To date, the global coronavirus disease 2019 (COVID-19) pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has resulted in more than 90 million people infected and over 2 million deaths. A safe and effective vaccine is in high demand. For an effective vaccine, antibody persistence and long-term memory are favorable features. The poor antibody persistence after natural SARS-CoV-2 infection raised concerns about whether a vaccine could induce a long-lasting antibody response and whether a memory recall response would be induced upon reinfection.1,2 Currently, over 200 vaccine candidates have been documented, some of which have advanced to clinical trials with encouraging results. However, to the best of our knowledge, the extent of antibody persistence and long-term memory post vaccination is still unclear. Here, we report that a ferritin nanoparticle (NP)-based SARS-CoV-2 receptor-binding domain (RBD) vaccine induced an efficient antibody response in mice that lasted for at least 7 months post immunization. A high number of memory B cells (MBCs) were maintained and recalled significantly upon antigen challenge.
The SpyTag/SpyCatcher technique-based click vaccine platform was developed in our laboratory and has been widely used.3–5 The same strategy was applied for the construction of a ferritin NP-based SARS-CoV-2 RBD vaccine (Fig. 1a). Ferritin-NP-RBD was prepared as described in the supplementary information (Supplemental Fig. S1).
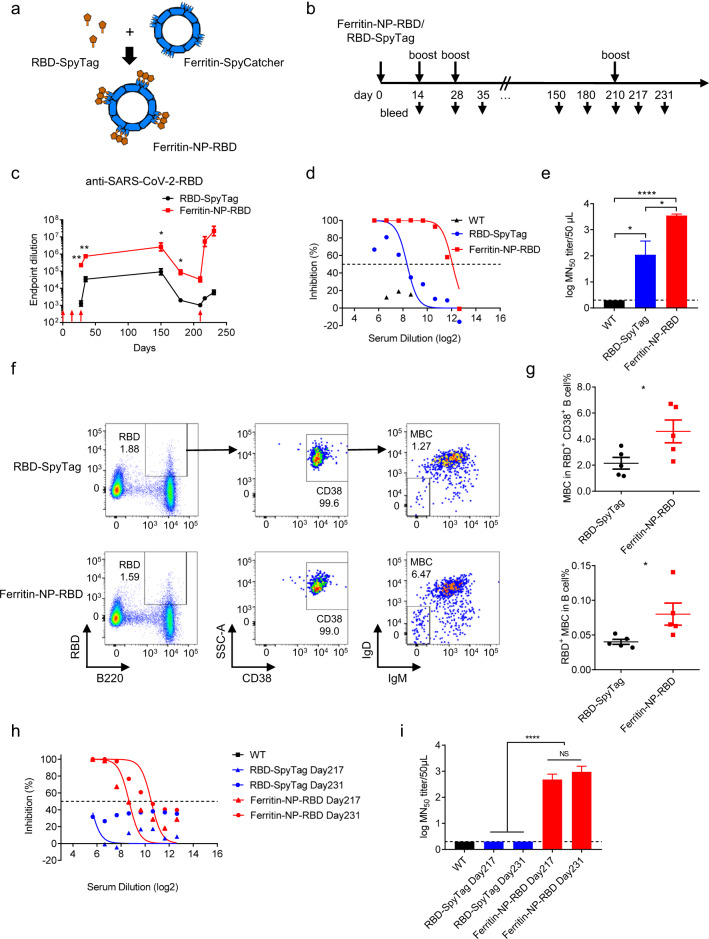
Fig. 1.
The ferritin-NP-RBD vaccine induces a persistent antibody response and long-term memory. a Schematic illustration of ferritin-NP-RBD vaccine construction. b Naive WT C57BL/6 mice (n = 5) were subcutaneously immunized, boosted and bled at the indicated time points. c Anti-RBD responses were monitored and analyzed by ELISA. The red arrows indicate the immunization time points. d, e Live SARS-CoV-2 neutralization assay for sera collected from ferritin-NP-RBD- or RBD-SpyTag-immunized mice on day 35 or WT unimmunized mice. The inhibition (d) and MN50 titer (e) were calculated. f, g At 6 months after the first immunization, memory B cells in the peripheral blood were present (f) and statistically analyzed (g). Numbers adjacent to the outlined areas indicate the percentage of each gate. Data are shown as the mean ± SEM. h, i Live SARS-CoV-2 neutralization assay for sera collected from ferritin-NP-RBD- or RBD-SpyTag-immunized mice on day 217 and day 231 or WT unimmunized mice. The inhibition (h) and MN50 titer (i) were calculated
To assess the immunogenicity of ferritin-NP-RBD, naive wild-type (WT) C57BL/6 mice were immunized with a ferritin-NP-RBD vaccine or equimolar RBD-SpyTag as a control in the presence of CpG-1826 adjuvant at days 0, 14, and 28 (Fig. 1b). The ferritin-NP-RBD vaccine induced an approximately 100-fold higher antibody level than soluble RBD-SpyTag at day 28 (Fig. 1c). After the third immunization, the control vaccine group reached antibody titers of ~105 on day 35, and the ferritin-NP-RBD group reached antibody titers of ~106 (Fig. 1c). Thus, the RBD conjugated to ferritin NPs elicited a dramatically enhanced RBD-specific antibody response.
To test whether the antiserum induced by the ferritin-NP-RBD vaccine could provide protection against live SARS-CoV-2 in vitro, Vero cells were infected with live SARS-CoV-2 (C-Tan-nCoV strain 04) in the presence of day 35 sera from different immunization groups. The results showed that four out of five mice from the RBD-SpyTag group neutralized over 50% of the live virus at serum dilutions ranging from only 1:100 to 1:400, with an average 50% microneutralization (MN50) titer of 103.8/ml (Fig. 1d, e). Strikingly, all five mice from the ferritin-NP-RBD vaccine group had neutralizing effects at serum dilutions ranging from 1:1600 to 1:3200, with an average MN50 of 104.8/ml (Fig. 1d, e). These results confirm that the antiserum to the RBD elicited by the ferritin-NP-RBD vaccine can prevent in vitro SARS-CoV-2 infection much more effectively than antiserum elicited by the RBD-SpyTag vaccine.
To determine the antibody persistence induced by the ferritin-NP-RBD vaccine in mice, we continued to monitor the antibody responses. The anti-RBD level at 5 months was comparable to that at day 35 (Fig. 1c). At 6 and 7 months, while the antibody endpoint titers of both groups gradually dropped, the ferritin-NP-RBD vaccine group still maintained significantly higher anti-RBD levels than the RBD-SpyTag control vaccine group (Fig. 1c), confirming the benefit of ferritin NPs for maintaining the antibody response.
To further determine whether ferritin NPs promote a better memory response, we first examined RBD-specific MBCs in the blood. At 6 months, a significantly higher number of RBD-specific MBCs was maintained in the ferritin-NP-RBD group than in the RBD-SpyTag control group (Fig. 1f, g). Consistent with the enhanced MBC formation and maintenance, when mice were challenged with RBD vaccine antigen at day 210, the ferritin-NP-RBD group elicited a dramatically increased antibody recall response at days 217 and 231 that was more than 2000 times stronger than that in the control group (Fig. 1c). More importantly, the antisera at days 217 and 231 from the ferritin-NP-RBD group demonstrated significant neutralizing activity against live virus, with an average MN50 titer of 104.0/ml for day 217 antisera and 104.3/ml for day 231 antisera, whereas no neutralization was detected in the RBD-SpyTag immunization group (Fig. 1h, i). Thus, the ferritin-NP-RBD vaccine induced not only a persistent RBD-specific antibody response but also long-term protective memory.
Ferritin NPs have recently been used in SARS-CoV-2 vaccine design,6 in which a similar approach was used as we previously reported and applied here.3,4 Upon two immunizations, titers of ~105 RBD-specific anti-IgG were detected. In our study, average titers of 2.2 × 105 in antisera were induced upon two immunizations, and titers of ~106 in antisera were induced upon three immunizations. Given this impressive antibody response, we further monitored antibody persistence and the memory response over 7 months, which is, to the best of our knowledge, the longest reported period for COVID-19 vaccine evaluation. The extended antibody persistence and well-boosted recall antibody response demonstrated in the current study support future success of ferritin-based COVID-19 vaccines.
Currently, multiple platforms are being used for SARS-CoV-2 vaccine development. Although vaccines come in different forms and are administered at different doses, our ferritin-based NP vaccine induced antibody titers (endpoint titer of 106) and live SARS-CoV-2-neutralizing activity roughly equal to those induced by the inactivated vaccine PiCoVacc,7 mRNA-based vaccines8,9 and an RBD-sc-dimer protein subunit vaccine.10 In addition, more importantly, the current ferritin-NP-RBD vaccine induced a persistent antibody response and impressive long-term memory.
Supplementary information
Acknowledgements
This work was supported by grants from the Strategic Priority Research Program of the Chinese Academy of Sciences (XDB29040202 to M.Z.), National Key R&D Program of China (2019YFA0905903 to M.Z.), National Natural Science Foundation of China (81991493 and 32000653 to W.W.) and Beijing Nova Program (Z201100006820032 to W.W.).
Author contributions
W.W. conducted vaccine preparation, immunization, antibody titer measurements, and memory B cell determination; B.H. conducted antiserum neutralization assays; Y.Z. prepared vaccines; W.W., B.H., Y.Z., W.T. and M.Z. designed the experiments, analyzed the data, and wrote the manuscript; W.T. and M.Z. supervised the project; and M.Z. conceived the project.
Competing interests
The authors declare no competing interests.
Footnotes
These authors contributed equally: Wenjun Wang, Baoying Huang
Contributor Information
Wenjie Tan, Email: tanwj28@163.com.
Mingzhao Zhu, Email: zhumz@ibp.ac.cn.
Supplementary information
The online version contains supplementary material available at 10.1038/s41423-021-00643-6.
References
- 1.Ibarrondo FJ, et al. Rapid decay of anti-SARS-CoV-2 antibodies in persons with mild covid-19. N. Engl. J. Med. 2020;383:1085–1087. doi: 10.1056/NEJMc2025179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Edridge AWD, et al. Seasonal coronavirus protective immunity is short-lasting. Nat. Med. 2020;26:1691–1693. doi: 10.1038/s41591-020-1083-1. [DOI] [PubMed] [Google Scholar]
- 3.Wang W, et al. Dual-targeting nanoparticle vaccine elicits a therapeutic antibody response against chronic hepatitis B. Nat. Nanotechnol. 2020;15:406–416. doi: 10.1038/s41565-020-0648-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang W, et al. Ferritin nanoparticle-based SpyTag/SpyCatcher-enabled click vaccine for tumor immunotherapy. Nanomedicine. 2019;16:69–78. doi: 10.1016/j.nano.2018.11.009. [DOI] [PubMed] [Google Scholar]
- 5.Liu Z, et al. A novel method for synthetic vaccine construction based on protein assembly. Sci. Rep. 2014;4:7266. doi: 10.1038/srep07266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ma X, et al. Nanoparticle vaccines based on the receptor binding domain (RBD) and heptad repeat (HR) of SARS-CoV-2 elicit robust protective immune responses. Immunity. 2020;53:1315–1330.e9. doi: 10.1016/j.immuni.2020.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gao Q, et al. Development of an inactivated vaccine candidate for SARS-CoV-2. Science. 2020;369:77–81. doi: 10.1126/science.abc1932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang NN, et al. A thermostable mRNA vaccine against COVID-19. Cell. 2020;182:1271–1283 e1216. doi: 10.1016/j.cell.2020.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Laczko D, et al. A single immunization with nucleoside-modified mRNA vaccines elicits strong cellular and humoral immune responses against SARS-CoV-2 in mice. Immunity. 2020;53:724–732 e727. doi: 10.1016/j.immuni.2020.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dai L, et al. A universal design of betacoronavirus vaccines against COVID-19, MERS, and SARS. Cell. 2020;182:722–733.e711. doi: 10.1016/j.cell.2020.06.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.