Abstract
The threat of plastic waste pollution in African countries is increasing exponentially since the World Health Organisation declared the coronavirus infection as a pandemic. Fundamental to this growing threat are multiple factors, including the increased public consumption for single-use plastics, limited or non-existence of adequate plastic waste management infrastructures, and urbanisation. Plastics-based personal protective equipment including millions of surgical masks, medical gowns, face shields, safety glasses, protective aprons, sanitiser containers, plastics shoes, and gloves have been widely used for the reduction of exposure risk to Severe Acute Respiratory Syndrome (SARS) Coronavirus 2 (SARS-CoV-2). This paper estimates and elucidates the growing plethora of plastic wastes in African countries in the context of the current SARS-CoV-2 pandemic. A Fourier transform infrared (FTIR) spectral fingerprint indicates that face masks were characterised by natural and artificial fibres including polyester fibres, polypropylene, natural latex resin. Our estimate suggests that over 12 billion medical and fabric face masks are discarded monthly, giving the likelihood that an equivalent of about 105,000 tonnes of face masks per month could be disposed into the environment by Africans. In general, 15 out of 57 African countries are significant plastic waste contributors with Nigeria (15%), Ethiopia (8.6%), Egypt (7.6%), DR Congo (6.7%), Tanzania (4.5%), and South Africa (4.4%) topping the list. Therefore, this expert insight is an attempt to draw the attention of governments, healthcare agencies, and the public to the potential risks of SARS-CoV-2-generated plastics (COVID plastic wastes), and the environmental impacts that could exacerbate the existing plastic pollution epidemic after the COVID-19 pandemic.
Keywords: SARS-CoV-2, Single-use plastics, COVID plastic wastes, Plastic pollution, SDG 3, SDG 11, SDG 14
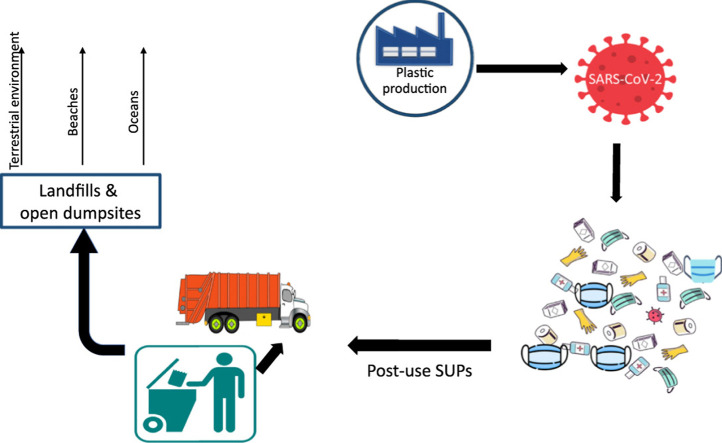
Graphical Abstract
1. Introduction
Plastic wastes are ubiquitous and acknowledged as an environmental stressor, adding micropollutants to the world's vulnerable ecosystems burdened by multiple changes. Across the African continent, land-based plastic waste is a notable challenge stemming from increasing plastic production and mismanaged disposal [1], [2]. Coronavirus Disease-2019 (COVID-19) has triggered an unprecedented glut of plastics waste globally. Given the abundant and burgeoning array of discarded surgical masks, medical gowns, face shields, safety glasses, protective aprons, sanitiser containers, plastics shoes, food packages, and gloves, it is likely that the threat from plastic pollution is imminent ( Fig. 1). The coronavirus pandemic has caused the development of emergency responses and cutting-edge approaches aimed at addressing and overcoming COVID-19 virus while minimising risks of exposures and promoting healthy lifestyles of all citizens. One of such COVID-19 precautionary measure designed to reduce community infection through droplet transmission is the mandatory use of plastic-based personal protective equipment by frontline healthcare practitioners and face masks for people leaving their homes.
Fig. 1.
Coronavirus-19 generated PPEs and single-use plastics littered or inappropriately discarded along Atlantic Ocean coast and dumpsites in Nigeria (Photo credits: Nsikak Benson).
In Africa, several countries including Kenya, Morocco, Egypt, Central African Republic, South Africa, Angola, Ethiopia, Equatorial Guinea, DR Congo, Liberia, Benin, Zambia, Sierra Leone, Gabon, Burkina Faso, Cameroun, and Rwanda have gazetted official regulations on the mandatory use of medical-grade or cloth face masks in public spaces and the workplace [3], [4], [5], [6]. In West Africa, the use of face mask in the public place has been made compulsory in Nigeria, Chad, Ghana, Mali, Mauritania, Senegal, Liberia, and Guinea Bissau. In contrast, Togo, Niger and Gambia have recommended face masks use in some areas [7]. In most countries, violators could face periods of imprisonment or pay fines. These policies became necessary, considering that an increasing number of researches have suggested that face masks serve as an efficacious means of controlling the spread of coronavirus. The prime vehicle of SARS-CoV-2 community transmission is through respiratory droplets when an infected or an asymptomatic patient sneezes, coughs or communicates with others. Hence, the mandatory use of face masks (surgical brands or homemade face coverings act as barriers to prevent or limit the virus-containing droplets from being transmitted from an infected patient to others in public spaces [8], [9], [10]. Presently, protecting public safety and conquering the virus remains the priority of governments and healthcare agencies. However, the measures adopted in stemming COVID-19 must not be misconstrued to mean the license to suspend the war on single-use plastics or the government-backed support to pollute our terrestrial and marine environments with disposable plastics.
Africa is the second-largest continent in the world, with a fast population growth estimated at 1.34 billion people for 2020 [11]. According to this estimate, Africa accounts for about 17% of the total world population, with an average of 49% of the people living in the urban and semiurban communities. Besides the unprecedented concentration of people in the urban centres, the burgeoning middle-class population in African countries has created vast consumer markets for plastic products [12], [2]. In most countries, traditional methods of food products and shop items packaging have been superseded by plastic food packages and plastic takeaway containers. In retail outlets, shops, supermarkets, street and food vending businesses, and major markets across Africa, single-use plastics are widely used for packaging merchandises and food products, thus increasing the consumption rate of plastics in the continent [1], [13].
In the last few decades, the African continent has witnessed a proportionate increase in plastic production and per capita consumption as its population grows coupled with rapid urbanisation [2], [14]. However, given inadequate facilities to manage the large quantity of plastic waste generated coupled with the existence of weak regulation on municipal waste management, a large number of plastic debris end up as inadequately disposed and littered wastes. These mismanaged plastics wastes are at high risk of polluting rivers, waterways, and the ocean.
Since the COVID-19 was discovered and the WHO declared its spread as a public health emergency, several African countries have made it mandatory for its citizens to wear face masks, or face shields especially while in public spaces. Several commercially sold surgical grade masks are manufactured from sheets of plastics intended for use as single-use plastics (SUPs). However, in most countries, these imported surgical grade masks largely made from non-woven polypropylene are expensive and in short supply. As a result, people have resorted to improvisation and homemade production of cloth face covering or masks, sewed commonly from textiles (mainly cotton). These cloth face masks are mostly reusable and are recommended as a substitute for surgical-grade masks to reduce the transmission of coronavirus [15], [16], [17]. However, most of these single-use personal protective equipment are mismanaged resulting in indiscriminate disposal and widespread contamination of the terrestrial, atmospheric and aquatic environments. This paper provides a survey of the polymeric characteristics of some commercially available face masks in Africa. We report here the first estimates of single-use face masks generated by countries in Africa during the COVID-19 pandemic, as well as highlight the potential risks mismanaged SUPs could pose to public health and the environment. The paper has also identified some plastic management challenges in Africa and proposes mitigation measures to address the problem of plastic pollution epidemic in Africa.
2. Methodology
2.1. Face masks polymeric characterisation with ATR-FTIR
We collected samples of commercially available surgical-grade (SG) (n = 100) and Filtering facepiece 2 (FFP2) (n = 50) face masks bought from major pharmaceutical companies in Ogun State, while the homemade (HM) (n = 30) face masks were purchased from street hawkers in Lagos and Ogun States. The sample collections were randomly done in June 2020. After collection, the face masks were sorted and cut into 3 × 3 cm using a Sparco stainless steel scissors. It is imperative to note that the face masks used in this work does not represent all the various single-use PPEs in Africa or the multiple products and brands commercially available in African countries. It could however be taken as random representatives of face masks used and discarded in the continent. To determine the types of polymer in the various face masks collected, Fourier transform infrared (FTIR) spectroscopy was used to characterise the SG, HM and FFP2 face masks samples. The characterization was performed in the attenuated total reflectance (ATR) mode using the Agilent 630 Cary FTIR Spectrometer equipped with a diamond crystal at a resolution of 8 cm−1, 32 sample scans and a range of 4000–650 cm−1. For measurement of spectra of face masks samples collected, each sample was introduced directly and clamped onto the ATR diamond crystal after performing the clean check. A relative pressure was applied to close the press, and the analysis was done using the Agilent MicroLab® software for the determination of a spectrum of satisfactory intensity. The Agilent polymer ATR library and the Sigma-Aldrich® Online Infra-red Spectrum Table and Chart were utilised to evaluate the absorptions and vibrations for functional groups in each polymer. The acceptable match quality was fixed at ≥ 80% [18], [19], [20]. The representative spectra for samples of SG, HM and FFP2 face masks polymers are presented in Fig. 2.
Fig. 2.
Representative spectra and absorption bands for surgical-grade (SG), homemade (HM) and Filtering facepiece 2 (FFP2) face masks polymers: polyester fibres (PE), natural latex resin (NL), and polypropylene (PP).
2.2. Estimation of COVID-19 Face masks generation
The daily single-use face masks generated by each country in Africa is estimated as a function of the total population of a country, daily face mask use per capita and an arbitrary percent of facemask acceptance rate by the urban population [21]. The total monthly and daily estimated face mask generations were computed according to the following equations:
| (1) |
| (2) |
Where Tp = the estimated population of the country, Up = the percentage of urban population of the country, Ar = the percent face mask acceptance rate, Ac = the average daily face masks per capita. The average number of days in a month per year was estimated as 30 days.
3. Results and discussion
3.1. Polymer characterisation
The spectra established that the textile fibres of the face mask brands were characterised by a combination of natural and artificial fibres including polyester fibres (PE), polypropylene (PP), natural latex resin (NL), polyethylene terephthalate, styrene isoprene, and styrene butadiene rubber. The FTIR spectra verified the appearance of the absorption bands that are typical of polypropylene: vibrations linked with C–C bonding (1200–800 cm−1), CH2 scissor vibrations and CH3 symmetric deformation vibrations or CH3 asymmetric deformation vibrations (1453–1356 cm−1), and CH2 and CH3 symmetric and asymmetric stretching vibrations (2950–2830 cm−1) (Fig. 2) [22], [23].
Also, the FTIR spectra confirmed the presence of PE synthetic fibres in the FFP2 (3 M) and homemade face masks (Fig. 2). The spectra showed various characteristic absorption bands associated with polyester fibres including the moderately intense C-H stretching (2840–3000 cm−1), strong C-H bending (723 cm−1) and medium C˭C out-of-plane bending vibrations of the benzene rings (872 cm−1). The absorption bands that appear at 1013 and 3369 cm−1 are linked with the OH out-of-plane bending in the terminal carboxylic groups and intermolecular OH bonded to C˭O groups in the polyester chains, respectively, while the peak at 1710 cm−1 indicates the appearance of a strong C˭O stretching band for the carboxylic group [24], [25], [26]. On the other hand, the spectral fingerprints of natural latex rubber (NL) indicated characteristic absorption peaks at 2952, 2914, 2870, and 2836 cm−1 and are assigned to moderately intense C–H stretching vibration, medium C˭C stretching for alkene at peak 1651 cm−1, while the absorption peaks at 1457 cm−1 and 1375 cm−1 are attributed to carbon-hydrogen deformation for CH2 group and carbon-hydrogen deformation for CH3 group, respectively [27]. Therefore, it is well established that PE, PP and NL were the most dominant fibres in face mask brands.
3.2. Single-use face masks consumption across Africa
With the current consumption of SUPs especially surgical masks and homemade (fabric) face masks, if people in the urban and semi-urban areas in all countries in Africa used at least one mask each day at the rate 70% face mask acceptance, the estimated volume of face masks generated and disposed of in a day per capita would be about 412 million pieces, with over 100 million metric tonnes (Mtn) of other contaminated plastics (surgical masks, medical gowns, face shields, safety glasses, protective aprons, sanitiser containers, plastics shoes, gloves, plastic water containers, flipflops, etc.) wastes produced per year ( Table 1). The report by the World Wide Fund for Nature indicated that an average mask weighs approximately 4 g [28], [29]. However, in order to ascertain the average weight of mask commonly available in the continent, we collected several samples of gloves, FFP2 (3 M) (Filtering Facepiece 2), surgical-grade and homemade masks and measured their weights. According to our findings, the average weight of face mask varied according to the mask's brand and grade, ranging from 2.50.1, 10.580.2, and 10.294.06 g for surgical-grade, FFP2 and homemade masks, respectively. On the other hand, the average weight of the glove was found to be 5.030.01 g. Thus, the current estimate in this research indicated that the average weight of a face masks is 8.58 g. Accordingly, calculations using the present data have shown that 3.5 million kg per capita of plastic wastes from face masks use would be littered or inadequately disposed of each day in urban centers in African countries. This means that with over 12 billion single-use face masks discarded monthly, about 105,000 tonnes of face masks per month could be disposed into the environment by people living in the African continent. This quantity of plastic wastes may exacerbate the existing plastic pollution epidemic after the COVID-19 pandemic.
Table 1.
Estimated face masks disposal and plastic waste generation by African countries.
| Country | Populationa | Urban Population (%)a | Total casesa | Total deathsa | Active casesa | Rate (%) of face mask acceptanceb | Face mask / capitab | Estimated daily face mask disposed | Estimated weight of face masks (Kg) | Estimated daily plastic waste (Tonnes) |
|---|---|---|---|---|---|---|---|---|---|---|
| Algeria | 43,854,590 | 73 | 15,941 | 952 | 3497 | 70 | 1 | 22,409,695 | 190,482 | 3289,094 |
| Angola | 32,863,687 | 67 | 346 | 19 | 219 | 70 | 1 | 15,413,069 | 131,011 | 2464,777 |
| Benin | 12,123,248 | 48 | 1199 | 21 | 845 | 70 | 1 | 4073,411 | 34,624 | 909,244 |
| Botswana | 2351,786 | 73 | 277 | 1 | 247 | 70 | 1 | 1201,763 | 10,215 | 176,384 |
| Burkina Faso | 20,902,979 | 31 | 987 | 53 | 80 | 70 | 1 | 4535,946 | 38,556 | 1567,723 |
| Burundi | 11,890,146 | 14 | 191 | 1 | 72 | 70 | 1 | 1165,234 | 9904 | 891,761 |
| Cabo Verde | 556,036 | 68 | 1421 | 16 | 751 | 70 | 1 | 264,673 | 2250 | 41,703 |
| Cameroon | 26,546,427 | 56 | 12,592 | 313 | 2179 | 70 | 1 | 10,406,199 | 88,453 | 1990,982 |
| Central African Rep. | 4830,173 | 43 | 3969 | 48 | 3007 | 70 | 1 | 1453,882 | 12,358 | 362,263 |
| Chad | 16,425,296 | 23 | 871 | 74 | 10 | 70 | 1 | 2644,473 | 22,478 | 1231,897 |
| Comoros | 869,652 | 29 | 309 | 7 | 61 | 70 | 1 | 176,539 | 1501 | 65,224 |
| Congo | 5518,223 | 70 | 1557 | 44 | 1012 | 70 | 1 | 2703,929 | 22,983 | 413,867 |
| Côte d′Ivoire | 26,378,877 | 51 | 10,462 | 72 | 5583 | 70 | 1 | 9417,259 | 80,047 | 1978,416 |
| Djibouti | 988,091 | 79 | 4736 | 55 | 101 | 70 | 1 | 546,414 | 4645 | 74,107 |
| DR Congo | 89,555,575 | 46 | 7379 | 182 | 4236 | 70 | 1 | 28,836,895 | 245,114 | 6716,668 |
| Egypt | 102,342,235 | 43 | 74,035 | 3280 | 50,652 | 70 | 1 | 30,805,013 | 261,843 | 7675,668 |
| Equatorial Guinea | 1402,824 | 73 | 3071 | 51 | 2178 | 70 | 1 | 716,843 | 6093 | 105,212 |
| Eritrea | 3546,748 | 63 | 215 | – | 159 | 70 | 1 | 1564,116 | 13,295 | 266,006 |
| Eswatini | 1160,266 | 30 | 988 | 13 | 428 | 70 | 1 | 243,656 | 2071 | 87020 |
| Ethiopia | 114,966,205 | 21 | 5846 | 103 | 3313 | 70 | 1 | 16,900,032 | 143,650 | 8622,465 |
| Gabon | 2225,815 | 87 | 5620 | 44 | 3021 | 70 | 1 | 1355,521 | 11,522 | 166,936 |
| Gambia | 2416,608 | 59 | 57 | 2 | 28 | 70 | 1 | 998,059 | 8484 | 181,246 |
| Ghana | 31,074,883 | 57 | 20,085 | 122 | 5093 | 70 | 1 | 12,398,878 | 105,390 | 2330,616 |
| Guinea | 13,132,670 | 39 | 5570 | 34 | 1040 | 70 | 1 | 3585,219 | 30,474 | 984,950 |
| Guinea-Bissau | 1968,072 | 45 | 1765 | 25 | 1064 | 70 | 1 | 619,943 | 5270 | 147,605 |
| Kenya | 53,774,120 | 28 | 7886 | 160 | 5439 | 70 | 1 | 10,539,728 | 89,588 | 4033,059 |
| Lesotho | 2142,413 | 31 | 79 | – | 68 | 70 | 1 | 464,904 | 3952 | 160,681 |
| Liberia | 5057,871 | 53 | 869 | 37 | 463 | 70 | 1 | 1876,470 | 15,950 | 379,340 |
| Libya | 6871,927 | 78 | 989 | 27 | 704 | 70 | 1 | 3752,072 | 31,893 | 515,395 |
| Madagascar | 27,691,313 | 39 | 2941 | 32 | 1801 | 70 | 1 | 7559,728 | 64,258 | 2076,848 |
| Malawi | 19,130,121 | 18 | 1613 | 17 | 1279 | 70 | 1 | 2410,395 | 20,488 | 1434,759 |
| Mali | 20,250,095 | 44 | 2303 | 118 | 669 | 70 | 1 | 6237,029 | 53,015 | 1518,757 |
| Mauritania | 4649,671 | 57 | 4827 | 129 | 2893 | 70 | 1 | 1855,219 | 15,769 | 348,725 |
| Mauritius | 1271,795 | 41 | 341 | 10 | 1 | 70 | 1 | 365,005 | 3103 | 95,385 |
| Mayotte | 272,823 | 46 | 2661 | 35 | 251 | 70 | 1 | 87,849 | 747 | 20,462 |
| Morocco | 36,913,924 | 64 | 14,215 | 235 | 4255 | 70 | 1 | 16,537,438 | 140,568 | 2768,544 |
| Mozambique | 31,254,703 | 38 | 987 | 8 | 723 | 70 | 1 | 8313,751 | 70,667 | 2344,103 |
| Namibia | 2541,110 | 55 | 412 | – | 387 | 70 | 1 | 978,327 | 8316 | 190,583 |
| Niger | 24,201,945 | 17 | 1088 | 68 | 55 | 70 | 1 | 2880,031 | 24,480 | 1815,146 |
| Nigeria | 206,144,243 | 52 | 28,167 | 634 | 16,071 | 70 | 1 | 75,036,504 | 637,810 | 15,460,818 |
| Réunion | 895,376 | 100 | 536 | 2 | 62 | 70 | 1 | 626,763 | 5327 | 67,153 |
| Rwanda | 12,952,510 | 18 | 1092 | 3 | 566 | 70 | 1 | 1632,016 | 13,872 | 971,438 |
| Sao Tome & Principe | 219,176 | 74 | 719 | 13 | 439 | 70 | 1 | 113,533 | 965 | 16,438 |
| Senegal | 16,743,956 | 49 | 7400 | 133 | 2397 | 70 | 1 | 5743,177 | 48,817 | 1255,797 |
| Seychelles | 98,353 | 56 | 81 | – | 70 | 70 | 1 | 38,554 | 328 | 7376 |
| Sierra Leone | 7977,515 | 43 | 1533 | 62 | 420 | 70 | 1 | 2401,232 | 20,410 | 598,314 |
| Somalia | 15,892,879 | 47 | 2961 | 92 | 1896 | 70 | 1 | 5228,757 | 44,444 | 1191,966 |
| South Africa | 59,314,150 | 67 | 187,977 | 3026 | 93,724 | 70 | 1 | 27,818,336 | 236,456 | 4448,561 |
| South Sudan | 11,194,743 | 25 | 2021 | 38 | 1650 | 70 | 1 | 1959,080 | 16,652 | 839,606 |
| Sudan | 43,850,981 | 35 | 9767 | 608 | 4486 | 70 | 1 | 10,743,490 | 91,320 | 3288,824 |
| Tanzania | 59,732,362 | 37 | 509 | 21 | 305 | 70 | 1 | 15,470,682 | 131,501 | 4479,927 |
| Togo | 8279,041 | 43 | 676 | 15 | 229 | 70 | 1 | 2491,991 | 21,182 | 620,928 |
| Tunisia | 11,819,657 | 70 | 1186 | 50 | 90 | 70 | 1 | 5791,632 | 49,229 | 886,474 |
| Uganda | 45,736,977 | 26 | 939 | – | 48 | 70 | 1 | 8324,130 | 70,755 | 3430,273 |
| Western Sahara | 597,354 | 87 | 10 | 1 | 1 | 70 | 1 | 363,789 | 3092 | 44,802 |
| Zambia | 18,383,527 | 45 | 1632 | 30 | 254 | 70 | 1 | 5790,811 | 49,222 | 1378,765 |
| Zimbabwe | 14,864,287 | 38 | 698 | 8 | 509 | 70 | 1 | 3953,900 | 33,608 | 1114,822 |
Data retrieved from https://www.worldometers.info/population/ on July 05, 2020.
Hypothetical data.
Given the likelihood that several people in the continent have complied with the governments' directive to use personal protective equipment, and that much of the PPEs (face masks, gloves, and medical gowns) are used for protection of health workers, this could cause littering. Much of these contaminated PPEs may culminate in mismanaged plastic wastes and could pose serious threats to human health and the environment [30], [21]. African countries have seen several tonnes of SUPs either inadequately discarded in dumpsites and uncontrolled solid waste landfills, or littered openly in available public spaces including parks, markets, beaches, and sidewalks. The unprecedented rise in the number of disposable surgical masks and hand gloves can contribute to the plethora of plastic pollution [31], [32].
According to our estimations based on the proportion of total plastic wastes (TPWs) in municipal solid wastes, and the quantity of waste generation per capita in African countries, the calculated fraction of mismanaged plastic waste produced by each country is presented in Table 1. However, it should be noted that the estimated TPWs generation by a country is the quantity derived before formal waste management involving sorting, recycling, or incineration. Thus, TPWs does not depict the volume of plastics at risk of polluting the gullies, inland waterways, canals, creeks, rivers, estuarine and the marine ecosystems. ( Fig. 3).
Fig. 3.
Projected share of face masks generated daily per country Map created with mapchart.net©.
The results of this study indicated that 15 out of 57 countries in Africa are major contributors of single-use plastic wastes, contributing about 75% of the TPWs in the continent per year with Nigeria (15%), Ethiopia (8.6%), Egypt (7.6%), DR Congo (6.7%), Tanzania (4.5%), and South Africa (4.4%) topping the list ( Fig. 4, Fig. 5). These countries mostly have extensive maritime coastal zones bordering the ocean. Therefore, the existence of poor or limited waste management facilities in these countries could result in the littering and direct introduction of land-based derived plastic wastes into the beaches and ocean.
Fig. 4.
Major contributors of plastic waste that is inadequately managed in 2020 Map created with mapchart.net©.
Fig. 5.
Continental percent share of plastic waste generation per country measured in metric tonnes per year.
In most developing countries in Africa, it is a common practice to discard domestic and industrial wastes in open landfills, wastewater gullies, inland waterways, poorly managed and uncontrolled dumpsites, street bins, drainage canals and paved walkways. Over the years, these dumpsites and landfills have become very problematic to manage, and a rallying point where waste scavengers visit to forage for the recovery of waste recyclables. Waste pickers or hunters are essential players in informal waste management, especially in developing countries where waste picking serves as a quick source of income for the urban and semi-urban poor [33], [34], [35]. Informal waste management in most African countries is dominated by landfill scavengers, itinerant waste hunters, and neighbourhood waste pickers who primarily engage in uncontrolled activities of waste collection, sorting and recycling [36], [37], [38]. The scavenging of littered heaps for potentially recyclable materials is usually carried out without wearing suitable personal protective equipment. In Nigeria, it has been reported that scavengers are engaged in collecting discarded face masks from open dumps for recycling and resale to the unsuspecting public [39]. Although waste picking in third world countries may serve as a means of livelihood and escape from poverty for the impoverished few, it could potentially be a vehicle for the spread of infectious diseases including COVID-19 [40], [41], [42]. Recent reports have identified the stability and survivability of COVID-19 virus on contaminated fomites including plastics, banknotes, stainless steel, cardboard, copper, wood, and face masks [43], [40]. The studies showed that the infectious viral particles of SARS-CoV-2 is exceptionally contagious and could remain viable on a range of surfaces for several minutes and up to 9 days [40], [30]. Coronaviruses on plastics and stainless-steel surfaces were found to be more viable and stable for 2–3 days than cardboard, wood, banknotes and copper [43], [40]. Therefore, the spread and infectivity of COVID-19 through inadequately disposed or littered wastes could be filliped by scavengers and informal waste collectors upon exposure to contaminated materials.
The question surrounding how COVID-19 virus is transmitted and the strategies to stop the virus from spreading has generated a growing global concern over the use of single-use plastics, thus dampening the war against plastic pollution. Over the past months, millions of people around the world have been compelled to observe the government-issued directives on lockdown as a measure of reducing the spread of the virus. COVID-19 has been described as a zoonotic disease that originated at the end of December 2019 in Wuhan in Hubei Province, China and has spread to over 212 countries and territories around the world and two international conveyances [11], [44], [45], [46]. As of early July 2020, the outbreak recorded over 12 million confirmed coronavirus cases worldwide, with at more than half a million deaths [11]. In Africa, over 500,000 and 12,000 confirmed COVID-19 cases and deaths have been recorded as at early July 2020 ( Fig. 6, Table 1). According to the WHO, SARS-CoV-2 virus is primarily transmitted via saliva droplets or release from the nostril when an infected patient sneezes or coughs [47].
Fig. 6.
Total confirmed COVID-19 cases per million people in African countries.
Past investigations have shown that contaminated surfaces are principal vehicles for the spread of viral infections [48], [49]. The presence of COVID-19 ribonucleic acid on surfaces of inappropriately released single-use clinical materials has been reported [43], [40]. As indicated by reported studies, COVID-19 RNA has been discovered to be more stable and potent for 2–3 days on plastics and treated steel surfaces than on cardboard, wood, banknotes and copper [43], [40]. In addition, the epidemiological information from the studies revealed that coronavirus could be detected on the outer surfaces of face masks for a few minutes and as long as 2.8 days after exposure ( Fig. 7). These data confirm the stability and viability of COVID-19 infection through infected face masks and other clinical wastes [40], [50], [51]. Thus, it is imperative to reappraise existing waste management in Africa countries to avoid community infection of people through exposed surfaces and disposed contaminated face masks. Additionally, inappropriate collection and management of COVID-19 wastes, including littering, disposal in uncontained landfills and open dumps may likely exacerbate the current plastic waste pollution in the continent.
Fig. 7.
Epidemiological data on the stability of COVID-19 on contaminated surfaces.
4. Conclusion and recommendations
Plastic pollution has been identified as a growing environmental and public health challenge. The sorption of carcinogenic and endocrine-disrupting chemicals onto bulk plastics and micro-, meso-, and macro-plastics in the terrestrial environment and marine ecosystems has been widely reported [52], [53], [54], [55], [56], [57]. However, the magnitude of this problem and the call for measures to address the worsening plastic pollution crises have grown only lately to a higher level of public consciousness, especially since the inception of the COVID-19 pandemic. To address the problem of plastic pollution epidemic in Africa, the following recommendations are advocated:
-
a)
The disposal of contaminated PPEs should be meticulously handled by trained waste collectors and rightly bagged, discarded or recycled to prevent infection and associated health risks, environmental pollution, and injuries to marine mammals and other marine wildlife.
-
b)
The regular and thorough cleaning of surfaces in public places and isolation centers using 60–71% ethanol or 0.1% sodium hypochlorite would significantly degrade the infectivity of COVID-19 virus within a minute of application of a disinfectant.
-
c)
Due to the growing consumption of plastics globally, a glut of SUPs would likely end up as mismanaged plastic wastes. Therefore, emphasis should be placed on the intentional reduction in discarded plastic wastes before mismanagement. This could drastically reduce the millions of PPEs that could have been littered the gutters, thus preventing the blockage of waterways and flooding of urban areas as well as support the reduction in transmission of infectious diseases.
-
d)
The government of the various African countries should urgently create a working infrastructure for the collection, transportation, recycling, or incineration of plastic medical wastes at designated facilities far away from the urban areas. Besides, a functional and efficient on-site healthcare waste management facility should be installed in rural areas for the disposal of hazardous biomedical wastes to forestall the community spread of human coronaviruses and other infectious diseases. Additionally, this approach will replace the existing practice of open incineration or burying of biomedical wastes.
-
e)
We advocate the use of reusable face masks by the general populace as this could significantly reduce plastic wastes as well as the impacts of the post-COVID-19 pandemic on the marine environment resulting from policy obligations of wearing face masks.
-
f)
Given that people in the various countries are determined to adhere to the mandatory face mask order and other related COVID-19 policy regulations by taking personal responsibility to contain the community spread of COVID-19, now it is imperative for everyone to be fairly responsible in managing the disposal of their used personal protection equipment and not dispersed into the environment.
-
g)
Africa is nearly losing its quintessence and environmental magnificence to burgeoning waste pollution from single-use plastics. The volume of plastic wastes generation, especially SUPs is expected to double in the coming years as the size and population of its urban communities increase. In order to address plastic waste pollution, public education about efficient and sustainable approaches to waste management needs to be adopted. Public awareness education targeted on behavioural change and improving people's knowledge toward reducing plastic wastes, open dumping of used face masks, and the promotion of recycling, reuse, and source reduction activities are of most extreme significance.
-
h)
Furthermore, we suggest that designated waste receptacles should be provided at marked points in public places, healthcare facilities, shopping malls, markets, banks, worship centres, schools, and residential estates to collect used PPEs. In view of this, periodical emptying and routine decontamination of the waste containers must be carried out by trained hazardous waste handlers in line with laid down guidelines [58], [59], [60].
-
i)
In general, as the coronavirus pandemic continues, a strong recommendation to the government, health workers, medical experts, and the public would be to prevent plastic pollution by being individually, communally and globally responsible.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Nsikak Benson, David Bassey: Conceptualization; Nsikak Benson: Data curation; Nsikak Benson, Omowunmi Fred-Ahmadu: Formal analysis; Nsikak Benson, David Bassey: Investigation; Nsikak Benson, Omowunmi Fred-Ahmadu, David Bassey, Aderemi Atayero: Writing - original draft; Nsikak Benson, Omowunmi Fred-Ahmadu, David Bassey, Aderemi Atayero: Writing - review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors acknowledge the invaluable comments by reviewers.
Data sharing
All data used in this study are publicly available and are referenced in the manuscript.
Editor: Dr. Zhang Xiwang
References
- 1.Adam I., Walker T.R., Bezerra J.C., Clayton A. Policies to reduce single-use plastic marine pollution in West Africa. Mar. Policy. 2020;116(2020) doi: 10.1016/j.marpol.2020.103928. [DOI] [Google Scholar]
- 2.Jambeck J., Hardesty B.D., Brooks A.L., Friend T., Teleki K., Fabres J., Beaudoin Y., Bamba A., Francis J., Ribbink A.J., Baleta T., Bouwman H., Knox J., Wilcox C. Challenges and emerging solutions to the land-based plastic waste issue in Africa. Mar. Policy. 2018;96:256–263. doi: 10.1016/j.marpol.2017.10.041. [DOI] [Google Scholar]
- 3.Aljazeera News, (2020). Which country have made wearing face masks compulsory; accessed 22.06.2020, 〈https://www.aljazeera.com/news/2020/04/countries-wearing-face-masks-compulsory-200423094510867.html〉.
- 4.Kabatanya, M. (2020). Wearing face masks now compulsory in CAR; accessed 22.06.2020; 〈https://minusca.unmissions.org/en/wearing-face-masks-now-compulsory-car〉.
- 5.PDA, Pharmacists’ Defence Association, (2020). Wearing face masks in public: Approach of different countries across the world; accessed 22.06.2020, 〈https://www.the-pda.org/wp-content/uploads/002-Face-masks-Global-Iman-V2.pdf〉.
- 6.Tasamba, J. (2020). COVID-19: Rwanda, DR Congo make mask wearing mandatory; accessed 22.06.2020; 〈https://www.aa.com.tr/en/africa/covid-19-rwanda-dr-congo-make-mask-wearing-mandatory/1810165〉.
- 7.SWAC, Sahel and West Africa Club Secretariat, (2020). West Africa makes face mask use compulsory; accessed 22.06.2020, 〈http://www.west-africa-brief.org/content/en/west-africa-makes-face-mask-use-compulsory〉.
- 8.Aydin O., Emon B., Saif M.T.A. Performance of fabrics for home-made masks against spread of respiratory infection through droplets: a quantitative mechanistic study. medRxiv Prepr. 2020 doi: 10.1101/2020.04.19.20071779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Furukawa N.W., Brooks J.T., Sobel J. Evidence supporting transmission of severe acute respiratory syndrome coronavirus 2 while presymptomatic or asymptomatic. Emerg. Infect. Dis. 2020;26(7) doi: 10.3201/eid2607.201595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rothe C., Schunk M., Sothmann P., Bretzel G., Froeschl G., Wallrauch C., Zimmer T., Thiel V., Janke C., Guggemos W., Seilmaier W., Drosten C., Vollmar P., Zwirglmaier K., Zange S., Wölfel R., Hoelscher M. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N. Engl. J. Med. 2020;382:970–971. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Worldometers (2020). COVID-19 Coronavirus pandemic; accessed 05.07.2020, 〈https://www.worldometers.info/coronavirus/〉.
- 12.Deloitte (2014). The Deloitte Consumer Review Africa: A 21st century View, accessed 12.05.2020, 〈https://www2.deloitte.com/content/dam/Deloitte/ng/Documents/consumer-business/the-deloitte-consumer-review-africa-a-21st-century-view.pdf〉.
- 13.Miezah K., Obiri-Danso K., Kádár Z., Fei-Baffoe B., Mensah M.Y. Municipal solid waste characterization and quantification as a measure towards effective waste management in Ghana. Waste Manag. 2015;46:15–27. doi: 10.1016/j.wasman.2015.09.009. [DOI] [PubMed] [Google Scholar]
- 14.Jambeck J.R., Geyer R., Wilcox C., Siegler T.R., Perryman M., Andrady A., Narayan R., Law K.L. Plastic waste inputs from land into the ocean. Science. 2015;347:768–771. doi: 10.1126/science.1260352. [DOI] [PubMed] [Google Scholar]
- 15.CDC, (2020). Centers for Disease Control and Prevention. Use of cloth face coverings to help slow the spread of COVID-19. Accessed 29.06.2020, 〈https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/diy-cloth-face-coverings.html〉.
- 16.MacIntyre C.R., Chughtai A.A. Face masks for the prevention of infection in healthcare and community settings. BMJ. 2015;350:h694. doi: 10.1136/bmj.h694. [DOI] [PubMed] [Google Scholar]
- 17.Mahase E. Covid-19: what is the evidence for cloth masks? BMJ. 2020;2020(369) doi: 10.1136/bmj.m1422. [DOI] [PubMed] [Google Scholar]
- 18.Baskaran S., Sathiavelu M. Application of attenuated total reflection - fourier transform infrared spectroscopy to characterize the degradation of littered multilayer food packaging plastics. Vib. Spectrosc. 2020;109 doi: 10.1016/j.vibspec.2020.103105. [DOI] [Google Scholar]
- 19.Fred-Ahmadu O.H., Ayejuyo O.O., Benson N.U. Dataset on microplastics and associated trace metals and phthalate esters in sandy beaches of tropical Atlantic ecosystems, Nigeria. Data Brief. 2020;31 doi: 10.1016/j.dib.2020.105755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fred-Ahmadu O.H., Ayejuyo O.O., Benson N.U. Microplastics distribution and characterization in epipsammic sediments of tropical Atlantic Ocean, Nigeria. Reg. Stud. Mar. Sci. 2020;38 doi: 10.1016/j.rsma.2020.101365. [DOI] [Google Scholar]
- 21.Nzediegwu C., Chang S.X. Improper solid waste management increases potential for COVID-19 spread in developing countries. Resour. Conserv. Recycl. 2020;161 doi: 10.1016/j.resconrec.2020.104947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kostov K.G., Nishime T.M.C., Hein L.R.O., Toth A. Study of polypropylene surface modification by air dielectric barrier discharge operated at two different frequencies. Surf. Coat. Technol. 2013;234:60–66. doi: 10.1016/j.surfcoat.2012.09.041. [DOI] [Google Scholar]
- 23.Marković D., Tseng H.-H., Nunney T., Radoičić M., Ilic-Tomic T., Radetić M. Novel antimicrobial nanocomposite based on polypropylene non-woven fabric, biopolymer alginate and copper oxides nanoparticles. Appl. Surf. Sci. 2020;527 doi: 10.1016/j.apsusc.2020.146829. [DOI] [Google Scholar]
- 24.Kale R.D., Bansal P.S., Gorade V.G. Extraction of microcrystalline cellulose from cotton sliver and its comparison with commercial microcrystalline cellulose. J. Polym. Environ. 2018;26:355–364. doi: 10.1007/s10924-017-0936-2. [DOI] [Google Scholar]
- 25.Peets P., Leito I., Pelt J., Vahur S. Identification and classification of textile fibres using ATR-FT-IR spectroscopy with chemometric methods. Spectrochim. Acta Part A Mol. Biomol. Spectrosc. 2017;173:175–181. doi: 10.1016/j.saa.2016.09.007. [DOI] [PubMed] [Google Scholar]
- 26.Sharma K., Khilari V., Chaudhary B.U., Jogi A.B., Pandit A.B., Kale R.D. Cotton based composite fabric reinforced with waste polyester fibres for improved mechanical properties. Waste Manag. 2020;107:227–234. doi: 10.1016/j.wasman.2020.04.011. [DOI] [PubMed] [Google Scholar]
- 27.Bhadra S., Mohan N., Parikh G., Nair S. Possibility of Artocarpus heterophyllus latex as an alternative source for natural rubber. Polym. Test. 2019;79 doi: 10.1016/j.polymertesting.2019.106066. [DOI] [Google Scholar]
- 28.Syam, N. (2020). Is the pandemic triggering a spike in plastic pollution?; accessed 22.05.2020; 〈https://newseu.cgtn.com/news/2020–05-22/Is-the-pandemic-triggering-a-spike-in-plastic-pollution--QBobeagfok/index.html〉.
- 29.WWF, World Wide Fund for Nature (2020). In the disposal of masks and gloves, responsibility is required, accessed 22.06.2020; 〈https://www.wwf.it/scuole/?53500%2FNello-smaltimento-di-mascherine-e-guanti-serve-responsabilita〉.
- 30.Kampf G., Todt D., Pfaender S., Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J. Hosp. Infect. 2020;104(3):246–251. doi: 10.1016/j.jhin.2020.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Boyle, l. (2020). Discarded coronavirus face masks and gloves rising threat to ocean life, conservationists warn, accessed 29.04.2020, https://www.independent.co.uk/news/coronavirus-masks-gloves-oceans-pollution-waste-a9469471.html.
- 32.Chaudhuri, S. (2020). War on plastic takes a back seat in coronavirus crisis; accessed 10.05.2020, 〈https://www-wsj-com.cdn.ampproject.org/c/s/www.wsj.com/amp/articles/war-on-plastic-takes-a-back-seat-in-coronavirus-crisis-11584624140〉.
- 33.Ahmed A.S., Ali M. Partnerships for solid waste management in developing countries: linking theories to realities. Habitat Int. 2004;28(3):467–479. [Google Scholar]
- 34.Asim M., Batool S.A., Chaudhry M.N. Scavengers and their role in the recycling of waste in Southwestern Lahore. Resour. Conserv. Recycl. 2012;58:152–162. [Google Scholar]
- 35.Sembiring E., Nitivattananon V. Sustainable solid waste management toward an inclusive society: integration of the informal sector. Resour. Conserv. Recycl. 2010;54:759–1026. [Google Scholar]
- 36.Imam A., Mohammed B., Wilson D.C., Cheeseman C. Solid waste management in Abuja, Nigeria. Waste Manag. 2007;28:468–472. doi: 10.1016/j.wasman.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 37.Oguntoyinbo O.O. Informal waste management system in Nigeria and barriers to an inclusive modern waste management system. Public Health. 2012;126:441–447. doi: 10.1016/j.puhe.2012.01.030. [DOI] [PubMed] [Google Scholar]
- 38.Tremblay C., Gutberlet J., Peredo A.M. United we can: resource, recovery, place and social enterprise. Resour. Conserv Recycl. 2010;54:422–428. [Google Scholar]
- 39.Folorunsho-Francis, F. (2020). Scavengers pick face masks from dumpsites for recycling –SGF; accessed 03.07.2020, 〈https://healthwise.punchng.com/scavengers-pick-face-masks-from-dumpsites-for-recycling-sgf/〉.
- 40.Doremalen N. van, Morris D.H., Holbrook M.G., Gamble A., Williamson B.N. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020 doi: 10.1056/nejmc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Moss, E., Eidson, A., Jambeck, J. (2017). Sea of Opportunity: Supply Chain Investment Opportunities to Address Marine Plastic Pollution, Encourage Capital on behalf of Vulcan, Inc., New York, New York.
- 42.Vasickova P., Pavlik I., Verani M., Carducci A. Issues concerning survival of viruses on surfaces. Food Environ. Virol. 2010;2:24–34. doi: 10.1007/s12560-010-9025-6. [DOI] [Google Scholar]
- 43.Chin A.W.H., Chu J.T.S., Perera M.R.A., Hui K.P.Y., Yen H.-L., Chan M.C.W., Peiris M., Poon L.L.M. Stability of SARS-CoV-2 in different environmental conditions. Lancet Microb. 2020 doi: 10.1016/S2666-5247(20)30003-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bogoch A., Watts A., Thomas-Bachli C., Huber M.U.G., Kraemer K., Khan K. Pneumonia of unknown aetiology in Wuhan, China: potential for international spread via commercial air travel!Abstract. J. Travel Med. 2020;27 doi: 10.1093/jtm/taaa008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Guo Y.-R., Cao Q.-D., Hong Z.-S., Tan Y.-Y., Chen S.-D., Jin H.-J., Tan K.-S., Wang D.-Y., Yan Y. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak - An update on the status. Mil. Med. Res. 2020;7:1–10. doi: 10.1186/s40779-020-00240-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mackenzie J.S., Smith D.W. COVID-19: a novel zoonotic disease caused by a coronavirus from China: what we know and what we don’t. Microbiol. Aust. 2020;41:45. doi: 10.1071/MA20013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.WHO, World Health Organisation (2020a). Coronavirus; accessed 01.05.2020; 〈https://www.who.int/health-topics/coronavirus#tab=tab_1〉.
- 48.Jones S.L., Gibson K.E. Characterization of polyurethane foam environmental monitoring tools for the recovery and release of viruses. Food Environ. Virol. 2020;12:158–166. doi: 10.1007/s12560-020-09421-5. [DOI] [PubMed] [Google Scholar]
- 49.Park G.W., Lee D., Treffiletti A., Hrsak M., Shugart J., Vinjé J. Evaluation of a new environmental sampling protocol for detection of human norovirus on inanimate surfaces. Appl. Environ. Microbiol. 2015;81(17):5987–5992. doi: 10.1128/AEM.01657-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nghiem L.D., Morgan B., Donner E., Short M.D. The COVID-19 pandemic: considerations for the waste and wastewater services sector. Case Study Chem. Environ. Eng. 2020;1 doi: 10.1016/j.cscee.2020.100006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Todd E.C., Greig J.D., Bartleson C.A., Michaels B.S. Outbreaks where food workers have been implicated in the spread of foodborne disease. Part 6. Transmission and survival of pathogens in the food processing and preparation environment. J. Food Prot. 2009;72:202–219. doi: 10.4315/0362-028x-72.1.202. [DOI] [PubMed] [Google Scholar]
- 52.Amereh F., Babaei M., Eslami A., Fazelipour S., Rafiee M. The emerging risk of exposure to nano(micro)plastics on endocrine disturbance and reproductive toxicity: from a hypothetical scenario to a global public health challenge. Environ. Pollut. 2020;261 doi: 10.1016/j.envpol.2020.114158. [DOI] [PubMed] [Google Scholar]
- 53.Benson N.U., Fred-Ahmadu O.H. Occurrence and distribution of microplastics-sorbed phthalic acid esters (PAEs) in coastal psammitic sediments of tropical Atlantic Ocean, Gulf of Guinea. Sci. Total Environ. 2020;730 doi: 10.1016/j.scitotenv.2020.139013. [DOI] [PubMed] [Google Scholar]
- 54.Chae Y., An Y.-J. Effects of micro- and nanoplastics on aquatic ecosystems: current research trends and perspectives. Mar. Pollut. Bull. 2017;124(2):624–632. doi: 10.1016/j.marpolbul.2017.01.070. [DOI] [PubMed] [Google Scholar]
- 55.Jiang X., Chang Y., Zhang T., Qiao Y., Klobučar G., Li M. Toxicological effects of polystyrene microplastics on earthworm (Eisenia fetida) Environ. Pollut. 2020;259 doi: 10.1016/j.envpol.2019.113896. [DOI] [PubMed] [Google Scholar]
- 56.Prata J.C., da Costa J.P., Lopes I., Duarte A.C., Rocha-Santos T. Environmental exposure to microplastics: an overview on possible human health effects. Sci. Total Environ. 2020;702 doi: 10.1016/j.scitotenv.2019.134455. [DOI] [PubMed] [Google Scholar]
- 57.Trifuoggi M., Pagano G., Oral R., Pavičić-Hamer D., Burić P., Kovačić I., Siciliano A., Toscanesi M., Thomas P.J., Paduano L., Guida M., Lyons D.M. Microplastic-induced damage in early embryonal development of sea urchin Sphaerechinus granularis. Environ. Res. 2019;179 doi: 10.1016/j.envres.2019.108815. [DOI] [PubMed] [Google Scholar]
- 58.Africa CDC, (2020). Guidance on Environmental decontamination in the context of COVID-19; accessed 04.07.2020, 〈https://africacdc.org/download/guidance-on-environmental-decontamination-in-the-context-of-covid-19/〉.
- 59.EU, European Union (2020). Waste management in the context of the coronavirus crisis; accessed 02.07.2020, 〈https://ec.europa.eu/info/sites/info/files/waste_management_guidance _dg-env.pdf〉.
- 60.WHO, World Health Organisation (2020b). Cleaning and disinfection of environmental surfaces in the context of COVID-19: Interim guidance; accessed 02.07.2020; 〈https://www.who.int/publications-detail/ cleaning-and-disinfection-of-environmental-surfaces-inthe-context-of-covid-19〉.