Abstract
Atherosclerosis is the main cause of cardiovascular disease. Systemic inflammation is one important characteristic in atherosclerosis. Pro-inflammatory macrophages can secrete inflammatory factors and promote the inflammation of atherosclerosis. It has a great value for the treatment of atherosclerosis by inhibiting the release of inflammatory factors in macrophages. However, the detailed mechanism of this process is still unclear. In this study, we constructed an APOE-/- mice model of atherosclerosis to research the molecular mechanism of atherosclerosis. Protein tyrosine phosphatase non-receptor type 2 (PTPN2), an anti-inflammatory gene, was dramatically decreased in inflammatory mice. Deletion of PTPN2 could significantly induce monocytes toward M1 phenotype of macrophages, enhance the secretion of IL-12 and IL-1, and promote cell proliferation, invasion and metastasis. Mechanism research showed that PTPN2-mediated p65/p38/STAT3 de-phosphorylation could block the process of macrophage inflammation. In vivo experiments showed that PTPN2 may effectively inhibit the inflammatory response during atherosclerosis. In conclusion, we uncovered the negative role of PTPN2 in the occurrence of atherosclerosis, and this study provides a new potential target for atherosclerosis treatment.
Keywords: PTPN2, inflammation, macrophage, atherosclerosis
INTRODUCTION
Cardiovascular disease is the leading cause of mortality in the world [1]. Atherosclerosis is the main cause of cardiovascular disease, the dominant global health threat, and a huge burden for society [2, 3]. Atherosclerotic plaque and symptoms are two typical characteristics of atherosclerosis in early stage [4]. The plaques will become larger and more unstable with the progress of atherosclerosis. This leads to the obstruction of blood flow, and induces myocardial infarction or stroke [5]. Atherosclerosis is also a chronic inflammatory disease [6]. Accumulation of immune cells and necrotic debris, and endothelial dysfunction are its typical characteristics. This will lead to vascular endothelium formation of atherosclerotic plaques [7–9]. Systemic inflammation is another feature of this disease, and high levels of C-reactive protein (CRP) is a biomarker for it [10, 11]. Despite decades of research, the molecular mechanism underlying atherosclerosis is still unclear.
Persistent systemic inflammation is one typical characteristic in atherosclerosis. Exploring its molecular mechanisms has a great value for atherosclerosis treatment. Studies have found that a large number of immune cells are present in atherosclerotic lesions [12]. The main cells among these are macrophages [13]. Macrophages are mainly derived from monocytes which differentiation in the intima of arteries [14]. This process is mainly affected by the local microenvironment [15], the metabolic status of macrophages [16], and some epigenetic factors [17]. But the detailed molecular mechanism is unclear. The main types of macrophages include M1 and M2 types, which are also called as pro-inflammatory and anti-inflammatory macrophages, respectively [18, 19]. M1 macrophage could secrete multiple pro-inflammatory factors, such as TNF-α, IL-1α, IL-1β, IL-12, as well as the chemokine CXCL9, CXCL10, ROS and nitric oxide (NO) [20–22]. These inflammatory cytokines, chemokines, and ROS may cause the continuous inflammation around atherosclerotic plaques, the recruitment of inflammatory cells, and the formation of plaque [23, 24]. All of these researches illuminate the important role of macrophages in the process of atherosclerosis. However, the detailed regulation mechanism of inflammatory factors secreted by macrophages remains unclear. It is still lacking effective target for atherosclerosis treatment.
In this study, we performed a preliminary study on the molecular mechanism of atherosclerosis, and attempted to find an effective target to block the occurrence of macrophage inflammation and atherosclerotic plaque. We constructed an APOE-/- mice model of atherosclerosis, and found that PTPN2 was dramatically decreased in inflammatory mice. Loss-of-function study showed that, PTPN2 deficiency could induce monocytes to M1 phenotype of macrophages, enhance the secretion of IL-12 and IL-1β, and promote cell proliferation, invasion and metastasis. Mechanism research indicated that PTPN2-mediated p65/p38/STAT3 de-phosphorylation could block macrophages inflammation. In vivo experiments showed that PTPN2 could inhibit the inflammatory response in atherosclerosis. We uncovered the negative role of PTPN2 in macrophages inflammation, and this work may provide a new potential target for atherosclerosis treatment.
RESULTS
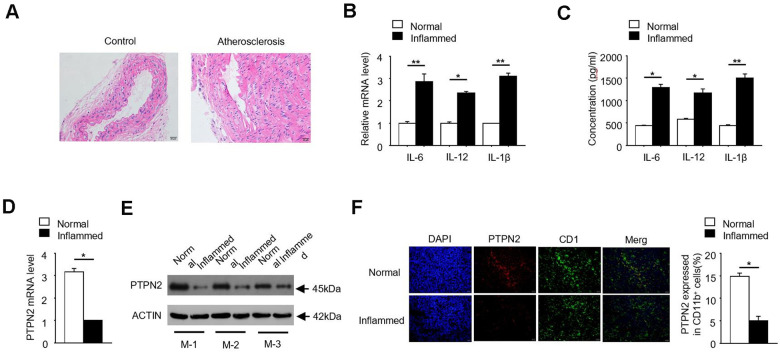
PTPN2 is negatively correlated with inflammation in ApoE-/- mice
In order to investigate the pathogenesis of atherosclerosis, we constructed an APOE-/- mice model of atherosclerosis. The photomicrograph of atherosclerotic lesions stained with Hematoxylin-Eosin was showed in Figure 1A. Due to the release of inflammatory factors is one of its typical characteristics, we detected the expression of IL-6, IL-12 and IL-1β in normal and inflammatory aortic roots of ApoE-/- mice. qRT-PCR assay showed that the mRNA levels of inflammatory factors IL-6, IL-12 and IL-1β were significantly increased in inflammatory APOE-/- mice (Figure 1B). Consistently, the protein concentrations of IL-6, IL-12 and IL-1β were also significantly increased in inflammatory APOE-/- mice (Figure 1C). PTPN2, which is one of non-receptor protein tyrosine phosphatases, is related to the occurrence of various inflammatory-linked diseases [25, 26]. In order to explore the relationship between PTPN2 and inflammation in APOE-/- mice, we detected the expression of PTPN2 in normal and inflammatory APOE-/- mice. qRT-PCR assay showed that the mRNA expression of PTPN2 was significantly reduced in inflammatory APOE-/- mice (Figure 1D). Consistently, the protein level of PTPN2 in three different inflammatory APOE-/- mice was also lower than that in normal control mice (Figure 1E). In addition, we also analyzed the protein level of PTPN2 in normal and inflammatory APOE-/- mice by confocal microscopy. Compared with the normal control, PTPN2 in inflammatory APOE-/- mice was significantly reduced, while the expression level of CD11b has no obvious change (Figure 1F). These results indicate that the APOE-/- mice model of atherosclerosis has obvious inflammation, and PTPN2 is negatively correlated with inflammation in ApoE-/- mice.
Figure 1.
PTPN2 is negatively correlated with inflammation in ApoE-/- mice. (A) Photomicrograph of atherosclerotic lesions stained with Hematoxylin-Eosin. (B) The mRNA level of IL-6, IL-12 and IL-1β in macrophages from normal and inflamed aortic roots were analyzed by qRT-PCR. (C) ELISA assay analysis the production of IL-6, IL-12, IL-1β in macrophages from normal and inflamed fictions. (D) PTPN2 mRNA level in normal and inflamed aortic roots were analyzed by qRT-PCR. (E) IB analysis PTPN2 expression from three different ApoE-/- mice. M-1, M-2, M-3 were three different ApoE-/- mice. (F) Confocal microscopy analysis CD11b and PTPN2 in normal and inflamed aortic roots in ApoE-/- mice. Data is representative of at least three independent experiments and are presented as mean ± SD. ns, not statistically significant; *, P < 0.05. **, P < 0.01.
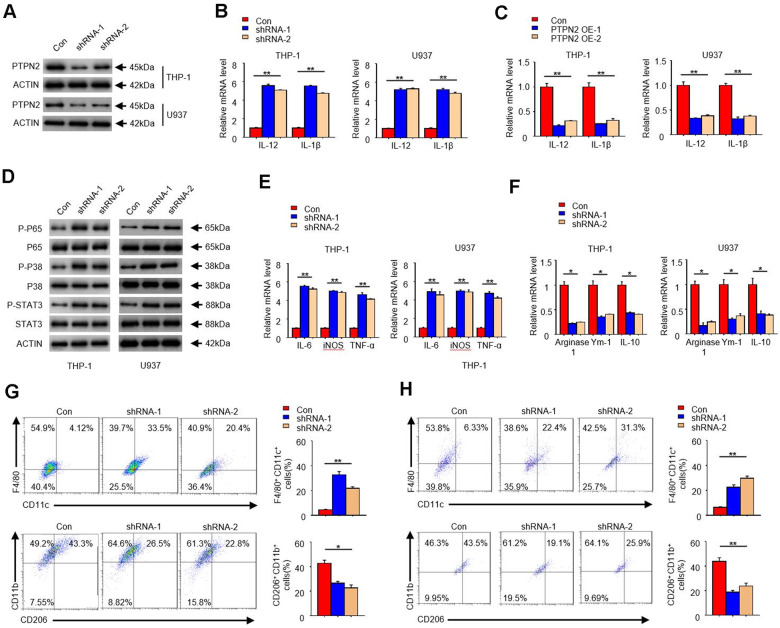
PTPN2 deficiency enhances the secretion of inflammatory cytokines in THP-1 cells and U937 cells, and toward M1 phenotype
In order to reveal the function of PTPN2 in the occurrence of atherosclerosis, we artificially synthesized two shRNA of PTPN2 gene, and used the THP-1 cell and U937 cell as the model to research. Firstly, we transfected these two shRNA segments into THP-1 cell and U937 cell, and analyzed the protein of PTPN2 by Western blot assay. Results showed that both shRNA could significantly inhibit the expression of PTPN2 protein (Figure 2A). To explore the effect of PTPN2 deficiency on the secretion of inflammatory factors, we examined the changes of IL-12 and IL-1β in THP-1cells and U937 cells. qRT-PCR assay showed that PTPN2 deficiency could enhance the mRNA expression of IL-12 and IL-1β (Figure 2B). Conversely, overexpression of PTPN2 could also significantly inhibit the expression of IL-12 and IL-1β in THP-1 cells and U937 cells (Figure 2C). In addition, the activation of NF-κB signal pathway, MAPK signal pathway and JAK-STAT signal pathway are closely related to the secretion of inflammatory factors [27–29]. We also tested the phosphorylation levels of p65, p38 and STAT3 in THP-1 cells and U937 cells. Western blot experiments showed that shRNA-1 or shRNA-2 of PTPN2 could increase the phosphorylation levels of p65, p38 and STAT3, but it has no obvious change on total p65, p38 and STAT3 proteins (Figure 2D). These results indicate that PTPN2 deficiency induces the secretion of inflammatory factors by activating the p65/p38 /STAT3 signal pathway.
Figure 2.
PTPN2 deficiency enhances the secretion of inflammatory cytokines in THP-1 cells and U937 cells, and toward M1 phenotype. shRNA-1 and shRNA-2 of PTPN2 were used to knock down the expression of PTPN2 in THP-1 cells and U937 cells. (A) IB analysis PTPN2 expression in THP-1 cells and U937 cells. (B) The mRNA level of IL-12 and IL-1β in THP-1 cells and U937 cells were analyzed by qRT-PCR. (C) Expression of IL-12 and IL-1β in THP-1 cells or U937 cells with PTPN2 overexpression were detected by qRT-PCR. (D) IB analysis the protein levels of p65, p38 and STAT3 in THP-1 cells and U937 cells. (E, F) M1 and M2 related polarization genes were analyzed by qRT-PCR assay in THP-1 cells and U937 cells. (G, H) Flow cytometry analysis the polarization of THP-1 cells and U937 cells. Data are representative of at least three independent experiments and are presented as mean ± SD. ns, not statistically significant; *, P < 0.05. **, P < 0.01.
In addition, we also analyzed the polarization characteristics of THP-1 cells and U937 cells. As shown in Figure 2E, the expression of IL-6, TNF-a, and iNOS, which associated with M1 polarization, were significantly increased in PTPN2 deficiency cells. Conversely, the expression of Arginase1, Ym1, and IL-10, which associated with M2 polarization, were reduced in PTPN2 deficiency cells (Figure 2F). F4/80+ CD11C+ is the surface antigen marker of M1 phenotype, while CD206+ / CD11B+ is the surface antigen marker of M2 phenotype. Flow cytometry assays showed that THP-1 cell with F4/80+CD11C+ were significantly increased, and THP-1 cell with CD206+ / CD11B+ were significantly decreased after PTPN2 was suppressed by its shRNA (Figure 2G). The results observed in U937 cells were consistent with those results in THP-1 cells (Figure 2H). All of these results showed that the loss of PTPN2 will lead to enhance the secretion of inflammatory cytokines and toward M1 phenotype.
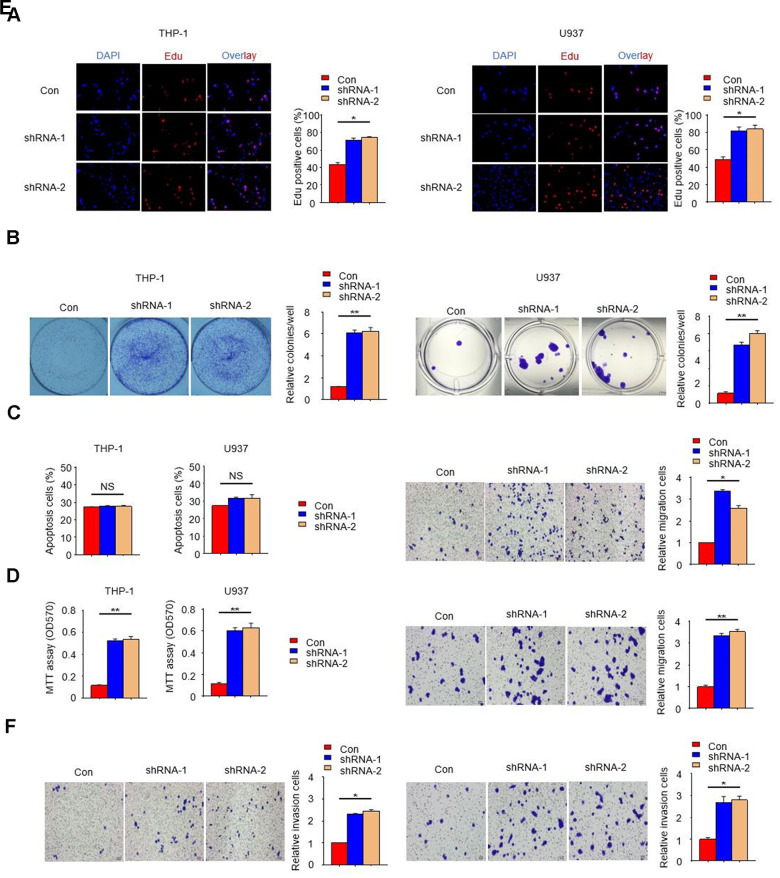
PTPN2 deficiency promotes the proliferation, migration and invasion of THP-1 cells and U937 cells
In order to further reveal the effect of PTPN2 deletion on THP-1 cells and U937 cells, we examined the cell proliferation ability with PTPN2 deficiency by EDU assay. Results showed that the proliferation ability of THP-1 cells and U937 cells with PTPN2 deficiency was enhanced when compared to control cells (Figure 3A). The proliferation and apoptotic capacity were also detected by clone formation assay and flow cytometry. Results showed that cells with PTPN2 deficiency has stronger proliferation ability than the control cells (Figure 3B). Flow cytometry assay showed that there was no difference in the proportion of apoptotic cells between PTPN2 deficiency cells and control cells (Figure 3C). In addition, we also incubated HUVEC cells with THP-1 cells or U937 cells for a period of time, and found that the proliferation ability of HUVEC cells was increased significantly (Figure 3D). These results showed that interference with the expression of PTPN2 gene could promote cell proliferation, with no effect on its apoptosis. In addition, we also evaluated the migration and invasion ability of THP-1 cells and U937 cells. Results showed that deletion of PTPN2 could enhance the migration and invasion of cells (Figure 3E, 3F). The above results suggested that PTPN2 deficiency promotes proliferation, metastasis and invasion of THP-1 cells and U937 cells.
Figure 3.
PTPN2 deficiency promotes the proliferation, migration and invasion of THP-1 cells and U937 cells. (A, B) EDU assay and colony formation assay were used to analyze the proliferation ability of THP-1 cells and U937 cells. (C) Apoptosis of THP-1 cells and U937 cells were evaluated by flow cytometry. (D) MTT assay were used to examine the viability of HUVEC cell after incubated with THP-1 cells or U937 cells. (E, F) Transwell migration and invasion assays were performed in THP-1 cells and U937 cells. The upper is THP-1 cells and the lower is U937 cells in Figure 3E. The left is THP-1 cells and the right is U937 cells in Figure 3F. Bar= 20μM. Data are representative of at least three independent experiments and are presented as mean ± SD. ns, not statistically significant; *, P < 0.05. **, P < 0.01.
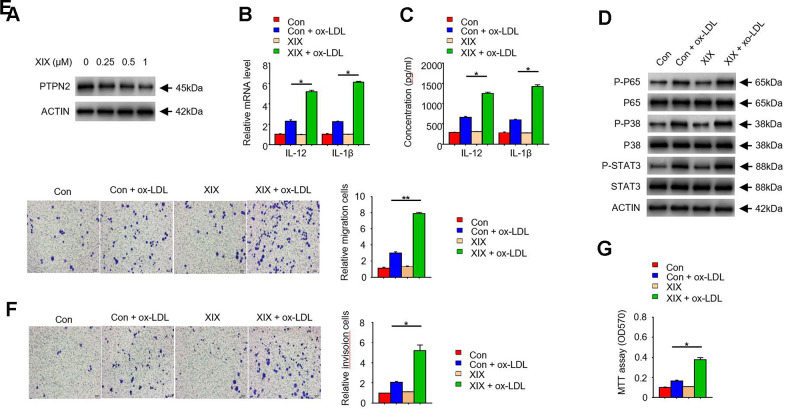
PTPN2 inhibitor XIX mimics the effects of PTPN2 deletion in THP-1 cells
To further examine the function of PTPN2 in macrophages, we used several concentrations of XIX, a PTPN2 inhibitor, to treat with THP-1 cells. The expression of PTPN2 and the secretion of IL-12 and IL-1β were detected. Results showed that XIX with 0.25uM, 0.5uM, and 1.0uM could inhibit the expression of PTPN2 protein, and the effect of inhibition was more obvious when the concentration of XIX increased (Figure 4A). Furthermore, we combined XIX (1.0 μM) and ox-LDL to treat with THP-1 cells and examined the secretion of IL-12 and IL-1β. Compared with the group which only treated with ox-LDL, the mRNA of IL-12 and IL-1β were increased in the XIX + ox-LDL group (Figure 4B). Consistently, the secretion of IL-12 and IL-1β were also enhanced in the XIX + ox-LDL group (Figure 4C). In addition, we detected the phosphorylation levels of p65, p38, and STAT3 proteins in different groups. Results showed that the levels of p-p65, p-p38, and p-STAT3 proteins were higher in XIX + ox-LDL group than in ox-LDL group (Figure 4D). We also examined the effect of XIX on the migration, invasion, and proliferation ability of THP-1 cells. Compared with the group which treated with ox-LDL alone, the metastatic and invasion capacity of cells in the XIX + ox-LDL group were enhanced (Figure 4E, 4F). MTT assay showed that the proliferation ability of cells was enhanced in the XIX + ox-LDL group (Figure 4G). These results showed that, similar to the shRNA of PTPN2, XIX combined with ox-LDL could also induce the phosphorylation of p65, p38 and STAT3, enhance the secretion of IL-12 and IL-1β, and promote cell proliferation, invasion and metastasis.
Figure 4.
PTPN2 inhibitor XIX mimics the effects of PTPN2 deletion in THP-1 cells. (A) Expression of PTPN2 in THP-1 cells with different concentration of XIX were detected by IB assay. (B) mRNA levels of IL-12 and IL-1β in THP-1 cells were analyzed by qRT-PCR assay. (C) ELISA assay was used to analyze the production of IL-12 and IL-1β in THP-1 cells in the presence of XIX or ox-LDL. (D) Indicated proteins in THP-1 cells were detected by IB assay. (E, F) Transwell migration and invasion assays were performed in THP-1 cells. Bar= 20μM. (G) MTT assay was used to analyze the viability of HUVEC cell after incubated with THP-1 cells. Data are representative of at least three independent experiments and are presented as mean ± SD. ns, not statistically significant; *, P < 0.05. **, P < 0.01.
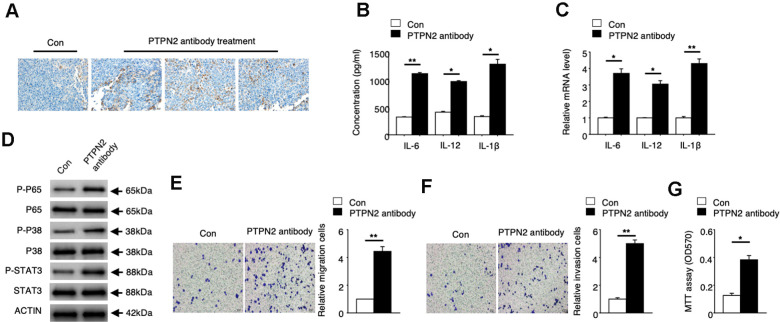
PTPN2 can be a potential treatment target of atherosclerosis
To explore the potential application value of PTPN2 on the treatment of atherosclerosis, we performed an in vivo assay in APOE-/- mice. PBS control or PTPN2 antibody were injected into APOE-/- mice by tail vein injection. Expression of PTPN2 proteins were detected by immunohistochemistry assay. The mRNA and protein levels of IL-6, IL-12 and IL-1β were analyzed by qRT-PCR assay and ELISA assay. Immunohistochemistry assay showed that PTPN2 antibody could reduce the expression of PTPN2 in macrophages of mice (Figure 5A). The mRNA and protein levels of IL-6, IL-12 and IL-1β was increased in macrophages when treated with PTPN2 antibody (Figure 5B, 5C). The phosphorylation levels of p65, p38, and STAT3 protein were also elevated after treatment with PTPN2 antibody (Figure 5D). Further research revealed that the ability of metastasis and invasion were enhanced when treatment with PTPN2 antibody (Figure 5E, 5F). MTT experiments showed that PTPN2 antibody could significantly promote the proliferation of macrophages (Figure 5G). These results indicated that PTPN2 plays a negative role in the occurrence of atherosclerosis by inhibiting the secretion of inflammatory cytokines, and may be a potential treatment target of atherosclerosis.
Figure 5.
PTPN2 can be a potential atherosis treatment target. PBS control and PTPN2 antibody were injected into ApoE-/- mice by tail vain injected. (A) Immunohistochemistry of CD68 in aortic roots of ApoE-/- mice which treated with PBS or PTPN2 antibody were performed. (B) ELISA assay was used to analyze the production of IL-6, IL-12 and IL-1β in macrophages. (C) The mRNA levels of IL-6, IL-12 and IL-1β in macrophages were analyzed by qRT-PCR assay. (D) IB assay was used to detect the expression of indicated proteins in macrophages. (E, F) Transwell migration and invasion assays in macrophages were performed. Bar= 20μM. (G) MTT assay was used to analyze the viability of HUVEC cell which incubated with macrophages. Data are representative of at least three independent experiments and are presented as mean ± SD. ns, not statistically significant; *, P < 0.05. **, P < 0.01.
DISCUSSION
PTPN2 is an enzyme for protein de-phosphorylation, and cloned from T cell cDNA library [30]. It is abnormally high expression in lymphocytes and functions as a negative regulator in multiple inflammatory signaling pathways [31–33]. Abnormal expression of PTPN2 will lead to the occurrence of many inflammatory diseases [25, 26]. In vivo experiments have shown that deletion of PTPN2 will lead to severe systemic inflammation, multiple organ dysfunction, and die within 4-5 weeks [34, 35]. All of these researches indicate that PTPN2 is closely related to the occurrence of inflammation. One typical characteristic of atherosclerosis is the systemic inflammation. Therefore, we analyzed the expression of PTPN2 in APOE-/- mice model of atherosclerosis. As we expected, the mRNA and protein expression levels of PTPN2 were significantly decreased in inflammatory mice. Deletion of PTPN2 could induce the secretion of inflammatory cytokines and promote the proliferation, invasion and metastasis of macrophages. These works suggested that PTPN2 plays an anti-inflammatory role in the occurrence of atherosclerosis, and the absence of PTPN2 may lead to the persistent inflammation in macrophages.
Macrophage can be divided into M1 and M2 phenotype. M1 phenotype is a type of pro-inflammatory macrophages which can secrete inflammatory factors [36]. This will lead to the recruitment of inflammatory cells, and cause abnormal events such as thrombosis [37]. Conversely, M2 phenotype of macrophage is an anti-inflammatory cell. It will block the recruitment of inflammatory cells, inhibit the release of inflammatory factors, reduce the formation of foam cells, and relieve the development of atherosclerosis [38, 39]. To explore the differentiation process of monocyte toward M1 phenotype is very important for atherosclerosis treatment. In this study, we investigated that whether PTPN2 can induce monocytes toward M1 phenotype. The results showed that PTPN2 deficiency could significantly enhance the THP-1 cells and U937 cells toward M1 phenotype but not toward M2 phenotype. The proportion of F4/80+ CD11C+ positive cells was increased after deletion of PTPN2. The levels of IL-6, TNF-a and iNOS, which are associated with M1 polarization, were also notably increased. These results showed that PTPN2 deficiency can not only regulate the proliferation, invasion and metastasis, but also induce monocyte toward M1 phenotype of macrophages.
p65 is a transcription factor that encoded by RELA gene and is also known as the nuclear factor NF-κB p65 subunit [40, 41]. It is a key subunit of NF-κB and involves in the formation of heterodimers, nuclear translocations, and activation of NF-κB signal pathway [42]. p38 is a protein associated with MAPK signaling pathway. It can respond to stress stimuli and participate in regulating various biological processes, such as cell differentiation, apoptosis, and autophagy [43, 44]. STAT3 is the transcriptional activator of JAK-STAT signaling pathway and activated by the phosphorylation of receptor-associated Janus kinase (JAK) [45, 46]. The JAK-STAT signaling pathway can regulate the release of multiple inflammatory factors in various diseases [47]. In this study, we found that deletion of PTPN2 could promote the phosphorylation of p65, p38 and STAT3, and activate the release of related inflammatory factors. We also performed the similar experiment in mice by PTPN2 antibodies. Results showed that loss of PTPN2 enhanced the phosphorylation of p65, p38 and STAT3, and then activated the related signaling pathways. These results indicate that PTPN2 may play a negative role in the occurrence of macrophage inflammation by regulating the dephosphorylation of p65, p38 and STAT3.
In summary, we have preliminary studied the molecular mechanism of atherosclerosis by constructing an APOE-/- mice model. We found that the expression of PTPN2 is negative correlation with inflammation in APOE-/- mice. shRNA of PTPN2 could significantly enhance the secretion of inflammatory cytokines in macrophages, induce monocyte toward M1 phenotype of macrophages, and promote cell proliferation, invasion and metastasis. PTPN2 inhibitor XIX combined with ox-LDL could observed a similar phenomenon as the absence of PTPN2. In vivo experiments revealed that PTPN2 antibody could reduce the protein level of PTPN2, promote the secretion of inflammatory cytokines, and induce the proliferation, invasion and metastasis of macrophages. In a word, in vitro and in vivo results suggested that PTPN2 has a negative role on the regulation of macrophage inflammation in atherosclerosis, and it may become a potential target for atherosclerosis treatment.
MATERIALS AND METHODS
Atherosclerosis model in mice
All of animal assays in this study were carried out and approved by Animal Care Committee of Jiangxi Provincial People's Hospital Affiliated to Nanchang University according to the guidelines. ApoE-/- mice (6-week old male) were fed with high-fat diet (HFD) and induced to be atherosclerosis mice model. 12 weeks later, all ApoE-/- mice were killed by cervical dislocation, and the aortic roots were isolated and frozen in liquid nitrogen for subsequent experiments. PTPN2 antibody were intravenously injected through tail vein of ApoE-/- mice. Macrophages in aortic roots were isolated by use of tissue lymphocyte separation solution (TBD, Tianjin, China) according to the protocol, and cultured in DMEM medium (Invitrogen, USA) with 1% penicillin/streptomycin (Sigma-Aldrich, USA), used in following experiments.
Cell culture
THP-1 cells were purchased from the ATCC (Manassas, USA). RPMI1640 culture medium (Invitrogen, USA) was used for the culture of this cells. 10% heat-inactivated FBS (Invitrogen, USA) and 1% penicillin/streptomycin (Sigma, USA) were added in the medium. These cells were incubated in a humidified atmosphere of 5% CO2 at 37° C. PTP inhibitor XIX is purchased from Sigma Aldrich. The Lot No. of PTP inhibitor XIX is 540215.
Enzyme-linked immunosorbent assay (ELISA)
The protein expression of IL-6, IL-12 and IL-1β were detected by ELISA kits (R&D Systems, Minneapolis, MN, USA) following the manufacturer's protocols.
RNA isolation and qRT-PCR assay
Total RNA was extracted using the RNAiso Plus and reversely transcribed into cDNA using the Prime Script RT Master Mix. SYBR Premix Ex Taq II (Takara Bio, China) was used for qPCR assay. The primers used in human cells are as follows:
PTPN2-Forward (5'-3'): CATGCTGAACCGCATTGTGGAG,
PTPN2-Reverse (5'-3'): GACAAGAGCTTCACACTGAATCC;
IL-6-Forward (5'-3'): AGACAGCCACTCACCTCTTCAG,
IL-6-Reverse (5'-3'): TTCTGCCAGTGCCTCTTTGCTG;
IL-12-Forward (5'-3'): TGCCTTCACCACTCCCAAAACC,
IL-12-Reverse (5'-3'): CAATCTCTTCAGAAGTGCAAGGG;
IL-1β-Forward (5'-3'): CCACAGACCTTCCAGGAGAATG,
IL-1β-Reverse (5'-3'): GTGCAGTTCAGTGATCGTACAGG;
iNOS-Forward (5'-3'): GCTCTACACCTCCAATGTGACC,
iNOS-Reverse (5'-3'): CTGCCGAGATTTGAGCCTCATG;
TNF-α-Forward (5'-3'): CTCTTCTGCCTGCTGCACTTTG,
TNF-α-Reverse (5'-3'): ATGGGCTACAGGCTTGTCACTC;
Arginase-1-Forward (5'-3'): TCATCTGGGTGGATGCTCACAC,
Arginase-1-Reverse (5'-3'): GAGAATCCTGGCACATCGGGAA;
Ym-1-Forward (5'-3'): TACTCACTTCCACAGGAGCAGG,
Ym-1- Reverse (5'-3'): CTCCAGTGTAGCCATCCTTAGG;
IL-10-Forward (5'-3'): TCTCCGAGATGCCTTCAGCAGA,
IL-10-Reverse (5'-3'): TCAGACAAGGCTTGGCAACCCA;
GAPDH-Forward (5'-3'): GTCTCCTCTGACTTCAACAGCG,
GAPDH-Reverse (5'-3'): ACCACCCTGTTGCTGTAGCCAA.
The primers used in mouse cells are as follows:
IL-12-Forward (5'-3'): ACGAGAGTTGCCTGGCTACTAG,
IL-12-Reverse (5'-3'): CCTCATAGATGCTACCAAGGCAC;
IL-6-Forward (5'-3'): TACCACTTCACAAGTCGGAGGC,
IL-6-Reverse (5'-3'): CTGCAAGTGCATCATCGTTGTTC;
IL-1β-Forward (5'-3'): TGGACCTTCCAGGATGAGGACA,
IL-1β-Reverse (5'-3'): GTTCATCTCGGAGCCTGTAGTG;
GAPDH-Forward (5'-3'): CATCACTGCCACCCAGAAGACTG,
GAPDH-Reverse (5'-3'): ATGCCAGTGAGCTTCCCGTTCAG.
The Applied Biosystems 7900 Real Time PCR System (Applied Biosystems, USA) was used according to the manufacturer's instruction. CT values were recorded and expression of genes was calculated using the equation 2-ΔΔCt.
Transfection of shRNA
Scrambled shRNA control and PTPN2-shRNA were transfected into THP-1 cells using Lipofectamine 2000 (Thermo Fisher) in 24-well plates. THP-1 cells were incubated for 18 h with in Opti-MEM containing 3μL Lipofectamine 2000 per 2×105 cells and 20-50 nM shRNA according to the instructions. The sequence of shRNA are as follows:
shRNA-1-F: GTGTGAAGCTCTTATCTGA,
shRNA-1-R: TCAGATAAGAG CTTCACAC;
shRNA-2-F: GCTCTTATCTGAAGATGTA,
shRNA-2-R: TACATCTTCAGATAAGAGC.
Western blot analysis
Total proteins were extracted with SDS lysis buffer, and then separated by 10% SDS polyacrylamide gels. Proteins were transferred to the PVDF membrane after electrophoresis and blocked with 5% defatted milk for 1 hour. The blots were incubated with primary antibodies overnight, and then incubated with goat-anti-mouse IgG or goat-anti-rabbit IgG. β-actin or GAPDH was used as a loading control. The primary antibodies: anti-p38(1:1000, Abcam), anti-p-p38 (1:1000, Cell Signaling Technology), anti-p65 (1:1000, Cell Signaling Technology), anti-p-p65 (1:1000, Cell Signaling Technology), anti-STAT3 (1:1000, Cell Signaling Technology), anti-p-STAT3 (1:1000, Abcam), anti-PTPN2 (1:1000, Cell Signaling Technology), and anti-β-actin (1:5000, Cell Signaling Technology) were used in this study.
Confocal microscopy assay
Macrophages were isolated from the aortic roots of mice and were incubated with primary antibodies of PTPN2 and CD11b (CST, USA) and following secondary fluorescence-labelled antibodies (CST, USA). DAPI solution was applied to stain cell nucleus. Cells were scanned under the confocal laser scanning microscope.
EDU assay
EDU assay (Beyotime, Nanjing, China) was carried out to determine macrophages proliferation. 1x104 cells were incubated in a 96-well plate overnight and then transfected by shRNA-1 or shRNA-2. The cell viability was detected after adding EDU solution to each well and incubating. Immunofluorescence analysis was performed for EDU detection.
Cell proliferation, migration and invasion assay
MTT assay was performed to analyze the proliferation ability of cells. 2×105 cells were plated in 24-well plates and cultured for 3 days. Cell viability was evaluated by the absorbance of 490nm (OD490) according to the instructions. 500 cells were plated in 6-well plates and cultured for 10-14 days in colony formation assay. Cell viability was evaluated by the count of colonies. 2×105 cells were seeded into the chamber (migration) or matrigel coated chambers (invasion) and incubated 24h or 36h. The migration and invasion cells were evaluated by the count of five randomly selected optical fields.
Flow cytometry assay
The THP-1 cells which transfected with shRNA-1 or shRNA-2 of PTPN were harvested, and the Annexin V-APC kit (eBioscience, USA) was performed to evaluate the apoptosis of THP-1 cells. Antibodies against F4/80, CD11b, CD11c, CD206 and controls and secondary antibodies (eBioscience, USA) were incubated with cells according to the manufacturers’ instructions. All experiments were performed independently in triplicate.
Statistical analysis
Student's t-test was carried out to analyze the difference between groups, and it is statistical significance when P value was less than 0.05. At least three independent experiments were performed for data analysis. GraphPad Prism (Version5.0) were used for the statistical analysis.
Footnotes
AUTHOR CONTRIBUTIONS: XC and YF designed the study; XH, RM, JC and XD performed the experiments and participated in the data analysis; XH drafted the manuscript; XC revised the manuscript; All authors approved the final proof.
CONFLICTS OF INTEREST: All authors declare no conflicts of interest.
FUNDING: This study was supported by a grant from National Natural Science foundation of China [Grant No. 81370308] and a grant from Natural Science foundation of Hubei [Grant No.2015CFB701] and Zhongnan Hospital of Wuhan University Science, Technology and Innovation Seed Fund, [Project znpy2018099].
REFERENCES
- 1.Dahlöf B. Cardiovascular disease risk factors: epidemiology and risk assessment. Am J Cardiol. 2010; 105:3A–9A. 10.1016/j.amjcard.2009.10.007 [DOI] [PubMed] [Google Scholar]
- 2.Libby P, Lichtman AH, Hansson GK. Immune effector mechanisms implicated in atherosclerosis: from mice to humans. Immunity. 2013; 38:1092–104. 10.1016/j.immuni.2013.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, Abbastabar H, Abd-Allah F, Abdela J, Abdelalim A, Abdollahpour I, Abdulkader RS, Abebe Z, et al. , and GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018; 392:1789–858. 10.1016/S0140-6736(18)32279-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berenson GS, Srinivasan SR, Bao W, Newman WP 3rd, Tracy RE, Wattigney WA. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The bogalusa heart study. N Engl J Med. 1998; 338:1650–56. 10.1056/NEJM199806043382302 [DOI] [PubMed] [Google Scholar]
- 5.Hansson GK, Libby P, Tabas I. Inflammation and plaque vulnerability. J Intern Med. 2015; 278:483–93. 10.1111/joim.12406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ross R. Atherosclerosis—an inflammatory disease. N Engl J Med. 1999; 340:115–26. 10.1056/NEJM199901143400207 [DOI] [PubMed] [Google Scholar]
- 7.Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005; 352:1685–95. 10.1056/NEJMra043430 [DOI] [PubMed] [Google Scholar]
- 8.Bäck M, Hansson GK. Anti-inflammatory therapies for atherosclerosis. Nat Rev Cardiol. 2015; 12:199–211. 10.1038/nrcardio.2015.5 [DOI] [PubMed] [Google Scholar]
- 9.Galkina E, Ley K. Immune and inflammatory mechanisms of atherosclerosis (*). Annu Rev Immunol. 2009; 27:165–97. 10.1146/annurev.immunol.021908.132620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pepys MB, Hirschfield GM. C-reactive protein: a critical update. J Clin Invest. 2003; 111:1805–12. 10.1172/JCI18921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xu MM, Murphy PA, Vella AT. Activated T-effector seeds: cultivating atherosclerotic plaque through alternative activation. Am J Physiol Heart Circ Physiol. 2019; 316:H1354–65. 10.1152/ajpheart.00148.2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abdolmaleki F, Gheibi Hayat SM, Bianconi V, Johnston TP, Sahebkar A. Atherosclerosis and immunity: a perspective. Trends Cardiovasc Med. 2019; 29:363–71. 10.1016/j.tcm.2018.09.017 [DOI] [PubMed] [Google Scholar]
- 13.Xu H, Jiang J, Chen W, Li W, Chen Z. Vascular macrophages in atherosclerosis. J Immunol Res. 2019; 2019:4354786. 10.1155/2019/4354786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chinetti-Gbaguidi G, Colin S, Staels B. Macrophage subsets in atherosclerosis. Nat Rev Cardiol. 2015; 12:10–17. 10.1038/nrcardio.2014.173 [DOI] [PubMed] [Google Scholar]
- 15.Lavin Y, Winter D, Blecher-Gonen R, David E, Keren-Shaul H, Merad M, Jung S, Amit I. Tissue-resident macrophage enhancer landscapes are shaped by the local microenvironment. Cell. 2014; 159:1312–26. 10.1016/j.cell.2014.11.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Joseph P, Tawakol A. Imaging atherosclerosis with positron emission tomography. Eur Heart J. 2016; 37:2974–80. 10.1093/eurheartj/ehw147 [DOI] [PubMed] [Google Scholar]
- 17.Phan AT, Goldrath AW, Glass CK. Metabolic and epigenetic coordination of T cell and macrophage immunity. Immunity. 2017; 46:714–29. 10.1016/j.immuni.2017.04.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goerdt S, Politz O, Schledzewski K, Birk R, Gratchev A, Guillot P, Hakiy N, Klemke CD, Dippel E, Kodelja V, Orfanos CE. Alternative versus classical activation of macrophages. Pathobiology. 1999; 67:222–26. 10.1159/000028096 [DOI] [PubMed] [Google Scholar]
- 19.Shapouri-Moghaddam A, Mohammadian S, Vazini H, Taghadosi M, Esmaeili SA, Mardani F, Seifi B, Mohammadi A, Afshari JT, Sahebkar A. Macrophage plasticity, polarization, and function in health and disease. J Cell Physiol. 2018; 233:6425–40. 10.1002/jcp.26429 [DOI] [PubMed] [Google Scholar]
- 20.Bobryshev YV, Ivanova EA, Chistiakov DA, Nikiforov NG, Orekhov AN. Macrophages and their role in atherosclerosis: pathophysiology and transcriptome analysis. Biomed Res Int. 2016; 2016:9582430. 10.1155/2016/9582430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mosser DM. The many faces of macrophage activation. J Leukoc Biol. 2003; 73:209–12. 10.1189/jlb.0602325 [DOI] [PubMed] [Google Scholar]
- 22.Chistiakov DA, Bobryshev YV, Nikiforov NG, Elizova NV, Sobenin IA, Orekhov AN. Macrophage phenotypic plasticity in atherosclerosis: the associated features and the peculiarities of the expression of inflammatory genes. Int J Cardiol. 2015; 184:436–45. 10.1016/j.ijcard.2015.03.055 [DOI] [PubMed] [Google Scholar]
- 23.Thorp E, Subramanian M, Tabas I. The role of macrophages and dendritic cells in the clearance of apoptotic cells in advanced atherosclerosis. Eur J Immunol. 2011; 41:2515–18. 10.1002/eji.201141719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thorp E, Tabas I. Mechanisms and consequences of efferocytosis in advanced atherosclerosis. J Leukoc Biol. 2009; 86:1089–95. 10.1189/jlb.0209115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wellcome Trust Case Control Consortium. Genome-wide association study of 14,000 cases of seven common diseases and 3,000 shared controls. Nature. 2007; 447:661–78. 10.1038/nature05911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Todd JA, Walker NM, Cooper JD, Smyth DJ, Downes K, Plagnol V, Bailey R, Nejentsev S, Field SF, Payne F, Lowe CE, Szeszko JS, Hafler JP, et al. , and Genetics of Type 1 Diabetes in Finland, and Wellcome Trust Case Control Consortium. Robust associations of four new chromosome regions from genome-wide analyses of type 1 diabetes. Nat Genet. 2007; 39:857–64. 10.1038/ng2068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sun SC. The non-canonical NF-κB pathway in immunity and inflammation. Nat Rev Immunol. 2017; 17:545–58. 10.1038/nri.2017.52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reustle A, Torzewski M. Role of p38 MAPK in atherosclerosis and aortic valve sclerosis. Int J Mol Sci. 2018; 19:3761. 10.3390/ijms19123761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Villarino AV, Kanno Y, O’Shea JJ. Mechanisms and consequences of Jak-STAT signaling in the immune system. Nat Immunol. 2017; 18:374–84. 10.1038/ni.3691 [DOI] [PubMed] [Google Scholar]
- 30.Cool DE, Tonks NK, Charbonneau H, Walsh KA, Fischer EH, Krebs EG. cDNA isolated from a human T-cell library encodes a member of the protein-tyrosine-phosphatase family. Proc Natl Acad Sci USA. 1989; 86:5257–61. 10.1073/pnas.86.14.5257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Doody KM, Bourdeau A, Tremblay ML. T-cell protein tyrosine phosphatase is a key regulator in immune cell signaling: lessons from the knockout mouse model and implications in human disease. Immunol Rev. 2009; 228:325–41. 10.1111/j.1600-065X.2008.00743.x [DOI] [PubMed] [Google Scholar]
- 32.Aradi B, Kato M, Filkova M, Karouzakis E, Klein K, Scharl M, Kolling C, Michel BA, Gay RE, Buzas EI, Gay S, Jüngel A. Protein tyrosine phosphatase nonreceptor type 2: an important regulator of lnterleukin-6 production in rheumatoid arthritis synovial fibroblasts. Arthritis Rheumatol. 2015; 67:2624–33. 10.1002/art.39256 [DOI] [PubMed] [Google Scholar]
- 33.Scharl M, Hruz P, McCole DF. Protein tyrosine phosphatase non-receptor type 2 regulates IFN-γ-induced cytokine signaling in THP-1 monocytes. Inflamm Bowel Dis. 2010; 16:2055–64. 10.1002/ibd.21325 [DOI] [PubMed] [Google Scholar]
- 34.You-Ten KE, Muise ES, Itié A, Michaliszyn E, Wagner J, Jothy S, Lapp WS, Tremblay ML. Impaired bone marrow microenvironment and immune function in T cell protein tyrosine phosphatase-deficient mice. J Exp Med. 1997; 186:683–93. 10.1084/jem.186.5.683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Heinonen KM, Nestel FP, Newell EW, Charette G, Seemayer TA, Tremblay ML, Lapp WS. T-cell protein tyrosine phosphatase deletion results in progressive systemic inflammatory disease. Blood. 2004; 103:3457–64. 10.1182/blood-2003-09-3153 [DOI] [PubMed] [Google Scholar]
- 36.Pirro M, Schillaci G, Savarese G, Gemelli F, Mannarino MR, Siepi D, Bagaglia F, Mannarino E. Attenuation of inflammation with short-term dietary intervention is associated with a reduction of arterial stiffness in subjects with hypercholesterolaemia. Eur J Cardiovasc Prev Rehabil. 2004; 11:497–502. 10.1097/01.hjr.0000152243.51327.2a [DOI] [PubMed] [Google Scholar]
- 37.Morris DL, Singer K, Lumeng CN. Adipose tissue macrophages: phenotypic plasticity and diversity in lean and obese states. Curr Opin Clin Nutr Metab Care. 2011; 14:341–46. 10.1097/MCO.0b013e328347970b [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Llodrá J, Angeli V, Liu J, Trogan E, Fisher EA, Randolph GJ. Emigration of monocyte-derived cells from atherosclerotic lesions characterizes regressive, but not progressive, plaques. Proc Natl Acad Sci USA. 2004; 101:11779–84. 10.1073/pnas.0403259101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shioi A, Ikari Y. Plaque calcification during atherosclerosis progression and regression. J Atheroscler Thromb. 2018; 25:294–303. 10.5551/jat.RV17020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Oeckinghaus A, Ghosh S. The NF-kappaB family of transcription factors and its regulation. Cold Spring Harb Perspect Biol. 2009; 1:a000034. 10.1101/cshperspect.a000034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chen LF, Williams SA, Mu Y, Nakano H, Duerr JM, Buckbinder L, Greene WC. NF-kappaB RelA phosphorylation regulates RelA acetylation. Mol Cell Biol. 2005; 25:7966–75. 10.1128/MCB.25.18.7966-7975.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mussbacher M, Salzmann M, Brostjan C, Hoesel B, Schoergenhofer C, Datler H, Hohensinner P, Basílio J, Petzelbauer P, Assinger A, Schmid JA. Cell type-specific roles of NF-κB linking inflammation and thrombosis. Front Immunol. 2019; 10:85. 10.3389/fimmu.2019.00085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Roux PP, Blenis J. ERK and p38 MAPK-activated protein kinases: a family of protein kinases with diverse biological functions. Microbiol Mol Biol Rev. 2004; 68:320–44. 10.1128/MMBR.68.2.320-344.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cuenda A, Rousseau S. P38 MAP-kinases pathway regulation, function and role in human diseases. Biochim Biophys Acta. 2007; 1773:1358–75. 10.1016/j.bbamcr.2007.03.010 [DOI] [PubMed] [Google Scholar]
- 45.Zhu F, Wang KB, Rui L. STAT3 activation and oncogenesis in lymphoma. Cancers (Basel). 2019; 12:19. 10.3390/cancers12010019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stark GR, Darnell JE Jr. The JAK-STAT pathway at twenty. Immunity. 2012; 36:503–14. 10.1016/j.immuni.2012.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Banerjee S, Biehl A, Gadina M, Hasni S, Schwartz DM. JAK-STAT Signaling as a Target for Inflammatory and Autoimmune Diseases: Current and Future Prospects. Drugs. 2017; 77:521–46. 10.1007/s40265-017-0701-9 [DOI] [PMC free article] [PubMed] [Google Scholar]