Abstract
There is increasing recognition that young children’s self-regulation provides a foundation for overall wellness later in life. Yet, infants reared in poverty may exhibit less-developed self-regulation compared to their more advantaged peers. Factors associated with poverty that may influence early self-regulation include maternal depression and parenting self-efficacy. However, few researchers have examined how both parenting self-efficacy and maternal depression may affect young children’s self-regulation. The purpose of this study was to investigate the associations among maternal depression, parenting self-efficacy, and infant self-regulation for a racially diverse sample of 142 mother-infant dyads living in low-income households in the United States. Maternal depressive symptomatology was determined with the Edinburgh Postnatal Depressive Scale. Parenting self-efficacy was determined with a self-report measure, reflecting caregivers’ mindset or feelings reflecting competency as a parent of an infant. Infant self-regulation was measured by parental report of the Infant Behavior Questionnaire Short Form Effortful Control subscale. While maternal depressive symptomatology and self-efficacy were directly and significantly correlated with infant self-regulation, results of a mediation model suggested that parenting self-efficacy mediated the relationship between maternal depressive symptomatology and infant self-regulation. Lower maternal depressive symptomatology predicted better parenting self-efficacy, in turn predicting better infant self-regulation. This study increases our understanding of how early factors shape the self-regulation of infants reared in low-income homes – highlighting the potential role of targeting parenting self-efficacy for parenting interventions for mothers experiencing depressive symptoms.
Keywords: self-regulation, mother-infant dyad, maternal depression, maternal self-efficacy, mediation
Over the past decade, there has been growing recognition that early childhood self-regulation provides a foundation for overall adult well-being (Moffitt et al., 2011). Self-regulation refers to the concerted, effortful control of behavior and thoughts to meet one’s goals (Blair & Diamond, 2008; McClelland, Geldhof, Cameron, & Wanless, 2015; McCoy & Raver, 2014; Rothbart & Rueda, 2005), which evolves over development. Self-regulation development may be particularly sensitive to environmental influences during the first year of life (Shonkoff, 2012), a timeframe in which the child’s self-regulation skills emerge (Berger, 2011; Rothbart, Sheese, Rueda, & Posner, 2011) and stabilize (Kochanska, Murray, & Harlan, 2000; Kochanska, Tjebkes, & Forman, 1998). Evidence has also suggested a heightened vulnerability for low self-regulation among youngsters living in low-income homes as compared to those more socioeconomically advantaged (e.g., Radesky, Silverstein, Zuckerman, & Christakis, 2014). Given the significant developmental trajectory from early self-regulation, it is important for scientists to identify contributors to early self-regulation development for youngsters born into low-income homes.
A key environmental influence negatively associated with infant self-regulation development is maternal depression (Goodman & Gotlib, 1999). Maternal depression can adversely affect a child’s self-regulation well into adulthood (Goodman & Gotlib, 1999) and even in future generations (Hancock, Mitrou, Shipley, Lawrence, & Zubrick, 2013). Depression is highly prevalent among mothers living in poverty, affecting nearly 1 in 2 (Chung, McCollum, Elo, Lee, & Culhane, 2004) compared to depression affecting 1 in 5 mothers overall (Gaynes et al., 2005). Maternal depression is also 71–79% more prevalent among mothers of male infants versus female (Myers & Johns, 2019). Maternal depression is thought to indirectly shape infant self-regulation through its effect on maternal parenting characteristics (Carter, Garrity-Rokous, Chazan-Cohen, Little, Briggs-Gowan, 2001; Goodman & Gotlib, 1999; Granat et al., 2017) such as behavior and mindset.
While much research has examined the effect of maternal depression on parenting behavior behavior (e.g., Carter et al., 2001), limited studies have examined how maternal depression may affect parenting mindset such as parenting self-efficacy. Parenting self-efficacy is the mindset or thoughts that one is competently parenting their child (Sevigny & Loutzenhiser, 2010; Teti & Gelfand, 1991; Vance & Brandon, 2017). Parents with higher parenting self-efficacy have a higher likilhood of engaging in quality parenting practices that support optimal self-regulation development in children (Wittkowski, Garrett, Calam, Weisberg, 2017). As such, parenting self-efficacy has sometimes been the focus of effective parenting interventions for mothers with distress (Tucker, Gross, Fogg, Delaney, Lapporte, 1998). While discussions of parenting self-efficacy often appear in popular parenting blogs and editorials (e.g., Organ, n.d.), it has not been frequently examined in its connection with maternal depression and infant self-regulation in the research literature. Parenting self-efficacy may be an important consideration in understanding early self-regulation and designing early self-regulation interventions – especially for those children with mothers experiencing depression or postpartum depression, which has a high likelihood of occuring for mothers living in low income homes.
While studies have reported linkages among maternal depression, parenting self-efficacy, and infant self-regulation, these interrelationships have rarely been explored simultaneously. For example, Atkins (2010) outlined how numerous theories connect maternal depression and self-efficacy, particularly for mothers of lower socioeconmic status. Leerkes and Crockenberg (2002) found relationships among maternal self-efficacy, caregiving behavior, and infant self-regulation. In turn, other work has found that parenting self-efficacy is associated with children’s self-regulation (Coleman & Karraker, 2003). In the aggregate, such work suggests that parenting self-efficacy may represent a key pathway through which maternal depression shapes the development of self-regulation in young children. Teti and Gelfand (1991) were the only researchers of which we are aware to have explored this premise in mother-infant dyads focused on a sample of mostly white, married, educated, and mother-infant dyads practicing Mormonism. Teti and Gelfand showed that maternal self-efficacy was negatively correlated with maternal depression and with perceptions of infant difficulty. Teti and Gelfand also showed that depressed mothers had lower scores of maternal self-efficacy versus those who were not depressed. Together, this evidence suggests a significant interplay among maternal depression, parenting self-efficacy, and infant self-regulation and that maternal self-efficacy may mediate the relationship between maternal depression and infant self-regulation. However, to the best of our knowledge, researchers have not examined these relations in mothers and infants living in low-income homes.
The potential mediating relationship of maternal parenting self-efficacy on maternal depression and infant self-regulation may be considered within the lens of cognitive behavior theory by Beck (1979), which outlines key connections among feelings, thoughts, and behaviors – specifically for those experiencing depression. According to cognitive behavior theory, Beck surmises that how an individual feels (i.e. depression) can affect their thinking and behaviors in a negative fashion. From this theoretic perspective and extending this theory to the mother-infant dyad, the mother’s feelings (e.g., depression symptomatology) predicts her thoughts and appraisals (e.g., maternal parenting self-efficacy), which in turn influences the mother’s perception of the infant’s self-regulation, an important reflection of the infant’s actual self-regulatory behavior. This may be because mothers, versus other assessors or observers, typically have much familiarity with their children’s behavior over time and over a variety of contexts (Mangelsdorf, Schoppe, & Buur, 2000), and in situation-specific interactions (Achenbach, McConaughy, & Howell, 1987). Further extending Beck’s cognitive behavior theory for those experiencing depression, we might surmise that a mother’s depression will influence how she thinks about her parenting abilities of an infant. Depression, or even increased symptoms of depression, can create a tendency to view the world in a negative way. Even without depression, caring for an infant can be challenging and/or overwhelming – but with the extra burden of depression, a mother may further negatively misinterpret her parenting abilities of an infant (i.e., parenting self-efficacy). The mother’s negative view of her parenting self-efficacy may in turn influence how she appraises her infant’s self-regulation. If the mother thinks that she is not competently parenting, she may view the infant as having poor self-regulatory abilities, to include poor soothing abilities and high distractibility. The mother’s negative thoughts or mindset of her parenting self-efficacy may also influence her actual parenting. That is, the mother’s poor view of her parenting self-efficacy will influence actual poor parenting behaviors that will then cause the mother to misinterpret her infant’s communication cues and needs. Because the mother is not appropriately meeting the communication demands of the infant, the infant will react in such a way that will seem that it has poor self-regulation because the mother is not meeting the infant’s needs. As such, a mother’s depression or increasing depressive symptoms will influence her negative thoughts about her parenting self-efficacy, which will then in turn influence how she appraises her infant’s self-regulation abilities.
For the present study, we extend work on the interplay among maternal depression, parenting self-efficacy, and infant self-regulation in a sample of mother-infant dyads residing in low-income homes. This is an important contribution to the literature because mother-infant dyads residing in low-income homes are disproportionately at risk for maternal depression and adverse infant self-regulation compared to their more socioeconomically advantaged peers. As such, potential targets for interventions for this low-income group at high-risk for maternal depression and adverse self-regulation need to be identified. As the literature reviewed suggests that the linkage between maternal depression and infant self-regulation may be through parenting self-efficacy, parenting self-efficacy could be a potential target for improving early self-regulation among children in low-income homes. The purpose of this study was to investigate the associations among maternal depression symptomatology, parenting self-efficacy, and infant self-regulation for mother-infant dyads living in low-income homes in the United States. There are two specific aims of this study. Aim 1 is to characterize relationships among maternal depression symptoms, maternal parenting self-efficacy, and infant self-regulation for high-risk dyads – that is, dyads at high risk for maternal depression and poor infant self-regulation given that they live in low-income households. Consistent with prior literature, we hypothesize that maternal depression is negatively associated with parenting self-efficacy and infant self-regulation, but that parenting self-efficacy is positively associated with infant self-regulation. Aim 2 is to test whether and the extent to which maternal parenting self-efficacy is the mediating pathway through which maternal depression symptomatology predicts infant self-regulation. Based on Beck’s (1979) cognitive behavior theory, we hypothesize that maternal depression symptomatology indirectly predicts infant self-regulation through parenting self-efficacy.
Methods
Participants
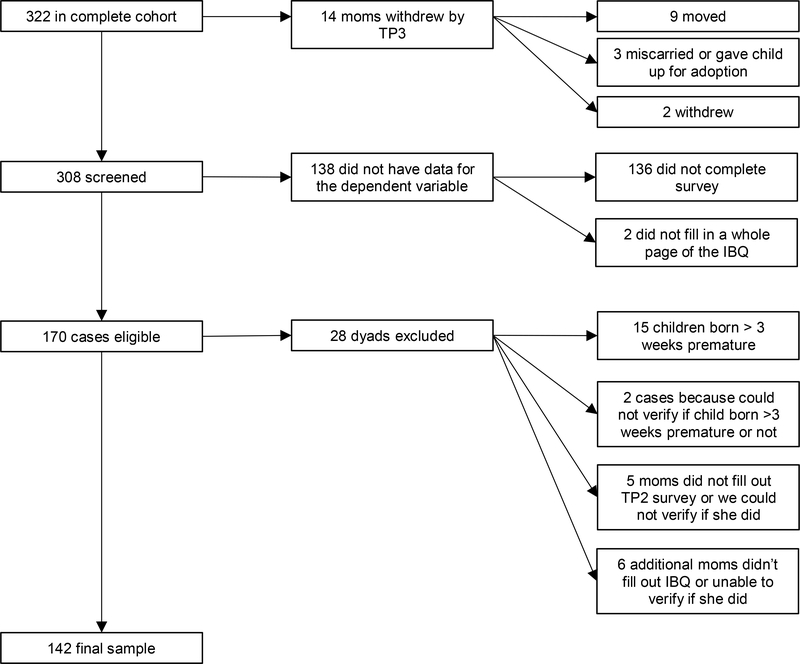
Participants were drawn from a longitudinal birth cohort designed to determine how access to and use of community resources affects early development for children born into poverty (Salsberry et al., 2016). These mother-infant dyads (n = 322) were recruited from Women Infant and Children (WIC) centers within a Midwestern metropolis using robust quota sampling, designed to represent the racial and ethnic composition of families living below the Federal Poverty Level in the locale. Mothers were asked to participate in the study if they: a) provided informed consent for themselves and their infant; b) were 18 years of age or older; c) resided within the targeted Midwestern county; d) spoke conversational English; and e) were pregnant or had a child no older than three months of age who was not born premature or diagnosed at birth with severe cognitive or physical disabilities. Regarding the last criterion, we sought to ascertain mothers at or near the time of the birth of a target child, although there was no restriction on whether the mother had additional, older children. For our purposes, data only represented the target children. A subset of 142 dyads from the larger sample is represented in this study, representing those dyads in which all key data from the dependent variable, infant self-regulation, were available. See Figure 1 for details on the subsample size and Table 1 for demographics on the full sample and the subsample. The sample was generally low-income or considered in a low socioeconomic bracket as over 80% of the sample lived with a household income of less than $30,000 USD each year and most mothers (55%) had never attended college. Additionally, the sample was relatively racially diverse as about ½ of the children in the sample were identified as being Black or having African American ancestry and the other ½ were identified as White/Caucasian.
Figure 1.
Arrival to the subsample size for the current study. IBQ = Infant Behavior Questionnaire-Revised Very Short Form; TP1 = Time Point 1; TP2 = Time Point 2; TP3 = Time Point 3.
Table 1.
Participant Demographics
| % |
||
|---|---|---|
| Full Sample | Subsample | |
| Annual household income | ||
| $10,000 or less | 50.3 | 45.8 |
| $10,001 to $30,000 | 35.8 | 35.9 |
| > $30,000 | 13.8 | 18.4 |
| Main language spoken at home | ||
| English | 92.5 | 91.5 |
| Spanish | 3.7 | 5.6 |
| Mother’s education | ||
| Eighth grade or less | 3.1 | 2.8 |
| Some high school, no diploma | 16.7 | 13.5 |
| High school diploma or GED | 39.9 | 39.0 |
| Some college, no degree | 29.9 | 31.2 |
| Associate’s degree | 3.1 | 4.3 |
| Bachelor’s degree | 6.3 | 7.8 |
| Master’s degree | 0.9 | 1.4 |
| Some college versus not | 40.8 | 44.7 |
| Mother married or living with partner at TP1 | 50.6 | 54.6 |
| Infant race | ||
| Unknown | 4.3 | 4.9 |
| Black/African American | 54.5 | 51.9 |
| Of Black/African American, % mixed race | 18.5 | 15.7 |
| Non Black/African American (“Other” race) | 45.5 | 48.1 |
| Of Other, % mixed race | 1.4 | 0 |
| Of Other, % White/Caucasian only | 90 | 93.9 |
| Of Other, % Asian only | 7.1 | 6.1 |
| Of Other, % American Indian/Alaskan Native only | 4.3 | 4.9 |
| Infant ethnicity Latino/Hispanic | 7.4 | 9.3 |
| Infant sex Female | 56.5 | 55.6 |
Note. TP1 = Time point one. Percentages are based on participants who responded to the respective survey question. For the full sample, the mothers’ mean age (SD) was 26.3 years (5.4) with a range of 18–46. For the subsample, the mothers’ mean age (SD) was 26.6 (4.8) and the range was 18–38. For reference, full sample n = 322 and subsample n = 142.
Procedure
The present study uses data from the first three time points, which occurred prior to or during the child’s first year of life. Time point one occurred from December 2014 to August 2015 when children were in-utero or up to 3 months of age. Time point two occurred from April 2015 to August 2016 when infants were 4- to 7-months-old. Time point three visit occurred from September 2015 to February 2017 when the infant was 9- to 12-months-old. During 2015 and 2016, the poverty level was approximately $24,000 for a family of four (U.S. Census Bureau, 2019). Time point one occurred at the WIC clinic and time points two and three were generally conducted at the infant’s home. Home visits were conducted by research staff who had completed training and demonstrated competence to collect measures and conduct observational assessments. Mothers were compensated for their time with a gift card and child care items. The study was conducted in accordance with the ethical standards of the American Psychological Association and had full approval by the Institutional Review Board of the authors’ university.
Measures
Infant self-regulation
We surveyed mothers on their infant’s self-regulation at time point three with the Infant Behavior Questionnaire-Revised Very Short Form (IBQ-R VSF, hereafter also named IBQ; Putnam, Helbig, Gartstein, Rothbart, & Leerkes, 2014). The IBQ reflects categories of infant temperament, or day-to-day behavior, according to context-specific infant behavior observed in the past week. The IBQ has 37 questions divided into three categories: surgency, negative affect, and effortful control. Self-regulation within the present study is represented by the 12 questions from the effortful control subscale (Putnam, Jacobs, Gartstein, & Rothbart, 2010). The effortful control subscale assesses cognitive and socio-emotional self-regulation, specifically duration of orienting, low intensity pleasure, cuddliness, and soothability. The questions are scored on a scale from 1 – 7, where 1 = Never and 7 = Always with higher scores indicating better infant effortful control/self-regulation. The IBQ-R VSF is strongly correlated with the full-scale IBQ-R (r range .71 to .86; Putnam et al., 2014), which is psychometrically appropriate for representing young children’s effortful control/self-regulation (Gartstein, Bridgett, & Low, 2012; Gartstein, Putnam, & Rothbart, 2012; Parade & Leerkes, 2008; Rothbart, 2011). The Cronbach’s alpha for the current study = .80.
Maternal depression symptomatology
Maternal depression symptomatology was measured using the Edinburgh Postnatal Depression Scale (EPDS; Cox, Holden, & Sagovsky, 1987) at time point two. The EPDS is the most commonly used screener of depression symptomatology specifically occurring during the postpartum period, that is within one year after birth (American College of Obstetricians and Gynecologists, 2018; Gibson et al., 2009). Mothers respond to 10 items surveying depressive mood symptoms in the past week. Items include “I have blamed myself unnecessarily when things went wrong” and “I have felt sad or miserable.” The questions are scored on a 0- to 3-point scale; higher scores indicate more depressive symptomatology. The Cronbach’s alpha for the current sample is .85. We dichotomized the predictor maternal depression into symptomatology of minor depressive disorder versus not, based on research with a similar high-risk sample (Chaudron et al., 2010). The EPDS score for symptomatology of minor depressive disorder is 7 or greater (sensitivity 81%, specificity 77%; assigned value = 1 in this study and lower scores assigned value = 0).
Maternal parenting self-efficacy
Maternal parenting self-efficacy was measured at time point two with a validated 10-question survey for mothers of infants (Teti & Gelfand, 1991). The survey questions were designed to capture mothers’ sense of self-efficacy while parenting an infant. Sample items included: “When your baby is upset, fussy, or crying, how good are you at soothing him or her?” and “In general, how good a parent do you feel you are with your baby?” Each question is answered on scale from 0 = not good at all to 3 = very good. The total score range is 0–30, with higher scores indicating higher maternal self-efficacy. The scale has shown strong correlation with reverse-scored items from the Parenting Stress Index Sense of Competence Scale (r = −.75, p < .001; Teti & Gelfand, 1991). In the current sample, the Cronbach’s alpha = .82.
Covariates
Covariates in this investigation included infant race (Black vs. not), maternal education (no college education vs. at least some college education), infant sex, infant age at time point three (when self-regulation was measured), infant negative affect, and infant cognition. Infant race was explored as a covariate due to reports that mothers may vary in their reports of infant self-regulation by infant race (Palmer et al., 2013). Maternal education was used to characterize socioeconomic status for the low-income mother-infant dyads given its association with resources and training to be able to provide enriching experiences for their child (Davis-Kean, 2005; Zimmerman & Woolf, 2015). Infant sex was used as a covariate due to reports that both maternal depression (de Tychey et al., 2008; Myers & Johns, 2019) and early child self-regulation may vary by child sex (Hosseini-Kamkar & Morton, 2014). Infant age at time point three, measured at the time of the primary outcome variable of infant self-regulation, was used as a covariate due to differences in self-regulation abilities by age.
Infant negative affect (high distress and fear) was assessed due to differences in self-regulation in United States infants by infant negative affect (Paulussen-Hoogeboom et al., 2007) and potential confounding by depressed mothers (Granat et al., 2017). Infant negative affect was assessed at time point three with a 12-question maternal-report subscale from the IBQ-R VSF (higher scores = higher infant negative affect).
Given our primary measure of infant self-regulation is based on maternal report, we controlled for observable, cognitive aspects of infant self-regulation such as attention and working memory with raw scores from the cognitive scale of the Bayley Scale of Infant and Toddler Development, 3rd edition (Bayley-III) at TP3 (Bayley, 2006). The Bayley-III is a gold-standard observational measure of infant development and functioning. We used raw scores rather than standard scores given that age at time of assessment was controlled for (at time point three) and because lack of standardization information is available for high-risk infants living in poverty or low-income homes.
Data Analysis
Data were analyzed with SPSS (version 24) and the PROCESS macro for SPSS (version 2.16) by Hayes (2016). To characterize relations for Aim 1, we examined summary statistics and performed correlations. To examine the potential mediation for Aim 2, we employed PROCESS. We specifically used PROCESS to test whether and the extent to which maternal parenting self-efficacy was the mediator between maternal depression symptomatology and infant self-regulation, controlling for infant race, negative affect, age at time point three, cognition, sex, and maternal education. PROCESS estimates the coefficients in a mediation model using a bootstrapping method in estimating confidence intervals (Hayes, 2016, 2013). This study employs 10,000 bootstrap samples to calculate bias-corrected 95% confidence intervals. Effect sizes (d) for the mediation analysis were calculated by dividing the Beta coefficient by the SD of that variable.
To better understand the patterns of missingness, we also examined differences in the demographics between the full sample and subsample and missing data in the subsample with Chi-Square tests for all categorical variables and an independent sample t-test on a difference between the mean age of the mothers in the samples. Across all of these analyses we found no significant differences between the cases where data was missing and the sample. Specifically, of the present study’s 142 participants, 13 had data missing on one or more variables. To further understand the missingness, we used the SPSS Missing Value Analysis Expectation-Maximization (EM) function with all study variables (and one additional variable unrelated to the examination of present study). From this analysis, we examined Little’s MCAR test, which was not significant, and therefore these cases were considered missing at random. Missing data were imputed with SPSS 24 (five imputations). We ran the mediation analysis twice, once with the imputed data and once using list-wise deletion for completeness and to strengthen interpretation of the findings (Tabachnick & Fidell, 2007).
Results
Aim 1: Characterize Relationships among Maternal Depression Symptoms, Maternal Parenting Self-efficacy, and Infant Self-Regulation for High-Risk Dyads
The first aim was to characterize relations among maternal depression symptomatology, maternal parenting self-efficacy, and infant self-regulation in the low-income sample. Summary statistics appear in Table 2. Of note in this low-income sample, 40% of mothers had minor depression symptomatology. However, most mothers reported relatively high levels of parenting self-efficacy (M = 26.53, SD = 3.25; possible range 0–30) and moderately high perceptions of their infant’s self-regulation (M = 5.26; SD = 0.84; possible range 1–7).
Table 2.
Sample Statistics
| Variable (range, if applicable) | TP | n | Mean | SD | Sample Range |
|---|---|---|---|---|---|
| Maternal EPDS symptomatology 2G (score ≥ 7 = 1) | 2 | 138 | 0.39 | 0.49 | 0 – 1 |
| Maternal self-efficacy (0 – 30) | 2 | 139 | 26.53 | 3.25 | 18 – 30 |
| Maternal education 2G (some college = 1) | 1 | 141 | 0.44 | 0.50 | 0 – 1 |
| IBQ infant self-regulation (1 – 7) | 3 | 142 | 5.26 | 0.84 | 2.08 – 6.92 |
| IBQ infant negative affect (1 – 7) | 3 | 142 | 4.23 | 1.08 | 1.45 – 6.67 |
| Bayley-III infant cognition raw score | 3 | 137 | 37.13 | 4.37 | 27 – 47 |
| Infant age in months | 3 | 142 | 11.18 | 0.91 | 8.7 – 12.8 |
| Infant race 2G (Black or African American = 1) | 1 | 142 | 0.51 | 0.50 | 0 – 1 |
| Infant sex (female = 1) | 1–3 | 142 | 0.56 | 0.50 | 0 – 1 |
Note. Results from non-imputed data and values rounded to the nearest hundredth when applicable. For the variable scores that were transformed into dummy variables, or two groups (2G), the group given value = 1 is listed in parentheses next to the variable name. The other continuous variables have the possible range in parentheses after the variable name, when applicable. For infant race non-Black or African American, 93.9% mothers reported only White or Caucasian race and 6.1% mothers reported only Asian race. Other acronyms used in the table include TP = Time Point; SD = standard deviation; IBQ = Infant Behavior Questionnaire-Revised Very Short Form.
Pearson correlations between all study variables with pooled imputed data are in Table 3. Infant self-regulation was negatively correlated with maternal depression symptomatology (r = −.18, p < .05) but positively correlated with maternal self-efficacy (r = .34, p < .01). Maternal self-efficacy and maternal depression symptomatology were negatively correlated (r = −.30 , P < maternal depression symptomatology, maternal self-efficacy) were not associated with the covariates (maternal education, infant race, infant cognition, infant negative affect) except between infant sex and maternal depression, such that mothers of male infants had higher depression symptomatology than mothers of female infants (r = −0.22, P < .01),
Table 3.
Pearson Correlations among Key Measures
| Measure | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| 1. Infant Self-Regulation | - | ||||||||
| 2. Infant Negative Affect | .13 | - | |||||||
| 3. Infant Cognition | −.12 | −.05 | - | ||||||
| 4. Infant Sex | .08 | −.08 | .10 | - | |||||
| 5. Infant Age at TP3 | −.11 | −.17* | .25** | −.07 | - | ||||
| 6. Infant Race Black | .09 | .16 | −.02 | .01 | −.11 | - | |||
| 7. Maternal Depression | −.18* | .08 | −.08 | −.22** | .07 | −.05 | - | ||
| 8. Maternal Self-Efficacy | .34** | .01 | −.01 | .05 | −.06 | .11 | −.30** | - | |
| 9. Maternal Education | .03 | .13 | −.01 | .08 | −.11 | .12 | −.05 | .10 | - |
Note. Values determined with pooled multiple imputation data and values rounded to the nearest hundredth.
p < .05
p < .01
We next explored this relationship post hoc with logistic regression predicting maternal depression symptomatology with all of the original study variables (maternal self-efficacy, infant self-regulation, maternal education, infant self-regulation, infant cognition, infant age, infant sex, infant race). The model showed that mothers of male infants had 2.3 times the odds of having maternal depression symptomatology compared to mothers of females (exp(β) = 2.32, p = .03). For the variables of focus, mothers with one point higher self-efficacy had 17% lower odds of experiencing maternal depression symptomatology (exp(β) = 0.84, p = .005).
Aim 2: Whether and the Extent to Which Maternal Parenting Self-efficacy is the Mediating Pathway through which Maternal Depression Symptomatology Predicts Infant Self-Regulation
The second aim was to examine whether and to what extent maternal parenting self-efficacy mediates the relation between maternal depression symptomatology and infant self-regulation. We tested this aim using the PROCESS macro. Again, the mediation inference in the PROCESS macro uses bootstrapping to determine the indirect effect of the independent variable (maternal depressive symptomatology) on the dependent variable (infant self-regulation). This is the modern and preferred method to test and estimate indirect effects (Hayes & Rockwood, 2017) rather than the classic “causal steps approach” outlined by Baron and Kenny (1986), which was used in the Teti and Gelfand (1991) study. Because PROCESS is unable to handle multiple imputation at this time, we examined both the original data and the imputed data for completeness and to strengthen interpretation of the findings (Tabachnick & Fidell, 2007).
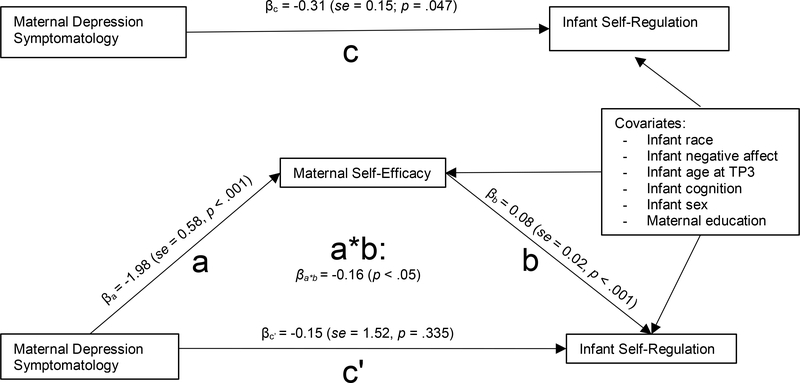
The mediation analysis showed that maternal depression symptomatology indirectly influenced infant self-regulation through its effect on maternal self-efficacy. As shown in Figure 2, the total effects model showed that mothers without minor depression disorder symptomatology had an infant with 0.31 points better self-regulation, on average, controlling for covariates listed (maternal self-efficacy not included in this model). For the mediation of maternal self-efficacy, dyads with no maternal depression symptomatology endorsed higher levels of maternal self-efficacy (βa = −1.98; se= 0.58; t = −3.40; p < .001; 95% CI −3.129, −0.837; n = 142; d = 0.29), which in turn led to slightly better infant self-regulation (βb = 0.08; se = 0.02; t = 3.69; p < .001; 95% CI 0.04, 0.12; n = 142; d = 0.34). The complete indirect effect, βa*b = −0.16, was obtained by multiplying βa and βb from the pooled data and was determined to be statistically significant based on the PROCESS calculation of a bias-corrected bootstrap confidence interval of 10,000 samples for each of the five multiple imputation datasets (βa*b = −0.17 to −0.15, se = 0.06 to 0.07, 95% CI range −0.28 to −0.06) and with the original dataset (n = 130 dyads, βa*b = −0.15; Boot se = 0.07; Boot 95% CI −0.31, −0.04; d = 0.19). This means that on average, mothers with little to no depression symptomatology have infants with 0.16 points better self-regulation from the effect of depression on maternal self-efficacy. No evidence suggested that maternal depression symptomatology influenced infant self-regulation independent of its effect on maternal self-efficacy or among mothers equal in self-efficacy (βc’ = −0.15; se = 1.52, t = −0.93, p = .335, 95% CI −0.446, 0.152). In sum, lower levels of maternal depression symptomatology predicted higher levels of maternal self-efficacy, which then predicted higher levels of infant self-regulation.
Figure 2.
Mediation model demonstrating results of statistical analysis used to test aim 1. “C” is the total effects model, where C is the total effect of X (maternal depression symptomatology) on Y (infant self-regulation). For the mediation model, a*b is the indirect effect of X on Y and c’ is the direct effect of X on Y. The indirect effect (a*b) was obtained by multiplying path a and path b together – demonstrated to be statistically significant based on PROCESS analyses.
Discussion
Numerous lines of research have shown that early self-regulation provides a foundation for wellness later in life including academic, health, and financial well-being. Yet, infants reared in low-income households show poorer self-regulation skills than that of their more socioeconomically advantaged peers. Maternal factors such as maternal depression and parenting self-efficacy may shape infant self-regulation in disadvantaged homes, yet the mechanisms for how this occurs is less clear. Factors within low-income environments, including maternal depression and self-efficacy, may help elucidate the mechanisms for how infant self-regulation develops. Drawing upon cognitive behavior theory (Beck, 1979) and modern mediation methods, the aims of this study were to better characterize the relations among maternal depression symptomatology, maternal self-efficacy, and infant self-regulation for mother- infant dyads living in low-income homes. Additionally, this study was the first to investigate if infant self-regulation was indirectly shaped by maternal depression through maternal self-efficacy in a sample of mother-infant dyads living in low-income homes in the U.S. The major finding of this study was that elevated maternal depression symptomatology predicted poorer infant self-regulation through its effect on poorer maternal self-efficacy. This finding adds to the literature in two major ways: adding knowledge to disentangling processes of early self-regulation development and highlighting novel areas for intervention.
The findings from this study help clarify how processes in the high-risk infant’s caregiving environment, such as maternal depression and parenting mindset, lead to impaired self-regulation even at infancy. Although cognitive behavior theories typically focus on a person’s (i.e., mother) thoughts, feelings and behavior, we find evidence that it also matters for the mothers and infants as a unit. This may be due to the critical importance of mother’s mental health for infant self-regulation development (Goodman & Gotlib, 1999), and that this relationship is shaped in part by maternal feelings, or mindset, of parenting competence (Coleman & Karraker, 2003).
When characterizing the interrelations among maternal depression symptomatology, maternal self-efficacy, and infant self-regulation, we found a high prevalence of depression during the postpartum period in this low-income sample. About 40% of mothers reported minor depression symptomatology during the postpartum period; this is a much higher rate of depression symptomatology compared to the general population norms of about 20% as reported in Gaynes et al. (2005). However, the prevalence we found among the sample is comparable to the 50% in impoverished mothers found by Chung et al. in 2004. Additionally, the present low-income sample had slightly lower self-efficacy scores as compared to the Teti and Gelfand (1991) sample. In this sample, the mean of parenting self-efficacy was 26.53 (SD = 3.25), whereas in the Teti and Gelfand (1991) sample, non-depressed mothers reported a self-efficacy score of 29.63 and 33.05 in depressed mothers. Yet, the mean infant self-regulation score in this sample was comparable to many diverse samples reported by Putnam et al. (2013). These findings suggest that despite decades of research and interventions, mothers living in low-income homes may still be facing high rates of depression and feelings of poor parenting competency. Addressing poverty may actually be necessary to improve all of the constructs we have investigated including maternal depression, parenting self-efficacy, and ultimately infant’s self-regulation. Such investigations are underway, for example, in programs supporting universal basic income in Alaska (Ruckert, Huynh, & Labonté, 2018) and with other high-risk groups (Shaefer et al., 2018). In the words of Bowlby, “If a community values its children it must cherish their parents” (Bowlby, 1951, p. 84).
However, the mediation finding suggests that a novel intervention area to improve infant self-regulation for high-risk dyads with depressive symptomatology may be through self-efficacy. This is because, despite the smaller effect size for the whole mediation model, there was a large association between maternal depressive feelings and maternal self-efficacy. The results suggest that because of the strong relationship between mother’s depressive symptoms and her appraisal of her parenting ability, perhaps focusing on improving maternal self-efficacy may help decrease the indirect effect that maternal depression may have on infant self-regulation. This is particularly important given that high-risk dyads are at increased risk for depression and postpartum depression (Chung et al., 2004; Gaynes et al., 2005) and under treatment (Kozhimannil, Trinacty, Busch, Huskamp, & Adams, 2011). While health care practitioners and policymakers work to improve treatment for maternal depression in high-risk dyads, researchers could investigate if improving the mother’s parenting self-efficacy may help improve infant self-regulation for these high-risk dyads. This could occur in a number of ways: through existing interventions to help mothers feel that they are capable of parenting or to improve mothers’ knowledge to help improve their maternal self-efficacy. One example of an intervention to deliver these messages could be through local parenting support groups – the social support may also be helpful in improving depressive symptoms as well (Schwab-Reese, Schafer, & Ashida, 2017). Another example of an intervention could be the Nurse-Family Partnership home visiting program to support high-risk mother infant dyads adjust to the parenting role. Randomized control trials of the Nurse Family Partnership show that home visits from pregnancy to 2 years of age is associated with better self-regulation skills and less behavior problems at 4, 6, and 9 years of age (Olds et al., 2014). Another novel area of intervention may be to focus efforts to improve maternal self-efficacy at the same time as treating maternal depression or postpartum depression. These interventions are particularly important to explore to see if they improve self-regulation and even later life-course outcomes, given self-regulation skills are key to success later in life (Moffitt et al., 2011).
One final finding of note was that maternal depression varied by infant sex in this sample. We found that mothers of male infants had about 2.3 times the odds of having minor depression disorder during the postpartum period compared to mothers of females, which corresponds with other emerging research from the United Kingdom (Myers & Johns, 2019) and France (de Tychey et al., 2007). Myers and Johns (2019) hypothesized that the reason for the finding was related to potential inflammation associated with growing a male fetus in a female body as compared to growing a female fetus in a female body. This relationship should be explored in the future and considered when understanding risks of maternal depression in high-risk mother-infant dyads.
Limitations and Conclusions
Although our findings suggest that maternal depression may undermine mother’s feelings that she can competently parent, which in turn may negatively affect infant’s self-regulation at a later time period, our reliance on maternal report for these factors is a limitation of this study. That is, with mothers reporting their own depression, parenting self-efficacy, and infant self-regulation, it is possible that mothers who are more depressed perceive poorer infant self-regulation. However, a classic review on comparing child behavior between depressed mothers and other informants found that 94% of studies failed to show that depression distorted mother’s assessment of child behavior (Richters, 1992). Nevertheless, maternal report of infant self-regulation may actually be a unique window into the infant’s microenvironment (Mangelsdorf et al., 2000). For example, a depressed mother may exhibit maladaptive parenting behaviors towards her infant and consequently elicit more distressful reactions from an infant (Goodman & Gotlib, 1999) versus a caregiver without depression, causing the depressed mother to observe that her infant shows signs of poorer self-regulation while the non-depressed caregiver observes better self-regulatory behaviors. In addition, several maternal reports of infant behavior have revealed that maternal self-report assesses both subjective and objective components of the mother’s perception of her infant (Bates & Bayles, 1984; Mebert, 1991). This may be because mothers, versus other assessors or observers, typically have much familiarity with their child’s behavior over time, over a variety of contexts (Mangelsdorf et al., 2000), and in situation-specific interactions between mother and infant versus other caretakers (Achenbach et al., 1987). In addition to objective reports of infant behavior, maternal perception of infant behavior is also linked to later child outcomes (Molfese et al., 2010). Thus, maternal report of infant behavior is important to consider when assessing infant self-regulation in the context of the caregiving environment. Building upon this previous research, this work adds convincing evidence that maternal thoughts and feelings may play important roles in shaping infant’s self-regulation.
In conclusion, this study examined the effect of the interplay of maternal depression and parenting self-efficacy on infant self-regulation in a sample of racial diversity and living in low-income homes in the United States – an understudied population. This study importantly illustrates the significant role maternal self-efficacy has in mediating the relationship between maternal depression symptomatology and infant self-regulation in high-risk dyads during a critical period of self-regulation development: the first year of life. Although much remains to be studied in regards to early infant self-regulation, particularly for racially diverse dyads living in poverty, we hope that scholars can use this current study to extend the science of infant self-regulation in socioeconomically disadvantaged and racially diverse mother-infant dyads or to use as an impetus for improving conceptual understanding of infant self-regulation for diverse samples. We also hope that this study could be an additional springboard for researchers to focus on strategies to optimize the caregiving environment even earlier than anticipated to optimize life course self-regulation for children of high-risk dyads and give families the best future possible.
Data Availability Statement
For this longitudinal study, data cleaning is still underway for later time points. However, data and code for the first three time points used in this study are clean can be made available by emailing the corresponding author.
Highlights.
We investigated infant self-regulation in low-income homes in the US
Maternal self-efficacy mediated depression and infant self-regulation relation
Lower maternal depression predicted better self-efficacy and better self-regulation
Acknowledgments
Funding: This work was supported by the Crane Center for Early Childhood Research and Policy of The Ohio State University (study design, data analysis, data interpretation, writing of report) and in part by the National Institute of Nursing Research of the National Institutes of Health (F31NR017103 and T32NR014225), and the Jonas Foundation. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Crane Center for Early Childhood Research and Policy, National Institutes of Health, or the Jonas Foundation.
Footnotes
Conflicts of interest: There are no actual or perceived conflicts of interest in the conduct or reporting of this research.
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
References
- Achenbach TM, McConaughy SH, & Howell CT (1987). Child/adolescent behavioral and emotional problems: Implications of cross-informant correlations for situational specificity. Psychological Bulletin, 101, 213–222. doi: 10.1037/0033-2909.10L2.213 [DOI] [PubMed] [Google Scholar]
- American College of Obstetricians and Gynecologists. (2018). Committee opinion no. 757: Screening for perinatal depression. Obstetrics & Gynecology, 132(5), e208–e212. doi: 10.1097/A0G.0000000000002927 [DOI] [PubMed] [Google Scholar]
- Atkins R (2010). Self-efficacy and the promotion of health for depressed single mothers. Mental Health in Family Medicine, 7, 155–168. [PMC free article] [PubMed] [Google Scholar]
- Baron RM, & Kenny DA (1986). The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51, 1173–1182. doi: 10.1037/0022-3514.51.61173 [DOI] [PubMed] [Google Scholar]
- Bates JE, & Bayles K (1984). Objective and subjective components in mothers’ perceptions of their children from age 6 months to 3 years. Merrill-Palmer Quarterly, 30, 111–130. [Google Scholar]
- Bayley N (2006). Bayley Scales of Infant Development-III. San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Beck AT (1979). Cognitive therapy of depression. New York: Guilford Press. [Google Scholar]
- Berger A (2011). Self-regulation: Brain, cognition, and development. Washington, DC: American Psychological Association. [Google Scholar]
- Blair C, & Diamond A (2008). Biological processes in prevention and intervention: The promotion of self-regulation as a means of preventing school failure. Development and Psychopathology, 20(3), 899–911. doi: 10.1017/S0954579408000436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowlby J (1951). Maternal care and mental health. World Health Organization Monograph Series, 2, 179 Retrieved from https://apps.who.int/iris/handle/10665/40724 [PMC free article] [PubMed] [Google Scholar]
- Carter AS, Garrity-Rokous FE, Chazan-Cohen R, Little C, & Briggs-Gowan MJ (2001). Maternal depression and comorbidity: Predicting early parenting, attachment security, and toddler social-emotional problems and competencies. Journal of the American Academy of Child & Adolescent Psychiatry, 40, 18–26. doi: 10.1097/00004583-200101000-00012 [DOI] [PubMed] [Google Scholar]
- Chaudron LH, Szilagyi PG, Tang W, Anson E, Talbot NL, Wadkins HIM, … Wisner KL (2010). Accuracy of depression screening tools for identifying postpartum depression among urban mothers. Pediatrics, 125, e609–e617. doi: 10.1542/peds.2008-3261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung EK, McCollum KF, Elo IT, Lee HJ, & Culhane JF (2004). Maternal depressive symptoms and infant health practices among low-income women. Pediatrics, 113, e523–529. doi: 10.1542/peds.113.6.e523 [DOI] [PubMed] [Google Scholar]
- Coleman PK, & Karraker KH (2003). Maternal self-efficacy beliefs, competence in parenting, and toddlers’ behavior and developmental status. Infant Mental Health Journal, 24, 126–148. doi: 10.1002/imhj.10048 [DOI] [Google Scholar]
- Cox JL, Holden JM, & Sagovsky R (1987). Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. British Journal of Psychiatry, 150, 782–786. doi: 10.1192/bjp.150.6.782 [DOI] [PubMed] [Google Scholar]
- Davis-Kean PE (2005). The influence of parent education and family income on child achievement: The indirect role of parental expectations and the home environment. Journal of Family Psychology, 19(2), 294–304. doi: 10.1037/0893-3200.19.2.294 [DOI] [PubMed] [Google Scholar]
- de Tychey C, Briancon S, Lighezzolo J, Spitz E, Kabuth B, de Luigi V, … Vincent S (2008). Quality of life, postnatal depression and baby gender. Journal of Clinical Nursing, 17, 312–322. doi: 10.1111/j.1365-2702.2006.01911.x [DOI] [PubMed] [Google Scholar]
- Gartstein M, Bridgett DJ, & Low CM (2012). Asking questions about temperament: Self- and other-report measures across the lifespan. New York, NY: Guilford. [Google Scholar]
- Gartstein MA, Putnam SP, & Rothbart MK (2012). Etiology of preschool behavior problems: Contributions of temperament attributes in early childhood. Infant Mental Health Journal, 33, 197–211. doi: 10.1002/imhj.21312 [DOI] [PubMed] [Google Scholar]
- Gaynes BN, Gavin N, Meltzer-Brody S, Lohr KN, Swinson T, Gartlehner G, … Miller WC (2005). Perinatal depression: Prevalence, screening accuracy, and screening outcomes (Evidence Report/Technology Assessment No. 119. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK37740/ [DOI] [PMC free article] [PubMed]
- Gibson J, McKenzie-McHarg K, Shakespeare J, Price J, & Gray R (2009). A systematic review of studies validating the Edinburgh Postnatal Depression Scale in antepartum and postpartum women. Acta Psychiatrica Scandinavica, 119, 350–364. doi: https://doi.org/10.nn/j.1600-0447.2009.01363.x [DOI] [PubMed] [Google Scholar]
- Goodman SH, & Gotlib IH (1999). Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review, 106, 458–490. doi: 10.1037/0033-295X.1063.458 [DOI] [PubMed] [Google Scholar]
- Granat A, Gadassi R, Gilboa-Schechtman E, & Feldman R (2017). Maternal depression and anxiety, social synchrony, and infant regulation of negative and positive emotions. Emotion, 17, 11–27. doi: 10.1037/emo0000204 [DOI] [PubMed] [Google Scholar]
- Hayes AF (2013). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York, New York: Guilford Press. [Google Scholar]
- Hayes AF (2016). The PROCESS macro for SPSS and SAS [SPSS macro download and description]. Retrieved from http://www.processmacro.org/index.html
- Hayes AF, & Rockwood NJ (2017). Regression-based statistical mediation and moderation analysis in clinical research: Observations, recommendations, and implementation. Behaviour Research and Therapy, 98, 39–57. doi: 10.1016/j.brat.2016.11.001 [DOI] [PubMed] [Google Scholar]
- Hancock KJ, Mitrou F, Shipley M, Lawrence D, & Zubrick SR (2013). A three generation study of the mental health relationships between grandparents, parents and children. BMC Psychiatry, 13, 299. doi: 10.1186/1471-244X-13-299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosseini-Kamkar N, & Morton JB (2014). Sex differences in self-regulation: An evolutionary perspective. Fronteirs in Neuroscience, 8. doi: 10.3389/fnins.2014.00233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochanska G, Murray KT, & Harlan ET (2000). Effortful control in early childhood: Continuity and change, antecedents, and implications for social development. Developmental Psychology, 36(2), 220–232. doi: 10.1037/0012-1649.36.2.220 [DOI] [PubMed] [Google Scholar]
- Kochanska G, Tjebkes TL, & Forman DR (1998). Children’s emerging regulation of conduct: Restraint, compliance, and internalization from infancy to the second year. Child Development, 69, 1378–1389. doi: 10.1111/j.1467-8624.1998.tb06218.x [DOI] [PubMed] [Google Scholar]
- Kozhimannil KB, Trinacty CM, Busch AB, Huskamp HA, & Adams AS (2011). Racial and ethnic disparities in postpartum depression care among low-income women. Psychiatric Services, 62, 619–625. doi: 10.1176/ps.62.6.pss6206_0619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leerkes EM, & Crockenberg SC (2002). The development of maternal self-efficacy and its impact on maternal behavior. Infancy, 3, 227–247. doi: 10.1207/S15327078IN0302_7 [DOI] [PubMed] [Google Scholar]
- Mangelsdorf SC, Schoppe SJ, & Buur H (2000). The meaning of parental reports: A contextual approach to the study of temperament and behavior problems in childhood In Molfese D & Molfese VJ (Eds.), Temperament and personality development across the lifespan (pp. 121–140). Hillsdale, NJ: Erlbaum. [Google Scholar]
- McClelland MM, Geldhof GJ, Cameron CE, & Wanless SB (2015). Development and self-regulation In Lerner RM (Ed.), Handbook of child psychology and developmental science (pp. 1–43). Hoboken, NJ: John Wiley & Sons, Inc. [Google Scholar]
- McCoy DC, & Raver CC (2014). Household instability and self-regulation among poor children. Journal of Children and Poverty, 20, 131–152. doi: 10.1080/10796126.2014.976185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mebert CJ (1991). Dimensions of subjectivity in parents’ ratings of infant temperament. Child Development, 62, 352–361. doi: 10.1111/j.1467-8624.1991.tb01536.x [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Arseneault L, Belsky D, Dickson N, Hancox RJ, Harrington H, … Caspi A (2011). A gradient of childhood self-control predicts health, wealth, and public safety. Proceedings of the National Academy of Sciences of the United States of America, 108, 2693–2698. doi: 10.1073/pnas.1010076108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molfese VJ, Rudasill KM, Beswick JL, Jacobi-Vessels JL, Ferguson MC, & White JM (2010). Infant temperament, maternal personality, and parenting stress as contributors to infant developmental outcomes. Merrill-Palmer Quarterly, 56, 49–79. doi: 10.1353/mpq.0.0039 [DOI] [Google Scholar]
- Myers S, & Johns SE (2019). Male infants and birth complications are associated with increased incidence of postnatal deprssion. Social Science & Medicine, 220, 56–64. doi: 10.1016/j.socscimed.2018.10.008 [DOI] [PubMed] [Google Scholar]
- Olds DL, Holmberg JR, Donelan-McCall N, Luckey DW, Knudtson MD, & Robinson J (2014). Effects of home visits by paraprofessionals and by nurses on children: Follow-up of a randomized trial at ages 6 and 9 years. JAMA Pediatrics, 168, 114–121. doi: 10.1001/jamapediatrics.2013.3817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Organ C (n.d.). Maybe I’m Not Totally F*cking This Mom Thing Up. Scary Mommy. Retrieved from https://www.scarymommy.com/not-perfect-mom/ [Google Scholar]
- Palmer FB, Anand KJS, Graff JC, Murphy LE, Qu Y, Volgyi E, … Tylavsky FA (2013). Early adversity, socioemotional development, and stress in urban 1-year-old children. The Journal of Pediatrics, 163(6), 1733–1739. doi: 10.1016/j.jpeds.2013.08.030 [DOI] [PubMed] [Google Scholar]
- Parade SH, & Leerkes EM (2008). The reliability and validity of the Infant Behavior Questionnaire-Revised. Infant Behavior and Development, 31, 637–646. doi: 10.1016/j.infbeh.2008.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulussen-Hoogeboom MC, Stams GJ, Hermanns JM, & Peetsma TT (2007). Child negative emotionality and parenting from infancy to preschool: A meta-analytic review. Developmental Psychology, 43, 438–453. doi: 10.1037/0012-1649.43.2.438 [DOI] [PubMed] [Google Scholar]
- Putnam SP, Helbig AL, Gartstein MA, Rothbart MK, & Leerkes E (2014). Development and assessment of short and very short forms of the infant behavior questionnaire-revised. Journal of Personality Assessment, 96, 445–458. doi: 10.1080/00223891.2013.841171 [DOI] [PubMed] [Google Scholar]
- Putnam SP, Jacobs JF, Gartstein MA, & Rothbart MK (2010). Development and assessment of short and very short forms of the Early Childhood Behavior Questionnaire. Poster session presented at International Conference on Infant Studies, Baltimore, MD. [Google Scholar]
- Radesky JS, Silverstein M, Zuckerman B, & Christakis DA (2014). Infant self-regulation and early childhood media exposure. Pediatrics, 133, e1172–e1178. doi: 10.1542/peds.2013-2367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richters JE (1992). Depressed mothers as informants about their children: A review of evidence for distortion. Psychological Bulletin, 112, 485–499. doi: 10.1037/0033-2909.112.3.485 [DOI] [PubMed] [Google Scholar]
- Rothbart MK (2011). Becoming who we are: Temperament and personality in development. New York: Guilford Press. [Google Scholar]
- Rothbart MK, & Rueda MR (2005). The development of effortful control In Mayr U, Awh E, & Keele SW (Eds.), Developing individuality in the human brain: A tribute to Michael I. Posner (pp. 167–188). Washington, DC: American Psychological Association. [Google Scholar]
- Rothbart MK, Sheese BE, Rueda MR, & Posner MI (2011). Developing mechanisms of self-regulation in early life. Emotion Review, 3, 207–213. doi: 10.1177/1754073910387943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruckert A, Huynh C, & Labonte R (2018). Reducing health inequities: Is universal basic income the way forward? Journal of Public Health, 40(1), 3–7. doi: 10.1093/PUBMED/FDX006 [DOI] [PubMed] [Google Scholar]
- Salsberry P, Gugiu M, Dynia J, Justice L, Logan J, Purtell K, & Snyder-Hill S (2016). The Kids in Columbus Study. Retrieved from https://earlychildhood.ehe.osu.edu/files/2016/09/The-Kids-in-Columbus-Study-KICS.pdf. [Google Scholar]
- Schwab-Reese LM, Schafer EJ, & Ashida S (2017) Associations of social support and stress with postpartum maternal mental health symptoms: Main effects, moderation, and mediation. Women & Health, 57, 723–740. doi: 10.1080/03630242.2016.1181140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sevigny PR, & Loutzenhiser L (2010). Predictors of parenting self-efficacy in mothers and fathers of toddlers. Child: Care, Health and Development, 36, 179–189. doi: 10.1111/j.1365-2214.2009.00980.x [DOI] [PubMed] [Google Scholar]
- Shaefer HL, Collyer S, Duncan G, Edin K, Garfinkel I, Harris D, … Yoshikawa H (2018). A universal child allowance: A plan to reduce poverty and income instability among children in the United States. The Russel Sage Foundation Journal of the Social Sciences, 4(2), 22–42. doi: 10.7758/RSF.2018.4.2.02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shonkoff JP (2012). Leveraging the biology of adversity to address the roots of disparities in health and development. Proceedings of the National Academy of Sciences of the United States of America, 109 (Suppl. 2), 17302–17307. doi: 10.1073/pnas.1121259109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnick BG, & Fidell LS (2007). Using multivariate statistics. Boston: Pearson/Allyn & Bacon. [Google Scholar]
- Teti DM, & Gelfand DM (1991). Behavioral competence among mothers of infants in the first year: The mediational role of maternal self-efficacy. Child Development, 62, 918–929. doi: 10.1111/j.1467-8624.1991.tb01580.x [DOI] [PubMed] [Google Scholar]
- Tucker S, Gross D, Fogg L, Delaney K, & Lapporte R (1998). The long-term efficacy of a behavioral parent training intervention for families with 2-year-olds. Research in Nursing and Health, 21, 199–210. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. (2019). Poverty thresholds. Retrieved at https://www.census.gov/data/tables/time-series/demo/income-poverty/historical-poverty-thresholds.html
- Vance AJ, & Brandon DH (2017). Delineating among parenting confidence, parenting self-efficacy and competence. Advances in Nursing Science, 40(4), E18–E37. doi: 10.1097/ANS.0000000000000179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wittkowski A, Garrett C, Calam R, & Weisberg D (2017). Self-report measures of parental self-efficacy: A systematic review of the current literature. Journal of Child and Family Studies, 26, 2960–2978. doi: 10.1007/s10826-017-0830-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman EB, Woolf SH, & Haley A (2015). Understanding the relationship between education and health: A review of the evidence and an examination of community perspectives. Washington, DC: Agency for Healthcare Research and Quality; Retrieved from: https://archive.ahrq.gov/professionals/education/curriculum-tools/population-health/zimmerman.html [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
For this longitudinal study, data cleaning is still underway for later time points. However, data and code for the first three time points used in this study are clean can be made available by emailing the corresponding author.