Abstract
Background and Objectives:
There is no consensus on an ideal abdominal entry in laparoscopic surgery; as such, we aimed to assess the feasibility of the fingertip technique for safe entry and the establishment of pneumoperitoneum in transperitoneal laparoscopic surgery.
Methods:
We prospectively assessed 96 consecutive patients who underwent laparoscopic transperitoneal surgery between December 2018 and September 2019. For all patients, pneumoperitoneum was performed using the fingertip technique, which we recently defined. The duration of time for initial entry, the occurrence of gas leakage, and the complications were evaluated.
Results:
The median duration of initial entry was 90 (75 – 145) seconds. Pneumoperitoneum was established on the first attempt in all patients. Some events were encountered at the time of implementation of the fingertip technique, such as subcutaneous minor bleeding (5.2%) and gas leakage (4.1%). These events were controlled with cauterization and suturing. There was no visceral or major vascular injury in any patient case.
Conclusions:
The fingertip technique is a fast, safe, and feasible method for establishing pneumoperitoneum in transperitoneal laparoscopic surgery.
Keywords: Laparoscopy, Novel technique, Abdominal entry, Fingertip technique, Hasson
INTRODUCTION
Establishing pneumoperitoneum and initial trocar entry are important steps in laparoscopic surgery. Approximately 50% of the complications that occur during laparoscopic surgery are related to access maneuvers and insufflation into the peritoneal cavity.1,2 This fact has not altered in recent years, despite various techniques having been described to provide safe and easy abdominal access. In addition, no significant superiority of one technique over the other, based on the safety of the techniques, has yet been proven.1 Although major complications (i.e., intestinal injury and vascular injury) that may cause death are rarely seen,3,4 minor complications (i.e., failure to obtain entry, gas leakage around the trocar, and subcutaneous bleeding) are seen more frequently. These complications require longer procedure times and affect surgeons focusing on the operation perioperatively.
The Veress needle technique is the most commonly used closed-entry method. However, the disadvantage of this method is the higher number of needle insertion attempts needed to obtain pneumoperitoneum, due to failure to gain access, in comparison to other methods; this is particularly problematic at the beginning of the learning curve.5 In contrast, the Hasson technique, and its modifications, is a widely used open-entry technique. Although this method is probably safer than the Veress technique, it has some limitations, such as the need for assistance, the occurrence of gas leakage, the risk of subcutaneous bleeding, and the prolonged procedure time.6,7
Since introducing the fingertip technique in 2018, we have routinely used it for the establishment of pneumoperitoneum and initial port placement in our laparoscopic practice.8 We have clinically observed that the technique allows for easy and fast port placement with a lower complication rate than that observed when using other methods. Herein, we aimed to report our preliminary results related to the use of the fingertip technique for laparoscopic procedures in the field of urology.
MATERIALS AND METHODS
Ninety-six consecutive patients who underwent laparoscopic transperitoneal surgery for their routine medical care between October 2018 and January 2020 are included in the study. The patients’ data were collected prospectively and analyzed retrospectively. The study protocol was approved by the local ethics committee (ID: 2018/09). All steps of the study were planned and applied carefully, according to the Declaration of Helsinki. All surgeries were done by a single surgeon (AS) to eliminate confounding factors.
Initial Entry Site
The 60 degree right or left lateral decubitus positions or the supine position were used based on the planned surgery. The initial port placement was decided on in the reference to the mid-clavicular line in upper urinary system surgeries. We planned to place an upper working channel into the interior of the costal margin. Initially, a 10 mm camera port was placed 4 to 5 finger-widths inferior to the medial side of the upper working channel. In pelvic surgeries, we placed initial access 2 cm superior to the umbilicus.
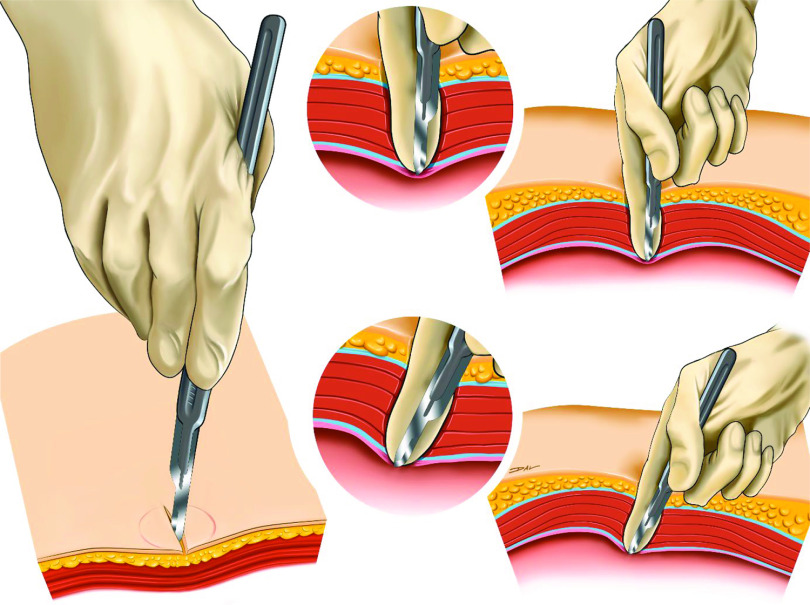
Fingertip Technique
We described the fingertip technique in an abstract previously.8 Briefly, in the fingertip technique, the skin is marked with a 10 mm empty disposable trocar tip to prevent excessive incision. The skin is vertically incised at the boundaries of the marked area until the subcutaneous adipose tissue can be seen. Then, blunt dissection is done with the index finger down until the upper sheet of the abdominal fascia is felt. A 15 mm scalpel is placed on the inside of the index finger and held with the proximal part of the thumb. The tip of the scalpel should not exceed the tip of the finger. After that, the finger and the scalpel are held perpendicular to the fascia while applying mild pressure on the fascia. The finger and scalpel are bent 30 degrees medially, without moving the tip of the finger or the scalpel. Due to the softness of the fingertip, the scalpel passes the fingertip by only a few millimeters and incises the fascia. Only mild pressure on the layer during the maneuver is needed to achieve a 3 to 4 mm incision. Then, the abdominal muscle is dissected bluntly with the index finger. Finally, the peritoneal layer is incised again using the fingertip technique and enlarged bluntly with the index finger to enter the abdomen. Then, the abdominal wall is elevated bilaterally next to the incision, and a 10 mm trocar is inserted bluntly through the incision (Figures 1 and 2).8,9 Since the port size is at least 10 mm at the entry site of the fingertip technique, the port defect is closed at the end of the operation either by traditional methods or by a trocar closure device.
Figure 1.
Illustration of Fingertip Technique.
Figure 2.
Camera View of Entry with the Fingertip Technique in a Patient with Pneumoperitoneum. a) Image of the Tip of the Scalpel During Peritoneal Incision, b) Millimetric Peritoneal Incision, c) Insertion of the Fingertip into the Peritoneal Cavity, d) Initial Entry After Trocar Insertion Intraperitoneally, e) Skin is Firmly Covering the Cannula.
We prospectively collected the patients' demographics such as gender, age, body mass index (BMI), presence of previous abdominal surgery, and perioperative outcomes such as the type of surgery, the time required for initial entry, the occurrence of gas leakage, and complications (i.e., major and minor vascular injury, intestinal injury, solid organ injury).
The duration of entry in seconds was recorded under the surgeon's control. The operating room staff switch on the chronometer when the surgeon started the abdominal entry and switch off the chronometer when the surgeon entered into the peritoneal cavity and saw the intra-abdominal organs successfully. Gas leakage was defined as significant leakage for which intervention such as suturing was needed essential.
RESULTS
A total of 96 patients who underwent various laparoscopic transperitoneal surgeries between December 2018 and September 2019 were included in this study. The median age of the patients was 52 years (minimum 21 years, maximum 76 years). The mean BMI of the patients was 25.5 (19 – 36) kg/m2. Seven patients had undergone previous open abdominal surgery, and two had undergone previous laparoscopic abdominal surgery.
The patients were placed in a lateral decubitus position (85.1%) for laparoscopic upper-system surgery, whereas the supine position (14.9%) was chosen for pelvic surgeries. Pneumoperitoneum was successfully achieved in all patients. There were no major vascular complications or abdominal organ injuries related to the initial abdominal entry. The median procedural time was 90 (75 – 145) seconds. Gas leakage was observed in four patients, which required additional intervention such as suturing or bringing the incision sides closer with a towel clamp, while subcutaneous bleeding occurred in five patients, requiring only required cauterization. However, no further complications including solid organ and vascular injury were observed. No injury to the surgeon was noted during the application of the fingertip technique.
Overall, the percentage of normal weight, overweight, and obese patients was 44.8%, 43.8%, and 11.5%, respectively. The median time required for initial entry was longer in patients with gas leakage and subcutaneous bleeding (p = 0.002 and p = 0.001, respectively). We could not show a correlation with the complication rates in terms of the BMI groups and/or the history of previous abdominal surgery (p > 0.05; Table 2).
Table 2.
Comparison of Minor Events and Patient Characteristics
|
Gas Leakage |
|||
|---|---|---|---|
| Absent (n = 92) | Present (n = 4) | p-value | |
| BMI; median (min-max) kg/m2 | 25.5 (19.0 – 35.0) | 29.5 (21.0 – 36.0) | 0.392 |
| History of abdominal surgery; n (%) | 3 (3.2%) | 1 (25%) | 0.330 |
| Median time required for initial entry; (min-max), seconds | 90 (70 – 150) | 125 (110 – 160) | 0.002 |
| Subcuteneous bleeding | 2 (2.1%) | 3 (75%) | 0.013 |
|
Subcutaneous Bleeding |
|||
|---|---|---|---|
| Absent (n = 91) | Present (n = 5) | p-value | |
| BMI; median (min-max) kg/m2 | 25.0 (19.0 – 35.0) | 30.0 (21.0 – 36.0) | 0.129 |
| History of abdominal surgery; n (%) | 4 (4.4%) | 1 (20%) | 0.395 |
| Median time required for initial entry; (min-max), seconds | 90 (70 – 120) | 145 (130 –160) | 0.001 |
Min, minimum; max, maximum; BMI, body mass index.
Table 1.
Patient Demographics and Perioperative Procedural Outcomes
| Age; median (min – max), years | 52.0 (21.0 – 76.0) |
| Gender; M/F | 65/31 |
| BMI (kg/m2) | 25.5 (19.0 – 36.0) |
| Presence of previous abdominal surgery; n (%) | 9 (9.4%) |
| The time required for initial entry with the camera; median (min –max), seconds | 90 (75 – 145) |
| Gas leakage; n (%) | 4 (4.2%) |
| Subcutaneous bleeding; n (%) | 5 (5.2%) |
| Major vascular complication; n (%) | None |
| Solid-organ complications; n (%) | None |
| Type of surgery performed | |
| Radical nephrectomy; n (%) | 21 (21.8%) |
| Partial nephrectomy; n (%) | 24 (25.0%) |
| Simple nephrectomy; n (%) | 26 (27.0%) |
| Pyeloplasty; n (%) | 6 (6.2%) |
| Pyelolithotomy-Ureterolithotomy; n (%) | 5 (5.2%) |
| Radical prostatectomy; n (%) | 11 (11.4%) |
| Radical cystectomy; n (%) | 3 (3.1%) |
Min, minimum; max, maximum.
DISCUSSION
Establishing pneumoperitoneum is an important step in laparoscopic surgery due to the risk of iatrogenic injury to major vascular structures (i.e., vena cava and iliac vessels) and abdominal organs during abdominal entry (i.e., intestine, liver, spleen, and omentum).3, 4 Over 50% of major vasculature (0.2/1000) and intestinal (0.4/1000) injuries occur upon initial abdominal entry.1,2 A total of 80% of the complications that occur are directly associated with inserting the initial Veress needle and trocar or cannula.1,2 Ahmad et al. studied the benefits and risks of different laparoscopic entry techniques in a review that included 57 well-designed randomized controlled trials and 25 abdominal entry methods.10 Although some studies favored open abdominal entry (i.e., the Hasson technique), most showed no significant differences between many of the techniques.10,11 The main difference observed was that open-entry techniques resulted in fewer failed entry attempts than did closed-entry methods.10 In the present study, there were no failed entries using the fingertip technique.
Various types of equipment—such as a Veress needle; visual bladeless cannula; reusable, threaded, disposable optical trocar; and micro-optical system—have been produced to facilitate initial entry in a safe way.11–15 However, the main aim of the fingertip technique is to facilitate fast and easy initial abdominal entry with a small incision and to reduce the track-related complications (e.g., gas leakage, major vascular and abdominal organ injury). In addition, in the fingertip technique, pneumoperitoneum can be achieved with only a 15 mm scalpel using the guidance of the finger and no further device. Additional instruments and retractors, assistance, and suturing are not required in the fingertip technique.
Alternative abdominal localizations for entry have been suggested when intra-abdominal adhesions are suspected. However, any cases can present unsuspected adhesions in any intraperitoneal field. For this reason, in the closed abdominal entry, Palmer’s point is the most recommended point of entry in patients with previous abdominal surgery, but it is not suggested for entry in cases with splenomegaly or gastric distention.16,17 In contrast, in open-entry techniques, a bladeless trocar or cannula is inserted blindly through the peritoneal space after the abdominal fascia is opened up. In these methods, there is a risk of intestinal injury if adherent intestinal tissue still exists, and gas leakage can occur around the margin of the cannula. Furthermore, direct abdominal entry using a bladeless trocar without achieving pneumoperitoneum is not suggested for a surgeon who is new to performing laparoscopic surgery, as blind entry—even with a bladeless trocar—is not always safe, easy, or effective.18
In the fingertip technique, the fascial layer can be felt and incised securely. This minimizes the risk of solid organ or major vascular injury because the fascia is incised by only millimeters using the tip of the scalpel, and the peritoneal cavity is bluntly entered with the tip of the finger. However, in cases with severe intra-abdominal adhesions, the risk of injury to adherent bowels cannot be eliminated with this technique. Unfortunately, this problem exists in all techniques, including Veress needle, optical entry, and Hasson.7 However, with the fingertip technique, the abdomen can be entered at any location, meaning the risk of bowel injury can be relatively decreased ensuring distance between previous surgical scars and the point of incision. In the present study, nine patients had a history of previous open abdominal surgery, and we did not encounter any major vascular or abdominal organ injury in these patients.
Gas leakage is a common problem during laparoscopic surgery, especially when open abdominal entry methods are used, which requires special equipment, such as a Hasson cannula, or suturing around the trocar. Gas leakage has been reported as occurring in 15% of cases when using the open-entry technique and 9.5% of cases when using the Veress needle technique.19 Kaistha et al. reported that gas leakage occurred in 1% of cases when using the direct trocar entry method and in 8.2% of cases when using the open-entry technique.20 The fingertip technique minimizes the gas leakage, as well as the need for additional interventions such as suturing or the use of special instruments to prevent gas leakage. When using the fingertip technique, we made a fascial defect that was smaller than the size of the cannula. Also, we did not use any instruments or retractors that minimize the enlargement of the incision to see the abdominal layers while entering the abdomen. In the present study, gas leakage was seen in two patients with subcutaneous bleeding and the other three patients with leakage were obese (BMI > 35 kg/m2), for these obese patients suturing around the trocar was performed. Mild gas leakage can be controlled by changing the trocar with a 15 mm size. Furthermore, using a cannula with a helical structure shaft can also decrease the gas leakage more effectively than a straight shaft cannula.
The upper layers of the abdomen may be enlarged during blunt dissection with the finger in the fingertip technique. However, the insertion of only the fingertip through the parietal peritoneal layer is an important step to prevent gas leakage. The peritoneal layer, in particular, holds the trocar tightly. For surgeons with a large index finger, the risk of gas leakage may increase; in such situations, a smaller finger may be used as the guide.
It may take more time to establish pneumoperitoneum when using open abdominal entry techniques, in which assistance and additional equipment may also be required. The mean procedure time has been reported to be 2 – 4 minutes in open-entry methods, 2 – 3 minutes in Veress needle methods, and 1 – 3 minutes in direct trocar entry methods, according to previous studies.12,21,22 While the fingertip technique naturally follows the principles of previous open-entry techniques, interestingly, it seems to be as quick as closed-entry methods (e.g., the Veress needle and direct trocar insertion technique), according to previous reports. Entering the abdomen using a Veress needle seems to be faster than other open techniques; however, the diameter of the needle is small and the airflow rate is low, so it takes more time to achieve pneumoperitoneum. In contrast, in the fingertip technique, pneumoperitoneum is obtained through the trocar, which has a larger diameter and higher airflow, accelerating the procedure.
Another important issue is the cost-effectivity of this technique. Especially for developing countries such as ours, it is not always possible to achieve special instruments such as Visiport because of the high cost of these devices.
Habibi et al. stated that obesity is the most challenging factor for a successful abdominal entry during laparoscopic surgery irrespective of the technique.23 The fingertip technique enables easy reachment into the peritoneum to finger length, and the abdominal wall layers are passed with the fingertip bluntly. In upper urinary tract surgery, the initial entry point is located in a more lateral position. In that specific location, abdominal wall thickness is shorter than the one in the medial abdominal wall. Thus, the fingertip technique seems to be more efficient in urologic surgeries even in overweight or obese patients.
In addition to widely known entry techniques, techniques using specific devices are described in the literature. Carlson used the fluid-based peritoneal entry indication technique, which is very fast and easy, but requires a special instrument (the EndoTIP trocar).2 The rate of failure for initial entry is also higher (9%) in this technique, especially in initial cases. Many techniques have been defined based on a similar principle to that of the fluid-based peritoneal entry indication; however, these typically require a large incision or the use of special instruments.24 The all-seeing needle technique is another interesting closed-entry method, which was used in 11 pediatric cases without any complications by Silay et al.15 However, safety profile requirements for special instruments have limited the use of this technique.
The relatively small sample size and lack of long-term follow-up data are the main limitations of the present study. To avoid confounding bias, all procedures were performed by a single surgeon; however, this resulted in insufficient information regarding the feasibility of this technique for use by other surgeons. It is difficult to remove the “experience factor” when popularizing the use of a novel surgical technique. The fingertip technique is used by the trainees and surgeons as an option in certain laparoscopic surgeries at various times in our center. Last, the application of the fingertip technique is relatively hard and probably not quite feasible in pediatric cases due to the size of the finger as the preferred trocar size in them is 5 mm.
CONCLUSION
The fingertip technique is a safe, easy method for abdominal entry in laparoscopic surgery that shortens the length of the procedure and decreases the need for additional instruments. It is a good alternative method for initial abdominal entry, particularly for surgeons who do not prefer to use the Veress needle technique for laparoscopic entry.
Contributor Information
Ahmet Şahan, Department of Urology, Kartal Dr. Lutfi Kirdar Training and Research Hospital, Istanbul, Turkey.
Orkunt Ozkaptan, Department of Urology, Kartal Dr. Lutfi Kirdar Training and Research Hospital, Istanbul, Turkey.
Alkan Cubuk, Department of Urology, Kartal Dr. Lutfi Kirdar Training and Research Hospital, Istanbul, Turkey.
Berkan Şimşek, Department of Urology, Kartal Dr. Lutfi Kirdar Training and Research Hospital, Istanbul, Turkey.
Yiloren Tanidir, Department of Urology, Marmara University, Istanbul, Turkey.
Oktay Akça, Department of Urology, Kartal Dr. Lutfi Kirdar Training and Research Hospital, Istanbul, Turkey.
References:
- 1.Angioli R, Terranova C, De Cicco Nardone C, et al. A comparison of three different entry techniques in gynecological laparoscopic surgery: a randomized prospective trial. Eur J Obstet Gynecol Reprod Biol. 2013;171(2):339–342. [DOI] [PubMed] [Google Scholar]
- 2.Carlson WH, Tully G, Rajguru A, Burnett DR, Rendon RA: Cameraless peritoneal entry in abdominal laparoscopy. JSLS. 2012;16(4):559–563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tinelli A (ed). Laparoscopic Entry. 1st ed. London: Springer, 2012. [Google Scholar]
- 4.Alkatout I. Complications of laparoscopy in connection with entry techniques. J Gynecol Surg. 2017;33(3):81–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Veress J. A needle for the safe use of pheumoperitoneum. Gastroenterologia. 1961;96:150–152. [PubMed] [Google Scholar]
- 6.Hasson HM. A modified instrument and method for laparoscopy. Am J Obstet Gynecol. 1971;110(6):886–887. [DOI] [PubMed] [Google Scholar]
- 7.Hasson HM. Open laparoscopy. Biomed Bull. 1984;5(1):1–6. [PubMed] [Google Scholar]
- 8.Sahan A, Orkunt O, Alkan C, Mete K, Oktay A. A novel open abdominal entry method: fingertip technique. Videourology. 2020;34(4). [Google Scholar]
- 9.Şahan A. The fingertip technique (a novel laparoscopic abdominal entry method). 2020; https://www.youtube.com/watch?v=DEuw_uiFYBY&t=599s. [Google Scholar]
- 10.Ahmad G, Baker J, Finnerty J, Phillips K, Watson A. Laparoscopic entry techniques. Cochrane Database Syst Rev. 2019;1:CD006583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vilos GA, Ternamian A, Dempster J, Laberge PY. Clinical practice gynaecology c: laparoscopic entry: a review of techniques, technologies, and complications. J Obstet Gynaecol Can. 2007;29(5):433–447. [DOI] [PubMed] [Google Scholar]
- 12.Tinelli A, Malvasi A, Mynbaev OA, et al. Bladeless direct optical trocar insertion in laparoscopic procedures on the obese patient. JSLS. 2013;17(4):521–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ertugrul I, Kayaalp C, Yagci MA, Sumer F, Karagul S, Tolan K. Comparison of direct trocar entry and Veress needle entry in laparoscopic bariatric surgery: randomized controlled trial. J Laparoendosc Adv Surg Tech A. 2015;25(11):875–879. [DOI] [PubMed] [Google Scholar]
- 14.Ciravolo G, Donarini P, Rampinelli F, Visenzi C, Odicino F. Laparoscopic access with optical gasless trocar: a single-center experience of 7431 procedures. J Minim Invasive Gynecol. 2020;27(2):535–540. [DOI] [PubMed] [Google Scholar]
- 15.Silay MS, Tepeler A, Sancaktutar AA, et al. The all-seeing needle instead of the Veress needle in pediatric urologic laparoscopy. J Endourol. 2013;27(11):1376–1380. [DOI] [PubMed] [Google Scholar]
- 16.Palmer R: Safety in laparoscopy. J Reprod Med. 1974;13(1):1–5. [PubMed] [Google Scholar]
- 17.Royal College of Obstetricians and Gynaecologists Guidelines (2008). Preventing entry-related gynaecological laparoscopic injuries; Green-Top Guideline No. 49. RCOG L. [Google Scholar]
- 18.Kassir R, Blanc P, Lointier P, et al. Laparoscopic entry techniques in obese patient: Veress needle, direct trocar insertion or open entry technique? Obes Surg. 2014;24(12):2193–2194. [DOI] [PubMed] [Google Scholar]
- 19.Shayani-Nasab H, Amir-Zargar MA, Mousavi-Bahar SH, et al. Complications of entry using direct trocar and/or Veress needle compared with modified open approach entry in laparoscopy: six-year experience. Urol J. 2013;10(2):861–865. [PubMed] [Google Scholar]
- 20.Kaistha S, Kumar A, Gangavatiker R, Br S, Sisodiya N. Laparoscopic access: direct trocar insertion versus open technique. J Laparoendosc Adv Surg Tech A. 2019;29(4):489–494. [DOI] [PubMed] [Google Scholar]
- 21.Pantoja Garrido M, Frias Sanchez Z, Zapardiel Gutierrez I, et al. Direct trocar insertion without previous pneumoperitoneum versus insertion after insufflation with Veress needle in laparoscopic gynecological surgery: a prospective cohort study. J Obstet Gynaecol. 2019;39(7):1000–1005. [DOI] [PubMed] [Google Scholar]
- 22.Sangrasi AK, Memon AI, Memon MM, Abbasi MR, Laghari AA, Qureshi JN. A safe quick technique for placement of the first access port for creation of pneumoperitoneum. JSLS. 2011;15(4):504–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Habibi M, Seyit H, Kones O, Kartal B, Alis H. Direct trocar insertion with elevation of the rectus sheath in bariatric surgery: a novel technique. Pol Przegl Chir. 2017;89(6):23–25. [DOI] [PubMed] [Google Scholar]
- 24.Uranues S, Ozkan OV, Tomasch G. Safe and easy access technique for the first trocar in laparoscopic surgery. Langenbecks Arch Surg. 2016;401(6):909–912. [DOI] [PubMed] [Google Scholar]