Abstract
Purpose of review
The aim of this study was to evaluate the relationship between infection with SARS-CoV-2 and autoimmunity.
Recent findings
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by severe acute respiratory syndrome (SARS) associated coronavirus 2 (SARS-CoV-2). Although most of the infected individuals are asymptomatic, a proportion of patients with COVID-19 develop severe disease with multiple organ injuries. Evidence suggests that some medications used to treat autoimmune rheumatologic diseases might have therapeutic effect in patients with severe COVID-19 infections, drawing attention to the relationship between COVID-19 and autoimmune diseases. COVID-19 shares similarities with autoimmune diseases in clinical manifestations, immune responses and pathogenic mechanisms. Robust immune reactions participate in the pathogenesis of both disease conditions. Autoantibodies as a hallmark of autoimmune diseases can also be detected in COVID-19 patients. Moreover, some patients have been reported to develop autoimmune diseases, such as Guillain--Barré syndrome or systemic lupus erythematosus, after COVID-19 infection. It is speculated that SARS-CoV-2 can disturb self-tolerance and trigger autoimmune responses through cross-reactivity with host cells. The infection risk and prognosis of COVID-19 in patients with autoimmune diseases remains controversial, but patient adherence to medication regimens to prevent autoimmune disease flares is strongly recommended.
Summary
We present a review of the association between COVID-19 and autoimmune diseases, focusing on similarities in immune responses, cross-reactivity of SARS-CoV-2, the development of autoimmune diseases in COVID-19 patients and the risk of COVID-19 infection in patients with preexisting autoimmune conditions.
Keywords: autoimmune diseases, COVID-19, cross-reactivity, molecular mimicry, SARS-CoV-2
INTRODUCTION
Since December 2019, a novel infection named coronavirus disease 2019 (COVID-19) broke out in Wuhan, China, and has been sweeping across the globe. COVID-19 was officially declared a pandemic by WHO on 11 March 2020 [1]. The disease is caused by a newly identified strain of severe acute respiratory syndrome (SARS) associated coronavirus, which was named SARS-CoV-2 after SARS-CoV that caused the epidemic of SARS in 2002 [2].
SARS-CoV-2 belongs to the coronavirus family, which are enveloped viruses with a spherical morphology and a single-stranded RNA (ssRNA) genome [3]. The spike glycoproteins (S protein) cross through the peplos of the virus and form a crown-like surface [4]. Through the receptor binding domain (RBD) located in the S1 subunit of the S protein, the virus can ligate to the host cell receptor angiotensin-converting enzyme 2 (ACE2) and invade into the cell [5–7].
In many cases, hosts infected by SARS-CoV-2 present with flu-like symptoms, such as fever, fatigue and dry cough. Headache, myalgia, sore throat, nausea and diarrhoea can also be seen in patients with COVID-19 [8,9]. Shortness of breath and hypoxemia occur in severe cases. In critical cases, the disease progresses rapidly and patients can develop septic shock and multiorgan dysfunction [10]. As such, COVID-19 can be a systemic disease affecting multiple organ systems, including the skin, kidneys, respiratory system, cardiovascular system, digestive system, nervous system and haematological system [11]. The dysregulated immune response and increased pro-inflammatory cytokines induced by SARS-CoV-2 contribute to the disease pathogenesis and organ damage, which brought attention to immune-regulatory therapy in the treatment of COVID-19 [12]. Medications used to treat autoimmune diseases are widely used in critical cases of COVID-19 [13]. Further, some autoantibodies can be detected in patients with COVID-19 [14]. These observations suggest that examining pathways known to contribute to the pathogenesis of autoimmunity might provide clues to better understand and treat COVID-19.
Box 1.
no caption available
SIMILARITIES IN IMMUNE RESPONSES BETWEEN SARS-COV-2 INFECTION AND AUTOIMMUNE DISEASES
Autoimmune diseases are characterized by the existence of autoantibodies and perpetuated inflammatory reactions due to the loss of immune tolerance and dysregulated immune system, leading to target organ damage and malfunction [15]. These immune-mediated injuries also exist in COVID-19 (Fig. 1). Infection with SARS-CoV-2 induces immune reactions, which might have important implications in the development of vaccine strategies against this virus [16]. T cell immunity plays a central role in the control of SARS-CoV-2 infection. Antigen-specific CD4+ and CD8+ T cells and neutralizing antibody responses play protective roles against SARS-CoV-2, while impaired adaptive immune responses such as scarcity of naive T cells may lead to poor disease outcomes [17].
FIGURE 1.
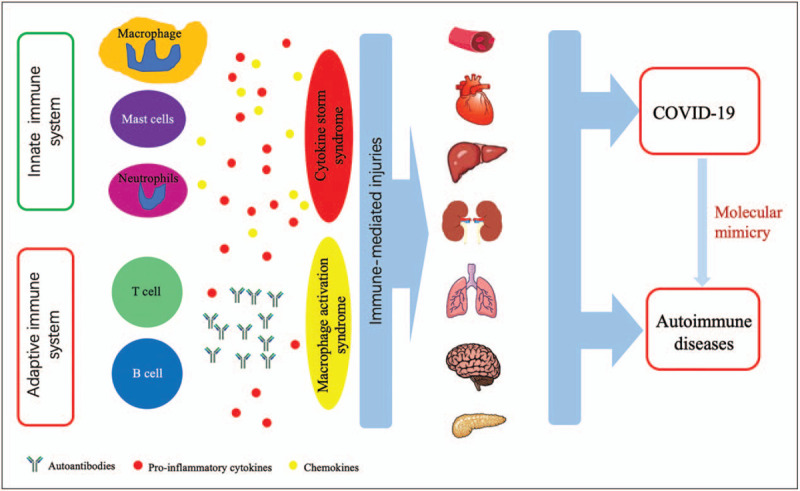
Similar immune reactions in SARS-CoV-2 infection and autoimmune diseases. Both COVID-19 and autoimmune diseases present with various clinical symptoms involving different organs and systems, such as the haematological system, cardiovascular system, digestive system, kidneys, lungs, neurological system and pancreas. Organ damage is caused by uncontrolled immune response characterized by excessive production of cytokines and overactivation of immune cells, and the break of immune tolerance leading to the production of autoantibodies. SARS-CoV-2 infection can trigger cross-reactivity through molecular mimicry, leading to autoimmunity in patients with COVID-19.
In clinical laboratory tests, lymphopenia (lymphocyte count ≤1.0 x 109 /l) is associated with severe illness in COVID-19 patients and might be a prognostic factor for disease severity and mortality [18–21]. Another notable haemocytological change is neutrophilia and associated excessive neutrophil extracellular traps, which paralleled lung injury in severe COVID-19 patients [12]. Therefore, the immune response is a double-edged sword in COVID-19, with outcomes affected by the degree of cytokine imbalance and activation of immune cells. Excessive production and release of pro-inflammatory cytokines and chemokines can cause severe organ damage in critical cases, which is observed in autoimmune diseases as well. In COVID-19 patients, pro-inflammatory cytokines and chemokines, including interleukin (IL)-1, IL-2, IL-6, IL-8, IL-10, IL-17, IL-18, CXCL10 and CCL2, increased significantly and the expression levels of some of these cytokines, such as IL-1, IL-6, IL-10 and IL-18, have been demonstrated to be associated with disease severity [22–25]. Similar to autoimmune diseases, damage-associated molecular patterns (DAMPs) also participate in the pathogenesis of COVID-19 and are related to disease outcome. Chen et al.[26] revealed that serum levels of S100A8/A9 and HMGB1 increased significantly in patients with severe COVID-19 and that significant elevation of the two DAMPs was associated with higher mortality.
Activation and infiltration of immune cells participate in the pathogenesis of organ injury in patients with COVID-19. Macrophage activation syndrome (MAS) could be a continuum of cytokine storm syndrome leading to life-threatening complications in COVID-19 [27]. In this condition, activated macrophages will produce excessive pro-inflammatory cytokines, polarize into the inflammatory M1 phenotype and exhibit cytotoxic dysfunction [28]. Recently, Conti et al.[29] proposed that SARS-CoV-2 activated mast cells could release histamine to increase IL-1 levels to initiate cytokine storm and aggravate lung injury. Woodruff et al.[30] found extrafollicular B cell activation in critically ill patients with COVID-19, similar to what has been observed in autoimmunity. Further, extrafollicular B cell activation correlated strongly with the production of high concentrations of SARS-CoV-2 specific neutralizing antibodies and poor disease outcome [30]. Peripheral blood B-cell subpopulations are altered during COVID-19. In COVID-19 patients, atypical memory B-cells (CD21lo/CD27−/CD10−) expanded significantly, while classical memory B-cells (CD21+/CD27+/CD10−) were significantly reduced [31]. Analysis of immune profiles of severe COVID-19 patients revealed an increased proportion of mature natural killer (NK) cells and decreased proportion of T-cell numbers [32].
Similar to some autoimmune and immune-mediated thromboinflammatory diseases, including lupus, antiphospholipid syndrome and ANCA-associated vasculitis, neutrophil activation and neutrophil extracellular trap production (NETosis) appear to have a pathogenic role in COVID-19. Zuo et al.[33▪] reported increased markers of NETs in sera from patients with COVID-19, and significantly more in patients requiring mechanical ventilation. In-vitro experiments demonstrated that sera from COVID-19 patients triggered NETosis in normal neutrophils, similar to sera from patients with antiphospholipid syndrome [33▪,34].
In severe and critical cases, immunomodulatory drugs and biological agents targeting pro-inflammatory cytokines have been applied to contain the robust immune response in COVID-19. Corticosteroids, JAK inhibitors, IL-1 blockade and IL-6 receptor antagonists, which are familiar to rheumatologists, have been used to treat COVID-19 patients [35–38]. Similarities in immunopathogenesis of COVID-19 and autoimmune diseases are summarized in Table 1.
Table 1.
Similarities in immunopathogenesis of COVID-19 and autoimmune diseases
| Items | COVID-19 immunological features similar to autoimmune diseases | Refs. |
| Innate immune cells | Overactivation of monocytes, macrophages, mast cells and neutrophils. Increased proportion of mature natural killer (NK) cells. | [12,27,29,32,33▪] |
| Adaptive immune cells | Decreased T-cell numbers, altered B-cell subsets, dysregulation of T cells and B cells. | [17,30,31] |
| Cytokines and chemokines | Increased levels of IL-1, IL-2, IL-6, IL-8, IL-10, IL-17, IL-18, CXCL10, CCL2. | [22–24] |
| Autoantibodies | ANA, APL, lupus anticoagulant, cold agglutinins, anti-Ro/SSA antibodies, anti-Caspr2 antibody, anti GD1b antibody, anti-MOG antibody | [14,51▪,52▪,53,54▪,55–58] |
| Clinical conditions | Immune-mediated haemolysis, decreased white blood cell counts, cytokine storm syndrome, macrophage activation syndrome, procoagulant condition | [25,28,57,74] |
| Other immunopathogenesis | Increased levels of DAMPs, molecular mimicry | [26,46] |
MOLECULAR MIMICRY AND SARS-COV-2
The production of autoantibodies is a key feature of autoimmune diseases. However, the underlying mechanisms are complicated and still not fully understood. Molecular mimicry by infectious pathogens is believed to be one of the mechanisms [39]. Viral infection can disturb immunologic tolerance by exposure of antigen epitopes that elicit cross-reactive antibodies. There are a large number of reports indicating antigenic mimicry between viral and human proteins. Perhaps one of the most established examples of molecular mimicry in autoimmunity is the immune response to Epstein–Barr virus (EBV) in lupus patients [40]. An abnormal immune repose to Epstein–Barr virus Nuclear Antigen-1 (EBNA-1) can induce an autoimmune response targeting the Sm and Ro autoantigen systems [41]. Cross-reactivity between anti-EBNA-1 antibodies and myelin basic protein in patients with multiple sclerosis has also been demonstrated [42]. Moreover, EBNA-1 showed structural similarity with β synuclein, a brain protein implicated in multiple sclerosis, and predicted to bind HLA class II DR2b (HLA-DRB1∗15 : 01) [43]. In-silico analysis revealed that an envelope protein of human endogenous retroviruses (HERV) shares similar sequence with three myelin proteins that induced an autoimmune response in multiple sclerosis and was predicted to bind to HLA-DRB1∗15 : 01. Basavalingappa et al.[44] demonstrated that Coxsackievirus B3 (CVB3) infection can induce the generation of autoreactive T cells for multiple antigens.
Some epitopes from SARS-CoV-2 were revealed to exhibit cross-reactivity with autoantigens. Anand et al.[45] reported that a unique S1/S2 cleavage site in SARS-CoV-2 identically mimicked a FURIN-cleavable peptide on the human epithelial sodium channel α-subunit (ENaC-α), which plays a critical role in the homeostasis of airway surface liquid. Mimicry between SARS-CoV-2 and three proteins namely DAB1, AIFM and SURF1 that are present in the human brainstem pre-Bötzinger complex (preBötC) may contribute to the respiratory failure in COVID-19 [46]. In addition, SARS-CoV-2 infection can elicit autoimmune responses through molecular mimicry. Marino Gammazza et al.[47] compared viral proteins with human molecular chaperones and postulated that the chaperones, most of which were heat shock proteins, could participate in molecular mimicry phenomena after SARS-CoV-2 infection. Furthermore, Lucchese and Flöel [48] compared viral amino acid sequence with human autoantigens associated with immune-mediated polyneuropathies and showed that peptides embedded in immunoreactive epitopes of SARS-CoV-2 shared the same sequence with human heat shock proteins 90 and 60 that are associated with Guillain-Barré syndrome and other autoimmune diseases. Venkatakrishnan et al.[49▪] reported 33 distinct 8-mer or 9-mer peptides with potential cross-reactivity between SARS-CoV-2 and the human reference proteome, among which 20 human peptides have not been observed in any previous coronavirus strains. Moreover, four of these human 8-mer/9-mer peptides mimicked by SARS-CoV-2 showed similarity with host pulmonary-arterial peptides and were predicted to bind with HLA-B∗40 : 01, HLA-B∗40 : 02, and HLA-B∗35 : 01 [49▪]. A recent study analysed sharing between hexapeptides that define minimal epitopic sequences of the virus and the human proteome, and documented numerous immunoreactive epitopes shared with human proteins [50]. The results of this study imply the possibility that SARS-CoV-2 might induce cross-reactivity with host autoantigens and offer hints to possibly explain the various clinical manifestations and pathologies involving different organs and systems after SARS-CoV-2 infection.
AUTOANTIBODIES IN PATIENTS WITH COVID-19
Autoantibodies known to occur in a number of autoimmune diseases have been detected in patients with COVID-19 (Table 2). Pascolini et al.[14] determined the presence of antinuclear antibodies (ANA), anticytoplasmic neutrophil antibodies (ANCA) and antiantiphospholipid (APL) antibodies in 33 consecutive patients with COVID-19. The results showed that 45% of the patients were positive for at least one autoantibody and patients with positive autoantibodies tended to have a worse prognosis and a significantly higher respiratory rate at admission. The positive rate for ANA was 33%, the positive rate for anticardiolipin antibodies (IgG and/or IgM) was 24% and three patients tested positive for antiβ2-glycoprotein-I antibodies (IgG and/or IgM) (9%). However, ANCA was negative in all patients [14]. Coagulopathy is a threatening complication of SARS-CoV-2 infection. Recently, a cohort study was performed in Montefiore Medical Center to assess lupus anticoagulant positivity in COVID-19 patients. The researchers found that patients with COVID-19 had an increased incidence of lupus anticoagulant positivity compared with controls who tested negative by COVID-19 reverse transcriptase–PCR. In addition, COVID-19 patients with positive lupus anticoagulant had an increased rate of thrombosis [51▪]. Amezcua-Guerra et al.[52▪] also demonstrated a higher frequency of APL antibodies in patients with severe and critical COVID-19, and that the presence of APL antibodies seems to be associated with a hyperinflammatory state with extremely high levels of ferritin, C reactive protein and IL-6, and with pulmonary thromboembolism. The data discussed above provide a possible explanation for the hypercoagulable state in severe and critical COVID-19 cases and indicate that SARS-CoV-2 can induce autoimmune responses.
Table 2.
Autoantibodies detected in patients with COVID-19
| Autoantibodies | Clinical significance | Refs. |
| ANA | Poor prognosis and a significant higher respiratory rate | [14] |
| APL | Poor prognosis and a significant higher respiratory ratePossible association with a hyperinflammatory state and thrombosis and thromboembolism | [14,52▪] |
| Lupus anticoagulant | A higher rate of thrombosis | [51▪] |
| Cold agglutinins | Haemolytic anaemia.Complicating laboratory assessment and renal replacement therapy | [55,58] |
| Anti-Ro/SSA antibodies | Possible association with severe pneumonia | [56] |
| Anti-Caspr2 antibody | Unclear | [54▪] |
| Anti-GD1b antibody | Unclear | [54▪] |
| Anti-MOG antibody | Unclear | [53] |
| Red cell bound antibodies | Associated with the severity of anaemia | [57] |
In COVID-19 patients presenting with neurological symptoms, the existence of autoantibodies against contactin-associated protein 2 (anti-Caspr2), ganglioside GD1b (anti-GD1b) and myelin oligodendrocyte glycoprotein (anti-MOG) has been shown in case reports or retrospective studies [53,54▪]. However, the clinical significance of these antibodies remains unclear. In addition, there are case reports demonstrating the presence of cold agglutinins and autoantibodies against RBC antigens in critically ill patients with COVID-19 [55], and the presence of anti-Ro/SSA antibodies in patients with aggravated COVID-19 pneumonia [56]. A research including 113 samples studied red cell antibodies by direct and indirect antiglobulin test (DAT or IAT). A positive DAT was found in 46% of COVID-19 patients, which was significantly higher than that in non-COVID-19 controls. The presence of red cell membrane bound immunoglobulins contributes to haemolytic anaemia and is related to the severity of anaemia in COVID-19 [57].
DEVELOPMENT OF AUTOIMMUNE DISEASES AFTER SARS-COV-2 INFECTION
Because SARS-CoV-2 infection can break immune tolerance and trigger autoimmune responses, it is also likely to induce clinical autoimmunity. Indeed, many reports have confirmed the development of autoimmune diseases after SARS-CoV-2 infection. Cold agglutinin syndrome (CAS) and autoimmune haemolytic anaemia have been reported as a complication of COVID-19 [55,58,59]. Meanwhile, Guillain--Barré syndrome (GBS) is also emerging as an autoimmune disease that may occur in COVID-19 patients. In most cases of COVID-19 associated GBS SARS-CoV-2 antibodies cannot be detected in the cerebrospinal fluid (CSF); however, Gigli et al.[60] recently reported a case of GBS with a positive test for the SARS-CoV-2 antibodies in the CSF [61,62]. The mechanisms of how SARS-CoV-2 triggers GBS are debated. However, immune cross reaction between epitopes and host antigens may be a possible explanation [62]. Recently, a case of systemic lupus erythematosus has also been reported to be triggered by SARS-CoV-2 [63▪]. It is possible that additional autoimmune diseases induced by SARS-CoV-2 will be reported in the future.
RISK OF PATIENTS WITH AUTOIMMUNE DISEASES DURING THE COVID-19 PANDEMIC
Autoimmune diseases are heterogeneous and linked to a dysregulated immune system. Most of the patients with autoimmune diseases have received or are receiving immunomodulatory medications or biological agents. During the pandemic of COVID-19, a proportion of the autoimmune disease patients suspended their medication due to fear of the immunosuppressive effect of medications or lack of availabilities [64], and decreased medical visits because of concerns of the contagious nature of SARS-CoV-2 [65]. However, disrupted continuity of medical care and medication nonadherence are associated with rheumatologic disease flares and worsened disease activity [66]. Therefore, building a reliable telemedicine platform and education on medication adherence should be strongly recommended.
Since the beginning of this pandemic, infection risk in patients with autoimmune diseases has been a subject of interest [67▪,68,69]. The results of a cross-sectional study conducted in northeast Italy indicated that autoimmune disease patients had a similar rate of infection of SARS-CoV-2 compared with the general population [70]. Another Italian study performed in Milan also confirmed that autoimmune disease is not a risk factor of being positive for COVID-19 [71]. To the contrary, the results of a multicentre retrospective study conducted in Hubei, China, indicated that patients with autoimmune diseases might be more susceptible to SARS-CoV-2 infection compared with controls. Further, this study examined family members of the patients that resided at the same environment during the outbreak as controls [72]. Of interest, the study from Milan indicated that patients with autoimmune diseases do not have a worse prognosis compared with non-autoimmune disease individuals [71]. However, a Spanish study revealed that hospitalized patients with autoimmune diseases have a more severe course of COVID-19 [73]. At this time, until more data become available, it is crucial to emphasize the importance of physical distancing, wearing masks and frequent hand washing for everyone and especially in our patients with autoimmune diseases. Adherence to medications is also very important to prevent flares of autoimmune diseases that might result in organ damage.
CONCLUSION
COVID-19 is a novel pandemic that has had significant global health consequences. Similar to systemic autoimmune diseases, COVID-19 can present with heterogeneous and systemic clinical manifestations. To some extent, there are similarities in the immune response in both disease conditions, and organ damage in COVID-19 appears to be largely immune-mediated, similar to autoimmune diseases. The SARS-CoV-2 virus can disturb self-tolerance of host antigens at least in part through molecular mimicry. Indeed, the development of autoantibodies and sometimes organ-specific (e.g. GBS) or systemic (e.g. SLE-like disease) autoimmunity has been observed in COVID-19. Overall, more data are needed to further understand the relationship between COVID-19 and autoimmunity and characterize the risk and severity of COVID-19 in patients with preexisting autoimmune diseases.
Acknowledgements
None.
Financial support and sponsorship
This study is supported by grants from the National Natural Science Foundation for Young Scientists of China (Grant No. 81502732) to Y.L., and an urgent grant of Hunan Province for fighting against coronavirus disease- 2019 epidemic (2020SK3005) to Q.L. A.H.S is supported by the National Institutes of Health (NIH) grants number R01AI097134 and R01AR070148, and the Lupus Research Alliance.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Pollard C, Morran M, Nestor-Kalinoski A. The COVID-19 pandemic: a global health crisis. Physiol Genomics 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Domingues R, Lippi A, Setz C, et al. SARS-CoV-2, immunosenescence and inflammaging: partners in the COVID-19 crime. Aging 2020; 12:18778–18789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hopfer H, Herzig M, Gosert R, et al. Hunting coronavirus by transmission electron microscopy: a guide to SARS-CoV-2-associated ultrastructural pathology in COVID-19 tissues. Histopathology 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De P, Bhayye S, Kumar V, Roy K. In silico modeling for quick prediction of inhibitory activity against 3CL enzyme in SARS CoV diseases. J Biomol Struct Dynamics 2020; 1–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yu F, Xiang R, Deng X, et al. Receptor-binding domain-specific human neutralizing monoclonal antibodies against SARS-CoV and SARS-CoV-2. Signal Transduc Target Ther 2020; 5:212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yi C, Sun X, Ye J, et al. Key residues of the receptor binding motif in the spike protein of SARS-CoV-2 that interact with ACE2 and neutralizing antibodies. Cell Mol Immunol 2020; 17:621–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hoffmann M, Kleine-Weber H, Schroeder S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 2020; 181:271–280. e278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bai Y, Xu Y, Wang X, et al. Advances in SARS-CoV-2: a systematic review. Eur Rev Med Pharmacol Sci 2020; 24:9208–9215. [DOI] [PubMed] [Google Scholar]
- 9.Rothan H, Byrareddy S. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun 2020; 109:102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schettino M, Pellegrini L, Picascia D, et al. Clinical characteristics of COVID-19 patients with gastrointestinal symptoms in Northern Italy: a single-center cohort study. Am J Gastroenterol 2020. [DOI] [PubMed] [Google Scholar]
- 11.Qian S, Hong W, Lingjie-Mao, et al. Clinical characteristics and outcomes of severe and critical patients with 2019 novel coronavirus disease (COVID-19) in Wenzhou: a retrospective study. Front Med 2020; 7:552002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang J, Li Q, Yin Y, et al. Excessive neutrophils and neutrophil extracellular traps in COVID-19. Front Immunol 2020; 11:2063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Esmaeilzadeh A, Elahi R. Immunobiology and immunotherapy of COVID-19: a clinically updated overview. J Cell Physiol 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pascolini S, Vannini A, Deleonardi G, et al. COVID-19 and immunological dysregulation: can autoantibodies be useful? Clin Transl Sci 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hejrati A, Rafiei A, Soltanshahi M, et al. Innate immune response in systemic autoimmune diseases: a potential target of therapy. Inflammopharmacology 2020; 28:1421–1438. [DOI] [PubMed] [Google Scholar]
- 16.Singh A, Thakur M, Sharma L, Chandra K. Designing a multiepitope peptide based vaccine against SARS-CoV-2. Sci Rep 2020; 10:16219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rydyznski Moderbacher C, Ramirez S, Dan J, et al. Antigen-specific adaptive immunity to SARS-CoV-2 in acute COVID-19 and associations with age and disease severity. Cell 2020; 183:996–1012.e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lancman G, Mascarenhas J, Bar-Natan M. Severe COVID-19 virus reactivation following treatment for B cell acute lymphoblastic leukemia. J Hematol Oncol 2020; 13:131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Setiati S, Harimurti K, Safitri E, et al. Risk factors and laboratory test results associated with severe illness and mortality in COVID-19 patients: a systematic review. Acta Med Indones 2020; 52:227–245. [PubMed] [Google Scholar]
- 20.Ziadi A, Hachimi A, Admou B, et al. Lymphopenia in critically ill COVID-19 patients: a predictor factor of severity and mortality. Int J Lab Hematol 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ciceri F, Castagna A, Rovere-Querini P, et al. Early predictors of clinical outcomes of COVID-19 outbreak in Milan, Italy. Clin Immunol 2020; 217:108509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Satiş H, Özger H, Aysert Yildiz P, et al. Prognostic value of interleukin-18 and its association with other inflammatory markers and disease severity in COVID-19. Cytokine 2020; 137:155302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vassallo M, Manni S, Pini P, et al. Patients with Covid-19 exhibit different immunological profiles according to their clinical presentation. Int J Infect Dis 2020; 101:174–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Azar M, Shin J, Kang I, Landry M. Diagnosis of SARS-CoV-2 infection in the setting of cytokine release syndrome. Expert Rev Mol Diagn 2020. [DOI] [PubMed] [Google Scholar]
- 25.Sun Y, Dong Y, Wang L, et al. Characteristics and prognostic factors of disease severity in patients with COVID-19: the Beijing experience. J Autoimmun 2020; 112:102473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen L, Long X, Xu Q, et al. Elevated serum levels of S100A8/A9 and HMGB1 at hospital admission are correlated with inferior clinical outcomes in COVID-19 patients. Cell Mol Immunol 2020; 17:992–994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Conti P, Caraffa A, Gallenga C, et al. Coronavirus-19 (SARS-CoV-2) induces acute severe lung inflammation via IL-1 causing cytokine storm in COVID-19: a promising inhibitory strategy. J Biol Regulat Homeost Agents 2020; 34: [DOI] [PubMed] [Google Scholar]
- 28.Wampler Muskardin T. Intravenous Anakinra for macrophage activation syndrome may hold lessons for treatment of cytokine storm in the setting of coronavirus disease 2019. ACR Open Rheumatol 2020; 2:283–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Conti P, Caraffa A, Tetè G, et al. Mast cells activated by SARS-CoV-2 release histamine which increases IL-1 levels causing cytokine storm and inflammatory reaction in COVID-19. J Biol Regul Homeost Agents 2020; 34:1629–1632. [DOI] [PubMed] [Google Scholar]
- 30.Woodruff M, Ramonell R, Nguyen D, et al. Extrafollicular B cell responses correlate with neutralizing antibodies and morbidity in COVID-19. Nat Immunol 2020; 21:1506–1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Oliviero B, Varchetta S, Mele D, et al. Expansion of atypical memory B cells is a prominent feature of COVID-19. Cell Mol Immunol 2020; 17:1101–1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Varchetta S, Mele D, Oliviero B, et al. Unique immunological profile in patients with COVID-19. Cell Mol Immunol 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33▪.Zuo Y, Yalavarthi S, Shi H, et al. Neutrophil extracellular traps in COVID-19. JCI Insight 2020; 5: [DOI] [PMC free article] [PubMed] [Google Scholar]; This study demonstrates a possible role for neutrophils and NETs in the pathogeneis of COVID-19.
- 34.Ali RA, Gandhi AA, Meng H, et al. Adenosine receptor agonism protects against NETosis and thrombosis in antiphospholipid syndrome. Nat Commun 2019; 10:1916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kaminski M, Sunny S, Balabayova K, et al. Tocilizumab therapy of COVID-19: a comparison of subcutaneous and intravenous therapies. Int J Infect Dis 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liu Y, Chang C, Lu Q. Management strategies for patients with autoimmune diseases during the COVID-19 pandemic: a perspective from China. Eur J Rheumatol 2020; 7:S94–S96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Canziani L, Trovati S, Brunetta E, et al. Interleukin-6 receptor blocking with intravenous tocilizumab in COVID-19 severe acute respiratory distress syndrome: a retrospective case-control survival analysis of 128 patients. J Autoimmunity 2020; 114:102511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Iglesias-Julián E, López-Veloso M, de-la-Torre-Ferrera N, et al. High dose subcutaneous Anakinra to treat acute respiratory distress syndrome secondary to cytokine storm syndrome among severely ill COVID-19 patients. J Autoimmun 2020; 115:102537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Reyes-Castillo Z, Valdés-Miramontes E, Llamas-Covarrubias M, Muñoz-Valle J. Troublesome friends within us: the role of gut microbiota on rheumatoid arthritis etiopathogenesis and its clinical and therapeutic relevance. Clin Exp Med 2020. [DOI] [PubMed] [Google Scholar]
- 40.Harley JB, James JA. Everyone comes from somewhere: systemic lupus erythematosus and Epstein-Barr virus induction of host interferon and humoral anti-Epstein-Barr nuclear antigen 1 immunity. Arthritis Rheum 2010; 62:1571–1575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jog NR, Young KA, Munroe ME, et al. Association of Epstein-Barr virus serological reactivation with transitioning to systemic lupus erythematosus in at-risk individuals. Ann Rheum Dis 2019; 78:1235–1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jog NR, McClain MT, Heinlen LD, et al. Epstein Barr virus nuclear antigen 1 (EBNA-1) peptides recognized by adult multiple sclerosis patient sera induce neurologic symptoms in a murine model. J Autoimmun 2020; 106:102332.doi: 10.1016/j.jaut.2019.102332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ramasamy R, Mohammed F, Meier U. HLA DR2b-binding peptides from human endogenous retrovirus envelope, Epstein-Barr virus and brain proteins in the context of molecular mimicry in multiple sclerosis. Immunol Lett 2020; 217:15–24. [DOI] [PubMed] [Google Scholar]
- 44.Basavalingappa R, Arumugam R, Lasrado N, et al. Viral myocarditis involves the generation of autoreactive T cells with multiple antigen specificities that localize in lymphoid and nonlymphoid organs in the mouse model of CVB3 infection. Mol Immunol 2020; 124:218–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Anand P, Puranik A, Aravamudan M, et al. SARS-CoV-2 strategically mimics proteolytic activation of human ENaC. eLife 2020; 9: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lucchese G, Flöel A. Molecular mimicry between SARS-CoV-2 and respiratory pacemaker neurons. Autoimmun Rev 2020; 19:102556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Marino Gammazza A, Légaré S, Lo Bosco G, et al. Human molecular chaperones share with SARS-CoV-2 antigenic epitopes potentially capable of eliciting autoimmunity against endothelial cells: possible role of molecular mimicry in COVID-19. Cell Stress Chaperones 2020; 25:737–741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lucchese G, Flöel A. SARS-CoV-2 and Guillain-Barré syndrome: molecular mimicry with human heat shock proteins as potential pathogenic mechanism. Cell Stress Chaperones 2020; 25:731–735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49▪.Venkatakrishnan A, Kayal N, Anand P, et al. Benchmarking evolutionary tinkering underlying human-viral molecular mimicry shows multiple host pulmonary-arterial peptides mimicked by SARS-CoV-2. Cell Death Discov 2020; 6:96. [DOI] [PMC free article] [PubMed] [Google Scholar]; This is one of several articles suggesting molecular mimickry as a possible mechnism underlying the development of immune-mediated manifestations in COVID-19.
- 50.Kanduc D. From anti-SARS-CoV-2 immune responses to COVID-19 via molecular mimicry. Antibodies (Basel) 2020; 9: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51▪.Reyes Gil M, Barouqa M, Szymanski J, et al. Assessment of lupus anticoagulant positivity in patients with coronavirus disease 2019 (COVID-19). JAMA Netw Open 2020; 3:e2017539. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study and reference [51] below describe the presence of antiphospholipd antibodies in COVID-19 patients, which provides an insight to thrombo-inflammatory features observed in COVID-19.
- 52▪.Amezcua-Guerra L, Rojas-Velasco G, Brianza-Padilla M, et al. Presence of antiphospholipid antibodies in COVID-19: case series study. Ann Rheum Dis 2020. [DOI] [PubMed] [Google Scholar]; This study and reference [50] above describe the presence of antiphospholipd antibodies in COVID-19 patients, which provides an insight to thromboinflammatory features observed in COVID-19.
- 53.Pinto A, Carroll L, Nar V, et al. CNS inflammatory vasculopathy with antimyelin oligodendrocyte glycoprotein antibodies in COVID-19. Neurol Neuroimmunol Neuroinflamm 2020; 7: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54▪.Guilmot A, Maldonado Slootjes S, Sellimi A, et al. Immune-mediated neurological syndromes in SARS-CoV-2-infected patients. J Neurol 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study summarizes immune-mediated neurological complications in 349 patients with COVID-19.
- 55.Jensen C, Wilson S, Thombare A, et al. Cold agglutinin syndrome as a complication of Covid-19 in two cases. Clin Infect Pract 2020; 7:100041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fujii H, Tsuji T, Yuba T, et al. High levels of anti-SSA/Ro antibodies in COVID-19 patients with severe respiratory failure: a case-based review: high levels of anti-SSA/Ro antibodies in COVID-19. Clin Rheumatol 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Berzuini A, Bianco C, Paccapelo C, et al. Red cell-bound antibodies and transfusion requirements in hospitalized patients with COVID-19. Blood 2020; 136:766–768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Maslov D, Simenson V, Jain S, Badari A. COVID-19 and cold agglutinin hemolytic anemia. TH Open 2020; 4:e175–e177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Patil N, Herc E, Girgis M. Cold agglutinin disease and autoimmune hemolytic anemia with pulmonary embolism as a presentation of COVID-19 infection. Hematol Oncol Stem Cell Ther 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gigli G, Vogrig A, Nilo A, et al. HLA and immunological features of SARS-CoV-2-induced Guillain-Barré syndrome. Neurol Sci 2020; 41:3391–3394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Finsterer J, Scorza F, Fiorini A. SARS-CoV-2 associated Guillain-Barre syndrome in 62 patients. Eur J Neurol 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Uncini A, Vallat J, Jacobs B. Guillain-Barré syndrome in SARS-CoV-2 infection: an instant systematic review of the first six months of pandemic. J Neurol Neurosurg Psychiatry 2020; 91:1105–1110. [DOI] [PubMed] [Google Scholar]
- 63▪.Bonometti R, Sacchi M, Stobbione P, et al. The first case of systemic lupus erythematosus (SLE) triggered by COVID-19 infection. Eur Rev Med Pharmacol Sci 2020; 24:9695–9697. [DOI] [PubMed] [Google Scholar]; This case report suggests the development of new-onset lupus as a complication of COVID-19.
- 64.Khabbazi A, Kavandi H, Paribanaem R, et al. Adherence to medication in patients with rheumatic diseases during COVID-19 pandemic. Ann Rheum Dis 2020. [DOI] [PubMed] [Google Scholar]
- 65.Chuah S, Teh C, Wan Mohd Akbar S, et al. Impact of COVID-19 pandemic on hospitalisation of patients with systemic lupus erythematosus (SLE): report from a tertiary hospital during the peak of the pandemic. Ann Rheum Dis 2020. [DOI] [PubMed] [Google Scholar]
- 66.Hassen L, Almaghlouth I, Hassen I, et al. Impact of COVID-19 outbreak on rheumatic patients’ perceptions and behaviors: a cross-sectional study. Int J Rheum Dis 2020; 23:1541–1549. [DOI] [PubMed] [Google Scholar]
- 67▪.Sawalha AH, Zhao M, Coit P, Lu Q. Epigenetic dysregulation of ACE2 and interferon-regulated genes might suggest increased COVID-19 susceptibility and severity in lupus patients. Clin Immunol 2020; 215:108410. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study suggests that epigenetic dysregulation of host genes might be relavent to the pathogenesis of COVID-19.
- 68.Sawalha AH, Manzi S. Coronavirus disease-2019: implication for the care and management of patients with systemic lupus erythematosus. Eur J Rheumatol 2020; 7:S117–S120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sawalha AH. Patients with lupus are not protected from COVID-19. Ann Rheum Dis 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zen M, Fuzzi E, Astorri D, et al. SARS-CoV-2 infection in patients with autoimmune rheumatic diseases in northeast Italy: a cross-sectional study on 916 patients. J Autoimmun 2020; 112:102502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Murtas R, Andreano A, Gervasi F, et al. Association between autoimmune diseases and COVID-19 as assessed in both a test-negative case-control and population case-control design. Auto Immun Highlights 2020; 11:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zhong J, Shen G, Yang H, et al. COVID-19 in patients with rheumatic disease in Hubei province, China: a multicentre retrospective observational study. Lancet Rheumatol 2020; 2:e557–e564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Pablos J, Galindo M, Carmona L, et al. Clinical outcomes of hospitalised patients with COVID-19 and chronic inflammatory and autoimmune rheumatic diseases: a multicentric matched cohort study. Ann Rheum Dis 2020; 79:1544–1549. [DOI] [PubMed] [Google Scholar]
- 74.Voicu S, Delrue M, Chousterman B, et al. Imbalance between procoagulant factors and natural coagulation inhibitors contributes to hypercoagulability in the critically ill COVID-19 patient: clinical implications. Eur Rev Med Pharmacol Sci 2020; 24:9161–9168. [DOI] [PubMed] [Google Scholar]


