Mindfulness has become an increasingly popular clinical intervention for a host of psychological and medical disorders in adults, beginning with Kabat-Zinn’s (1982) study of a mindfulness-based program (MBP) for adults with chronic pain (Castellanos et al. 2020; Goldberg et al. 2018; Khoury et al. 2015; Lomas et al. 2019; McClintock et al. 2019; Turgon et al. 2019; Vonderlin et al. 2020). While the first MBPs for youth were not developed until several years later – resulting in far fewer studies than in adults – the literature is nevertheless increasing at a similar pace (Klingbeil et al., 2017). Figure 1 displays this impressive growth, reflecting PubMed-indexed publications on mindfulness in youth from 1980-2019.
Figure 1.
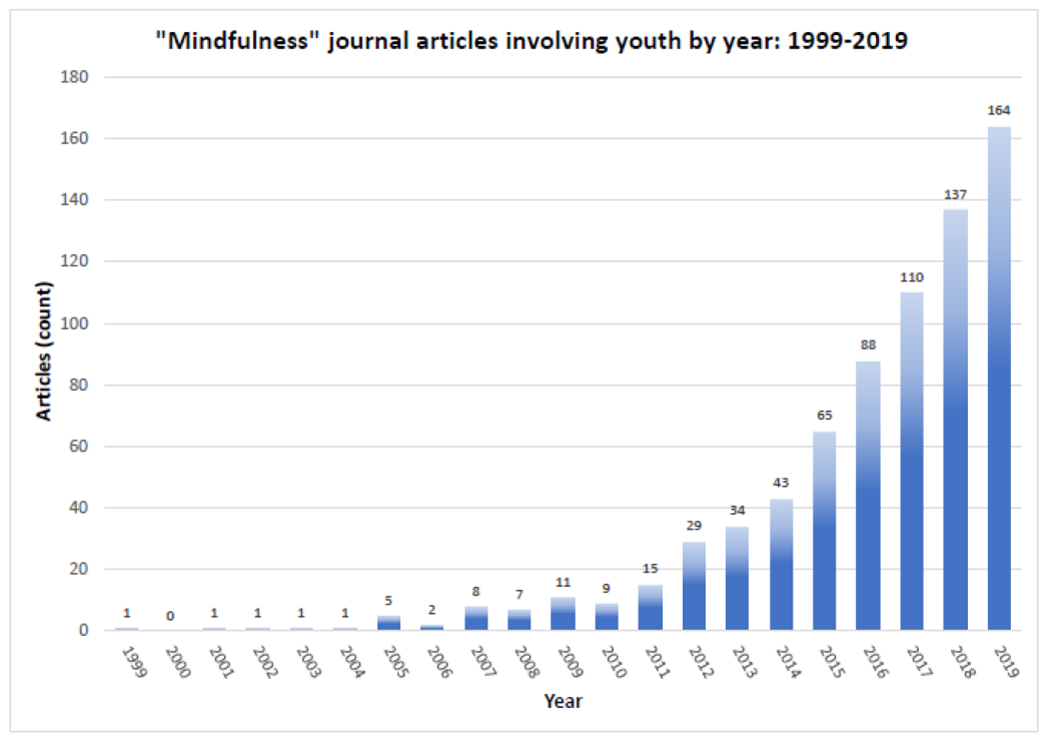
Child and Adolescent Mindfulness Publications by Year, 1981-2019.
However, public appetite for MBPs may outpace the evidence base (Davidson & Kaszniak 2015; Dimidjian & Segal 2015; Van Dam et al. 2018). Specifically, several recent reviews of mindfulness-based programs in children and adolescents have cited lack of methodological rigor as a chief concern, recommending more rigorous evaluation of existing MBP research methods and evidence-based development of future MBPs (Black 2015; Klingbeil et al. 2017; Saunders 2015; Zenner 2014). Consistently, in a “state-of-the-science review” of mindfulness training for children. Black (2015) concluded that high-quality evidence on mindfulness in young persons is sparse. The meta-analysis by Zoogman et al. (2015) noted that, while MBPs in youth may be promising, the average effect size is in the small to moderate range, and for school-based mindfulness programs in particular, Zenner et al. (2014) concluded that an accurate and precise assessment of the literature is difficult owing to profound heterogeneity of studies, underpowered sample sizes, and an absence of active controls. Altogether, MBPs in child and adolescent psychology and psychiatry (CAPP) may be promising, but both the quantity and quality of evidence is lacking at present. It therefore behooves researchers invested in the development of MBPs within CAPP to think critically about the methodological validity and utility of data from existing publications, the design and execution of current research projects, and the development of future studies. Indeed, new research in this area should address its many methodological shortcomings and conform to a set of more stringent methodological considerations in order to ensure that the quality of produced evidence improves.
Thus, the primary goal of this paper is to help CAPP researchers develop, evaluate, and disseminate MBPs specifically designed for pediatric populations based on rigorous methodological principles that are championed by the National Center for Complementary and Integrative Health (NCCIH) – the primary MBP funding agency in the United States – so as to improve the likelihood that their studies may be rigorous and fundable. The secondary, more distal goal is to cultivate a community of CAPP researchers committed to rigorously studying mindfulness in young persons, with the ultimate objective of benefiting children for many years to come. This is done in two steps. First, we review the “Framework for Developing and Testing Mind and Body Interventions” put forth by the NCCIH (hereafter, “NCCIH framework”; National Center for Complementary and Integrative Health 2017), which proposes six stages of treatment development, including methods for designing, collecting, analyzing, understanding, and interpreting data from treatment protocols. Second, based on our own success in obtaining funding for MBPs in CAPP through the NCCIH, we apply its principles to the unique needs of child and adolescent populations, offering specific and actionable research recommendations. As such, this paper is not a broad review of mindfulness research methodology, but rather, a focused and practical set of recommendations to CAPP researchers who may not be exposed to or familiar with the NCCIH framework.
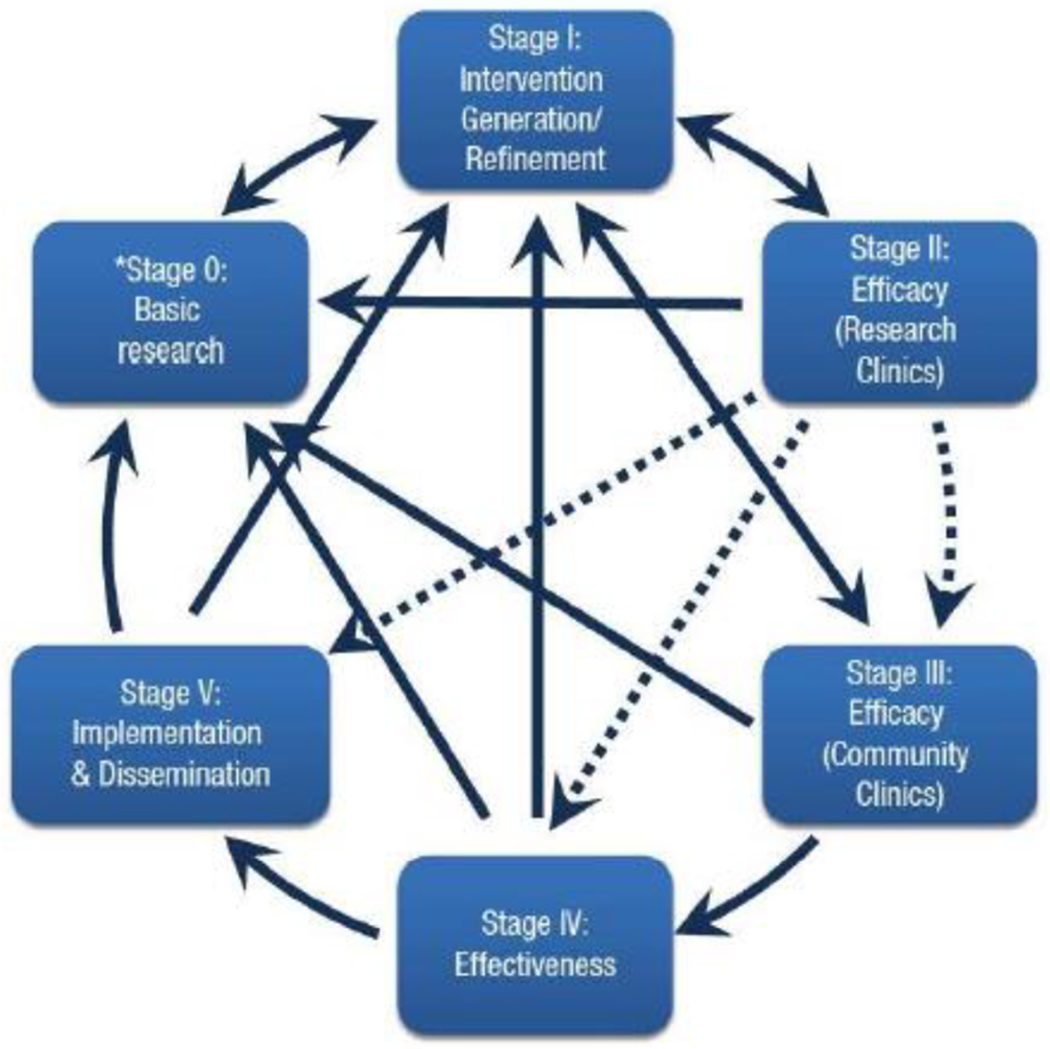
The NCCIH Framework for Developing and Testing Mind and Body Interventions:
The NCCIH framework values the notion that “work is not complete until an intervention reaches its highest level of potency and is implementable with the maximum nmnber of people in the population for which it was developed” (National Center for Complementary and Integrative Health 2017). The framework seeks to codify certain key principles in intervention development, execution, and dissemination – principles that serve as the foundation for research of the highest standard. The ultimate purpose, naturally, is to help researchers execute coherent and effective scientific investigation for the benefit of individual patients, communities, and society at large. The six stages that comprise the NCCIH framework are described in detail below (and see Figure 2).
Figure 2:

Framework for Developing and Testing Mind-Body Interventions. (National Center for Complementary and Integrative Health, 2017; reprinted with permission).
While the NCCIH framework partially overlaps with the more well-known National Institutes of Health “Stage Model for Behavioral Intervention Development” (hereafter, “NIH stage model”; Onken et al. 2014; Figure 2) and similar conceptual stages appear in both, the former is focused on for two reasons. First, and most importantly, because the NCCIH is the primary funding agency for mindfulness-based research in the United States. Given this, discussing their framework in detail, rather than the NIH stage model, and offering practical stage-by-stage recommendations, contributes to the literature by aiding CAPP researchers in designing studies that are more likely to be funded by the NCCIH. Second, the NCCIH framework is designed specifically for mind-body interventions, unlike the NIH stage model, perhaps motivating the development of their own model, and this focus has led to changes in the breakdown of stages. That said, the NIH stage model is referenced occasionally for several reasons. For example, the importance of the NIH stage model is already well-established in the field, therefore, noting its similarities with the much-newer NCCIH framework will legitimize the latter. Further, highlighting their similarities empowers researchers to design studies in accordance with the NCCIH framework – which is in their best interest if they are seeking funding from the NCCIH – with the assurance that it is sufficiently similar to the more well-known NIH stage model. Finally, highlighting differences between the two models can help researchers tailor their intervention development to the NCCIH model specifically when designing mind-body interventions, and when applying for funding from NCCIH. To illustrate their significant overlap, but occasional differences, please see Figure 3.
Figure 3:
National Institutes of Health Stage Model of Intervention Development (Onken et al., 2014; reprinted with permission).
Of note, neither the NIH stage model nor NCCIH framework is specific to research with children and adolescents. In fact, to our knowledge, there are no CAPP models for intervention development – certainly not for mind-body interventions. This paper therefore represents an attempt to provide tailored CAPP-specific recommendations in relation to the NCCIH model. As such, the paper might serve as a unique guide to CAPP researchers who want to develop mind-body interventions for young individuals, and who might hope to receive funding from NCCIH for this purpose. In fact, implementing many of the recommendations discussed below, we were recently successful in obtaining NCCIH funding for a novel clinical trial of an MBP for children and adolescents, and would like to share those insights with the reader so as to improve their chances of receiving funding for their own work on MBPs in young persons.
NCCIH Stage 1. Studies to Demonstrate Clinically Meaningful Signal
The first task of clinical researchers is to demonstrate that a MBP can produce a clinically meaningful effect. Tliis can be accomplished through several methods of investigation, namely: a case series, a small uncontrolled trial, or a retrospective chart review (among others). These methodologies can provide researchers with enough evidence that the possibility of a clinical benefit exists to justify further investigation. Importantly, Stage 1 studies do not “prove” that an intervention is effective, nor would negative findings eliminate the possibility of benefit. The essential goal of this first stage is simply to detennine whether further investigation on the outcome is warranted. While methodologically-weak studies are not recommended on the one hand, it would be wasteful to fully develop an intervention, and/or run full-scale clinical trials (and ultimately effectiveness trials) unless there exists at least minimal evidence that such an intervention may be helpful in the first place – evidence that is provided by studies in this first stage.
In contrast, an appealing feature of the NIH stage model is the presence of an antecedent to this stage that focuses on “basic research” (Stage 0), the goal of which is to “provide the basis for the generation of a new intervention or modification of an existing one” (Onken et al. 2014, p. 28). Motivating the inclusion of basic research – including the social, behavioral, cognitive, and neural/biological sciences – is the desire to initiate intervention development based on the mechanisms by which an intervention might exert its effects. In this way. Stage 0 of the NIH stage model provides an explicit platform for mechanism-based research. Within the NCCIH framework, however, the role of basic science is implicit in or before the first stage. In any case, basic research can and should have an important role in intervention development.
Interestingly, neither the NIH stage model nor the NCCIH framework emphasize the role of theory in intervention development at these stages; theory may be particularly salient for MBPs, which rest on a rich Buddhist theoretical context (Bodhi 2011; Dunne 2011; Harrington & Dunne 2015; Sharf 2015). Further, MBPs are not ahistorical phenomena and, as such, are also informed by other theoretical perspectives, including psychodynamic thought, cognitive-behavioral theory, and neuroscience (to name a few).
NCCIH Stage 2. Intervention Development, Refinement, and Standardization
Next in the NCCIH framework, researchers use the preliminary results from Stage 1 to further develop and refine the execution of the intervention for subsequent stages. Having determined that the intervention may reap some benefit (i.e., “clinically meaningful signal”) – and based on the theoretical underpinning of the intervention, as well as direct experience of teaching to a particular population in a given context – both intervention and study parameters are modified to produce an optimal benefit. Intervention variables that can be modified at this stage include “dosing,” frequency, and duration of the intervention, and various elements of its content (e.g., homework). Method of delivery and participant characteristics are also worth considering here, including the selection of an appropriate patient population and the mode of delivery (i.e., online, in person, in groups). Finally, specific outcomes and measurement tools are chosen, with the goal of generating the most robust (and clinically-relevant) signal.
Most of the published studies on MBPs in children and adolescents could be categorized as NCCIH Stage 2 research, and few MBPs for youth have progressed beyond Stage I of the NIH model, or Stage 2 of the NCCIH model. Indeed, there is a lacuna of rigorous, refined, standardized, and adequately-powered evaluations of MBPs in youth, even while some have masqueraded as efficacy studies (NCCIH Stage 4). This is an important distinction because the goal of Stage 2 is not to assess efficacy, but rather to codify and therefore standardize the intervention into a manual, such that the intervention can be reliably and consistently delivered with the highest fidelity in subsequent efficacy trials. Rigorous and systematic protocols also enable replication of the intervention, increasing the validity of any subsequent studies using it. If the ultimate goal of the intervention is to benefit the greatest nmnber of patients – and not just the cohort being tested at the time – this is arguably the most critical step in intervention development. Importantly, this second stage of the NCCIH framework represents only one part of Stage I of the NIH model, “Intervention Generation/Refmement.” Indeed, the second part of NIH Stage I includes feasibility and pilot studies, represented in NCCIH framework Stage 3, as described below.
NCCIH Stage 3. Feasibility and Pilot Studies
Stage 3 in this framework provides the first opportunity for researchers to test the intervention, as standardized in a protocol, in a veritable clinical trial. Outcomes of interest at this stage include acceptability of the intervention, protocol adherence, attendance, tolerance of the intervention, and completion of study measures, as well as recruitment and retention. The primary goal of this stage is not to evaluate the efficacy of the standardized intervention, but rather to determine whether a full-scale, adequately-powered efficacy trial can be conducted in the first place. This is important because efficacy studies require far more participants and, therefore, are much more expensive. Without feasibility data, the intervention risks failure on the scale of an efficacy trial, because researchers have not been given the opportunity to amend and correct flaws that would have otherwise been detected in a feasibility setting (Arain et al. 2010; Bowen et al. 2009; Orsmond & Colm 2015). Thus, efficacy studies that have not been evaluated from a feasibility perspective may prove to be an inefficient and wasteful use of resources.
Critically, Stages 2 and 3 in the NCCIH framework represent an iterative process, driven by theoretical considerations as well as data collected in earlier stages. Researchers should revert to Stage 2 after a review of the feasibility and/or pilot results, making changes to the protocol based on preliminary Stage 3 data. After amending the protocol, another feasibility or pilot study can be conducted. It would not be uncommon, therefore, to conduct multiple pilot studies before proceeding to more advanced stages of intervention development, as the results from the first pilot study may force researchers to change the intervention specifics to improve subsequent pilot studies. Consistently, and as noted above, this NCCIH Stage 3 is one of two components represented in NIH model’s Stage I. “Intervention Generation/Refmement.” Tliis underscores the iterative nature of Stages 2 and 3 within the NCCIH framework.
NCCIH Stage 4. Efficacy Studies with Appropriate Comparison
Studies at this stage determine whether an intervention has an effect on a given outcome. Within the NCCIH framework, the efficacy phase implicates three key study features that distinguish it from prior stages: optimal study conditions, appropriate comparison, and statistical power. Specifically, determination of efficacy at this stage takes place under optimal study conditions so as to maximize internal validity as well as the possibility that researchers will detect a measurable effect. This is on the opposite side of a continumn from effectiveness studies, discussed in the next section, which take place in non-ideal conditions and maximize external validity. Optimization of study components can include, for example, employing the most well-trained providers or teachers, precise and consistent enrollment of selected participants, a refined and codified intervention that has been evaluated on a smaller scale, statistically sound and well-validated measures of the outcome of interest, rigorous randomization, and extensive follow-up. These various components are optimized in this in vitro stage of evaluation, insulated from complicating factors endemic to studies in the “real world.” Ultimately, the goal of all efficacy studies, and NCCIH Stage 4, is to detect a difference between the intervention and control groups. Unlike pilot and feasibility studies, statistical power – the probability that a true difference between two groups in a study sample can be detected – is a critical factor (Whitley & Ball 2002). Greater power (represented by larger samples) increases the probability of detecting a difference between study groups if one exists.
Finally, efficacy trials use comparison groups that are carefully and thoughtfully selected to detect the specific effects of the intervention (rather than nonspecific effects such as expectation of benefit). In the most ideal setting, the intervention is tested against an active control or placebo (when applicable), rather than a waitlist or other forms of control. Additionally, researchers and participants are ideally blinded, so as to prevent the introduction of expectation bias (Jadad & Enkin 2008; Jiini et al. 2001); however, this is near-impossible to implement with psychological/behavioral (non-phannacological) interventions, for obvious reasons.
In sum, proper comparison groups, adequate statistical power, and optimal study conditions differentiate this phase from prior and subsequent stages. Interestingly, efficacy studies at NCCIH Stage 4 could take place either in research clinics or in community clinics, so long as optimal study conditions, appropriate comparison, and statistical power are upheld. This is different from the NIH stage model in which Stage II includes these characteristics in research clinics only, whereas Stage III applies them in community clinics.
NCCIH Stage 5. Effectiveness or Comparative Effectiveness Research
In contrast to efficacy, which is assessed in optimal research settings, effectiveness is determined in less-controlled enviromnents, often community-based settings. As above, effectiveness studies seek to maximize external validity and generalizability, or whether a given intervention can be reasonably utilized in routine practice (Rothwell, 2005). Some call it pragmatic research, based on the assmnption that efficacy trials do not sufficiently inform community practice because they are conducted under optimal study conditions, and therefore, lack pragmatism (Fleming 2012; Ford & Nome 2016; Roland & Torgerson 1998).
The difference between efficacy and effectiveness parallels the in vitro versus in vivo distinction, with the former designed to detect an effect size in an ideal research setting, and the latter designed to assess real-world applicability. The effectiveness research stage introduces several changes to the study approach, of which two are worth mentioning here. First, the providers delivering the intervention are more varied, some with ideal training, others less so. This heterogeneity reflects real world settings, where there is likely a normal distribution of provider quality. Second, the participants are similarly heterogeneous, a byproduct of less stringent enrollment criteria. Again, the intent is to approximate real-world heterogeneity – in which some patients are not ideally suited for the intervention – to assess effectiveness. What this stage may lose in tenns of effect size, it gains in applicability to organic, real-world venues, i.e., pragmatism.
Of note, effectiveness can be studied from multiple vantage points, including cost- and comparative-effectiveness. The former, unsurprisingly, evaluates whether or not a given intervention is cost-effective according to a given metric of interest (Neumann & Cohen 2015). The latter seeks to compare effectiveness of the intervention against comparable extant interventions (ideally, the gold standard; Sox & Goodman 2012).
Importantly, the NIH stage model separates this stage into two parts (Stages III and IV). Both stages take place in the community rather than in an optimal research setting, but the former maximizes internal validity, measuring efficacy, and the latter maximizes external validity, measuring effectiveness. Indeed, NIH Stage III represents an intermediate step, and seeks to test efficacy in the community – dipping a toe in the proverbial water of effectiveness studies. This involves testing the intervention in the community setting while still maintaining a relatively high level of control. In NIH Stage IV, however, researchers relinquish this degree of control over intervention deployment, in order to maximize external validity. The separation of these two NIH model stages was motivated by a perceived need for a step between traditional efficacy and effectiveness research (Carroll & Rounsaville 2003), although this intennediate stage is absent from the NCCIH model.
NCCIH Stage 6. Dissemination and Implementation
Once efficacy and effectiveness have been demonstrated, the terminus of the NCCIH framework (as well as the NIH stage model) involves studying the dissemination and implementation of a given intervention. One specific goal of this stage is to assess and ensure the distribution and adoption of an intervention on a large scale (Flay et al. 2005; McHugh & Barlow 2010). As Onken et al. put it, “dissemination and implementation research focuses at least as much if not more on the service delivery system as opposed to the intervention itself’ (Onken et al. 2014, p. 30). Indeed, to complete the process of treatment development, it is not enough to demonstrate that an intervention is both efficacious and effective. Rather, the intervention needs to then be adopted by relevant groups, who then use it to demonstrate that the intervention can help patients across a variety of settings. One of the greatest challenges in this stage – especially for MBPs – is training practitioners and/or clinicians to competently and consistently deliver the intervention (McHugh & Barlow 2010). Nevertheless, dissemination and implementation studies represent the ultimate stage of intervention development.
Stage-specific Recommendations for Mindfulness Researchers in CAPP:
Recent reviews by prominent mindfulness researchers have offered insightful commentary on the interpretation and design of MBPs, including recommendations on measuring mindfulness, clinician training, intervention specificity, comparison and active control groups, over-estimation of efficacy, and effectiveness research (Davidson & Kaszniak 2015; Dimidjian & Segal 2015). These commentaries have also specifically discussed the need to move beyond methodologically-weak studies, a category that sadly includes most research on MBPs in youth to date (and corresponding to early model stages). These highly influential recommendations will not be reviewed here, but should be adhered to by adult and child researchers alike.
The recommendations offered to CAPP researchers in this paper differ in two ways from prior reviews. First, the focus in this paper is on strategies for improving MBPs in child and adolescent populations in particular. Second, the recommendations are based explicitly on the NCCIH framework, so as to increase the likelihood that a given study in a pediatric population will get funded. While most of the research on MBPs in youth falls into the early stages of treatment development (Stages 1 and 2), recommendations are offered for researchers at all stages, given the bi-directional and fluid nature of the framework, with the expectation that the literature will continue to mature in the years to come.
Further, what follows is not a comprehensive review of the many ways in which mindfulness-based research in young populations could be improved. While a broad review would be an interesting paper (and is much-needed), this would be beyond the scope of this paper, and may distract the reader from our stage-by-stage actionable recommendations geared toward NCCIH priorities. Rather, a selective, simple and focused set of actionable recommendations is presented to CAPP researchers – not necessarily clinical trial methodologists – that can be implemented without great difficulty for the explicit purpose of improving research design, and can thus improve the likelihood of being funded by the NCCIH. For example, all possible considerations at every stage will not be addressed, including the need for nesting in statistical analysis, issues of treatment fidelity, or the multitude of options for active control – all are important issues that are relevant to MBP research.
We further note that several recommendations could be applied to and discussed at multiple stages within the NCCIH framework; however, each was discussed in their respective stage because the recommendation was particularly salient at that point in the framework. For example, the importance of assessing teacher quality is discussed in the context of Stage 5, in the interest of highlighting the importance of measuring teacher quality in assessing effectiveness. However, teacher quality can and ought to be taken into account and measured at other stages. Similarly, each stage represents a balance between interal and external validity, and issues related to both apply to and can be addressed at multiple stages. Specifically, especially as stages progress from efficacy to effectiveness, the continuum shifts from maximizing internal validity to maximizing generalizability. Thus, while a few such validity issues are discussed in the following stages, none are exclusive to a given stage.
Studies to Demonstrate a Clinically Meaningful Signal: Measuring Mindfulness in Kids
The goal of this stage is to determine whether full-scale investigations of the intervention in question are warranted. This could be demonstrated with promising results from pilot studies, uncontrolled trials, etc. A key question here could be, what counts as “promising results”? First and foremost, this would include a demonstration of clinical improvement in a disorder- or symptom-specific manner. However, this is no small feat, given the complexities involved in subjective and/or objective measurements of clinically-meaningful outcomes (i.e., anxiety, depression). Importantly, MBP researchers are subject to these challenges, like all clinical trialists. However, unique to MBP researchers is the urgent need to obtain and adopt a valid measurement of mindfulness, which is our focus here. After all, promising results in MBPs would presumably need to demonstrate an increase in mindfulness from pre- to post-intervention, in addition to improvement in clinical symptoms (and other potentially relevant outcomes). Thus, a critical task for MBP researchers is determining how to measure mindfulness. The task of measuring mindfulness is inherently complicated given the conceptual difficulties inherent in defining mindfulness, which underscores the role of theory – specifically, Buddhist, philosophical, psychodynamic, cognitive-behavioral, and neuroscientific theories of mind and mental functioning – in the development of MBPs (discussed at length elsewhere; e.g.. Bishop et al. 2004; Chiesa 2013; Dunne 2015; Gilpin 2008; Grossman 2008; Grossman & Van Dam 2011). Further, even if the field adopts a consensus definition (e.g.. Bishop 2004), the task of operationalizing mindfulness into an empirical variable for comparison across time, subject, community, and context has been a topic of fervent academic debate (Davidson & Kaszniak 2015; Dimidjian & Segal 2015; Mikulas 2011; Park et al. 2013).
But perhaps the most pressing unresolved question within the child and adolescent literature is the extent to which self-reports of mindfulness are valid predictors of salutary outcomes (Park et al. 2013); one review concluded that, based solely on psychometric indices, mindfulness scales cannot be strongly recommended (Park et al. 2013). This is particularly salient in the context of children: Whereas adult self-reports of mindfulness have been correlated with some salutary outcomes (Khoury et al. 2015), to our knowledge, there are no such data in children or adolescents. Nevertheless, four self-report scales of mindfulness have been at least preliminarily validated in peer-reviewed journals, including: Child and Adolescent Mindfulness Measure (CAMM; Greco et al. 2011); Mindful Attention Awareness Scale for Adolescents (MAAS-A; Brown et al. 2011); Mindful Attention Awareness Scale for Children (MAAS-C; Lawlor et al 2014); and the recently-developed Comprehensive Inventory of Mindfulness Experiences-Adolescents (CHIME-A; Johnson et al. 2017). However, notably, only MAAS-C was tested in children under 10 years of age (Lawlor et al. 2014), and only the CAMM was validated in multiple published studies in English-speaking individuals (Goodman et al. 2017; Greco et al. 2011; Kuby et al. 2015; Lawlor et al. 2014). This suggests that additional efforts are needed to establish the reliability and validity of these measurements for young populations (for further details, see the excellent in-depth review by Goodman et al. of mindfulness measures in child and adolescent populations, including a useful table of all available measures; Goodman et al. 2017).
Further complicating matters, meditators (novices, in particular) may perceive themselves as being less mindful during early practice phases because one’s awareness of an inability to focus on one object for an extended period of time may increase – a specific kind of response-shift bias (Goodman et al. 2017; Hasenkamp et al. 2012; Howard 1980; Park et al. 2013). In other words, while participants may report decreased mindfulness after an intervention, such a report may actually indicate increased mindfulness, as they become more aware of their inherent distractedness. For children, whose meta-cognitive capabilities are in the nascent stages of development, this phenomenon may be even more pronounced.
Thus, despite the existence of these four self-report measures (of variable quality and utility), objective measures of mindfulness remain elusive. Two promising, but understudied, examples of more objective measurement of mindfulness in adults involve breath-counting as a behavioral proxy measure of mindfulness (Levinson et al. 2014) and momentary ecological assessment (which can also include a subjective component; Dockray et al. 2010; Killingsworth & Gilbert 2010). However, such measures have not been optimized and/or rigorously studied in youth, and would therefore benefit from further investigation.
In short, the problem of identifying a clinically-meaningful signal for mindfulness has troubled researchers since the inception of MBPs. While adult research has made some progress towards more objective and reliable measures of mindfulness, CAPP lags behind. CAPP researchers should be aware of the critical need to use validated measures, improve on existing self-reports, and develop non-subjective indices of mindfulness.
Intervention Development, Refinement and Standardization: Kids Are Not Just Small Adults
The goal of this stage is to standardize the MBP being tested. An MBP may be an already-established MBP (i.e., MBSR in adults, or MindUP in children and adolescents), a program adapted from an established MBP, or a novel program developed by the investigators. When deciding which intervention to test, researchers should consider using an established intervention first, assuming that it is developmentally appropriate and clinically relevant. The upshot to using established interventions is that more data are generated for single given intervention, rather than spread across many, thus improving the ability of the field to assess feasibility, efficacy, or effectiveness, etc. Failing that, researchers should strongly consider adapting programs rather than creating novel ones without a clear reason to do so. Further, any chosen adaptations should have a rationale, such as developmental considerations, theory-driven justification, or direct experience teaching to a particular population in a given context. In the event these two options are not feasible, a de-novo MBP may be indicated, again, with justification.
Regardless of the origin of the MBP, a precise and comprehensive intervention protocol needs to be developed, complete with child- and/or adolescent-specific adaptations if the intervention is adapted from an adult MBP (as is often the case). Unfortunately, current MBPs for children are rarely standardized and/or tested in rigorous clinical trials in such a way, complicating attempts to assess the efficacy or effectiveness of such interventions, and to replicate results.
The notion that adults and children differ in important ways – above and beyond mere size and age – is captured by the aphorism “kids aren’t just small adults,” a quip that may be heard in the pediatric ward of a teaching hospital. In other words, the clinical assessment, diagnostic practices, and treatments that may be applicable in adults do not always transfer easily to the pediatric arena (Ferro 2015; Joseph et al. 2015; Moore 1998). The basic premise of the adage applies to the study and practice of mindfulness in children as well. Critically, optimal features of child and adolescent MBPs may be very different than adult MBPs, and thus require careful consideration and possibly experimentation. These features include meditation “dosing” (e.g., how much time is spent in seated meditation?), treatment duration (e.g., how many minutes per session? How many sessions per week? How many sessions total and over what time frame?), meditation style (e.g., what combination of seated, walking, body scan, or other meditation is used?), discussion points, ancillary activities, and homework (e.g., how long to practice at home and how often?). The list is long, and each item likely requires child-specific adaptation (speculatively, in the absence of available data on what works and/or does not work in children).
Furthermore, researchers at this stage of MBP development need to develop age-specific MBPs that are scrupulously and meticulously codified into replicable and reliable manuals that can then be tested in randomized controlled trials (RCT). Intervention standardization procedures, in conjunction with availing the protocol to the research community, are pivotal if the MBP is to be replicated, validated, and disseminated in subsequent stages of intervention development. Fortunately, there are several examples of precise and standardized mindfulness curricula for children that have been implemented in communities and schools (i.e., “,b” [dot-be]. Paws b, MindUP, and Learning 2 Breathe). These protocols present the opportunity for rigorous testing in clinical trials. “,b” is a good example of a standardized protocol that has been implemented into an RCT. Nevertheless, the testing and re-testing of such interventions lags far behind adult populations. For even “,b.” the most widely and rigorously tested MBP for children, has only been tested in two RCTs as a standalone intervention (Johnson et al. 2016, 2017a). Other examples of standardized mindfulness curricula for children that have been implemented widely include Learning 2 Breathe (Bluth et al. 2016), Master Mind (Parker et al. 2014), and MindUP (Schonert-Reichl et al. 2015). However, to our knowledge, each has only been rigorously studied in one RCT (Dunning et al. 2018).
Perhaps most telling, a recent meta-analysis of mindfulness-based programs in youth showed that the 48 published clinical trials tested 30 unique mindfulness programs (Klingbeil et al. 2017). This speaks to profound intervention heterogeneity, which limits the field’s ability to assess efficacy. The antidote to intervention heterogeneity, of course, is intervention homogeneity, which requires standardization, distribution, evaluation, publication, and repetition of child-specific MBPs in the setting of RCTs.
Feasibility and Pilot Studies: Protocol Adherence in Pediatrics
The explicit goal of this stage is to detennine whether the protocol developed in Stage 2 is feasible. Importantly, a host of difficult and complex methodological questions confront MBP researchers at this stage, including recruitment strategies, mode of delivery (e.g., individual vs. group), and teacher training. One of the most important, but challenging, features of this stage is assuring participant adherence to the treatment protocol, including its various components (i.e., attendance, participation, engagement, and home practice completion). While there exists a vast literature on improving treatment adherence in adults (Julius et al. 2009; Osterberg & Blaschke 2005; van Dulmen et al. 2007), the problem is uniquely troublesome in children. As one researcher studying medication adherence in children noted, “the problem of getting children to follow a treatment regimen is widespread and is frustrating for physicians. The extent to which any patient adheres to a medical regimen is an essential determinant of clinical success” (Gardiner & Dvorkin 2006, p. 793). Of course, adherence is a recurring issue in adult MBP research as well (Davidson & Kaszniak 2015), but studies have shown that pediatric adherence in all medical and psychological research settings is even lower than for adults (Costello et al. 2004; Lask 2003; Matsui 2007; Nevins 2002; Santer et al. 2014).
First, designers of MBPs in children need to know that adherence in children is often lower than in adults, because only then can the necessary child-specific adaptations be implemented. With this knowledge, researchers should make adaptations that would enhance acceptance of and adherence to the MBP regimen (e.g., shortening meditation periods). Secondly, and perhaps more importantly, adherence must be measured directly. This should include attendance in sessions, adherence to instructions within sessions, and homework completion, among many other indices of adherence. Finally, interpretation of results should be done in light of adherence data, as both favorable and unfavorable results in the context of poor adherence should be interpreted with great caution.
Several strategies to increase pediatric adherence to medication regimens have proven successful in other areas of medicine (Gardiner & Dvorkin 2006; Hilt 2013). Among them are “adherence action plans,” simplified drug regimens, pleasant-tasting medicines, regular phone contact between parents and physicians, individualized supervision, and clear instructions. These strategies have analogues for adherence in child MBPs, including simplified meditation practices, pleasant activities and/or meditation practices, regular contact between parents and MBP teachers (or researchers), individualized supervision, and clear instruction – for meditation as well as for intervention participation more generally. Despite these promising strategies for improving adherence, however, they have not yet been implemented and rigorously studied in MBP research in CAPP.
In short, CAPP researchers need to be aware of the possibility that adherence may be a larger impediment in children than in adult populations. Careful assessment of adherence in the feasibility and acceptability stage – and implementation of strategies to improve adherence – are critical to the development of MBPs in CAPP.
Efficacy Studies with Appropriate Comparison: Pediatric Recruitment Challenges
The main goal of this stage is to determine whether the intervention that was standardized in NCCIH Stage 2 and found feasible in Stage 3 is efficacious. There are two considerations that are important for CAPP MBP researchers at this stage to consider: recruiting enough participants and developing an appropriate comparison group.
The first of these represents one of the hallmark challenges of conducting efficacy trials: volume, meaning the recruitment of enough participants to detect a difference between control and treatment arms. Unfortunately, recruitment of participants – especially children – can be an onerous, time-consuming, and costly process. The barriers to pediatric recruitment stem in part from the sensible need to protect vulnerable participants such as children – and are much needed (Wendler 2008). The most promising effort to recruit high nmnbers of participants is the work of Johnson et al. (2016, 2017a), in which 269 and 330 participants were recruited, respectively. With that being said, most current RCTs have between 20 and 60 subjects. Therefore, researchers ought to be aware that more resources, time, and consideration are often required to recruit enough participants for pediatric efficacy studies.
Interestingly, one study showed that parents experience the invitation of their child to participate in a clinical trial much differently than the recruiting researcher (Shilling et al. 2011). Specifically, while many researchers felt it may be interpreted as burdensome for parents to be invited, parents reported that they did not mind being approached and often felt it was an exciting opportunity (Shilling et al., 2011). These findings suggest that any researcher concerns about being intrusive – a factor that could limit recruitment – may be unfounded at times. Instead, non-invitation of eligible participants has been shown to be a severely limiting factor to recruitment (Amiel et al. 2007). Furthermore, the Standards for Research (StaR) in Child Health summit – a World Health Organization-supported venture founded to address the paucity and shortcomings of pediatric clinical trials – recommended increased communication between researcher and child/parent, improved education about the study of interest, and optimization of the risk-benefit ratio for participation (Hartling et al. 2012). In fact, StaR Child Health argued that the scarcity of pediatric research is a “violation of children’s human rights,” with recruitment challenges being a chief contributing factor. Improving recruitment of children to MBP trials through strategies described above may help begin to address the issue in some small way, and improve the quality of MBP evidence as well.
Another critical piece of efficacy studies in MBP research, as many authors have already noted (Black 2015; Davidson & Kaszniak 2015; Dimidjian & Segal 2015) is development of appropriate control and comparison groups. The arguments in favor of more active and rigorous control groups – especially with gold-standard psychotherapies – have been published elsewhere and will not be reviewed here (Davidson & Kaszniak 2015; Dimidjian & Segal 2015). Suffice it to say that appropriate and feasible blinding strategies, properly matched comparison groups, and active controls are the most important methodological tools for gold-standard clinical studies. These are strategies that need to be employed in MBPs in children and adults alike.
For child and adolescent psychiatrists in particular, whose skills include medication management, pharmacotherapy should be considered more often for active control. Indeed, other active comparison groups (i.e., gold-standard psychotherapies such as cognitive-behavioral therapy, or other MBPs) are important to study. However, the focus here is on incorporating medication as an active control because of the dearth of studies incorporating medication in child and adolescent populations. In fact, due to any nmnber of factors – including the aforementioned barriers to the recruitment of children – to our knowledge, there are no RCTs comparing medication and MBPs in pediatric populations, and only one RCT in adult MBP research evaluating medication as a control group (Kuyken et al. 2015). The next step in the evolution of mindfulness research in children is the further integration of active controls such as gold standard psychotherapies or medication comparison groups, including medication alone and medication combined with mindfulness.
Medication control groups are critical for at least two reasons. First, medication is a “gold-standard” treatment-as-usual for many psychiatric conditions (e.g., ADHD, depression, and anxiety, to name a few), and thus is a natural control condition. However, in a search of the literature on MBPs for ADHD, for example, 11 studies of MBPs in children or adolescents were found, only two of which were randomized (Kiani et al. 2017; Lo et al. 2017), none had an active control, and consistently, none used medication as a control condition (Bögels et al. van Dun et al. 2008; Carboni al. 2013; Haydickyt al. 2013; Singh et al. 2016, 2018; van de Weijer-Bergsma et al. 2012; van der Oord et al. 2012; Zhang et al. 2017; Zylowska et al. 2008). Second, utilization of combined groups may be an ideal opportunity to evaluate medication as a MBP augmentation strategy. For example, in a combined group it is possible that medication would enhance the efficacy of the MBP. This may be especially true in cases of ADHD or depression, in which concentration and attention span are typically impaired (Gupta & Kar 2009; Rock et al. 2014). In turn, MBPs may enhance the effects of medication treatment. For example, it is entirely conceivable that a participant on a medication-only arm may not receive the psychological support they require in the course of treatment, so that the addition of an MBP would improve outcomes. Furthermore, medications may enhance the effects of MBPs. Specifically, medications could support attention regulation in the early stages of a combined intervention, and therefore augment a participant’s ability to meditate. Then, with enough time and mindfulness training, the patient may conceivably be able to taper off medication altogether, having become proficient in the skills taught in the MBP Further, there may be additional long-term benefits to combined medication-MBP interventions. In these ways, the incorporation of medication arms into clinical trials may be a promising tool. In sum, MBP efficacy trials in CAPP face many challenges, including participant recruitment and development of an appropriate comparison; however, finding such appropriate comparisons – including medication and/or gold-standard psychotherapy – is necessary and important in the long run.
Effectiveness or Comparative Effectiveness Research: Teacher Quality and Cost-Effectiveness
The effectiveness of an intervention, as discussed above, refers to its efficacy in a healthcare and/or community-based venue (i.e., outside an optimized research setting; Onken et al. 2014). Effectiveness can be measured by a variety of outcomes, including comparative-effectiveness and cost-effectiveness. A host of factors are implicated in assuring the effectiveness (comparative, cost, or otherwise) of an intervention, but among the most important variables are the quality and consistency of the therapist or teacher in a given intervention. Indeed, across treatment types, studies show that therapist quality, competence, fidelity, and training may be more determinant of outcome than the kind of therapy that is delivered (Branson et al. 2015; Fairbum & Cooper 2011). While teacher quality is important at every stage of intervention development, the issue manifests prominently in effectiveness research, which is why the issue is discussed in this section. Specifically, given that effectiveness research takes place in “in vivo”, non-optimal conditions, teacher quality will not be ideal (by definition). As such, the impact of teacher quality may be magnified in comparison to prior stages.
Like with other interventions, treatment fidelity in MBPs may dictate the success (or failure), thus its measurable effectiveness (Dimidjian & Segal 2015). In addition to fidelity of adherence to the MBP protocol, other indices of teacher quality are critical to effective delivery of an MBP including management of group dynamics, embodiment, interpersonal effectiveness, emotional intelligence, pacing, etc. Because effectiveness is likely to vary according to teacher quality and fidelity, it would benefit the field to develop criteria for teacher assessment specifically for MBPs in children. One promising avenue for assessing teacher quality in adult is the Mindfulness-Based Intervention – Teaching Assessment Criteria (MBLTAC; Crane et al. 2013; Crane et al. 2010). However, it only applies to Mindfulness-Based Stress Reduction and Mindfulness-Based Cognitive Therapy, neither of which is designed for children. Similarly, to assess fidelity, a teacher adherence and competence scale was recently developed exclusively for Mindfulness-Based Relapse Prevention (Chawla et al. 2010).
Even if the MBI:TAC is adapted to MBPs for youth, it is far from a perfect measure, and no panacea for teacher assessment. After all, indices of teacher quality for MBPs are notoriously difficult to measure – in adults and children alike – and current assessment tools may not provide all of the answers. Adapting MBI:TAC to children is a good place to start. After all, it is likely the case that qualities in a teacher that are helpful for the transmission of mindfulness to children may not necessarily be as effective in adults (and vice versa). If this is borne out in the literature, one would expect the MBI:TAC for children to assess for qualities that are particularly important for children. Naturally, such a measure would allow researchers to quantify the contribution of these factors to intervention effectiveness in child and adolescent populations, which would be particularly important if, for example, efficacy in research settings has been demonstrated, but effectiveness studies report overall negative results.
It is also possible that adapting the MBI:TAC to children is not enough, and additional measures are needed (for both adult and child teachers of MBPs). For example, one hypothetical (but untested) index of teacher quality is teacher mindfulness, which may be difficult to quantify, especially objectively. Indeed, MBI:TAC attempts to measure mindfulness via the embodiment domain within the scale. But embodiment is a mere approximation of mindfulness, is subjective, and may not capture the variance in outcome attributable to teacher mindfulness that an objective measure might. In any case, the point remains that current tools to assess MBP teacher quality and fidelity are imperfect – especially in children, for which there are no documented scales – and ought to be subject to revision, improvement, and testing across all levels of the NCCIH framework (we include the discussion here because teacher quality may be particularly salient to effectiveness). Indeed, measures of teacher quality and fidelity may prove to be important in explaining the variance in outcomes. Specifically, if the data suggest that an MBP is ineffective in a community or school setting, teacher assessment tools would allow researchers to evaluate whether teacher quality and/or fidelity plays a role.
Additionally, the cost-effectiveness of MBPs in children and adolescents is a relatively unexplored avenue of inquiry in the literature. Kuyken et al.’s (2015) study of the cost-effectiveness of Mindfulness-Based Cognitive Therapy (MBCT) for depression relapse in adults represents the best example of a cost-effectiveness analysis of an MBP to date, and one that child and adolescent researchers ought to emulate. Alongside clinical outcomes, the authors evaluated multiple indices of cost-effectiveness, including mean cost, productivity losses, out-of-pocket expenditure and use of health-care and social services, comparing MBCT and maintenance medication treatment. However, to our knowledge, no such studies have been published for child and adolescent populations. Studies that incorporate such outcomes could help guide the allocation of financial (and other) resources to mindfulness programs by, for example, school boards seeking to fund programming and teacher training, or insurance companies setting reimbursement rates for mental health treatments. Regardless of their application, the utility of cost-effectiveness studies is unquestioned, as is their absence in the literature on MBPs in children and adolescents.
In sum, effectiveness researchers in child and adolescent MBPs would benefit greatly from the development of child-specific teacher assessment criteria for both quality and fidelity improvement, as well as the incorporation of cost-effectiveness outcomes, to assist the transition from efficacy to effectiveness studies.
Dissemination and Implementation: The Promise (and Peril) of School-based Interventions
Stage 6 is concerned with disseminating and implementing interventions that are found to be effective and efficacious in prior stages. However, to our knowledge, there are no Stage 6 studies of MBPs in child and adolescent populations. This is no surprise, given that even in adult populations – in which MBPs have a much larger body of evidence than children and adolescents – there are only three examples of MBP dissemination and implementation studies (Crane & Kuyken 2013; Lau et al. 2012; Patten & Meadows 2009). To address this gap, schools present the ideal venue for assessing dissemination and implementation. Of course, schools can serve as the setting for studies at earlier stages as well (for example, a Stage 1 pilot study of an MBP for disruptive behavior in elementary school children), especially in the case of interventions that are inherently school-based (for a review of ten of these programs, see Semple et al. 2017). However, schools also present the unique opportunity to assess widespread dissemination and implementation of mindfulness programs to the greatest number of children, in a semi-standardized way – even for interventions not initially designed for this setting.
For example, from a recruitment perspective, logistics are often relatively facile in schools (e.g., identification of participants, transportation, location, etc.), because children do not need to be individually identified and recruited, and are already physically present. Further, schools are increasingly considered to be important arenas for mental health promotion and intervention (Nathanson et al. 2016; O’Toole et al. 2017; Sharman 2017). Thus, schools may be more open to MBPs that may benefit both healthy children as well as those who have already developed symptoms of a clinical disorder. For example, the United Kingdom recently announced that govermnent funding will support school-based mindfulness education for the first time – across the entire country (Sharman 2017).
From a public health perspective, schools can provide a mutually beneficial location for educators and CAPP researchers alike, especially for treating children with unidentified clinical disorders. Indeed, only a small percentage of children with mental health problems access mental health services, and collaboration between schools and researchers may help close that gap, allowing CAPPs to identity and treat children with undiagnosed mental illness (Ford 2008; Ford et al. 2008; O’Toole et al. 2017). In this way, schools may present the best opportunity to teach mindfulness to the greatest nmnber of children, and therefore could be ideal for assessing dissemination and implementation on a broad scale.
Despite these promises, administration of MBPs to children in schools also poses unique challenges. For example, what if students are unwilling to participate but are obligated to do so by the school (as is the case currently in the UK, in which 370 schools across the country will be taught mindfulness exercises as part of a mental health promotion program; Magra 2019; Sharman 2017; UK Department of Education 2019)? What if teachers feel obligated or are otherwise uninterested? To our knowledge, there are no data on differences in outcome between voluntary and obligatory mindfulness programs, but it is not inconceivable that required participation in a mindfulness program may generate differential effects in comparison to voluntary programs. However, to our knowledge, this has never been tested with MBPs, with adults or children. Similarly, it is not clear how to avoid cohort effects in school-based interventions, or whether teachers should (or could) assmne dual roles of educators and mindfulness instructors. One additional challenge in school-based MBP studies pertains to who might be teaching. Many MBPs are delivered by self-selected and highly-trained teachers. If interventions are disseminated across many schools, this would not be feasible. Alternatively, if school teachers deliver the intervention, is it fair to require them to become certified to teach mindfulness, especially when many of whom are already burdened with countless trainings and certifications? These questions (and more) are bound to arise if interest in school-based MBPs continues to persist. Indeed, it is precisely these questions that the implementation and dissemination phase seeks to evaluate – the extent to which various “real-world” complications offset any potential benefit the MBP may have for the public health of children in the community.
In sum, the NCCIH Framework for Developing and Testing Mind and Body Interventions (National Center for Complementary and Integrative Health 2017) is a six-stage model for research development that shares common elements with the NIH Stage Model for Intervention Development (Onken et al. 2014). This framework should guide the design and implementation of MBPs for CAPP researchers. Doing so will not only improve the quality of evidence but will also improve the likelihood that a given study will be funded by the NCCIH. Here, we offered six focused and actionable recommendations corresponding to the six stages of the NCCIH framework that may benefit child and adolescent psychologists and psychiatrists interested in developing and testing MBPs. Importantly, we are careful not to suggest that this set of recommendations is exhaustive, and surely many other “good practice” guidelines would be helpful to follow (Davidson & Kaszniak 2015; Dimidjian & Segal 2015). Nevertheless, we hope that these recommendations will improve MBP research in child and adolescent psychology and psychiatry.
Figure 4:
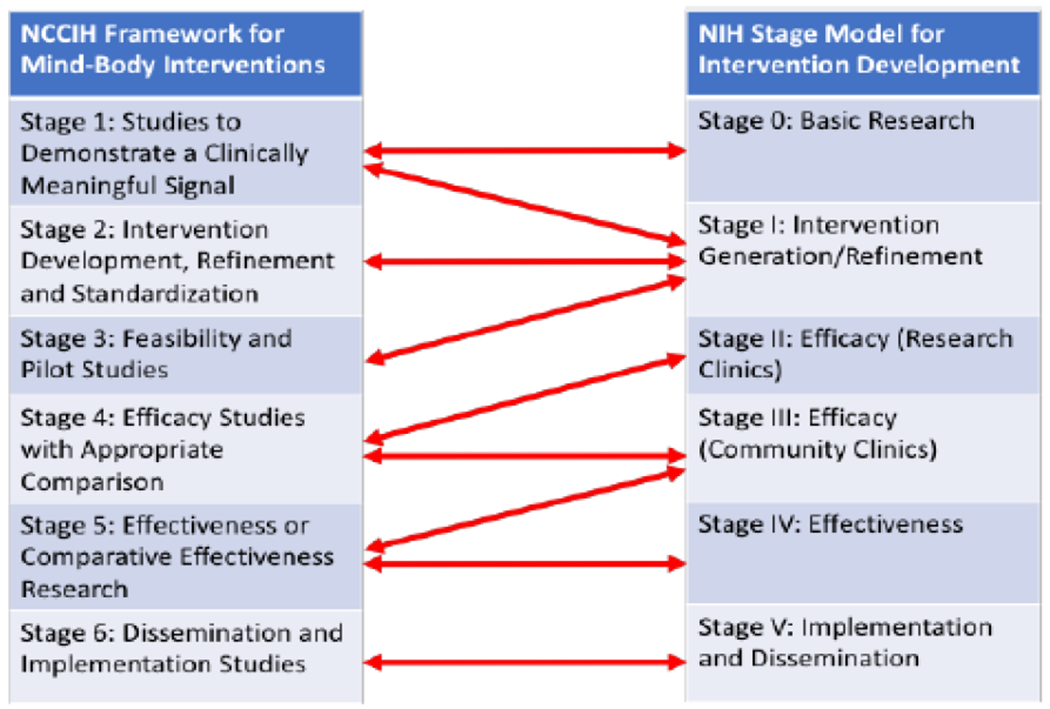
Comparison of National Center for Complementary and Integrative Health (NCCIH) and National Institute of Health (NIH) models of intervention development.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Conflict of Interest:
Dr. Saunders declares that he has no conflict of interest. Dr. Kober has provided consultation to Indivior, Inc. and declares that she has no conflict of interest with any material in this manuscript.
Conflict of Interest:
DS declares that he has no conflict of interest. HK has provided consultation to Indivior, Inc. and declares that she has no conflict of interest with any material in this manuscript.
This article does not contain any studies with human participants or animals performed by any of the authors.
Contributor Information
David Saunders, Clinical and Research Fellow, Child and Adult Psychiatry, Yale Child Study Center.
Hedy Kober, Associate Professor, Department of Psychiatry, Department of Psychology, Cognitive Science Program, Interdepartmental Neuroscience Program, Yale University School of Medicine.
REFERENCES
- Amiel P, Moreau D, Vincent-Genod C, Alberti C, Hankard R, Ravaud P, … Gaultier C (2007). Noninvitation of eligible individuals to participate in pediatric studies: a qualitative study. Archives of Pediatrics & Adolescent Medicine , 161(5), 446–450. 10.1001/archpedi.161.5.446 [DOI] [PubMed] [Google Scholar]
- Arain M, Campbell MJ, Cooper CL & Lancaster GA (2010). What is a pilot or feasibility study? A review of current practice and editorial policy. BMC Medical Research Methodology, 10(1), 67 10.1186/1471-2288-10-67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop SR, Lau M, Shapiro S, Carlson L Anderson ND, Carmody J, … Devins G (2004). Mindfulness: a proposed operational definition. Clinical Psychology: Science and Practice, 11(3), 230–241. 10.1093/clipsy/bph077 [DOI] [Google Scholar]
- Black DS (2015). Mindfulness training for children and adolescents: a state-of-the-science review In Brown KW, Creswell JD, & Ryan RM (Eds.), Handbook of Mindfulness: Theory, Research, and Practice. (pp. 283–310). New York: Guilford Press. [Google Scholar]
- Bluth K Campo RA, Pruteanu-Malinici S, Reams A, Mullarkey M & Broderick PC (2016). A school-ased mindfulness pilot study for ethnically diverse at-risk adolescents. Mindfulness, 7(1), 90–104. 10.1007/s12671-014-0376-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodhi B (2011). What does mindfulness really mean? A canonical perspective. Contemporary Buddhism, 12(1), 19–39. 10.1080/14639947.2011.564813 [DOI] [Google Scholar]
- Bögels S, Hoogstad B, van Dun L, de Schutter S, & Restifo K (2008). Mindfulness training for adolescents with externalizing disorders and their parents. Behavioural and Cognitive Psychotherapy, 36(02), 307–314. 10.1017/S1352465808004190 [DOI] [Google Scholar]
- Bowen DJ, Kreuter M, Spring B, Cofta-Woerpel L, Linnan L, Weiner D, … Fernandez M (2009). How we design feasibility studies. American Journal of Preventive Medicine, 36(5), 452–457. 10.1016/j.amepre.2009.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branson A, Shafran R, & Myles P (2015). Investigating the relationship between competence and patient outcome with CBT. Behaviour Research and Therapy, 68, 19–26. 10.1016/j.brat.2015.03.002 [DOI] [PubMed] [Google Scholar]
- Brown KW, West AM, Loverich TM, & Biegel GM (2011). Assessing adolescent mindfulness: validation of an adapted mindful attention awareness scale in adolescent nonnative and psychiatric populations. Psychological Assessment, 23(4), 1023–1033. 10.1037/a0021338 [DOI] [PubMed] [Google Scholar]
- Carboni JA, Roach AT, & Fredrick LD (2013). Impact of mindfulness training on the behavior of elementary students with attention-deficit/hyperactive disorder. Research in Human Development, 10(3), 234–251. 10.1080/15427609.2013.818487 [DOI] [Google Scholar]
- Carroll KM, & Rounsaville BJ (2003). Bridging the gap: a hybrid model to link efficacy and effectiveness research in substance abuse treatment. Psychiatric Sendees, 54(3), 333–339. 10.1176/appi.ps.54.3.333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castellanos R, Yildiz Spinel M, Phan V, Orengo-Aguayo R, Humphreys KL, & Flory K (2020). A systematic review and meta-analysis of cultural adaptations of mindfulness-based interventions for Hispanic populations. Mindfulness, 11(2), 317–332. 10.1007/s12671-019-01210-x [DOI] [Google Scholar]
- Chawla N, Collins S, Bowen S, Hsu S, Grow J, Douglass A, & Marlatt GA (2010). The mindfulness-based relapse prevention adherence and competence scale: development, interrater reliability, and validity. Psychotherapy Research, 20(4), 388–397. 10.1080/10503300903544257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiesa A (2013). The difficulty of defining mindfulness: current thought and critical issues. Mindfulness, 4(3), 255–268. 10.1007/s12671-012-0123-4 [DOI] [Google Scholar]
- Costello I, Wong ICK, & Nunn AJ (2004). A literature review to identify interventions to improve the use of medicines in children. Child: Care, Health and Development, 30(6), 647–665. 10.1111/j.1365-2214.2004.00478.x [DOI] [PubMed] [Google Scholar]
- Crane RS, Eames C, Kuyken W, Hastings RP, Williams JMG, Bartley T, … Surawy C (2013). Development and validation of the mindfulness-based interventions – teaching assessment criteria (MBI:TAC). Assessment, 20(6), 681–688. 10.1177/1073191113490790 [DOI] [PubMed] [Google Scholar]
- Crane RS, & Kuyken W (2013). The implementation of mindfulness-based cognitive therapy: learning from the UK Health Service experience. Mindfulness, 4(3), 246–254. 10.1007/s12671-012-0121-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crane RS, Kuyken W, Hastings RP, Rothwell N, & Williams JMG (2010). Training teachers to deliver mindfulness-based interventions: learning from the UK experience. Mindfulness, 1(2), 74–86. 10.1007/s12671-010-0010-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson RJ, & Kaszniak AW (2015). Conceptual and methodological issues in research on mindfulness and meditation. American Psychologist, 70(7), 581–592. 10.1037/a0039512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimidjian S, & Segal ZV (2015). Prospects for a clinical science of mindfulness-based intervention. American Psychologist, 70(7), 593–620. 10.1037/a0039589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dockray S, Grant N, Stone AA, Kahneman D, Wardle J, & Steptoe A (2010). A comparison of affect ratings obtained with ecological momentary assessment and the day reconstruction method. Social Indicators Research, 99(2), 269–283. 10.1007/s11205-010-9578-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunne JD (2011). Toward an understanding of non-dual mindfulness. Contemporary Buddhism, 12( 1), 71–88. 10.1080/14639947.2011.564820 [DOI] [Google Scholar]
- Dunne JD (2015). Buddhist styles of mindfulness: a heuristic approach. In Ostafin BD, Robinson MD, & Meier BP (Eds.), Handbook of Mindfulness and Self-Regulation (pp. 251–270). New York, NY: Springer New York, 10.1007/978-1-4939-2263-518 [DOI] [Google Scholar]
- Dunning DL, Griffiths K, Kuyken W, Crane C, Foulkes L, Parker J, & Dalgleish T (2018). Research review: the effects of mindfulness-based interventions on cognition and mental health in children and adolescents – a meta-analysis of randomized controlled trials. Journal of Child Psychology and Psychiatry, 60(3), 244–258. 10.1111/jcpp.12980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG, & Cooper Z (2011). Therapist competence, therapy quality, and therapist training. Behaviour Research and Therapy, 49(6–7), 373–378. 10.1016/j.brat.2011.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferro A (2015). Paediatric prescribing: why children are not small adults. British Journal of Clinical Pharmacology, 79(3), 351–353. 10.1111/bcp.12540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flay BR, Biglan A, Boruch RF, Castro FG, Gottfredson D, Kellam S, … Ji P (2005). Standards of evidence: criteria for efficacy, effectiveness and dissemination. Prevention Science, 6(3), 151–175. 10.1007/s11121-005-5553-y [DOI] [PubMed] [Google Scholar]
- Fleming M, Kirby B, & Penny KI (2012). Record linkage in Scotland and its applications to health research. Journal of Clinical Nursing, 2/(19–20), 2711–2721. 10.1111/j.1365-2702.2011.04021.x [DOI] [PubMed] [Google Scholar]
- Ford I, & Norrie J (2016). Pragmatic trials. New England Journal of Medicine, 375(5), 454–463. 10.1056/NEJMra1510059 [DOI] [PubMed] [Google Scholar]
- Ford T (2008). Practitioner review: How can epidemiology help us plan and deliver effective child and adolescent mental health services? Journal of Child Psychology and Psychiatry, and Allied Disciplines, 49(9), 900–914. 10.1111/j.1469-7610.2008.01927.X [DOI] [PubMed] [Google Scholar]
- Ford T, Hamilton H, Meltzer H, & Goodman R (2008). Predictors of service use for mental health problems among british schoolchildren. Child and Adolescent Mental Health, I3( 1). 32–40. 10.1111/j.1475-3588.2007.00449.X [DOI] [PubMed] [Google Scholar]
- Gardiner P, & Dvorkin L (2006). Promoting medication adherence in children. American Family Physician, 74(5), 793–798. [PubMed] [Google Scholar]
- Gilpin R (2008). The use of theravāda buddhist practices and perspectives in mindfulness-based cognitive therapy. Contemporary Buddhism, 9(2), 227–251. 10.1080/14639940802556560 [DOI] [Google Scholar]
- Goldberg SB, Tucker RP, Greene PA, Davidson RI, Wampold BE, Kearney DI, & Simpson TL Mindfulness-based interventions for psychiatric disorders: a systematic review and meta-analysis, 59 Clinical Psychology Review § (2018). 10.1016/j.cpr.2017.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman MS, Madni LA, & Semple RJ (2017). Measuring mindfulness in youth: review of current assessments, challenges, and future directions. Mindfulness, 8(6), 1409–1420. 10.1007/s12671-017-0719-9 [DOI] [Google Scholar]
- Greco LA, Baer RA, & Smith GT (2011). Assessing mindfulness in children and adolescents: development and validation of the child and adolescent mindfulness measure (CAMM). Psychological Assessment, 23(3), 606–614. 10.1037/a0022819 [DOI] [PubMed] [Google Scholar]
- Grossman P (2008). On measuring mindfulness in psychosomatic and psychological research. Journal of Psychosomatic Research, 64(4), 405–408. 10.1016/jjpsychores.2008.02.001 [DOI] [PubMed] [Google Scholar]
- Grossman P, & Van Dam NT (2011). Mindfulness, by any other name…: trials and tribulations of sati in western psychology and science. Contemporary Buddhism, 12(1), 219–239. 10.1080/14639947.2011.564841 [DOI] [Google Scholar]
- Gupta R, & Kar BR (2009). Development of attentional processes in ADHD and nonnal children. Progress in Brain Research, 176, 259–276. 10.1016/S0079-6123(09)17614-8 [DOI] [PubMed] [Google Scholar]
- Harrington A, & Dunne JD (2015). When mindfulness is therapy. American Psychologist, 70(7), 621–631. 10.1037/a0039460 [DOI] [PubMed] [Google Scholar]
- Hartling L, Wittmeier KDM, Caldwell P, van der Lee H, Klassen TP, Craig JC, & Oifringa M (2012). StaR cliild health: developing evidence-based guidance for the design, conduct, and reporting of pediatric trials. Pediatrics, 129(Supplement 3), S112–S117. 10.1542/peds.2012-0055C [DOI] [PubMed] [Google Scholar]
- Hasenkamp W, Wilson-Mendenhall CD, Duncan E, & Barsalou LW (2012). Mind wandering and attention during focused meditation: a fine-grained temporal analysis of fluctuating cognitive states. NeuroImage, 59(1), 750–760. 10.1016/j.nemoimage.2011.07.008 [DOI] [PubMed] [Google Scholar]
- Haydicky J, Shecter C, Wiener J, & Ducharme JM (2013). Evaluation of mbct for adolescents with adhd and their parents: impact on individual and family functioning. Journal of Child and Family Studies, 24(1), 76–94. 10.1007/s10826-013-9815-1 [DOI] [Google Scholar]
- Hilt RJ (2013). Adherence and behavioral health care. Pediatric Annals, 42(8), 306–306. 10.3928/00904481-20130723-03 [DOI] [PubMed] [Google Scholar]
- Howard GS (1980). Response-shift bias: a problem in evaluating interventions with pre/post self-reports. Evaluation Review, 4(1), 93–106. 10.1177/0193841X8000400105 [DOI] [Google Scholar]
- Jadad A, & Enkin M (2008). Bias in randomized controlled trials In Randomized Controlled Trials (pp. 29–47). Oxford, UK, UK: Blackwell Publishing Ltd; 10.1002/9780470691922.ch3 [DOI] [Google Scholar]
- Johnson C, Burke C, Brinkman S, & Wade T (2016). Effectiveness of a school-based mindfulness program for transdiagnostic prevention in young adolescents. Behaviour Research and Therapy, 81, 1–11. 10.1016/j.brat.2016.03.002 [DOI] [PubMed] [Google Scholar]
- Johnson C, Burke C, Brinkman S, & Wade T (2017a). A randomized controlled evaluation of a secondary school mindfulness program for early adolescents: Do we have the recipe right yet? Behaviour Research and Therapy, 99, 37–46. 10.1016/j.brat.2017.09.001 [DOI] [PubMed] [Google Scholar]
- Johnson C, Burke C, Brinkman S, & Wade T (2017b). Development and validation of a multifactor mindfulness scale in youth: the comprehensive inventory of mindfulness experiences-adolescents (CHIME-A). Psychological Assessment, 29(3), 264–281. 10.1037/pas0000342 [DOI] [PubMed] [Google Scholar]
- Joseph PD, Craig JC, & Caldwell PΗY (2015). Clinical trials in children. British Journal of Clinical Pharmacology, 79(3), 357–369. 10.1111/bcp.12305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Julius RJ, Novitsky MA, & Dubin WR (2009). Medication adherence: a review of the literature and implications for clinical practice. Journal of Psychiatric Practice, 15(1), 34–44. 10.1097/01.pra.0000344917.43780.77 [DOI] [PubMed] [Google Scholar]
- Jüni P. Altman DG, & Egger M (2001). Systematic reviews in health care: assessing the quality of controlled clinical trials. BMJ, 323(7303), 42–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoury B, Sharma M, Rush SE, & Fournier C (2015). Mindfulness-based stress reduction for healthy individuals: a meta-analysis. Journal of Psychosomatic Research. 78(6), 519–528. 10.1016/j.jpsychores.2015.03.009 [DOI] [PubMed] [Google Scholar]
- Kiani B, Hadianfard H, & Mitchell JT (2017). The impact of mindfulness meditation training on executive functions and emotion dysregulation in an Iranian sample of female adolescents with elevated attention-deficit/hyperactivity disorder symptoms. Australian Journal of Psychology, <59(4), 273–282. 10.1111/ajpy.12148 [DOI] [Google Scholar]
- Killingsworth M. a, & Gilbert DT (2010). A wandering mind is an unhappy mind. Science (New York, N. Y.), 330(6006), 932 10.1126/science.1192439 [DOI] [PubMed] [Google Scholar]
- Klingbeil DA, Renshaw TL, Willenbrink JB, Copek RA, Chan KT, Haddock A, … Clifton J (2017). Mindfulness-based interventions with youth: a comprehensive meta-analysis of group-design studies. Journal of School Psychology, 63, 77–103. 10.1016/j.jsp.2017.03.006 [DOI] [PubMed] [Google Scholar]
- Kuby AK, McLean N, & Allen K (2015). Validation of the child and adolescent mindfulness measure (caimn) with non-clinical adolescents. Mindfulness, 6(6), 1448–1455. 10.1007/s12671-015-0418-3 [DOI] [Google Scholar]
- Kuyken W, Hayes R, Barrett B, Byng R, Dalgleish T, Kessler D, … Byford S (2015). Effectiveness and cost-effectiveness of mindfulness-based cognitive therapy compared with maintenance antidepressant treatment in the prevention of depressive relapse or recurrence (PREVENT): a randomised controlled trial. The Lancet, 386(9988), 63–73. 10.1016/S0140-6736(14)62222-4 [DOI] [PubMed] [Google Scholar]
- Lask B (2003). Motivating children and adolescents to improve adherence. The Journal of Pediatrics, 143(A), 430–433. 10.1067/S0022-3476(03)00447-5 [DOI] [PubMed] [Google Scholar]
- Lau MA, Colley L, Willett BR, & Lynd LD (2012). Employee’s preferences for access to mindfulness-based cognitive therapy to reduce the risk of depressive relapse-a discrete choice experiment. Mindfulness, 3(4), 318–326. 10.1007/s12671-012-0108-3 [DOI] [Google Scholar]
- Lawlor MS, Schonert-Reichl KA, Gadermann AM, & Zumbo BD (2014). A validation study of the mindful attention awareness scale adapted for children. Mindfulness, 5(6), 730–741. 10.1007/s12671-013-0228-4 [DOI] [Google Scholar]
- Levinson DB, Stoll EL, Kindy SD, Merry HL, & Davidson RJ (2014). A mind you can count on: validating breath counting as a behavioral measure of mindfulness. Frontiers in Psychology, 5(Oct), 1–10. 10.3389/fpsyg.2014.01202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo H, Wong S, Wong J, Yeung J, Snel E, & Wong S (2017). The effects of family-based mindfulness intervention on adlid symptomology in young children and their parents: a randomized control trial. Journal of Attention Disorders, 1–14. 10.1177/1087054717743330 [DOI] [PubMed] [Google Scholar]
- Lomas T, Medina JC, Ivtzan I, Rupprecht S, & Eiroa-Orosa FJ (2019). A systematic review and meta-analysis of the impact of mindfulness-based interventions on the well-being of healthcare professionals. Mindfulness, 10(7), 1193–1216. 10.1007/s12671-018-1062-5 [DOI] [PubMed] [Google Scholar]
- Magra I (2019). Schools in england introduce a new subject: mindfulness. The New York Times. Retrieved July 9, 2019, from https://www.nytimes.com/2019/02/04/world/europe/uk-mindfulness-children-school.html
- Matsui D (2007). Current issues in pediatric medication adherence. Paediatric Drugs, 9(5), 283–288. 10.2165/00148581-200709050-00001 [DOI] [PubMed] [Google Scholar]
- McClintock AS, Rodriguez MA, & Zerubavel N (2019). The effects of mindfulness retreats on the psychological health of non-clinical adults: a meta-analysis. Mindfulness, 10(8), 1443–1454. 10.1007/s12671-019-01123-9 [DOI] [Google Scholar]
- McHugh RK, & Barlow DH (2010). The dissemination and implementation of evidence-based psychological treatments: a review of current efforts. American Psychologist, (65(2), 73–84. 10.1037/a0018121 [DOI] [PubMed] [Google Scholar]
- Mikulas WL (2011). Mindfulness: significant common confusions. Mindfulness, 2(1), 1–7. 10.1007/s12671-010-0036-z [DOI] [Google Scholar]
- Moore P (1998). Children are not small adults. The Lancet, 352(9128), 630 10.1016/S0140-6736(05)79591-X [DOI] [PubMed] [Google Scholar]
- Nathanson L, Rivers SE, Flynn LM, & Brackett MA (2016). Creating emotionally intelligent schools with ruler. Emotion Review, 8(4), 305–310. 10.1177/1754073916650495 [DOI] [Google Scholar]
- National Center for Complementary and Integrative Health. (2017). Framework for developing and testing mind and body interventions. Retrieved March 3, 2017, from https://nccih.nih.gov/grants/mindbody/framework
- Neumann PJ, & Cohen JT (2015). Measuring the value of prescription drugs. New England Journal of Medicine, 373(27), 2595–2597. 10.1056/NEJMp1512009 [DOI] [PubMed] [Google Scholar]
- Nevins TE (2002). Non-compliance and its management in teenagers. Pediatric Transplantation, (5(6), 475–479. 10.1034/j.1399-3046.149.ptrls077.l.x [DOI] [PubMed] [Google Scholar]
- O’Toole C, Furlong M, McGilloway S, & Bjørndal A (2017). Preschool and school-based mindfulness programmes for improving mental health and cognitive functioning in young people aged 3 to 18 years. Cochrane Database of Systematic Reviews, 2017(1). 10.1002/14651858.CD012518 [DOI] [Google Scholar]
- Onken LS, Carroll KM, Shoham V, Cuthbert BN, & Riddle M (2014). Reenvisioning clinical science: unifying the discipline to improve the public health. Clinical Psychological Science, 2(1), 22–34. 10.1177/2167702613497932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orsmond GI, & Cohn ES (2015). The distinctive features of a feasibility study. OTJR: Occupation, Participation and Health, 35(3), 169–177. 10.1177/1539449215578649 [DOI] [PubMed] [Google Scholar]
- Osterberg L, & Blaschke T (2005). Adherence to medication. The New England Journal of Medicine, 353(5), 487–497. 10.1056/NEJMra050100 [DOI] [PubMed] [Google Scholar]
- Park T, Reilly-Spong M, & Gross CR (2013). Mindfulness: a systematic review of instruments to measure an emergent patient-reported outcome (PRO). Quality of Life Research, 22(10), 2639–2659. 10.1007/s11136-013-0395-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker AE, Kupersmidt JB, Mathis ET, Scull TM, & Sims C (2014). The impact of mindfulness education on elementary school students: evaluation of the master mind program. Advances in School Mental Health Promotion, 7(3), 184–204. 10.1080/1754730X.2014.916497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patten SB, & Meadows GM (2009). Population-based service planning for implementation of mbct: linking epidemiologic data to practice. Psychiatric Services. 60(11), 1540–1542. 10.1176/ps.2009.60.11.1540 [DOI] [PubMed] [Google Scholar]
- Rock PL, Roiser JP, Riedel WJ, & Blackwell AD (2014). Cognitive impairment in depression: a systematic review and meta-analysis. Psychological Medicine, 44(\0), 2029–2040. 10.1017/S0033291713002535 [DOI] [PubMed] [Google Scholar]
- Roland M, & Torgerson DJ (1998). Understanding controlled trials: what are pragmatic trials? BMJ, 316(7127), 285–285. 10.1136/bmj.316.7127.285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothwell PM (2005). External validity of randomised controlled trials: “to whom do the results of this trial apply?” The Lancet 365(9453), 82–93. 10.1016/S0140-6736(04)17670-8 [DOI] [PubMed] [Google Scholar]
- Santer M, Ring N, Yardley L, Geraghty AWA, & Wyke S (2014). Treatment non-adherence in pediatric long-tenn medical conditions: systematic review and synthesis of qualitative studies of caregivers’ views. BMC Pediatrics, 14(1), 63 10.1186/1471-2431-14-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders DC (2015). Being mindful of mindfulness: past, present, and future of mindfulness in child and adolescent psychiatry. Journal of the American Academy of Child and Adolescent Psychiatry, 54(6), 437–439. 10.1016/j.jaac.2015.03.006 [DOI] [PubMed] [Google Scholar]
- Schonert-Reichl KA, Oberle E, Lawlor MS, Abbott D, Thomson K, Oberlander TF, & Diamond A (2015). Enhancing cognitive and social-emotional development through a simple-to-administer mindfulness-based school program for elementary school children: a randomized controlled trial. Developmental Psychology, 51(1), 52–66. 10.1037/a0038454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semple RJ, Droutman V, & Reid BA (2017). Mindfulness goes to school: tilings learned (so far) from research and real-world experiences. Psychology in the Schools, 54(1), 29–52. 10.1002/pits.21981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharf RH (2015). Is mindfulness buddhist? (and why it matters). Transcultural Psychiatry, 52(4), 470–484. 10.1177/1363461514557561 [DOI] [PubMed] [Google Scholar]
- Sharman J (2017). Eight-year-olds to get mindfulness lessons to promote wellbeing. Retrieved July 9, 2019, from http://www.independent.co.uk/news/uk/home-news/children-eight-mindfulness-lessons-relaxation-mental-health-school-education-a7625296.html
- Shilling V, Williamson P, Hickey H, Sowden E, Smyth R, & Young B (2011). Processes in recruitment to randomised controlled trials of medicines for children (RECRUIT): a qualitative study. Health Technology Assessment, 75(15), 1–116. 10.3310/hta15150 [DOI] [PubMed] [Google Scholar]
- Singh NN, Lancioni GE, Karazsia BT, Felver JC, Myers RE, & Nugent K (2016). Effects of samatha meditation on active academic engagement and math performance of students with attention deficit/hyperactivity disorder. Mindfulness, 7(1), 68–75. 10.1007/s12671-015-0424-5 [DOI] [Google Scholar]
- Singh NN, Lancioni GE, Nabors L, Myers RE, Felver JC, & Manikam R (2018). Samatha meditation training for students with attention deficit/hyperactivity disorder: effects on active academic engagement and math performance. Mindfulness, 9(6), 1867–1876. 10.1007/s12671-018-1014-0 [DOI] [Google Scholar]
- Sox HC, & Goodman SN (2012). The methods of comparative effectiveness research. Annual Review of Public Health, 33(1), 425–445. 10.1146/annurev-publhealth-031811-124610 [DOI] [PubMed] [Google Scholar]
- Turgon R, Ruffault A, Juneau C, Blatier C, & Shankland R (2019). Eating disorder treatment: a systematic review and meta-analysis of the efficacy of mindfulness-based programs. Mindfulness, 10(11), 2225–2244. 10.1007/s12671-019-01216-5 [DOI] [Google Scholar]
- UK Department of Education. (2019). One of the largest mental health trials launches in schools. Retrieved July 9, 2019, from https://www.gov.uk/govermnent/news/one-of-the-largest-mental-health-trials-launches-in-schools
- Van Dam NT, van Vugt MK, Vago DR, Schmalzl L, Saron CD, Olendzki A, … Meyer DE (2018). Mind the hype: a critical evaluation and prescriptive agenda for research on mindfulness and meditation. Perspectives on Psychological Science, 13(1), 36–61. 10.1177/1745691617709589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van de Weijer-Bergsma E, Formsma AR, de Bruin EI, & Bögels SM (2012). The effectiveness of mindfulness training on behavioral problems and attentional functioning in adolescents with adhd. Journal of Child and Family Studies, 21(5), 775–787. 10.1007/s10826-011-9531-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Oord S, Bögels SM, & Peijnenburg D (2012). The effectiveness of mindfulness training for children with adhd and mindful parenting for their parents. Journal of Child and Family Studies, 21(1). 139–147. 10.1007/s10826-011-9457-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Dulmen S, Sluijs E, van Dijk L, de Ridder D, Heerdink R, & Bensing J (2007). Patient adherence to medical treatment: a review of reviews. BMC Health Sendees Research, 7(1), 55 10.1186/1472-6963-7-55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vonderlin R, Biermann M, Bohus M, & Lyssenko L (2020). Mindfulness-based programs in the workplace: a meta-analysis of randomized controlled trials. Mindfulness, 10.1007/s12671-020-01328-3 [DOI] [Google Scholar]
- Wendler D (2008). Is it possible to protect pediatric research subjects without blocking appropriate research? Journal of Pediatrics, 752(4), 467–470. 10.1016/j.jpeds.2007.09.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitley E, & Ball J (2002). Statistics review 4: sample size calculations. Critical Care, 6(4), 335 10.1186/cc1521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zenner C, Herrnleben-Kurz S, & Walach H (2014). Mindfulness-based interventions in schools-a systematic review and meta-analysis. Frontiers in Psychology, 5, 1–20. 10.3389/fpsyg.2014.00603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang D, Chan SKC, Lo HHM, Chan CYH, Chan JCY, Ting KT, … Wong SYS (2017). Mindfulness-based intervention for Chinese children with adhd and their parents: a pilot mixed-method study. Mindfulness, 8(4), 859–872. 10.1007/s12671-016-0660-3 [DOI] [Google Scholar]
- Zoogman S, Goldberg SB, Hoyt WT, & Miller L (2015). Mindfulness interventions with youth: a meta-analysis. Mindfulness, (5(2), 290–302. 10.1007/s12671-013-0260-4 [DOI] [Google Scholar]
- Zylowska L, Ackerman DL, Yang MH, Futrell JL, Horton NL, Hale TS, … Smalley SL (2008). Mindfulness meditation training in adults and adolescents with adhd: a feasibility study. Journal of Attention Disorders, 11(6), 737–746. 10.1177/1087054707308502 [DOI] [PubMed] [Google Scholar]


