Abstract
COVID-19 pandemic is mainly related with the pulmonary problems initially but now as the pandemic is growing it is observed that almost all organ systems of the body are affected. Up to 20-30% patients who are admitted in Covid hospitals are showing cardiovascular involvement. Severity of cardiovascular disease in a COVID-19 patient depends whether a patient is having pre-existing cardiac disease or not. Patients with pre-existing cardiac disease have more severe infection and associated mortality. Severe COVID-19 infection shows close association with myocardial damage and various arrythmias. The cardiovascular involvement occurs by either engagement directly with the angiotensin converting enzyme 2 or indirectly by the effect of inflammatory mediators which are generated as a result of viral-host response to infection. The COVID-19 disease is said to produce a wide spectrum of affliction ranging between even asymptomatic patient to Cardiovascular syndrome. Even after recovering from COVID-19 patients can reappear in the hospital with cardiomyopathies and arrythmias.
Keywords: Arrythmia, cardiac, Cardiac Injury, COVID-19, myocarditis, myocardium, SARS -COV 2
Introduction
COVID-19 disease has engulfed almost all the countries in the world and the three major countries that are worst affected are USA, Brazil, and now India. The disease was first reported from Wuhan, China in late December 2019 and said to be caused by severe acute respiratory syndrome corona virus 2 (SARS-CoV2), a member of the genus Beta corona virus. The two other Corona viruses that have caused pandemics earlier were severe acute respiratory syndrome Corona virus (SARS-CoV) and Middle East respiratory syndrome Corona virus (MERS-CoV), these viruses along with SARS-CoV-2 cause respiratory infection leading to viral pneumonia and acute distress syndrome in few patients. Along with the respiratory ailments the SARS-CoV-2 infection also causes abnormal production and release of various pro-inflammatory cytokines and chemokines by the immune system resulting in various types of organ damage apart from the lungs which are being most commonly affected. There is abnormal and unregulated release of inflammatory mediators due to host response to viral infection is said to be known as cytokine storm.
This SARS COV-2 virus directly engages the ACE 2 receptors which are present in various organ systems. ACE2 expression is detected on type I and type II alveolar epithelium, upper respiratory system, heart, kidney tubular epithelium, pancreas, stomach, liver, ileum, endothelial cells, enterocytes, urinary bladder, and testis.[1] Since these ACE2 receptors are widely spread in the body, so not only pulmonary but the extra-pulmonary manifestations are present and associated with the presence of ACE2 receptors.[2] Table 1 shows various organ system involved along with their manifestation. SARS-CoV-2 may also cause various coagulation abnormalities as per severity of disease leading to myriad thromboembolic events. Up to 20–30% patients who are hospitalized with COVID-19 show cardiovascular involvement.
Table 1.
Showing various organ system involved in COVID-19 disease along with their manifestation
| Organ System | MEDIAN AGE (DAYS) |
|---|---|
| Neurologic | Headaches, Dizziness Encephalopathy, Ageusia, Myalgia Anosmia, Stroke, Cortical vein thrombosis |
| Hepatic | raised SGPT/SGOT, raised bilirubin |
| Gastrointestinal | Diarrhoea, Nausea/vomiting, Abdominal pain, Anorexia |
| Renal | Acute Kidney Injury, haematuria, Proteinuria |
| Cardiac | Takotsubo cardiomyopathy Myocardial injury/myocarditis Cardiac arrhythmias Cardiogenic shock Myocardial ischemia Acute cor pulmonale |
| Thromboembolism | DVT, Pulmonary thromboembolism and catheter related thrombosis |
| Endocrine | Hyper glycemia /Diabetic ketoacidosis /hyper glycaemic hyper osmolar state |
| Dermatological | Petechiae, Livedo reticularis, Erythematous rash |
A meta-analysis of 6 studies was done to study the prevalence of CVD in 1,527 patients of COVID-19 revealed the hypertension, cardiac and cerebrovascular disease, and diabetes to be 17.1%, 16.4%, and 9.7%, respectively.[3] Due to the virtue of production of inflammatory mediators and coagulation abnormalities the SARS-CoV2 can cause cardiovascular dysfunction in patients with COVID-19 which may be associated with high mortality. COVID-19 can cause cardiovascular disorders which may include myocardial injury, arrhythmias, acute coronary syndrome, and venous thromboembolism which are collectively known as Cardiovascular syndrome in COVID-19 shown in Figure 1.
Figure 1.

Spectrum of the acute coronavirus disease 2019 (COVID-19) can be seen as cardiovascular syndrome
There is considerable amount of overlap between cardiovascular symptoms and respiratory symptoms and typical presenting symptoms like fatigue, dyspnoeas, and cough are common in both. COVID-19 patient rarely present with palpitation and chest tightness.
The pattern of COVID-19 on patients can be in two forms in terms of cardiovascular involvement i.e., Patients with pre-existing cardiovascular disease and patients without any pre-existing cardiovascular disease however there is considerable imbricating in between these two. Broadly the primary cardiac involvement includes myocarditis, arrythmia, and Acute coronary Syndrome (ACS) and secondary cardiac involvement includes acute myocardial injury, heart failure along with the evidence of other end organ damage as well.
Interaction between SARS-COV2 with ACE2
Comorbidity like hypertension is very common in patients admitted in Covid setup with variable clinical presentation and often severe illness.[4,5] Renin angiotensin aldosterone system (RAAS) and its blockers have complex interaction in COVID-19 infection. ACE2 is basically an enzyme which degrades Angiotensin II to Angiotensin 1-7 and Angiotensin I to Angiotensin 1-9. SARS-CoV 2 enters cell by attaching to ACE2 with help of its spike protein and further by endocytosis into the cell. After this endocytosis the ACE2 undergoes downregulation so there is no degradation of accumulated Angiotensin II and its unopposed action.[6] This accumulated Angiotensin II is said to cause the acute Lung Injury, vasoconstriction, altered vascular permeability, and adverse myocardial remodeling.[7,8] The understanding of physiology of ACE2 and entry of virus into the host cell is very relevant. ACE2 is expressed in the lungs and also in myocardium, endothelial cells, kidney, and intestines.[9,10] Ongoing viral replication reduces the membrane ACE2 expression as seen in the vitro culture[11] and this causes the down regulation of ACE2 in lungs. There is a lot of controversy regarding use of Ace inhibitors and angiotensin receptor blockers in COVID-19 patients with pre-existing hypertension. The Interaction between SARS-CoV-2 and ACE-2 is shown in Figure 2.
Figure 2.
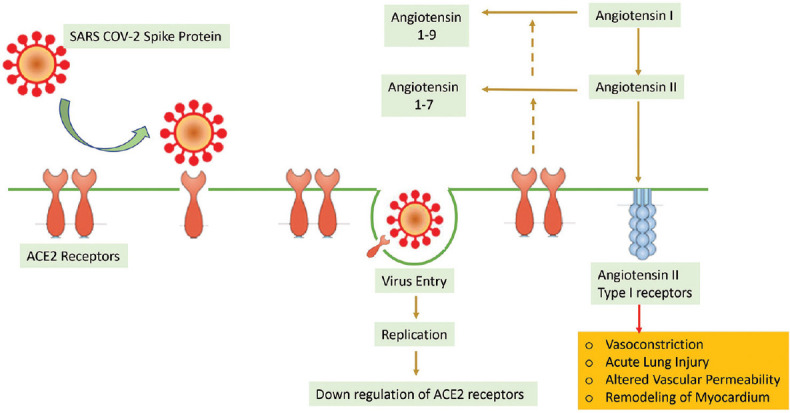
SARS COV-2 attaches to ACE2 receptor by spike protein and then it is interiorized by endocytosis and it undergo further replication, this causes downregulation of ACE2. ACE 2 plays important role in degradation of Angiotensin I and Angiotensin II into Angiotensin 1-9 and Angiotensin 1-7 respectively. The accumulated Angiotensin is responsible for vasoconstriction, Acute Lung Injury, altered vascular permeability, and myocardial remodeling associated with COVID-19 disease
Change of RAAS inhibitors to some other class of antihypertensive drug in any patient may require careful dose titration as well as monitoring of blood pressure to prevent undesired spikes of blood pressure. Small periods of blood pressure instability may also corelate with cardiovascular problems.[12,13,14] In fact, many Institutions around the globe are doing losartan trials for patients with COVID-19 patients who require hospitalization and also to evaluate the safety of losartan in respiratory failure due to COVID-19.
In COVID-19 patient's hypokalemia is a common finding in few studies which could be due to enhanced Kaliuresis in comparison to the gastrointestinal loss. This hypokalemia is said to be driven by RAAS activation and it corelates with the severity of disease and often difficult to manage.[15] In a way the ARBs (angiotensin receptor blockers) effect on potassium metabolism may be advantageous in COVID-19 patients. But various other studies however do not report hypokalemia in COVID-19 patients as a common finding.
The poor control of blood pressure contributes to immune dysregulation. In hypertensive patients it has been seen that there is CD8+T cell dysfunction and such immunosenescent CD8+T cell lacks in effective defense against viral infection, resulting in overproduction of cytokines.[16,17] The introduction of a new group of antihypertensive in previously hypertensive patient requires monitoring and switch over to different class of drug may often bring wide fluctuations in blood pressure.
So as of now the recommendation is that, those who are already on Ace inhibitors and angiotensin receptor blockers must continue the medication and those who are recently diagnosed with COVID-19 along with hypertension there blood pressure should be managed with other antihypertensive agents except RAAS antagonist.[18]
Patho physiology of heart disease in COVID-19
SARS COV-2 mainly interacts with ACE2 receptors in lungs; however, the virus interacts with almost all organs system and the effect of this virus infection on the myocardium could be direct as a result of the interaction of the virus with organ or via the immune system. Though the most common manifestation of COVID-19 is pneumonia; however, COVID-19 may also cause myocarditis, myocardial injury, arrhythmias, ACS, and thromboembolism.[19,20,21,22]
The pathophysiology of the cardiac disease is summarized in Figure 3. The Myocardial injury as per fourth universal definition of Myocardial infarction has been defined as elevation of cardiac troponin above the 99th percentile of upper reference limit (URL).[23] The myocardial injury during COVID-19 infection may occur due to either ischemic cause or non-ischemic cause and this may have varied clinical effects.[24] Acute myocardial Injury in COVID-19 is characterized by marked cardiac troponin elevation along with ECG changes and angiography revealing no coronary artery disease or culprit lesions. The myocardial injury has been independently associated with high mortality among COVID-19 patients.[25]
Figure 3.
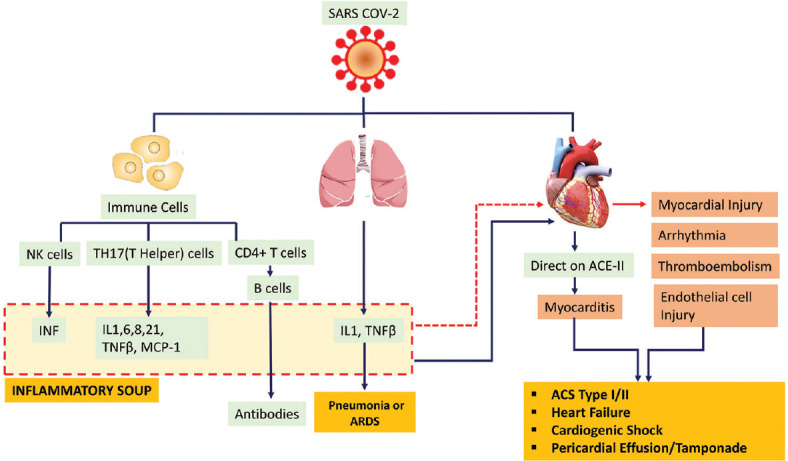
The SARS COV2 may cause myocardial effect either directly or indirectly. Interaction of the virus with the immune cells results in proinflammatory response by induction of T- and B- cells and production of inflammatory soup which comprises of Interferon, Interleukin (IL) -1,6,8,21, monocyte chemotactic protein (MCP)-1 and Tumor Necrosis factor ß etc. This inflammatory soup can act on myocardium to cause myocarditis and myocardial Injury. The SARS COV 2 can also act on myocardium directly causing myocarditis, myocardial injury, and Endothelial injury. Together the effect on myocardium may result in Acute Coronary syndrome (ACS), Heart failure, and Cardiogenic shock
Sometimes patient may present without any symptoms of fever/cough but cardiac symptom only.[26,27] The Myocardial injury in COVID-19 is associated with high mortality.[24] In children a link between Kawasaki disease and COVID-19 has also been seen.[28] When autopsies were done in patients with COVID-19 disease, myocardial infiltration of interstitial mononuclear cells was seen.[29]
Myocardial Injury and Myocarditis
Myocardial injury could be due to ischemia or non-ischemic event like myocarditis.[4,23,30] A study done to confirm the rate of death among patients having elevated Cardiac troponin with and without underlying cardiovascular disease and it was seen that patients with underlying cardiovascular disease have almost double the rate of death.[31] Patient presenting with elevated level of cardiac biomarkers, recent arrhythmia or acute onset heart dysfunction with COVID-19 patient raises high suspicion of acute myocarditis. The SARS-CoV 2 infection accentuates prothrombotic, inflammatory and procoagulant responses resulting in increased risk of acute nonischemic myocardial injury and acute MI (both type I and type II). In the early studies in China elevated level of cardiac enzymes and ECG abnormalities were seen in 7-20% cases with COVID-19.[4,32,33,34,35] In COVID-19 patients raised level of troponins had been associated with poor outcomes after review of all studies till date.
In COVID-19 patients who have evidence of acute myocardial injury (>99 percentile of URL) along with evidence of ECG and Echocardiographic changes are associated with more severe disease and grave prognosis. Elevation of cardiac troponins 2-3 times of the upper limit of normal (ULN) particularly in an older patient with a pre-existing cardiac disease does not warrant a workup unless accompanied with anginal chest discomfort or ECG changes. These mild elevations can easily be explained by either pre-existing cardiac disease or acute myocardial injury associated with COVID-19. However, marked elevation beyond 5 times of ULN may indicate shock, severe respiratory failure, myocarditis, and Type 1 MI.[4,24,36,37] These troponins levels may also remain elevated in renal insufficiency patients due to delayed excretion.
The BNP/NT pro-BNP being an indicator of hemodynamic stress and heart failure and their elevations can be related to pre-existing cardiac disease or due to the COVID-19 illness itself.[24,38,39,40] However, the rise of these enzymes may also corelate with the stress of right ventricle associated with COVID-19 due to pulmonary cause. Myocarditis is seen in COVID-19 patients after initiation of fever and this myocarditis could be due to upregulation of ACE2 in the myocardium and coronary vessels.[31,41] The hypoxia and immune mechanism of myocardial inflammation are also relevant in this scenario.[19,31,41]
Typical features of myocarditis with elevated levels of high sensitivity (hs) cardiac troponins during course of COVID-19 also require echocardiographic or MRI evidence.[42,43,44,45] However, most of the studies done lack echocardiography and MRI data. In a 112 patients cohort study it was seen that 14 patients had raised hs cardiac troponins but echo/ECG abnormalities were not typical of myocarditis so they suggested that myocardial injury was secondary to systemic cause rather than virus directly effecting myocardium.[27] However, in several case reports typical signs of myocarditis were seen along with elevated level of cardiac biomarkers and diffuse ST segment elevation had diffuse hypokinesia of both ventricles along with severe LV dysfunction.[31] MRI findings suggestive of active myocarditis include marked myocardial interstitial edema, diffuse late gadolinium enhancement and circumferential pericardial effusion. Presently role of endomyocardial biopsy in these patients is still under study and non-invasive imaging techniques like MRI or PET to diagnose myocardial inflammation can only be done if separate isolation facility is available to do such imaging.
Myocarditis was also seen in all historical epidemics with other corona viruses based on Cardiac MRI.[46] It is still not clear whether SARS CoV2 infects myocardium directly or not. If we presume that SARS-CoV 2 directly infects myocardium any myocarditis will manifests itself in acute or sub-acute stage.[47] Presence of mild inflammation and viral RNA in the myocardium of patients in COVID-19 have also been reported in autopsy reports.[48,49] A case report described a patient with low grade myocardial inflammation and corona virus particles at the myocardium but outside cardiomyocytes as seen I in endomyocardial biopsy suggest SARS CoV 2 may directly effects myocardium.[25]
Myocarditis has been seen suspected in many COVID-19 cases but its confirmation warrants tissue histology and Immunohistochemistry (IHC) but data is lacking in the literature in this regard. The myocardial injury from the COVID-19 can be explained by two mechanism i.e., either associated with the release of cytokines as inflammatory soup or direct effect of SARC-CoV-2 virus on the myocardium. This virus has a potential to infect cardiomyocytes, pericytes and fibroblasts via ACE 2 pathway leading to direct myocardial injury though this is still unproven and may require further autopsies and endomyocardial biopsies. Proposed investigations in suspected myocarditis in Covid-19 patients are summarized in Figure 4.
Figure 4.
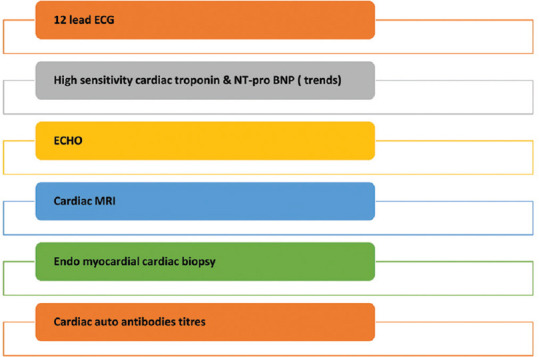
Proposed Investigation in suspected myocarditis in COVID-19 patients
Acute Coronary Syndrome
Several case series have been published regarding acute coronary syndrome in COVID-19 patients. A case series from United States described 18 patients with COVID-19 along with ST segment elevation indicative of acute MI and five required invasive percutaneous coronary procedures.[50] Similarly, in a case series from Italy in which 28 patients with COVID-19 presented with similar ECG changes 17 were candidates of coronary revascularization due to the culprit lesion.[26] However, in an Italian case series 24 out of 28 patients have not received positive COVID-19 results even at the time of coronary angiography suggesting the possibility that COVID-19 can cause ACS independently even when there is lack of systemic inflammation. Plaque rupture and thrombus formation is the main cause of type I MI in COVID-19 patients however Type II MI risk is higher due to demand supply mismatch which is mainly attributed to hypoxia and hemodynamic disturbances. The mechanism of ACS is summarized in the Figure 5 and that of Type I MI mechanism in Figure 6. The number of reported cases of ACS during COVID-19 period outbreak in Italy, Spain, United States and even in India has significantly lowered when the data was compared with Pre COVID-19 periods, despite the fact that COVID-19 may induce ACS in terms of both hospitalization as well as percutaneous intervention.[51,52,53] However out of hospital cardiac arrest was increased during COVID-19 outbreak in Italy which has been corelated with COVID-19 outbreak.[54,55]
Figure 5.
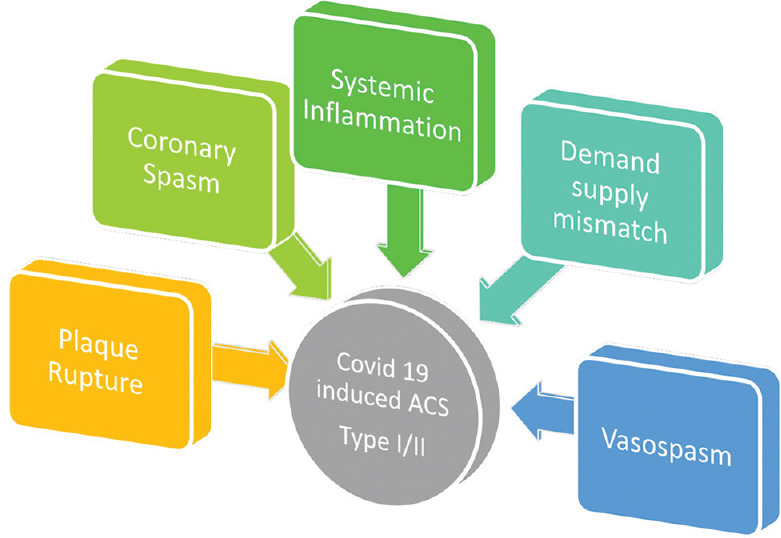
Mechanism of ACS in COVID-19
Figure 6.
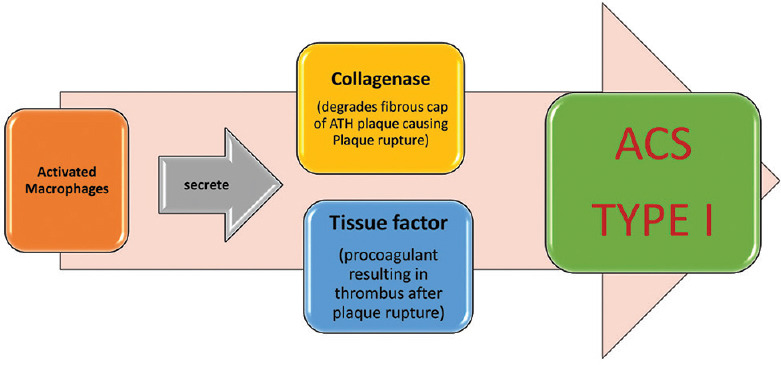
Type I MI in COVID-19
Heart Failure and Cardiogenic Shock
In 23% of patients presenting with COVID-19 heart failure was seen and this heart failure was more common in non survivors.[4] The heart failure in a COVID-19 infection may be just an unfolding of a subclinical cardiac dysfunction with a back ground of comorbidities of coronary artery disease, diabetes, hypertension, and various other diseases. An elevated levels of NT pro-BNP was found in 49% of all patients and 85% of these patients died. The exact aetiology of acute or decompensated heart failure is not yet known.[56]
During the COVID-19 disease the high grade fever, tachycardia, volume overload, and renal dysfunction can initiate the heart failure in elderly patients with diastolic dysfunction with preserved ejection fraction.[56] Development of stress-induced cardiomyopathy can also be seen in relation to immune response and cytokine-induced myocardial dysfunction.[57,58]
Covid pneumonia is the main cause of ARDS and pulmonary edma is mainly noncardiogenic, how ever since heart failure is not uncommon among COVID-19 patients so pulmonary plethora due to cardiac origin cannot be ignored.[56] Appropriate hemodynamic monitoring in respiratory failure can differentiate the pulmonary or cardiac cause. In patients with severe Covid pneumonia/ARDS and associated pulmonary hypertension, right sided heart failure must be evaluated.
In COVID-19 infection there is acute emotional/physical distress, increased sympathetic stimulation, vasospasm and a proinflammatory state. All these factors can precipitate stress cardiomyopathy, in stress cardiomyopathy troponin levels are low in comparison to the amount of cardiac dysfunction but BNP levels are high. This stress cardiomyopathy is diagnosed by exclusion of other underlying cardiovascular diseases and after identification of the acute trigger.[46]
Arrhythmias
Cardiac Palpitation is a common symptom mainly in patients without fever and cough.[59] These palpitations were even part of the presenting complaints in 7.3% cases in a cohort of 137 patients admitted for COVID-19 infection.[59]
From the main land China, a study done in 187 patients admitted in a hospital in the epicenter city Wuhan showed that the patients who had raised level of troponin have more likelihood of development of malignant arrythmia in comparison to those who had normal troponin levels.[29,50,60]
In COVID-19, genesis of cardiac arrythmia (atrial or ventricular) may be due either to myocardial injury or to inflammatory stress, neurohormonal, fever, hypoxia, metabolic disarray, sepsis and dyselectrolemia but it cannot be ascertained with clarity. The arrythmias can even be induced by various antivirals and antibiotics that are used to treat the disease itself.[20,61] Any new malignant tachyarrhythmia in combination with cardiac troponin rise must raise a query of underlying myocarditis.[41,45]
Thromboembolism
The COVID-19 disease has high rates of venous thromboembolism and Klok et al. suggested that these thromboembolic complications may be seen up to 31% in critically ill patients.[62] In COVID-19 features of the disseminated intravascular coagulation (DIC) and pulmonary embolism are common and marked by increase in D-dimer levels and FDPs. DIC has been 71.4% of non survivors.[63] Massive pulmonary embolism has been widely reported.[42] Elevated d dimers (>1 g/dl) is considered to be associated with in hospital death as suggested by a multi-center retrograde cohort study from China.[4] When COVID-19 survivors were compared with non survivors, the non survivors had significant high level of d dimers and FDP when compared with survivors and 71.4% of non-survivors had met clinical parameters for DIC.[63]
Rudolf Virchow historically described the three key predisposing factors to thromboembolic complications: vessel wall abnormalities (endothelial injury), abnormal flow, and coagulation state. The COVID-19 patients have all inflammatory mediators which are secondary to viremia, these inflammatory mediators may cause endothelial injury and when patient is sick prolong immobilization occurs. A total of 97 COVID-19 patients with sepsis induced coagulation dysfunction were studied retrospectively in whom prophylactic dose of low molecular weight of heparin was given and it was seen that this prophylactic anticoagulation could be the reason for lower mortality among them.[4]
Pericardial Effusion and Tamponade
COVID-19 elicit an immune response and may lead to pericarditis and effusion in later stages. It is hypothesized that due to immune-inflammatory responses and cytokine mediated effect there is development of effusive pericarditis. However, acute effusive pericarditis still remains a rare manifestation of COVID-19 disease.[31,64]
Case report also showed that this acute effusive pericarditis can also present as late complication in a COVID-19 patient as life-threating Cardiac Tamponade.[65,66] However, the pericardial effusion could also be secondary to post myocardial infraction in COVID-19 patients.
Conclusion
Due to sudden appearance of this pandemic, the planned and randomized trials are lacking for COVID-19 infection. The pathophysiology of cardiac involvement in COVID-19 infection is still under study. Several prospective randomized trials are ongoing to study the cardiac effect of COVID-19. Presently post Covid cardiac follow-up there is no clear guidelines however it is prudent for that patients who had cardiac involvement should be seen every 2-3 months. The convalescent phase (2-6 months) includes detailed history, physical examination, 12 lead ECG, 2D doppler echo, and preferably cardiac MRI with late gadolinium enhancement. Standard advice must be given as per physical activity. These patients must undergo regular CV assessment as shown in Figure 7. The future trajectory of this novel viral disease is still not known however cardiovascular problems associated with COVID-19 increases morbidity and mortality associated with the disease. A large number of treatment modalities are under trial but no treatment strategy has yet proven effective. Till the vaccine arrives, social distancing and use of face mask can reduce the burden of the disease and associated cardiovascular complications.
Figure 7.
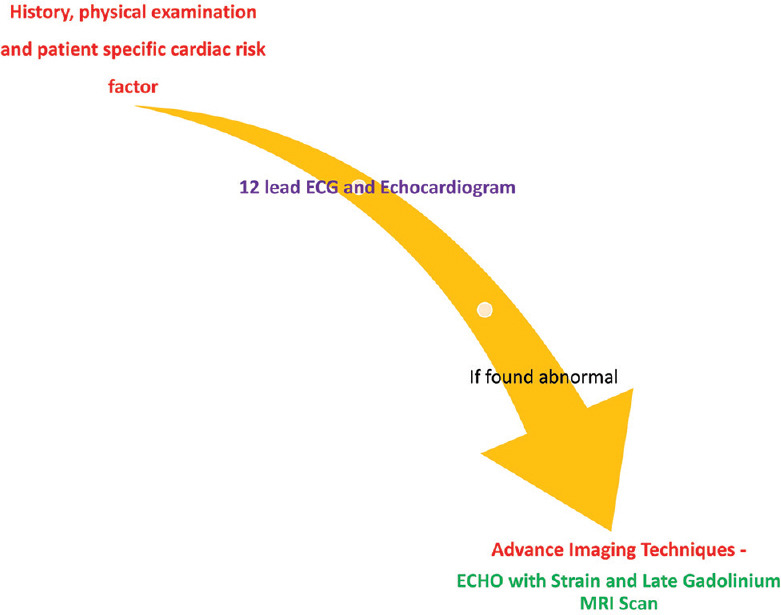
Regular CV assessment in post COVID-19 patient follow up
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
Authors wants to acknowledge Dr Neha Nigam Assistant Professor Department of Pathology, SGPGI Lucknow for help in Figure 1 and Figure 2 in the manuscript.
References
- 1.Guzik TJ, Mohiddin SA, Dimarco A, Patel V, Savvatis K, Marelli-Berg FM, et al. COVID-19 and the cardiovascular system: Implications for risk assessment, diagnosis, and treatment options. Cardiovasc Res. 2020;116:1666–87. doi: 10.1093/cvr/cvaa106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gupta A, Madhavan MV, Sehgal K, Nair N, Mahajan S, Sehrawat TS, et al. Extrapulmonary manifestations of COVID-19. Nat Med. 2020;26:1017–32. doi: 10.1038/s41591-020-0968-3. [DOI] [PubMed] [Google Scholar]
- 3.Li J, Gong X, Wang Z, Chen R, Li T, Zeng D, et al. Clinical features of familial clustering in patients infected with 2019 novel coronavirus in Wuhan, China? Virus Res. 2020;286:198043. doi: 10.1016/j.virusres.2020.198043. doi: 10.1016/j.virusres.2020.198043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020;395:1054–62. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fang L, Karakiulakis G, Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir Med. 2020;8:e21. doi: 10.1016/S2213-2600(20)30116-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vickers C, Hales P, Kaushik V, Dick L, Gavin J, Tang J, et al. Hydrolysis of biological peptides by human angiotensin-converting enzyme-related carboxypeptidase. J Biol Chem. 2002;277:14838–43. doi: 10.1074/jbc.M200581200. [DOI] [PubMed] [Google Scholar]
- 7.Gurwitz D. Angiotensin receptor blockers as tentative SARS-CoV-2 therapeutics. Drug Dev Res. 2020;81:537–40. doi: 10.1002/ddr.21656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu Y, Yang Y, Zhang C, Huang F, Wang F, Yuan J, et al. Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury. Sci China Life Sci. 2020;63:364–74. doi: 10.1007/s11427-020-1643-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tikellis C, Thomas MC. Angiotensin-Converting Enzyme 2 (ACE2) is a key modulator of the renin angiotensin system in health and disease. Int J Peptides. 2012;2012:256294. doi: 10.1155/2012/256294. doi: 10.1155/2012/256294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang H, Penninger JM, Li Y, Zhong N, Slutsky AS. Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: Molecular mechanisms and potential therapeutic target. Intensive Care Med. 2020;46:586–90. doi: 10.1007/s00134-020-05985-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dijkman R, Jebbink MF, Deijs M, Milewska A, Pyrc K, Buelow E, et al. Replication-dependent downregulation of cellular angiotensin-converting enzyme 2 protein expression by human coronavirus NL63. J Gen Virol. 2012;93:1924–9. doi: 10.1099/vir.0.043919-0. [DOI] [PubMed] [Google Scholar]
- 12.Julius S, Kjeldsen SE, Weber M, Brunner HR, Ekman S, Hansson L, et al. Outcomes in hypertensive patients at high cardiovascular risk treated with regimens based on valsartan or amlodipine: The VALUE randomised trial. Lancet. 2004;363:2022–31. doi: 10.1016/S0140-6736(04)16451-9. [DOI] [PubMed] [Google Scholar]
- 13.Sever P. The VALUE trial: A commentary. J Renin Angiotensin Aldosterone Syst. 2004;5:99–101. doi: 10.3317/jraas.2004.033. [DOI] [PubMed] [Google Scholar]
- 14.Di Somma S. Importance of rapid and effective reduction of blood pressure in treating hypertension for the prevention of cardiovascular diseases: A lesson from the VALUE study. High Blood Press Cardiovasc Prev. 2005;12:135–40. doi: 10.2165/00151642-200512030-00004. [DOI] [PubMed] [Google Scholar]
- 15.Chen D, Li X, Song Q, Hu C, Su F, Dai J, et al. Assessment of hypokalemia and clinical characteristics in patients with coronavirus disease 2019 in Wenzhou, China. JAMA Netw Open. 2020;3:e2011122. doi: 10.1001/jamanetworkopen.2020.11122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Siedlinski M, Jozefczuk E, Xu X, Teumer A, Evangelou E, Schnabel RB, et al. White blood cells and blood pressure: A mendelian randomization study. Circulation. 2020;141:1307–17. doi: 10.1161/CIRCULATIONAHA.119.045102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Youn JC, Yu HT, Lim BJ, Koh MJ, Lee J, Chang DY, et al. Immunosenescent CD8+T cells and C-X-C chemokine receptor type 3 chemokines are increased in human hypertension. Hypertension. 2013;62:126–33. doi: 10.1161/HYPERTENSIONAHA.113.00689. [DOI] [PubMed] [Google Scholar]
- 18.Vaduganathan M, Vardeny O, Michel T, McMurray JJV, Pfeffer MA, Solomon SD. Renin-angiotensin-aldosterone system inhibitors in patients with Covid-19. N Engl J Med. 2020;382:1653–9. doi: 10.1056/NEJMsr2005760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O. Potential effects of coronaviruses on the cardiovascular system: A review. JAMA Cardiol. 2020;5:831–40. doi: 10.1001/jamacardio.2020.1286. [DOI] [PubMed] [Google Scholar]
- 20.Clerkin KJ, Fried JA, Raikhelkar J, Sayer G, Griffin JM, Masoumi A, et al. COVID-19 and cardiovascular disease. Circulation. 2020;141:1648–55. doi: 10.1161/CIRCULATIONAHA.120.046941. [DOI] [PubMed] [Google Scholar]
- 21.Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, Biondi-Zoccai G, et al. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2352–71. doi: 10.1016/j.jacc.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zheng YY, Ma YT, Zhang JY, Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020;17:259–60. doi: 10.1038/s41569-020-0360-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth universal definition of myocardial infarction (2018) J Am Coll Cardiol. 2018;72:2231–64. doi: 10.1016/j.jacc.2018.08.1038. [DOI] [PubMed] [Google Scholar]
- 24.Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5:802–10. doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tavazzi G, Pellegrini C, Maurelli M, Belliato M, Sciutti F, Bottazzi A, et al. Myocardial localization of coronavirus in COVID-19 cardiogenic shock. Eur J Heart Fail. 2020;22:911–5. doi: 10.1002/ejhf.1828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stefanini GG, Montorfano M, Trabattoni D, Andreini D, Ferrante G, Ancona M, et al. ST-elevation myocardial infarction in patients with COVID-19: Clinical and angiographic outcomes. Circulation. 2020;141:2113–6. doi: 10.1161/CIRCULATIONAHA.120.047525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Deng Q, Hu B, Zhang Y, Wang H, Zhou X, Hu W, et al. Suspected myocardial injury in patients with COVID-19: Evidence from front-line clinical observation in Wuhan, China. Int J Cardiol. 2020;311:116–21. doi: 10.1016/j.ijcard.2020.03.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Riphagen S, Gomez X, Gonzalez-Martinez C, Wilkinson N, Theocharis P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet. 2020;395:1607–8. doi: 10.1016/S0140-6736(20)31094-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8:420–2. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sarkisian L, Saaby L, Poulsen TS, Gerke O, Jangaard N, Hosbond S, et al. Clinical characteristics and outcomes of patients with myocardial infarction, myocardial injury, and nonelevated troponins. Am J Med. 2016;129:446 e5–e21. doi: 10.1016/j.amjmed.2015.11.006. [DOI] [PubMed] [Google Scholar]
- 31.Inciardi RM, Lupi L, Zaccone G, Italia L, Raffo M, Tomasoni D, et al. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:819–24. doi: 10.1001/jamacardio.2020.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–9. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–20. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72314 cases from the Chinese center for disease control and prevention. JAMA. 2020;323:1239–42. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 36.Arentz M, Yim E, Klaff L, Lokhandwala S, Riedo FX, Chong M, et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State. JAMA. 2020;323:1612–4. doi: 10.1001/jama.2020.4326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gao C, Wang Y, Gu X, Shen X, Zhou D, Zhou S, et al. Association between cardiac injury and mortality in hospitalized patients infected with avian influenza A (H7N9) virus. Crit Care Med. 2020;48:451–8. doi: 10.1097/CCM.0000000000004207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Christ-Crain M, Breidthardt T, Stolz D, Zobrist K, Bingisser R, Miedinger D, et al. Use of B-type natriuretic peptide in the risk stratification of community-acquired pneumonia. J Intern Med. 2008;264:166–76. doi: 10.1111/j.1365-2796.2008.01934.x. [DOI] [PubMed] [Google Scholar]
- 39.Mueller C, McDonald K, de Boer RA, Maisel A, Cleland JGF, Kozhuharov N, et al. Heart Failure Association of the European Society of Cardiology practical guidance on the use of natriuretic peptide concentrations. Eur J Heart Fail. 2019;21:715–31. doi: 10.1002/ejhf.1494. [DOI] [PubMed] [Google Scholar]
- 40.Mueller C, Laule-Kilian K, Frana B, Rodriguez D, Scholer A, Schindler C, et al. Use of B-type natriuretic peptide in the management of acute dyspnea in patients with pulmonary disease. Am Heart J. 2006;151:471–7. doi: 10.1016/j.ahj.2005.03.036. [DOI] [PubMed] [Google Scholar]
- 41.Chen C, Zhou Y, Wang DW. SARS-CoV-2: A potential novel etiology of fulminant myocarditis. Herz. 2020;45:230–2. doi: 10.1007/s00059-020-04909-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Danzi GB, Loffi M, Galeazzi G, Gherbesi E. Acute pulmonary embolism and COVID-19 pneumonia: A random association? Eur Heart J. 2020;41:1858. doi: 10.1093/eurheartj/ehaa254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Violi F, Pastori D, Cangemi R, Pignatelli P, Loffredo L. Hypercoagulation and antithrombotic treatment in coronavirus 2019: A new challenge. Thromb Haemost. 2020;120:949–56. doi: 10.1055/s-0040-1710317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Courand PY, Harbaoui B, Bonnet M, Lantelme P. Spontaneous coronary artery dissection in a patient with COVID-19. JACC Cardiovasc Interv. 2020;13:e107–8. doi: 10.1016/j.jcin.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475–81. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cheng R, Leedy D. COVID-19 and acute myocardial injury: The heart of the matter or an innocent bystander? Heart. 2020;106:1122–4. doi: 10.1136/heartjnl-2020-317025. [DOI] [PubMed] [Google Scholar]
- 47.Hendren NS, Drazner MH, Bozkurt B, Cooper LT., Jr Description and proposed management of the acute COVID-19 cardiovascular syndrome. Circulation. 2020;141:1903–14. doi: 10.1161/CIRCULATIONAHA.120.047349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wichmann D, Sperhake JP, Lutgehetmann M, Steurer S, Edler C, Heinemann A, et al. Autopsy findings and venous thromboembolism in patients with COVID-19: A prospective cohort study. Ann Intern Med. 2020;173:268–77. doi: 10.7326/M20-2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Schaller T, Hirschbuhl K, Burkhardt K, Braun G, Trepel M, Markl B, et al. Postmortem examination of patients with COVID-19. JAMA. 2020;323:2518–20. doi: 10.1001/jama.2020.8907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bangalore S, Sharma A, Slotwiner A, Yatskar L, Harari R, Shah B, et al. ST-segment elevation in patients with Covid-19-A case series. N Engl J Med. 2020;382:2478–80. doi: 10.1056/NEJMc2009020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Garcia S, Albaghdadi MS, Meraj PM, Schmidt C, Garberich R, Jaffer FA, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.De Filippo O, D’Ascenzo F, Angelini F, Bocchino PP, Conrotto F, Saglietto A, et al. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N Engl J Med. 2020;383:88–9. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.De Rosa S, Spaccarotella C, Basso C, Calabro MP, Curcio A, Filardi PP, et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. 2020;41:2083–8. doi: 10.1093/eurheartj/ehaa409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Baldi E, Sechi GM, Mare C, Canevari F, Brancaglione A, Primi R, et al. COVID-19 kills at home: The close relationship between the epidemic and the increase of out-of-hospital cardiac arrests. Eur Heart J. 2020;41:3045–54. doi: 10.1093/eurheartj/ehaa508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Reinier K, Stecker EC, Uy-Evanado A, Chugh HS, Binz A, Nakamura K, et al. Sudden cardiac death as first manifestation of heart disease in women: The Oregon sudden unexpected death study, 2004-2016. Circulation. 2020;141:606–8. doi: 10.1161/CIRCULATIONAHA.119.044169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mehra MR, Ruschitzka F. COVID-19 illness and heart failure: A missing link? JACC Heart Fail. 2020;8:512–4. doi: 10.1016/j.jchf.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fried JA, Ramasubbu K, Bhatt R, Topkara VK, Clerkin KJ, Horn E, et al. The variety of cardiovascular presentations of COVID-19. Circulation. 2020;141:1930–6. doi: 10.1161/CIRCULATIONAHA.120.047164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Prabhu SD. Cytokine-induced modulation of cardiac function. Circ Res. 2004;95:1140–53. doi: 10.1161/01.RES.0000150734.79804.92. [DOI] [PubMed] [Google Scholar]
- 59.Liu K, Fang YY, Deng Y, Liu W, Wang MF, Ma JP, et al. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin Med J. 2020;133:1025–31. doi: 10.1097/CM9.0000000000000744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Baldi E, Sechi GM, Mare C, Canevari F, Brancaglione A, Primi R, et al. Out-of-hospital cardiac arrest during the Covid-19 outbreak in Italy. N Engl J Med. 2020;383:496–8. doi: 10.1056/NEJMc2010418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sanders JM, Monogue ML, Jodlowski TZ, Cutrell JB. Pharmacologic treatments for coronavirus disease 2019 (COVID-19): A review. JAMA. 2020;323:1824–36. doi: 10.1001/jama.2020.6019. [DOI] [PubMed] [Google Scholar]
- 62.Klok FA, Kruip M, van der Meer NJM, Arbous MS, Gommers D, Kant KM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–7. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18:844–7. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Dabbagh MF, Aurora L, D’Souza P, Weinmann AJ, Bhargava P, Basir MB. Cardiac tamponade secondary to COVID-19. JACC Case Rep. 2020;2:1326–30. doi: 10.1016/j.jaccas.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fox K, Prokup JA, Butson K, Jordan K. Acute effusive pericarditis: A late complication of COVID-19. Cureus. 2020;12:e9074. doi: 10.7759/cureus.9074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Asif T, Kassab K, Iskander F, Alyousef T. Acute pericarditis and cardiac tamponade in a patient with COVID-19: A therapeutic challenge? Eur J Case Rep Intern Med. 2020;7:001701. doi: 10.12890/2020_001701. doi: 10.12890/2020_001701. [DOI] [PMC free article] [PubMed] [Google Scholar]


