Abstract
Nipah virus (NiV) and Hendra virus (HeV) are zoonotic paramyxoviruses classified in the genus Henipavirus of the family Paramyxoviridae. The entry of henipaviruses occurs through a pH-independent membrane-fusion mechanism mediated by the cooperation of the viral attachment (G) and fusion (F) envelope glycoproteins following virion binding to susceptible host cells. Virus attachment is mediated by the interaction of the G glycoprotein with ephrin-B2 or ephrin-B3, which were identified as the functional receptors of henipavirus. Several residues of the G glycoprotein that are important for receptor binding have been determined through mutagenesis and structural analyses; however, similar approaches have not been carried out for the viral receptor ephrin-B2. Here, an alanine-scanning mutagenesis analysis was performed to identify residues of ephrin-B2 which are critical for NiV binding and entry by using an NiV-F- and -G-glycoprotein pseudotyped lentivirus assay. Results indicated that the G–H loop of ephrin-B2 was indeed critical for the interaction between ephrin-B2 and NiV-G. Unexpectedly, however, some alanine-substitution mutants located in the G–H loop enhanced the infectivity of the NiV pseudotypes, in particular an L124A mutation enhanced entry >30-fold. Further analysis of the L124A ephrin-B2 mutant demonstrated that an increased binding affinity of the mutant receptor with NiV-G was responsible for the enhanced infectivity of both pseudovirus and infectious virus. In addition, cell lines that were stably expressing the L124A mutant receptor were able to support NiV infection more efficiently than the wild-type molecule, potentially providing a new target-cell platform for viral isolation or virus-entry inhibitor screening and discovery.
Introduction
Nipah virus (NiV) and Hendra virus (HeV) are zoonotic paramyxoviruses classified in the genus Henipavirus of the family Paramyxoviridae (Eaton et al., 2006). NiV first emerged in Malaysia in 1998–1999 as the causative agent of an outbreak of respiratory disease in pigs and severe encephalitic disease with high case fatality in humans (Chua et al., 2000). Similar outbreaks of NiV have been reported in India and Bangladesh, on nearly a yearly basis, since 2001 (Chadha et al., 2006; Hsu et al., 2004; Luby et al., 2009). HeV was discovered in Australia in 1994 (Murray et al., 1995) and continues to cause sporadic outbreaks there in horses and humans (Field et al., 2007). Epidemiological studies have demonstrated that several species of fruit bats (flying foxes) of the genus Pteropus are the principal natural reservoirs of henipaviruses and are responsible for the spill-over events that resulted in both animal and human infections (Epstein et al., 2008; Iehlé et al., 2007; Reynes et al., 2005; Wacharapluesadee et al., 2005; Yob et al., 2001).
The henipavirus virion contains two viral membrane-anchored envelope glycoproteins, the attachment (G) and the fusion (F) glycoproteins. Henipavirus entry occurs through a pH-independent membrane-fusion mechanism between the virion membrane and the plasma membrane of the host cell, which is mediated by the cooperation of these two structural glycoproteins following receptor binding. A recent report has also provided some evidence that NiV fusion and entry can also occur following virion endocytosis (Pernet et al., 2009). The henipavirus G glycoprotein is a type-II integral membrane protein consisting of an N-terminal cytoplasmic tail, a single transmembrane domain, a stalk region and a C-terminal globular head domain. The F glycoprotein is a class-I fusion protein, containing two heptad repeat regions and a hydrophobic fusion peptide (reviewed by Bossart & Broder, 2009). Ephrin-B2 and ephrin-B3 have been identified as functional receptors for both NiV and HeV (Bishop et al., 2007; Bonaparte et al., 2005; Negrete et al., 2005). Ephrins are the highly conserved ligands that bind to Eph receptor tyrosine kinases. The Eph receptors and their ephrin ligands make up an important group of bidirectional signalling molecules that function in both embryonic and adult tissues by regulating processes such as angiogenesis, neuron axonal guidance and tumorigenesis (Murai & Pasquale, 2003).
Recently, the crystal structures of the henipavirus G–ephrin-B2/B3 complexes have been resolved (Bowden et al., 2008; Xu et al., 2008). The complex structure indicates that the receptor-binding domain of glycoprotein G is conformation-dependent and consists predominantly of two regions: a large docking region of polar residues near the rim of the globular head and a distinct channel which accepts the G–H loop residues of the B class ephrins. However, neither of those studies were complemented by mutagenesis in conjunction with functional studies. Some important structural elements and/or residues within the ephrin-B2 and -B3 binding sites on the NiV-G or HeV-G proteins were identified in earlier studies by using site-directed mutagenesis (Bishop et al., 2007; Guillaume et al., 2006; Negrete et al., 2007; reviewed by Hickey & Broder, 2009). However, the NiV-G binding sites on ephrin-B2 have not been analysed in detail by mutagenesis, although a previous report did indicate that the G–H loop of ephrin-B2 is involved in binding with NiV-G (Bonaparte et al., 2005). Following the identification of the ephrin-B2 and -B3 henipavirus receptors, we initiated an alanine-scanning mutagenesis study to identify the critical residues of ephrin-B2 that are responsible for NiV entry. Our results, reported here, functionally confirm that the G–H loop of ephrin-B2 is critical for the interaction between ephrin-B2 and NiV-G (Negrete et al., 2007). However, unexpectedly, by taking a functional approach in our analysis our study also revealed that some alanine-substitution mutations located within the G–H loop of ephrin-B2 were able to enhance virus entry and infection by both henipavirus pseudotypes as well as by infectious viruses. Our study potentially provides a new target host-cell platform for either virus isolation or virus entry inhibitor screening and discovery.
Results
Alanine substitutions in the G–H loop of ephrin-B2 enhance virus entry
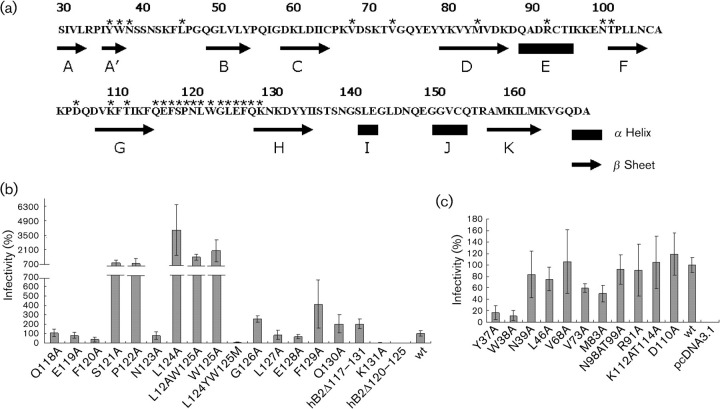
The original aim of the present study was to identify the critical determinants for NiV entry on the ephrin-B2 molecule. Previous reports showed that the ephrin-B2 partner receptors EphB3 and EphB4 could significantly inhibit HeV and NiV infections, suggesting that the Eph-binding domain (G–H loop) of the ephrin ligands may overlap with that of the henipavirus G protein (Negrete et al., 2006). Here, two deletion mutants (hB2Δ117–131 and hB2Δ120–125), in which G–H loop is completely or partially deleted, failed to support the entry of pseudotyped particles (NiVpp) (Fig. 1b), consistent with the notion that the G–H loop of ephrin-B2 is critical for the NiV-G–ephrin-B2 interaction.
Fig. 1.
NiV glycoprotein pseudotyped virus infection of HeLa-USU cells expressing wild-type (wt) or mutant ephrin-B2. NiV-G and NiV-F glycoproteins were pseudotyped onto a human immunodeficiency virus (HIV)-1 based core virus using the NL4-3-Luc-E−R+ backbone (NiVpp) and used to infect HeLa-USU cells transfected with either wt or mutant ephrin-B2. Entry efficiency of NiVpp was measured by luciferase reporter-gene assay and is expressed as a percentage of wt ephrin-B2 (100 %). The enhanced infectivity of cells expressing some of the mutant ephrin-B2 molecules is highlighted by using a split y-axis. Data shown are the mean of triplicates±sd and one representative experiment of three is shown. (a) Schematic of ephrin-B2. Secondary structure elements are shown with an arrow (β-sheet) and black box (α-helix). The asterisks indicate residues that were targeted by alanine-scanning mutagenesis. (b) Mutations located within the G–H loop of ephrin-B2. (c) Mutations located outside the G–H loop of ephrin-B2.
Additional alanine substitution mutations were selected with two considerations in mind: first, we wished to target residues known to be critical for Eph and ephrin-B2/B3 binding; second, we wanted to focus on residues outside the G–H loop that are conserved in ephrin-B2 and ephrin-B3, but not in ephrin-B1. In addition, the unique sites of ephrin-B2, which were specific for interaction between ephrin-B2 and its ligands, were selected. A total of 26 alanine-substitution mutants were generated in ephrin-B2, including 15 within and 11 outside the G–H-loop domain (Table 1 and Fig. 1a). The plasmids containing either the wild-type (wt) or mutation-containing ephrin-B2 gene were transfected into HeLa-USU cells, allowed to express the encoded protein and then these target cells were tested for susceptibility to infection by the NiVpp. Except for mutants Y37A and W38A, which exhibited a significant reduction in their ability to support pseudovirus infection, the majority of the ephrin-B2 mutants, all located outside the G–H loop, had only minor effects on NiVpp infection in comparison to wt ephrin-B2 (Fig. 1c). The Asn39 residue of ephrin-B2 is a predicted N-linked glycosylation site and is conserved in ephrin-B2 and ephrin-B3; however, mutation of Asn39 to alanine had no significant effect on NiVpp infection. Alanine-substitution mutation of the unique sites, including Val68, Asn98, Thr99 and Lys112, also had little effect on NiVpp infection, with only mutations Val73A and Met83A showing slightly lower infectivity, on average, in comparison to wt ephrin-B2.
Table 1.
Summary of ephrin-B2 substitution mutants
Class I, Critical for Eph and ephrin-B2/B3 binding; class II, critical for Nipah-G and ephrin-B2 binding; class III, conservation in ephrin-B2/B3, but not in ephrin-B1 or unique sites of ephrin-B2. The expression levels of ephrin-B2 and its mutants are presented as: +++, high; ++, medium; +, low.
| Ephrin-B2 mutant | Class | Expression | Infectivity (%) | Note |
| wt | +++ | 100 | ||
| Y37A | III | ++ | 17 | |
| W38A | + | 12 | Structure stabilization | |
| N39A | III | +++ | 84 | Glycosylation site |
| L46A | +++ | 76 | Unique site of ephrin-B3 | |
| V68A | III | +++ | 106 | |
| V73A | III | +++ | 60 | |
| M83A | III | +++ | 50 | |
| R91A | III | +++ | 93 | |
| N98AT99A | I, III | +++ | 91 | |
| D110A | I | +++ | 105 | |
| K112AT114A | I, III | +++ | 119 | |
| Q118A | I, II | +++ | 108 | |
| E119A | I | +++ | 80 | |
| F120A | II | +++ | 38 | |
| S121A | I, II | +++ | 1021 | |
| P122A | I, II | +++ | 1008 | |
| N123A | I, II | +++ | 78 | |
| L124A | I, II, III | +++ | 3674 | Enhanced binding affinity with NiV-G |
| W125A | I, II, III | +++ | 1504 | |
| L12AW125A | I, II, III | +++ | 2022 | |
| L124YW125M | I, II, III | +++ | 5 | |
| G126A | II | +++ | 257 | |
| L127A | II | +++ | 86 | |
| E128A | I, II | +++ | 68 | |
| F129A | +++ | 411 | Conservation among ephrin-B1/B2/B3 | |
| Q130A | I | +++ | 204 | |
| K131A | +++ | 204 | Unique site of ephrin-B3 | |
| hB2del117–131 | I, II | + | 1 | Complete deletion of G–H loop |
| hB2del120–125 | I, II | ++++ | 1 | Partial deletion of G–H loop |
In contrast, most mutations located within the G–H loop, with the exception of the F120A mutant, could support NiVpp entry to reporter signal levels comparable to wt ephrin-B2. However, and unexpectedly, we also observed that several of these ephrin-B2 mutations facilitated an enhanced level of NiVpp infection (Fig. 1b), including S121A, P122A, L124A and W125A. Indeed, a previous report suggested that two residues in ephrin-B2, Leu124 and Trp125, were important for NiV entry, and replacement of these two residues in ephrin-B2 with the corresponding Tyr–Met residues from ephrin-B1 showed a markedly reduced level of NiV entry (Negrete et al., 2006). For comparison, a double alanine-substitution ephrin-B2 mutant (L124A–W125A) was then constructed as well as a control double mutation containing the construct L124Y–W125M. Infectivity assays using these constructs revealed that while the L124Y–W125M ephrin-B2 mutant yielded an approximately 90 % reduction in NiVpp infection, as compared to wt ephrin-B2, the L124A/W125A ephrin-B2 mutant increased infectivity approximately 20-fold in the NiVpp-based assay (Fig. 1b).
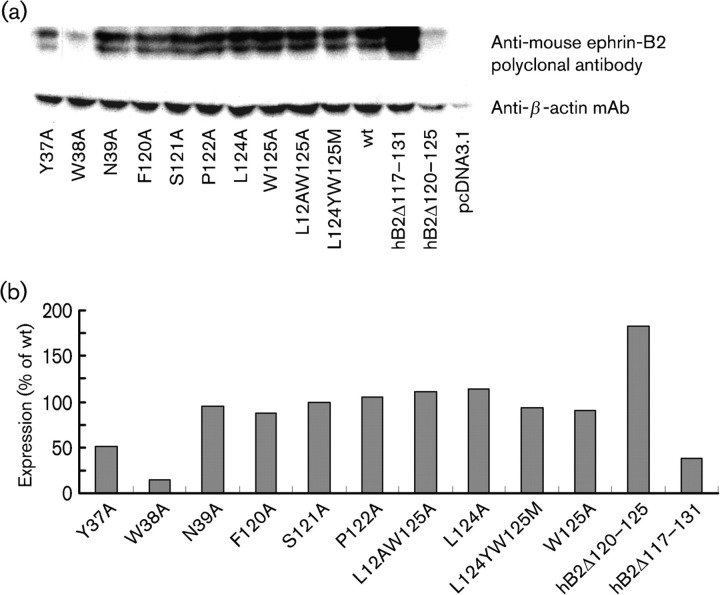
To eliminate the possibility that the observed infectivity difference was a result of differences in protein expression level for the different mutants, lysates of HeLa-USU cells transfected with equal amounts of plasmids encoding wt or mutant ephrin-B2 were analysed by Western blot (Fig. 2a) and quantified by densitometry (Fig. 2b). These results showed that the Y37, W38A and hB2Δ117–131 mutants did have lower levels of expression in comparison to the wt ephrin-B2 expression level. Other ephrin-B2 mutation-containing constructs, including S121A, P122A and L124A, were expressed at levels similar to that of wt ephrin-B2 (Fig. 2). Immunofluorescence-based analysis of wt or mutant ephrin-B2 on cell-surface expression level by both confocal immunofluorescence microscopy (Fig. 3a) and flow cytometry (Fig. 3b) further indicated that the mutations appeared to have little effect on cell surface expression for L124A, hB2Δ120–125 and wt ephrin-B2. Identical results were obtained with the other ephrin-B2 mutants (data not shown).
Fig. 2.
Western blot analysis of ephrin-B2 expression. (a) Equal amounts of a plasmid encoding either the wt or a mutant ephrin-B2 gene were transfected into equivalent cultures of HeLa-USU cells. Following expression for 48 h, cells were lysed and equal amounts (volume in µl) of the various lysates were resolved by using SDS-PAGE and transferred onto a PVDF membrane. Duplicate membranes were probed with goat anti-mouse ephrin-B2 (top) or mouse anti-human β-actin (bottom), respectively. (b) Quantification of the expression of the wt and mutant ephrin-B2. The bands in (a) were quantified by densitometry using the ImageJ program (version 1.44) by using values obtained from densitometric measurements of the bands. The values of the ephrin-B2 mutations are expressed as a percentage of wt ephrin-B2 (100 %). The data were normalized with the corresponding values for β-actin.
Fig. 3.
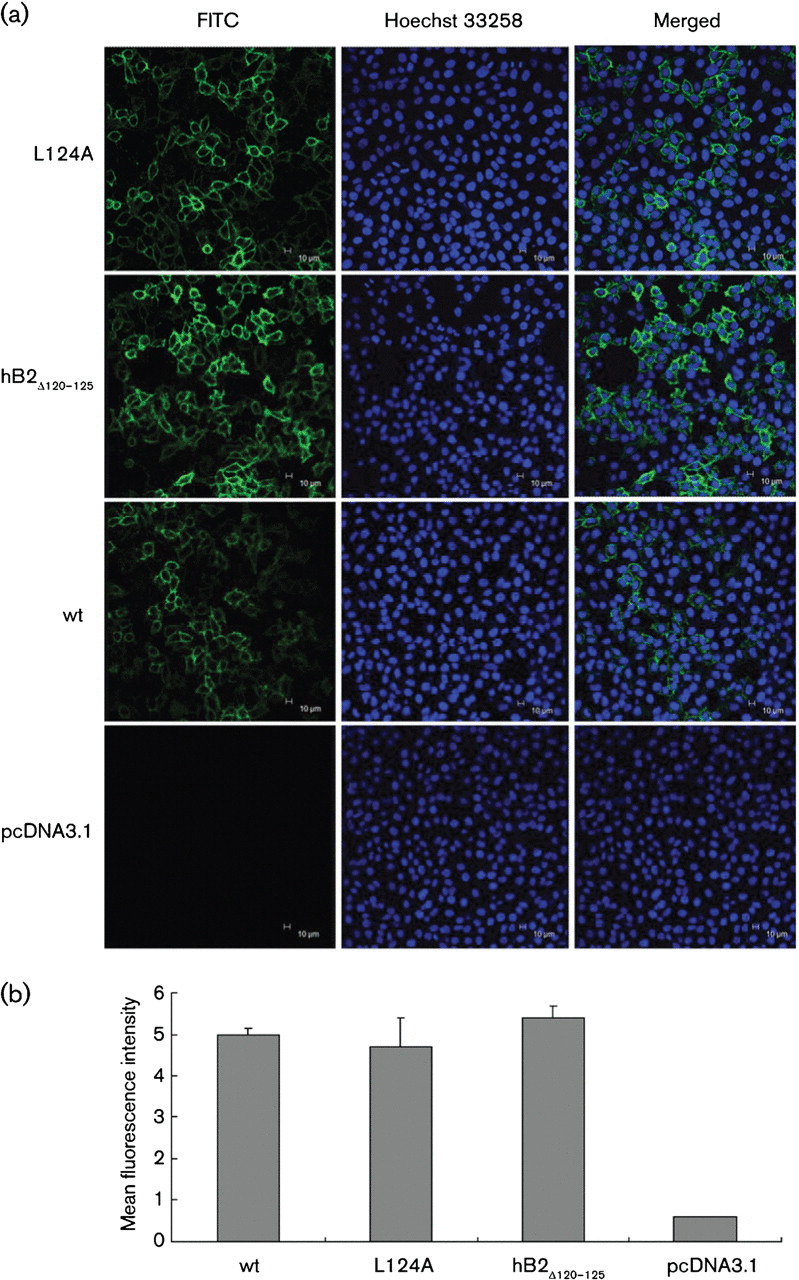
Immunofluorescence detection and flow cytometry of ephrin-B2 expression on cell surface. HeLa-USU cells were transfected with the indicated expression plasmids. Following expression for 24 h, cells were incubated with goat anti-ephrin-B2 antibody, followed by probing with FITC-conjugated donkey anti-goat IgG. The surface expression of wt or mutant ephrin-B2 was detected by confocal immunofluorescence microscopy (a) and quantified by flow cytometry (b). (a) The expression plasmids are shown at the left side of the panels. The columns (from left to right) represent staining of expressed ephrin-B2 (FITC, in green), cell nuclei (Hoechst 33258, in blue) and the superimposed images of the two. (b) Surface expression of wt or mutant ephrin-B2 was quantified by flow cytometry. The data are shown as the mean fluorescence intensity of the transfected cells indicated.
Analysis of binding specificity between ephrin-B2 L124A and pseudovirus
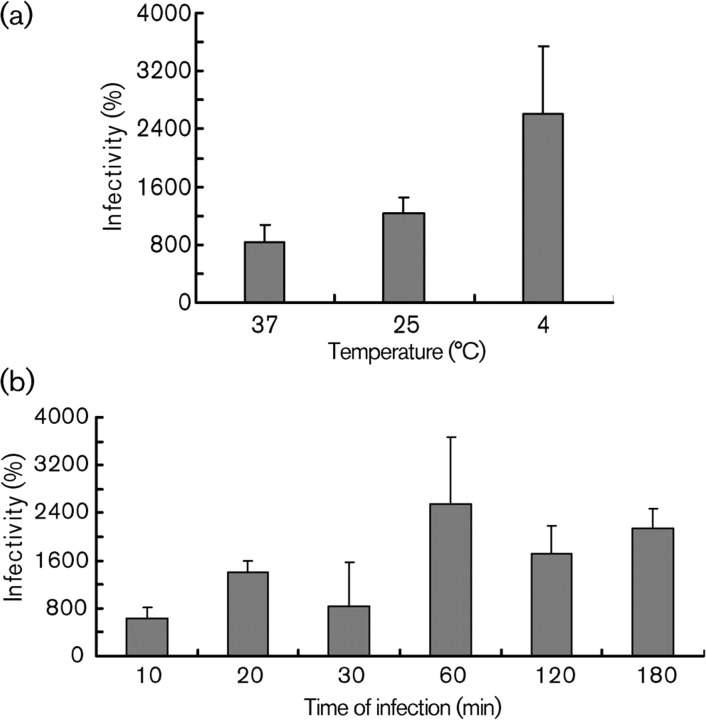
Among the panel of different ephrin-B2 mutants, mutant L124A showed a significant enhancement of virus entry by the pseudotyped virus luciferase-reporter-gene assay, and therefore L124A was selected for more detailed analysis. To determine the binding specificity between NiVpp and the L124A mutant, NiVpp was pre-adsorbed to cultures of HeLa-USU cells expressing L124A mutant or wt ephrin-B2 for 1 h at different temperatures (4, 25 and 37 °C), followed by assaying for virus entry. The results showed that the enhanced entry by cultures expressing L124A mutant over wt epherin-B2 was consistently higher at all three temperatures (Fig. 4a). Notably, this enhanced entry by the L124A mutants was higher at lower temperature. These results suggested that the binding stage, and not some post-fusion event, contributed to enhanced entry by L124A mutants. To further investigate the difference between the wt and mutant ephrin-B2 in the kinetics of the virus entry process, NiVpp was pre-adsorbed to HeLa-USU cells expressing L124A mutant or wt ephrin-B2 for different times at 37 °C, followed by washing and processing in the virus-entry assay as before. As shown in Fig. 4(b), the entry mediated by L124A was again consistently higher regardless of the time of incubation. Taken together, these data clearly indicate that the L124A mutant enhances NiVpp entry during the virion adsorption phase of infection, regardless of the temperature or time tested here.
Fig. 4.
Kinetic analysis of NiV-glycoprotein pseudovirus entry into HeLa-USU cells expressing wt or mutant L124A ephrin-B2. (a) Various pseudovirus preparations were adsorbed to ephrin-B2-expressing cells at 4, 25 or 37 °C for 1 h. The inoculum was removed and cells were washed with PBS and cultured with fresh media at 37 °C. Entry efficiency of the NiVpp at the different incubation temperatures was measured by luciferase reporter-gene assay at 48 h post-infection (p.i.) and is expressed as the percentage of wt ephrin-B2 at the corresponding temperature (100 %). (b) Pseudotyped viruses were adsorbed to ephrin-B2-expressing cells at 37 °C for different time intervals, and entry efficiency of the NiVpp was measured by luciferase reporter-gene assay at 48 h p.i. and is expressed as the percentage of wt ephrin-B2 at the corresponding time point (100 %). Error bars indicate sd.
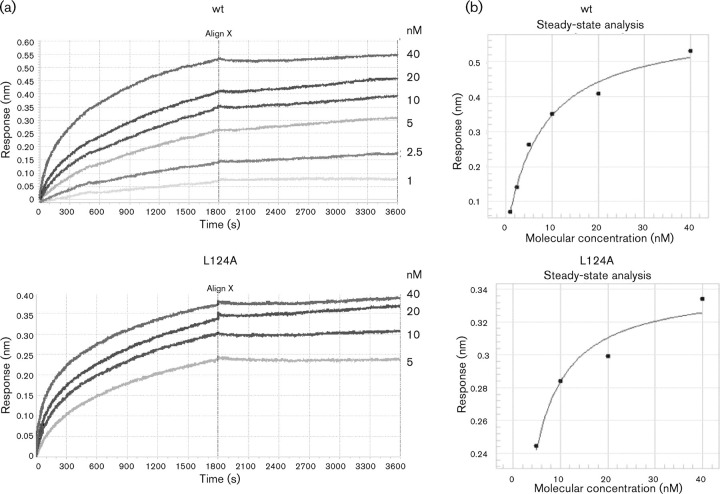
L124A binds NiV-G at higher affinity than wt ephrin-B2
Using bio-layer interferometry technology, the difference in binding affinities between the NiV-G and the wt ephrin-B2 or the L124A mutant was further examined. Soluble wt ephrin-B2 and the L124A mutant were expressed and purified from 2–5 l of Sf9 cells and used as the analyte. Steady-state analysis of the real-time binding curves (Fig. 5a) indicated that the K D value for wt ephrin-B2 binding to NiV-G (3.36×10−10) was in fact more than tenfold greater than for the binding observed for the L124A mutant (2.66×10−11) (Fig. 5b). NiV-G binds to the wt and L124A mutant ephrin-B2 molecules with similar on-rates (6.72×104 and 8.89×104, respectively). However, their off-rates were significantly different. The K off for the binding of the L124A mutant to NiV-G (2.37×10−6) was more than tenfold slower than that observed for wt ephrin-B2 (2.26×10−5). Together, these results demonstrate that NiV-G engages the L124A mutant with significantly higher affinity compared with wt ephrin-B2, and these observations were consistent with the temperature- and time-varied infectivity assays.
Fig. 5.
Binding kinetic analysis of NiV-G to wt or mutant L124A ephrin-B2 by bio-layer interferometry. (a) Real-time binding analysis of NiV-G to the wt or mutant L124A ephrin-B2. Bio-layer interferometry was used to measure the binding kinetics of soluble NiV-G to both ephrin-B2 (wt) and its mutant (L124A) in response units (nm). Biotinylated soluble NiV glycoprotein G (sNiV-G) was immobilized to streptavidin-coated biosensors, and the binding of wt and mutant ephrin-B2 was assessed at the indicated concentrations. (b) Steady-state analysis of real-time binding data obtained with the Octet Red system. The plots in each panel show response versus protein concentration curves derived from the raw binding data. One representative experiment of two is shown.
The L124A mutant enhances NiV glycoprotein-mediated cell-to-cell fusion
We next examined whether the increased affinity between NiV-G and the L124A mutant ephrin-B2 correlated with enhancement of the glycoprotein-mediated cell-to-cell fusion. The wt or L124A mutant ephrin-B2 were co-transfected with plasmids encoding NiV-F and -G proteins, and syncytia formation was monitored at 24 h post-transfection. As expected, syncytia formation was observed in HeLa-USU cells transfected with the wt or L124A ephrin-B2 (Fig. 6a). The mean size of syncytia in HeLa-USU cells transfected with L124A ephrin-B2 was larger than that for cells transfected with wt ephrin-B2 and was significantly different (P = 0.002) (Fig. 6b).
Fig. 6.
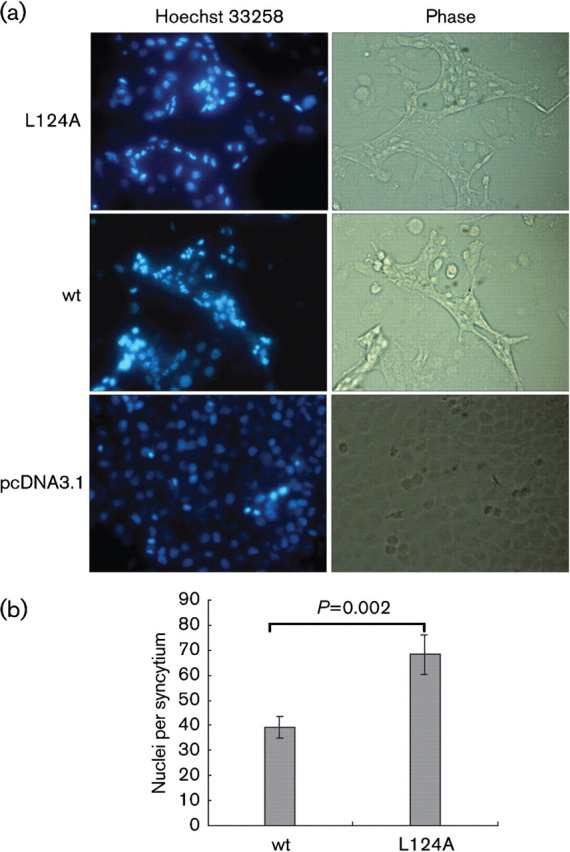
NiV-glycoprotein-mediated cell-to-cell fusion in HeLa-USU cells transfected with wt or L124A mutant ephrin-B2. (a) HeLa-USU cells were co-transfected with plasmids encoding NiV-F, NiV-G and the indicated ephrin-B2 genes. Cells were fixed 24h post-transfection and nuclei were visualized by Hoechst 33258 staining. Twenty randomly selected syncytia were photographed. (b) Syncytium formation in HeLa-USU cells expressing wt or mutant ephrin-B2 was measured by counting the mean number of nuclei per syncytium in 20 randomly selected syncytia. Data shown are the means of 20 syncytia±sem. Statistical analysis was performed by using Student’s t-tests with spss (version 13.0). Results where P<0.05 were considered to be significant.
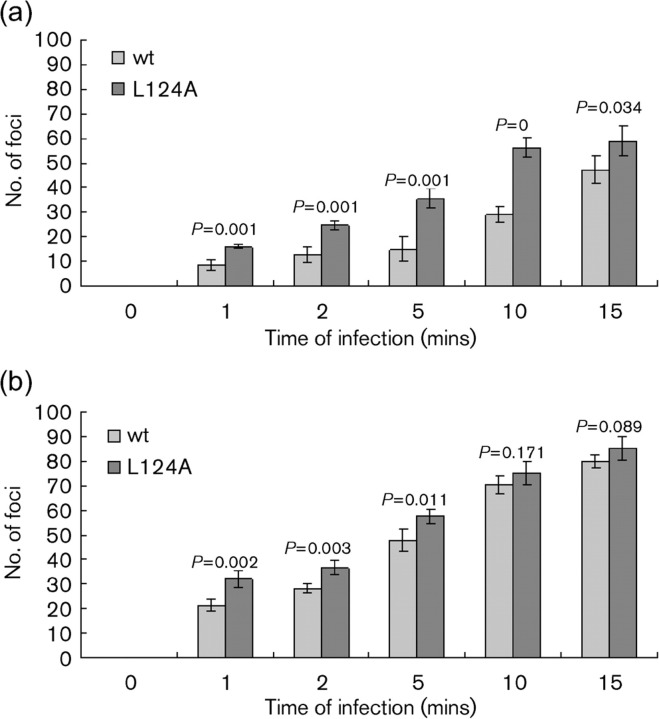
The L124A mutant enhances entry of infectious NiV and HeV
Infectious NiV or HeV were used to infect HeLa-USU cells, stably expressing either the wt or mutant L124A version of ephrin-B2. The entry and infection efficiency was determined by using a semi-quantitative immunofluorescence staining approach, which demonstrated a modest but significant (P<0.05) increase in virus infection of target cells expressing the L124A ephrin-B2, in comparison to those target cells expressing wt ephrin-B2, for both HeV and NiV at all time points, except 10 and 15 min for HeV (P<0.2) (Fig. 7). The enhancement was more pronounced when the time of incubation between infectious virus and the target cells was decreased, suggesting that the L124A mutant might provide a more rapid adsorption phase of henipavirus infection. We also noted that HeLa-USU cells expressing the mutant L124A-containing ephrin-B2 receptor resulted in larger staining foci when infected with NiV or HeV, which may also indicate a faster cell-to-cell spread of progeny virus.
Fig. 7.
Infection by NiV or HeV in HeLa-USU cells stably expressing wt (USU-hB2) or L124A mutant (USU-hB2 m) ephrin-B2. Cells were seeded at 20 000 cells per well 1 day before infection. Cells were infected with 500 TCID50 of NiV (a) or HeV (b) in 50 µl. Virus and cells were incubated for the time indicated on the x-axis and then virus was washed off by washing five times with PBS. DMEM+10 % FCS was added to wells and the cells were incubated for 24 h. Cells were then fixed and infected cells visualized by immunofluorescence by using polyclonal rabbit anti-HeV P antisera. Infected cell foci were counted microscopically (n = 4). Statistical analysis was performed by using Student’s t-tests with spss.
Discussion
The original aim of the present study was to identify the critical amino acid residues within the ephrin-B2 receptor that were important for NiV entry, and perhaps some that were also involved in its interaction with the NiV-G glycoprotein, while at the same time being of less importance for the Eph–ephrin-B2 interaction. Indeed, the identification of such residues could aid in the derivation of a potential therapeutic agent that could block virus while having little interaction with Eph receptors. Unexpectedly, however, no single alanine-substitution mutation within the G–H loop structure of ephrin-B2 could abrogate its NiVpp entry-supporting ability, indicating that multiple residues or elements within ephrin-B2 are important for its interaction with NiV-G. A possible explanation for the observed different sensitivities of any individual point mutation within the G–H loop towards either NiV-G and/or an Eph receptor is that the NiV-G–ephrin-B2 interaction may cover a more extensive interface than that of ephrin-B2–Eph receptor binding (Bowden et al., 2008).
However, although none of the single alanine-substitution mutants were able to abrogate NiV-G binding and virus infection, several single-site mutations within the G–H loop of ephrin-B2 were able to significantly enhance NiV entry. In particular, an L124A mutant of ephrin-B2 was able to enhance the infectivity of NiV pseudotypes >30-fold, and it also enhanced the entry of infectious NiV, not only in terms of the number of infection foci measured but also in the apparent kinetics of infection and the markedly enhanced size of the NiV-mediated syncytia that were formed. The clear difference in the fold-increase or fold-difference between the pseudotyped virus versus infectious virus results was because of the two very different assays. The pseudotyped virus infection and entry was determined by measuring the luciferase activity, and the live virus infection was determined by semi-quantitative immunofluorescence staining. The former is much more sensitive than the latter. However, the data from these two very different assays yielded the same trend; the effect of the mutation is increased virus infectivity.
Another single-site ephrin-B2 mutant, W125A, also exhibited an enhanced ability to support NiVpp infection. The double ephrin-B2 mutant, L124A/W125A, did not result in an additive or synergistic effect on virus infection, suggesting that the W125A mutation alone perhaps had a modulating effect on the binding and infection stage of the NiVpp in the context of the L124A mutation. A quantitative binding-affinity assay using bio-layer interferometry confirmed that NiV-G bound the L124A ephrin-B2 mutant with higher affinity compared with wt ephrin-B2. Taken together, our data demonstrate that the L124A mutation-containing ephrin-B2 molecule has a greater binding affinity to the henipavirus G glycoproteins, which in turn results in increased virus adsorption, entry and infection.
During the course of our study, the crystal structures of NiV-G bound to either ephrin-B2 or ephrin-B3 were reported (Bowden et al., 2008; Xu et al., 2008). These structural studies revealed that the contribution of ephrin-B2 to the binding interface in fact occurs overwhelmingly via the residues in, and surrounding, the G–H loop, which is consistent with our work with the two larger deletion mutants, hB2Δ117–131 and hB2Δ120–125, both of which lost their ability to support NiVpp entry. However, our data regarding enhanced entry by single alanine-substitution mutations of ephrin-B2 were unexpected and remarkable. The structural studies suggest that residues Leu124 and Trp125 of ephrin-B2 are in direct contact with residues Trp504 and Phe458 of NiV-G; however, alanine substitution of these residues (L124A or W125A) failed to reduce the overall binding of the two molecules; rather they enhanced NIV-G binding and virus entry. Although we have no definitive clues to account for the enhancement of the overall binding, one possible interpretation would be that substitution with an alanine residue eliminates some steric hindrance which may enhance the binding interaction between NiV-G and ephrin-B2. In a similar way, the change from L124/W125 to Y124/M125 might result in steric clashes (Negrete et al., 2006).
An alternative possibility is that the single alanine-substitution mutations actually increased the plasticity of the G–H loop region of ephrin-B2, resulting in an enhancement of overall binding affinity. From the structural studies reported, it was clear that binding of ephrin-B2 with either NiV-G or Eph receptor molecules required a conformational change to bind to the interacting molecule (Bowden et al., 2008). In this context, it is plausible to consider that amino acid changes leading to increased plasticity of the G–H loop could have a positive effect on the overall binding affinity.
Further studies will be required to determine whether a mutant ephrin-B2 variant with an even higher affinity can be derived from the lead molecules obtained in this study or whether the enhanced binding with NiV-G of such receptor mutants will have the opposite effect, i.e. reduced binding towards Eph receptors. If such ephrin-B2 mutants could be identified, they might be attractive candidates for the development of novel anti-henipavirus therapeutics, serving as henipavirus inhibitors that will not engage or impact Eph receptor function.
Methods
Cell lines and antibodies.
293T human embryonic kidney cells were maintained in Dulbecco’s modified Eagle’s medium supplemented with 10 % FCS (DMEM-10) at 37 °C in a humidified 5 % CO2 atmosphere. HeLa-USU cells have been described previously (Bonaparte et al., 2005). Spodoptera frugiperda (Sf9) cells were grown in Grace's insect medium (Invitrogen) containing 10 % (v/v) FBS (Gibco), 0.1 mg streptomycin ml−1 and 100 U penicillin ml−1 (Invitrogen). The rabbit polyclonal antibody, which recognizes NiV-P, was produced at the Australian Animal Health Laboratory.
Mutagenesis of ephrin-B2.
The ephrin-B2 gene was amplified from 293T cells based on the human ephrin-B2 gene sequence (GenBank Accession no. NM004093) and cloned into a pcDNA3.1 vector (Invitrogen). All alanine-substitution mutations of the ephrin-B2 gene were generated by site-directed mutagenesis with a QuikChange mutagenesis kit (Stratagene) according to the manufacturer’s protocols. Two deletion mutants (hB2Δ120–125 and hB2Δ117–131) were generated by overlapping PCR. All mutations were confirmed by sequencing.
Establishment of wt and mutant ephrin-B2-expressing cell lines.
Cell lines expressing wt or mutant ephrin-B2 were established by using replication-defective retroviral gene-transfer systems (Stratagene) and by following the supplier’s protocols. Briefly, the ephrin-B2-encoding region was cloned into a retroviral vector, pFB vector, and then co-transfected with pVPack-GP and pVpack-VSV-G into 293T cells to generate infectious virus particles that carry the gene of interest. Replication-defective virus was used to transduce HeLa-USU, and positive clones were selected by neomycin selection. The stable expression of ephrin-B2 in the transduced HeLa-USU cells was confirmed by immunofluorescence.
Construction and purification of NiV pseudotypes.
NiV-F and -G glycoprotein-bearing pseudotyped particles (NiVpp) were produced by co-transfecting plasmids expressing wt NiV-G and -F and the envelope glycoprotein-deficient HIV-1 backbone plasmid pNL4-3-Luc-E−R+ into 293T cells (Khetawat & Broder, 2010). A ratio of 8 µg of NiV-G : 2 µg of NiV-F : 10 µg of pNL4-3-Luc-E−R+ DNAs was used to transfect 293T cells (40–60 % confluent) in 10 cm dish plates with a ProFection Mammalian Transfection System (calcium phosphate; Promega). Culture supernatants containing pseudovirus were collected 48 h post-transfection and filtered through a 0.45 µm-pore filter (Pall). NiV pseudotypes in the cell supernatant (4 ml) were purified by ultracentrifugation through a 20 % sucrose cushion (4 ml) at 55 000 g for 60 min in a Ty90 rotor (Beckman). The pelleted pseudovirions were resuspended in 100 µl of PBS (pH 7.2) and stored at −80 °C in aliquots. A single virus stock was used for all infection assays.
Assessment of ephrin-B2 mutant-mediated infection.
HeLa-USU cells (2×104 cells) were grown in 96-wells plates and transfected with expression plasmids encoding either the wt or mutant ephrin-B2 protein. Each well was transfected with 0.2 µg of plasmid using Lipofectamine 2000 (Invitrogen). For infection, 2 µl of purified pseudovirus mixed with 28 µl of medium was added to the target cells. The mixture was removed and replaced with fresh medium at 3 h p.i. The infection was monitored by measuring the luciferase activity, expressed from the reporter gene carried by the pseudovirus, by using a Luciferase Assay System (Promega). Briefly, cells were lysed at 48 h p.i. by adding 30 µl of the lysis buffer provided with the kit, and 10 µl of the resulting lysate was tested for luciferase activity by the addition of 20 µl of luciferase substrate in a Turner Designs TD-20/20 luminometer (Promega). Each infection experiment was conducted in triplicate, and all experiments were repeated three times.
Kinetics of viral entry.
To compare the kinetics of pseudovirus entry mediated by wt or mutant ephrin-B2, pseudoviruses were adsorbed to cells at the indicated times and/or temperatures for 1 h. The inoculum was removed and washed with PBS, and infected cells were transferred to 37 °C after being replaced with fresh culture medium. Luciferase activity was measured at 48 h p.i. as described previously.
Bio-layer interferometry.
Recombinant wt or mutant ephrin-B2 proteins were expressed in Sf9 insect cells using a Bac-to-Bac baculovirus expression system (Invitrogen) according to the product manual. Soluble NiV glycoprotein G (sNiV-G) was expressed using recombinant vaccine virus (vKB-22) and purified through an S-protein agarose affinity column (EMD Biosciences) as described previously (Chan et al., 2009). An Octet RED platform (ForteBio) was used to perform binding affinity kinetics experiments. Briefly, streptavidin-coated sensor tips (Fortebio) were used to capture biotinylated sNiV-G onto the surface of the sensor. After reaching baseline, sensors were moved to the association step containing the indicated concentrations of wt or mutant ephrin B2 diluted with kinetics buffer for 30 min and then dissociated for 30 min at 25 °C. A buffer-only reference was subtracted from all curves. Dissociation constants K D, K on (association rate) and K off (dissociation rate) were determined by fitting binding chromatogram data with the Octet User Software (version 3.1).
Western blotting.
Lysates of target cells or pelleted pseudovirions were separated by SDS-PAGE (10 % polyacrylamide gels), followed by transfer to a PVDF membrane (Millipore). For Western blotting, incubation with different antibodies was done at 37 °C for 1 h. Expression of ephrin-B2 mutants in HeLa-USU cells was detected using a goat anti-mouse ephrin-B2 antibody as a primary antibody (R&D Systems), followed by incubation with HRP-conjugated donkey anti-goat IgG (1 : 20000) (PTGLab). Detection was achieved using a chemiluminescent substrate (SuperSignal; Pierce).
Immunoflorescence assays for ephrin-B2 molecules.
HeLa-USU cells were seeded in 24-well dishes on coverslips. At 24 post-transfection, cells were fixed with 5 % formaldehyde for 10 min at room temperature. Cells were incubated with PBS containing 1 % BSA (w/v) for 30 min at 37 °C, and then incubated with goat anti-mouse ephrin-B2 antibody at a dilution of 1 : 100 for 1 h at 37 °C. After washing with PBS, cells were incubated with FITC-labelled donkey anti-goat IgG at a dilution of 1 : 100 for 30 min at 37 °C. For nuclear staining, cells were incubated with Hoechst 33258 for 5 min. After washing three times, coverslips were mounted on slides with Aqua-PolyMount (Polysciences) and observed under a confocal microscope (Leica).
Flow cytometry.
HeLa-USU cells were transfected with wt or mutant ephrin-B2 expression plasmids. Twenty-four hours post-transfection, 106 cells were detached with PBS containing 5 mM EDTA, washed twice with PBS and subsequently incubated with goat anti-mouse ephrin-B2 antibody for 30 min on ice, followed by washing and staining with FITC-conjugated anti-goat IgG for 30 min at 4 °C. The cells were then washed again with PBS and fixed with 2 % paraformaldehyde, and the data were collected by using a BD FACScalibur (Becton Dickinson).
Fusion assays.
To address the ability of wt or mutant ephrin-B2 molecules to support NiV glycoprotein-mediated cell-to-cell fusion, HeLa-USU cells were contransfected with plasmids encoding the NiV-F and -G proteins at a ratio of 1 : 5, respectively, in addition to the plasmid encoding wt or mutant ephrin-B2 as described previously (Thiel et al., 2008). At 24 h post-transfection, cells were fixed with 4 % formaldehyde for 10 min and incubated with Hoechst 33258 for 5 min to stain the nuclei. Representative microscopic fields were photographed. To quantify the size of syncytia, the number of nuclei per syncytium of twenty randomly chosen syncytia were counted and averaged. Statistical analysis was performed using Student’s t-tests with spss (version 13.0).
HeV and NiV infection and immunofluorescence assay.
All infectious virus experiments were conducted under strict bio-containment procedures in the biological safety level 4 (BSL-4) laboratory at the Australian Animal Health Laboratory. Cells were seeded at 20 000 cells per well on the day before infection. A volume of 50 µl containing 500 TCID50 of NiV (Malaysia virus stock) or HeV (1994 isolate) was added to each well of HeLa-USU monolayers. All infections were done in DMEM-10 in a total volume of 150 µl per well and were incubated overnight at 37 °C in a humidified 5 % CO2 atmosphere. The culture medium was discarded the next day, and plates were immersed in ice-cold absolute methanol for 20 min prior to air-drying outside the BSL-4 laboratory. Infected cells were detected by immunofluorescence by using an anti-henipavirus phosphoprotein antiserum and were viewed as previously described (Bonaparte et al., 2005; Bossart et al., 2008).
Acknowledgements
This work was funded by the State Key Program for Basic Research Grant (2010CB530100, 2011CB504700) from the Chinese Ministry of Science and Technology.
References
- Bishop K. A., Stantchev T. S., Hickey A. C., Khetawat D., Bossart K. N., Krasnoperov V., Gill P., Feng Y. R., Wang L., et al. Identification of Hendra virus G glycoprotein residues that are critical for receptor binding. J Virol. 2007;81:5893–5901. doi: 10.1128/JVI.02022-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonaparte M. I., Dimitrov A. S., Bossart K. N., Crameri G., Mungall B. A., Bishop K. A., Choudhry V., Dimitrov D. S., Wang L. F., et al. Ephrin-B2 ligand is a functional receptor for Hendra virus and Nipah virus. Proc Natl Acad Sci U S A. 2005;102:10652–10657. doi: 10.1073/pnas.0504887102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bossart K. N., Broder C. C. Paramyxovirus entry. In: Pöhlmann S., Simmons. G., editors. Viral Entry into Host Cells. Austin, TX: Landes Bioscience; 2009. Edited by. [Google Scholar]
- Bossart K. N., Tachedjian M., McEachern J. A., Crameri G., Zhu Z., Dimitrov D. S., Broder C. C., Wang L. F. Functional studies of host-specific ephrin-B ligands as Henipavirus receptors. Virology. 2008;372:357–371. doi: 10.1016/j.virol.2007.11.011. [DOI] [PubMed] [Google Scholar]
- Bowden T. A., Aricescu A. R., Gilbert R. J., Grimes J. M., Jones E. Y., Stuart D. I. Structural basis of Nipah and Hendra virus attachment to their cell-surface receptor ephrin-B2. Nat Struct Mol Biol. 2008;15:567–572. doi: 10.1038/nsmb.1435. [DOI] [PubMed] [Google Scholar]
- Chadha M. S., Comer J. A., Lowe L., Rota P. A., Rollin P. E., Bellini W. J., Ksiazek T. G., Mishra A. Nipah virus-associated encephalitis outbreak, Siliguri, India. Emerg Infect Dis. 2006;12:235–240. doi: 10.3201/eid1202.051247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan Y. P., Yan L., Feng Y. R., Broder C. C. Preparation of recombinant viral glycoproteins for novel and therapeutic antibody discovery. Methods Mol Biol. 2009;525:31–58, xiii. doi: 10.1007/978-1-59745-554-1_2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chua K. B., Bellini W. J., Rota P. A., Harcourt B. H., Tamin A., Lam S. K., Ksiazek T. G., Rollin P. E., Zaki S. R., et al. Nipah virus: a recently emergent deadly paramyxovirus. Science. 2000;288:1432–1435. doi: 10.1126/science.288.5470.1432. [DOI] [PubMed] [Google Scholar]
- Eaton B. T., Broder C. C., Middleton D., Wang L. F. Hendra and Nipah viruses: different and dangerous. Nat Rev Microbiol. 2006;4:23–35. doi: 10.1038/nrmicro1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein J. H., Prakash V., Smith C. S., Daszak P., McLaughlin A. B., Meehan G., Field H. E., Cunningham A. A. Henipavirus infection in fruit bats (Pteropus giganteus), India. Emerg Infect Dis. 2008;14:1309–1311. doi: 10.3201/eid1408.071492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field H. E., Breed A. C., Shield J., Hedlefs R. M., Pittard K., Pott B., Summers P. M. Epidemiological perspectives on Hendra virus infection in horses and flying foxes. Aust Vet J. 2007;85:268–270. doi: 10.1111/j.1751-0813.2007.00170.x. [DOI] [PubMed] [Google Scholar]
- Guillaume V., Aslan H., Ainouze M., Guerbois M., Wild T. F., Buckland R., Langedijk J. P. Evidence of a potential receptor-binding site on the Nipah virus G protein (NiV-G): identification of globular head residues with a role in fusion promotion and their localization on an NiV-G structural model. J Virol. 2006;80:7546–7554. doi: 10.1128/JVI.00190-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hickey A. C., Broder C. C. The mechanism of henipavirus fusion: examining the relationships between the attachment and fusion glycoproteins. Virol Sin. 2009;24:110–120. doi: 10.1007/s12250-009-3027-2. [DOI] [Google Scholar]
- Hsu V. P., Hossain M. J., Parashar U. D., Ali M. M., Ksiazek T. G., Kuzmin I., Niezgoda M., Rupprecht C., Bresee J., Breiman R. F. Nipah virus encephalitis reemergence, Bangladesh. Emerg Infect Dis. 2004;10:2082–2087. doi: 10.3201/eid1012.040701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iehlé C., Razafitrimo G., Razainirina J., Andriaholinirina N., Goodman S. M., Faure C., Georges-Courbot M. C., Rousset D., Reynes J. M. Henipavirus and Tioman virus antibodies in pteropodid bats, Madagascar. Emerg Infect Dis. 2007;13:159–161. doi: 10.3201/eid1301.060791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khetawat D., Broder C. C. A functional henipavirus envelope glycoprotein pseudotyped lentivirus assay system. Virol J. 2010;7:312. doi: 10.1186/1743-422X-7-312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luby S. P., Hossain M. J., Gurley E. S., Ahmed B. N., Banu S., Khan S. U., Homaira N., Rota P. A., Rollin P. E., et al. Recurrent zoonotic transmission of Nipah virus into humans, Bangladesh, 2001-2007. Emerg Infect Dis. 2009;15:1229–1235. doi: 10.3201/eid1508.081237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murai K. K., Pasquale E. B. ‘Eph’ective signaling: forward, reverse and crosstalk. J Cell Sci. 2003;116:2823–2832. doi: 10.1242/jcs.00625. [DOI] [PubMed] [Google Scholar]
- Murray K., Selleck P., Hooper P., Hyatt A., Gould A., Gleeson L., Westbury H., Hiley L., Selvey L., et al. A morbillivirus that caused fatal disease in horses and humans. Science. 1995;268:94–97. doi: 10.1126/science.7701348. [DOI] [PubMed] [Google Scholar]
- Negrete O. A., Levroney E. L., Aguilar H. C., Bertolotti-Ciarlet A., Nazarian R., Tajyar S., Lee B. EphrinB2 is the entry receptor for Nipah virus, an emergent deadly paramyxovirus. Nature. 2005;436:401–405. doi: 10.1038/nature03838. [DOI] [PubMed] [Google Scholar]
- Negrete O. A., Wolf M. C., Aguilar H. C., Enterlein S., Wang W., Mühlberger E., Su S. V., Bertolotti-Ciarlet A., Flick R., Lee B. Two key residues in ephrinB3 are critical for its use as an alternative receptor for Nipah virus. PLoS Pathog. 2006;2:e7. doi: 10.1371/journal.ppat.0020007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Negrete O. A., Chu D., Aguilar H. C., Lee B. Single amino acid changes in the Nipah and Hendra virus attachment glycoproteins distinguish ephrinB2 from ephrinB3 usage. J Virol. 2007;81:10804–10814. doi: 10.1128/JVI.00999-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pernet O., Pohl C., Ainouze M., Kweder H., Buckland R. Nipah virus entry can occur by macropinocytosis. Virology. 2009;395:298–311. doi: 10.1016/j.virol.2009.09.016. [DOI] [PubMed] [Google Scholar]
- Reynes J. M., Counor D., Ong S., Faure C., Seng V., Molia S., Walston J., Georges-Courbot M. C., Deubel V., Sarthou J. L. Nipah virus in Lyle’s flying foxes, Cambodia. Emerg Infect Dis. 2005;11:1042–1047. doi: 10.3201/eid1107.041350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiel L., Diederich S., Erbar S., Pfaff D., Augustin H. G., Maisner A. Ephrin-B2 expression critically influences Nipah virus infection independent of its cytoplasmic tail. Virol J. 2008;5:163. doi: 10.1186/1743-422X-5-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wacharapluesadee S., Lumlertdacha B., Boongird K., Wanghongsa S., Chanhome L., Rollin P., Stockton P., Rupprecht C. E., Ksiazek T. G., Hemachudha T. Bat Nipah virus, Thailand. Emerg Infect Dis. 2005;11:1949–1951. doi: 10.3201/eid1112.050613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu K., Rajashankar K. R., Chan Y. P., Himanen J. P., Broder C. C., Nikolov D. B. Host cell recognition by the henipaviruses: crystal structures of the Nipah G attachment glycoprotein and its complex with ephrin-B3. Proc Natl Acad Sci U S A. 2008;105:9953–9958. doi: 10.1073/pnas.0804797105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yob J. M., Field H., Rashdi A. M., Morrissy C., van der Heide B., Rota P., bin Adzhar A., White J., Daniels P., et al. Nipah virus infection in bats (order Chiroptera) in peninsular Malaysia. Emerg Infect Dis. 2001;7:439–441. doi: 10.3201/eid0703.017312. [DOI] [PMC free article] [PubMed] [Google Scholar]