Abstract
Intrusion is the most severe luxation injury type, which results in both soft and hard tissue damage. In severe intrusions, the crown must be re-positioned in the arch to avoid periapical pathology and marginal bone loss. There is minimal information about the effect of treatment delay on pulpal and periodontal healing in intrusion trauma. The present paper reports on two cases of severe intrusive luxation applied late at different times treated with surgical extrusion. The first patient, an 11-year-old female, referred to Tokat GOP pediatric dentistry clinic three days after the intrusion tooth 21. The second patient, a 13-year-old male, referred to our clinic fifteen days after a traffic accident. The intruded teeth were positioned surgically and splinted. Surgical extrusion should be preferred as soon as possible to initiate root canal treatment in teeth, the crown of which is fully embedded in the alveolar bone.
Keywords: Delay treatment, intrusion, splint, surgical extrusion
HIGHLIGHTS.
Healing of severe intruded teeth re-positioned was not influenced by the delay in treatment in three weeks.
Intruded teeth must be re-positioned within the first three weeks after injury to avoid the difficulty of bone remodeling.
Surgical extrusion of teeth can be preferable than orthodontic extrusion due to its disadvantages, such as prolonged treatment duration in low cooperation with a dentist.
INTRODUCTION
Injuries to the periodontal tissues are classified into five groups based on treatment and healing; concussion, subluxation, extrusion, lateral luxation, and intrusion (1, 2). One of the most severe dental trauma types amongst these groups is intrusion, which is defined as the displacement of the tooth into the alveolar bone. Treatment and prognosis of intrusive dental traumas vary by patient age, dentition type, root development, time from trauma, and the severity of trauma (2, 3). Nowadays, the treatment of traumatic injuries in the permanent teeth may include waiting for spontaneous eruption if the amount of intrusion is less than 3 mm in teeth with open apex; orthodontic re-positioning if it is between 3-7 mm, and orthodontic/surgical re-position if it is more severe than 7 mm (4-6).
In intruded teeth with mature apex, the use of orthodontic/surgical re-position methods is preferred (2, 6). After treatment, the pulp may have maintained its vitality in teeth with open apex, while the possible outcome is pulp necrosis in teeth with closed apex. In periodontal tissue, infection and ankylosis-related resorption are one of the most common findings. Serious complications such as ankylosis may occur even 5-10 years after trauma (4).
All trauma injuries need to be urgently treated to ensure patient comfort and reduce wound healing complications. Depending on the type of trauma or the interest of the individual/caregiver, application times may not always applied at the ideal time. Treatment in trauma within the first 24 hours is called early intervention, after-treatment is called delayed intervention. There is minimal information about the effect of treatment delay on pulpal and periodontal healing in dental traumas. The present paper reports on two cases of severe intrusive luxation applied late at different times treated with surgical extrusion and one year follow-up.
CASE PRESENTATION
Case 1
A Turkish 11-year-old female patient suffered from falling, and referred to Tokat GOP pediatric dentistry clinic three days after trauma. Clinically, the cooperation level of the child with the dentist was low and had poor oral hygiene. Intraoral examination showed that tooth 21 was intruded into the alveolar socket (Fig. 1). It was also observed that there was a complicated crown fracture in tooth 21. The cemento-enamel junction of intruded tooth 21 is located more 6 mm apically than in adjacent non-injured tooth 11 and 22. Radiographs confirmed a completed root formation in tooth 21, and periodontal space was absent (Fig. 2).
Figure 1.

Intraoral photograph showing posttraumatic injury (Case 1)
Figure 2.

Radiographic image showing the posttraumatic intrusion of tooth 21 (Case 1)
At the first appointment, pulp sensitivity of all anterior teeth was evaluated with an electric pulp test. Teeth 13, 12, 22, and 23 responded positively; only tooth 11 gave a late positive response. The patient and her parents were informed about treatment options and the expected prognosis of each procedure.
Given that the tooth apex was closed and the intrusion was approximately 7 mm, it was decided to perform surgical re-positioning. After the administration of local anesthesia, the surgical re-positioning procedure was completed by loosening the tooth in the socket by using a dental extracting forceps to extrude it and then stabilizing it through suture and fiber splint after being positioned according to the adjacent tooth (Fig. 3). Augmentin (400 mg, 2*1,5), a penicillin-derived antibiotic, a mouthwash containing chlorhexidine, and Parol, an analgesic agent, were prescribed for 7 days against the risk of pain and infection. Eating habits and oral hygiene maintenance were instructed to the patient and her parents.
Figure 3.

A photograph showing tooth 21 after surgical extrusion (Case 1)
Three days after the surgery, the root canal treatment for tooth 21 was initiated, the pulp tissue was removed and was irrigated with 2.5% sodium hypochloride (Cerkamed). The root canal was filled with calcium hydroxide for 15 days. Before removing splint, the root canal treatment for tooth 21 was completed with gutta-percha. Tooth 11 gave a negative response to the vitality test and was done root canal treatment, too. Aesthetic restoration of the tooth 21 was performed (Fig. 4). 4 weeks after the surgery, the splint was removed, and a follow-up radiograph was taken. In the first month after surgical reposition, the patient was called for clinical examinations at first, second and fourth weeks. Clinical and radiographic images of the treatment condition were examined in months 3, 6, 9 and 12. In follow up sessions, clinically, there were no clinical symptoms such as mobility, sensitivity, periodontal bleeding, periodontal pocket, and colour change. The radiographic examination revealed the absence of a periapical lesion and inflammatory root resorption of the treated teeth (Figs. 5, 6).
Figure 4.

Photographic image after final restoration (Case 1)
Figure 5.

Radiographic image - One year follow up (Case 1)
Figure 6.

Intra-oral photographic image - one year follow up (Case 1)
Case 2
A Turkish 13-year-old boy was referred to our clinic fifteen days after a car accident. Clinically, the cooperation level of the child with the dentist was high, but oral hygiene was poor. After assessing medical history, the patient was examined for extraoral signs. He had no facial swelling, facial asymmetry, limited mouth opening, and pain on palpation. Intraoral examination revealed severe intrusive luxation in tooth 12 and moderate intrusive luxation in tooth 11. The tooth 11 was not mobile and did not interfere with the occlusion (Fig. 7). The patient was in the mixed dentition, had a deep bite, and tooth 13 was still erupting.
Figure 7.

Intra-oral photograph showing posttraumatic injury (Case 2)
At the first appointment, pulp sensitivity of all anterior teeth was evaluated with an electric pulp test. Teeth 21 and 22 gave positive responses, while teeth 11 and 13 gave negative responses. Radiographs confirmed a complete root formation in all permanent anterior teeth, and periodontal space was absent (Fig. 8). Given that multiple severe luxation traumas, it was decided to perform surgical re-positioning. A photograph was requested from the family to see the anterior teeth positions. The patient and his parents were informed about treatment options and the expected prognosis of each procedure.
Figure 8.

Posttraumatic radiographic image of teeth 11 and 12 (Case 2)
The difficulties encountered during surgery were i) reaching stability after re-positioning in adjacents multiple luxation teeth on the arch; ii) re-positioning of intruded teeth 11 and 12 in the alveolar socket due to the start of remodeling in the bone in 15 days. The teeth 11 and 12 were surgically extruded and stabilized in a position similar to the symmetrical teeth by 0.5 mm stainless steel splint (Fig. 9). Because the tooth 13 continued erupting, it was left to the spontaneous eruption and not included in the splint.
Figure 9.
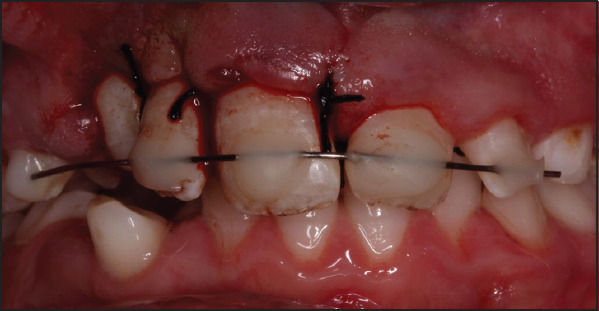
Photographic image showing teeth after surgical extrusion (Case 2)
After surgery, Augmentin (625 mg, 2*1), a penicillin-derived antibiotic, a mouthwash containing chlorhexidine, Parol, an analgesic agent, were prescribed for 7 days to the patient against the risk of pain and infection. Eating habits and vigorous oral hygiene maintenance were instructed to the patient and his parents.
One week after the surgery, the root canal treatment for teeth 11 and 12 was initiated, the pulp tissue was removed and was irrigated with 2.5% sodium hypochloride (Cerkamed). The root canal was filled with calcium hydroxide for 15 days. The root canal treatment of teeth 11 and 12 of the patient was completed without removal of the splint after four weeks (Fig. 10). Tooth 13 was also scheduled for root canal treatment because it was non-vital. In the first month after surgical reposition, the patient was called for clinical examinations at first, second and fourth weeks. Clinical and radiographic controls of the treatment condition were examined in months 3, 6, 9 and 12. In control sessions, clinically, there were no clinical symptoms such as mobility, sensitivity, periodontal bleeding, periodontal pocket, and colour change. The radiographic examination revealed the absence of a periapical lesion and inflammatory root resorption of the treated teeth (Figs. 11, 12).
Figure 10.

Intra-oral photograph showing teeth after final restoration (Case 2)
Figure 11.

Radiographic image showing one year follow up (Case 2)
Figure 12.

Intra-oral photograph showing teeth after one year follow up (Case 2)
DISCUSSION
Three current treatment modalities for permanent intruded teeth are spontaneous eruption, surgical extrusion, and orthodontic extrusion. The choice of treatment depends on the degree of intrusion and the degree of root development. For moderate intrusions between 3 and 6 mm, surgical or orthodontic re-positioning is recommended, and for severe intrusion (greater than 6 mm), surgical re-positioning is recommended (2, 7, 8). To provide evidence-based treatment, certain pre-traumatic and trauma factors must be incorporated to choose treatment alternatives.
The essential criteria in treatment selection of intrusion are the root development stage and intrusion degree. Besides, the critical period in intrusion injuries is the first 2-3 weeks (2, 7-10). If root canal treatment is not initiated during these weeks, external root resorption may occur. The primary reason why we chose surgical extrusion as a treatment option was that it could allow rapid positioning (11) to initiate root canal treatment in which the tooth was totally embedded in the alveolar bone in late applied cases. Also, the second case was presented with teeth of multiple intrusion injuries and, re-positioning by surgical extrusion in the first three weeks after trauma is recommended. However, many difficulties were experienced in re-positioning teeth in the second case because bone remodeling was initiated because of the long time passed after trauma and reaching splint stability in the arch was more difficult than first case because there was be many neighbouring tooth luxation in second case. Surgical extrusions may cause a secondary trauma, especially when applied in intrusion injuries with delayed treatment, and this may lead to marginal bone resorptions (12). In our cases, such a condition was not experienced after a one-year follow-up.
The success of the intrusion cases depends on the time of pulp extirpation, filling of root canals, and splinting duration (2, 13). Splinting should be performed so that it would not affect physiological tooth movement, and the splinting duration should be kept short to prevent ankylosis of teeth. In the study carried out by Berude et al. (14), periodontal healing of teeth to which no splint, semi-rigid splint, or rigid splint was applied was evaluated, and it was reported that there was no significant difference between these three types (15). It was reported that fiber splint showed optimum success in periodontal tissue healing, while in stainless steel-composite splints, mobility decreased with an increasing thickness (16). In our first case, tooth 21 was surgically extruded, and fiber splint was applied from tooth 13 to tooth 24 for the four-week period. In the second case, 0.5 mm stainless steel wire splint was applied from tooth 14 to tooth 22 after surgical extrusion because of the presence of multiple traumatic injuries, and the long time passed since the trauma.
Since the incidence of pulp necrosis in teeth with closed root apex was reported to be 96%, it is recommended to perform root canal treatment as soon as possible to prevent inflammatory root resorption (6). Calcium hydroxide is commonly used in root canals due to its advantages, such as being an antibacterial agent, preventing bacterial growth in the root canal, and preventing the occasion of root resorptions (17). The International Association of Dental Traumatology reported that the canals should be kept in calcium hydroxide until root canal filling, especially in luxation injuries. Calcium hydroxide that is applied as a medicament into the canal after a trauma prevents possible internal resorptions and infection-related root resorption (18, 19). We used calcium hydroxide as an intra-canal medicament in an intermediate session of our cases to benefit from its antibacterial effect.
CONCLUSION
Treatment of intrusion injuries should be planned according to factors such as the severity of the trauma, application time, dental period, and degree of cooperation in patients. Surgical extrusion should be preferred as soon as possible to initiate root canal treatment in teeth, the crown of which is fully embedded in the alveolar bone.
Footnotes
Informed consent: Written informed consent was obtained from the patient for the publication of the case report and the accompanying images.
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
Ethics Committee Approval: No ethical appointment.
Peer-review: Externally peer-reviewed.
Financial Disclosure: No financial support is received in this article.
Authorship contributions: Concept – M.B., H.A.; Design – M.B., H.A.; Supervision – H.A.; Funding - None; Materials - A.A., M.B.; Data collection &/or processing – A.A., M.B.; Analysis and/or interpretation – M.B.; Literature search – M.B., H.A.; Writing – M.B.; Critical Review – H.A.
REFERENCES
- 1.Yanar NÖ. Treatment of traumatized central teeth with extrusion:A case report. Selcuk Dent J. 2014;1(3):129–33. [Google Scholar]
- 2.Andreasen JO, Bakland LK, Andreasen FM. Traumatic intrusion of permanent teeth Part 3. A clinical study of the effect of treatment variables such as treatment delay method of repositioning type of splint length of splinting and antibiotics on 140 teeth. Dent Traumatol. 2006;22(2):99–111. doi: 10.1111/j.1600-9657.2006.00423.x. [DOI] [PubMed] [Google Scholar]
- 3.Güngör HC, Cengiz SB, Altay N. Immediate surgical repositioning following intrusive luxation:a case report and review of the literature. Dent Traumatol. 2006;22(6):340–4. doi: 10.1111/j.1600-9657.2005.00356.x. [DOI] [PubMed] [Google Scholar]
- 4.Kirzioğlu Z, Karayilmaz H. Repositioning of a completely intruded permanent incisor with surgical extrusion:a 4-year follow-up case. Pediatr Dent. 2009;31(3):253–6. [PubMed] [Google Scholar]
- 5.Yeşilöz E, Doğan S, Öz FT. Three case reports:Intrusion treatment. Atatürk Üniv DişHek Fak Derg. 2012;22(3):293–7. [Google Scholar]
- 6.Diangelis AJ, Andreasen JO, Ebeleseder KA, Kenny DJ, Trope M, Sigurdsson A, et al. International Association of Dental Traumatology. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries:1. Fractures and luxations of permanent teeth. Dent Traumatol. 2012;28(1):2–12. doi: 10.1111/j.1600-9657.2011.01103.x. [DOI] [PubMed] [Google Scholar]
- 7.Kinirons MJ. UK national clinical guidelines in paediatric dentistry:Treatment of traumatically intruded permanent incisor teeth in children. Int J Paediatr Dent. 1998;8:165–8. doi: 10.1111/j.1365-263X.2010.01085.x. [DOI] [PubMed] [Google Scholar]
- 8.Faria G, Silva RA, Fiori-Júnior M, Nelson-Filho P. Re-eruption of traumatically intruded mature permanent incisor:case report. Dent Traumatol. 2004;20(4):229–32. doi: 10.1111/j.1600-9657.2004.00237.x. [DOI] [PubMed] [Google Scholar]
- 9.Oulis C, Vadiakas G, Siskos G. Management of intrusive luxation injuries. Endod Dent Traumatol. 1996;12(3):113–9. doi: 10.1111/j.1600-9657.1996.tb00108.x. [DOI] [PubMed] [Google Scholar]
- 10.Shivayogi MH, Anand LS, Dayanand DS. Management of traumatically intruded permanent incisors. J Indian Soc Pedod Prev Dent. 2007;25(Suppl):S13–6. [PubMed] [Google Scholar]
- 11.Mazumdar D, Roy P, Kumar P. Management of intrusive luxation with immediate surgical repositioning. J Conserv Dent. 2009;12(2):69–72. doi: 10.4103/0972-0707.55621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Andreasen JO, Andreasen FM. Essentials of Traumatic Injuries to the Teeth:A Step-by-Step Treatment Guide. Second Edition. Copenhagen: Munksgaard; 2000. pp. 9–20. [Google Scholar]
- 13.Calişkan MK. Surgical extrusion of a completely intruded permanent incisor. J Endod. 1998;24(5):381–4. doi: 10.1016/S0099-2399(98)80140-4. [DOI] [PubMed] [Google Scholar]
- 14.Berude JA, Hicks ML, Sauber JJ, Li SH. Resorption after physiological and rigid splinting of replanted permanent incisors in monkeys. J Endod. 1988;14(12):592–600. doi: 10.1016/S0099-2399(88)80056-6. [DOI] [PubMed] [Google Scholar]
- 15.Ebeleseder KA, Santler G, Glockner K, Hulla H, Pertl C, Quehenberger F. An analysis of 58 traumatically intruded and surgically extruded permanent teeth. Endod Dent Traumatol. 2000;16(1):34–9. doi: 10.1034/j.1600-9657.2000.016001034.x. [DOI] [PubMed] [Google Scholar]
- 16.Altan H, Coşgun A. Splint types used in trauma patients in pediatric dentistry removal. Atatürk Üniv DişHek Fak Derg. 2016;26:4. [Google Scholar]
- 17.Mohammadi Z, Dummer PM. Properties and applications of calcium hydroxide in endodontics and dental traumatology. Int Endod J. 2011;44(8):697–30. doi: 10.1111/j.1365-2591.2011.01886.x. [DOI] [PubMed] [Google Scholar]
- 18.Chan AW, Cheung GS, Ho MW. Different treatment outcomes of two intruded permanent incisors-a case report. Dent Traumatol. 2001;17(6):275–80. doi: 10.1034/j.1600-9657.2001.170606.x. [DOI] [PubMed] [Google Scholar]
- 19.Karakaya E, Aksoy M, Kıvrak A, Öz FT. Revascularization of Traumatically Intruded and Subluxated Immature Permanent Incisors:A Case Report A.Ü. DişHek Fak Derg Special Issue 2018 [Google Scholar]


