inconsistent reporting time frames for various measures.
Any discrepancies in the coding were discussed at weekly meetings with the review team, including the senior author (J.C.), to reach a consensus. For each article, we also completed a standardized assessment-of-bias form with 14 criteria (see Web Appendix 2) to evaluate the strength of the potential causal relationship between the reported exposures and outcomes among the studies included in the review. Each article was discussed by the coding authors and assigned a quality rating (good, fair, or poor) based on how many of the criteria were met according to the assessment-of-bias form (Web Appendix 2). To ensure that all potentially eligible studies could be included during the full text review, we reviewed the bibliographies of all manuscripts included in the final review to identify any references relevant to the scope of the systematic review. Two of the authors (C.V. and L.A.) then determined whether these references had already been captured in our search. If not, we conducted a full-text review to determine eligibility.
RESULTS
Overall, we screened 8,201 unique abstracts (Figure 1). We reviewed 175 full-text articles; 27 articles met our inclusion criteria and were included in the review (Table 1). Eligible studies originated from 9 different countries (Canada, China, India, Malaysia, Mexico, Russia, Thailand, Ukraine, and the United States) across various income levels (low, low-middle, upper middle, and high). The region with the most included studies was North America (n = 15), followed by Southeast Asia (n = 5) and Eastern Europe (n = 5). The earliest article included in the review was published in 1999, though most (n = 19) were published in 2013 or later.
Figure 1.
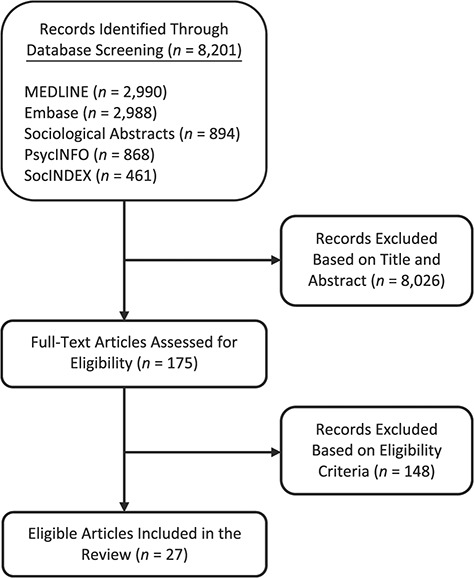
Selection of studies for a systematic review of the literature on policing practices and risk of human immunodeficiency virus (HIV) infection among people who inject drugs, 1981–2018.
Table 1.
Characteristics of Eligible Studies and Reported Policing Exposures, HIV-/Drug-Related Outcomes, and Measures of Association (n = 27) in a Systematic Literature Review, 1981–2018a
| First Author, Year (Reference No.) | City and Country | Sample Size (No.) | Policing Exposure | HIV/Drug-Related Outcome | Crude OR | 95% CI |
Adjusted
OR |
95% CI | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Exposure | Time Frame | Outcome | Time Frame | |||||||
| Bluthenthal, 1999 (37) | San Francisco, California, United States | 1,257 | Fear of arrest | Ever | HIV-positive | Current | 0.62 | 0.42, 0.93 | ||
| Fear of arrest | Ever | Shared syringe | Last 30 days | 4.80 | 3.32, 6.94 | |||||
| Fear of arrest | Ever | Shared injection supplies | Last 30 days | 2.37 | 1.86, 3.02 | |||||
| Rhodes, 2004 (47) | Togliatti City, Russia | 426 | Police confiscated injecting equipment | Ever | Receptive syringe-sharing | Last 4 weeks | 2.6 | 1.5, 4.5 | ||
| Arrested | Ever | Receptive syringe-sharing | Last 4 weeks | 2.1 | 1.2, 3.8 | |||||
| Arrested/detained for drugs | Last time arrested | Receptive syringe-sharing | Last 4 weeks | 3.2 | 1.7, 6.1 | |||||
| Pollini, 2008 (21) | Tijuana and Ciudad Juarez, Mexico | 426 | Arrested | Ever | Receptive syringe-sharing | Last 6 months | 2.44 | 1.14, 5.21 | ||
| Arrested for syringe possession (used) | Ever | Receptive syringe-sharing | Last 6 months | 4.31 | 2.75, 6.73 | 2.87b | 1.76, 4.69 | |||
| Arrested for syringe possession (sterile) | Ever | Receptive syringe-sharing | Last 6 months | 2.87 | 1.84, 4.49 | 2.05c | 1.26, 3.35 | |||
| Werb, 2008 (48) | Vancouver, British Columbia, Canada | 465 | Stopped, searched, or detained | Last 6 months | Receptive syringe-sharing | Last 6 months | 1.77 | 0.70, 4.42 | ||
| Stopped, searched, or detained | Last 6 months | Distributive syringe-sharing | Last 6 months | 5.66 | 2.23, 14.36 | 3.18d | 1.09, 9.30 | |||
| Flath, 2017 (49) | Baltimore, Maryland, United States | 367 | Any arrest | Last 6 months | Receptive syringe-sharing | Last 6 months | 1.36 | 0.85, 2.18 | ||
| Arrested | Last 6 months | Receptive syringe-sharing | Last 6 months | 2.13 | 1.32, 3.45 | |||||
| Stopped but not arrested | Last 6 months | Receptive syringe-sharing | Last 6 months | 1.74 | 1.07, 2.85 | |||||
| Beletsky, 2013 (38) | Tijuana and Ciudad Juarez, Mexico | 624 | Syringe confiscated | Last 6 months | Receptive syringe-sharing | Last month | 0.92 | 0.67, 1.27 | ||
| Syringe confiscated | Last 6 months | Injected in public | Last month | 1.74 | 1.26, 2.41 | |||||
| Syringe confiscated | Last 6 months | Injection help from “hit doctor” | Last month | 1.15 | 0.84, 1.59 | |||||
| Syringe confiscated | Last 6 months | HIV-positive | Current | 2.04 | 1.00, 4.21 | 2.54e | 1.11, 5.80 | |||
| Booth, 2013 (39) | Odessa, Ukraine | 200 | New syringes confiscated | Ever | HIV-positive | Current | 5.5 | 1.8, 16.6 | ||
| Arrested for carrying syringes | Ever | HIV-positive | Current | 2.4 | 0.9, 6.5 | |||||
| Did not buy syringes for fear of police | Ever | HIV-positive | Current | 3.3 | 1.4, 7.6 | |||||
| Avoided carrying syringes due to fear | Ever | HIV-positive | Current | 2.2 | 1.1, 4.4 | |||||
| Rushed injection due to police presence | Ever | HIV-positive | Current | 20.6 | 10.0, 42.7 | 12.6f | 5.4, 29.3 | |||
| Preloaded syringes confiscated | Ever | HIV-positive | Current | 3.5 | 1.9, 6.4 | |||||
| Forced by police to buy back syringes | Ever | HIV-positive | Current | 2.9 | 1.5, 5.4 | |||||
| Arrested for planted drugs | Ever | HIV-positive | Current | 3.0 | 1.3, 6.8 | |||||
| Bribe demanded | Ever | HIV-positive | Current | 1.4 | 0.8, 2.5 | |||||
| Detained | Ever | HIV-positive | Current | 1.4 | 0.8, 2.5 | |||||
| Beaten or tortured | Ever | HIV-positive | Current | 3.1 | 1.5, 6.5 | |||||
| Beletsky, 2014 (22) | New York, New York, United States | 500 | Stopped and frisked | Last 12 months | Less likely to use SEP | Last 12 months | 2.13 | 1.47, 3.13 | 1.69g | 1.12, 2.50 |
| Syringes confiscated | Last 12 months | Less likely to use SEP | Last 12 months | 1.64 | 0.83, 3.23 | |||||
| Stopped and frisked | Last 12 months | Receptive syringe-sharing | Last 12 months | 0.68 | 0.46, 1.00 | |||||
| Syringes confiscated | Last 12 months | Receptive syringe-sharing | Last 12 months | 1.67 | 0.92, 3.04 | 1.76h | 0.90, 3.44 | |||
| Hayashi, 2013 (50) | Bangkok, Thailand | 435 | Beaten by police | Ever | Syringe-sharing | Last 6 months | 1.81 | 1.06, 3.11 | 1.82i | 1.04, 3.20 |
| Tested for drugs by police | Ever | Syringe-sharing | Last 6 months | 2.17 | 1.18, 3.99 | 2.00i | 1.16, 3.45 | |||
| Beaten and tested for drugs by police | Ever | Syringe-sharing | Last 6 months | 2.61 | 1.46, 4.65 | 2.40i | 1.35, 4.26 | |||
| Hayashi, 2013 (40) | Bangkok, Thailand | 639 | Beaten by police | Ever | Syringe-sharing | Ever | 1.93 | 1.52, 2.45 | 1.44j | 1.15, 1.80 |
| Beaten by police | Ever | MMT use | Ever | 1.74 | 1.30, 2.33 | |||||
| Beaten by police | Ever | HIV-positive | Current | 1.35 | 1.08, 1.67 | |||||
| Lunze, 2014 (23) | St. Petersburg, Russia | 582 | Arrested for syringe possession/planted evidence | Ever | Receptive needle-sharing | Last 3 months | 1.68 | 1.12, 2.53 | ||
| Heath, 2016 (51) | Bangkok, Thailand | 437 | Tested for drugs by police | Ever | Avoiding health care | Ever | 1.80 | 1.10, 2.93 | ||
| Beaten by police | Ever | Avoiding health care | Ever | 1.38 | 0.90, 2.13 | |||||
| Michalopolous, 2016 (52) | Kuantan, Panang State, Malaysia | 154 | Rushed injection due to fear of police | Ever | Risky injection behavior | Last month | 2.29 | 1.15, 4.59 | ||
| Arrested | Ever | Risky injectio behavior | Last month | 2.71 | 0.66, 11.15 | |||||
| Avoided carrying syringes due to fear | Ever | Risky injection behavior | Last month | 1.49 | 0.74, 3.02 | |||||
| Clean syringe confiscated | Ever | Risky injection behavior | Last month | 1.93 | 1.01, 3.70 | |||||
| Drugs planted | Ever | Risky injection behavior | Last month | 1.08 | 0.53, 2.19 | |||||
| Forced by police to buy back drugs | Ever | Risky injection behavior | Last month | 1.51 | 0.75, 3.03 | |||||
| Armenta, 2015 (53) | San Diego, California, United States | 574 | Rushed injection due to police presence | Ever | Prefilled syringe use | Ever | 2.63 | 1.79, 3.86 | ||
| Police presence affected where to use drugs | Ever | Prefilled syringe use | Ever | 1.86 | 1.31, 2.66 | |||||
| Gu, 2014 (25) | Guangzhou, China | 133 | Worry about police arrest | Ever | MMT nonattendance | Recent | 12.0 | 1.6, 92.3 | ||
| Philbin, 2008 (27) | Tijuana, Mexico | 222 | Arrested for syringe possession (sterile) | Ever | Shooting gallery use | Last 6 months | 1.74 | 0.98, 3.10 | ||
| Arrested for syringe possession (used) | Ever | Shooting gallery use | Last 6 months | 2.79 | 1.51, 5.14 | 2.62k | 1.38, 4.97 | |||
| Ciudad Juarez, Mexico | 205 | Arrested for syringe possession (sterile) | Ever | Shooting gallery use | Last 6 months | 2.74 | 1.53, 4.92 | 1.96l | 1.01, 3.79 | |
| Arrested for syringe possession (used) | Ever | Shooting gallery use | Last 6 months | 2.82 | 1.58, 5.03 | |||||
| Strathdee, 2008 (54) | Tijuana, Mexico | 1,052 | Arrested | Ever | HIV-positive | Current | 0.92 | 0.38, 2.22 | ||
| Fairbairn, 2009 (24) | Bangkok, Thailand | 238 | Drugs planted | Ever | Syringe-sharing (receptive) | Ever | 2.16 | 1.27, 3.65 | ||
| Drugs planted | Ever | Syringe-sharing (distributive) | Ever | 2.06 | 1.22, 3.48 | 2.08m | 1.19, 3.66 | |||
| Drugs planted | Ever | MMT use | Ever | 1.82 | 1.10, 3.02 | |||||
| Strathdee, 2011 (36) | Tijuana and Ciudad Juarez, Mexico | 620 | Bribe demanded | Last 6 months | HIV-positive | Current | 1.61 | 0.73, 3.52 | ||
| Syringes confiscated | Last 6 months | HIV-positive | Current | 2.38 | 1.17, 4.81 | |||||
| Wagner, 2013 (55) | Los Angeles, California, United States | 187 | Received a citation | Last 2 years | Syringe-sharing (receptive) | Last 30 days | 1.51 | 0.82, 2.79 | ||
| Arrested | Last 2 years | Syringe-sharing (receptive) | Last 30 days | 1.71 | 0.93, 3.15 | |||||
| Shaw, 2015 (56) | Ottawa, Ontario, Canada | 270 | “Redzoned” by police | Ever | SIF use | Intended | 2.33 | 1.29, 4.20 | ||
| Stopped/searched | Ever | SIF use | Intended | 1.37 | 0.75, 2.48 | |||||
| Rafful, 2015 (57) | Tijuana, Mexico | 557 | Arrested | Ever | Use of high-dead-space syringes | Ever | 1.74 | 1.11, 2.71 | 1.84n | 1.11, 3.07 |
| Werb, 2015 (58) | Tijuana, Mexico | 637 | Paid police a bribe | Last 6 months | Receipt of OST | Last 6 months | 1.07 | 0.77, 1.50 | 1.69o | 1.02, 2.81 |
| Kutsa, 2016 (26) | 5 cities, Ukraine | 1,613 | Sexual assault by police | Ever | HIV-positive | Current | 1.48 | 0.77, 2.82 | ||
| Sexual assault by police | Ever | Receipt of OST | Ever | 1.10 | 0.68, 1.77 | |||||
| Physical assault by police | Ever | Receipt of OST | Ever | 1.48 | 1.20, 1.82 | |||||
| Lunze, 2016 (59) | St. Petersburg, Russia | 228 | Sexual assault by police | Ever | Receptive syringe-sharing | Last 3 months | 1.67 | 0.86, 3.26 | ||
| Beletsky, 2016 (32) | Tijuana, Mexico | 737 | Stopped/arrested | Last 6 months | Receptive syringe-sharing | Last 6 months | 1.77 | 1.21, 2.60 | ||
| Sarin, 2013 (60) | Delhi, India | 343 | Arrested for syringe possession and drug use | Ever | Receiving OST or attending an SEP | Last year | 0.51 | 0.27, 0.95 | ||
Abbreviations: CI, confidence interval; HIV, human immunodeficiency virus; MMT, methadone maintenance therapy; OR, odds ratio; OST, opioid substitution therapy; PWID, people who inject drugs; SEP, syringe exchange program; SIF, supervised injection facility.
a The table shows the number of significant decimal digits (up to 2 digits) reported by investigators. In 3 articles (25, 47, 39), only 1 decimal digit was reported.
b Results were adjusted for injecting in a shooting gallery, injecting in the street, injecting methamphetamine alone, and injecting cocaine alone.
c Results were adjusted for injecting in a shooting gallery, injecting in the street, injecting methamphetamine alone, and injecting cocaine alone.
d Results were adjusted for requiring help injecting, frequent “crack” cocaine use, homelessness, and recent incarceration.
e Results were adjusted for being sexually abused by a police officer, groin injection, normally injecting in public spaces, obtaining syringes from a pharmacy, years of education, and often/always injecting with a client around.
f Results were adjusted for number of times of injecting in the last 30 days, being perceived to be a safe injector most/all of the time, front-/back-loading with a dealer, and getting a drug solution from a preloaded syringe.
g Results were adjusted for Borough (New York City).
h Results were adjusted for sex, age, borough (New York City), and public/semipublic drug injection patterns.
i Results were adjusted for sex, injecting with others on a frequent basis, accessing voluntary drug treatment, and difficulty accessing sterile syringes.
j Results were adjusted for year of study enrollment, sex, ever being in prison, ever being in compulsory drug detention, reporting barriers in accessing health care, and ever having a nonfatal overdose.
k Results were adjusted for homelessness.
l Results were adjusted for age, homelessness, and ever having an overdose.
m Results were adjusted for midazolam use, history of overdose, and forced drug treatment.
n Results were adjusted for sex, cocaine being the first drug injected, age at first heroin injection, perception of legal status of carrying new syringes in Tijuana, and being deported to Tijuana.
o Results were adjusted for recent methamphetamine use, a more recent follow-up visit, and visit × bribe (interaction between the independent variable “paid bribe to police” and the variable “visit” (more recent follow-up visit)).
While each article included PWID in the study population, 2 included female sex workers who also injected drugs (35, 36), and another included PWID living with HIV who were heavy alcohol users (23). The most common recruitment methods were respondent-driven sampling, venue sampling, street outreach, and snowball sampling. The analytical sample sizes ranged from 133 to 1,613. Approximately half of the studies (n = 15) reported race/ethnicity data; only 1 study reported transgender status (22).
All manuscripts included in the review utilized a cross-sectional or serial cross-sectional analysis; no longitudinal analyses were identified. Half of the studies (n = 14) reported a single policing exposure, while the remainder reported multiple policing exposures. The most commonly measured policing exposures were arrest, arrest for syringe possession, syringe confiscation, being detained or frisked, and being beaten or sexually assaulted by police. Many of the articles (n = 12) presented HIV seroprevalence data; however, only 8 studies measured associations between prevalent HIV infection and at least 1 exposure to police practices. The most commonly measured HIV risk behaviors included syringe-sharing (receptive and/or distributive), use of a shooting gallery, and avoiding harm reduction services (opioid agonist therapy or syringe service programs) due to the presence of police.
As Table 1 shows, 1 study (37) reported a policing-related exposure (fear of arrest) that was significantly associated with reduced odds of HIV infection (odds ratio (OR) = 0.62, 95% confidence interval (CI): 0.42, 0.93). In 4 studies (36, 38–40), numerous policing practices were found to be significantly associated with increased odds of prevalent HIV infection. HIV infection was significantly associated with syringe confiscation (last 6 months) (OR = 2.38 (95% CI: 1.17, 4.81) (36) and OR = 2.04 (95% CI: 1.00, 4.21) (38)), confiscation of a new syringe (ever) (OR = 5.5, 95% CI: 1.8, 16.6) (39), not buying syringes for fear of police (OR = 3.3, 95% CI: 1.4, 7.6) (39), avoiding carrying syringes for fear of police (OR = 2.2, 95% CI: 1.1, 4.4) (39), rushing injections due to the presence of police (OR = 20.6, 95% CI: 10.0, 42.7) (39), preloaded syringe confiscation (OR = 3.5, 95% CI: 1.9, 6.4) (39), being forced to buy back syringes from police (OR = 2.9, 95% CI: 1.5, 5.4) (39), being arrested for planted drugs (OR = 3.0, 95% CI: 1.3, 6.8) (39), and being beaten or tortured (OR = 3.1 (95% CI: 1.5, 6.5) (39) and OR = 1.35 (95% CI: 1.08, 1.67) (40)).
Among the studies with a valid association between HIV infection and at least 1 policing exposure, the reported prevalence of HIV infection in the sample populations varied from 4.0% to 54.5%. The policing exposures with the highest reported prevalence among these studies were being arrested (87.0%), having a bribe demanded (73.0%), and having syringes confiscated (48.0%). Figure 2 demonstrates the relative prevalence of HIV infection and reported policing exposures for several studies with valid associations, taking into account the relative sample size for each study (size of the bubble).
Figure 2.
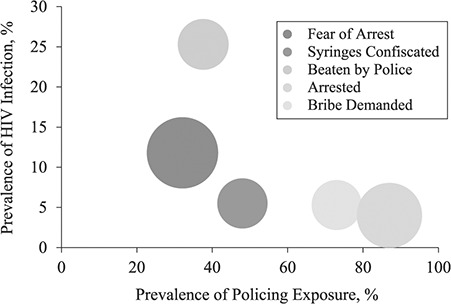
Prevalence of policing exposure, prevalence of human immunodeficiency virus (HIV) infection, and relative sample size (bubble size) among 5 studies (36–40) that found a valid association between HIV infection and at least 1 policing exposure in a systematic literature review, 1981–2018.
Most studies (n = 21) identified a significant association between at least 1 policing exposure and an HIV risk behavior related to injection drug use, of which syringe-sharing was the most common. Syringe-sharing was significantly associated with fear of arrest, confiscation of injection equipment, syringe confiscation, any arrest, an arrest for syringe possession, being detained, being beaten by police, being tested for drugs by police, and having drugs planted by police. For example, in Bangkok, Thailand, the odds of sharing syringes were 1.93–2.45 times higher among PWID who reported being beaten by police than among those who did not.
Several studies (n = 9) also described associations be-tween police practices and utilization of community harm reduction resources. Events such as being stopped and frisked, having syringes confiscated, being tested for drugs by police, and being arrested for syringe possession, as well as worrying about being arrested, were significantly associated with nonuse of opioid agonist therapy, avoidance of syringe service programs, and/or avoidance of health care. For example, among PWID in Delhi, India, the odds of participating in syringe service programs or receiving opioid agonist therapy in the past year were 5%–73% lower among PWID arrested for syringe or drug possession than among those who were not arrested.
DISCUSSION
Overall, we found data from 27 studies across 9 countries reporting significant associations between policing practices and prevalent HIV infection or injection-related risk behavior among PWID. Our findings indicate that certain policing practices are overwhelmingly detrimental to the HIV risk environment of PWID. For example, we that found syringe confiscation was consistently associated with either higher HIV seroprevalence or riskier injection practices. Only 1 study showed a protective effect of policing, as fear of arrest was associated with lower odds of HIV infection (37).
The socioeconomic and geographic diversity in the settings identified suggests that this phenomenon is not limited to settings with poorly trained police officers or weak judicial systems that enable officers who violate the civil and human rights of citizens to act with impunity. Indeed, many of the studies we identified were from the United States or Canada, high-income countries with institutions to ensure reasonable due process and legal recourse for persons who may have had negative interactions with police. Importantly, over 179 countries have documented injection drug use (2). Thus, despite a lack of published findings, the associations we analyzed in this review are probably relevant to these countries as well (Web Figure 1).
Our review extends findings from previous global systematic reviews and meta-analyses that have examined the role of criminal justice in public health. Footer et al. (33) found that individual-level policing practices, such as arrest, extortion, and condom confiscation, were commonly committed among female sex workers. Indeed, some of these behaviors were also common in our review, illustrating that populations at heightened risk of HIV are regular targets of police. Female sex workers who also inject drugs are likely to be especially vulnerable due to injection-related and sexual risk factors (30).
In a recent review by DeBeck et al. (17), laws criminalizing drug use were found to adversely affect PWID health and increase HIV risks. While the authors did identify certain policing practices as a general contributor to these harms, they did not focus on specific policing practices at the individual level. This is an important distinction, as we have identified specific practices, such as syringe confiscation (irrespective of its legality), arrest, bribery, and violence/torture, as behaviors that exacerbate HIV risk. Formal legal structures are widely recognized as drivers of the individual risk environment, but it is the enforcement of the law on the ground by police officers that most directly impacts PWID.
Previous research has demonstrated substantial treatment gaps and challenges for achieving success along the HIV care continuum for PWID (41). As was demonstrated in this review, street policing is a pervasive force in the lives of many PWID which bears the potential to interfere at each level of the prevention and treatment cascades. Additional evidence suggests that unofficial police detentions regularly interrupt adherence to opioid agonist therapy and antiretroviral therapy. This further exacerbates efforts to improve the latter pillars of the HIV care continuum for PWID, including retention in care and viral suppression (42, 43). Given the high frequency of these practices and associations with HIV risk, mitigating these specific practices through interventions such as police education programs is vital.
As we noted above, we did not focus on incarceration, since the injection-related risks of HIV infection in incarceration settings have been well characterized. For example, in a recent meta-analysis, Stone et al. (19) found that the immediate postrelease period was associated with an 81% increased risk of HIV seroconversion. In addition, the negative public health effects of incarceration are conditional on arrest and detainment, which are often performed by street-level police officers. Thus, officers often serve as the “gatekeepers” to the deleterious consequences of incarceration and are therefore critical agents in aligning public health with criminal justice involvement. In attempts to reform drug policy, including decriminalization and legalization, officials will need to allocate resources to ensure that police are knowledgeable of the reforms and have the ability to successfully implement them. Baseline findings from a police education program in Tijuana, Mexico, found that police knowledge of drug decriminalization laws was low, but the program was successful in improving knowledge of drug and syringe possession policy, as well as intent to inform suspects of the laws (30, 44, 45). Correct legal knowledge among police and access to public health resources, such as harm reduction, for PWID will be necessary to successfully implement any drug policy reform.
In several studies, we found that PWID did not attend or avoided harm reduction programs due to some form of police harassment, arrest, or fear thereof. The perception that PWID should avoid these critical prevention programs due to police is problematic and complicates program implementation. The effectiveness of harm reduction is proportional to the self-efficacy of PWID in accessing these sites without experiencing a negative encounter with police. To ensure greater uptake and scale, harm reduction programs should be supported by an appropriate policy environment where police are shown the role that harm reduction plays in public health.
Police also hold the capacity to play an enabling role for PWID to improve public health outcomes and reduce recidivism rates. For example, the Law Enforcement Assisted Diversion (LEAD) program has demonstrated that participants have 60% lower odds of subsequent arrest than those who do not receive the intervention (46). While we did not identify any studies documenting positive policing practices, such as referral to harm reduction programs, future interventions and research should focus on facilitating and incentivizing police-initiated referrals.
Overall, we found a high degree of heterogeneity among the reported odds ratios. This is due, in part, to a lack of harmonization between both policing variables and risk behavior factors, including reporting time frames. Varying prevalences of both exposure and outcome variables across study settings may also have contributed to the odds ratio heterogeneity. Further, a number of analytical explanations should be considered and may be especially relevant among studies that report results from multivariable models. For example, the relative prevalence and statistical treatment of effect modifiers was not consistent. Additionally, the model selection process varied among the included studies.
We did not conduct a meta-analysis because of high heterogeneity in the various measures. The formulation of summary measures and forest plots would have provided additional insight but would require that variables be similar enough in construction to be combined. Future studies in this line of research should utilize standardized factors to allow for quantitative synthesis and meta-analysis. Additionally, future research should prioritize the inclusion of data on race, ethnicity, and sex (including transgender individuals) to allow for insight into the relative impact of policing on particularly vulnerable groups.
Our review was not without limitations. First, caution is warranted in interpreting the findings, since all studies included in the review were cross-sectional, and thus we could not determine the temporality of the policing practices and HIV seroprevalence and associated risk behaviors. Second, selection bias is a concern, as persons with more severe substance use disorders who engage in riskier injection behaviors could also be more likely to have a negative encounter with police. Despite this, we note that the prevalence of many policing practices was high (>50%), indicating that police most likely do not exclusively target particularly vulnerable high-risk groups (e.g., homeless PWID). In a systematic review, publication bias is a concern, as some investigators may have neglected to publish nonsignificant findings. Because of the heterogeneity of the constructs included in this review, we were unable to produce symmetry tests to make inferences regarding publication bias. However, many of the reported associations included in our review were not from the primary analysis of the article in which they were published. Therefore, we reason that publication bias may not have played a significant role in the reporting of these associations. Lastly, we did not include qualitative data in our review; however, we note the importance of formative qualitative data to contextualize these structural-level factors.
In conclusion, these results highlight robust evidence associating harmful policing practices with prevalent HIV infection and risky injection behaviors worldwide. The role of police should be viewed as a single agent within an intricate system of conflicting policy, public safety, and public health priorities. As such, the success of public health programs for PWID will require coordination and cooperation from police agencies.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Division of Infectious Diseases and Global Public Health, School of Medicine, University of California, San Diego, La Jolla, California, United States (Pieter Baker, Leo Beletsky, Liliana Avalos, Carlos Rivera, Steffanie A. Strathdee, Javier Cepeda); Graduate School of Public Health, San Diego State University, San Diego, California, United States (Pieter Baker, Carlos Rivera); Health in Justice Action Lab, School of Law, Northeastern University, Boston, Massachusetts, United States (Leo Beletsky); and Department of Health Sciences, Bouvé College of Health Sciences, Northeastern University, Boston, Massachusetts, United States (Leo Beletsky).
This work was supported by the National Institute on Drug Abuse (grants R01DA039073 (P.B., L.B., S.A.S., J.C.), K01DA043421 (J.C.), and T32DA023356 (P.B.)) and the University of California, San Diego, Center for AIDS Research (National Institute of Allergy and Infectious Diseases international pilot grant 5P30AI036214).
The funding sources played no role in the writing of the manuscript or the decision to submit it for publication. No authors were paid to write this article by a pharmaceutical company or other agency. The corresponding author had full access to all of the data in the study and takes final responsibility for the decision to submit the article for publication.
Conflict of interest: none declared.
REFERENCES
- 1. Degenhardt L, Charlson F, Mathers B, et al. The global epidemiology and burden of opioid dependence: results from the Global Burden of Disease 2010 Study. Addiction. 2014;109(8):1320–1333. [DOI] [PubMed] [Google Scholar]
- 2. Degenhardt L, Peacock A, Colledge S, et al. Global prevalence of injecting drug use and sociodemographic characteristics and prevalence of HIV, HBV, and HCV in people who inject drugs: a multistage systematic review. Lancet Glob Health. 2017;5(12):e1192–e1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Degenhardt L, Charlson F, Stanaway J, et al. Estimating the burden of disease attributable to injecting drug use as a risk factor for HIV, hepatitis C, and hepatitis B: findings from the Global Burden of Disease Study 2013. Lancet Infect Dis. 2016;16(12):1385–1398. [DOI] [PubMed] [Google Scholar]
- 4. Peters PJ, Pontones P, Hoover KW, et al. HIV infection linked to injection use of oxymorphone in Indiana, 2014–2015. N Engl J Med. 2016;375(3):229–239. [DOI] [PubMed] [Google Scholar]
- 5. Strathdee SA, Beyrer C. Threading the needle—how to stop the HIV outbreak in rural Indiana. N Engl J Med. 2015;373(5):397–399. [DOI] [PubMed] [Google Scholar]
- 6. Mathers BM, Degenhardt L, Ali H, et al. HIV prevention, treatment, and care services for people who inject drugs: a systematic review of global, regional, and national coverage. Lancet. 2010;375(9719):1014–1028. [DOI] [PubMed] [Google Scholar]
- 7. Stone K, Shirley-Beavan S. The Global State of Harm Reduction 2018. 6th ed. London, United Kingdom: Harm Reduction International; 2018. https://www.hri.global/files/2019/02/05/global-state-harm-reduction-2018.pdf. Accessed October 22, 2019. [Google Scholar]
- 8. Heimer R The policy-driven HIV epidemic among opioid users in the Russian Federation. Curr HIV/AIDS Rep. 2018;15(3):259–265. [DOI] [PubMed] [Google Scholar]
- 9. Rudd RA, Aleshire N, Zibbell JE, et al. Increases in drug and opioid overdose deaths—United States, 2000–2014. MMWR Morb Mortal Wkly Rep. 2016;64(50-51):1378–1382. [DOI] [PubMed] [Google Scholar]
- 10. Mummolo J Militarization fails to enhance police safety or reduce crime but may harm police reputation. Proc Natl Acad Sci U S A. 2018;115(37):9181–9186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Puras D, Hannah J. Reasons for drug policy reform: prohibition enables systemic human rights abuses and undermines public health. BMJ. 2017;356:i6586. [DOI] [PubMed] [Google Scholar]
- 12. Wildeman C, Wang EA. Mass incarceration, public health, and widening inequality in the United States. Lancet. 2017;389(10077):1464–1474. [DOI] [PubMed] [Google Scholar]
- 13. Wohl DA HIV and mass incarceration: where infectious diseases and social justice meet. N C Med J. 2016;77(5):359–364. [DOI] [PubMed] [Google Scholar]
- 14. American Civil Liberties Union War Comes Home: The Excessive Militarization of American Policing. New York, NY: American Civil Liberties Union; 2014. https://www.aclu.org/sites/default/files/assets/jus14-warcomeshome-report-web-rel1.pdf. Accessed May 1, 2018. [Google Scholar]
- 15. Strathdee SA, Beletsky L, Kerr T. HIV, drugs and the legal environment. Int J Drug Policy. 2015;26(suppl 1):S27–S32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. van Dijk AJ, Herrington V, Crofts N, et al. Law enforcement and public health: recognition and enhancement of joined-up solutions. Lancet. 2019;393(10168):287–294. [DOI] [PubMed] [Google Scholar]
- 17. DeBeck K, Cheng T, Montaner JS, et al. HIV and the criminalisation of drug use among people who inject drugs: a systematic review. Lancet HIV. 2017;4(8):e357–e374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Koh HK, Kerlikowske RG, Botticelli MP. A smarter war on drugs. JAMA. 2018;320(22):2301–2302. [DOI] [PubMed] [Google Scholar]
- 19. Stone J, Fraser H, Lim AG, et al. Incarceration history and risk of HIV and hepatitis C virus acquisition among people who inject drugs: a systematic review and meta-analysis. Lancet Infect Dis. 2018;18(12):1397–1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Dolan K, Wirtz AL, Moazen B, et al. Global burden of HIV, viral hepatitis, and tuberculosis in prisoners and detainees. Lancet. 2016;388(10049):1089–1102. [DOI] [PubMed] [Google Scholar]
- 21. Pollini RA, Brouwer KC, Lozada RM, et al. Syringe possession arrests are associated with receptive syringe sharing in two Mexico-US border cities. Addiction. 2008;103(1):101–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Beletsky L, Heller D, Jenness SM, et al. Syringe access, syringe sharing, and police encounters among people who inject drugs in New York City: a community-level perspective. Int J Drug Policy. 2014;25(1):105–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lunze K, Raj A, Cheng DM, et al. Punitive policing and associated substance use risks among HIV-positive people in Russia who inject drugs. J Int AIDS Soc. 2014;17(1):19043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Fairbairn N, Kaplan K, Hayashi K, et al. Reports of evidence planting by police among a community-based sample of injection drug users in Bangkok, Thailand. BMC Int Health Hum Rights. 2009;9:Article 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Gu J, Xu H, Lau JT, et al. Situation-specific factors predicting nonadherence to methadone maintenance treatment: a cross-sectional study using the case-crossover design in Guangzhou, China. AIDS Care. 2014;26(suppl 1):S107–S112. [DOI] [PubMed] [Google Scholar]
- 26. Kutsa O, Marcus R, Bojko MJ, et al. Factors associated with physical and sexual violence by police among people who inject drugs in Ukraine: implications for retention on opioid agonist therapy. J Int AIDS Soc. 2016;19(4 suppl 3):20897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Philbin M, Pollini RA, Ramos R, et al. Shooting gallery attendance among IDUs in Tijuana and Ciudad Juarez, Mexico: correlates, prevention opportunities, and the role of the environment. AIDS Behav. 2008;12(4):552–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. United Nations Office on Drugs and Crime Outcome Document of the 2016 United Nations General Assembly Special Session on the World Drug Problem (Thirtieth Special Session of the United Nations General Assembly, New York, New York, April 19–21, 2016). New York, NY: United Nations; 2016. https://www.unodc.org/documents/postungass2016/outcome/V1603301-E.pdf. Accessed October 8, 2019. [Google Scholar]
- 29. Arredondo J, Gaines T, Manian S, et al. The law on the streets: evaluating the impact of Mexico’s drug decriminalization reform on drug possession arrests in Tijuana, Mexico. Int J Drug Policy. 2018;54:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Arredondo J, Strathdee SA, Cepeda J, et al. Measuring improvement in knowledge of drug policy reforms following a police education program in Tijuana, Mexico. Harm Reduct J. 2017;14(1):Article 72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Beletsky L, Thomas R, Smelyanskaya M, et al. Policy reform to shift the health and human rights environment for vulnerable groups: the case of Kyrgyzstan’s instruction 417. Health Hum Rights. 2012;14(2):34–48. [PubMed] [Google Scholar]
- 32. Beletsky L, Wagner KD, Arredondo J, et al. Implementing Mexico’s “narcomenudeo” drug law reform: a mixed methods assessment of early experiences among people who inject drugs. J Mixed Methods Res. 2016;10(4):384–401. [Google Scholar]
- 33. Footer KH, Silberzahn BE, Tormohlen KN, et al. Policing practices as a structural determinant for HIV among sex workers: a systematic review of empirical findings. J Int AIDS Soc. 2016;19(4 suppl 3):20883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Centers for Disease Control and Prevention Pneumocystis pneumonia—Los Angeles. MMWR Morb Mortal Wkly Rep. 1981;30(21):250–252. [PubMed] [Google Scholar]
- 35. Beletsky L, Martinez G, Gaines T, et al. Mexico’s northern border conflict: collateral damage to health and human rights of vulnerable groups. Rev Panam Salud Publica. 2012;31(5):403–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Strathdee SA, Lozada R, Martinez G, et al. Social and structural factors associated with HIV infection among female sex workers who inject drugs in the Mexico-US border region. PLoS One. 2011;6(4):e19048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Bluthenthal RN, Lorvick J, Kral AH, et al. Collateral damage in the war on drugs: HIV risk behaviors among injection drug users. Int J Drug Policy. 1999;10(1):25–38. [Google Scholar]
- 38. Beletsky L, Lozada R, Gaines T, et al. Syringe confiscation as an HIV risk factor: the public health implications of arbitrary policing in Tijuana and Ciudad Juarez, Mexico. J Urban Health. 2013;90(2):284–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Booth RE, Dvoryak S, Sung-Joon M, et al. Law enforcement practices associated with HIV infection among injection drug users in Odessa, Ukraine. AIDS Behav. 2013;17(8):2604–2614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Hayashi K, Ti L, Csete J, et al. Reports of police beating and associated harms among people who inject drugs in Bangkok, Thailand: a serial cross-sectional study. BMC Public Health. 2013;13:Article 733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Escudero DJ, Lurie MN, Mayer KH, et al. The risk of HIV transmission at each step of the HIV care continuum among people who inject drugs: a modeling study. BMC Public Health. 2017;17(1):Article 614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Izenberg JM, Bachireddy C, Soule M, et al. High rates of police detention among recently released HIV-infected prisoners in Ukraine: implications for health outcomes. Drug Alcohol Depend. 2013;133(1):154–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Polonsky M, Azbel L, Wegman MP, et al. Pre-incarceration police harassment, drug addiction and HIV risk behaviours among prisoners in Kyrgyzstan and Azerbaijan: results from a nationally representative cross-sectional study. J Int AIDS Soc. 2016;19(4 suppl 3):20880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Arredondo J, Beletsky L, Baker P, et al. Interactive versus video-based training of police to communicate syringe legality to people who inject drugs: the SHIELD Study, Mexico, 2015–2016. Am J Public Health. 2019;109(6):921–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Mittal ML, Artamonova I, Baker P, et al. Improving police conceptual knowledge of Mexico’s law on cannabis possession: findings from an assessment of a police education program. Am J Addict. 2018;27(8):608–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Collins SE, Lonczak HS, Clifasefi SL. Seattle’s Law Enforcement Assisted Diversion (LEAD): program effects on recidivism outcomes. Eval Program Plann. 2017;64:49–56. [DOI] [PubMed] [Google Scholar]
- 47. Rhodes T, Judd A, Mikhailova L, et al. Injecting equipment sharing among injecting drug users in Togliatti City, Russian Federation: maximizing the protective effects of syringe distribution. J Acquir Immune Defic Syndr. 2004;35(3):293–300. [DOI] [PubMed] [Google Scholar]
- 48. Werb D, Wood E, Small W, et al. Effects of police confiscation of illicit drugs and syringes among injection drug users in Vancouver. Int J Drug Policy. 2008;19(4):332–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Flath N, Tobin K, King K, et al. Enduring consequences from the war on drugs: how policing practices impact HIV risk among people who inject drugs in Baltimore City. Subst Use Misuse. 2017;52(8):1003–1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Hayashi K, Ti L, Buxton JA, et al. The effect of exposures to policing on syringe sharing among people who inject drugs in Bangkok, Thailand. AIDS Behav. 2013;17(8):2615–2623. [DOI] [PubMed] [Google Scholar]
- 51. Heath AJ, Kerr T, Ti L, et al. Healthcare avoidance by people who inject drugs in Bangkok, Thailand. J Public Health (Oxf). 2016;38(3):e301–e308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Michalopoulos LM, Jiwatram-Negrón T, Choo MK, et al. The association between psychosocial and structural-level stressors and HIV injection drug risk behavior among Malaysian fishermen: a cross-sectional study. BMC Public Health. 2016;16:Article 464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Armenta RF, Roth AM, Wagner KD, et al. Prevalence and correlates of the use of prefilled syringes among persons who inject drugs in San Diego, CA. J Urban Health. 2015;92(6):1081–1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Strathdee SA, Lozada R, Pollini RA, et al. Individual, social, and environmental influences associated with HIV infection among injection drug users in Tijuana, Mexico. J Acquir Immune Defic Syndr. 2008;47(3):369–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Wagner KD, Simon-Freeman R, Bluthenthal RN. The association between law enforcement encounters and syringe sharing among IDUs on skid row: a mixed methods analysis. AIDS Behav. 2013;17(8):2637–2643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Shaw A, Lazarus L, Pantalone T, et al. Risk environments facing potential users of a supervised injection site in Ottawa, Canada. Harm Reduct J. 2015;12:Article 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Rafful C, Zule W, González-Zúñiga PE, et al. High dead-space syringe use among people who inject drugs in Tijuana, Mexico. Am J Drug Alcohol Abuse. 2015;41(3):220–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Werb D, Wagner KD, Beletsky L, et al. Police bribery and access to methadone maintenance therapy within the context of drug policy reform in Tijuana, Mexico. Drug Alcohol Depend. 2015;148:221–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Lunze K, Raj A, Cheng DM, et al. Sexual violence from police and HIV risk behaviours among HIV-positive women who inject drugs in St. Petersburg, Russia—a mixed methods study. J Int AIDS Soc. 2016;19(4 suppl 3):20877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Sarin E, Samson LJ, Sweat MD. Impact of acts of discrimination on quality of life among injecting drug users in Delhi, India. Soc Indic Res. 2013;113(1):319–334. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


