Abstract
Background
The U.S. Centers for Disease Control and Prevention (CDC) recognizes that older adults and individuals with certain medical conditions are at increased risk of severe COVID-19 infection. Understanding the proportion of the population at risk of severe infection, including among those with heart disease, could assist current vaccine strategy efforts.
Methods
Using data from the 2015-2018 National Health and Nutrition Examination Survey (NHANES), we estimated the weighted prevalence of any of eight of eleven increased-risk conditions (including age ≥65) in U.S. adults aged ≥18 (N = 10,581) and extrapolated these results to a population of 233.8 million U.S. adults ≥18, and subgroups from the overall population defined by race/ethnicity, education, income and history of heart disease.
Results
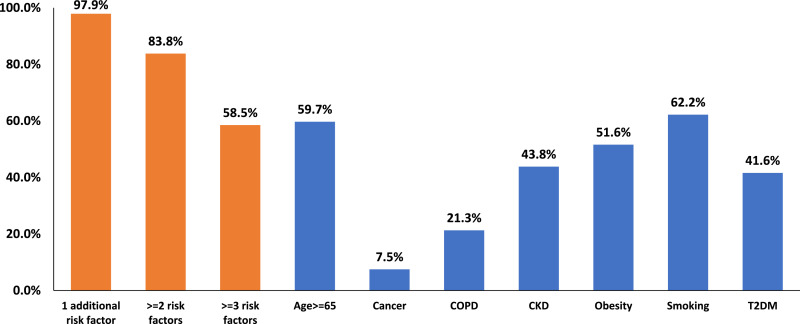
An estimated 176.1 million individuals representing 75.4% of U.S. adults had at least one increased-risk condition, 40.3% ≥2 and, 18.5% ≥3 conditions. Approximately 129 million adults aged <65 (69.2%) were also estimated to be at increased-risk. Compared to Whites, similar proportions of Blacks in the overall population (78.0 vs. 75.6%, p>0.05) and Hispanics in the younger population (70.8 vs 68.4%) were estimated to be at increased-risk. Conversely, a greater proportion of individuals with lower education and income levels were estimated to be at increased-risk both in the overall and younger population. In addition, an estimated 6.2 million individuals (14.5%) had heart disease. Among these, virtually all had at least one additional CDC risk factor (97.9%) and most had ≥2 or ≥3 risk factors (83.8% and 58.5%, respectively).
Conclusions
As vaccination strategies are being explored, these results demonstrate that >75% of adults in the U.S. would be considered at increased-risk for severe COVID-19 infection by CDC criteria. Risk factor prevalence alone may not adequately capture the totality of risk, particularly among Black and Hispanic racial/ethnic groups and those with heart disease.
1. Introduction
Certain chronic medical conditions predispose individuals to severe illness from COVID-19 infection, including hospitalization, need for intensive care, or death [1]. The U.S. Centers for Disease Control and Prevention (CDC) has delineated criteria that indicate an increased risk of severe COVID-19 infection including older age and ten specific medical conditions [2]. Recognizing that initial vaccine supply will be limited, the CDC and the National Institutes of Health have commissioned the National Academies to produce guidance to assist policymakers in determining an optimal strategy for the equitable allocation of a COVID-19 vaccine [3]. An understanding of the proportion of the population at risk of severe COVID-19 infection, based on current CDC guidance, could contribute meaningfully to these efforts.
2. Methods
2.1. Population
A detailed description of the National Health and Nutrition Examination Survey (NHANES) is provided on the NHANES website [4]. Briefly, NHANES is a series of cross-sectional surveys conducted using a stratified probability sampling design to enroll a representative sample of U.S. civilian, non-institutionalized individuals with deliberate oversampling of certain subgroups to provide more precise estimates in these groups. NHANES has been conducted since 1959 with continuous data collection and data release every two years since 1999. The data collected includes a comprehensive demographic and health survey, physical examination and laboratory studies [4]. The present study used data from the 2015–2016 and 2017–2018 NHANES surveys. NHANES de-identified datasets are publicly available from the CDC and the protocols have been reviewed and approved by the National Center for Health Statistics Ethics Review Board. Local institutional review board review is not required for use of NHANES data.
2.2. Demographics
In NHANES, a standardized questionnaire was used to collect information on age, gender, race/ethnicity, family income and educational attainment. For this study, educational attainment was categorized into three groups: less than a high school education, a high school education and more than a high school education. Poverty income ratio (measure of family income to Department of Health and Human Services (HHS) defined poverty level) was selected as the income variable for this study and categorized into two groups: less than 1.5 and equal to or greater than 1.5.
2.3. Variable definitions
The ten medical conditions identified by the CDC include current cancer, chronic obstructive pulmonary disease (COPD), chronic kidney disease (CKD), immunocompromised state from solid organ transplant, obesity (BMI ≥30 kg/m2), serious heart condition such as heart failure, coronary artery disease or cardiomyopathies, sickle cell disease, current or past smoking, pregnancy and type 2 diabetes [2]. Only conditions for which there was stronger evidence per the CDC of increased risk of severe COVID-19 infection were included in this analysis. The current analysis used age ≥65 as an additional risk criteria based on prior CDC criteria which included it as an increased risk condition, and sensitivity analyses were performed removing this risk factor. Pregnancy was not coded in NHANES. Sickle cell and solid organ transplant were also not coded in NHANES but at a prevalence of 0.03% [5] and 0.25% [6], respectively, these represent a very small proportion of the US population.
Serious heart conditions was defined as an affirmative response to “ever told you had coronary heart disease” or “ever told you had heart attack” or ever told you had congestive heart failure”. Cerebrovascular disease was not including in the serious heart conditions definition as cerebrovascular disease was specifically excluded as an increased risk condition by the CDC, and was designated one of the 11 conditions where an individual “might be at increased risk” for severe COVID-19 infection. Current cancer was ascertained based on an affirmative response to the following question “ever told you had cancer or malignancy” and a response to the follow-up question “age cancer diagnosed” that confirmed the diagnosis had been made within two years of the survey. Sensitivity analyses were performed assessing 1 year and 5 years intervals since cancer diagnosis. CKD was defined by urine/albumin creatinine ratio ≥ 30 mg/g or estimated glomerular filtration rate 15–59 mL/min/1.73m2 or ESRD, defined by an affirmative response to the question “ever told you had weak/failing kidneys” and “received dialysis in past 12 months” [7]. COPD was defined by an affirmative response to the question “ever told you had emphysema” or “ever told you had COPD” or “ever told you have chronic bronchitis”. Obesity was defined by a calculated body mass index ≥ 30 kg/m2 that was determined from direct measurement of height and weight by study personnel. Smoking was defined as an affirmative response to “smoked ≥ 100 cigarettes in life”. Type 2 diabetes mellitus was defined by a1c ≥ 6.5% or fasting plasma glucose ≥ 126 mg/dL or an affirmative response to “doctor told you have diabetes” [8].
2.4. Statistical analysis
The NHANES analytic guidelines recommend combining survey cycles to obtain more precise subgroup estimates [9]. We determined the prevalence of the nine risk factors including age ≥65 coded in NHANES in the unweighted 2015–2016 and 2017–2018 overall sample of adults aged ≥18 (N = 10,581) and extrapolated these results to a population of 233.8 million U.S. adults ≥ 18. We then examined the prevalence of these risk factors in subgroups defined by gender, age, race/ethnicity, educational attainment, income and history of heart disease. Using NHANES-supplied sample weights, these prevalence estimates were weighted to obtain nationally representative prevalence estimates. NHANES sample weights take into account the complex NHANES survey design including differential probability of sampling, non-response, and differences between the final sample distribution and target population distribution [9]. Sample weights for the combined 2015–2018 period were obtained by dividing the 2-year weight from the 2015–2016 and 2017–2018 periods by two (the number of two-year cycles) [9]. The weighted prevalence estimates were then used to determine the estimated average population numbers at risk during the 2015–2018 time period per methods provided by the National Center for Health Statistics [9].
We performed sensitivity analyses excluding those aged ≥65, evaluating the proportion with ≥2 or ≥3 risk factors, and excluding obesity and age ≥65 as increased-risk conditions. Comparisons between the proportions with any increased-risk condition among subgroups were performed using a first-order Rao-Scott chi-square test that accommodates the NHANES sampling methodology.
3. Results
An estimated 176.1 million individuals representing 75.4% of U.S. adults had at least one increased-risk condition (Table 1), 40.3% had ≥2 conditions and, 18.5% ≥3 conditions. Excluding age as a risk factor, 72.6% of U.S. adults were estimated to be at increased risk of severe COVID-19 infection (Table 1). Notably, the proportion at risk was considerable amongst those at younger ages (<65), with 69.2% at increased-risk overall, including 58.8% in those 18–29. Obesity was the most prevalent risk condition (41.3%), followed by age ≥65 (20.2%) and CKD (15.8%) (Table 2). Excluding obesity, 61.1% of the overall population and 51.2% <65 remained at increased-risk (Table 1).
Table 1.
Proportion of the U.S. Population at increased risk of severe COVID-19 infection.
| All | Age <65 | ||||||
|---|---|---|---|---|---|---|---|
| Any risk factor†%* ± SE (No. in millions) | Two or more risk factors†,%* ± SE (No. in millions) | Three or more risk factors†,%* ± SE (No. in millions) | Any risk factor excluding obesity‡,%* ± SE (No. in millions) | Any risk factor excluding age ≥65§,%* ± SE (No. in millions) | Any risk factor†%* ± SE (No. in millions) | Risk factors excluding obesity%* ± SE (No. in millions) | |
| All | 75.4 ± 1.1 176.1 |
40.3 ± 1.2 94.2 |
18.5 ± 0.7 43.2 |
61.1 ± 1.0 142.7 |
72.6 ± 1.0 169.6 |
69.2 ± 1.3 129.0 |
51.2 ± 1.2 95.6 |
| Gender | |||||||
| Male | 78.1 ± 1.3 87.6 |
41.9 ± 1.6 47.0 |
19.8 ± 0.9 22.2 |
64.7 ± 1.0 72.5 |
76.6 ± 1.2 86.0 |
73.1 ± 1.5 66.8 |
56.6 ± 1.2 51.7 |
| Female | 72.9 ± 1.2 88.5 |
38.8 ± 1.4 47.2 |
17.2 ± 0.9 20.9 |
57.8 ± 1.4 70.2 |
68.8 ± 1.3 83.6 |
65.3 ± 1.4 62.2 |
46.1 ± 1.6 43.8 |
| Age | |||||||
| 18–29 | 58.8 ± 2.1 25.5 |
16.4 ± 1.5 7.1 |
1.4 ± 0.4 0.6 |
39.4 ± 2.1 17.1 |
58.8 ± 2.1 25.5 |
58.8 ± 2.1 25.5 |
39.4 ± 2.1 17.1 |
| 30–39 | 67.5 ± 1.4 27.9 |
24.7 ± 1.4 10.2 |
4.8 ± 0.6 2.0 |
47.2 ± 1.5 19.5 |
67.5 ± 1.4 27.9 |
67.5 ± 1.4 27.9 |
47.2 ± 1.5 19.5 |
| 40–49 | 78.0 ± 1.5 48.7 |
29.5 ± 1.8 11.6 |
8.0 ± 0.9 3.2 |
50.5 ± 1.9 19.9 |
68.3 ± 2.0 26.9 |
68.3 ± 2.0 26.9 |
50.5 ± 1.9 19.9 |
| 50–64 | 100 28.5 |
39.5 ± 1.9 24.7 |
17.5 ± 1.2 10.9 |
62.6 ± 1.7 39.1 |
78.0 ± 1.5 48.7 |
78.0 ± 1.5 48.7 |
62.6 ± 1.7 39.1 |
| 65–74 | 100 18.6 |
84.3 ± 1.6 24.1 |
54.1 ± 2.5 15.4 |
100 28.5 |
84.3 ± 1.6 24.1 |
– | – |
| ≥75 | 88.8 ± 1.2 16.5 |
59.4 ± 2.2 11.1 |
100 18.6 |
88.8 ± 1.2 16.5 |
– | – | |
| Race/Ethnicity | |||||||
| Hispanic | 71.6 ± 1.3|| 25.9 |
33.5 ± 1.8 12.1 |
12.7 ± 1.0 4.6 |
51.4 ± 1.8 18.6 |
70.3 ± 1.2 25.5 |
68.4 ± 1.2# 22.3 |
46.0 ± 1.7 15.0 |
| White | 78.0 ± 1.3 115.0 |
43.3 ± 1.5 63.8 |
20.5 ± 0.8 30.3 |
65.4 ± 1.3 96.5 |
74.5 ± 1.3 109.9 |
70.8 ± 1.8 78.8 |
54.1 ± 1.7 60.3 |
| Black | 75.6 ± 1.5# 20.1 |
39.7 ± 1.5 10.5 |
18.2 ± 1.1 4.8 |
56.5 ± 1.7 15.0 |
74.2 ± 1.6 19.7 |
71.5 ± 1.6# 16.2 |
49.1 ± 1.8 11.1 |
| Asian | 50.7 ± 1.6 7.0 |
20.7 ± 1.7 2.8 |
9.0 ± 1.2 1.2 |
42.7 ± 1.7 5.9 |
46.8 ± 1.5 6.4 |
42.0 ± 1.4 4.9 |
32.6 ± 1.5 3.8 |
| Other | 84.7 ± 2.6 8.2 |
50.6 ± 3.8 4.9 |
22.8 ± 2.3 2.2 |
70.1 ± 2.8 6.8 |
84.2 ± 2.6 8.2 |
82.1 ± 3.0 6.8 |
65.1 ± 3.4 5.4 |
| Education | |||||||
| <High School | 83.0 ± 1.2 ⁎⁎ 24.9 |
48.5 ± 1.9 14.5 |
26.4 ± 1.6 7.9 |
71.9 ± 1.9 21.5 |
80.6 ± 1.3 24.1 |
77.6 ± 1.5⁎⁎ 17.6 |
62.9 ± 2.2 14.3 |
| High School | 82.8 ± 1.0 46.3 |
46.5 ± 1.6 26.0 |
21.9 ± 1.2 12.2 |
69.2 ± 1.3 38.7 |
80.6 ± 1.0 45.1 |
78.4 ± 1.2 34.8 |
61.2 ± 1.6 27.2 |
| >High School | 71.0 ± 1.2 104.8 |
36.3 ± 1.3 53.6 |
15.5 ± 0.7 23.0 |
55.8 ± 1.1 82.4 |
67.9 ± 1.2 100.3 |
64.1 ± 1.4 76.5 |
45.3 ± 1.2 54.1 |
| Income | |||||||
| <150% FPL | 80.1 ± 1.5 †† 40.9 |
44.2 ± 1.8 22.6 |
21.0 ± 1.2 10.7 |
67.1 ± 1.6 34.3 |
78.7 ± 1.5 40.2 |
76.4 ± 1.6†† 32.9 |
61.0 ± 1.7 26.3 |
| ≥150% FPL | 73.6 ± 1.2 118.1 |
38.5 ± 1.3 61.8 |
17.5 ± 0.7 28.0 |
58.7 ± 1.2 94.1 |
70.3 ± 1.1 112.9 |
66.7 ± 1.4 84.7 |
47.8 ± 1.4 60.6 |
Abbreviations: FPL, federal poverty line.
*Percentages are relative to the total in each row – for example, in the second row of the second column, 60.5% refers to the proportion of the overall population with any risk factor for severe COVID-19 infection.
Risk criteria include current cancer, chronic kidney disease, chronic obstructive pulmonary disease, obesity, serious heart conditions, and type 2 diabetes mellitus (T2DM), as well as age ≥ 65. Current cancer was ascertained based on an affirmative response to the following question “ever told you had cancer or malignancy” and a response to the follow-up question “age cancer diagnosed” that confirmed the diagnosis had been made within two years of the survey.
Individuals of all ages are included in this group, but the obesity risk criteria was omitted.
Individuals of all ages are included in this group, but the age risk criteria (≥65 years) was omitted.
p<0.05 compared to Whites.
p>0.05 comparted to Whites.
p<0.05 compared to > High School.
p<0.05 compared to ≥150% FPL.
The estimated average U.S. adult population at the time of the NHANES survey in 2015–2018 was 233.8 million. The estimated number of individuals within each subgroup of the population during the survey period was as follows: gender – male, 112.2 million, female, 121.6 million; age – 18–29, 43.3 million; 30–39, 41.4 million, 40–49, 39.4 million, 50–64, 62.4 million; 65–74, 28.6 million, ≥ 75, 18.7 million; race/ethnicity – Hispanic, 36.2 million, White, 147.6, Black, 26.5 million, Asian, 13.7 million, Other, 9.7 million; Education – <High school, 30.0 million, High school, 55.9 million, >High school, 147.8 million; Income – <150% poverty 51.2 million, ≥ 150% poverty 160.5 million.
The estimated average U.S. population <65 at the time of the NHANES survey in 2015–2018 was 186.5 million. The estimated number of individuals within each subgroup of this population during the survey period was as follows: gender – male, 91.4 million, female, 95.2 million; age – 18–29, 43.3 million; 30–39, 41.4 million, 40–49, 39.4 million, 50–64, 62.4 million; race/ethnicity – Hispanic, 32.6 million, White, 111.3, Black, 22.7 million, Asian, 11.7 million, Other, 8.3 million; Education – <High school, 22.8 million, High school, 44.4 million, >High school, 119.4 million; Income – <150% FPL, 43.1 million, ≥ 150% FPL, 127.0 million.
Table 2.
Proportion of the U.S. Population with each CDC risk factor for severe COVID-19 infection.
| Age ≥ 65%* ± SE (No. in millions) | Current Cancer,%* ± SE (No. in millions) | COPD,%* ± SE (No. in millions) | CKD,%* ± SE (No. in millions) | Heart Disease,%* ± SE (No. in millions) | Obesity,%* ± SE (No. in millions) | Smoking,%* ± SE (No. in millions) | T2DM,%* ± SE (No. in millions) | |
|---|---|---|---|---|---|---|---|---|
| All | 20.2 ± 0.9 (47.2) |
1.9 ± 0.2† (4.4) |
4.1 ± 0.4 (9.6) |
15.8 ± 0.6 (36.8) |
6.2 ± 0.5 (14.5) |
41.3 ± 1.2 (96.4) |
42.9 (100.2) |
13.8% ±0.6 (32.2) |
| Gender | ||||||||
| Male | 18.6 ± 1.1 (20.8) |
1.9 ± 0.3 (2.1) |
3.9 ± 0.5 (4.4) |
14.4 ± 0.7 (16.1) |
7.7 ± 0.7 (8.7) |
40.5 ± 1.7 (45.4) |
51.6 (57.9) |
15.2 ± 0.8 (17.0) |
| Female | 21.7 ± 0.9 (26.4) |
1.9 ± 0.3 (2.4) |
4.3 ± 0.5 (5.2) |
17.0 ± 0.9 (20.7) |
4.8 ± 0.4 (5.8) |
41.9 ± 1.2 (51.0) |
34.8 (42.3) |
12.5 ± 0.8 (15.2) |
| Age | ||||||||
| 18–29 | – | 0.3 ± 0.2 (0.1) |
0.1 ± 0.1 (0.06) |
6.0 ± 0.9 (2.6) |
0.1 ± 0.1 (0.03) |
34.2 ± 2.3 (14.8) |
33.9 (14.7) |
2.1 ± 0.4 (0.9) |
| 30–39 | – | 0.2 ± 0.1 (0.09) |
0.5 ± 0.2 (0.2) |
7.4 ± 0.8 (3.0) |
1.0 ± 0.3 (0.4) |
42.4 ± 1.5 (17.5) |
41.5 (17.1) |
5.0 ± 0.5 (2.1) |
| 40–49 | – | 0.4 ± 0.2 (0.2) |
1.8 ± 0.4 (0.7) |
8.2 ± 0.8 (3.2) |
1.7 ± 0.3 (0.7) |
43.8 ± 2.1 (17.2) |
41.3 (16.3) |
10.6 ± 1.1 (4.2) |
| 50–64 | – | 2.5 ± 0.5 (1.5) |
7.3 ± 0.8 (4.6) |
15.7 ± 1.1 (9.8) |
7.6 ± 0.9 (4.7) |
44.6 ± 1.8 (27.9) |
46.2 (28.8)) |
19.4 ± 1.1 (12.1) |
| 65–74 | 100 (28.6) |
2.4 ± 0.6 (0.7) |
7.2 ± 1.2 (2.1) |
29.6 ± 1.8 (8.5) |
15.4 ± 1.5 (4.4) |
44.0 ± 2.4 (12.6) |
51.2 (14.6) |
27.2 ± 1.9 (7.8) |
| ≥75 | 100 (18.7) |
9.7 ± 1.2 (1.8) |
10.8 ± 1.0 (2.0) |
51.8 ± 1.8 (9.7) |
22.9 ± 1.6 (4.3) |
34.4 ± 2.0 (6.4) |
46.4 (8.7) |
27.5 ± 1.5 (5.1) |
| Race/Ethnicity | ||||||||
| Hispanic | 10.1 ± 1.0 (3.7) |
0.7 ± 0.2 (0.2) |
1.5 ± 0.2 (0.6) |
12.5 ± 0.7 (4.5) |
3.5 ± 0.5 (1.3) |
45.9 ± 1.3 (16.6) |
34.5 (12.5) |
15.0 ± 1.2 (5.4) |
| White | 24.6 ± 1.1 (36.3) |
2.5 ± 0.3 (3.7) |
5.0 ± 0.6 (7.4) |
16.5 ± 0.8 (24.4) |
7.0 ± 0.6 (10.4) |
40.8 ± 1.5 (60.2) |
46.7 (68.9) |
12.7 ± 0.7 (18.7) |
| Black | 14.5 ± 0.8 (3.9) |
1.1 ± 0.2 (0.3) |
2.9 ± 0.4 (0.8) |
16.9 ± 1.1 (4.5) |
5.9 ± 0.6 (1.6) |
48.2 ± 1.3 (12.8) |
38.6 (10.2) |
16.7 ± 0.8 (4.4) |
| Asian | 15.0 ± 1.6 (2.1) |
0.6 ± 0.2 (0.08) |
0.7 ± 0.2 (0.09) |
13.4 ± 1.3 (1.8) |
3.2 ± 0.6 (0.4) |
15.3 ± 1.0 (2.1) |
20.3 (2.8) |
15.4 ± 1.0 (2.1) |
| Other | 14.4 ± 2.4 (1.4) |
1.6 ± 0.8 (0.2) |
8.4 ± 2.1 (0.8) |
16.5 ± 1.8 (1.6) |
9.2 ± 2.0 (0.9) |
48.7 ± 3.5 (4.7) | 59.5 (5.8) |
15.2 ± 2.0 (1.5) |
| Education | ||||||||
| <High School | 24.2 ± 1.7 (7.2) |
1.7 ± 0.4 (0.5) |
6.8 ± 0.7 (2.0) |
21.2 ± 0.7 (6.4) |
9.2 ± 1.0 (2.8) |
40.5 ± 1.4 (12.2) |
51.0 (15.3) |
20.7 ± 1.3 (6.2) |
| High School | 20.6 ± 1.5 (11.5) |
2.1 ± 0.5 (1.2) |
5.8 ± 0.7 (3.2) |
18.2 ± 1.2 (10.2) |
6.6 ± 0.9 (3.7) |
45.6 ± 1.6 (25.5) |
52.6 (29.4) |
14.5 ± 0.9 (8.1) |
| >High School | 19.2 ± 1.0 (28.4) |
1.8 ± 0.2 (2.7) |
2.9 ± 0.4 (4.3) |
13.7 ± 0.6 (20.2) |
5.5 ± 0.5 (8.1) |
39.8 ± 1.5 (58.8) |
37.6 (55.5) |
12.1 ± 0.7 (17.8) |
| Income | ||||||||
| <150% FPL | 15.7 ± 1.2 (8.0) |
1.7 ± 0.2 (0.8) |
7.6 ± 0.7 (3.9) |
18.4 ± 1.0 (9.4) |
7.5 ± 0.6 (3.9) |
42.9 ± 1.2 (21.9) |
40.4 (64.8) |
15.3 ± 0.7 (7.9) |
| ≥150% FPL | 20.9 ± 1.1 (33.5) |
1.7 ± 0.2 (2.7) |
3.0 ± 0.4 (4.9) |
14.7 ± 0.6 (23.7) |
5.5 ± 0.5 (8.9) |
41.2 ± 1.3 (66.1) |
51.1 (26.1) |
13.1 ± 0.7 (21.0) |
Abbreviations, FPL, federal poverty line.
Risk criteria include current cancer, chronic obstructive pulmonary disease (COPD), chronic kidney disease (CKD), immunocompromised state from solid organ transplant, obesity (BMI >30kg/m2), serious heart conditions, sickle cell disease, current or past smoking, pregnancy, type 2 diabetes, as well as age>=65.
Current cancer was ascertained based on an affirmative response to the following question “ever told you had cancer or malignancy” and a response to the follow-up question “age cancer diagnosed” that confirmed the diagnosis had been made within two years of the survey. Sensitivity analyses were performed assessing 1 year and 5 years intervals since cancer diagnosis. The prevalence of current cancer in the overall cohort was 1.0% ± 0.2 when current cancer was defined using a 1-year window from cancer diagnosis and 4.0% ± 0.3 with a 5-year window from diagnosis.
The estimated average U.S. population at the time of the NHANES survey in 2015–2018 was 233.8 million. The estimated average number of individuals within each subgroup of the population during the survey period was as follows: gender – male, 112.2 million, female, 121.6 million; age – 18–29, 43.3 million; 30–39, 41.4 million, 40–49, 39.4 million, 50–64, 62.4 million; 65–74, 28.6 million, ≥ 75, 18.7 million; race/ethnicity – Hispanic, 36.2 million, White, 147.6, Black, 26.5 million, Asian, 13.7 million, Other, 9.7 million; Education – <High school, 30.0 million.
The proportions at risk were similar among Black and White individuals in the overall population (75.6 vs 78.0%, p>0.05), and in younger adults (71.5 vs. 70.8%, p>0.05) (Table 1). In addition, similar proportions of younger Hispanics and Whites were estimated to be at increased-risk (68.4 vs 70.8%, p>0.05), with proportionally fewer Hispanics in the overall population at increased-risk compared to Whites (71.6 vs 78.0%, p<0.05). Those with lower education levels (<high school vs. >high school, 83.0 vs 71.0%, p<0.05) and lower income levels (<150% vs. ≥150% federal poverty level, 54.7% vs 49.1%, p<0.05) had a greater proportion at increased-risk.
An estimated 6.2 million individuals (14.5% of the population) had heart disease. Among these, almost all had at least one additional CDC risk factor (97.9%) and most had ≥2 or ≥3 risk factors (83.8% and 58.5%, respectively) (Fig. 1). The most common additional risk factor was current or prior smoking (62.2%) followed by age ≥65 years (59.7%).
Fig. 1.
Prevalence of additional risk factors among those with heart disease (n = 6.2 million).
COPD indicates chronic obstructive pulmonary disease; CKD, chronic kidney disease, T2DM, type 2 diabetes mellitus.
4. Discussion
Using NHANES, we demonstrate that more than three-quarters of the U.S. adult population would be considered at increased-risk for severe illness from COVID-19 infection applying CDC criteria, including almost seventy percent of those <65 years of age. Recent studies reported lower COVID-19 at-risk population proportions compared with the current study (28.5–43%) [10], [11], [12]. However, one report did not include obesity [4], and the others used data from the Behavioral Risk Factor Surveillance System (BRFSS) which is known to underestimate obesity prevalence [13,14]. None applied the most recent CDC criteria which includes smoking status. Thus, these prior reports likely underestimate the population at risk [14] and our estimates may be valuable in planning for a priority group for vaccination and other public health interventions.
Numerous studies have described characteristics associated with severe COVID-19 infection [1,[15], [16], [17], [18]]. These studies vary in populations studied, setting, and outcome measures, and despite much consistency in findings, they do observe some differences in finding. The main objective of this study was to specifically evaluate the CDC criteria as they were derived from careful curation and amalgamation across the spectrum of studies, and are the criteria currently being applied to inform vaccine prioritization policies in the U.S [19]. The estimates of the population proportion at risk of severe COVID-19 infection are somewhat sensitive to the components that comprise these criteria. For example, excluding those with obesity the proportion at risk decreased from 75.4% to 61.1%. However, excluding aged ≥65 had minimal impact on these estimates. It appears that varying the number of risk conditions (ie: ≥2 or ≥3 conditions vs. having any 1 condition) has a greater impact on the prevalence of those deemed at increased risk than exclusion of any component condition.
An excess in COVID-19 hospitalizations and mortality amongst Black and Hispanic compared to White populations in the U.S. is well documented [14,20,21,22]. In a national morbidity and mortality report, the greatest excess in deaths for the period Jan 26-October 3, 2020 was reported in Hispanic individuals, amongst whom a 53.6% increase in deaths was recorded. During this period, a 32.9% increase in deaths was recorded amongst Black individuals compared to a 11.9% increase amongst White individuals [23]. The current study did not evaluate actual clinical outcomes. However, the comparable proportions of Blacks and Hispanics deemed to be at increased-risk by having at least one CDC risk condition relative to Whites appear paradoxical to contemporary observations of substantially greater mortality rates from COVID-19 infections in these groups. Our findings suggest that the prevalence of risk factors does not convey the increment in risk conferred by this risk factor burden in a particular group. Further, overall access and patterns of care and other social determinants of health play a considerable role in health status. Of note, although we found that fewer Hispanics would be at increased risk compared to Whites in the overall population, this is likely due to the younger Hispanic population included in this sample.
Individuals with heart disease are known to be a particularly vulnerable group in terms of complications from COVID-19 infection [24,25]. In the NHANES cohort, almost all had at least two additional increased-risk factors whereas in the overall sample, only ~ 20% had this degree of multimorbidity. Thus, the presence of heart disease is an important risk factor for severe COVID-19 infection because it both confers increased risk and is a marker of the presence of multiple risk factors for severe COVID-19 infection. Moreover, given the prevalence of multimorbity in this group, the CDC proposed risk factors for severe COVID-19 infection are likely a poor discriminator of risk in this population.
Several potential limitations of this study should be noted. This study relies on the accuracy and adequacy of representation provided by the sample in the NHANES 2015–2018 surveys for the U.S. population. Second, risk factor definitions might differ from those intended by the CDC. However, the definitions employed here were based on NHANES variable definitions that have been used in prior literature where available. Further, the CDC does not provide specific definitions for the increased risk conditions specified. Third, the effect size of each risk factor was not taken into account in our analysis, so this report does not address degree of risk. This limitation is inherent to all studies of this kind at this time as effect estimates of severe COVID-19 risk factors are widely variable and ultimately unreliable [11,26].
As vaccination strategies are being explored, these data highlight the sizeable proportion of the population considered at risk of severe COVID-19 infection using CDC criteria, including young individuals. The vast majority of those with heart disease also have multiple risk factors, meaning the presence of risk factors will not differentiate risk amongst this group. These results also suggest that medical co-morbidity data alone may fail to capture the totality of COVID-19 related risk in Black and Hispanic racial/ethnic groups, and demonstrate the need for ongoing efforts to refine parameters that capture risk in vulnerable populations.
Funding
No funding was sought for this project.
Author disclosures
The other authors report no conflict of interest relevant to this manuscript.
Author contributions
Conceptualization: EA, AK
Formal Analysis: EA, CRA, AK
Writing – original draft: EA, SR, AMN, AP, CRA, AK
Writing – review and editing: EA, SR, AMN, AP, CRA, AK
References
- 1.Kim L., Garg S., O'Halloran A. Risk factors for intensive care unit admission and in-hospital mortality among hospitalized adults Identified through the U.S. Coronavirus Disease 2019 (COVID-19)-Associated Hospitalization Surveillance Network (COVID-NET) Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.CDC Risk Criteria. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fneed-extra-precautions%2Fgroups-at-higher-risk.html. Accessed 20 July 2020.
- 3.A framework for equitable allocation of vaccine for the novel coronavirus. https://www.nationalacademies.org/our-work/a-framework-for-equitable-allocation-of-vaccine-for-the-novel-coronavirus. Accessed 25 October 2020.
- 4.About the national health and nutrition examination survey. https://www.cdc.gov/nchs/nhanes/about_nhanes.html.
- 5.Data & statistics on sickle cell disease. https://www.cdc.gov/ncbddd/sicklecell/data.html. Accessed 11 May 2020.
- 6.Transplants in the U.S. by recipient age. U.S. transplants performed: 1988 - September 30, 2020.
- 7.Murphy D., McCulloch C.E., Lin F. Trends in prevalence of chronic kidney disease in the United States. Ann Intern Med. 2016 doi: 10.7326/M16-0273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Selvin E., Wang D., Lee A.K., Bergenstal R.M., Coresh J. Identifying trends in undiagnosed diabetes in U.S. Adults by using a confirmatory definition: a cross-sectional study. Ann Intern Med. 2017 doi: 10.7326/M17-1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen T.C., Clark J., Riddles M.K., Mohadjer L.K., Fakhouri T.H.I. National health and nutrition examination survey, 2015−2018: sample design and estimation procedures. Vital Heal Stat Ser 2 Data Eval Methods Res. 2019;2020(184):1–28. [PubMed] [Google Scholar]
- 10.Razzaghi H., Wang Y., Lu H. Estimated county-level prevalence of selected underlying medical conditions associated with increased risk for severe COVID-19 Illness - United States, 2018. MMWR Morb Mortal Wkly Rep. 2020;69(29):945–950. doi: 10.15585/mmwr.mm6929a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clark A., Jit M., Warren-Gash C. Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study. Lancet Glob Heal. 2020 doi: 10.1016/S2214-109X(20)30264-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Selden T.M., Berdahl T.A. Risk of severe COVID-19 among workers and their household members. JAMA Intern Med. 2020 doi: 10.1001/jamainternmed.2020.6249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yun S., Zhu B.P., Black W., Brownson R.C. A comparison of national estimates of obesity prevalence from the behavioral risk factor surveillance system and the national health and nutrition examination survey. Int J Obes. 2006 doi: 10.1038/sj.ijo.0803125. [DOI] [PubMed] [Google Scholar]
- 14.Raifman M.A., Raifman J.R. Disparities in the Population at Risk of Severe Illness From COVID-19 by Race/Ethnicity and Income. Am J Prev Med. 2020;59(1):137–139. doi: 10.1016/j.amepre.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Williamson E.J., Walker A.J., Bhaskaran K. OpenSAFELY: factors associated with COVID-19 death in 17 million patients. Nature. 2020 doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grasselli G., Pesenti A., Cecconi M. Critical care utilization for the COVID-19 Outbreak in Lombardy, Italy. JAMA. 2020 doi: 10.1001/jama.2020.4031. [DOI] [PubMed] [Google Scholar]
- 17.Kabarriti R., Brodin N.P., Maron M.I. Association of race and ethnicity with comorbidities and survival among patients With COVID-19 at an Urban Medical Center in New York. JAMA Netw open. 2020 doi: 10.1001/jamanetworkopen.2020.19795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ioannou G.N., Locke E., Green P. Risk factors for hospitalization, mechanical ventilation, or death among 10 131 US Veterans With SARS-CoV-2 Infection. JAMA Netw Open. 2020 doi: 10.1001/jamanetworkopen.2020.22310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.COVID-19 vaccine information. https://dshs.texas.gov/coronavirus/immunize/vaccine.aspx. Accessed 4 January 2021.
- 20.Karaca-Mandic P., Georgiou A., Sen S. Assessment of COVID-19 Hospitalizations by Race/Ethnicity in 12 States. JAMA Intern Med. 2020 doi: 10.1001/jamainternmed.2020.3857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cowger T.L., Davis B.A., Etkins O.S. Comparison of weighted and unweighted population data to assess inequities in coronavirus disease 2019 Deaths by Race/Ethnicity Reported by the US Centers for Disease Control and Prevention. JAMA Netw Open. 2020;3(7) doi: 10.1001/jamanetworkopen.2020.16933. e2016933-e2016933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gu T., Mack J.A., Salvatore M. Characteristics associated with racial/Ethnic Disparities in COVID-19 outcomes in an academic health care system. JAMA Netw Open. 2020;3(10) doi: 10.1001/jamanetworkopen.2020.25197. e2025197-e2025197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rossen L.M., Branum A.M., Ahmad F.B., Sutton P., Anderson R.N. Excess deaths associated with COVID-19, by age and race and ethnicity - United States, January 26-October 3, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(42):1522–1527. doi: 10.15585/mmwr.mm6942e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shi S., Qin M., Shen B. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5(7):802–810. doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Guo T., Fan Y., Chen M. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5(7):811–818. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Evidence used to update the list of underlying medical conditions that increase a person's risk of severe illness from COVID-19. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/evidence-table.html. Accessed 6 November 2020.