Abstract
Objective:
The purpose of this randomized, double-blind study was to evaluate the anesthetic efficacy of lidocaine-ketorolac administration by Inferior Alveolar Nerve Block (IANB) in patients with irreversible pulpitis.
Methods:
Eighty-eight adult patients received a combination of either one cartridge of “2% lidocaine with 1:80.000 epinephrine” (Li) plus one cartridge of a mixture of 0.8 mL of the same solution and 1mL ketorolac tromethamine (KT)(30 mg/mL), or one cartridge of Li solution plus one cartridge of a mixture of the same solution and saline. Endodontic access was prepared after fifteen minutes. Anesthetic success was defined as no or mild pain [less than 54 mm on the Heft-Parker visual analog scale (HP-VAS)] during access cavity preparation and initial file insertion. Chi-square test was used for data analysis, and the level of significance was set at 0.05 (P=0.05).
Results:
Results showed that the success rates were 34.1% and 27.3% for Li-KT and Li-Saline groups, respectively, with no significant difference between the two groups (P=0.48). However, significant decrease of baseline mean VAS pain score of the participants in both groups was found during access cavity preparation or initial file insertion (P<0.05).
Conclusion:
Mixed Li-KT solution did not increase the success rate of IANB injection significantly.
Keywords: Inferior alveolar nerve block, irreversible pulpitis, ketorolac, iidocaine
HIGHLIGHTS.
Owing to the fact that achieving profound local anesthesia is necessary in dentistry, various approaches have been examined in order to increase the success rate of local anesthesia.
Anesthetizing inferior alveolar nerve, which innervates all mandibular teeth, is a challenge for dentists, with only 70% success rate in blocking this nerve.
Inflammatory condition, which is observed in irreversible pulpitis, increases the unsuccessful nerve block rate. The aim of this study was to evaluate the effect of combined KT and Li on IANB. However, the results of this study showed this combination did not increase the success rate of IANB, so further research is required to shed more light on this area of research.
INTRODUCTION
Inferior Alveolar Nerve Block (IANB) is the most common injection technique for achieving pulpal anesthesia in mandibular teeth. However, it has a high failure rate, especially in patients with irreversible pulpitis (1-4). This can be attributed to various mechanisms, including increased local vascularity and possible loss of anesthetic solution via sinus drainage, expression of sodium channels resistant to the local anesthetic effects, and decreased local pH. The inflammation process can lead to allodynia and hyperalgesia, commonly observed in irreversible pulpitis, and profound anesthetic failure (5, 6). Further, another reason for the failure of anesthesia is the altered response of peripheral nociceptors in the presence of inflammatory mediators such as Prostaglandins (PGs) (5). PGs are the end-products of arachidonic acid (AA) metabolism via the Cyclo-Oxygenase (COX) pathway (5, 7). PGs sensitize the nociceptors and reduce their activation threshold. In addition, the inflammatory mediators increase the activity of tetrodotoxin-resistant sodium channels, thus reducing the efficacy of the local anesthetic solution.
Non-steroidal anti-inflammatory drugs (NSAIDs) have a prohibitory role in the PG synthesis by inactivating the COX enzyme pathway (8, 9). Moreover, NSAIDs such as ketorolac can affect the central pathways of PG-modulated nociception (8-10). Deposition of NSAIDs near the inflamed nerve appears to be a logical method to reduce the PG synthesis and improve the anesthetic success rate. Few studies investigated this approach and reported an increased success rate of IANB in patients with irreversible pulpitis receiving buccal infiltrations of KT and articaine (1, 2). The addition of KT to Li for local anesthesia in different medical procedures has shown to provide a longer duration and better quality of analgesia (11-13). To the best of our knowledge, no study has investigated the effect of KT and Li combination on IANB. Although the traditionally accepted site of action for NSAIDs is nerve terminals by blocking the peripheral synthesis of PGs, researchers have recently reported evidence for a more central action of these agents (13). Keeping these in mind, the aim of this study was to evaluate the anesthetic efficacy of combined KT and Li, administered by IANB injection, in patients with irreversible pulpitis.
MATERIALS AND METHODS
The Ethical Committee of Dental Faculty approved the trial protocol with ID number “IR.MUI.RESEARCH.REC.1397.285”. Written informed consent was taken from all the participants. Sample size calculation was performed based on a previous study by Saatchi et al. (14). With a two-sided alpha risk of 0.05, a sample size of 44 subjects per group was required to detect a difference of 30 percentage points in anesthetic success with a power of more than 0.80.
The primary outcome was defined as “success or failure”. The treatment was considered successful if the clinician was able to undertake access cavity preparation and initial file insertion with no or mild pain. Eighty-eight healthy patients aged 18-60 years participated in this prospective, randomized, double-blind study (Fig. 1). The patients attended the endodontic department of Isfahan Dental School and required emergency treatment. The socio-economic status of the patients was estimated to be low to moderate based on the data extracted from their charts. After taking preoperative radiographs, the subjects were assessed based on the following inclusion criteria: moderate to severe pain in a carious-exposed mandibular molar, >54 mm on Heft-Parker Visual Analogue Scale (HP-VAS) (15), prolonged response to thermal sensitivity tests with an ice stick, and vital pulp on coronal access opening. Patients with a periapical lesion, except for a widened periodontal ligament space, were not included in the study. The exclusion criteria were allergy, sensitivity, or contraindications to NSAIDs, history of active peptic ulcer within the past 12 months, history of bleeding problems or anticoagulant use within the last month, patients who were pregnant or breastfeeding, and patients who were taking any drugs that could have affected the pain perception.
Figure 1.
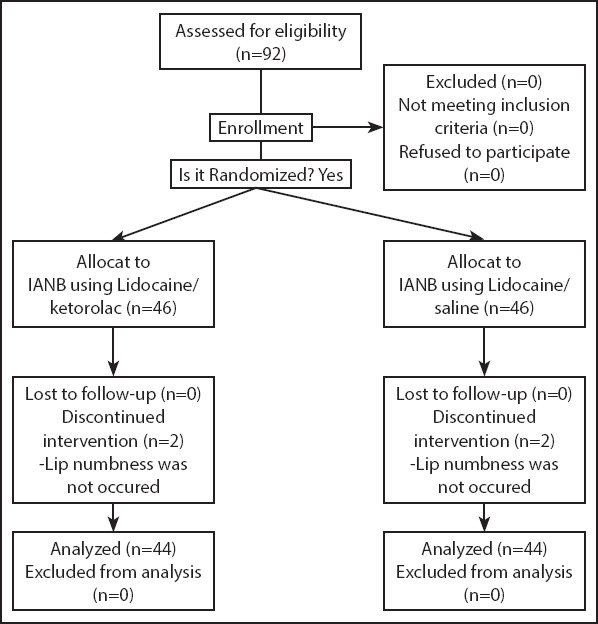
Study flow diagram
The patients were instructed by one of the investigators (H.F) to rate their pretreatment pain and any pain felt during the procedure on a 170-mm HP-VAS. This scale is a 170-mm horizontal line divided into four categories. No pain corresponded to 0 mm and mild pain was defined as >0 mm and ≤54 mm. The mild pain category included faint, weak, and mild pain. A score >54 mm and <114 mm indicated moderate pain and included the descriptor of moderate pain. Severe pain was defined as ≥114 mm. The patients were randomly allocated to two treatment groups using an online permuted block randomization protocol (randomization.com). Every patient received two anesthetic cartridges aqdministered by a single dentist (A.Kh). In the first group, patients received an IANB injection of 1.8 mL of 2% Li containing 1:80000 epinephrine (Li) (Darupakhsh, Tehran) using a self-aspirating syringe and 27-gauge long needles (Nik Rahnama Kar Co, Tehran). Immediately after the first injection, another cartridge containing a mixture of Li solution and KT (30 mg/mL, Exir pharmaceutical Company, Boroojerd) was injected using the same technique by the same operator. A trained dental pharmacologist prepared the cartridge immediately before the injections. A total of 1 mL of the anesthetic solution was drawn via an insulin syringe from the Li cartridge and replaced by 1mL of KT solution (30 mg/mL) that was slowly injected into the cartridge under sterile conditions. The syringe was inverted ten times to mix the solution, and the absence of any precipitation was confirmed. An alpha-numeric code was written on the cartridges. The operator and the patients were blinded to the content of the cartridges. The code was broken at the end of the study. The patients were asked to report any circumstance of severe intolerable injection pain.
The patients in the second group received IANB injection as described for the first group by the same operator. The second cartridge was prepared immediately before administration by mixing Li with 1mL normal saline. Further, no additional supplementary injection was applied. The total dose of KT each patient received in the first group was 30 mg and the total dose of Li all patients received was 56 mg.
Fifteen minutes after the injections, the patients were asked for the lip numbness. If the lip numbness was not achieved, the IANB was regarded as missed and the patient was excluded (two patients in each group) and replaced by another patient to reach the calculated sample size. The same clinician prepared access cavities by means of a #4 diamond round bur with a high-speed hand piece after isolation by a rubber dam. Then, #15 K-files as initial files were inserted into the root canals, and a periapical radiograph was taken to determine the root canal length. Patients were instructed to report any pain they experienced during these two procedures. In case of pain during access cavity preparation or initial file insertion to reach the estimated root canal length, the procedure was stopped and patients were asked to rate the pain on HP-VAS. The success of the IANB was defined as no or mild pain experience (HP-VAS score ≤54).
The root canal preparation was continued by the step-back technique using hand K-files. Working length was measured 0.5 mm short of the radiographic apex, and 5.25% sodium hypochlorite solution was used for irrigation of the root canals followed by instrumentation, root canal filling and coronal restoration.
Statistical analysis
Initial patient/tooth characteristics were fed into SPSS 23.0 (SPSS Inc. IL, USA) for statistical evaluation. The subjects’ age was summarized by calculating the means and standard deviations. Independent t-tests were used to determine significant differences between age and HP-VAS scores. Differences in the tooth type, sex and, anesthetic success of the two groups were compared by the chi-square test. The significance level was set at 0.05 (P=0.05).
RESULTS
Eighty-eight adult patients, 42 women and 46 men, aged 18-60 years participated in this clinical trial. Table 1 shows the distribution of the study population on the basis of sex, mean age, and tooth type. There was no statistically significant difference between the two groups in these variables.
TABLE 1.
Patient/tooth characteristics of the study groups
| Li+KT | Li+Saline | P | |
|---|---|---|---|
| Age (year), mean±SD | 30.8±10.2 | 32.8±9.9 | 0.35 |
| Sex | |||
| Female, n (%) | 20 (45) | 26 (59) | 0.20 |
| Male, n (%) | 24 (55) | 18 (41) | |
| Tooth type | |||
| First Molar, n (%) | 36 (81.8) | 37 (84.1) | 0.69 |
| Second Molar, n (%) | 8 (18.2) | 7 (15.9) |
SD: Standard deviation, There was no significant difference (P>0.05) between the groups
The comparisons of mean HP-VAS scores before and during treatment between the two groups as well as the percentage of patients with successful anesthesia (no pain or weak/mild pain during endodontic access preparation and initial file insertion) are presented in Tables 2 and 3, respectively. No statistically significant difference was observed between groups (P>0.05). However, significant decrease of baseline mean VAS pain score of the participants in both groups was found during access cavity preparation or initial file insertion (P<0.05).
TABLE 2.
Inter- and Intra- group comparisons of mean HP-VAS score before and during treatments (access cavity preparation or initial file insertion)
| Li+KT | Li+Saline | P | |
|---|---|---|---|
| Mean HP-VAS scores before treatment mm±SD | 105.2±38.7 | 109.6±35.6 | 0.58 |
| Mean HP-VAS scores during treatment mm±SD | 57.5±28.5 | 70.2±44.9 | 0.14 |
| P value | <0.01 | <0.01 |
There was no significant inter- or intra- group differences (P>0.05) (t-test)
TABLE 3.
Comparison of percentage of successful anesthesia between control and test groups
| Li+KT | Li+Saline | P | ||
|---|---|---|---|---|
| Successful anesthesia | 34.1% (15 of 44 patients) | 27.3% (12 of 44 patients) | 0.48 |
There was no significant difference (Chi-Square, P=0.48) between the groups
DISCUSSION
Achieving profound pulpal anesthesia is a common clinical problem, particularly in patients with irreversible pulpitis (16). A systematic review of the literature indicated that preoperative oral administration of NSAIDs can induce superior intraoperative analgesia in patients with irreversible pulpitis (17). Clinical studies in medicine demonstrated an enhanced anesthetic effect of NSAIDs when injected at a peripheral site, and promising reports are available for the epidural and intraarticular administration of indomethacin and ketorolac (18). Reinhart (13) reported that addition of KT to Li for ankle block contributed to longer duration of anesthesia as well as longer time of the first reported pain and intake of the first oral pain medications after foot surgery compared with plain 1.73% Li.
Results of the present study showed that addition of KT to Li solution did not improve the success rate of Li in IANB. Studies evaluated the effect of supplemental KT administered through oral, intra-nasal, and submucosal infiltration pathways on the success rate of IANB in patients with irreversible pulpitis (1, 5, 19-23). Consistent with the results of the current study, Stentz (23) reported that “premedication with intranasal KT did not significantly increase the odds of success for the IANB over the use of nitrous oxide/oxygen alone”. The reported success rate of IANB was 46% for intranasal saline/nitrous oxide and 54% for intranasal KT/nitrous oxide groups. Saha et al. (22) used 10 mg oral KT in 42 patients and reported 76% success rate for IANB. The different route of KT administration as well as the longer waiting time before treatment initiation may explain the higher success rate of IANB in Saha’s study. In addition, the HP-VAS score of initial pain presentation was 86 mm in that study compared with 105-109 mm of the present study. It is assumed that the lower initial pain in the sample population resulted in a higher success than that of the present investigation. Aggarwal et al. (5) reported 39% and 27% success rates for IANB by oral KT versus oral ibuprofen as premedication, respectively. The results of this study revealed that KT and ibuprofen did not increase the success rate of IANB significantly compared to the placebo with 29% success rate. In another study, Aggarwal et al. (1) evaluated the effect of articaine and articaine plus KT buccal infiltration on the success rate of IANB. The authors concluded that “articaine and articaine plus KT infiltration can increase the success rate of IANB in patients with irreversible pulpitis”. The authors argued that, due to the severe injection pain after the infiltration of KT (without prior injection of articaine) experienced by the first two patients, they had to inject articaine before KT. The control group’s success rate of 39% significantly increased to 54% and 62% in articaine and articaine plus KT groups, respectively. Furthermore, Akhlaghi et al. (2) reported an increase in the success rate of IANB anesthesia by KT buccal infiltration after IANB and buccal infiltration of articaine. The success rate of IANB increased from 15% in the control group to 40% in the KT group.
Unlike previous studies (1, 24), none of the patients in this trial experienced severe injection pain after KT+Li injection. This can be attributed to various reasons. Although the first Li injection may have decreased the pain of KT+Li injection by numbness of the injection site, soft tissue discomfort varies in different areas of the mouth (25). We used KT+Li in IANB site, while previous studies have administered KT as a buccal infiltration. Additionally, mixing KT with Li may decrease the injection pain. Injection pain can be greatly reduced by administering drugs in combination with local anesthetics like Li. Some studies have assessed the use of Li as a diluent to reduce the injection pain (26). Although we did not find a study on using Li as a diluent for KT, Patel et al. (27) reported that diluting ceftriaxone with Li considerably decreased the pain intensity and frequency at the injection site.
To ensure blindness, the patients in the second group received Li mixed with normal saline. Moreover, the addition of KT to Li decreased the total concentration of Li. Thus, the need for an extra injection to provide a sufficient volume of Li for anesthesia was inevitable in this study, and can be considered a limitation. None of the side effects of KT were observed in this study. However, KT should be used with caution in patients with renal or hepatic dysfunction.
CONCLUSION
The addition of KT 30 mg/mL to a lidocaine solution administered in an IANB injection for mandibular posterior teeth with irreversible pulpitis did not improve the success rate compared with a Li solution mixed with normal saline. Future research is required to improve the success rate of IANB in patients with irreversible pulpitis.
Footnotes
Conflict of Interest: Authors declared no conflict of interest.
Ethics Committee Approval: The ethical committee of dental faculty approved the trial protocol with ID number “IR.MUI.RESEARCH.REC.1397.285”. The project was found to be in accordance to the ethical principles and the national norms and standards for conducting medical research in Iran.
Peer-review: Externally peer-reviewed.
Financial Disclosure: This study was supported by the Isfahan University of Medical Sciences, School of Dentistry. #397425
Authorship contributions: Concept – H.F., R.F., A.K., V.A.; Design – H.F., R.F., A.K., V.A.; Supervision – H.F., R.F., A.K., V.A.; Funding - H.F., A.K.; Materials - H.F.; Data collection &/or processing – R.F.; Analysis and/or interpretation – R.F., V.A.; Literature search – H.F., R.F.; Writing – H.F., R.F., A.K., V.A.; Critical Review – R.F., H.F.
REFERENCES
- 1.Aggarwal V, Singla M, Rizvi A, Miglani S. Comparative evaluation of local infiltration of articaine articaine plus ketorolac and dexamethasone on anesthetic efficacy of inferior alveolar nerve block with lidocaine in patients with irreversible pulpitis. J Endod. 2011;37(4):445–9. doi: 10.1016/j.joen.2011.01.016. [DOI] [PubMed] [Google Scholar]
- 2.Akhlaghi NM, Hormozi B, Abbott PV, Khalilak Z. Efficacy of Ketorolac Buccal Infiltrations and Inferior Alveolar Nerve Blocks in Patients with Irreversible Pulpitis:A Prospective Double-blind, Randomized Clinical Trial. J Endod. 2016;42(5):691–5. doi: 10.1016/j.joen.2016.02.003. [DOI] [PubMed] [Google Scholar]
- 3.Oleson M, Drum M, Reader A, Nusstein J, Beck M. Effect of preoperative ibuprofen on the success of the inferior alveolar nerve block in patients with irreversible pulpitis. J Endod. 2010;36(3):379–82. doi: 10.1016/j.joen.2009.12.030. [DOI] [PubMed] [Google Scholar]
- 4.Prasanna N, Subbarao CV, Gutmann JL. The efficacy of pre-operative oral medication of lornoxicam and diclofenac potassium on the success of inferior alveolar nerve block in patients with irreversible pulpitis:a double-blind randomised controlled clinical trial. Int Endod J. 2011;44(4):330–6. doi: 10.1111/j.1365-2591.2010.01833.x. [DOI] [PubMed] [Google Scholar]
- 5.Aggarwal V, Singla M, Kabi D. Comparative evaluation of effect of preoperative oral medication of ibuprofen and ketorolac on anesthetic efficacy of inferior alveolar nerve block with lidocaine in patients with irreversible pulpitis:a prospective double-blind, randomized clinical trial. J Endod. 2010;36(3):375–8. doi: 10.1016/j.joen.2009.11.010. [DOI] [PubMed] [Google Scholar]
- 6.Monteiro MR, Groppo FC, Haiter-Neto F, Volpato MC, Almeida JF. 4% articaine buccal infiltration versus 2% lidocaine inferior alveolar nerve block for emergency root canal treatment in mandibular molars with irreversible pulpits:a randomized clinical study. Int Endod J. 2015;48(2):145–52. doi: 10.1111/iej.12293. [DOI] [PubMed] [Google Scholar]
- 7.Goodchild JH, Donaldsın M, Conte NR. Mitigating Post-Operative Dental Pain:as easy as 1, 2,, 4, 24. [Accessed Aug 28 2020]. Available at: http://djph.delamed.org/V3_I4/OP012.pdf . [DOI] [PMC free article] [PubMed]
- 8.Madani ZS, Moghadamnia AA, Panahi A, Poorsattar Bejeh Mir A. Analgesic effect of etoricoxib compared to ibuprofen on post endodontic pain. Oral Health Dent Manag. 2013;12(3):186–90. [PubMed] [Google Scholar]
- 9.Cohen S, Burns RC, Walton R, Torabenijad M. Pathways of the Pulp (1) Learning. 1998;30:10. [Google Scholar]
- 10.Ong KS, Tan JM. Preoperative intravenous tramadol versus ketorolac for preventing postoperative pain after third molar surgery. Int J Oral Maxillofac Surg. 2004;33(3):274–8. doi: 10.1006/ijom.2003.0515. [DOI] [PubMed] [Google Scholar]
- 11.Jankovic RJ, Visnjic MM, Milic DJ, Stojanovic MP, Djordjevic DR, Pavlovic MS. Does the addition of ketorolac and dexamethasone to lidocaine intravenous regional anesthesia improve postoperative analgesia and tourniquet tolerance for ambulatory hand surgery? Minerva Anestesiol. 2008;74(10):521–7. [PubMed] [Google Scholar]
- 12.Leow MQH, Chua KS, Tay SC. Mixing local anaesthetics corticosteroid, and ketorolac tromethamine leads to no extreme pH or precipitation. J Hand Surg Eur Vol. 2017;42(9):963–5. doi: 10.1177/1753193417714386. [DOI] [PubMed] [Google Scholar]
- 13.Reinhart DJ, Stagg KS, Walker KG, Wang WP, Parker CM, Jackson HH, et al. Postoperative analgesia after peripheral nerve block for podiatric surgery:clinical efficacy and chemical stability of lidocaine alone versus lidocaine plus ketorolac. Reg Anesth Pain Med. 2000;25(5):506–13. doi: 10.1053/rapm.2000.7624. [DOI] [PubMed] [Google Scholar]
- 14.Saatchi M, Khademi A, Baghaei B, Noormohammadi H. Effect of sodium bicarbonate-buffered lidocaine on the success of inferior alveolar nerve block for teeth with symptomatic irreversible pulpitis:a prospective randomized double-blind study. J Endod. 2015;41(1):33–5. doi: 10.1016/j.joen.2014.09.011. [DOI] [PubMed] [Google Scholar]
- 15.Heft MW, Parker SR. An experimental basis for revising the graphic rating scale for pain. Pain. 1984;19(2):153–61. doi: 10.1016/0304-3959(84)90835-2. [DOI] [PubMed] [Google Scholar]
- 16.Parirokh M, Yosefi MH, Nakhaee N, Abbott PV, Manochehrifar H. The success rate of bupivacaine and lidocaine as anesthetic agents in inferior alveolar nerve block in teeth with irreversible pulpitis without spontaneous pain. Restor Dent Endod. 2015;40(2):155–60. doi: 10.5395/rde.2015.40.2.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shirvani A, Shamszadeh S, Eghbal MJ, Marvasti LA, Asgary S. Effect of preoperative oral analgesics on pulpal anesthesia in patients with irreversible pulpitis-a systematic review and meta-analysis. Clin Oral Investig. 2017;21(1):43–52. doi: 10.1007/s00784-016-1974-1. [DOI] [PubMed] [Google Scholar]
- 18.Christiansson L. Update on adjuvants in regional anaesthesia. Periodicum biologorum. 2009;111(2):161–70. [Google Scholar]
- 19.Aggarwal V, Jain A, Kabi D. Anesthetic efficacy of supplemental buccal and lingual infiltrations of articaine and lidocaine after an inferior alveolar nerve block in patients with irreversible pulpitis. J Endod. 2009;35(7):925–9. doi: 10.1016/j.joen.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 20.Ben-David B, Katz E, Gaitini L, Goldik Z. Comparison of i.m and local infiltration of ketorolac with and without local anaesthetic. Br J Anaesth. 1995;75(4):409–12. doi: 10.1093/bja/75.4.409. [DOI] [PubMed] [Google Scholar]
- 21.Jung IY, Kim JH, Kim ES, Lee CY, Lee SJ. An evaluation of buccal infiltrations and inferior alveolar nerve blocks in pulpal anesthesia for mandibular first molars. J Endod. 2008;34(1):11–3. doi: 10.1016/j.joen.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 22.Saha SG, Jain S, Dubey S, Kala S, Misuriya A, Kataria D. Effect of Oral Premedication on the Efficacy of Inferior Alveolar Nerve Block in Patients with Symptomatic Irreversible Pulpitis:A Prospective Double-Blind, Randomized Controlled Clinical Trial. J Clin Diagn Res. 2016;10(2):ZC25–9. doi: 10.7860/JCDR/2016/16873.7195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stentz D, Drum M, Reader A, Nusstein J, Fowler S, Beck M. Effect of a Combination of Intranasal Ketorolac and Nitrous Oxide on the Success of the Inferior Alveolar Nerve Block in Patients with Symptomatic Irreversible Pulpitis:A Prospective Randomized, Double-blind Study. J Endod. 2018;44(1):9–3. doi: 10.1016/j.joen.2017.09.011. [DOI] [PubMed] [Google Scholar]
- 24.Mellor AC, Dorman ML, Girdler NM. The use of an intra-oral injection of ketorolac in the treatment of irreversible pulpitis. Int Endod J. 2005;38(11):789–94. doi: 10.1111/j.1365-2591.2005.01015_1.x. [DOI] [PubMed] [Google Scholar]
- 25.Meechan JG, Day PF. A comparison of intraoral injection discomfort produced by plain and epinephrine-containing lidocaine local anesthetic solutions:a randomized double-blind, split-mouth volunteer investigation. Anesth Prog. 2002;49(2):44–8. [PMC free article] [PubMed] [Google Scholar]
- 26.Emami AZ, Khezri HD. Can Lidocaine be Safely Used to Reduce Pain Caused by Intramuscular Penicillin Injections?A Short Literature Review. Oman Med J. 2012;27(4):337. doi: 10.5001/omj.2012.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Patel IH, Weinfeld RE, Konikoff J, Parsonnet M. Pharmacokinetics and tolerance of ceftriaxone in humans after single-dose intramuscular administration in water and lidocaine diluents. Antimicrob Agents Chemother. 1982;21(6):957–62. doi: 10.1128/aac.21.6.957. [DOI] [PMC free article] [PubMed] [Google Scholar]


