Abstract
We conducted a systematic review that examined the link between individual drug categories and violent outcomes. We searched for primary case-control and cohort investigations that reported risk of violence against others among individuals diagnosed with drug use disorders using validated clinical criteria, following Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines. We identified 18 studies published during 1990–2019, reporting data from 591,411 individuals with drug use disorders. We reported odds ratios of the violence risk in different categories of drug use disorders compared with those without. We found odds ratios ranging from 0.8 to 25.0 for most individual drug categories, with generally higher odds ratios among individuals with polydrug use disorders. In addition, we explored sources of between-study heterogeneity by subgroup and meta-regression analyses. Cohort investigations reported a lower risk of violence than case-control reports (odds ratio = 2.7 (95% confidence interval (CI): 2.1, 3.5) vs. 6.6 (95% CI: 5.1, 8.6)), and associations were stronger when the outcome was any violence rather than intimate partner violence (odds ratio = 5.7 (95% CI: 3.8, 8.6) vs. 1.7 (95% CI: 1.4, 2.1)), which was consistent with results from the meta-regression. Overall, these findings highlight the potential impact of preventing and treating drug use disorders on reducing violence risk and associated morbidities.
Keywords: crime, meta-analysis, opioid, sedative, stimulant, substance misuse, substance use disorder, violence
Abbreviations
- CI
confidence interval
- OR
odds ratio
INTRODUCTION
Drug misuse is a global public health concern (1, 2). Worldwide, around 70 million individuals were diagnosed with a drug use disorder (1). Drug use disorders have been associated with a wide range of adverse outcomes, including suicide, comorbid mental illness, and premature mortality (3–5). In addition, drug use disorders increase risk of violence against others (3, 6–9). Further, the prevalence of drug use disorder in prison ranges from 10% to 61% in men and 30% to 69% in women (10), which is substantially elevated compared with the prevalence, ranging from 0.6% to 4.0% in men and 0.3% to 2.9% in women, in the general population (11).
The prevalence differs between individual categories of drug use disorders. Globally, the prevalence rate per 100,000 people is 65 for stimulants such as amphetamines, 78 for cocaine, 290 for cannabis, 353 for opioids, and less than 52 for other drugs including hallucinogens and sedatives (12). Although research has consistently found increased violence risk in drug use disorders, individual studies have shown that the magnitude of this increased risk varies depending on the drug category. For example, when compared with the general population, odds ratios of violence in cannabis use disorder have ranged from 1 to 7 (13–17), and in cocaine, they have varied from 2 to 11 (18–21). This might be due to different methodologies adopted and specific outcomes used in different studies. Furthermore, it has been suggested that certain type of stimulants, such as crack cocaine, that are associated with irritability and aggressiveness (7, 22), might have a higher risk of criminal behavior than others, including less-strong forms of cannabis that might reduce risks due to sedative and calming effects (23, 24). This is important to clarify further in that more precise estimates would allow for risk stratification, better treatment allocation (especially if liaison with criminal justice agencies is required), and more evidence-based estimates of the population impact of certain drug policies.
Previous reviews have explored associations between general drug misuse and violence against others but have mostly investigated selected samples, such as prisoners (25) or psychiatric patients (26–29). In addition, most existing reviews have not used standardized clinical criteria to identify drug use disorders (22, 30). This could introduce bias given that self-report of the extent of drug use is often unreliable (31). Validated diagnostic tools based on validated criteria (such as the Diagnostic and Statistical Manual of Mental Disorders or International Classification of Diseases) can identify individuals with a severe form of drug misuse, who might present to clinical and addiction services, and for whom there is evidence-based treatment available. In addition, diagnostic categories enable consistent communication between clinicians and researchers because the criteria are widely known and validated cross-culturally with decent reliability measures (32, 33). Furthermore, the most recent review that examined the link between general drug use disorders and violence was conducted more than 2 decades ago (34) and did not explore potential source of between-study heterogeneity or differences between individual categories of druguse.
The link between drug use and violent outcomes is complex; a wide range of factors—such as experiences of violence including both as victim and perpetrator, the comorbidity of other mental disorders, and social determinants such as sex, ethnicity, and poverty—might moderate and mediate this link. For instance, previous violence victimization might trigger development of drug use disorders, which might in turn lead to later perpetration of violence (35–39). Moreover, structural causes of drug use problems are relevant, given that they have been linked to criminalization (23), as well as factors such as poverty (40), poor mental health (4, 41), treatment availability (42), and homelessness (43). In addition, physical and psychological effects of drugs can lead to agitation, aggression, and cognitive impairment that might in turn heighten risk of violence. Individuals with drug use disorders might also turn to violence to finance their drug use, and disputes within illegal drug markets might be associated with violence (44). To address these gaps in the evidence, in this review, we aimed to synthesize the odds of violence in individual drug use disorders and explore sources of heterogeneity between studies.
METHODS
We conducted this review following the Meta-analyses of Observational Studies in Epidemiology (MOOSE) (45) and Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines (46). The study was registered with an international prospective register of systematic reviews (PROSPERO CRD42019119533).
Search strategy
We conducted searches in the following digital databases from the inception of the databases (dated from January 1, 1927) to February 18, 2019: PubMed, Web of Science, Embase, Ovid MEDLINE, PsycINFO, Global Health, and US National Criminal Justice Reference Service Abstract Database. We used a combination of search terms related to drug misuse (i.e., illegal drug OR illegal substance OR marijuana OR cocaine OR cannabis OR opioid OR heroin OR methamphetamine OR stimulant*) AND violence (i.e., violen* OR crim* OR homicide OR aggress* OR offen*) AND study design (i.e., cohort OR longitudinal OR follow-up OR prospective OR case-control). We included studies of both illegally and legally obtained drugs. There were no language restrictions, and non-English-language articles were translated. We also scanned reference lists in an attempt to identify additional articles. We searched for unpublished literature including conference proceedings, theses, and dissertations. The first author (S.Z.) conducted the initial screening of the titles and abstracts for inclusion and exclusion. S.Z. and R.Y. screened full-text publications for eligibility. Any uncertainties were discussed with S.F.
Study selection
Inclusion criteria were: 1) cohort and case-control studies that examined link between individual categories of drug use disorders and violent outcomes and provided data for calculation of odds ratio between individuals with and without the drug use disorder being studied, and eligible case-control studies were those that reported prevalence of drug use disorders in cases with and without violence perpetration; 2) investigations that reported drug use disorders (or, in older studies, equivalent diagnostic categories of drug abuse or dependence) meeting diagnostic criteria for Diagnostic and Statistical Manual of Mental Disorders and International Classification of Diseases; and 3) studies that reported violent outcomes, including any violence and not being limited to context (e.g., community, domestic, intimate partner), type of crime (e.g., homicide, assault, threat or intimidation, and all sexual offenses), and measures (self-report, family report, or official/criminal records).
We excluded: 1) animal investigations; 2) experimental, cross-sectional, qualitative studies, or randomized controlled trials; 3) investigations with within-individual designs; 4) studies that used self-report (47) (e.g., Addiction Severity Index) or urine tests to identify drug use or that did not separate drug misuse from alcohol and nicotine misuse; 5) reports with recidivism or reoffending as outcomes (48); 6) studies in selected samples (e.g., offenders, cohorts with mental disorders) so we could increase the generalizability of risk estimates to the general population; 7) investigations that used the nonspecific outcome of all criminal behavior, antisocial behavior, or delinquency, which was not broken down for violence specifically; 8) studies that reported selected participants under medication (e.g., antidepressant, antipsychotic drugs, or other prescription drugs) or individuals undergoing other interventions for drug use disorders; or 9) case-series studies or reviews.
In case of duplicate samples, we included the study that was most recent, used the most common outcome, or had the largest sample. If a study reported outcomes at multiple time points, outcomes with the longest follow-up period were included.
Data extraction
We used a standardized form to extract data. The following information was recorded: study design, country, sample characteristics, diagnostic criteria, category of drug use disorders, type of drugs, comparison group, sex, age, years of follow-up, and study period. S.Z. conducted the initial data extraction. In case of uncertainties, R.Y. and S.F. were consulted.
Statistical analysis
Quality of the individual study was assessed using the Newcastle-Ottawa Quality Assessment Scale (49). Heterogeneity was estimated using I2. I2 is reported as a percentage out of 100%, where 0%–40% represents low heterogeneity, 30%–60% might indicate moderate heterogeneity, 50%–90% might denote substantial heterogeneity, and 75%–100% might indicate considerable heterogeneity (50, 51). All effect sizes were converted into odds ratios and converted from Pearson’s r and Cohen’s d using standard approaches (52). Sources of heterogeneity were explored using subgroup analyses and meta-regression analyses. Meta-regression was conducted to estimate the extent to which one or more measured covariates (the same variables as used in the subgroup analysis) explained the observed heterogeneity in risk estimates between primary studies (50). The same variables were used in the subgroup and meta-regression analyses, and only nonoverlapping samples were included in the analyses. When testing the effect of sample size, we excluded 2 studies that were disproportionately large (53, 54). We set the years of follow-up as a continuous variable and also a dichotomous variable using the median period as the cut-off. Other analyses included estimating associations between drug use disorders and violence while excluding studies published before 2000 and subgroup analyses by different comparison groups. We tested publication bias using Egger’s test (55), with P < 0.05 indicating publication bias. Analyses were performed using STATA, version 13 (StataCorp LP, College Station, Texas).
RESULTS
We identified 18 eligible studies (for details, see Figure 1 and Table 1) that included 591,411 individuals with drug use disorders. Studies were from 5 countries: 14 from the United States (n = 542,393, 91.7%) (53, 54, 56–67) and 1 each from New Zealand (n = 182, 0.03%) (68), Denmark (n = 43,403, 7.3%) (69), the Netherlands (n = 5,303, 0.9%) (70), and Turkey (n = 130, 0.02%) (71). Eight studies used case–control designs (53, 54, 56, 58, 63, 66, 67, 71); the remaining 10 studies were longitudinal cohorts with a median follow-up of 9.5 years.
Figure 1.
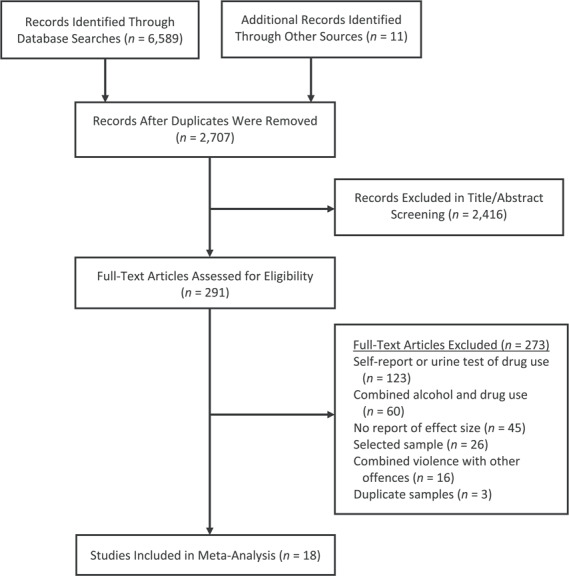
Flowchart of systematic search strategy of primary studies on drug use disorders and violence in multiple countries, 1990–2019.
Table 1.
Summary of Included Studies on Risk of Violence in Drug Use Disorders
| First Author, Year (Reference No.) | Country | Source of Population | DiagnosisCriteria | Design | Type of Drugs | ComparisonGroups a | Sample Size | Age, years | Sex | Year | Follow-up, years | Outcome | Source of Outcome | Assessed Alcohol Use |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Swanson, 1990 (56) | US | The Epidemiologic Catchment Area surveys | DSM-IIIa | Case-control | Cannabis use dependence, other drugs | Non–drug use disorder | 8,061 | ≥18 | Mixed | 1983 | N/A | Violence | Self-report | Yes |
| Friedman, 1996 (57) | US | A longitudinal study of the National Collaborative Perinatal Project | DSM-III | Cohort | Marijuana use, drug abuse | Non– marijuana use, non–drug abuse | 380 | 25.5 ± 6.1 | Mixed | 1985 | 2.5 | Violence | Self-report | Yes |
| Arseneault, 2000 (68) | New Zealand | The Dunedin Study | DSM-III-R | Cohort | Marijuana dependence disorder | Non–marijuana dependence disorder | 182 | Mean, 21 | Mixed | 1994 | 21 | Violence | Court convictions and/or self-report | Yes |
| Corrigan, 2005 (66) | US | The National Comorbidity Survey (NCS) | DSM-III-R | Case-control | Any drug use disorder | Non–drug use | 5,865 | 18–54 | 18–54 | 1990–1992 | N/A | Violent behavior | Self-report | Yes |
| Payer, 2011 (58) | US | Participants diagnosed with methamphetamine dependence | DSM-IV | Case-control | Methamphetmine dependence | Healthy controls without drug use disorder | 44 | 32.8 ± 8.8 | Female | Not stated | N/A | Aggression | Self-report | Yes |
| Christoffersen, 2003 (69) | Denmark | The 1966 birth cohort in Denmark | ICD-8b | Cohort | Drug addicts | Non–drug addicts | 43,403 | 15–47 | Male | 1993 | 13 | Violent crimes | Official records | No |
| Feingold, 2008 (59) | US | The Couple Study associated with the Oregon Youth Study | DSM-IV | Cohort | Cannabis, hallucinogen, cocaine, opiates, amphetamines, sedatives | Non–cannabis, hallucinogen, cocaine, opiates, amphetamines, sedatives | 150 | 19–28 | Male | Not stated | 9 | Intimate partner violence | Self-report, other’s report, interview ratings | Yes |
| Van Dorn, 2012 (60) | US | National Epidemiologic Survey on Alcohol and Related Conditions | DSM-IV | Cohort | Drug use disorder | Non–drug use disorder | 36,019 | ≥18 | Mixed | 2005 | 3 | Any violence | Self-report | Yes |
| Smith, 2014 (61) | US | National Epidemiologic Survey on Alcohol and Related Conditions | DSM-IV | Cohort | Cocaine, cannabis, opioid use disorder | Non–cocaine use disorder, non–opioid use disorder | 25,633 | Mean, 46.4 | Mixed | 2005 | 3 | Intimate partner violence | Self-report | Yes |
| Feingold, 2014 (62) | US | The Couple Study associated with the Oregon Youth Study | DSM-IV-TR | Cohort | Cannabis, hallucinogen, cocaine, opiates, amphetamines, sedatives | Non–cannabis, hallucinogen, cocaine, opiates, amphetamines, sedtives | 146 | Mean, 35 | Female | Not stated | 10 | Intimate partner violence | Others’ report | Yes |
| Have, 2014 (70) | Netherlands | A cohort study of the Dutch general population | DSM-IV | Cohort | Drug dependence | Non–drug dependence | 5,303 | 18–64 | Mixed | 2012 | 3 | Physical violence | Self-report | Yes |
| McCauley, 2015 (63) | US | The National Comorbidity Survey Replication | WHO-CIDIc | Case-control | Drug abuse | Non–drug abuse | 5,692 | 21–99 | Mixed | 2003 | N/A | Physical dating violence | Self-report | Yes |
| Harford, 2016 (53) | US | National Survey on Drug Use and Health | DSM-IV | Case-control | Drug use disorder | Non–drug use disorder | 108,560 | 12–17 | Mixed | 2008–2013 | N/A | Other-directed violence | Self-report | Yes |
| White, 2015 (64) | US | A cohort of the Pittsburgh Youth Study | DSM-IV | Cohort | Cannabis use disorder, hard drug use disorder | No substance use disorder | 240 | 35.8 ± 0.8 | Male | 2010 | 10 | Persist in violence | Self-reports and official charges | Yes |
| Trauffer, 2017 (65) | US | A cohort study in which children were followed into adulthood | DSM-III-R | Cohort | Drug abuse and, or dependence | Non–drug abuse/dependence | 413 | 29.6± 3.9 | Female | 2014 | 28 | Violent offender | Official records | Yes |
| Harford, 2018 (54) | US | National Survey on Drug Use and Health | DSM-IV | Case-control | Any drug use disorder | Non–drug use | 314,881 | ≥18 | Mixed | 2008–2015 | N/A | Other-directed violence | Self-report | Yes |
| Harford, 2018 (67) | US | The National Epidemiologic Survey on Alcohol Related Conditions-III | DSM-V | Case-control | Cannabis, opioid, other drug use disorder | Non–drug use | 36,309 | ≥18 | Mixed | 2012–2013 | N/A | Other-directed violence | Self-report | Yes |
| Altintas, 2019 (71) | Turkey | Outpatients | DSM-IV | Case-control | Synthetic cannabinoid use disorders | Healthy volunteers without substance use disorders | 130 | 28.2 ± 7.6 | Mixed | Not stated | N/A | Aggression | Self-report | No |
Abbreviations: DSM, Diagnostic and Statistical Manual of Mental Disorders; ICD, International Classification of Diseases; N/A, not available; WHO-CIDI; World Health Organization’s Composite International Diagnostic Interview.
a Non–drug, non–drug use disorder, and non–drug addicts served as a control group and they refer to people who might have used drugs before but did not meet diagnostic criteria for any drug use disorders. “Healthy volunteers without substance use disorders” refers to healthy volunteers without drug or alcohol use disorders.
In 16 investigations, diagnosis was made using the Diagnostic and Statistical Manual of Mental Disorders (version 3 onward). One study adopted the International Classification of Diseases, Eighth Revision (69), and 1 provided both International Classification of Diseases, Tenth Revision, and Diagnostic and Statistical Manual of Mental Disorders–IV diagnoses (63).
For outcome measurement, 2 studies used violent conviction from official records (65, 69) and 1 reported intimate partner violence from the partner’s report (62). Most used self-report items in the Diagnostic Interview Schedule (56), PPC Delinquency and Criminal Behavior inventory (57), Aggression Questionnaire (58), Conflict Tactics Scale (63), physical aggression subscale in Buss-Perry Scale (71), and specially developed questionnaires (53, 54, 60, 61, 66, 67, 70). A combination of several measures (e.g., official records and self-report) was applied in 3 studies (59, 64, 68).
Any drug or polydrug use disorder
We identified 6 cohort investigations (57, 60, 64, 65, 69, 70) and 6 case-control reports (53, 54, 56, 63, 66, 67) that examined the risk of violence in any or polydrug use disorder. The odds ratios ranged from 1.3 (95% confidence interval (CI): 0.1, 13.0) to 25.0 (95% CI: 16.1–39.0) (Figure 2). When excluding the 2 studies that were published prior to 2000, the odds ratio was 4.1 (95% CI: 3.0, 5.7).
Figure 2.
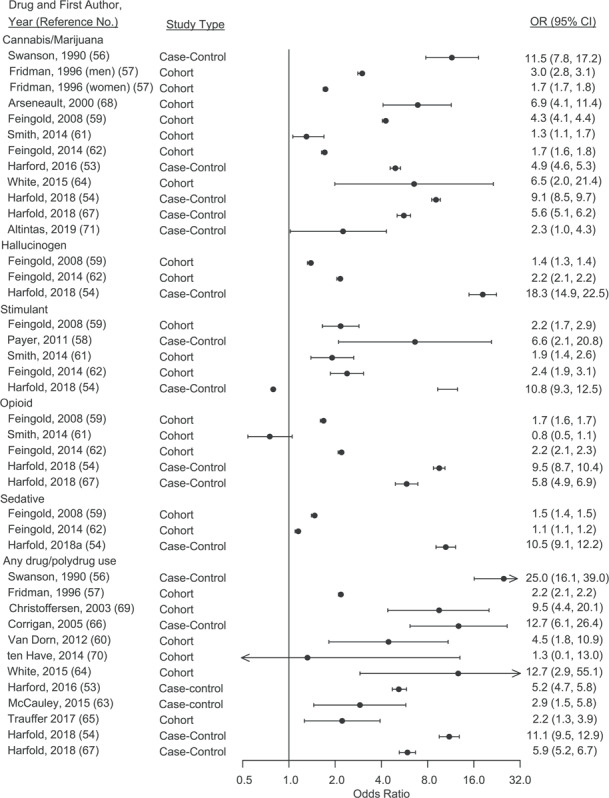
Odds ratios (ORs) and confidence interval (CIs) for the association between drug use disorders and violent outcome. Weights are from random effects analysis.
Cannabis/marijuana use disorder
Six cohort studies (57, 59, 61, 62, 64, 68) and 5 case-control investigations (53, 54, 56, 67, 71) examined the link between cannabis/marijuana use disorder and violence. The odds ratios ranged from 1.3 (95% CI: 1.1, 1.7) to 11.5 (95% CI: 7.8, 17.2). When excluding studies prior to 2000, the odds ratios ranged from 1.3 (95% CI: 1.1, 1.7) to 9.1 (95% CI: 8.5, 9.7). (See Figure 2).
Hallucinogen use disorder
Two cohort investigations (59, 62) and 1 case-control report (54) tested the association between hallucinogen use disorder and violence. The odds ratios varied from 1.4 (95% CI: 1.3, 1.4) to 18.3 (95% CI: 14.9, 22.5). (See Figure 2).
Stimulant use disorder
We identified 5 studies that reported risk estimates for violence in stimulant use disorder, with 3 studies (59, 61, 62) using a cohort study design and 2 (54, 58) using a case-control study design. All of these studies were conducted in the United States. The odds ratios ranged from 1.9 (95% CI: 1.4, 2.6) to 10.8 (95% CI: 9.3, 12.5). (See Figure 2).
Opioid use disorder
Three cohort investigations (59, 61, 62) and 2 case-control studies (54, 67) reported the risk of violence in opioid use disorder, all of which were conducted in the United States. The risk estimates ranged from an odds ratio of 0.8 (95% CI: 0.5, 1.1) to 9.5 (95% CI: 8.7, 10.4). (See Figure 2).
Sedative use disorder
Two cohort investigations (59, 62) and 1 case-control study (54) examined the association between sedative use disorder and violence. Odds ratios varied from 1.1 (95% CI: 1.1, 1.2) to 10.5 (95% CI: 9.1, 12.2). (See Figure 2).
Heterogeneity
No significant differences were found in risk estimates by sex, country, outcome measures, years of follow-up, and sample size in subgroup analyses (Table 2). The risk estimates in cohort investigations (odds ratio (OR) = 2.7, 95% CI: 2.1, 3.5) were lower than in the case-control reports (OR = 6.6, 95% CI: 5.1, 8.6). No differences were found among violence by self-report (OR = 4.6, 95% CI: 3.0, 7.2), informant report/official records (OR = 3.2, 95% CI: 1.3, 7.8), and combined measures (OR = 4.4, 95% CI: 1.3, 14.5).
Table 2.
Risk Estimates for Violence in Drug Use Disorders According to Sample or Study Characteristics, Multiple Countries, 1990–2019
| Source of Heterogeneity | No. of Studies | No. in Population | OR | 95% CI |
|---|---|---|---|---|
| Sex | ||||
| Male | 4 | 43,976 | 3.9 | 1.7, 8.9 |
| Female | 4 | 800 | 2.2 | 1.8, 2.7 |
| Mixed | 11 | 546,635 | 5.4 | 4.1, 7.0 |
| Study location | ||||
| United States | 14 | 542,393 | 4.2 | 2.9, 6.1 |
| Other high-income counties | 3 | 48,888 | 7.1 | 4.1, 12.2 |
| US study locations | ||||
| National | 8 | 533,339 | 4.4 | 2.9, 6.1 |
| Region-based | 6 | 9,054 | 3.9 | 2.0, 7.6 |
| Measures of outcome | ||||
| Self-reported outcome | 12 | 546,877 | 4.6 | 3.0, 7.2 |
| Others’ report/official records | 3 | 43,962 | 3.2 | 1.3, 7.8 |
| Combined measures | 3 | 572 | 4.4 | 1.3, 14.5 |
| Temporality in cohort studies | ||||
| Drug prior to violence | 4 | 85,105 | 3.8 | 1.6, 9.1 |
| Others | 6 | 26,764 | 2.6 | 1.6, 4.3 |
| Study design | ||||
| Cohort study | 10 | 111,869 | 2.7 | 2.1, 3.5 |
| Case-control study | 8 | 473,850 | 6.6 | 5.1, 8.6 |
| Years of follow-up | ||||
| <9.5 years | 5 | 67485 | 1.9 | 1.5, 2.4 |
| ≥9.5 years | 5 | 44384 | 4.5 | 2.2, 9.1 |
| sample size | ||||
| <500 | 8 | 1503 | 2.6 | 2.0, 3.4 |
| ≥500 | 8 | 166285 | 5.1 | 2.9, 9.2 |
| Violent outcome | ||||
| Intimate partner violence | 4 | 31,621 | 1.7 | 1.4, 2.1 |
| Intimate partner violence with general controls | 2 | 31,325 | 1.8 | 0.8, 4.2 |
| General violence | 14 | 559,790 | 5.7 | 3.8, 8.6 |
| Clinical criteria | ||||
| DSM-III (Revision) | 5 | 14,901 | 5.7 | 2.5, 13.0 |
| DSM-IV (Text Revision) | 10 | 491,106 | 3.4 | 2.0, 6.0 |
Abbreviations: CI, confidence interval; DSM, Diagnostic and Statistical Manual of Mental Disorders; OR, odds ratio.
The odds ratios for intimate partner violence (OR = 1.7, 95% CI: 1.4, 2.1) were lower than for general violence (OR = 5.7, 95% CI: 3.8, 8.6) (Table 2). When further exploring the associations of the comparison groups in studies of the association between drug use disorders and intimate partner violence, no significant differences were found. In the meta-regression analysis, we found that study design (cohort vs. case–control study) was associated with heterogeneity ( = 0.8, t = 2.3, P = 0.04), as was the violent outcome (intimate partner violence vs. general violence;
= 0.8, t = 2.3, P = 0.04), as was the violent outcome (intimate partner violence vs. general violence;  = −1.2, t = −3.3, P = 0.004). No other variables examined explained the heterogeneity between studies. Egger’s test did not suggest publication bias (t = 1.32, P = 0.20).
= −1.2, t = −3.3, P = 0.004). No other variables examined explained the heterogeneity between studies. Egger’s test did not suggest publication bias (t = 1.32, P = 0.20).
DISCUSSION
Main findings
This systematic review examined the association between drug use disorders and violence. We identified 18 eligible studies from 5 countries, with 591,411 individuals meeting diagnostic criteria for drug use disorders. There were 2 main findings. First, we found that individuals with a diagnosed drug use disorder have a 4- to 10-fold higher risk of perpetrating violence compared with general population or individuals without the drug use disorder being studied. All of the examined categories of drug use disorders—including cannabis, hallucinogens, stimulants, opioids, and sedatives—were associated with elevated violence risks. Of the total of 37 included studies, we found increased risk of violence in 34 studies with confidence intervals that did not cross 1. To examine the population impact, the odds of violence perpetration need to be seen in the context of general population prevalence of these disorders—which varies from 52 cases (per 100,000) of hallucinogen use disorders to 353 cases (per 100,000) of opioid use disorders (12). Second, there was substantial heterogeneity between studies, which was partially explained by study design and the type of outcome. Violence risk in drug use disorders was lower in cohort than in case-control studies, and when intimate partner violence was the outcome rather than general violence.
Implications
Although the odds of increased risk of violence in drug use disorders are not dissimilar to those in other neuropsychiatric conditions (72), their importance is greater from a public health perspective as drug use disorders are more prevalent than severe mental illnesses, such as schizophrenia or bipolar disorder. In addition, although drug use disorders are not more prevalent than disorders such as depression and anxiety, their risk of violence is usually higher (67, 73). Therefore, drug use disorders have greater population impact when taking into account both prevalence and relative risk. This underscores the importance of treating drug use disorders as part of any public health approach to violence prevention. Notably, long-term methadone maintenance programs and behavioral treatments can reduce crime (74). In addition, there are studies that demonstrate reduced crime after drug treatment (e.g., opioid maintenance treatment, methadone, buprenorphine, and naltrexone) and nonmedical treatment (e.g., therapeutic communities, drug courts), among individuals using cocaine (75) and opioids (76–79), as well as with general drug use disorders (80–83). Moreover, prison-based interventions—such as therapeutic communities, opiate maintenance treatment, and pharmacotherapies for drug use disorders—are effective in reducing recidivism in prisoners (84–86). Despite this, most individuals with drug use disorders do not receive treatment. In the United States, among individuals with 12-month and lifetime drug use disorders, only 14% and 25% received treatment, respectively (87). Thus, more efforts should be made to improve accessibility of treatment for individuals with drug use disorders. Together, the treatability of drug use disorders, unmet needs, and risk of adverse outcomes present an opportunity to improve public health and safety.
A second implication, regarding study design, is that 2 aspects of design explained some of the between-study heterogeneity. Cohort studies had lower risk estimates than case-control investigations. This difference is likely because cohort studies are more likely to take into account the temporal sequence between drug use disorders and violent outcome. This allowed for a more accurate estimation of the associations than case-control studies. Future observational research should prioritize cohort designs to longitudinally follow individuals with drug use disorders and examine their violent outcomes. We also found that the association with intimate partner violence was less strong than with general violence. This might be because individuals with drug use disorders are less likely to have partners (87, 88) and those who have partners might present with less severe symptoms of drug use disorders (89).
Strengths, limitations, and future directions
This review has several strengths. First, we included only studies that used validated diagnostic criteria to identify drug use disorders and excluded studies using self-report or other measures that might reflect short-term or recreational use. Second, we carefully explored heterogeneity using 2 methods (subgroup analyses and meta-regression). Third, we excluded studies examining drug use disorders and violent outcomes in selected samples such as offenders, cohorts with mental disorders, and individuals under treatment for drug use disorders, because not all individuals with drug use disorders are offenders or have other mental disorders, and the majority will not be subject to treatment. This likely increases the generalizability of our findings.
However, a number of limitations should be noted. First, all but one of the studies we included were conducted in high-income countries. We found an investigation from a middle-income country—Turkey—but no others, and none in Central Latin America, Tropical Latin America, and Southern sub-Saharan Africa, where violence is among the top 10 leading causes of disability-adjusted life-years (90). Many countries in these regions account for the majority of global drug manufacture, trafficking, and consumption (91, 92). Therefore, more research on the link in these settings is needed. A second limitation was that the amount of information on individual categories was not sufficient to draw definite conclusions about differences by drug class. We identified 3 studies (54, 59, 62) of sedative use disorder and 5 each for stimulant use disorder (54, 58, 59, 61, 62) and opioid use disorder (54, 59, 61, 62, 67). Furthermore, we found a limited literature on polydrug use, although it is common and linked to poorer treatment outcomes, social maladjustment, and overdose lethality (93–95). Future studies should investigate more carefully the different categories of drug use disorders, polydrug use, and links with novel psychoactive substances. Third, it is not possible to meta-analyze studies of selected populations because the effects of mediators cannot be modeled. Therefore, our findings are not necessarily risk estimates in specific subpopulations, such as prisoners or individuals who are participating in treatment programs. For example, our estimates might be overestimates given that we excluded studies of individuals under drug treatment, which could decrease risk of violence (96, 97). Fourth, we found links between hallucinogen use and violence in the general population, but there appears to be heterogeneity in their associations by population. For example, in criminal justice populations, recent work has found decreased associations between hallucinogen use and repeated offending in substance-involved offenders under community corrections supervision (48), which is also reported among intimate partner violence perpetrators (47, 98). Among individuals with schizophrenia, there is an increased risk (99). Finally, due to lack of data, we identified only a few factors that might explain heterogeneity between studies. For example, we were not able to examine whether some factors moderate the link between drug use disorders and violence, such as being subjected to violence, comorbidity of other substance use disorders (including alcohol) and mental health conditions, time between onset of drug use and violent outcome, and other social determinants (including poverty and access to services). In addition, the heterogeneity analyses were based on different drug categories and limited by variations in primary study settings. The results should therefore be interpreted with caution and read in the context of implications for future research rather than clinical practice.
Moreover, some factors could be associated with, could mediate, or could modify links between drug misuse and violence. For instance, an umbrella review of 22 meta-analyses based on over 120,000 individuals has shown that a range of neuropsychiatric disorders—including schizophrenia, personality disorders, and bipolar disorders—and perpetration, being a witness, or being a victim of violence during childhood are linked to increased risk of violence (72), suggesting that all of these comorbidities can be confounders. In addition, individuals who are victims of violence might use drugs as a coping mechanism, and victimization itself might in turn lead to later violence (35–39). Therefore, more research accounting for these factors is necessary.
Conclusions
This systematic review has synthesized evidence on associations between individual categories of drug use disorder and violent outcomes. The findings suggest that all categories of drug use disorder have an elevated risk of violence, and that study design and type of violent outcome partly explain variation in risk estimates between studies.
ACKNOWLEDGMENTS
Author affiliations: Department of Psychiatry, National Clinical Research Center for Mental Disorders, Second Xiangya Hospital of Central South University, Changsha, China (Shaoling Zhong); and Department of Psychiatry, University of Oxford, Oxford, United Kingdom (Rongqin Yu, Seena Fazel).
This work was funded by the China Scholarship Council (grant 201806370093 to S.Z) and the Wellcome Trust Senior Research Fellowship (grant 202836/Z/16/Z to S.F.).
Conflict of interest: none declared.
REFERENCES
- 1. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Degenhardt L, Whiteford HA, Ferrari AJ, et al. Global burden of disease attributable to illicit drug use and dependence: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382(9904):1564–1574. [DOI] [PubMed] [Google Scholar]
- 3. McGinty EE, Choksy S, Wintemute GJ. The relationship between controlled substances and violence. Epidemiol Rev. 2016;38(1):5–31. [DOI] [PubMed] [Google Scholar]
- 4. Degenhardt L, Hall W. Extent of illicit drug use and dependence, and their contribution to the global burden of disease. Lancet. 2012;379(9810):55–70. [DOI] [PubMed] [Google Scholar]
- 5. Nutt DJ, King LA, Phillips LD. Drug harms in the UK: a multicriteria decision analysis. Lancet. 2010;376(9752):1558–1565. [DOI] [PubMed] [Google Scholar]
- 6. Grann M, Fazel S. Substance misuse and violent crime: Swedish population study. BMJ. 2004;328(7450):1233–1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hoaken PN, Stewart SH. Drugs of abuse and the elicitation of human aggressive behavior. Addict Behav. 2003;28(9):1533–1554. [DOI] [PubMed] [Google Scholar]
- 8. Atkinson A, Anderson Z, Hughes K, et al. Interpersonal Violence and Illicit Drugs. Liverpool, UK: Centre for Public Health, Liverpool John Moores University; 2009. [Google Scholar]
- 9. Duke AA, Smith KM, Oberleitner L, et al. Alcohol, drugs, and violence: a meta-meta-analysis. Psychol Violence. 2018;8(2):238. [Google Scholar]
- 10. Fazel S, Yoon P, Haye AJ. Substance use disorders in prisoners: an updated systematic review and meta-regression analysis in recently incarcerated men and women. Addiction. 2017;112(10):1725–1739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ritchie H, Roser M. Substance Use. Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2017 (GBD 2017) Results. Seattle, WA: Institute for Health Metrics and Evaluation; http://ghdx.healthdata.org/gbd-results-tool. Accessed September 8, 2019. [Google Scholar]
- 12. Degenhardt L, Charlson F, Ferrari A, et al. The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Psychiatry. 2018;5(12):987–1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pedersen W, Skardhamar T. Cannabis and crime: findings from a longitudinal study. Addiction. 2010;105(1):109–118. [DOI] [PubMed] [Google Scholar]
- 14. Huas C, Hassler C, Choquet M. Has occasional cannabis use among adolescents also to be considered as a risk marker? Eur J Public Health. 2008;18(6):626–629. [DOI] [PubMed] [Google Scholar]
- 15. Schoeler T, Theobald D, Pingault JB, et al. Continuity of cannabis use and violent offending over the life course. Psychol Med. 2016;46(8):1663–1677. [DOI] [PubMed] [Google Scholar]
- 16. Swartout KM, White JW. The relationship between drug use and sexual aggression in men across time. J Interpers Violence. 2010;25(9):1716–1735. [DOI] [PubMed] [Google Scholar]
- 17. Green KM, Doherty EE, Stuart EA, et al. Does heavy adolescent marijuana use lead to criminal involvement in adulthood? Evidence from a multiwave longitudinal study of urban African Americans. Drug Alcohol Depend. 2010;112(1–2):117–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Farabee D, Joshi V, Anglin MD. Addiction careers and criminal specialization. Crime Delinquency. 2001;47(2):196–220. [Google Scholar]
- 19. Narvaez JC, Jansen K, Pinheiro RT, et al. Violent and sexual behaviors and lifetime use of crack cocaine: a population-based study in Brazil. Soc Psychiatry Psychiatr Epidemiol. 2014;49(8):1249–1255. [DOI] [PubMed] [Google Scholar]
- 20. El-Bassel N, Gilbert L, Wu E, et al. Perpetration of intimate partner violence among men in methadone treatment programs in New York City. Am J Public Health. 2007;97(7):1230–1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chermack ST, Grogan-Kaylor A, Perron BE, et al. Violence among men and women in substance use disorder treatment: a multi-level event-based analysis. Drug Alcohol Depend. 2010;112(3):194–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Moore TM, Stuart GL, Meehan JC, et al. Drug abuse and aggression between intimate partners: a meta-analytic review. Clin Psychol Rev. 2008;28(2):247–274. [DOI] [PubMed] [Google Scholar]
- 23. Bennett T, Holloway K, Farrington D. The statistical association between drug misuse and crime: a meta-analysis. Aggress Violent Behav. 2008;13(2):107–118. [Google Scholar]
- 24. Boles SM, Miotto K. Substance abuse and violence: a review of the literature. Aggress Violent Behav. 2003;8(2):155–174. [Google Scholar]
- 25. Collins RE The effect of gender on violent and nonviolent recidivism: a meta-analysis. J Crim Just. 2010;38(4):675–684. [Google Scholar]
- 26. Fazel S, Långström N, Hjern A, et al. Schizophrenia, substance abuse, and violent crime. JAMA. 2009;301(19):2016–2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Fazel S, Lichtenstein P, Grann M, et al. Bipolar disorder and violent crime: new evidence from population-based longitudinal studies and systematic review. Arch Gen Psychiatry. 2010;67(9):931–938. [DOI] [PubMed] [Google Scholar]
- 28. Yu R, Geddes JR, Fazel S. Personality disorders, violence, and antisocial behavior: a systematic review and meta-regression analysis. J Pers Disord. 2012;26(5):775–792. [DOI] [PubMed] [Google Scholar]
- 29. Large MM, Nielssen O. Violence in first-episode psychosis: a systematic review and meta-analysis. Schizophr Res. 2011;125(2–3):209–220. [DOI] [PubMed] [Google Scholar]
- 30. Stith SM, Smith DB, Penn CE, et al. Intimate partner physical abuse perpetration and victimization risk factors: a meta-analytic review. Aggress Violent Behav. 2004;10(1):65–98. [Google Scholar]
- 31. Clark CB, Zyambo CM, Li Y, et al. The impact of non-concordant self-report of substance use in clinical trials research. Addict Behav. 2016;58:74–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Denis CM, Gelernter J, Hart AB, et al. Inter-observer reliability of DSM-5 substance use disorders. Drug Alcohol Depend 2015;153:229–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hasin DS, O’Brien CP, Auriacombe M, et al. DSM-5 criteria for substance use disorders: recommendations and rationale. Am J Psychiatry. 2013;170(8):834–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bushman BJ Human aggression while under the influence of alcohol and other drugs: an integrative research review. Curr Dir Psychol Sci. 1993;2(5):148–151. [Google Scholar]
- 35. Afifi TO, Henriksen CA, Asmundson GJ, et al. Childhood maltreatment and substance use disorders among men and women in a nationally representative sample. Can J Psychiatry. 2012;57(11):677–686. [DOI] [PubMed] [Google Scholar]
- 36. Asberg K, Renk K. Substance use coping as a mediator of the relationship between trauma symptoms and substance use consequences among incarcerated females with childhood sexual abuse histories. Subst Use Misuse. 2012;47(7):799–808. [DOI] [PubMed] [Google Scholar]
- 37. Duke NN, Pettingell SL, McMorris BJ, et al. Adolescent violence perpetration: associations with multiple types of adverse childhood experiences. Pediatrics. 2010;125(4):e778–e786. [DOI] [PubMed] [Google Scholar]
- 38. Dardis CM, Dixon KJ, Edwards KM, et al. An examination of the factors related to dating violence perpetration among young men and women and associated theoretical explanations: a review of the literature. Trauma, Violence, and Abuse. 2015;16(2):136–152. [DOI] [PubMed] [Google Scholar]
- 39. Park S, Kim S-H. Who are the victims and who are the perpetrators in dating violence? Sharing the role of victim and perpetrator. Trauma, Violence, and Abuse. 2019;20(5):732–741. [DOI] [PubMed] [Google Scholar]
- 40. Funk M, Drew N, Knapp M. Mental health, poverty and development. J Public Ment Health. 2012;11(4):166–185. [Google Scholar]
- 41. Hall W, Degenhardt L. Adverse health effects of non-medical cannabis use. Lancet. 2009;374(9698):1383–1391. [DOI] [PubMed] [Google Scholar]
- 42. Degenhardt L, Glantz M, Evans-Lacko S, et al. Estimating treatment coverage for people with substance use disorders: an analysis of data from the World Mental Health Surveys. World Psychiatry. 2017;16(3):299–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Krupski A, Graves MC, Bumgardner K, et al. Comparison of homeless and non-homeless problem drug users recruited from primary care safety-net clinics. J Subst Abuse Treat. 2015;58:84–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Goldstein PJ The drugs/violence nexus: a tripartite conceptual framework. J Drug Issues. 1985;15(4):493–506. [Google Scholar]
- 45. Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2000;283(15):2008–2012. [DOI] [PubMed] [Google Scholar]
- 46. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Thiessen MS, Walsh Z, Bird BM, et al. Psychedelic use and intimate partner violence: the role of emotion regulation. J Psychopharmacol. 2018;32(7):749–755. [DOI] [PubMed] [Google Scholar]
- 48. Hendricks PS, Clark CB, Johnson MW, et al. Hallucinogen use predicts reduced recidivism among substance-involved offenders under community corrections supervision. J Psychopharmacol. 2014;28(1):62–66. [DOI] [PubMed] [Google Scholar]
- 49. Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Ottawa, Canada: Ottawa Hospital Research Institute; 2011. [Google Scholar]
- 50. Higgins J, Altman D, Sterne J. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.0. Chichester, UK: The Cochrane Collaboration; 2011. [Google Scholar]
- 51. Borenstein M, Hedges LV, Higgins JP, et al. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1(2):97–111. [DOI] [PubMed] [Google Scholar]
- 52. Borenstein M, Hedges LV, Higgins JP, et al. Introduction to Meta-Analysis. West Sussex, UK: John Wiley & Sons; 2009. [Google Scholar]
- 53. Harford TC, Chen CM, Grant BF. Other-and self-directed forms of violence and their relationship with number of substance use disorder criteria among youth ages 12–17: results from the National Survey on Drug Use and Health. J Stud Alcohol Drugs. 2016;77(2):277–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Harford TC, H-Y Y, Chen CM, et al. Substance use disorders and self-and other-directed violence among adults: results from the National Survey on Drug Use and Health. J Affect Disord. 2018;225:365–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Egger M, Smith GD, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Swanson JW, Holzer CE III, Ganju VK, et al. Violence and psychiatric disorder in the community: evidence from the Epidemiologic Catchment Area surveys. Psychiatr Serv. 1990;41(7):761–770. [DOI] [PubMed] [Google Scholar]
- 57. Friedman AS, Kramer S, Kreisher C, et al. The relationships of substance abuse to illegal and violent behavior, in a community sample of young adult African American men and women (gender differences). J Subst Abuse. 1996;8(4):379–402. [DOI] [PubMed] [Google Scholar]
- 58. Payer DE, Lieberman MD, London ED. Neural correlates of affect processing and aggression in methamphetamine dependence. Arch Gen Psychiatry. 2011;68(3):271–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Feingold A, Kerr DC, Capaldi DM. Associations of substance use problems with intimate partner violence for at-risk men in long-term relationships. J Fam Psychol. 2008;22(3):429–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Van Dorn R, Volavka J, Johnson N. Mental disorder and violence: is there a relationship beyond substance use? Soc Psychiatry Psychiatr Epidemiol. 2012;47(3):487–503. [DOI] [PubMed] [Google Scholar]
- 61. Smith PH Intimate Partner Violence Among Adults: the Role of Illicit Drug Use [thesis] Buffalo, NY: State University of New York; 2014. [Google Scholar]
- 62. Feingold A, Capaldi DM. Associations of women's substance dependency symptoms with intimate partner violence. Partn Abus. 2014;5(2):152–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. McCauley HL, Breslau JA, Saito N, et al. Psychiatric disorders prior to dating initiation and physical dating violence before age 21: findings from the National Comorbidity Survey Replication (NCS-R). Soc Psychiatry Psychiatr Epidemiol. 2015;50(9):1357–1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. White HR, Buckman J, Pardini D, et al. The association of alcohol and drug use with persistence of violent offending in young adulthood. J Dev Life Course Criminol. 2015;1(3):289–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Trauffer N, Widom CS. Child abuse and neglect, and psychiatric disorders in nonviolent and violent female offenders. Violence Gend. 2017;4(4):137–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Corrigan PW, Watson AC. Findings from the National Comorbidity Survey on the frequency of violent behavior in individuals with psychiatric disorders. Psychiatry Res. 2005;136(2–3):153–162. [DOI] [PubMed] [Google Scholar]
- 67. Harford TC, Chen CM, Kerridge BT, et al. Self-and other-directed forms of violence and their relationship with lifetime DSM-5 psychiatric disorders: results from the National Epidemiologic Survey on Alcohol Related Conditions–III (NESARC-III). Psychiatry Res. 2018;262:384–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Arseneault L, Moffitt TE, Caspi A, et al. Mental disorders and violence in a total birth cohort: results from the Dunedin study. Arch Gen Psychiatry. 2000;57(10):979–986. [DOI] [PubMed] [Google Scholar]
- 69. Christoffersen MN, Francis B, Soothill K. An upbringing to violence? Identifying the likelihood of violent crime among the 1966 birth cohort in Denmark. J Forensic Psychiatry Psychol. 2003;14(2):367–381. [Google Scholar]
- 70. ten Have M, de Graaf R, van Weeghel J, et al. The association between common mental disorders and violence: to what extent is it influenced by prior victimization, negative life events and low levels of social support? Psychol Med. 2014;44(7):1485–1498. [DOI] [PubMed] [Google Scholar]
- 71. Altintas M, Inanc L, Hunca AN, et al. Theory of mind, aggression and impulsivity in patients with synthetic cannabinoid use disorders: a case-control study. Anadolu Psikiyatr De. 2019;20(1):5–12. [Google Scholar]
- 72. Fazel S, Smith EN, Chang Z, et al. Risk factors for interpersonal violence: an umbrella review of meta-analyses. Br J Psychiatry. 2018;213(4):609–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Pulay AJ, Dawson DA, Hasin DS, et al. Violent behavior and DSM-IV psychiatric disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008;69(1):12–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. McLellan AT, Lewis DC, O'Brien CP, et al. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284(13):1689–1695. [DOI] [PubMed] [Google Scholar]
- 75. Koehn JD, Bach P, Hayashi K, et al. Impact of incarceration on rates of methadone use in a community recruited cohort of injection drug users. Addict Behav. 2015;46:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Bukten A, Skurtveit S, Gossop M, et al. Engagement with opioid maintenance treatment and reductions in crime: a longitudinal national cohort study. Addiction. 2012;107(2):393–399. [DOI] [PubMed] [Google Scholar]
- 77. Vorma H, Sokero P, Aaltonen M, et al. Participation in opioid substitution treatment reduces the rate of criminal convictions: evidence from a community study. Addict Behav. 2013;38(7):2313–2316. [DOI] [PubMed] [Google Scholar]
- 78. Bahji A, Carlone D, Altomare J. Acceptability and efficacy of naltrexone for criminal justice-involved individuals with opioid use disorder: a systematic review and meta-analysis. Addiction. 2020;115(8):1413–1425. [DOI] [PubMed] [Google Scholar]
- 79. Maremmani I, Rolland B, Somaini L, et al. Buprenorphine dosing choices in specific populations: review of expert opinion. Expert Opin Pharmacother. 2016;17(13):1727–1731. [DOI] [PubMed] [Google Scholar]
- 80. Mitchell O, Wilson DB, MacKenzie DL. The effectiveness of incarceration-based drug treatment on criminal behavior: a systematic review. Campbell Syst Rev. 2012;8(1):i–76. [Google Scholar]
- 81. Perry A, Woodhouse R, Neilson M, et al. Are non-pharmacological interventions effective in reducing drug use and criminality? A systematic and meta-analytical review with an economic appraisal of these interventions.Int J Environ Res Public Health. 2016;13(10):966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Shaffer DK Looking inside the black box of drug courts: a meta-analytic review. Justice Quarterly. 2011;28(3):493–521. [Google Scholar]
- 83. Mitchell O, Wilson DB, Eggers A, et al. Drug courts' effects on criminal offending for juveniles and adults. Campbell Syst Rev. 2012;8(1):i–87. [Google Scholar]
- 84. de Andrade D, Ritchie J, Rowlands M, et al. Substance use and recidivism outcomes for prison-based drug and alcohol interventions. Epidemiol Rev. 2018;40(1):121–133. [DOI] [PubMed] [Google Scholar]
- 85. Mitchell O, Wilson DB, MacKenzie DL. Does incarceration-based drug treatment reduce recidivism? A meta-analytic synthesis of the research. J Exp Criminol. 2007;3(4):353–375. [Google Scholar]
- 86. Chang Z, Lichtenstein P, Långström N, et al. Association between prescription of major psychotropic medications and violent reoffending after prison release. JAMA. 2016;316(17):1798–1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Grant BF, Saha TD, Ruan WJ, et al. Epidemiology of DSM-5 drug use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions–III. JAMA. Psychiat. 2016;73(1):39–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Merline AC, Schulenberg JE, O'Malley PM, et al. Substance use in marital dyads: premarital assortment and change over time. J Stud Alcohol Drugs. 2008;69(3):352–361. [DOI] [PubMed] [Google Scholar]
- 89. Schulenberg JE, Patrick ME, Kloska DD, et al. Substance use disorder in early midlife: a national prospective study on health and well-being correlates and long-term predictors. Substance Abuse: Research and Treatment. 2015;9(suppl 1):41–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Kassebaum NJ, Arora M, Barber RM, et al. Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1603–1658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. UNODC World Drug Report 2018. Vienna, Austria: United Nations Publications; 2018. [Google Scholar]
- 92. Chalk P The Latin American Drug Trade: Scope, Dimensions, Impact, and Response. Santa Monica, CA: Rand Corporation; 2011. [Google Scholar]
- 93. Leri F, Bruneau J, Stewart J. Understanding polydrug use: review of heroin and cocaine co-use. Addiction. 2003;98(1):7–22. [DOI] [PubMed] [Google Scholar]
- 94. Jones JD, Mogali S, Comer SD. Polydrug abuse: a review of opioid and benzodiazepine combination use. Drug Alcohol Depend. 2012;125(1–2):8–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Connor JP, Gullo MJ, White A, et al. Polysubstance use: diagnostic challenges, patterns of use and health. Curr Opin Psychiatry. 2014;27(4):269–275. [DOI] [PubMed] [Google Scholar]
- 96. van der Pol TM, Henderson CE, Hendriks V, et al. Multidimensional family therapy reduces self-reported criminality among adolescents with a cannabis use disorder. Int J Offender Ther Comp Criminol. 2018;62(6):1573–1588. [DOI] [PubMed] [Google Scholar]
- 97. Ward CL, Mertens JR, Bresick GF, et al. Screening and brief intervention for substance misuse: does it reduce aggression and HIV-related risk behaviours? Alcohol Alcohol. 2015;50(3):302–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Walsh Z, Hendricks PS, Smith S, et al. Hallucinogen use and intimate partner violence: prospective evidence consistent with protective effects among men with histories of problematic substance use. J Psychopharmacol. 2016;30(7):601–607. [DOI] [PubMed] [Google Scholar]
- 99. Lamsma J, Cahn W, Fazel S. Use of illicit substances and violent behaviour in psychotic disorders: two nationwide case-control studies and meta-analyses. Psychol Med. 2020;50(12):2028–2033. [DOI] [PMC free article] [PubMed] [Google Scholar]