Abstract
Background and Objectives
Many family members struggle to negotiate their aging relative’s care with nursing home staff, potentially leading to depression and other negative outcomes for residents’ families. This pilot study tested an intervention designed to empower residents’ family members to attend and participate in nursing home care plan meetings.
Research Design and Methods
We conducted a small, randomized, controlled trial of the Families Involved in Nursing home Decision-making (FIND) intervention, which used web conferencing to facilitate family participation in care plan meetings.
Results
Overall, FIND was feasible and acceptable. Family members who received the FIND intervention were more likely to experience decreased depressive symptoms than those who did not.
Discussion and Implications
FIND is a promising approach to reducing depression among family members of nursing home residents. Findings support the need for a follow up clinical trial.
Introduction
One and a half million Americans reside in nursing homes and have extensive care needs associated with serious illness or significant impairment in activities of daily living. In the United States, individualized care plans outline the specific supports provided to nursing home residents. Federal regulations require that nursing home staff review residents’ care plans quarterly or upon significant change in a resident’s condition. Regulations further stipulate that nursing homes must (Hertzberg, Ekman, & Axelsson, 2001) allow authorized representatives in all meetings during which the residents plan of care is reviewed (Taunton, Swagerty, Smith, Lasseter, & Lee, 2004).
Particularly for residents with cognitive impairment, family participation in care planning can be valuable (Davies & Nolan, 2006). Family members can provide information about residents’ personal histories, values, and care preferences. They are often able to help the resident access a broad system of support beyond the nursing home including friends and family, and they can provide a sense of continuity for residents, overseeing problem solving and tracking the outcomes of any changes to the plan of care. In addition to improving nursing home residents’ quality of life, participation in care planning may also benefit residents’ family members. Research has identified clear linkages among the quality of family members’ relationships with nursing home staff and the amount of stress and depression family members experience (Chen, Sabir, Zimmerman, Suitor, & Pillemer, 2007). By providing an opportunity to strengthen family members’ working relationships with nursing home staff, family involvement in care planning has the potential to improve family members’ quality of life as well. Despite these benefits, however, many family members are unable to participate in the care plan meetings (CPMs) during which their relative’s care is discussed. Attendance is particularly challenging for family members who live at a distance or whose work or other responsibilities limit their availability. Even when attendance is possible, there tend to be few supports in place to empower family members’ meaningful participation in CPMs (Garcia, Harrison, & Goodwin, 2016).
Our team developed the Families Involved in Nursing home Decision-making (FIND) intervention to facilitate family members’ meaningful participation in nursing home CPMs. The FIND intervention was grounded in a model of interdisciplinary team collaboration that describes four key components of collaboration: organizational context, team structure (including residents and family members), team processes, and outcomes, with feedback loops between all components (Saltz & Schaefer, 1996). Organizational context pertains to the philosophy, purpose, and culture that shape the CPMs. Team structure focuses on the scheduling, attendees, and meeting-dedicated resources. Team process includes how communication and decisions are accomplished. Finally, outcomes are the results of the collaboration. FIND worked within the organizational context and team structure of the nursing home, which supports family and resident involvement in CPMs, and changed the team process with technology that facilitated involvement of family members to improve family outcomes.
We sought to evaluate the intervention’s effectiveness in improving outcomes for residents’ family members by answering the following research question: What was the effect of the FIND intervention on family members’ depression, anxiety, burden, quality of life, and satisfaction with nursing home care?
Methods
A pilot study of the FIND intervention was approved by the University of Missouri Institutional Review Board and registered at clinicaltrials.gov (NCT02929108). We conducted the study in a 132-bed, not-for-profit, licensed nursing home located in the Midwestern United States. The facility had 108 licensed beds for long-term residents and had an average occupancy of 96%. Inclusion criteria required that participating residents were age 65 or older and diagnosed with a serious, life-limiting illness. Participating family members were required to be 18 or older, without cognitive impairment, and with access to an Internet-enabled device to allow for remote participation in CPMs via videoconferencing and electronic completion of outcome measures. Following informed consent and collection of baseline measures, participants were randomized to one of two groups: an usual care or an intervention group. Residents and their family members were randomized together; if more than one family member per resident participated, they were assigned to the same group. Measures were collected at baseline and after each CPM, whether attended by family or not. Participants were in the study until their family member died, changed facilities, or participated in 3 CPMs. The number of CPMs included varied between participants, depending on the amount of time they were enrolled in the study and the number of meetings held due to change in the resident’s condition.
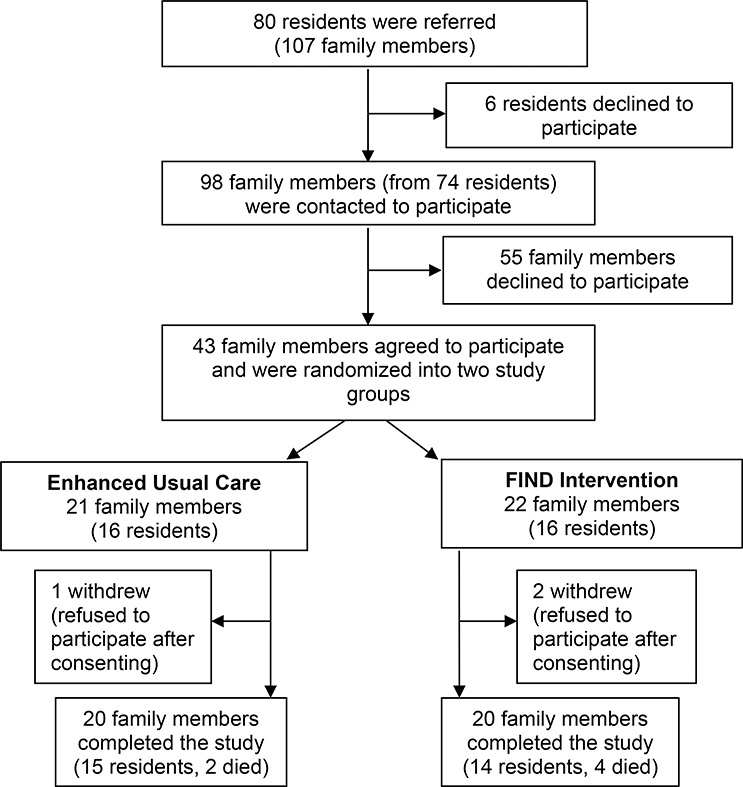
The recruitment process is summarized in Figure 1. We recruited 43 family members of 32 residents, who were randomized either the usual care group (21 family members of 16 residents) or the intervention group (22 family members of 16 residents). Three family members did not provide any baseline data after consenting to join the study and were excluded from analysis, leaving a final sample of 20 family members in each group.
Figure 1.
Flow Chart of Participant Recruitment into the FIND Study
A sample size calculation for this pilot study relied on a two-tailed test of significance and the following assumptions: (1) the difference in the 9-item Patient Health Questionnaire (PHQ-9) means between family members in the usual care and intervention groups would be 5 points, the documented clinically significant effect (McMillan, Gilbody, & Richards, 2010); (2) the variance of PHQ-9 scores would equal 5.33 (Authors, 2017); (3) α =.10 and β = .20 (Meinert, 2012); and (4) 15% attrition. Based on these assumptions, we concluded that 23 family members per group (46 total) would provide 80% power to detect a 5-point difference in PHQ-9 scores. Table 1 includes a description of all outcomes and corresponding measures.
Table 1.
Study Outcomes and Measures
| Outcome | Measure | Description |
|---|---|---|
| Family member depression | 9-item Patient Health Questionnaire (PHQ-9) | Residents’ family members indicate how often they experience common symptoms of depression. Total scores range from 027. Higher scores indicate more intense depressive symptoms (Kroenke, Spitzer, & Williams, 2001). |
| Family member anxiety | 7-item Generalized Anxiety Disorder scale (GAD-7) | Residents’ family members indicate how often they experience common symptoms of anxiety. Total scores range from 0–21. Higher scores indicate more intense anxiety symptoms (Spitzer, Kroenke, Williams, & Lowe, 2006). |
| Family member burden | Zarit Burden Interview-Revised | Residents’ family members indicate the extent to which they endorse statements related to burden. Total scores range from 0 to 88. Higher scores indicate greater caregiving burden (Bachner & O’Rourke, 2007). |
| Family member Quality of Life | Caregiver Quality of Life Index-Revised (CQLI-R) | Residents’ family members rate their quality of life in 4 domains: physical, social, emotional, and financial. Total scores range from 0 to 40. Higher scores indicate greater quality of life (Courtney, Demiris, Parker Oliver, & Porock, 2005). |
| Family member satisfaction with nursing home care | Nursing Facility Family Satisfaction Questionnaire (NF-FSQ) - Modified | Residents’ family members indicate the extent to which they are satisfied with their relative’s nursing home care. Total scores range from 23–230. Higher scores indicate greater satisfaction with care (Castle, 2004). |
Nursing home staff continued to coordinate all meeting logistics, communicating as they were required with family and residents regarding the schedule. During each FIND CPM, research staff managed technology, assisted with communicating and coordinating family member attendance, and video-recorded the meetings. Family members in both study groups completed measures at baseline/study enrollment and after all CPMs, which were typically spaced approximately 90 days apart. We examined descriptive statistics for all residents and family members and outcomes for the full study population and by study group. We used chi-square analyses (or t-tests for continuous variables) to compare study groups.
We separately estimated a mixed model for repeated measures of each study outcome (depression, anxiety, burden, quality of life, and satisfaction with care). Each model included: time, study group, a time x study group interaction term, and potential confounding variables (family member gender and number of days in the study). The main effect of study group was the average effect, the main effect of time was the trend, and the interaction term indicated whether the trends differed between groups. We used SAS version 9.4 (SAS Institute, Cary, NC) with the PROC MIXED procedure for all analyses.
Results
Table 2 provides a summary of participant characteristics. At baseline, there were no statistically significant differences between groups on family member characteristics, patient characteristics, or family member outcome measurements. Between consent and the final data collection point, family members were in the study for an average of 261 days (SD = 83.9).
Table 2.
Family and Resident Characteristics at Baseline
| Study group | |||||||
|---|---|---|---|---|---|---|---|
| Overall | EUC | Intervention | |||||
| Family Member Characteristics | N | % | N | % | N | % | p-value |
| All family members | 40 | 100.0 | 20 | 50.0 | 20 | 50.00 | |
| Age at time of consent, mean (SD) | 56.4 | (8.9) | 57.2 | (9.5) | 55.7 | (8.4) | .31 |
| Race | .31 | ||||||
| White/Caucasian | 39 | 97.50 | 19 | 95.0 | 20 | 100.0 | |
| Other | 1 | 2.50 | 1 | 5.00 | 0 | 0.0 | |
| Gender | .72 | ||||||
| Male | 11 | 27.50 | 5 | 25.0 | 6 | 30.00 | |
| Female | 29 | 72.50 | 15 | 75.0 | 14 | 70.00 | |
| Distance from nursing home | .19 | ||||||
| Less than or equal to 1 hour away | 24 | 60.00 | 14 | 70.0 | 10 | 50.00 | |
| More than 1 hour away | 16 | 40.00 | 6 | 30.0 | 10 | 50.00 | |
| Outcomes measures, mean (SD) | |||||||
| Depression (PHQ-9) | 2.03 | (2.79) | 2.55 | (3.6) | 1.50 | (1.47) | .24 |
| Anxiety (GAD-7) | 2.10 | (3.07) | 2.10 | (2.9) | 2.10 | (3.34) | -- |
| Burden (Zarit) | 3.08 | (3.08) | 3.70 | (3.6) | 2.45 | (2.37) | .20 |
| Quality of life (CQLI-R) | 32.35 | (6.25) | 30.9 | (7.0) | 33.7 | (5.14) | .15 |
| Care satisfaction (NF-FSQ) | 75.33 | (8.92) | 72.8 | (9.3) | 77.8 | (8.00) | .07 |
| Resident Characteristics | |||||||
| All residents | 29 | 100.0 | 15 | 51.7 | 14 | 48.3 | |
| Gender | .56 | ||||||
| Male | 5 | 17.24 | 2 | 13.3 | 3 | 21.43 | |
| Female | 24 | 82.76 | 13 | 86.6 | 11 | 78.57 | |
| Race (White/Caucasian) | 29 | 100.0 | 15 | 100 | 14 | 100.0 | |
| Comorbidities | |||||||
| Dementia | 14 | 48.28 | 5 | 33.3 | 9 | 64.29 | .10 |
| Depression | 12 | 41.38 | 6 | 40.0 | 6 | 42.86 | .87 |
| Heart Failure | 3 | 10.34 | 3 | 20.0 | 0 | 0.00 | .08 |
| Hypertension | 18 | 62.07 | 11 | 73.3 | 7 | 50.00 | .19 |
| Anemia | 3 | 10.34 | 2 | 13.3 | 1 | 7.14 | .58 |
| Stroke | 8 | 27.59 | 5 | 33.3 | 3 | 21.43 | .47 |
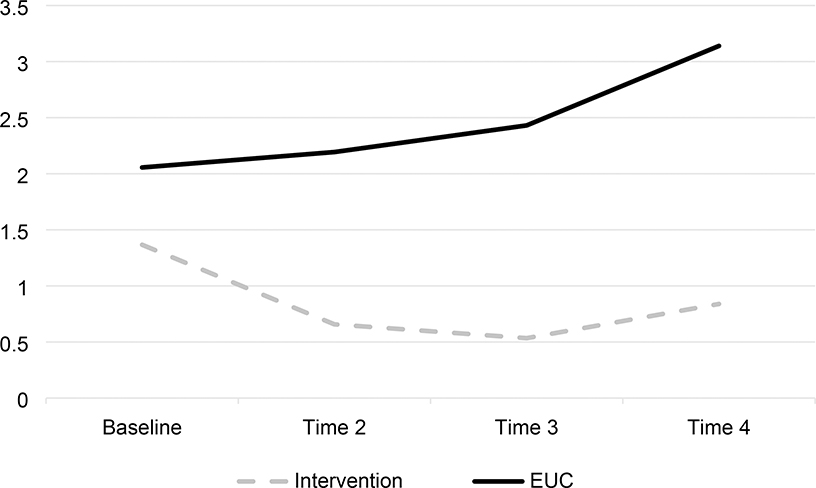
Upon reaching the primary study endpoint, family members in the intervention group were more likely to experience decreased depressive symptoms (p = .03) than those in the usual care group (Table 3). Depression increased in the usual care group in the same time period (Figure 2). Of the covariates in the model, only female gender was associated with depression (Table 3). Study outcomes other than depression were not associated with group membership, time, or time x group membership, and are therefore not presented. They were however, all in the desired direction.
Table 3.
Mixed Model Results for PHQ-9 (Depression) Total Score (N=40)
| 95% CI | |||||
|---|---|---|---|---|---|
| Estimate | SE | low | high | p-value | |
| Intercept | 4.245 | 1.588 | 1.00 | 7.48 | .01 |
| Family member is female | 1.844 | 0.816 | 0.18 | 3.50 | .03 |
| Days in the study | −0.010 | 0.004 | −0.01 | −0.0004 | .04 |
| Time (ref = baseline) | |||||
| After 1st CPM vs. baseline | 0.076 | 0.514 | −0.97 | 1.12 | .88 |
| After 2nd CPM vs. baseline | 0.338 | 0.469 | −0.61 | 1.29 | .47 |
| After 3rd CPM vs. baseline | 1.059 | 0.478 | 0.08 | 2.03 | .03 |
| Study group | |||||
| Intervention vs. UC | −1.461 | 0.970 | −3.44 | 0.51 | .14 |
| Group * time (ref = Intervention vs. UC at baseline) | |||||
| Intervention vs. UC Time 2 | −0.835 | 0.699 | −2.26 | 0.59 | .24 |
| Intervention vs. UC Time 3 | −1.199 | 0.647 | −2.51 | 0.12 | .07 |
| Intervention vs. UC Time 4 | −1.596 | 0.685 | −2.99 | −0.19 | .02 |
Figure 2.
Adjusted PHQ-9 Depression Total Scores
Discussion
Involving family members in CPMs had a beneficial effect on depression scores of family members. As well, the FIND intervention was feasible in the long-term care setting. We sought to identify the outcomes of involving family members in nursing home CPMs. The intervention was based on the premise that depression was a concern for family members of nursing home residents and was thought to be mediated through positive relationships with nursing home staff (Chen et al., 2007). The baseline levels of depression and anxiety were low and while the change in depression was statistically significant it was not clinically significant. It is possible that the change in the scores reflect fatigue or some other sleep disturbance, this should be investigated in a follow up trial.
Family participation in care plans had also been found beneficial, improving the relationship between family and staff (Davies & Nolan, 2006). Similarly, family involvement in care has been shown to improve the family caregiving experience (Jablonski, Reed, & Maas, 2005; Maas et al., 2004; Zimmerman et al., 2013). Similarly, FIND found promising improvements for the family caregiver depression. While only a small pilot study, the results of FIND support these premises, demonstrate its feasibility in the long-term care setting, and identify important issues for future testing on a larger scale.
During the COVID-19 pandemic the importance of these findings has been amplified. Long term care residents and staff have been victims to COVID 19 not only in the illness and death experienced directly by the disease, but also as a result of policies limiting of visitation, isolating residents from their family. Extensive media coverage has shown the toll that restricted visitation has had on the mental well-being of both residents and family members. FIND would allow family members access to their resident’s care team whenever nursing homes are quarantined and otherwise closed to the community, including not only COVID-19 but also during outbreaks such as the annual flu season.
The use of video to train staff and family was helpful and well received. Participating facility staff viewed a video focusing on ways in which they might use shared decision making in CPMs, illustrated with specific examples from long term care. For example, staff were encouraged to ask family members to discuss resident values regarding decisions related to goals of care. Additionally, all intervention family participants were given a YouTube link to view a five-minute orientation video with the research staff. It demonstrated ways in which family input and communication were valuable to a decision-making process. Future testing should include observations of the changes in facility staff behaviors resulting from the video training and experiences with family participation.
One of the most important lessons learned is the need for randomization at the nursing home level rather than the individual level to prevent contamination. Despite having previously been invited via routine nursing home processes to attend CPMs, participation in the study resulted in increased CPM attendance among family members randomized to the usual care group, likely contaminating study results and reducing our ability to detect change. Randomization at the facility level rather than the resident/family level would avoid this problem in the future. Additionally, the attention to the family from the interventionists may have influenced results, thus future trials should consider the use of an attention control group.
Finally, while it was not the intent of this pilot study to assess the outcomes of the intervention on residents, future research assessing both resident and family outcomes would provide a more complete picture of FIND’s clinical utility. While the results are supported by the published literature, few studies have focused on family outcomes related specifically to decision making. It is therefore suggested that the lessons from this pilot study inform a future large scale multi-site randomized clinical trial testing the efficacy of FIND.
Clinical Implications.
FIND holds promise as a strategy to reduce depression among family members of seriously ill nursing home residents, including those isolated by public health crisis impacting visitation policies and isolating residents from family.
Randomization at the facility level, as might occur in a cluster randomized trial, should be considered for future testing in multiple sites serving a diverse resident and family population.
Funding:
Research reported in this publication was supported by the National Institute on Aging under award number R21AG049999 (PI Parker Oliver). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Ethics Statement: University of Missouri Institutional Review Board has approved this study #2003012. The study is registered with clinicaltrials.gov NCT02917603
Conflict of Interest: All authors report no conflict of interest
Contributor Information
Debra Parker Oliver, Department of Family and Community Medicine, University of Missouri, Medical Annex 306, Columbia, Mo 65212, 573-356-6719.
Abigail J. Rolbiecki, Department of Family and Community Medicine, University of Missouri, Medical Annex 306, Columbia, Mo 65212.
Karla Washington, Department of Family and Community Medicine, University of Missouri, Medical Annex 306, Columbia, Mo 65212.
Robin L. Kruse, Department of Family and Community Medicine, University of Missouri, Medical Annex 306, Columbia, Mo 65212.
Lori Popejoy, Sinclair School of Nursing, University of Missouri, Columbia, Mo 65212.
Jamie B. Smith, Department of Family and Community Medicine, University of Missouri, Medical Annex 306, Columbia, Mo 65212.
George Demiris, Department of Biobehavioral Health Sciences, School of Nursing, University of Pennsylvania, 418 Curie Blvd, Room 324, Philadelphia PA 19104.
References
- Chen CK, Sabir M, Zimmerman S, Suitor J, & Pillemer K (2007). The importance of family relationships with nursing facility staff for family caregiver burden and depression. J Gerontol B Psychol Sci Soc Sci, 62(5), P253–260. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/17906166 [DOI] [PubMed] [Google Scholar]
- Davies S, & Nolan M (2006). ‘Making it better’: self-perceived roles of family caregivers of older people living in care homes: a qualitative study. Int J Nurs Stud, 43(3), 281–291. doi: 10.1016/j.ijnurstu.2005.04.009 [DOI] [PubMed] [Google Scholar]
- Garcia TJ, Harrison TC, & Goodwin JS (2016). Nursing Home Stakeholder Views of Resident Involvement in Medical Care Decisions. Qual Health Res, 26(5), 712–728. doi: 10.1177/1049732315573206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hertzberg A, Ekman SL, & Axelsson K (2001). Staff activities and behaviour are the source of many feelings: relatives’ interactions and relationships with staff in nursing homes. J Clin Nurs, 10(3), 380–388. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/11820548 [DOI] [PubMed] [Google Scholar]
- Jablonski RA, Reed D, & Maas ML (2005). Care intervention for older adults with Alzheimer’s disease and related dementias: effect of family involvement on cognitive and functional outcomes in nursing homes. J Gerontol Nurs, 31(6), 38–48. doi: 10.3928/0098-9134-20050601-10 [DOI] [PubMed] [Google Scholar]
- Maas ML, Reed D, Park M, Specht JP, Schutte D, Kelley LS, . . . Buckwalte KC (2004). Outcomes of family involvement in care intervention for caregivers of individuals with dementia. Nurs Res, 53(2), 76–86. doi: 10.1097/00006199-200403000-00003 [DOI] [PubMed] [Google Scholar]
- McMillan D, Gilbody S, & Richards D (2010). Defining successful treatment outcome in depression using the PHQ-9: A comparison of methods. Journal of Affective Disorders, 127(1–3), 122–129. doi: 10.1016/j.jad.2010.04.030 [DOI] [PubMed] [Google Scholar]
- Meinert C (2012). Clinical trials: Design, conduct and analysis (2nd ed.): Oxford University Press. [Google Scholar]
- Saltz CC, & Schaefer T (1996). Interdisciplinary teams in health care: integration of family caregivers. Soc Work Health Care, 22(3), 59–70. doi: 10.1300/J010v22n03_04 [DOI] [PubMed] [Google Scholar]
- Taunton RL, Swagerty DL, Smith B, Lasseter JA, & Lee RH (2004). Care Planning: for Nursing Home Residents: Incorporating the Minimum Data Set Requirements Into Practice. Journal of Gerontological Nursing, 30(12), 40–49. [DOI] [PubMed] [Google Scholar]
- Zimmerman S, Cohen LW, Reed D, Gwyther LP, Washington T, Cagle JG, . . . Preisser JS (2013). Families Matter in Long-Term Care: Results of a Group-Randomized Trial. Seniors Hous Care J, 21(1), 3–20. [PMC free article] [PubMed] [Google Scholar]