Abstract
Objective
The overarching objective of the scoping review was to examine peer reviewed and grey literature for best practices that have been developed, implemented and/or evaluated for delayed discharge involving a hospital setting. Two specific objectives were to review what the delayed discharge initiatives entailed and identify gaps in the literature in order to inform future work.
Design
Scoping review.
Methods
Electronic databases and websites of government and healthcare organisations were searched for eligible articles. Articles were required to include an initiative that focused on delayed discharge, involve a hospital setting and be published between 1 January 2004 and 16 August 2019. Data were extracted using Microsoft Excel. Following extraction, a policy framework by Doern and Phidd was adapted to organise the included initiatives into categories: (1) information sharing; (2) tools and guidelines; (3) practice changes; (4) infrastructure and finance and (5) other.
Results
Sixty-six articles were included in this review. The majority of initiatives were categorised as practice change (n=36), followed by information sharing (n=19) and tools and guidelines (n=19). Numerous initiatives incorporated multiple categories. The majority of initiatives were implemented by multidisciplinary teams and resulted in improved outcomes such as reduced length of stay and discharge delays. However, the experiences of patients and families were rarely reported. Included initiatives also lacked important contextual information, which is essential for replicating best practices and scaling up.
Conclusions
This scoping review identified a number of initiatives that have been implemented to target delayed discharges. While the majority of initiatives resulted in positive outcomes, delayed discharges remain an international problem. There are significant gaps and limitations in evidence and thus, future work is warranted to develop solutions that have a sustainable impact.
Keywords: health & safety, health policy, international health services, protocols & guidelines, primary care
Strengths and limitations of this study.
To our knowledge, this is the first scoping review to identify best practices for delayed discharges involving a hospital setting.
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews Checklist was followed.
A comprehensive search of peer reviewed and grey literature was conducted.
A critical appraisal of the interventions was not performed.
Introduction
A delayed hospital discharge (known as alternate level of care (ALC) in Canada and delayed transfer of care in the UK) occurs when a patient is medically approved to be discharged, but remains in hospital for non-medical reasons (eg, waiting for a long-term care bed to become available or to transfer home with services).1 While waiting for their next destination, patients’ level of care and activation often decrease or stop entirely. Delayed discharge can result in hospital patient flow issues (eg, emergency service backlogs, cancelled surgeries, delays in medically necessary care),2 increased healthcare costs,3 an increased risk of functional decline,4 5 falls,6 hospital-related adverse events (eg, medication error, exposure to infectious disease),6 7 mortality,8 as well as poor patient and family experiences.9
Patients who experienced a delayed discharge in previous studies exhibited the following characteristics: female,10 older,10 11 physically or cognitively impaired.4 12–15 Patients have also shown to exhibit aggressive behaviours,16 use assistive devices17 and have psychiatric conditions,10 neurological disorders15 and/or multimorbidity.17 In addition to these patient-level factors, there are a number of system-level factors that contribute to delayed discharges, including long wait lists for long-term care facilities,5 17–19 rehabilitation or other postacute care (eg, home care),11 12 20–23 the lack of culturally and religiously diverse long-term care facilities,15 limited or absent hospital services on weekends24 and organisational delays (eg, administrative delays, delayed assessments).24 25 There are also different pressures and priorities across sectors, with little incentive to work together as a system. For example, while hospitals may be focused on efficiency and throughput, community-based organisations may be focused on empowerment, longer-term quality of life outcomes and working at a pace that works for patients and families. The funding structure of hospitals and healthcare systems can also have an impact on overall patient flow, including discharge delays. Although there is wide variation in funding structures within and across countries, there is potential for funding to either incentivise or disincentivise timely hospital discharges.26–30
The combination of patient-level and system-level factors contributing to delayed discharges can also have a large financial impact on patients, families, healthcare providers and the healthcare system.3 A recent systematic review reported that delayed discharges cost approximately £200–565 ($C320–$C900) per patient, per day.3 Further, it was estimated that the National Health Service (NHS) (England) spends £820 million ($C1.3 billion) every year on patients who have a discharge delay.31 Similarly, a recent report from Canada stated that three hospitals located in Ottawa, Ontario, spend approximately $C250 000 per day (combined) on patients occupying beds at a level of care they no longer require.32 In addition to large costs for hospitals and healthcare systems, delayed hospital discharges can result in out-of-pocket costs for patients and families.33 Increased out-of-pocket costs, in addition to the other uncertainties associated with a delay, can heighten stress for patients and families, contribute to poor experiences and compromise quality of life.9
Overall, delayed hospital discharges are problematic internationally, highlighting a need to identify best practices and current initiatives that are concentrating on solutions to this complex problem. To date, the majority of published literature on delayed discharge has focused on risk factors and characteristics of patients who experience delayed discharge. There has been a limited focus on initiatives that address the delayed discharge problem. Therefore, the purpose of this scoping review was to examine peer reviewed and grey literature (literature published through non-traditional means) for initiatives that have been developed and/or evaluated for delayed discharge from a hospital setting, with the goal of identifying best practices for reducing delayed discharge. A scoping review methodology was appropriate for addressing this goal, in order to identify the types of available evidence on this topic, examine key characteristics relating to initiatives for delayed discharge and to identity knowledge gaps.34
Methods
This review followed the scoping review methodology outlined by Levac et al,35 as well as the recently developed Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (see online supplemental table 1).36 A protocol for this scoping review was developed in consultation with a librarian at the University of Toronto, with continuous input from members of the research team.
bmjopen-2020-044291supp001.pdf (133.6KB, pdf)
Stage 1: identifying the research question
The research question developed to lead this scoping review was: what is known in the literature about initiatives (eg, strategies, programmes, interventions) that have been developed, implemented and/or evaluated for delayed discharge involving a hospital setting? The two main aims were: (1) to review what delayed discharge initiatives entail (eg, characteristics, outcomes) and (2) to identify gaps in the literature in order to inform future studies.
Stage 2: identifying relevant articles
The search strategy was developed with a librarian at the University of Toronto and through consultations with an advisory group and collaborators who have experience in clinical practice or administration (see online supplemental table 2 for Medline search strategy). Each search strategy was adapted for the specific database using appropriate command line syntax and indexing. The following are examples of keywords searched using Boolean operators, proximity operators, wild cards and truncations: ALC, delayed discharge, delayed transfer, bed blocking, strategy, model, intervention, programme, policy.
Electronic databases were searched for relevant articles. The following electronic databases were searched on 16 August 2019: MEDLINE (Ovid Interface), EMBASE (Ovid Interface), AMED (Ovid Interface), Cumulative Index to Nursing and Allied Health Literature (EBSCO Interface) and Cochrane Library. Grey literature was searched on the following databases and repositories: OpenGrey, Health Services Research Projects in Progress, UpToDate, Community Research and Development Information Services and TSpace, as well as on numerous national and international healthcare and government websites. We also reached out to key stakeholders, including members of our advisory group, to send us relevant reports and presentations.
Stage 3: study selection
For inclusion, articles (peer-reviewed and grey literature) were required to meet the following criteria: (1) focused on delayed discharge, (2) included an initiative to address delayed discharge, (3) involved a hospital setting, (4) published between 1 January 2004 and 16 August 2019 and (5) peer-reviewed or grey literature. We focused our inclusion on initiatives involving a hospital setting because this is where the problem of delayed discharges surfaces. Articles were excluded if they met any one of the following criteria: (1) focused on changing the threshold/timing of discharge (early discharge), (2) books, book chapters, opinion pieces or editorials, (3) grey literature that did not sufficiently describe the initiative implemented (eg, implementation process, location, population, impact); (4) protocols, trial papers or chart reviews or (5) conference abstracts or articles without an accessible full text. Articles were excluded for criteria one (changing the threshold/timing of discharge) because the rationale for having an earlier discharge was often focused on other factors such as cost-savings by reducing length of stay, rather than specifically addressing a delayed discharge. Articles were excluded if they met criteria two (books, book chapters, opinion pieces or editorials) to eliminate articles with potential personal biases and summaries of peer-reviewed literature. Grey literature that did not provide sufficient details on the initiative (such as lacking a description of the components of the initiative) were excluded. Articles published more than 15 years ago, before 1 January 2004, were excluded to ensure the initiatives included in this scoping review were relevant to more current health service practices.
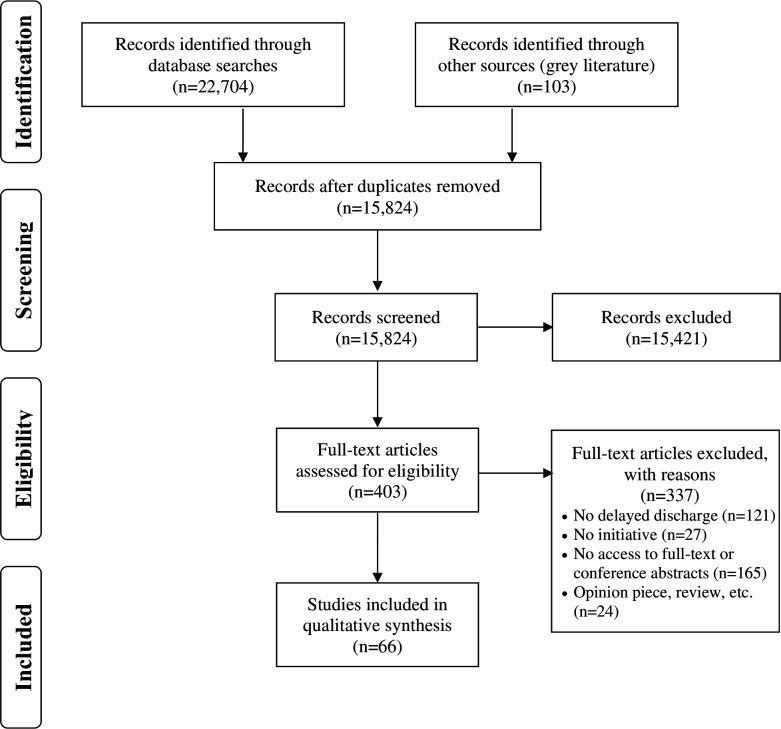
Articles identified from the database searches were imported into EndNote X9, a reference management software, where they were deduplicated following Bramer’s method.37 The initial database searches identified 22 704 articles, which were reduced to 15 824 following deduplication (figure 1). The titles and abstracts of the articles were reviewed on Covidence, a software platform for systematic and scoping reviews.38 The research team (LC, KK, SJTG, KMK and JK) independently screened the titles and abstracts of 40 articles to test their agreement. The reviewers had a good per cent agreement (85%), so the remaining articles were divided among the team and screened by single reviewers (LC, KMK and JK). All disagreements were discussed in-person by the reviewers until a consensus was reached; minor revisions were made to the eligibility criteria to ensure clarity and consistency. Following title and abstract screening, articles were reviewed at the full-text level. Thirty full-text articles were independently screened by the research team (LC, KK, SJTG, KMK, JK and MA) to test their interrater agreement. The remaining full-text articles (peer-reviewed and grey literature) were double screened by four reviewers (LC, KMK, JK and MA).
Figure 1.
PRISMA flow diagram of included articles. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Stage 4: charting the data
The data were charted by two reviewers (LC and KMK) using a data extraction form in Microsoft Excel. The form was developed and tested by the research team in a series of team meetings prior to the extraction of all data. We conducted spot checking of extracted data from 15% of the included articles to ensure completeness and accuracy of the extracted data. Any questions that arose during the charting process were discussed by the team. Charted data contained the following information: general information, study characteristics, population characteristics, initiative characteristics, characteristics of delayed discharge, study outcomes and conclusions.
Stage 5: collating, summarising and reporting results
Microsoft Excel was used to conduct a descriptive quantitative analysis of the included articles, as well as facilitate qualitative thematic analysis. The thematic analysis of the charted data was an inductive and iterative process, in which the team (LC, SJTG, KMK and KK) met in-person to discuss high level concepts and identified common themes across the included articles. When reviewing the extracted data, we found that the strategies appeared to cluster into core categories, which aligned with a conceptual framework developed by Doern and Phidd.39 This framework classifies policy instruments/tools along a continuum (from those that are least coercive like information sharing to those that are more coercive like public ownership or, in our case, new infrastructure). We deductively applied Doern and Phidd’s categories to classify our findings, with some minor adaptations. The five adapted categories were not mutually exclusive and included: (1) information sharing (live information sharing and documented recommendations); (2) tools and guidelines; (3) practice changes; (4) infrastructure and finance and (5) other (see table 1 for category descriptions and examples). The categories assisted with the organisation and presentation of the data.
Table 1.
Categories, descriptions and examples of initiative categorisation
| Category name | Description | Examples |
| Information Sharing A—live sharing B—recommended initiatives— calls to action |
|
|
| Tools and guidelines |
|
|
| Practice changes |
|
|
| Infrastructure and finance |
|
|
| Other initiatives |
|
|
Stage 6: consultation
The research team presented findings of the scoping review to key stakeholders (eg, hospital staff, patient and caregiver partners) through the planning process and analysis of results. These meetings were used to inform search terms, gather relevant documents, obtain feedback on the categorisation/organisation of initiatives, as well as identify knowledge gaps in order to develop targeted and actionable recommendations for future practice, policy and research.
Patient and public involvement
An advisory council (patient and caregiver partners), along with providers, managers and organisational leaders identified the lack of understanding about the state of evidence around best practices for delayed discharges, which informed the research question for this scoping review. The advisory council was involved with planning meetings where they provided feedback on the search terms and analysis. Results will be disseminated to the advisory council through presentations and a lay summary.
Results
Study characteristics
The database search identified 15 824 unique articles that were screened for eligibility; following title/abstract and full-text review, 66 articles were included in this scoping review, 49 articles from the database searches and 17 articles from the grey literature searches (figure 1). The majority of included articles were quantitative studies (n=34), with a few qualitative (n=5), mixed methods (n=6) or other designs (policy analyses, reviews, case studies and presentations; n=21). There was a large variety of study designs, with few randomised trials and prospective studies. Most initiatives were evaluated (n=42), with different types of evaluations such as process evaluations and outcome evaluations. The UK (n=21), USA (n=18) and Canada (n=17) were the most common countries where studies were conducted. Based on the year of publication, there was a fairly even distribution of peer-reviewed articles across the years of inclusion (from 2004 to 2019); however, the majority of grey literature was published in the last 10 years. Table 2 describes the characteristics of included articles.
Table 2.
Characteristics of included articles
| Author (year) | Country | Objective | Method Study design |
Participants | Sample size | Key conclusions |
| Database searches | ||||||
| Adlington (2018)40 | UK | Reduce length of stay, bed occupancy and delays in discharge and promote care in the appropriate setting among functional older adults on a psychiatric ward | Quantitative Quality Improvement |
Older adults (65+) on psychiatric ward | NR |
|
| Ardagh (2011)63 | New Zealand | Identify 10 common challenges and promising initiatives relating to patient flow and emergency department overcrowding | Qualitative NR |
NR | NR |
|
| Arendts (2013)68 | Australia | Determine if hospital length of stay for older patients is reduced when an allied health intervention is introduced in the emergency department (ED) | Quantitative Non-randomised prospective pragmatic study |
ED patients (65+) diagnosed with one or more of six conditions (cerebrovascular insufficiency; fractured neck of femur; cardiac failure; myocardial ischaemia; exacerbation of chronic airways disease; respiratory tract infection) | 3572 |
|
| Baumann (2007)55 | UK | Identify the factors causing good discharge practice performance and organisation of services | Qualitative Descriptive |
Health/social services staff with managerial involvement in discharges | 42 |
|
| Behan (2005)93 | UK | Explore the experience of service users across the UK during the first 6 months of the implementation of the Community Care (Delayed Discharges) Act | Qualitative Explorative |
NR | NR |
|
| Béland (2006)69 | Canada | Assess the transformation of the organisation and delivery of health and social services with additional interventions for frail elderly people | Quantitative Randomised controlled trial |
Frail elderly | 1309 |
|
| Blecker (2015)70 | USA | Evaluate the impact of a weekend hospital intervention on care processes, clinical outcomes and length of stay | Quantitative Interrupted time series observational study |
Non-obstetric patients hospitalised | 57 163 |
|
| Boutette (2018)71 | Canada | Serve frail elderly patients at risk of deconditioning and/or disability, caused by prolonged hospitalisation | NR Review/ description of programme |
Frail older patients who are at risk of deconditioning and/or disability | NR |
|
| Bowen (2014)72 | UK | Demonstrate that nurse-led discharges can improve efficiency on a short stay surgical ward, without impacting patients safety | Quantitative Case study |
Adult ear, nose, throat patients having routine, elective, short stay surgery | 265 |
|
| Boyd (2017)41 | USA | Explore the leadership strategies used by hospital business administrators to reduce delayed discharges and improve profitability | Qualitative Multiple case study |
Hospital administrators | 3 |
|
| Brankline (2009)47 | USA | Provide the appropriate level of care and patient choice when the patient is medically ready for transfer | Quantitative Pilot study |
Medical floors with primarily elderly patients who require nursing home placement after discharge | 25 |
|
| Brown (2008)64 | USA | Determine if the length of patient stay is reduced in the postanaesthesia care unit when nurses use discharge criteria | Quantitative Prospective clinical study |
Adult, ASA physical status I, II, and III patients (18+) requiring general anaesthesia | 1198 |
|
| Burr (2017)56 | Canada | Develop a framework that would support ALC avoidance strategies across the Toronto Central Local Health Integration Network | Case study Case study |
ALC patients | 3 hospitals |
|
| Caminiti (2013)42 | Italy | Evaluate the effectiveness of a strategy aimed to reduce delayed hospital discharge | Quantitative Cluster, parallel group, randomised trial/quality improvement |
Hospital units: geriatric, medicine, long-term care | 3498 |
|
| Chidwick (2017)54 | Canada | Discuss concepts and ideas that led to lowest ALC days in the province | Mixed methods Quality improvement |
ALC patients | NR |
|
| El-Eid (2015)73 | Lebanon | Assess the effectiveness of the Six Sigma method in improving discharge processes | Quantitative Pre and post-intervention study |
NR | 17 054 |
|
| Gaughan (2015)101 | England | Investigate the reduction in hospital bed-blocking due to a greater supply of nursing home beds or reduced costs | Quantitative Statistical modelling - Empirical analysis |
Patients waiting for hospital discharge | NR |
|
| Graham (2012)74 | UK | Evaluate the effect of the laparoscopic nurse specialist on patient discharge | Quantitative Retrospective comparison |
Laparoscopic cholecystectomy and laparoscopic inguinal hernia repair patients | 128 |
|
| Gutmanis (2016)65 | Canada | Outline change strategies and their impact health system transformation and those living with responsive behaviours and their family members | Mixed methods Quality improvement |
Individuals with responsive behaviours | NR |
|
| Henwood (2006)48 | UK | Examine the partnership between health and social care by exploring issues with hospital discharges | Case study Case study |
Inpatients | NR |
|
| Holland (2016)57 | USA | Report the development and evaluation of a discharge delay tracking and reporting mechanism | Quantitative Practice improvement project |
Inpatients | NR |
|
| Katsaliaki (2005)102 | UK | Describe a project investigating potential care pathways for elderly people after discharge from hospital | Quantitative Discrete-event simulation, simulation model |
Inpatients | NR |
|
| Lees-Deutsch (2019)66 | UK | Identify core characteristics of patient discharge criteria, recorded in clinical management plans or case notes | Quantitative Systematic observational retrospective review |
Patients discharged from the acute medicine unit and short-stay units | 50 |
|
| Levin (2019)94 | Scotland | Examine the impact of Intermediate Care and the 72-hour target on delayed hospital discharge | Quantitative Controlled interrupted time series design |
Patients aged 75+ | 107 022 |
|
| Lian (2008)58 | Singapore | Develop methods to reduce the hospital length of stay for premature infants by 30%, within 6 months | Quantitative Retrospective review |
Premature infants | 78 |
|
| Maessen (2008)75 | Netherlands | Assess the effect of enhanced recovery after surgery programme on discharge delays | Quantitative Retrospective/ prospective study |
Patients undergoing elective colorectal resection | 173 |
|
| Mahant (2008)59 | Canada | Determine if an audit-and-feedback intervention reduces delayed discharge in a general paediatric inpatient unit | Quantitative Prospective observational study |
Paediatric inpatient | 3194 |
|
| Mahto (2009)76 | UK | Determine the effect of a diabetes outreach service on delayed discharges and avoidable admissions | Quantitative Cross-sectional audit |
Acutely admitted patients with diabetes | 137 |
|
| Maloney (2007)49 | USA | Develop a web-based software application used to facilitate timely patient discharge | Quantitative Quality improvement pilot project |
Inpatients | NR |
|
| Manville (2014)95 | Canada | Determine if providing interdisciplinary care on a transitional care unit will result in improved clinical outcomes and lower costs | Quantitative Before-and-after structured retrospective chart audit |
Elderly ALC patients (70+) | 135 |
|
| Meehan (2018)77 | UK | Explore patients’ experiences of hospital discharge with the discharge to assess scheme | Qualitative Descriptive |
Patients discharged through discharge to assess | 30 |
|
| Moeller (2006)60 | Canada | Assess patient and physician-related barriers to discharging patients who have met objective criteria | Mixed methods Retrospective assessment |
Patients with community-acquired pneumonia | 31 |
|
| Mur-Veeman (2011)61 | The Netherlands | Explain the theory of buffer management and discuss related previous assumptions | NR Review/ theoretical paper |
Bed blockers | NR |
|
| Niemeijer (2010)62 | Netherlands | Reduce the average length of stay to create more admission capacity and reduce costs | Mixed methods Efficiency improvement project (retrospective and prospective data collection) |
Trauma patients | 2006:1114 2007:1124 |
|
| Panis (2004)78 | Netherlands | Reduce inappropriate hospital stay by adjusting patient logistics, increasing efficiency and providing comfortable surroundings | Quantitative Retrospective cohort study |
Mothers of newborn patients | 2889 days of hospital stay of gynaecology and obstetrics patients |
|
| Patel (2019)43 | USA | Evaluate the impact of team-based multidisciplinary rounds on discharge planning and care efficiency | Mixed methods Quality improvement initiative |
Dissatisfied patients with delayed discharge | 1584 |
|
| Ali Pirani (2010)44 | Pakistan | Emphasise the role of nurses to determine factors leading to a lack of discharge planning | NR Review/ summary |
Those experiencing delayed discharge | NR |
|
| Qin (2017)103 | Australia | Identify which barriers to discharge influence hospital occupancy when targeted by a hospital-wide policy | Quantitative Simulation modelling |
NR | NR |
|
| Rae (2007)96 | New Zealand | Illustrate how the Delayed Discharge Project solved a bed crisis and controlled expenditure | Quantitative Continuous quality improvement project |
Acute general medical | 20 034 |
|
| Roberts (2013)50 | Australia | Undertake a preliminary trial of the Goal Length of Stay tool at a rehabilitation centre | Quantitative Prospective study |
Inpatients in two units: SRU or BIRU | 202 |
|
| Sampson (2006)79 | UK | Describe bed occupancy data in people with diabetes before and after the introduction of a diabetes inpatient specialist nurse service | Quantitative Retrospective study |
Diabetes inpatients | 152 080 |
|
| Shah (2007)97 | England | Examine the impact of the Community Care (Delayed Discharge) Act on bed occupancy and length of stay in Geriatric Medicine (GM) and Old Age Psychiatry (OAP) services | Quantitative Retrospective study |
Inpatient - specialties of GM and OAP services | NR |
|
| Sobotka (2017)51 | USA | Describe a hospital-to-home transitional care model | Case study Illustrative case design/ review |
Paediatric inpatient | 1 |
|
| Starr-Hemburrow (2011)80 | Canada | Minimise the number of post-acute patients transitioning from hospital to long-term care and develop an integrated plan for appropriate care and placement | Quantitative Quality improvement |
ALC patients | NR |
|
| Sutherland (2013)45 | Canada | Describe structural challenges to reduce the impact of ALC patients and to propose policy alternatives that could reduce occupancy | NR Discussion and debate article |
ALC patients | NR |
|
| Taber (2013)81 | USA | Test a programme to improve length of stay, delayed discharges and early readmissions for kidney transplant recipients | Quantitative Observational study |
Adult kidney transplant recipients | 476 |
|
| Udayai (2012)82 | India | Reduce patient discharge time through a Six Sigma project | Quantitative Time motion study |
Cash patients | NR |
|
| Williams (2010)52 | Australia | Examine the impact of a critical care outreach service on frequency of discharge delay from the intensive care unit | Quantitative Prospective cohort study |
Patients discharged from the ICU | 1123 |
|
| Younis (2011)53 | UK | Compare the effect of an enhanced recovery programme with preoperative stoma education on the number of patients with prolonged hospital stay | Quantitative Prospective study |
Patients undergoing anterior resection with the formation of a loop ileostomy | 120 |
|
| Grey literature | ||||||
| Anonymous (2008)99 | USA | Create an expedited discharge fund to pay for goods and services inhibiting a patient’s discharge (medical equipment, medication and transportation) | N/A News article |
Uninsured patients | NR |
|
| Anonymous (2010)46 | USA | Improve patient flow through initiatives that decrease length of stay and increase capacity | N/A News article |
NR | NR |
|
| Calveley (2007)83 | UK | Create a tier of support to reduce the unnecessary and costly occupation of hospital beds | N/A Review |
NR | NR |
|
| Manzano-Santaella (2009)100 | UK | Analyse the relationship between Payment by Results and the Delayed Discharges Act | N/A Policy analysis |
NR | NR |
|
| Krystal (2019)86 | Canada | NR | Mixed methods Continuous quality improvement and evaluation |
Medically and socially complex and frail elderly | 100+ |
|
| Walker (2011)2 | Canada | Develop recommendations of care for frail Canadians | N/A N/A |
NR | NR |
|
| North West Community Care Access Centre (2011)88 | Canada | Create a fact sheet of the benefits of staying at home and using Wait at Home (enhanced home care services while people wait for long-term care) | N/A N/A |
Seniors waiting for LTC placement | NR |
|
| Toronto Central Community Care Access Centre (2015)67 | Canada | NR | N/A N/A |
NR | NR |
|
| Province of New Brunswick (2017)92 | Canada | Identify priority strategic initiatives and implement community support orders across the province | N/A Annual report |
NR | NR |
|
| NHS Improvement (2018)104 | UK | Create a how-to guide explaining implementation approaches to reduce length of stay | N/A Guide |
NR | NR |
|
| Starr-Hemburrow (2010)91 | Canada | Improve patient flow through the implementation of change management initiatives | Quantitative Quality improvement |
NR | NR |
|
| LHIN Collaborative (2011)87 | Canada | Help support patients in their homes for as long as possible by providing them with community supports | N/A Implementation guide and toolkit |
Patients (specifically high needs seniors) | NR |
|
| Shah (2011)90 | Canada | Ensure the appropriate community resources are in place to support the patient on discharge | N/A Implementation guide and toolkit |
High need seniors (75+) | NR |
|
| Central East LHIN ALC Task Group (2008)84 | Canada | Understand the impact of delayed discharges in the Central East regions of Ontario (reviewing data, reading reports, initiating a pilot study, developing a patient flow map) | N/A Report |
ALC patients | NR |
|
| Adams, Care & Repair England (2017)98 | UK | Assist older patients in returning home from hospital quickly and safely | Case study Case study |
Older patients | 1 |
|
| Shah (2010)89 | Canada | Describe the Home First approach, a philosophy for reducing ALC | Quantitative Quality improvement |
Elderly patients | NR |
|
| Joint Improvement Team (2013)85 | Scotland | Identify 10 action items to transform discharge processes | N/A Quality improvement/ stakeholder engagement |
N/A | NR |
|
ALC, alternate level of care; BIRU, brain injury rehabilitation unit; GM, geriatric medicine; ICU, intensive care unit; N/A, not applicable; NR, not reported; OAP, old age psychiatry; SRU, stroke rehabilitation unit.
The initiatives most commonly targeted adults and older adults; however, there were some initiatives targeting the paediatric population. Specific characteristics of the study population (ie, age, sex, gender, ethnicity/race, income level, education, marital status, household composition, employment status, comorbidities) were not reported in the majority of articles. Most peer-reviewed articles (n=31) defined a delayed discharge; however, there was a wide variety of definitions for these terms (see online supplemental table 3). The most common definition for delayed discharge was when a patient was identified as medically ready for discharge, but remained in hospital. Table 3 describes the initiative characteristics.
Table 3.
Initiative characteristics
| Author | Initiative Description/content |
Target population | Setting | Initiative category* | Results |
| Database Searches | |||||
| Adlington40 | Quality improvement programme
|
Older adults (>65) on psychiatric ward | Hospital Mile End Hospital (Leadenhall Ward), 26 beds |
Information sharing live |
|
| Ardagh63 | 10 promising initiatives
|
NR | Hospitals | Tools and guidelines Practice changes |
|
| Arendts68 | Allied health assessment
|
Patients (>65) diagnosed with one or more of six predetermined conditions | Hospitals Two Australian tertiary hospitals |
Practice changes |
|
| Baumann55 | N/A
|
Health/ social services staff with managerial involvement in discharges | Hospitals (6 sites) 4 southern sites, 2 northern sites |
Initiatives described touch on all categories |
|
| Behan93 | Community Care (Delayed Discharge) Act 2003
|
NR | 7 areas across the UK | Infrastructure and finance |
|
| Béland69 | Integrated care
|
Frail elderly | Community service centres/ organisations | Practice changes |
|
| Blecker70 | 7 day hospital initiative
|
Non-obstetric hospitalised patients | Hospital Tisch Hospital, 705 beds |
Practice changes |
|
| Boutette71 | Subacute care unit for frail elderly
|
Frail older patients who are at risk of deconditioning associated with a long hospitalisation | Hospitals Ottawa Hospital; Perley and Rideau Veterans’ Health Centre |
Practice changes |
|
| Bowen72 | Nurse-led discharge
|
Adult ear, nose, throat patients having routine, elective, short-stay surgery | Hospital University Hospital of South Manchester |
Practice changes |
|
| Boyd41 | Communication and leadership
|
NR | Hospitals (2) Part of a hospital conglomerate in Chicago |
Information sharing live |
|
| Brankline47 | Technology-assisted referrals
|
Elderly patients who require nursing home placement after hospital discharge | Academic Medical Centre | Information sharing live Tools and guidelines |
|
| Brown64 | Discharge criteria
|
Adult, ASA physical status I, II, and III patients, 18 years or older, requiring general anaesthesia | Hospital Postoperative recovery area of a large, tertiary-care, academic hospital |
Tools and guidelines Practice changes |
|
| Burr56 | ALC avoidance framework
|
ALC patients | Hospitals (3)
|
Tools and guidelines |
|
| Caminiti42 | Physician accountability
|
Hospital Units: geriatric, medicine, long-term care | Hospital University Hospital of Parma, 1267 beds |
Information sharing live |
|
| Chidwick54 | Change ideas
|
ALC patients | Hospital William Osler Health System |
Practice changes Tools and guidelines Information sharing live |
|
| El-Eid73 | Hospital throughput project using Six Sigma Methodology
|
NR | Hospital (tertiary care teaching hospital) American University of Beirut Medical Centre, 386 beds |
Practice changes |
|
| Gaughan101 | Increasing supply of nursing home beds
|
Patients waiting for hospital discharge | Hospital | Other initiative |
|
| Graham74 | Nurse-led discharge
|
Patients receiving laparoscopic cholecystectomy and laparoscopic inguinal hernia repair | Hospital Leicester Royal Infirmary |
Practice changes |
|
| Gutmanis65 | Behavioural Supports Ontario
|
Individuals with responsive behaviours | South West LHIN | Practice changes Tools and guidelines |
|
| Henwood48 | Change Agent Team
|
Inpatients | Information sharing live Tools and guidelines |
|
|
| Holland57 | Tracking and reporting system
|
Inpatients | Hospital (academic medical centre) | Tools and guidelines |
|
| Katsaliaki102 | Intermediate care services
|
Inpatients | Hampshire Social Services | Other initiative |
|
| Lees-Deutsch66 | Criteria led discharge - Selection of Patients for Efficient and Effective Discharge
|
Patients discharged from the AMU and both short-stay wards | Hospital (acute medicine service with four clinical areas) | Tools and guidelines Practice changes |
|
| Levin94 | Step-up intermediate care units
|
Aged 75+ | Hospital | Infrastructure and finance |
|
| Lian58 | New discharge guidelines for premature babies
|
Premature infants | Hospital Singapore General Hospital |
Tools and guidelines |
|
| Maessen75 | Enhanced recovery after surgery
|
Patients undergoing elective colorectal resection | Hospital | Practice changes |
|
| Mahant (2008)59 | Medical Care Appropriateness Protoco-audit and feedback
|
Paediatric inpatients | Hospital Hospital for Sick Children |
Tools and guidelines |
|
| Mahto 76 | Hospital diabetes outreach service
|
Acutely admitted patients with diabetes | Hospital New Cross Hospital, 700 beds |
Practice changes |
|
| Maloney49 | Patient tracker
|
Inpatients | Hospital Primary Children’s Medical Centre |
Tools and guidelines Information sharing live |
|
| Manville95 | Transitional care unit
|
Elderly ALC patients (70+) | Hospital St Joseph’s Hospital, 22-bed transitional care unit |
Infrastructure and finance |
|
| Meehan77 | Discharge to Assess
|
Patients discharged through D2A | Hospital | Practice changes |
|
| Moeller 60 | Critical pathway
|
Patients with community-acquired pneumonia | Hospital Queen Elizabeth II Health Sciences Centre, 637 beds |
Tools and guidelines |
|
| Mur-Veeman61 | Buffer management
|
Bed blockers | Hospital to nursing home (intermediate care department) | Tools and guidelines |
|
| Niemeijer62 | Lean Six Sigma
|
Trauma patients | Hospital University Medical Centre Groningen, 1339 beds |
Tools and guidelines |
|
| Panis78 | Dutch evaluation protocol
|
Mothers of newborn patients | Hospital Maternity unit of 17 beds (715 total hospital beds) |
Practice changes |
|
| Patel43 | Multidisciplinary team-based structure for discharge rounds
|
Dissatisfied patients with delayed discharge | Hospital University of Colorado Hospital, 673 beds |
Information sharing live |
|
| Pirani44 | Nurse participation and patient and family involvement
|
Those experiencing delayed discharge | NR | Information sharing live |
|
| Qin103 | Simulation modelling
|
Varies based on model | Hospital Flinders Medical Centre (FMC) |
Other initiative |
|
| Rae96 | Delayed discharge project
|
Acute general medical patients | Hospital Dunedin hospital |
Infrastructure and finance |
|
| Roberts50 | Royal Rehabilitation Centre, Sydney, goal length of stay tool
|
Inpatients in two units: SRU (stroke rehabilitation unit) or BIRU (Brain Injury Rehabilitation Unit | Hospital Hampstead Rehabilitation Centre, 128 beds |
Tools and guidelines Information sharing live |
|
| Sampson79 | Diabetes inpatient specialist nurse
|
Diabetes inpatients | Hospital Norfolk and Norwich University Hospital NHS Trust, 989 beds |
Practice changes |
|
| Shah97 | Community Care (Delayed Discharge) Act 2003
|
Inpatient - specialties of Geriatric Medicine (GM) and Old Age Psychiatry (OAP) services | Hospitals | Infrastructure and finance |
GM:
OAP:
|
| Sobotka51 | Hospital-to-home transitional care programme at AHK
|
Paediatric inpatient | Transitional and Respite Centre Almost Home Kids |
Practice changes Information sharing live |
|
| Starr-Hemburrow80 | Home First
|
ALC patients | Hospitals | Practice changes |
|
| Sutherland45 | Build more; Integrated care; and Financial incentives
|
ALC patients | Hospitals | Information sharing recommendation document |
|
| Taber81 | Comprehensive interdisciplinary improvement initiative
|
Adult kidney transplant recipients | Hospital Medical University of South Carolina |
Practice changes |
|
| Udayai82 | Improvement in discharge process - Six Sigma
|
NR | Hospital | Practice changes |
|
| Williams52 | Critical care outreach role
|
Patients discharged from the ICU | Hospital Royal Perth Hospital, 22-bed ICU (570 total beds) |
Practice changes Information sharing live |
|
| Younis53 | Enhanced recovery programme
|
Patients undergoing anterior resection with the formation of a loop ileostomy | Hospital Single district general hospital |
Practice change Information sharing live |
|
| Grey literature | |||||
| Anonymous99 | Expedited discharge fund
|
Uninsured patients | Hospital Iowa City, University of Iowa Hospital, 700 beds |
Infrastructure and finance |
|
| Anonymous46 | Meetings
|
NR | Hospital University of Cincinnati Health University Hospital, 693 beds |
Information sharing live |
|
| Calveley83 | Tiered community-based services
|
NR | Hospital Four Seasons Healthcare, 18 000 beds |
Practice changes |
|
| Manzano-Santaella100 | Payment by Results and Delayed Discharges Act
|
NR | NR | Infrastructure and finance |
|
| Krystal86 | Southlake@Home
|
Medically and socially complex and frail elderly | Hospital Southlake Regional Health Centre |
Practice changes |
|
| Walker2 | Recommendations for improving care for the ageing population
|
NR | NR | Information sharing recommendation document |
|
| North West Community Care Access Centre88 | Wait at home
|
Seniors waiting for LTC placement | NR | Practice changes |
|
| Toronto Central Community Care Access Centre67 | ALC avoidance framework
|
NR | NR | Tools and guidelines |
|
| Province of New Brunswick92 | ALC collaborative committee
|
NR | NR | Information sharing live Practice changes Infrastructure and finance |
|
| NHS Improvement104 | SAFER patient flow bundle
|
NR | NR | Information sharing recommendation document |
|
Red2Green days
|
NR | NR |
|
||
Long-stay patient reviews
|
NR | NR |
|
||
Multiagency Discharge Event
|
NR | NR |
|
||
| Central East LHIN ALC Task Group84 | Home First
|
NR | Hospital Halton Health Services, 459 beds |
Practice changes |
|
| Adams, Care and Repair England98 | Home First
|
Patients (specifically high needs seniors) | NR | Practice changes |
|
| Shah89 | Home First
|
High need seniors (75+) | Trillium Health Partners, various community and long-term care organisations | Practice changes |
|
| Joint Improvement Team85 |
|
ALC patients | 9 community hospital corporations, 14 hospital sites and a mental health centre in one Ontario region 1642 beds across the facilities |
Practice changes |
|
| Adams, Care and Repair England98 | West of England care and repair
|
Older patients | West of England Care and Repair | Infrastructure and finance |
|
| Shah89 | Home First
|
Elderly patients | Hospital/ community in Mississauga Halton Local Health Integration Network | Practice changes |
|
| Joint Improvement Team85 | Home First – 10 actions to transform discharge
|
NR | NR | Practice changes |
|
*Initiative category is based on Doern and Phidd’s adapted framework Hosseus and Pal.39
AHK, almost home kids; ALC, alternate level of care; D2A, discharge to assess; ED, emergency department; ERAS, enhanced recovery after surgery; GM, geriatric medicine; HRH, Humber River Hospital; ICU, intensive care unit; LHIN, local health integration network; LTC, long-term care; MGH, Michael Garron Hospital; N/A, not available; NR, not reported; OAP, old age psychiatry; TGH, Toronto General Hospital.
Based on Doern and Phidd’s adapted framework,39 we categorised the included initiatives as: information sharing (n=19); tools and guidelines (n=19); practice changes (n=36); infrastructure and finance (n=10); or other (n=3), which are described in detail below (see figure 2). Numerous articles used a combination of categories in their initiatives (eg, information sharing and practice change).
Figure 2.
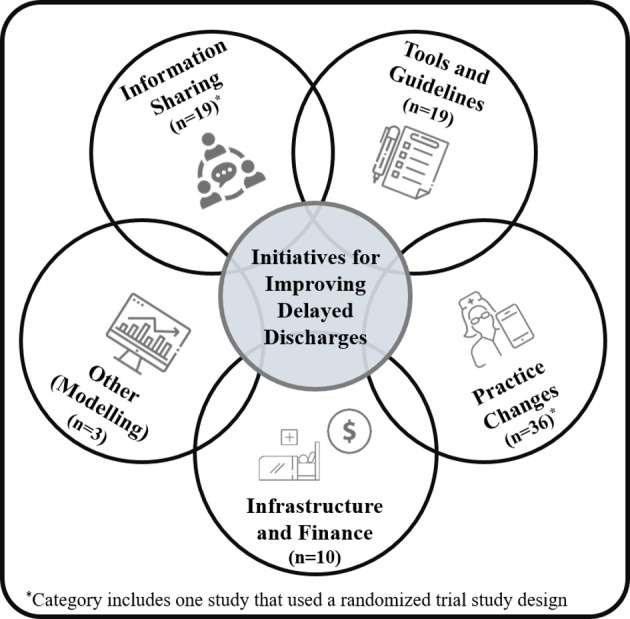
Categories of initiatives for improving delayed hospital discharges.
Information sharing
The information sharing category included initiatives that promoted communication, leadership from senior staff and information exchange within or across organisations.2 40–55 The majority of information sharing initiatives included team meetings and huddles to facilitate communication through in-person interactions between staff, and less often between staff and patients/families.40 41 43 44 46 Information sharing was promoted between multidisciplinary teams and patients to improve length of stay and continuity of care. For example, Adlington et al implemented Plan Do Study Act cycles during weekly quality improvement meetings, in which driver diagrams (visual displays) were used to share information with the multidisciplinary project team on issues affecting length of stay and hospital bed occupancy.40 This information was used to guide practice changes aimed at improving communication during the discharge process (daily rounds, focusing on long-stay patients), bed management (nursing support to prevent deterioration) and community services (email updates and involvement of care coordinators). The majority of initiatives shared information though in-person communication; however, some used technology. Caminiti et al used technology-assisted communication to develop reports and audits to motivate and hold physicians accountable,42 as in some health systems, physicians play a key role in designating patients as having a delayed discharge. Profiles for each physician were created monthly using hospital administrative data (containing length of stay, number of patients discharged that month). All information sharing initiatives resulted in positive outcomes (eg, reduced length of stay and a decrease in delayed discharges).
Tools and guidelines
The tools and guidelines category included initiatives with actionable, concrete steps or processes in the form of tools, guidelines and models to inform practice.47–50 54–67 Physicians and multidisciplinary teams (eg, nurses, social workers, discharge planners) frequently implemented tool and guideline initiatives. A promising initiative within this category included the ALC Avoidance Framework, developed by Burr and colleagues, with the goal of preventing ALC designations and reducing ALC rates.56 67 This framework contains 12 leading practices, with specific strategies for organisational assessment. Some of the leading practices include: providing patients and substitute decision makers with an estimated date of discharge, identifying high-risk patients of becoming ALC and implementing escalation processes for the management of ALC challenges. Additional initiatives focused on improving patient flow through criteria-led discharges (discharging patients once a predetermined set of criteria had been met) and critical pathways/discharge guidelines.
The majority of initiatives categorised as tools and guidelines had positive results,47–49 54–60 62 64–66 which included a reduction in hospital days and length of stay. However, one initiative, the Goal Length of Stay Tool, did not have positive outcomes on length of stay.50 This initiative incorporated information sharing into a computer-based programme to identify patients whose length of stay exceeded their benchmark figure. It had no change on length of stay and was perceived negatively by staff because they did not believe the benchmark figure was an accurate representation of a patient’s current functional status and readiness for discharge.
Practice changes
This category included initiatives that altered how usual care was delivered.51–55 63–66 68–92 Common practice change initiatives included hospital-based, nurse-led discharges and cross-sectoral transitional programmes (eg, Home First, Discharge to Assess, Hospital to Home). Most were implemented by nurses and multidisciplinary teams. Nurse-led and criteria-led discharges often involved a predetermined list of criteria (clinical parameters) that a patient was required to meet in order to be discharged from hospital by a member of the discharge team. For example, Graham et al conducted a retrospective study (N=128) to compare nurse-led and doctor-led discharge (standard discharge pathway) postlaparoscopic surgery.74 For nurse-led discharge, the patient had to meet 13 pre-established criteria (stable vital signs and comparable to baseline on admission; achieved optimal mobility; minimal nausea, vomiting and dizziness; adequate pain control; received written and verbal instructions about postoperative care, etc). When compared with the doctor-led discharge group (n=64), patients in the nurse-led group (n=64) were significantly more likely to be discharged on the day of surgery. In comparing reasons for the success of the nurse-led model, the authors did not tie it to patient factors but rather the ready availability of the nurse specialist who was able to implement the clearly outlined discharge criteria (specific for nurse-led discharge) much more quickly than the doctor-led group (who did not use such criteria).
Another unique example of a practice change initiative was the 7-day Hospital Initiative implemented by Blecker et al.70 The purpose of this observational study was to evaluate the impact of increasing weekend staff (hospitalists, care managers, social workers) and services on length of stay, percent of patients discharged on weekends, 30-day readmission rate and in-hospital mortality rate. This multifaceted intervention resulted in a decreased average length of stay, an increased proportion of weekend discharges and no impact on readmission rates or mortality.
The majority of initiatives categorised as a practice change resulted in positive outcomes on length of stay and rate of discharge delays. However, there were several initiatives that were perceived negatively by patients,77 or had no change68 75 or a negative impact52 on study outcomes (increase in delayed discharges). Meehan et al explored patient experiences with a programme (Discharge to Assess) that discharged patients who were clinically ready but still required support, in order for their needs to be assessed in their own environment (ie, at home).77 Negative experiences were described by participants (patients and caregivers) who indicated feeling ignored, had poor communication with their healthcare providers and were not involved in the decision-making process. Negative outcomes were also identified in Williams et al prospective cohort study.52 This study evaluated the impact of a critical care outreach role on delays in discharge and identified that discharge delays from the intensive care unit increased over the study period with the implementation of this role. The authors emphasised the importance of a multifaceted and collaborative approach (involving multiple stakeholders/ team members), focusing on patient flow throughout the hospital in order to address the numerous factors impacting delays.
Infrastructure and finance
The infrastructure and finance category included initiatives that involved tangible structural or financial changes (eg, building more long-term care beds to facilitate the transition of patients out of hospital, financial penalties for remaining in hospital after being medically ready for discharge).55 92–100 The Community Care (Delayed Discharges) Act in the UK was an initiative identified in multiple articles.93 96 97 100 This initiative required local authorities to make payments to acute hospitals when patients could not be discharged because appropriate community care arrangements had not been made. Although this measure was not necessarily enforced, it created incentive for the hospital and community to work together more collaboratively. Additionally, transitional care units94 95 and discharge funds98 99 were common initiatives implemented to address delayed discharges among elderly patients. Transitional care units focused on rehabilitation to promote recovery and the regaining of independence, while discharge funds paid for services that were preventing the patient from being discharged or returning home (eg, medical equipment, medications, transportation, home repairs). All initiatives categorised as infrastructure and finance had positive results on study outcomes, including reductions in discharge delays, length of stay and cost.93–98
Other initiatives
The other initiatives category included statistical and predictive modelling of initiatives to improve delayed discharges.101–103 These models explored the impact of increasing the supply of nursing home beds,101 potential care pathways for the elderly and reimbursement costs102 and discharge strategies to reduce hospital occupancy.103 Gaughan et al's modelling and empirical analysis identified that increasing the supply of long-term care beds can decrease delayed discharges caused by a lack of social care.101 Their models further emphasised the importance of communication between hospitals and the long-term care sector to reduce social care delayed discharges. Similarly, Katsaliaki et al used discrete-event simulations to determine care pathways and associated costs, in which they identified that adding new beds in hospital or intermediate care could reduce delay times.102
Recommended initiatives: calls to action
Several articles were not evaluations but reports or reviews consisting of recommended initiatives to address delayed hospital discharges, which often combined a number of the categories illustrated above.2 45 92 104 Sutherland and Crump outlined three key solutions for improving delayed discharges in Canada: building more acute and postacute care beds, increasing integrated care and creating financial incentives to improve the quality, quantity and effectiveness of healthcare.45 The authors discussed challenges and limitations to implementing each of these options and emphasised that a potential solution to addressing delayed discharges was to combine the three strategies. Another Canadian report developed recommendations for providing care to the ageing population and those experiencing a delayed discharge.2 Walker outlined recommendations for improving primary care, the care continuum and senior friendly acute care, responding to special needs populations (eg, persons with mental health concerns, addiction and neurological conditions, on dialysis or ventilators), and implementing an ‘Assess and Restore’ model (a programme to help patients maintain or regain functional independence, transition to home and remain in the community for as long as possible).
The NHS improvement (UK) also released a guide in 2019 on reducing long hospital stays.104 This guide contained several recommendations for tackling delayed discharges including: a patient flow bundle (a tool to reduce delays for patients on inpatient wards), Red2Green Days (a visual tool to reduce unnecessary waiting by patients by supporting the rounding process), long-stay patient reviews (weekly reviews of long-stay patients (>20 days), to help tackle obstacles that are delaying discharge) and multiagency discharge events (review of individual patient journeys by bringing together senior staff from the local health and social care system).
Discussion
The purpose of this scoping review was to identify best practices for reducing delayed discharges, examine the characteristics of identified initiatives and develop recommendations for future work. Based on the 66 included articles, our findings showed that: (1) initiatives are focused on quantitative outcomes, with limited assessment of the impact on patient, caregiver and provider experiences; (2) the sustainability of initiatives overtime is not measured (3) there is a lack of important contextual information reported (eg, population characteristics, setting, implementation processes) and (4) there are inconsistencies in how delayed discharges are defined.
This review highlighted where the majority of efforts around addressing delayed discharges have been placed. Practice change was the most common categorisation of initiatives (n=36), followed by information sharing (n=19) and infrastructure and finance (n=19). All initiatives categorised as information sharing and infrastructure and finance reported positive outcomes. Despite reporting positive outcomes, many information sharing initiatives promoted communication between staff, with a limited number targeting communication with patients and families. Additionally, there were more initiatives implemented in a single sector (eg, in hospital) in comparison to cross-sectoral initiatives (eg, hospital and home care).
Length of stay was the most common outcome measured in this scoping review, with a limited number of articles exploring patient, caregiver and provider experiences. For example, could it be considered a success if an initiative does not result in a reduced length of stay, but allows patients to obtain broader goals related to their care (ie, being able to return home) or enhance their care experience? Qualitative methods, including the capturing of patient, caregiver and provider experiences, would allow for a deeper exploration and understanding of success from the perspectives of different stakeholders involved in the initiative.105–107 Experiential evidence on whether an intervention is working is required. As noted in our review, a tool developed to better understand delayed discharge was deemed irrelevant by care providers who felt that the tool captured the wrong information.50 Therefore, capturing providers’ experiences and perspectives are essential in understanding effectiveness of strategies as well as uptake. Most articles included in this scoping review used a quantitative study design, with limited articles using mixed methods or qualitative approaches; thus highlighting a key focus for future research.
The majority of initiatives had an intervention or follow-up period of 1 year, but this ranged from 4 months to 3 years. Based on the limited number initiatives with a follow-up period of longer than 1 year (n=8), there is a need for more formal evaluations with longer follow-up periods to measure the sustainability of initiatives over time. For example, Shelton et al’s Integrated Sustainability Framework consists of five categories of factors associated with the sustainability of interventions across different contexts and settings: outer context (eg, policies, leadership, funding), inner context (eg, culture, mission, funding), intervention characteristics (eg, cost, adaptability, benefit), processes (eg, partnership, training/support, planning, capacity building) and implementer and population characteristics (eg, implementation skills/expertise, attitudes/motivation).108 Shelton et al recommended prospective, multi-level and mixed methods study designs for studying the impact and sustainability of interventions. Overall, the initiatives included in this scoping review had positive short-term impacts, but it is unclear if these outcomes are maintained over time. This emphasises the need to design and implement interventions with sustainability in mind.
The majority of categories of initiatives resulted in positive outcomes; however, initiatives classified as practice change had the most mixed outcomes (positive, negative and no change). Practice changes often require a greater number of resources and are more complex to implement than static solutions (ie, hosting daily rounds, developing a framework, etc). A recent systematic review (2018) conducted by Geerligs et al identified implementation barriers and facilitators of patient-focused, in-hospital interventions,109 highlighting the complex interplay of factors that can impact implementation. Three domains, with the potential to impact the implementation process, were identified: system (environmental context, culture, communication processes and external requirements), staff (commitment and attitudes, understanding and awareness, role identity and skills, ability and confidence) and intervention (ease of integration, face validity, safety and legality and supportive components). Thus, it is important for interventions to be nimble and adaptable to support the changing need of patients, caregivers, providers, organisations and policy contexts over time.
It was also unclear if some initiatives moved problems from one sector to another. For example, adding more intermediate care beds may alleviate pressures in acute care in the short-term but eventually also be at full capacity if community resources are not available. The 7-day hospital discharge initiative highlighted in this review, improved hospital throughput but had no impact on re-admissions,70 suggesting that thinking beyond one sector is required. It is encouraging that most practice change initiatives resulted in improved outcomes, but more clarity is needed to understand what the trade-offs were, as well as how to scale-up the successful initiatives.
Health systems also need to consider their broader goals around delayed hospital discharge—should it only be about reducing delays or should we place an equal focus on optimising patient and caregiver experiences and outcomes? The health system context, including the funding environment, will ultimately shape what interventions get implemented and how they are sustained over time. Some interventions may be considered low value in some countries and contexts and high value in others. Additionally, certain initiatives may be more effective in different environments, as variations in the number of hospital and long-term care beds per capita, infrastructure financing and degree of integration across sectors may impact the outcomes of an initiative. Future research needs to better understand why some strategies may thrive in some environments and not others.
Another key finding identified in the scoping review was the lack of information and details on the implementation strategy (how strategies were implemented, over what time period, how implementation challenges were dealt with), setting (where was it implemented) and population characteristics (who was it implemented for). The implementation of initiatives can be impacted by differences in healthcare system structure and funding. Further, this contextual information is essential for both understanding outcomes, scaling-up and sustainability of interventions because it is not only important to know if the intervention was effective, but also for whom and in what context it was effective.110 111
Finally, this review highlighted a lack of consistency in how delayed discharge was defined, both within and across countries. While there was one definition that was used more frequently (a patient was identified as medically ready/fit for discharge, but remained in hospital), there can be different interpretations of when a patient is considered ‘medically fit’ and who makes this decision. Inconsistent definitions can lead to variations in the reported rates of delayed discharge, which can further impact the perceived applicability and effectiveness of an intervention. Our finding was echoed in a narrative review conducted by Glasby et al, who further explained the challenges differing definitions create when attempting to compare findings.112 In order to mitigate these challenges, it is critical to be more consistent around how delayed discharges are defined.
Future work
From this review, we have identified areas for future research. First, patient, family and provider needs and experiences should be explored during the development and implementation of initiatives aimed at improving delayed discharges. Patient and family engagement is both important and recommended by healthcare and government organisations; however, they are often excluded in the development and write-up of best practice guidelines.113 Second, evaluation studies that track outcomes over a longer period of time should be conducted to study the sustainability of initiatives over time, how they are adapted (developmental evaluations), as well as their impact on other sectors (eg, primary and community care). Third, initiatives should be implemented and integrated across sectors (hospital, primary care and home and community care) to help get at the root of the problem and ensure the implementation of an initiative in one setting does not simply shift the problem to another. Fourth, a review should be conducted to assess the state of knowledge around initiatives that are more upstream in nature (eg, hospital admission avoidance, emergency department diversion and delivery models that proactively address the health and social care needs of individuals in community settings). Finally, there is an opportunity for future research to consider a realist review of the literature on delayed hospital discharge to understand the context, mechanisms of impact, outcomes and theories of change, given that addressing a delayed discharge is a complex problem. As a first step, we sought to include interventions that included hospitals, and this revealed a single sector and reactive approach to addressing delayed discharge.
Limitations
There are a few limitations of this review that should be noted. It is possible that some relevant articles were missed because the search was limited from 1 January 2004 and 16 August 2019 and conducted in English. Our search strategy was comprehensive and we conducted an in-depth search of grey literature to minimise the potential of missed articles. While we did not limit the inclusion of articles to the English language, our search strategy was in English, so there is a possibility that articles published in different languages were not identified. We excluded studies that changed the threshold/timing of discharge (early discharge), as they often focused on cost-savings. We acknowledge that some of these initiatives may have transferable lessons to address discharge delays, and thus, note their exclusion as a potential limitation of this review. Although it is not a requirement for scoping reviews,36 the interventions in this review were not critically appraised, and thus, we cannot make recommendations on which interventions should be scaled up. Given concerns with regression toward the mean, especially for quality improvement projects, any positive results need to be interpreted with caution. Health systems are complex, evolving environments, where various iterations of strategies are regularly implemented, but not necessarily formally reported or published. Future work by our team will include a process evaluation on how strategies are actually implemented in different health system contexts, as well as why they work or do not work.
Ethical considerations
There are a few ethical concerns associated with scoping reviews to be noted. These concerns include authorship, transparency and plagiarism. All authors met the International Committee of Medical Journal Editors’ recommended criteria for authorship and author order was based on overall contribution to the review. We clearly outlined our methods at each stage of the scoping review to ensure transparency and replicability. We also acknowledged individuals who contributed to the review, but who did not warrant authorship. Lastly, when reporting the results of individual studies, we wrote them in our own words and cited appropriately to avoid plagiarism.
Conclusions
This scoping review identified a variety of initiatives addressing delayed discharges across five categories: information sharing, tools and guidelines, practice changes, infrastructure and finance and other. The majority of initiatives were focused on practice changes and many incorporated more than one category. Initiatives were often implemented in a single sector, rather than across sectors. It appears that many strategies implemented in hospitals including communication huddles, nurse-led discharges, home first programmes and building more infrastructure had positive short-term impacts. Many initiatives that led to positive outcomes were implemented by a multidisciplinary team and included a number of components (eg, monthly reports and education). The success of these initiatives is based on a service-led definition of success (effective use of hospital resources), rather than success from the patient and family perspective. This highlights the need to shift to a more patient-centred approach that focuses on improving outcomes and experiences, rather than system and hospital outcomes (ie, length of stay and hospital occupancy) alone. Despite the number of unique initiatives aimed at addressing delayed discharges, current strategies may not be getting at the root of the problem (initiatives/intervention prior to hospital admission) and there is a need for solutions to this problem that have a long-term and sustainable impact.
Supplementary Material
Acknowledgments
The authors would like to thank the University of Toronto librarian for their contribution to the search strategy, as well as Juliane Koropeski (JK) and Maliha Asif (MA) for their help screening articles. We would like to thank the involvement of our stakeholders who provided feedback on our search terms and sent us grey literature. Lastly, we would like to thank our Alternate Level of Care Advisory Council and Ida McLaughlin (chair of council) for their continual support and feedback on this programme of work.
Footnotes
Twitter: @kmkokorelias
Contributors: KK, SJTG, JS, JG and TK were responsible for the conception and design of the study, as well as acquisition of funding for the study. LC, SJTG, KMK and KK led the screening of articles and the analysis and interpretation of data, but all authors contributed to the analysis and interpretation. Drafts of the manuscript were reviewed and revised by all authors. All of the authors read and approved the final manuscript.
Funding: This work was supported by the Canadian Institutes of Health Research-Transitions in Care Strategic Funding Initiative on Best and Wise Practices (Grant #163064). KK holds the Dr Mathias Gysler Research Chair in Patient and Family Centred Care. SJTG and TK are funded by the Canadian Institutes of Health Research Embedded Scientist Salary Award on Transitions in Care working with Ontario Health (Quality); the award also supported staff to assist with screening.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article or uploaded as online supplemental information.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
References
- 1.Bate A Delayed transfers of care in the NHS, 2017: 1–20. [Google Scholar]
- 2.Walker D Caring for our aging population and addressing alternate level of care: report submitted to the Minister of health and long-term care. Canada, 2011. [Google Scholar]
- 3.Rojas-García A, Turner S, Pizzo E, et al. Impact and experiences of delayed discharge: a mixed-studies systematic review. Health Expect 2018;21:41–56. 10.1111/hex.12619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barnable A, Welsh D, Lundrigan E, et al. Analysis of the influencing factors associated with being designated alternate level of care. Home Health Care Manag Pract 2015;27:3–12. 10.1177/1084822314539164 [DOI] [Google Scholar]
- 5.McCloskey R, Jarrett P, Stewart C, et al. Alternate level of care patients in hospitals: what does dementia have to do with this? Can Geriatr J 2014;17:88–94. 10.5770/cgj.17.106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Walker H, Langton D, Thomson L. 'New to forensic'; implementing a problem-based introductory educational programme for forensic practitioners in Scotland. J Psychiatr Ment Health Nurs 2011;18:934–42. 10.1111/j.1365-2850.2011.01778.x [DOI] [PubMed] [Google Scholar]
- 7.Jasinarachchi KH, Ibrahim IR, Keegan BC, et al. Delayed transfer of care from NHS secondary care to primary care in England: its determinants, effect on hospital bed days, prevalence of acute medical conditions and deaths during delay, in older adults aged 65 years and over. BMC Geriatr 2009;9:4. 10.1186/1471-2318-9-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rosman M, Rachminov O, Segal O, et al. Prolonged patients' in-hospital waiting period after discharge eligibility is associated with increased risk of infection, morbidity and mortality: a retrospective cohort analysis. BMC Health Serv Res 2015;15:246–46. 10.1186/s12913-015-0929-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Everall AC, Guilcher SJT, Cadel L, et al. Patient and caregiver experience with delayed discharge from a hospital setting: a scoping review. Health Expect 2019;22:863–73. 10.1111/hex.12916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Amy C, Zagorski B, Chan V, et al. Acute care alternate-level-of-care days due to delayed discharge for traumatic and non-traumatic brain injuries. Healthc Policy 2012;7:41–55. [PMC free article] [PubMed] [Google Scholar]
- 11.Hwabejire JO, Kaafarani HMA, Imam AM, et al. Excessively long Hospital stays after trauma are not related to the severity of illness: let's aim to the right target! JAMA Surg 2013;148:956–61. 10.1001/jamasurg.2013.2148 [DOI] [PubMed] [Google Scholar]
- 12.Challis D, Hughes J, Xie C, et al. An examination of factors influencing delayed discharge of older people from hospital. Int J Geriatr Psychiatry 2014;29:160–8. 10.1002/gps.3983 [DOI] [PubMed] [Google Scholar]
- 13.Costa AP, Hirdes JP. Clinical characteristics and service needs of Alternate-Level-of-Care patients waiting for long-term care in Ontario hospitals. Healthc Policy 2010;6:32–46. 10.12927/hcpol.2010.21899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Costa AP, Poss JW, Peirce T, et al. Acute care inpatients with long-term delayed-discharge: evidence from a Canadian health region. BMC Health Serv Res 2012;12:172. 10.1186/1472-6963-12-172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kozyrskyi A, De Coster C, St John P. Long stay patients in Winnipeg acute care hospitals. Healthc Manage Forum 2002;Suppl:15–20. 10.1016/s0840-4704(10)60177-9 [DOI] [PubMed] [Google Scholar]
- 16.Lorenzo RD, Formicola V, Carra E, et al. Risk factors for long-stay in an Italian acute psychiatric ward: a 7-year retrospective analysis. J Nurs Educ Pract 2013;4:p68 10.5430/jnep.v4n1p68 [DOI] [Google Scholar]
- 17.Rogers A, Clark EH, Rittenhouse K, et al. Breaking down the barriers! factors contributing to barrier days in a mature trauma center. J Trauma Acute Care Surg 2014;76:191–5. 10.1097/TA.0b013e3182aa3d5f [DOI] [PubMed] [Google Scholar]
- 18.Mitchell F, Gilmour M, McLaren G. Hospital discharge: a descriptive study of the patient journey for frail older people with complex needs. J Integr Care 2010;18:30–6. 10.5042/jic.2010.0247 [DOI] [Google Scholar]
- 19.Tan WS, Chong WF, Chua KSG, et al. Factors associated with delayed discharges after inpatient stroke rehabilitation in Singapore. Ann Acad Med Singap 2010;39:435–41. [PubMed] [Google Scholar]
- 20.Landeiro F, Leal J, Gray AM. The impact of social isolation on delayed Hospital discharges of older hip fracture patients and associated costs. Osteoporos Int 2016;27:737–45. 10.1007/s00198-015-3293-9 [DOI] [PubMed] [Google Scholar]
- 21.Poulos CJ, Magee C, Bashford G, et al. Determining level of care appropriateness in the patient journey from acute care to rehabilitation. BMC Health Serv Res 2011;11:291–91. 10.1186/1472-6963-11-291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zeitz KM, Carter L, Robinson C. The ebbs and flows of changing acute bed capacity delays. Aust Health Rev 2013;37:66–9. 10.1071/AH11077 [DOI] [PubMed] [Google Scholar]
- 23.Anderson ME, Glasheen JJ, Anoff D, et al. Understanding predictors of prolonged hospitalizations among general medicine patients: a guide and preliminary analysis. J Hosp Med 2015;10:623–6. 10.1002/jhm.2414 [DOI] [PubMed] [Google Scholar]
- 24.Hendy P, Patel JH, Kordbacheh T, et al. In-depth analysis of delays to patient discharge: a metropolitan teaching hospital experience. Clin Med 2012;12:320–3. 10.7861/clinmedicine.12-4-320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Salonga-Reyes A, Scott IA. Stranded: causes and effects of discharge delays involving non-acute in-patients requiring maintenance care in a tertiary hospital general medicine service. Aust Health Review 2017;41:54–62. 10.1071/AH15204 [DOI] [PubMed] [Google Scholar]
- 26.Sutherland JM, Repin N, Crump RT. Paying for hospital services: a hard look at the options. Toronto, Canada: CD Howe Institute, 2013: 1–32. [Google Scholar]
- 27.Sutherland J Hospital payment policy in Canada: options for the future. Canadian Health Services Research Foundation, 2011. [Google Scholar]
- 28.Ontario Ministry of Health and Long-Term Care Quality-based procedures indicators: an implementation guidance document. Ontario, Canada, 2014: 1–38. [Google Scholar]
- 29.David G, Polsky D. Economics of Home Health Services : Culyer AJ, Encyclopedia of health economics. San Diego: Elsevier, 2014: 477–83. [Google Scholar]
- 30.Treasury HM Spring budget 2017. United Kingdom, 2017. [Google Scholar]
- 31.Knowles G, Burke MR, Carr M. Independent expert review of delayed discharges: Department of health, 2018. [Google Scholar]
- 32.Fagan L 'Bed blockers' costing Ottawa hospitals millions. Glut of patients awaiting more appropriate care a 'crisis,' health workers say. Ottawa: CBC News, 2019. [Google Scholar]
- 33.McCloskey R, Jarrett P, Stewart C. The untold story of being designated an alternate level of care patient. Healthc Policy 2015;11:76–89. 10.12927/hcpol.2015.24364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Munn Z, Peters MDJ, Stern C, et al. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol 2018;18:143. 10.1186/s12874-018-0611-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5:69. 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467–73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 37.Bramer WM, Giustini D, de Jonge GB, et al. De-duplication of database search results for systematic reviews in endnote. J Med Libr Assoc 2016;104:240–3. 10.3163/1536-5050.104.3.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Babineau J Product review: Covidence (systematic review software). J Can Health Libr Assoc 2014;35:68–71. 10.5596/c14-016 [DOI] [Google Scholar]
- 39.Doern GB, Phidd RW. Canadian public policy: ideas, stucture and process. 2nd Toronto, Canada: Nelson Canada, 1992. 10.2307/3552071 [DOI] [Google Scholar]
- 40.Adlington K, Brown J, Ralph L, et al. Better care: reducing length of stay and bed occupancy on an older adult psychiatric ward. BMJ Open Qual 2018;7:e000149 10.1136/bmjoq-2017-000149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Boyd SS Hospital administrators' strategies for reducing delayed Hospital discharges and improving profitability. Walden Dissertations and Doctoral Studies 2017:1. [Google Scholar]
- 42.Caminiti C, Meschi T, Braglia L, et al. Reducing unnecessary Hospital days to improve quality of care through physician accountability: a cluster randomised trial. BMC Health Serv Res 2013;13:14. 10.1186/1472-6963-13-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Patel H, Yirdaw E, Yu A, et al. Improving early discharge using a team-based structure for discharge multidisciplinary rounds. Prof Case Manag 2019;24:83–9. 10.1097/NCM.0000000000000318 [DOI] [PubMed] [Google Scholar]
- 44.Ali Pirani SS Prevention of delay in the patient discharge process: an emphasis on nurses' role. J Nurses Staff Dev 2010;26:E1–5. 10.1097/NND.0b013e3181b1ba74 [DOI] [PubMed] [Google Scholar]
- 45.Sutherland J, Crump R. Alternative Level of Care: Canada’s Hospital Beds, the Evidence and Options. Hcpol 2013;9:26–34. 10.12927/hcpol.2013.23480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Anonymous Patient flow initiatives decrease LOS, up capacity. Hosp Case Manag 2010;18:117–24. [PubMed] [Google Scholar]
- 47.Brankline AL, Coyle CM, Jencks KA, et al. Practical innovations: technology-assisted referrals. Soc Work Health Care 2009;48:768–76. 10.1080/00981380902958213 [DOI] [PubMed] [Google Scholar]
- 48.Henwood M Effective partnership working: a case study of hospital discharge. Health Soc Care Community 2006;14:400–7. 10.1111/j.1365-2524.2006.00651.x [DOI] [PubMed] [Google Scholar]
- 49.Maloney CG, Wolfe D, Gesteland PH, et al. A tool for improving patient discharge process and hospital communication practices: the "Patient Tracker". AMIA Annu Symp Proc 2007:493–7. [PMC free article] [PubMed] [Google Scholar]
- 50.Roberts K, Stiller K, Harling R, et al. Impacts and perceptions of a computer-based length of stay benchmarking program. Int J Ther Rehabil 2013;20:237–45. 10.12968/ijtr.2013.20.5.237 [DOI] [Google Scholar]
- 51.Sobotka SA, Agrawal RK, Msall ME. Prolonged hospital discharge for children with technology dependency: a source of health care disparities. Pediatr Ann 2017;46:e365–70. 10.3928/19382359-20170919-01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Williams TA, Leslie GD, Brearley L, et al. Discharge delay, room for improvement? Aust Crit Care 2010;23:141–9. 10.1016/j.aucc.2010.02.003 [DOI] [PubMed] [Google Scholar]
- 53.Younis J, Salerno G, Fanto D, et al. Focused preoperative patient stoma education, prior to ileostomy formation after anterior resection, contributes to a reduction in delayed discharge within the enhanced recovery programme. Int J Colorectal Dis 2012;27:1–5. 10.1007/s00384-011-1252-2 [DOI] [PubMed] [Google Scholar]
- 54.Chidwick P, Oliver J, Ball D, et al. Six change ideas that significantly minimize alternate level of care (alc) days in acute care hospitals. Healthc Q 2017;20:37–43. 10.12927/hcq.2017.25226 [DOI] [PubMed] [Google Scholar]
- 55.Baumann M, Evans S, Perkins M, et al. Organisation and features of hospital, intermediate care and social services in English sites with low rates of delayed discharge. Health Soc Care Community 2007;15:295–305. 10.1111/j.1365-2524.2007.00697.x [DOI] [PubMed] [Google Scholar]
- 56.Burr E, Dickau S. Leading practices in alternate levels of care (alc) avoidance: a standardized approach. Hcq 2017;20:44–7. 10.12927/hcq.2017.25227 [DOI] [PubMed] [Google Scholar]
- 57.Holland DE, Pacyna JE, Gillard KL. Tracking discharge delays: critical first step toward mitigating process Breakdowns and Inefficiencies. J Nurs Care Qual 2016;31:17–23. [DOI] [PubMed] [Google Scholar]
- 58.Lian YC, Ying SHK, Peng CC, et al. Early discharge study for premature infants: Singapore General Hospital. Perm J 2008;12:15–18. 10.7812/TPP/08-040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mahant S, Peterson R, Campbell M, et al. Reducing inappropriate hospital use on a general pediatric inpatient unit. Pediatrics 2008;121:e1068–73. 10.1542/peds.2007-2898 [DOI] [PubMed] [Google Scholar]
- 60.Moeller JJ, Ma M, Hernandez P, et al. Discharge delay in patients with community-acquired pneumonia managed on a critical pathway. Can J Infect Dis Med Microbiol 2006;17:109–13. 10.1155/2006/375645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mur-Veeman I, Govers M. Buffer management to solve bed-blocking in the Netherlands 2000-2010. Cooperation from an integrated care chain perspective as a key success factor for managing patient flows. Int J Integr Care 2011;11:e080. 10.5334/ijic.650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Niemeijer GC, Trip A, Ahaus KTB, et al. Quality in trauma care: improving the discharge procedure of patients by means of lean six sigma. J Trauma 2010;69:614–9. 10.1097/TA.0b013e3181e70f90 [DOI] [PubMed] [Google Scholar]
- 63.Ardagh MW, Tonkin G, Possenniskie C. Improving acute patient flow and resolving emergency department overcrowding in New Zealand hospitals--the major challenges and the promising initiatives. N Z Med J 2011;124:64–73. [PubMed] [Google Scholar]
- 64.Brown I, Jellish WS, Kleinman B, et al. Use of postanesthesia discharge criteria to reduce discharge delays for inpatients in the postanesthesia care unit. J Clin Anesth 2008;20:175–9. 10.1016/j.jclinane.2007.09.014 [DOI] [PubMed] [Google Scholar]
- 65.Gutmanis I, Speziale J, Bussel L, et al. The South West local health integration network behavioural supports Ontario experience. Hcq 2016;18:50–6. 10.12927/hcq.2016.24482 [DOI] [PubMed] [Google Scholar]
- 66.Lees-Deutsch L, Jackson J, Balaji A, et al. Developing a process for Criteria-Led discharge: selection of patients for efficient and effective discharge (speed). J Nurs Care Qual 2020;35:35:140–6. 10.1097/NCQ.0000000000000423 [DOI] [PubMed] [Google Scholar]
- 67.Toronto Central Community Care Access Centre ALC avoidance leading practices and improvement strategies for the acute care sector. Ontario, Canada, 2015. [Google Scholar]
- 68.Arendts G, Fitzhardinge S, Pronk K, et al. Front-loading allied health intervention in the emergency department does not reduce length of stay for admitted older patients. Int J Clin Pract 2013;67:807–10. 10.1111/ijcp.12153 [DOI] [PubMed] [Google Scholar]
- 69.Béland F, Bergman H, Lebel P, et al. A system of integrated care for older persons with disabilities in Canada: results from a randomized controlled trial. J Gerontol A-Biol 2006;61:367–73. 10.1093/gerona/61.4.367 [DOI] [PubMed] [Google Scholar]
- 70.Blecker S, Goldfeld K, Park H, et al. Impact of an intervention to improve weekend hospital care at an academic medical center: an observational study. J Gen Intern Med 2015;30:1657–64. 10.1007/s11606-015-3330-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Boutette M, Hoffer A, Plant J, et al. Establishing an integrated model of subacute care for the frail elderly. Healthc Manage Forum 2018;31:133–6. 10.1177/0840470418774807 [DOI] [PubMed] [Google Scholar]
- 72.Bowen A, Kumar R, Howard J, et al. Nurse led discharge: improving efficiency, safely. Clin Govern Int J 2014;19:110–6. 10.1108/CGIJ-03-2013-0007 [DOI] [Google Scholar]
- 73.El-Eid GR, Kaddoum R, Tamim H, et al. Improving hospital discharge time: a successful implementation of six sigma methodology. Medicine 2015;94:e633. 10.1097/MD.0000000000000633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Graham L, Neal CP, Garcea G, et al. Evaluation of nurse-led discharge following laparoscopic surgery. J Eval Clin Pract 2012;18:19–24. 10.1111/j.1365-2753.2010.01510.x [DOI] [PubMed] [Google Scholar]
- 75.Maessen JMC, Dejong CHC, Kessels AGH, et al. Length of stay: an inappropriate readout of the success of enhanced recovery programs. World J Surg 2008;32:971–5. 10.1007/s00268-007-9404-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mahto R, Venugopal H, Vibhuti VS, et al. The effectiveness of a hospital diabetes outreach service in supporting care for acutely admitted patients with diabetes. QJM 2009;102:203–7. 10.1093/qjmed/hcn174 [DOI] [PubMed] [Google Scholar]
- 77.Meehan L, Banarsee R, Dunn-Toroosian V, et al. Improving outcomes for patients discharged early using a home assessment scheme. London J Prim Care 2018;10:62–7. 10.1080/17571472.2018.1489467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Panis LJGG, Verheggen FWSM, Pop P, et al. The impact of hospital discharge on inappropriate hospital stay. Int J Health Care Qual Assur Inc Leadersh Health Serv 2004;17:189–93. 10.1108/09526860410541504 [DOI] [PubMed] [Google Scholar]
- 79.Sampson MJ, Crowle T, Dhatariya K, et al. Trends in bed occupancy for inpatients with diabetes before and after the introduction of a diabetes inpatient specialist nurse service. Diabet Med 2006;23:1008–15. 10.1111/j.1464-5491.2006.01928.x [DOI] [PubMed] [Google Scholar]
- 80.Starr-Hemburrow L, Parks JM, Bisaillon S. Home first: reducing ALC and achieving better outcomes for seniors through inter-organizational collaboration. Healthc Q 2011;14:70–6. 10.12927/hcq.2011.22162 [DOI] [PubMed] [Google Scholar]
- 81.Taber DJ, Pilch NA, McGillicuddy JW, et al. Improved patient safety and outcomes with a comprehensive interdisciplinary improvement initiative in kidney transplant recipients. Am J Med Qual 2013;28:103–12. 10.1177/1062860612450309 [DOI] [PubMed] [Google Scholar]
- 82.Udayai K, Kumar P. Implementing six sigma to improve hospital discharge process. Int J Pharm Sci Res 2012;3:4528–32. [Google Scholar]
- 83.Calveley P Doing, not talking: hospital admission avoidance. Nursing and Residential Care 2007;9:230–2. 10.12968/nrec.2007.9.5.23554 [DOI] [Google Scholar]
- 84.Central East LHIN ALC Task Group Alternate level of care systems issues and recommendations. Ontario, Canada, 2008. [Google Scholar]
- 85.Joint Improvement Team Home First - Ten Actions to Transform Discharge. United Kingdom, 2013. [Google Scholar]
- 86.Krystal A Southlake at home Webinar. Canada, 2019. [Google Scholar]
- 87.LHIN Collaborative Sharing Best Practices: Transition Management in Ontario - Home First: Implementation Guide and Toolkit. Ontario, Canada, 2011. [Google Scholar]
- 88.North West Community Care Access Centre Wait at home fact sheet. Ontario, Canada, 2011. [Google Scholar]
- 89.Shah N A new philosophy towards solving the alc crisis (home first. Ontario, Canada, 2010. [Google Scholar]
- 90.Shah N A call to action on ER/ALC: promoting effective care across the health continuum. Ontario, Canada, 2011. [Google Scholar]
- 91.Starr-Hemburrow L Home First - Optimizing Patient Flow and Patient Centred Care Canada, 2010. [Google Scholar]
- 92.Province of New Brunswick Health annual report 2016-2017. New Brunswick, Canada, 2017. [Google Scholar]
- 93.Behan D Delayed transfers of care — an early review of progress. J Integr Care 2005;13:43–8. 10.1108/14769018200500008 [DOI] [Google Scholar]
- 94.Levin KA, Crighton E. Measuring the impact of step down intermediate care on delayed discharge: an interrupted time series analysis. J Epidemiol Community Health 2019;73:674–9. 10.1136/jech-2018-211628 [DOI] [PubMed] [Google Scholar]
- 95.Manville M, Klein MC, Bainbridge L. Improved outcomes for elderly patients who received care on a transitional care unit. Can Fam Physician 2014;60:e263–71. [PMC free article] [PubMed] [Google Scholar]
- 96.Rae B, Busby W, Millard PH. Fast-tracking acute hospital care - from bed crisis to bed crisis. Aust. Health Review 2007;31:50–62. 10.1071/AH070050 [DOI] [PubMed] [Google Scholar]
- 97.Shah A The impact of the community care (delayed discharge) act 2003 on the length of stay and bed occupancy in old age psychiatry units in England. Int J Geriatr Psychiatry 2007;22:1164–5. 10.1002/gps.1808 [DOI] [PubMed] [Google Scholar]
- 98.Adams S Care & Repair England. Reducing Delayed Transfer of Care through housing interventions: Evidence of Impact. United Kingdom, 2017. [Google Scholar]
- 99.Expedited discharge fund helps uninsured patients. Plan frees up beds for patients who can pay. Hosp Case Manag 2008;16:70–5. [PubMed] [Google Scholar]
- 100.Manzano-Santaella A Payment by results and delayed discharges. Bri J Healthcare Manag 2009;15:440–3. 10.12968/bjhc.2009.15.9.44008 [DOI] [Google Scholar]
- 101.Gaughan J, Gravelle H, Siciliani L. Testing the bed-blocking hypothesis: does nursing and care home supply reduce delayed Hospital discharges? Health Econ 2015;24(Suppl 1):32–44. 10.1002/hec.3150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Katsaliaki K, Brailsford S, Browning D, et al. Mapping care pathways for the elderly. J Health Organ Manag 2005;19:57–72. 10.1108/14777260510592130 [DOI] [PubMed] [Google Scholar]
- 103.Qin S, Thompson C, Bogomolov T, et al. Hospital occupancy and discharge strategies: a simulation-based study. Intern Med J 2017;47:894–9. 10.1111/imj.13485 [DOI] [PubMed] [Google Scholar]
- 104.NHS Improvement Guide to reducing long Hospital stays. United Kingdom, 2018. [Google Scholar]
- 105.Hamilton AB, Finley EP. Qualitative methods in implementation research: an introduction. Psychiatry Res 2019;280:112516 10.1016/j.psychres.2019.112516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Southam-Gerow MA, Dorsey S. Qualitative and mixed methods research in dissemination and implementation science: introduction to the special issue. J Clin Child Adolesc Psychol 2014;43:845–50. 10.1080/15374416.2014.930690 [DOI] [PubMed] [Google Scholar]
- 107.Qualitative Research in Implementation Science group Qualitative methods in implementation science. United States: National Cancer Institute, Division of Cancer Control and Population Sciences, 2019: 1–31. [Google Scholar]
- 108.Shelton RC, Cooper BR, Stirman SW. The sustainability of evidence-based interventions and practices in public health and health care. Annu Rev Public Health 2018;39:55–76. 10.1146/annurev-publhealth-040617-014731 [DOI] [PubMed] [Google Scholar]
- 109.Geerligs L, Rankin NM, Shepherd HL, et al. Hospital-based interventions: a systematic review of staff-reported barriers and facilitators to implementation processes. Implementation Sci 2018;13:36 10.1186/s13012-018-0726-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Green LW, Glasgow RE. Evaluating the relevance, generalization, and applicability of research: issues in external validation and translation methodology. Eval Health Prof 2006;29:126–53. 10.1177/0163278705284445 [DOI] [PubMed] [Google Scholar]
- 111.Balasubramanian BA, Cohen DJ, Davis MM, et al. Learning evaluation: blending quality improvement and implementation research methods to study healthcare innovations. Implementation Sci 2015;10:31 10.1186/s13012-015-0219-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Glasby J, Littlechild R, Pryce K. Show me the way to go home: a narrative review of the literature on delayed Hospital discharges and older people. Br J Soc Work 2004;34:1189–97. 10.1093/bjsw/bch136 [DOI] [Google Scholar]
- 113.Zhao G, Kennedy C, Mabaya G, et al. Patient engagement in the development of best practices for transitions from hospital to home: a scoping review. BMJ Open 2019;9:e029693 10.1136/bmjopen-2019-029693 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-044291supp001.pdf (133.6KB, pdf)