Abstract
Objectives
Patients on home parenteral nutrition (HPN) are prone to severe complications of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. The pandemic requires adaptation of the health care standards, including epidemiologic surveillance, logistics of home supply, and monitoring. Potential lack of medical professionals may worsen the standard of care. The aim of this study was to evaluate the medical staff resources in HPN units.
Results
The study was conducted by major Polish scientific societies in clinical nutrition. A questionnaire was distributed among all Polish adult HPN centers concerning statistics from the first 3 mo of the pandemic (March through May 2020). Data on medical staff resources and organizational issues of the units were collected. Modifications of the home procedures, SARS-CoV-2 infection rates of HPN patients and health care workers (HCW) were analyzed. Influence of the pandemic on the rates of new qualifications for home artificial nutrition (HAN) was estimated. Fourteen of 17 adult Polish HPN units took part in the study. The point prevalence of HPN in Poland was 30.75/1 million citizens. Of HCWs, 344 were involved in patient care in Polish HPN units; 18.9% were physicians (49% surgeons, 18.46% internal medicine specialists, 15.38% anesthesiologists, 7.69% pediatricians, 1.54% palliative care specialists), 32.27% nurses, 5.23% dietitians, 9.01% pharmacists, 4.94% pharmacy technicians, 3.2% pharmacy assistants, 5.81% administrative workers, 3.49% physiotherapists. HAN patient-to-HCW ratios for physicians, nurses, pharmacists, dietitians were 49.5, 29.15, 111.6, and 181.6, respectively. Medium ages of physicians and nurses were 45.6 and 44.15 y, respectively. Slightly less than half (53.8%) of physicians and 31.53% of nurses worked parallelly in hospital wards. Thirty-one pharmacists overall were working in all HPN units (2.21 per unit) as were 18 dietitians (1.3 per unit). Nine patients had a confirmed COVID-19 infection (four HPN, five home enteral nutrition). All the units introduced telemedicine solutions in the first months of the pandemic. The number of new qualifications for HPN and home enteral nutrition in the units did not significantly decline from March through May in comparison with a similar period in 2019.
Conclusions
A shortage of HPN medical professionals requires attention when planning health care organization, especially during a pandemic. Severe restrictions in public health systems may not reduce the number of new qualifications for the HPN procedure. There is a need for the continuation of data collection during the evolution of the pandemic as it may have a detrimental effect on HPN including serious issues with access to professional HCWs.
Keywords: Home parenteral nutrition, Home enteral nutrition, COVID-19, Pandemic, Health care workers, Human resources
Introduction
Home parenteral nutrition (HPN) is a lifesaving procedure for patients with no possibility for efficient oral or enteral nutrition who do not require hospital stay for other reasons. The complicity of the procedure involves specialized centers based on hospital units to provide safe care for patients with intestinal failure (IF). According to recent European Society for Clinical Nutrition and Metabolism (ESPEN)) guidelines on HPN, those are dedicated hospital units with nutritional support teams (NST) including specialists in HPN provision with the background of surgical care, supportive treatment, and protocols for managing possible complications. The safety of the procedure is to be provided by a multispecialized team of physicians, nurses, pharmacists, dietitians, physiotherapists, and psychologists [1].
In March 2020, the by the World Health Organization (WHO) proclaimed a global pandemic of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2 or COVID-19). Some 41 million cases and 1,136,530 deaths have been reported around the world by the WHO [2]. The first COVID-19–positive patients in Poland were diagnosed in March and relatively radical public health and epidemiologic restrictions were introduced: cancelation of mass events, limitations for gastronomic facilities and sports services, closing schools and cultural institutions, social distancing, and banned entry to Poland for foreigners [3]. On April 30, 12 877 laboratory-confirmed COVID-19 cases and 644 related deaths were reported in Poland [4].
Studies show that patients of advanced age and those with coexisting diseases like diabetes, cardiovascular disease, chronic respiratory disease, hypertension, and cancer were more susceptible to a severe course of COVID-19 infection [5,6]. According to epidemiologic data, most of the patients qualified for HPN due to short bowel syndrome (SBS) mechanism, mostly; mesenteric ischemia, Crohn's disease (CD), surgical complications, radiation enteritis, or chronic intestinal pseudoobstruction. Moreover, there is a growing number of newly qualified patients with cancer as a primary disease [1,7]. Polimorbidity is affecting >70% of adults in hospitals and is a significant health care problem among HPN patients as well [8], [9], [10]. HPN can be specifically affected by the pandemic due to several reasons. First, patients are often immunocompromised, malnourished, with comorbidities or on immunosuppressing drugs (e.g., patients with CD), and therefore are vulnerable to the worse outcomes of COVID-19 infection. Secondly, patients with IF often require to be transferred to a referral IF/HPN unit and monitored during the treatment and the procedure involves in-hospital training. Reliance on caregivers, repeated contacts with health care workers (HCWs) or pharmacy staff, delivering nutritional admixtures can amplify the risk for infection. However, there are no solid data to confirm that in the population of patients needing HPN, studies show possible chains of transmission of coronavirus during hospital stay from infected patients or asymptomatic HCWs [11], [12], [13].
Experiences from other countries show that the health care crisis is intensified and may be caused by insufficient resources of medical staff. This may limit access to professional care or increase the patient-to-physician or patient-to-nurse ratio. Many medical professionals may be in danger of contracting infection, causing a threat for their patients and themselves. A Polish study conducted in April 2020 showed that almost half of infected patients (48%) were HCWs—25% nurses, 9% physicians, 3% medical caretakers [14]. Nearly 50% of home-isolated patients transmitted the infection to another person. It was confirmed by other researchers that in the US and UK population frontline HCWs had at least a threefold increased risk for COVID-19 infection [15]. Italian data showed 10% (17 000 patients were HCWs) and in Spain 20% of all infections were HCWs [16].
ESPEN recommends self-isolation of HPN patients, personal protective equipment (PPE) during visits, the introduction of telemedicine, avoiding face-to-face consultations, and limiting blood testing to only those tests that are necessary. The need for established strategies for patient discharge from the hospital and transfer to the IF unit is underlined [17,18]. Those recommendations are similar to the position paper proposed by the Polish expert group concerning principles of home nutrition during a pandemic [19].
There are no data on the epidemiology of COVID-19 infections among adult home artificial nutrition (HAN) patients and the medical staff of IF units. The second wave of the pandemic is rising in many European countries and public health decisions must be discussed. Moreover, there is a probability that long-term actions and modifications of medical algorithms will have to be made to control the pandemic. Objective data on HCWs are valid to plan public health solutions and safe medical services. Consequently, we decided to conduct a nationwide study to gather information on HCWs and organization issues in the perspective of the COVID-19 pandemic. This point of view can be beneficial not only for home nutrition but for other ambulatory or home care medical services.
Materials and methods
The study was conducted by major Polish scientific societies in clinical nutrition (for adults): Polish Society for Parenteral, Enteral Nutrition and Metabolism; Polish Network of Intestinal Failure Centers and Polish Society of Clinical Nutrition. A multicenter and nationwide survey was based on a questionnaire designed by the study group and distributed among Polish centers of HPN for adult patients. Data concerning medical staff, basic prevalence of HPN, organizational features of the units, and epidemiologic information on the first 3 mo of the COVID-19 pandemic in Poland (March, April, May, 2020) were addressed. Patient and HCW epidemiologic statistics were anonymized, and it was not possible to identify individual participants. It was conducted in accordance with the ethical standards of the Helsinki Declaration.
Outcomes
Primary outcomes
The primary aim of this study was to analyze the medical staff resources and organizational issues of Polish HPN units in light of pandemic challenges. Data concerning physicians, nurses, dietitians, pharmacists, physiotherapists, and administrative workers were collected. Age (medium, HCW >50 and >60 y of age), parallel employment in hospital wards, medical specialty was recorded in the survey. Information on HPN centers; the number of HPN and home enteral nutrition (HEN) patients per medical staff, hospital ward background of the unit, the number of possible patients educated for HPN at the same time was noted. Basic prevalence of HPN for Poland and for 16 administrative regions (voivodeships) was calculated overall.
Secondary outcomes
The secondary outcomes involved the changes during the first 3 mo of the COVID-19 pandemic. We analyzed organizational modifications and the rates of new qualifications for HPN and HEN. Data were compared with the prepandemic period (the year 2019). Testing protocols for patients and medical staff, infections among patients, medical staff in HPN units, and base hospitals were noted.
Statistical analysis
Statistical computer analysis was calculated using StatSoft, Inc. (2011). STATISTICA (data analysis software system), version 13. Quantitative variables were characterized using the arithmetic mean, SD, median, minimum and maximum values (range) and 95% confidence interval (CI). Qualitative variables were presented using frequencies and percentages. To check whether the quantitative variable derived from a population of normal distribution, the Shapiro–Wilk test was used. The significance of differences between the two groups (model of unrelated variables) was controlled with the Student's t test (or in cases of the absence of homogeneity of variance the Welch test) or the Mann–Whitney test. In all the calculations, the level of significance was P = 0.05.
Results
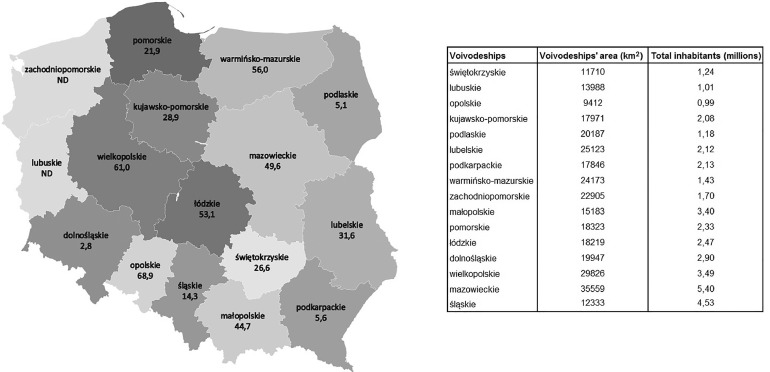
Of all 17 Polish adult HPN centers, 14 took part in the survey. According to the highest-level administrative division, there are 16 voivodeships in Poland (corresponding to "provinces" or "states" in many other countries). Ten voivodeships with one HPN center, three with two centers (dolnośląskie, śląskie, kujawsko-pomorskie, podlaskie), andtwo with no HPN center (lubuskie, zachodnio-pomorskie). One HPN unit is constituted for two voivodeships.
Prevalence of HPN in Poland
The general population of Poland, according to the Polish Central Statistical Office in 2019, was 38,411,148 [20]. The number of adult HPN patients reported was 1181, with a prevalence of 30.75/1 million citizens. Data from two units were not complete due to the lack of participation in the study (dolnośląskie, śląskie). Distribution among voivodeships is presented on the prevalence map (Fig. 1 ). All the Polish HPN units treat HEN patients as well. Median numbers of patients of HPN and HEN in units were 66 and 145 (Table 1 ).
Fig. 1.
Prevalence of home parenteral nutrition in Poland. Patients per 1 million citizens. ND, no complete data available.
Table 1.
Patients in HPN units
| Median | Min | Max | IQR | |
|---|---|---|---|---|
| HEN | 145 | 4 | 357 | 170 |
| HPN | 66 | 6 | 268 | 119 |
| HAN | 209 | 10 | 570 | 229 |
HAN, home artificial nutrition; HEN, home enteral nutrition; HPN, home parenteral nutrition; IQR, interquartile range.
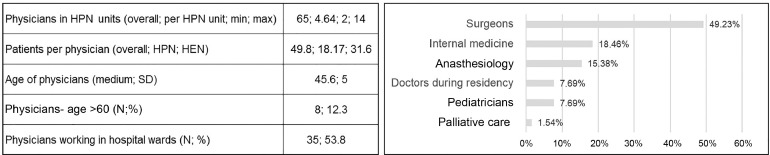
Medical staff data
Overall, 344 HCW were involved in patient care in Polish HPN units. Of these, 18.9% were physicians, 32.27% nurses, 5.23% dietitians, 9.01% pharmacists, 4.94% pharmacy technicians, 3.2% pharmacy assistants, 5.81% administrative workers, and 3.49% physiotherapists. Patients are qualified for HPN in the hospital setting. Education and training of the caregiver/patient for the procedure are provided in the surgical ward (seven units, 50%), other hospital ward depending on the primary diagnosis (three units, 21.4%), HPN outpatient clinic (two units, 14.3%), or in a special hospital ward dedicated for IF patients (two units, 14.3%). A median number of patients who can be educated for HPN simultaneously in one unit is 3.15 (SD 1.06; min–max 1–5), meaning that Poland has an overall educational activity of 41 patients trained for HPN at the same time.
Physicians
There were 65 physicians in all HPN units included in the survey (Fig. 2 ). Of these, most were surgeons, internal medicine, and anesthesiology specialists. In five of the units (35.7%), the medium age of physicians was >50 y and 53.8% of physicians worked in both hospital wards and HPN units. In six units (42.9%), all of the physicians worked in hospital wards. The median number of physicians per unit was 4.64 and only three of largest centers had more than four physicians working in the unit (21.4%). Three of the units (21.4%) had >90 HAN patients per physician; six (42.9%) had 50 to 90, and another six (42.9%) had <50 patients per physician.
Fig. 2.
Physicians in HPN units. HEN, home enteral nutrition; HPN, home parenteral nutrition.
Nurses, pharmacists, dietitians, and supportive HCW
Of the 111 nurses working in HPN centers, the average age was 44.15 y; with 27.9% being >50 y of age. Less than one-third worked in hospital wards (31.53%; Table 2 ). Of medical professionals, 59 were pharmacy workers (17.15%); 31 were pharmacists (9%); 15 of whom were clinical pharmacy specialists (48.39%) and 7 were during specialty (22.6%). There were 18 dietitians in all HPN units (1.3 dietitians per unit). Twenty administrative workers and 12 physiotherapists were working in HPN units. There were four HPN units (28.6%) with no administrative workers employed and eight (57.1%) had no physiotherapist on staff (Table 2).
Table 2.
Medical staff in HPN units
| Nurses | |
|---|---|
| Nurses in HPN units (overall; per HPN unit; min; max) | 111; 7.9; 2; 28 |
| Number of patients per nurse (overall; HPN; HEN) | 29.15; 10.63; 18.51 |
| Age of nurses (median, SD) | 44.15; 5.6 |
| Nurses; age >60 y (n; %) | 10; 9.01 |
| Nurses; age 50–60 y (n; %) | 21; 18.92 |
| Nurses; age <50 y (n; %) | 80; 72.07 |
| Nurses working in hospital wards (n; %) | 35; 31.53 |
| Pharmacy staff | |
| Pharmacists in HPN units (overall; per HPN unit; min; max) | 31; 2.21; 1; 4 |
| Number of patients per pharmacist (overall; HPN; HEN) | 111.6; 40.7; 70.9 |
| Pharmacy technicians (overall; per HPN unit) | 17; 1.3 |
| Pharmacy assistant (overall; per HPN unit) | 11; 0.8 |
| Dietitians | |
| Dietitians in HPN centers (overall; per HPN unit; min; max) | 18; 1.3; 1; 4 |
| Number of patients per dietitian (overall; HPN; HEN) | 181.61; 67.4; 114.2 |
| Physiotherapists in HPN centers (overall; per HPN unit; min; max) | 12; 0.86; 0; 5 |
| Number of patients per 1 physiotherapist | 272.4 |
| Administrative workers in HPN centers (overall; per HPN unit; min; max) | 20; 1.43; 0; 6 |
| Number of patients per 1 administrative worker | 163.4 |
HAN, home artificial nutrition; HEN, home enteral nutrition; HPN, home parenteral nutrition.
Changes during the COVID-19 pandemic
In most of the units, COVID-19 polymerase chain reaction testing was obligatory for patients admitted for HPN and previously treated in other hospitals. Of responders, 21.4% declared that only symptomatic patients were tested, and no routine screening was introduced. Of responding HPN units, half had no confirmed COVID-19 cases, as was the case for the base hospital of the unit during the first 3 mo of the epidemic. Three units confirmed cases in the hospital where HPN patients were educated. Overall, four patients on HPN had a confirmed COVID-19 infection in three units (21.4%), as did five HEN patients in two units (14.3%). Of HPN units, 28.6% declared at least one infection among HAN patients (Table 3 ). Medical staff were regularly tested in 42.9% of units when symptoms presented. Telemedicine methods were used to monitor HAN patients, in most cases and included telephone contact, email, or video conferences. In April, all units avoided face-to-face control visits unless the medical condition was life-threatening. In May, 28% of units returned to regular control visits in prepandemic mode (Table 4 ).
Table 3.
COVID-19 infections and testing protocols
| Confirmed COVID-19 infections | |
| No infections* | 7; 50 |
| In hospital ward† | 3; 21 |
| In hospital‡ | 7; 50 |
| Infected HPN patients (overall) | 4 |
| Units with infected patients (HPN) | 3; 21 |
| Infected HEN patients (overall) | 5 |
| Units with patients infected (HEN) | 2; 14.3 |
| Infected HEN and HPN patients (overall) | 9 |
| Units with patients infected (HPN and HEN) | 4; 28.6 |
| Testing new HPN patients | (HAN units; %) |
| External units were obliged to test new patients for COVID-19 | 7; 50 |
| External units tested or if not HPN unit did test on start | 4; 28.6 |
| No testing was routine (for asymptomatic patients) | 3; 21.4 |
| COVID-19 medical staff testing | (HAN units; %) |
| No tests | 1; 7 |
| <5 COVID-19 tests | 4; 28.6 |
| 5–15 COVID-19 tests | 3; 21.4 |
| >15 COVID-19 tests | 3; 21.4 |
| Regular testing regarding symptoms and history | 6; 42.9 |
HAN, home artificial nutrition; HEN, home enteral nutrition; HPN, home parenteral nutrition.
No COVID-19 infections among patients and medical staff of the unit and base hospital.
COVID-19 cases confirmed in hospital wards dedicated to the HPN unit.
COVID-19 infections among patients or medical staff of the base hospital of the HPN unit.
Table 4.
HAN monitoring
| Telemedicine tools used in HPN | (HAN units; %) | Control visits | (HAN units; %) |
|---|---|---|---|
| Phone contact | 5; 35.7 | April 2020 | |
| Phone contact and email | 4; 28.6 | Only telemedicine* | 14; 100 |
| Phone contact, email, and video connections | 5; 35.7 | May 2020 | |
| Only telemedicine* | 10; 71.4 | ||
| Like in prepandemic period | 4; 28.6 |
HAN, home artificial nutrition; HPN, home parenteral nutrition.
Face-to-face only in life-threatening situations.
We compared a medium number of qualified patients for HPN and HEN in 2019 with data concerning March, April, and May 2020. We found that there were no significant difference in the number of new patients during a pandemic (Table 5 ).
Table 5.
New qualifications for HAN
| 2019 | 2020 | P-value | |
|---|---|---|---|
| HPN | (median; min; max, Q1–Q3) | (median; min; max, Q1–Q3) | |
| March | 5.5; 1; 24; 2–8 | 5; 0; 18; 2–8 | 0.8542 |
| April | 5.5; 1; 24; 2–8 | 3.5; 0; 24; 2–8 | 0.4622 |
| May | 5.5; 1; 24; 2–8 | 4; 0; 23; 2–10 | 0.7828 |
| HEN | |||
| March | 10; 1; 30; 5–12 | 6; 0; 15; 2–8 | 0.0935 |
| April | 10; 1; 30; 5–12 | 8; 0; 15; 1–12 | 0.2977 |
| May | 10; 1; 30; 5–12 | 6; 0; 15; 3–15 | 0.3695 |
HAN, home artificial nutrition; HPN, home parenteral nutrition.
Discussion
To our knowledge, this was the first nationwide epidemiologic study including the majority of Polish HPN centers presenting basic epidemiologic data on the prevalence of HPN and organizational issues from the perspective of the pandemic situation. To our knowledge, there has been no other study concentrating on human resources of HPN units and no data on the situation during the COVID-19 pandemic.
We included 82.4% of Polish HPN units (14 of 17) with the majority of patients and point prevalence of 30.75 patients per 1 million citizens. This data supports the trend of the growing number of HPN patients observed in other studies. The first multicenter survey by the ESPEN HAN group reported the prevalence of HPN in Europe from 4.6 to 12.2 patients per million citizens [21]. However, more recent data demonstrate 17.1 and 22.3 HPN patients per million citizens in Italy and the United Kingdom [22,23] or even 79 patients in the U.S. population [24]. The study aimed to enroll Polish HPN centers. Those units take care of both HPN and HEN patients. We are aware that those data do not cover the Polish population of HEN patients. Considering that one of the primary goals was to analyze the burden of HCWs, full information on patient numbers was valid. Although there is no national registry, we estimate that there are nearly 6000 HEN patients in Poland, >4500 reported in our previous study analyzing data from the year 2018 [25].
HPN in Poland is based on hospital units and has been reimbursed from the National Health Fund since 1998. There is no medical specialty in clinical nutrition for physicians and no additional funding granting hospital wards for patients with IF. HPN units are most often based on surgical wards, palliative care units, or internal medicine wards. In 21% of units in Poland, patients are trained by the NST in the hospital ward depending on the primary disease and no specified beds are reserved in the hospital administrative structure. This organizational model may create difficulties in providing unified epidemiologic rules for the isolation of HPN patients and caregivers during education and training for the procedure. Data from other studies are supporting the thesis that hospitals may become “hubs” for the COVID-19 pandemic since 20% of infections of U.K. hospitalized patients and 89% of HCWs acquired infection in the hospital [26], [27], [28].
Available research indicates that PPE and mechanical ventilators are essential and possible shortages may contribute to the spread of virus and death rates [29]. Another major issue is the medical staff recourses. A limited number of physicians and nurses may require redistribution of HCWs to the centers struggling with the pandemic. Various solutions have been suggested to aid the crisis like the engagement of volunteers or medical students to support patient care [30,31]. Studies during the COVID-19 pandemic showed that hospitals have to adopt the working hours of HCWs to minimalize the risk for shortages of medical professionals. Epidemic-based staffing models include rotation work and “wash-out” quarantine intervals adjusted with the incubation period of the virus [32]. Screening protocols for HCWs may reduce the risk for infection for the patients and minimalize the problem of HCW shortages. Different strategies of COVID-19 screening for HCWs are suggested [21], following the growing knowledge of the characteristics of the pandemic spread. The present study determined that for every physician and nurse there is an average of 50.29 and 29.25 patient, respectively. There are 11 units (78%) in Poland with four or fewer physicians employed with an average of 4.6 physicians per every HPN unit included in the survey. According to ESPEN guidelines as well as Polish rules for reimbursement program of HPN, a minimal number of control visits is one per in 3 mo [1]. Calculating from our data, it requires >1086 control visits/mo in the overall Polish HAN population among enrolled units. Planning a rotation work to avoid transmissibility in HPN units may be exceedingly difficult to acquire. Additionally, more than half of the physicians and almost one-third of the nurses from the HPN units work in hospital wards as well, which may increase the risk for COVID-19 contraction. Quarantine of a physician/nurse/pharmacist in centers with a limited number of medical staff can paralyze the work, unable new qualifications and safe monitoring of HPN patients. Individuals with IF will be forced to stay at the hospital, which creates an additional risk for COVID-19 infection. Less than half of the Polish HPN units introduced regular testing of medical staff. Others provided swab testing only for HCWs with risk factors like contact with an infected patient, traveling to countries with increased infection rates, or respiratory tract infection symptoms like fever, cough, dyspnea or loss of smell. There were nine HAN patients with confirmed COVID-19 infection in HPN units during the observation time. Half of the units reported infections in the base hospital of the unit and 21% in the ward dedicated to IF patients. Of the units, 78% required COVID-19 swabs before the initiation of the HPN procedure if the patient was transferred from another hospital.
COVID-19 pandemic showed that telehealth solutions may be particularly useful and should be developed and integrated with the system [33]. HPN often requires contact with patients living a significant distance from the NST. New technologies develop new possibilities for HAN organization especially in the light of the COVID-19 pandemic. In April, all Polish units monitored the patients using telemedicine solutions, mostly phone contact and email. However, 28% of the units returned to classic in-person visits in May. Telemedicine reduces the need for personal contact with the NST to comply with the social distancing policy. A study in the United Kingdonm showed that remote solutions can be safely introduced in HPN. Considering the rapid growth of the number of HPN patients it can help with the demand of trained medical staff, reducing the need for hospital attendance of patients, and travelling miles to maximize the high satisfaction from medical care [17]. Other studies confirm that telehealth may be effective and cost-saving [18,19]. Singapore's experience shows that the development of IT solutions may enable safe PN and remote monitoring in a hospital setting [20]. However, a recent study on a pediatric HPN population determined that most of the responders considered that the COVID-19 crisis may negatively affect the quality of care of patients with IF. The authors mentioned that telemedicine solutions are unlikely to provide the same level of care as face-to-face contact. It has been shown that not all the patients/caregivers may have sufficient resources to engage tele-visits and the lack of PPE reported by families of HPN patients [34] may be an additional problem.
During the observation period of the study, significant changes were introduced to hospitals in Poland. Planned admissions were postponed and the work of most outpatient medical services was transferred to telemedicine solutions. European and Polish surgical guidelines suggested limitations of planned surgery, operating in cases of emergency or cancer if the immediate treatment was essential [35], [36], [37]. During the initial phase of the pandemic, many HCWs were afraid of contracting COVID-19 and transmitting it to their family members or other patients [38]. However, our data showed that the numbers of new qualifications for HPN and HEN in the units were similar to the comparable period in 2019. Although there may be areas of medicine where planned medical procedures can be postponed, HPN is a lifesaving treatment requiring continuity that can explain the constant need for the procedure.
Recent rapport showed that the number of physicians in Poland per 1000 citizens is the lowest in the European Union and 25% of them is above retirement age. Lack of nurses in hospitals is similarly a critical problem [39]. In analyzed data from HPN units, the median age of physicians was 45.6 y and there were nearly 36% of units with median age >50 y. Large studies showed that age is an independent risk factor of mortality for COVID-19 patients and increases >50 y [28]. However, our survey did not cover data concerning the health status of HCWs. Considering just the age and professional risks, we can assume that physicians from HPN units are not only more prone to acquire infection but additionally endangered of a more severe course of the disease.
The multidisciplinary approach of NST in HPN units involves the active role of hospital pharmacy, which is responsible for all hospital work as well as HPN provision. Save preparation of the HPN admixtures, pharmacotherapy, drugs, and clinical trial monitoring, organization of the delivery and active participation in the HPN training is provided by the pharmacy in the Polish health care system. Workload and the role of the pharmacist may depend on the usage of all-in-one HPN bags manufactured locally and customized admixtures to the individual patient (CA) versus commercially premixed (ready-to-use [RTU]) multichamber bags. The five biggest centers in the study (taking care of 71.5% of all polish HPN patients) use mainly CA bags, two centers use comparable amounts of RTU and CA (8.4% patients), and seven units based on RTU bags (20% of patients). The role of hospital pharmacy in a pandemic is rarely mentioned. Shanghai experience showed the importance of pharmacists in organizing the work of internet hospitals for telemedicine [40,41]. Community and hospital pharmacists are recognized as frontline HCWs during a pandemic [42]. Our survey revealed that only a little more than two pharmacists per one unit work in Polish HPN centers with >111 patients per one pharmacist calculated for the overall population. Although it might have been a barely sufficient number in the prepandemic period, we can assume that in the need for rotation work during the spread of pandemic serious problems in pharmacy staffing may emerge.
What is additionally presented in our study is the insufficient number of dietitians per HPN unit. Only 18 dietitians are employed in HPN centers in Poland giving little more than 1 per unit. Although there is little evidence for efficient dietetic interventions for COVID-19 treatment, we can anticipate from studies on septic patients, malnourished, with viral infections that the provision of micro- and micronutrients in the diet is crucial for the immunologic system. Patients in mild, moderate, and severe courses of the COVID-19 infection require the support of clinical dietitians [18]. HPN patients especially those with SBS, during bowel rehabilitation, or in the weaning phase of the treatment, need advanced dietetic counseling.
We are aware that the study was set in the first wave and initial phase of the pandemic. Due to advanced lockdown procedures, Polish rates of COVID-19 infections were relatively low. However, those data may be helpful to plan guidelines and strategies for home nutrition during the prolonged pandemic situation or following spread of the infection in autumn and winter. Although provided information is specific to the Polish health care system we assume that it is valuable to underline the specificity of home-based medical services like HPN. Our data can be compared with other local statistics and helpful to visualize the possible effect of the COVID-19 pandemic on patients and medical staff in this area of the system. There were some limitations to the present study. We were not able to conclude whether the testing protocols introduced in HPN units were effective and should be advised for other countries. This is a preliminary report and data needs to be collected in the following months to evaluate the evolution of the pandemic in the HAN population. An adequate level of staffing in home nutrition needs to be analyzed to provide preparedness for safe treatment also during a medical crisis like the COVID-19 pandemic.
Conclusions
Data from Polish centers show high patient-to-HCW ratios. Insufficient numbers of pharmacy workers and dietitians are objectively alarming. HCWs from a significant number of HPN units are >50 y of age and are more prone to a complicated course of COVID-19. To avoid transmission of the infection to HPN patients, HCW should be provided with sufficient PPE. Possible redistribution of HCW to other facilities struggling with pandemic may be impossible due to the need for the continuous care of HAN patients and a limited number of trained professionals. Public health organizers should take into consideration the pandemic evolution while planning the organization of hospital wards including HPN units. The location for training and education of the caregivers/patients should be adjusted to the epidemiologic situation. Limitations of planned medical procedures and health care restrictions may not reduce the need for HAN services as a life-saving procedure. Future studies are required to estimate the global influence of pandemic on home artificial nutrition support.
Footnotes
MF was responsible for the conceptualization, data curation, formal analysis, resources, supervision, writing, review, and editing. MF, SK, JS, and PM were responsible for writing the original draft. All authors were responsible for the investigation and have read and agreed to the published version of the manuscript. The authjors have no conflicts of interest to declare.
References
- 1.Pironi L, Boeykens K, Bozzetti F, Joly F, Klek S, Lal S, et al. ESPEN guideline on home parenteral nutrition. Clin Nutr. 2020;39:1645–1666. doi: 10.1016/j.clnu.2020.03.005. [DOI] [PubMed] [Google Scholar]
- 2.Coronavirus Disease Situation Reports. Available at: www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports. 2021
- 3.Pinkas J, Jankowski M, Szumowski L, Lusawa A, Zgliczynski WS, Raciborski F, et al. Public health interventions to mitigate early spread of SARS-CoV-2 in Poland. Med Sci Monit. 2020;26:1–7. doi: 10.12659/MSM.924730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Raciborski F, Pinkas J, Jankowski M, Sierpiński R, Zgliczyński WS, Szumowski Ł, et al. Dynamics of COVID-19 outbreak in Poland: an epidemiological analysis of the first two months of the epidemic. Polish Arch Intern Med. 2020;130:615–621. doi: 10.20452/pamw.15430. [DOI] [PubMed] [Google Scholar]
- 5.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 6.Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Di Napoli R. StatPearls Publishing; Treasure Island, FL: 2020. Features, evaluation and treatment of coronavirus. [PubMed] [Google Scholar]
- 7.Pironi L, Konrad D, Brandt C, Joly F, Wanten G, Agostini F, et al. Clinical classification of adult patients with chronic intestinal failure due to benign disease: an international multicenter cross-sectional survey. Clin Nutr. 2018;37:728–738. doi: 10.1016/j.clnu.2017.04.013. [DOI] [PubMed] [Google Scholar]
- 8.Steiner CA, Friedman B. Hospital utilization, costs, and mortality for adults with multiple chronic conditions, nationwide inpatient sample, 2009. Prev Chronic Dis. 2013;10:1–20. doi: 10.5888/pcd10.120292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380:37–43. doi: 10.1016/S0140-6736(12)60240-2. [DOI] [PubMed] [Google Scholar]
- 10.Gomes F, Schuetz P, Bounoure L, Austin P, Ballesteros-Pomar M, Cederholm T, et al. ESPEN guidelines on nutritional support for polymorbid internal medicine patients. Clin Nutr. 2018;37:336–353. doi: 10.1016/j.clnu.2017.06.025. [DOI] [PubMed] [Google Scholar]
- 11.Meredith LW, Hamilton WL, Warne B, Houldcroft CJ, Hosmillo M, Jahun AS, et al. Rapid implementation of SARS-CoV-2 sequencing to investigate cases of health-care associated COVID-19: a prospective genomic surveillance study. Lancet Infect Dis. 2020;20:1263–1272. doi: 10.1016/S1473-3099(20)30562-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wake RM, Morgan M, Choi J, Winn S. Reducing nosocomial transmission of COVID-19: Implementation of a COVID-19 triage system. Clin Med (London) 2020;20:E141–E145. doi: 10.7861/clinmed.2020-0411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arons MM, Hatfield KM, Reddy SC, Kimball A, James A, Jacobs JR, et al. Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. N Engl J Med. 2020;382:2081–2090. doi: 10.1056/NEJMoa2008457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sierpiński R, Pinkas J, Jankowski M, Juszczyk G, Topór-Mądry R, Szumowski Ł. Occupational risks for SARS-CoV-2 infection: the Polish experience. Int J Occup Med Environ Health. 2020;33:781–789. doi: 10.13075/ijomeh.1896.01663. [DOI] [PubMed] [Google Scholar]
- 15.Nguyen LH, Drew DA, Graham MS, Joshi AD, Guo C-G, Ma W, et al. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Heal. 2020;5:e475–e483. doi: 10.1016/S2468-2667(20)30164-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.https://www.ecdc.europa.eu/sites/default/files/documents/covid-19-rapid-risk-assessment-coronavirus-disease-2019-ninth-update-23-april-2020.pdf. 2021.
- 17.Lal S, Van Gossum A, Joly F, Bozzetti F, Cuerda C, Lamprecht G, et al. Considerations for the management of home parenteral nutrition during the SARS-CoV-2 pandemic: a position paper from the Home Artificial Nutrition and Chronic Intestinal Failure Special Interest Group of ESPEN. Clin Nutr. 2020;39:1988–1991. doi: 10.1016/j.clnu.2020.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barazzoni R, Bischoff SC, Breda J, Wickramasinghe K, Krznaric Z, Nitzan D, et al. ESPEN expert statements and practical guidance for nutritional management of individuals with SARS-CoV-2 infection. Clin Nutr. 2020;39:1631–1638. doi: 10.1016/j.clnu.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Matras P, Klek S, Folwarski M, Zmarzly A, Bartoszewska L, Cebulski W, et al. Home medical nutrition during SARS-CoV-2 pandemic – a position paper. Clin Nutr ESPEN. 2020;38:196–200. doi: 10.1016/j.clnesp.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Central Statistical Office. Local Data Bank. https://bdl.stat.gov.pl/BDL/start. Accessed April 12, 2020
- 21.Van Gossum A, Bakker H, De Francesco A, Ladefoged K, Leon-Sanz M, Messing B, et al. Home parenteral nutrition in adults: a multicentre survey in Europe in 1993. ESPEN - Home Artificial Nutrition Working Group. Clin Nutr. 1996;15:53–59. doi: 10.1016/s0261-5614(96)80019-7. [DOI] [PubMed] [Google Scholar]
- 22.Pironi L, Candusso M, Biondo A, Bosco A, Castaldi P, Contaldo F, et al. Prevalence of home artificial nutrition in Italy in 2005a survey by the Italian Society for Parenteral and Enteral Nutrition. Clin Nutr. 2007;26:123–132. doi: 10.1016/j.clnu.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 23.Smith T, Naghibi M, Stratton R, White S, Zeraschi S, Hughes SJ, et al. Artificial nutrition support in the UK 2005 e 2015. Adult home parenteral nutrition & home intravenous fluids A report by the British artificial nutrition survey (BANS), a committee of BAPEN (the British association for parenteral and enteral nutrition). 2016. ISBN: 978-1-899467-08-4. Available from: http://www.bapen.org.uk.
- 24.Mundi MS, Pattinson A, McMahon MT, Davidson J, Hurt RT. Prevalence of home parenteral and enteral nutrition in the United States. Nutr Clin Pract. 2017;32:799–805. doi: 10.1177/0884533617718472. [DOI] [PubMed] [Google Scholar]
- 25.Folwarski AM, Kłęk S, Wójcik AZ-, Szafrański W. Home enteral nutrition in adults — nationwide multicenter survey. Nutrients. 2020;12:2087. doi: 10.3390/nu12072087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jones NK, Rivett L, Sparkes D, Forrest S, Sridhar S, Young J, et al. Effective control of sars-cov-2 transmission between healthcare workers during a period of diminished community prevalence of covid-19. Elife. 2020;9:1–10. doi: 10.7554/eLife.59391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Evans S, Agnew E, Vynnycky E, Robotham J V. The impact of testing and infection prevention and control strategies on within-hospital transmission dynamics of COVID-19 in English hospitals. MedRxiv. 2020 doi: 10.1098/rstb.2020.0268. 2020.05.12.20095562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Iacobucci G. Covid-19: doctors sound alarm over hospital transmissions. BMJ. 2020;369:m2013. doi: 10.1136/bmj.m2013. [DOI] [PubMed] [Google Scholar]
- 29.Ranney ML, Griffeth V, Jha AK. Critical supply shortages - the need for ventilators and personal protective equipment during the Covid-19 pandemic. N Engl J Med. 2020;382:E41. doi: 10.1056/NEJMp2006141. [DOI] [PubMed] [Google Scholar]
- 30.Iserson K V. Augmenting the disaster healthcare workforce. West J Emerg Med. 2020;21:490–496. doi: 10.5811/westjem.2020.4.47553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rasmussen S, Sperling P, Poulsen MS, Emmersen J, Andersen S. Medical students for health-care staff shortages during the COVID-19 pandemic. Lancet. 2020;395:e79–e80. doi: 10.1016/S0140-6736(20)30923-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mascha EJ, Schober P, Schefold JC, Stueber F, Luedi MM. Staffing with disease-based epidemiologic indices may reduce shortage of intensive care unit staff during the COVID-19 pandemic. Anesth Analg. 2020;131:24–30. doi: 10.1213/ANE.0000000000004849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Provenzano DA, Sitzman BT, Florentino SA, Buterbaugh GA. Clinical and economic strategies in outpatient medical care during the COVID-19 pandemic. Reg Anesth Pain Med. 2020;45:579–585. doi: 10.1136/rapm-2020-101640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Galloway DP, Mathis MS, Wilkinson LT, Venick RS, Wendel D, Cole CR, et al. The effect of the COVID-19 pandemic on pediatric intestinal failure healthcare delivery. JPEN J Parenter Enteral Nutr. 2021;45:50–56. doi: 10.1002/jpen.2000. [DOI] [PubMed] [Google Scholar]
- 35.Moletta L, Pierobon ES, Capovilla G, Costantini M, Salvador R, Merigliano S, et al. International guidelines and recommendations for surgery during Covid-19 pandemic: a Systematic Review. Int J Surg. 2020;79:180–188. doi: 10.1016/j.ijsu.2020.05.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Updated Intercollegiate General Surgery Guidance on COVID-19 — Royal College of Surgeons n.d. Available at: https://www.rcseng.ac.uk/coronavirus/joint-guidance-for-surgeons-v2/. 2021.
- 37.Mitura K, Myśliwiec P, Rogula W, Solecki M, Furtak JP, Kazanowski M, et al. Guidelines for the management of surgical departments in non-uniform hospitals during the COVID-19 pandemic. Pol Prz Chir Polish J Surg. 2020;92:42–53. doi: 10.5604/01.3001.0014.1039. [DOI] [PubMed] [Google Scholar]
- 38.Rymarowicz J, Stefura T, Major P, Szeliga J, Wallner G, Nowakowski M, et al. General surgeons’ attitudes towards COVID-19: A national survey during the SARS-CoV-2 virus outbreak. Eur Surg Acta Chir Austriaca. 2020:1–6. doi: 10.1007/s10353-020-00649-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.OECD/European Observatory on Health Systems and Policies . OECD Publishing, Paris/European Observatory on Health Systems and Policies; Brussels: 2019. Poland: country health profile 2019, state of health in the EU. [Google Scholar]
- 40.Meng L, Huang J, Qiu F, Sun S. Roles of the Chinese clinical pharmacist during the COVID-19 pandemic. J Am Coll Clin Pharm. 2020;3:866–868. doi: 10.1002/jac5.1274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liao Y, Ma C, Lau AH, Zhong M. Role of pharmacists during the COVID-19 pandemic in China - Shanghai experiences. J Am Coll Clin Pharm. 2020;10 doi: 10.1002/jac5.1288. 1002/jac5.1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bukhari N, Rasheed H, Nayyer B, Babar ZUD. Pharmacists at the frontline beating the COVID-19 pandemic. J Pharm Policy Pract. 2020;13 doi: 10.1186/s40545-020-00210-w. [DOI] [PMC free article] [PubMed] [Google Scholar]