Abstract
Background
The aim of the study was to present the PET/CT imaging features in a small series of asymptomatic patients with known cancer pathologies, infected with the SARS-CoV-2 virus, which were incidentally discovered during their monitoring scan of F18-FDG PET/CT.
Methods
We included in our study a number of five cases (3 female and 2 male) out of 478 patients examined by F18-FDG PET/CT between March – April 2020, with confirmed diagnostic of cancer. Four patients had lung damages suggestive for the mentioned viral infection and 1 patient had multiple lung metastases from thyroid cancer. All patients were asymptomatic for acute respiratory disease at the time of examination, being subsequently confirmed for the viral infection by specific PCR analysis.
Results
The asymptomatic positive SARS-CoV-2 cancer patients discovered incidentally in PET/CT F18-FDG represent 0.83% and their imaging characteristics were suggestive for high FDG activity in the lung despite the lack of respiratory symptoms.
Conclusion
The SARS CoV-2 viral infection in asymptomatic cancer patients is a very rare possibility, but represents a challenging scenario both for the differential diagnosis in cancer and also for the epidemiologic context.
Keywords: COVID; 19, cancer patients, F18-FDG PET/CT, asymptomatic
Background and aims
A coronavirus is any virus belonging to the family Coronaviridae. In late 2019 a virus apparently closely related to already known SARS (Severe Acute Respiratory Syndrome) coronavirus that causes a highly contagious respiratory disease, emerged in Wuhan, China and was named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1]. By early 2020, it had spread throughout regions of China and had reached the Europe and United States, when WHO declared the outbreak a pandemic [2]. People with COVID–19 disease have reported a wide range of manifestations, from mild symptoms to severe illness, which could appear within 2–14 days after exposure to the virus. The main symptoms are: cough, shortness of breath or difficulty breathing, fever, chills, muscle pain, sore throat, loss of taste or smell [3]. Less common manifestations have been reported, including gastrointestinal symptoms like nausea, vomiting, or diarrhea [3]. Like other respiratory illnesses, COVID–19, can cause lasting lung damage. In COVID–19 pneumonias, the lungs become filled with fluid and inflamed, leading to breathing difficulties. The pneumonia tends to take hold in both lungs. While most people recover from pneumonia without any lasting lung damage, the pneumonia associated with COVID–19 may be severe. Even after the infection has passed, lung injury may result in breathing difficulties that might take months to improve [3,4]. An important number of subjects remain asymptomatic, despite the presence of the virus in organism. A particular situation is the occurrence of SARS-CoV-2 viral infection in cancer patients. Some cancer patients have a fragile immune system due to oncologic therapy or to the cancer itself. Patients with hematologic cancers, after bone marrow transplants, or those actively receiving chemotherapy or radiotherapy are at higher risk of immune deficiency. The UK Coronavirus Cancer Monitoring Project published in Lancet Oncology [5] that patients with specific types of cancer might be at an increased risk of COVID–19, with reports highlighting the high proportion of patients with lung cancer who are at a higher risk of developing severe complications following their infection by SARS-CoV-2 [6–8]. The role of F18-fluorodeoxyglucose positron emission tomography/computed tomography (F18-FDG PET/CT) is not yet well established in COVID–19 disease [9–16], but its fundamental role in the initial diagnosis, staging, prognosis, response evaluation and follow-up in cancer disease is well known and well established. Recent studies have found a potential role of F18-FDG PET/CT in the evaluation of positive patients during recovery [17].
The aim of this study is to analyze the incidental findings of COVID–19 in asymptomatic cancer patients evaluated by F18-FDG PET/CT; due to the fact that this pandemic situation of COVID–19 is a new scenario in our daily practice, the authors would also like to raise the attention about the issue of asymptomatic cancer patients referred for PET/CT investigations, as a potential source of infection for the medical staff.
Patients and methods
We analyzed retrospectively the F18-FDG PET/CT scans performed in a tertiary center between March–April 2020. A number of 478 patients were evaluated for different types of cancer during their oncologic protocol. Inclusion criteria: confirmed cancer, indication for PET/CT in initial staging, follow-up, monitoring of the treatment response. Exclusion criteria: none of these patients were symptomatic for an acute respiratory disease and all of them passed through an epidemiologic screening including: clinical data, information about a possible contact with an infected person, travel in known COVID–19 areas. All patients presenting fever, cough, shortness of breath or respiratory distress, thoracic pain or hemoptysis, symptoms that might be attributed to lung cancer, lung metastases or to viral lung infections, were not sent for investigation in the PET/CT center, the examination being postponed, until the status for SARS-CoV-2 infection was established. All patients with any acute respiratory symptoms were excluded from the study. All patients signed the informed consent for the evaluation and for using their medical data for scientific purposes. All patients were investigated by the same protocol. The F18-FDG PET/CT was performed on a GE Optima 560 equipment, with the following protocol: patient fasted for at least 6 h, serum glucose level ≤180 mg/dL, an activity of 2.3 MBq/kg body weight of F18-FDG was injected intravenously; the images were acquired at 50–60 min after tracer administration. The scan parameters of a low-dose CT were as follows: 110–130 kV, 80–100 mA; in the PET sequence we used 2.5 min/bed acquisition time; 4–8 beds were acquired, with the standardized uptake value (SUV) expressed in lean body mass (SUVlbm) as maximum uptake value (SUVlbm max). The results were interpreted by a nuclear medicine physician and an experimented radiologist; among the 478 asymptomatic patients we found 4 patients with pathologic lung imaging with highly suspicion for SARS-CoV-2 pneumonia and 1 patient with multiple lung metastases from thyroid cancer, who were tested positive for specific virus infection, by real-time PCR (RT-PCR) ARN 2019-nCoV. The analyses were performed on two systems: a) MagnaPure LC 2.0 and Light Cycler 480/Z480 devices with kit IVD-CE; the detection limit being 80 copies ARN for gene E and 30 copies for gene RdRP and b) on kit ELI COVID 19 Basic ART (Ref 90077-RT).
Results
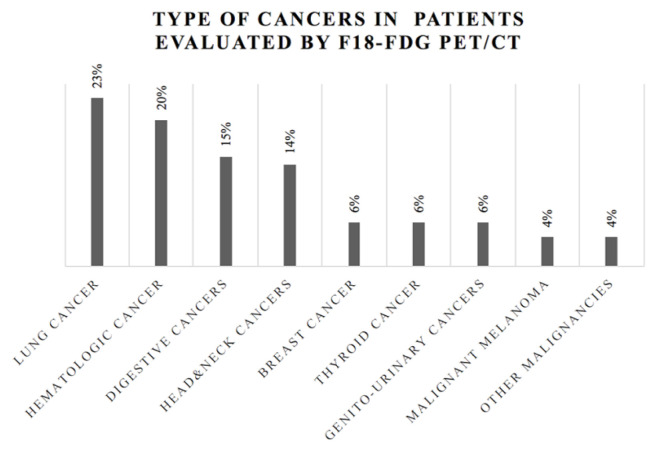
The cancer patients scanned between March and April 2020 have the distribution according to their oncologic pathology, presented in figure 1. Among the patients there were 4 (four) subjects (0.83%) discovered with lung damage highly suspicious for COVID–19 diseases and 1 patient with lung metastases from thyroid cancer, who was tested positive one day after the PET/CT, before starting the systemic oncologic therapy (case 3). No other suspicion lesions for viral pneumonia were seen in the rest of patients. The main characteristics of these patients are presented in table I.
Figure 1.
Distribution of patients evaluated by F18-FDG PET/CT according to the cancer type, in the period March–May 2020.
Table I.
Main characteristics of patients found with lung damages highly suspicious for COVID–19 infection.
| No | Age (years-old)/Gender | Cancer type | Indication PET/CT | Basal temperature* | Recent therapies** | Other medical conditions |
|---|---|---|---|---|---|---|
| 1 | 38/F Case 1 |
Nasopharyngeal carcinoma | Initial evaluation | 36.3° C | Yes RT |
None |
| 2 | 70/M Case 2 |
Maxillary sinus carcinoma | Restaging | 36.8° C | Yes RT, CHT |
DM |
| 3 | 64/F Case 3 |
Follicular thyroid carcinoma | Follow-up | 36.4° C | Yes RIT |
HTA hTir |
| 4 | 65/F Case 4 |
Rectal carcinoma | Follow-up | 37° C | No | HTA |
| 5 | 70/F Case 5 |
Breast carcinoma | Follow-up | 36.2° C | No | DM, HTA |
DM-diabetes mellitus; HTA-arterial hypertension; hTir-hypothyroidism treated with hormones substitutions;
– basal body temperature measured at the moment of performing F18-FDG PET/CT, measured in Celsius degrees;
– chemotherapy (CHT), external beam therapy (RT), radioiodine therapy in the last 3 months.
According to the data presented in table I, the majority of patients were female, 4, and only 1 male, the mean±SD age was 61.4±11.95 years and among the primary cancer pathologies, 2 were with head and neck cancers (nasopharyngeal and maxillary sinus cancers).
We would like to underline the observation that 2 out 5 patients had associated diabetes mellitus, 3 out of 5 had high blood pressure and one had associated hypothyroidism due to total thyroidectomy and radioiodine therapy.
The five cases are presented with their results of F18-FDG PET/CT scans in figure 2, figure 3, figure 4, figure 5 and figure 6.
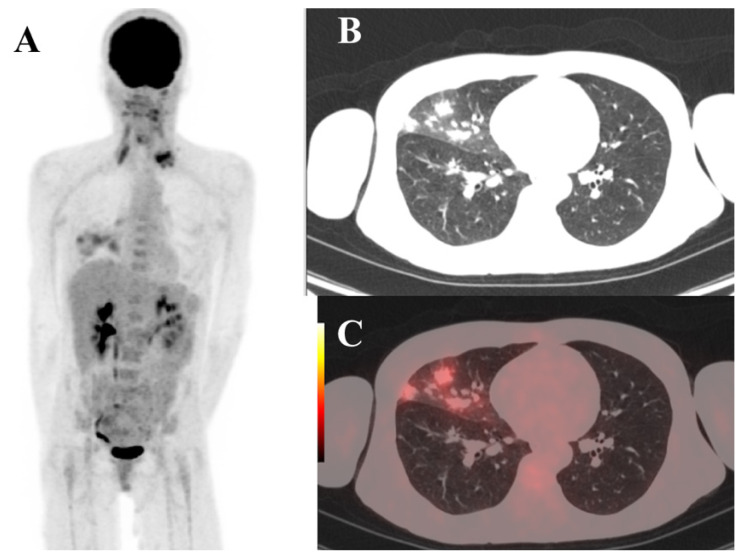
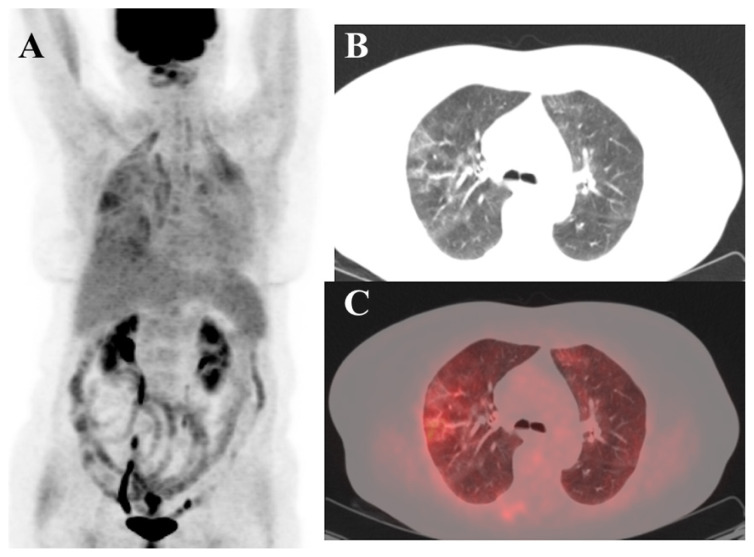
Figure 2.
Case 1. F18-FDG PET/CT scan images. MIP view (A) in a patient with nasopharyngeal cancer with pathologic F18-FDG uptake in left supraclavicular lymph nodes and in the right middle lung lobe. The CT axial view (B) revealed multiple lesions of “ground glass” in right middle lobe of the lung. The fused PET/CT axial section (C) shows high uptake of F18-FDG the right middle lobe lesions.
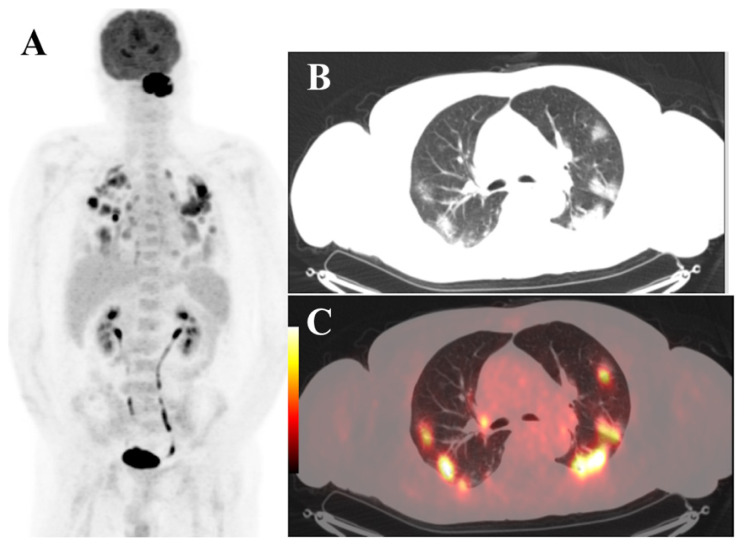
Figure 3.
Case 2. F18-FDG PET/CT scan images. MIP view (A) in a patient with left maxillary sinus cancer with pathologic F18-FDG uptake in the maxillary sinus and both lungs. The CT axial view (B) revealed multiple lesions of “ground glass” lesions that were diffusely disseminated in both lungs. The fused PET/CT axial section (C) is showing high uptake of F18-FDG in the lesions described in the lungs.
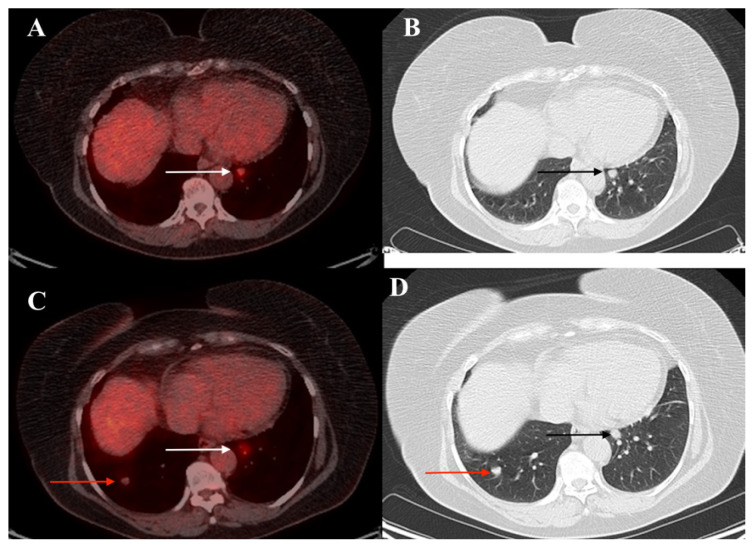
Figure 4.
Case 3. Axial F18-FDG PET/CT view (A) and axial CT view (B) in a patient with radically treated follicular thyroid carcinoma (total thyroidectomy and radioiodine therapy) with pathologic F18-FDG uptake in metastatic nodule in left lung, image from 10/05/2018 (white and black arrows). The fused PET/CT axial section (C) and the axial CT view (D) show, after 2 years of follow-up, in 16/04/2020, the increasing of the known metastatic left lung nodule with F18-FDG uptake and the presence in the right lung of a second nodule with minimally increased F18-FDG uptake in the lesion (red arrows). No lesions of “ground glass” are seen.
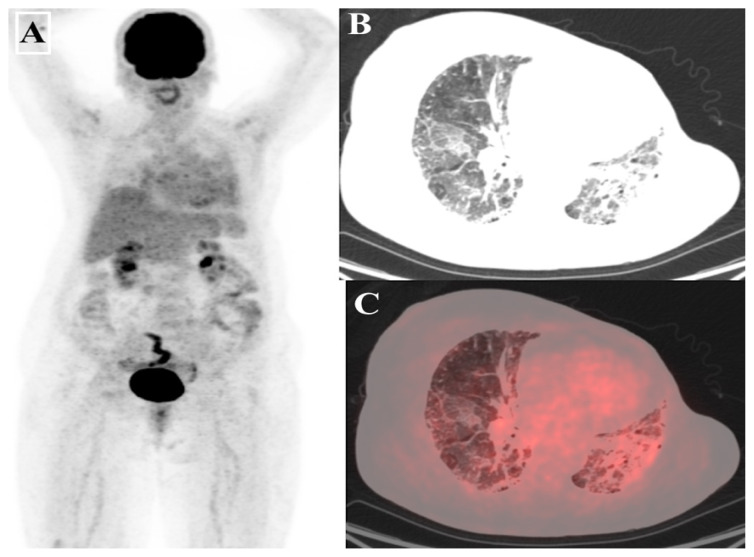
Figure 5.
Case 4. F18-FDG PET/CT scan images. MIP view (A) in a patient with rectal carcinoma during the initial staging, with pathologic F18-FDG uptake in rectal area suggestive for rectal malignant disease and also pathologic bilateral lungs uptake. The axial CT view (B) revealed multiple focal “ground glass” lesions diffusely disseminated in both lungs. The fused PET/CT axial section (C) shows slightly increased uptake of F18-FDG in the pulmonary lesions.
Figure 6.
Case 5. F18-FDG PET/CT scan images. MIP view (A) in a patient with left breast carcinoma, with radical mastectomy, during the follow-up, with pathologic F18-FDG bilateral in the lungs. The axial view CT (B) revealed multiple focal “ground glass” lesions diffusely disseminated in both lungs suggestive for an aspect of “crazy paving” and also important lung fibrosis associated with the radiotherapy. The fused PET/CT axial section (C) shows minimal increased uptake of F18-FDG in the pulmonary lesions.
In the present case is important to underline that lesions are mainly located in the right middle lobe, not bilateral, as the majority of authors have reported at that time; the standardized uptake value (SUVlbm) was 3.24, not significantly increased. Recently published recommendations [18,19] and also the specific guidelines have suggested that this possibility of occurrence is not very rare [20,21] (Figure 2).
The SUVlbm max in the lung lesions was 6.8, significantly increased. The lesions were disseminated mainly subpleurally in both lungs, and were associated with metastatic nodules, that were already known in this patient from previous examinations (Figure 3).
The uptake in the lung lesions was significantly increased SUVlbm max being 3.8 (Figure 5).
In this case, the lung fibrosis caused by radiotherapy was difficult to be differentiated from the aspect of “ground glass” due to viral infection; the F18-FDG uptake SUVlbm max was 3.7 (Figure 6).
All patients were referred to dedicated COVID–19 medical units and started the combined treatment with azithromycin and chloroquine, the oncological treatments being postponed. All patients are alive and under medical observation.
Discussion
The COVID–19 is a highly contagious respiratory disease [1–4] and due to the fact that the serial screening by PCR-RT tests was almost impossible in large groups, since March 2020 until end April, an important number of subjects without a known epidemiologic course of exposure, were positive and asymptomatic, being a source of infection.
As other authors described [9,10,18–21], the cases are characterized by the presence of peripheral “ground glass” lesions and/or consolidative opacities in more than two pulmonary lobes and all of these lesions showed a high tracer uptake, rarely being possible that the changes occur only in one lobe, as we described in figure 2. Also, the association with lung fibrosis and lung nodules suggestive for metastasis make the diagnosis even more difficult. The F18-FDG uptake was not in all cases very increased. The mean ± SD SUVlbm max was 4.18±1.32 (min 3.24 and max 6.8). We note that there was no dissemination in other organs that might be attributed to COVID–19, fact similar mentioned by other authors [10,12,15].
The cases with head and neck cancers were 2 out 5 positive patients; the risk factors in head and neck cancer patients, like smoking, male gender and age over 40 years-old are also risk factors involved in COVID-19 disease [3,22]. Also, very important from the clinical point of view is the fact that despite the severe lung damage, there were no symptoms, no specific recent changes in the clinical status of these patients and they did not express any other complaints that might be suggestive for the occurrence of another severe disease.
Even if F18-FDG PET/CT scan has no routine indication in an emergency setting and is generally not recommended for acute infection [9,21], our results shows that in cancer patients, where PET/CT is made on a regular basis, we need to pay special attention to the imaging work flow of these asymptomatic patients, taking into account that any image of suspicious lung damage needs to be urgently remitted to the referring physician with the recommendation of specific SARS-CoV-2 tests. The reports published on this topic in the recent months are still on small series [13], so any additional experience would improve our approach on this patients. Also, a special remark needs to be made for the possible contamination of healthcare staff. Because at the beginning of March 2020, the highly contagious potential of this category of patients was not reported and well documented, the PET/CT unit and the medical staff had no specific procedures regarding the epidemic viral context; the guidelines regarding the nuclear medicine procedures in case of suspected or positive SARS-Cov-2 patients have been published in May [21] and July [20]. Consequently, with the usual protection in a non-COVID–19 medical departments, the possibility of infection is high. Healthcare workers must use personal protective equipment (PPE) to shield themselves not only from radioactive sources, but also from droplets from coughs, sneezes or other body fluids from infected patients, and contaminated surfaces that might infect them. This new PPE were not common for nuclear medicine staff in PET/CT units. In this new pandemic situation, from our experience, for the nuclear medicine community we would like to raise a special attention, suggesting that in every unit of PET/CT any oncologic patient would be better to be tested before the examination and if is not, the staff should consider him as a possible positive person, taking all the necessary protective measures into consideration.
Conclusion
The SARS-CoV-2 viral infection in asymptomatic cancer patients is a rare possibility, but it represents a challenging scenario both for the diagnosis and also regarding the epidemiologic context. Our mission is to provide useful information to guide the management of patients with oncologic diseases, while keeping the patients and healthcare staff safe during the COVID-19 Pandemic.
Footnotes
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.Kobayashi KI, Kaki T, Mizuno S, Kubo K, Komiya N, Otsu S. Clinical Characteristics of Patients with Coronavirus Disease 2019 in Japan: A Single-Center Case Series. J Infect Dis. 2020;222:194–197. doi: 10.1093/infdis/jiaa244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO. Coronavirus disease (COVID–19) outbreak situation. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
- 3.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liang W, Guan W, Chen R, Wang W, Li J, Xu K, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21:335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.UK Coronavirus Cancer Monitoring Project team. The UK Coronavirus Cancer Monitoring Project: protecting patients with cancer in the era of COVID–19. Lancet Oncol. 2020;21:622–624. doi: 10.1016/S1470-2045(20)30230-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yu J, Ouyang W, Chua MLK, Xie C. SARS-CoV-2 Transmission in Patients With Cancer at a Tertiary Care Hospital in Wuhan, China. JAMA Oncol. 2020;6:1108–1110. doi: 10.1001/jamaoncol.2020.0980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, et al. Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern Med. 2020;180:934–943. doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gupta I, Rizeq B, Elkord E, Vranic S, Al Moustafa AE. SARS-CoV-2 Infection and Lung Cancer: Potential Therapeutic Modalities. Cancers (Basel) 2020;12:E2186. doi: 10.3390/cancers12082186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Treglia G. The role of 18F-FDG PET for COVID–19 infection: myth versus reality. Clin Transl Imaging. 2020:1–2. doi: 10.1007/s40336-020-00367-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Qin C, Liu F, Yen TC, Lan X. 18F-FDG PET/CT findings of COVID–19: a series of four highly suspected cases. Eur J Nucl Med Mol Imaging. 2020;47:1281–1286. doi: 10.1007/s00259-020-04734-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Halsey R, Priftakis D, Mackenzie S, Wan S, Davis LM, Lilburn D, et al. COVID-19 in the act: incidental 18F-FDG PET/CT findings in asymptomatic patients and those with symptoms not primarily correlated with COVID-19 during the United Kingdom coronavirus lockdown. Eur J Nucl Med Mol Imaging. 2020:1–13. doi: 10.1007/s00259-020-04972-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Colandrea M, Gilardi L, Travaini LL, Fracassi SLV, Funicelli L, Grana CM. 18F-FDG PET/CT in asymptomatic patients with COVID-19: the submerged iceberg surfaces. Jpn J Radiol. 2020;38:1007–1011. doi: 10.1007/s11604-020-01006-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Scarlattei M, Baldari G, Silva M, Bola S, Sammartano A, Migliari S, Graziani T, et al. Unknown SARS-CoV-2 pneumonia detected by PET/CT in patients with cancer. Tumori. 2020;106:325–332. doi: 10.1177/0300891620935983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dietz M, Chironi G, Claessens YE, Farhad RL, Rouquette I, Serrano B, et al. COVID-19 pneumonia: relationship between inflammation assessed by whole-body FDG PET/CT and short-term clinical outcome. Eur J Nucl Med Mol Imaging. 2020:1–9. doi: 10.1007/s00259-020-04968-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mattoli MV, Taralli S, Pennese E, D’Angelo C, Angrilli F, Villano C. Atypical Presentation of COVID-19 Incidentally Detected at 18F-FDG PET/CT in an Asymptomatic Oncological Patient. Clin Nucl Med. 2020;45:e383–e385. doi: 10.1097/RLU.0000000000003175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kamani CH, Jreige M, Pappon M, Fischbacher A, Borens O, Monney P, et al. Added value of 18F-FDG PET/CT in a SARS-CoV-2-infected complex case with persistent fever. Eur J Nucl Med Mol Imaging. 2020;47:2036–2037. doi: 10.1007/s00259-020-04860-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fu C, Zhang W, Li H, Bai Y, Bae KT, Wang M, et al. FDG PET/CT evaluation of a patient recovering from COVID-19. Eur J Nucl Med Mol Imaging. 2020;47:2703–2705. doi: 10.1007/s00259-020-04958-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.American College of Radiology. ACR Recommendations for the use of Chest Radiography and Computed Tomography (CT) for Suspected COVID-19 Infection. Available from: https://www.acr.org/Advocacy-and-Economics/ACR-PositionStatements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection. Updated 2020, 22 March.
- 19.Societatea de Radiologie şi Imagistică Medicală din România. Recomandări privind practica radiologică în relaţie cu infecţia SARS-CoV 2. Available from: https://www.srimr.ro/covid19.
- 20.IAEA International Atomic Energy Agency. COVID-19 Pandemic: Technical Guidance for Nuclear Medicine Departments. Available from: https://www-pub.iaea.org/MTCD/Publications/PDF/COVID19_web.pdf.
- 21.Tulchinsky M, Osmany S. The American College of Nuclear Medicine Guidance on Operating Procedures for a Nuclear Medicine Facility During COVID-19 Pandemic. Clin Nucl Med. 2020 May 1; doi: 10.1097/RLU.0000000000003146. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Glastonbury CM. Head and Neck Squamous Cell Cancer: Approach to Staging and Surveillance. In: Hodler J, Kubik-Huch RA, von Schulthess GK, editors. Diseases of the Brain, Head and Neck, Spine: Diagnostic Imaging. Chapter 17. Cham (CH): Springer; 2020. pp. 2020–2023. [PubMed] [Google Scholar]