Abstract
OBJECTIVE:
In this study, we aimed to draw attention to traumatic pulmonary pseudocysts, which are rare cavitary lesions resulting from thoracic trauma, and review the diagnostic and therapeutic approaches and results.
METHODS:
Between January 2014 and January 2017, 30 patients included in this study who were diagnosed with traumatic pulmonary pseudocysts, from 582 patients who were admitted to our hospital with blunt thoracic trauma. To obtain data from the hospital information management system of patients included in this study, permission was obtained from the medical specialization board and the data were analyzed retrospectively.
RESULTS:
The mean age of the patients with traumatic pulmonary pseudocysts was 40.8 years (range, 7–75 years), and 11 (36.7%) of the patients were under the age of thirty and 19 (63.3%) were over the age of thirty. Twenty-eight (93.3%) patients had lung contusion and among those who had traumatic pulmonary pseudocysts diameter less than 2 cm, in 10 (33.3%) patients, contusion was present. In 27 patients, TPP was seen in thoracic computed tomography and diagnosed in the first 12 hours, but only in 10 of these patients, traumatic pulmonary pseudocysts was seen on chest x-ray. The extrathoracic injury was found in 15 (50%) patients. Twenty-two (73.3%) patients underwent tube thoracostomy. No patient required a thoracotomy.
CONCLUSION:
Traumatic pneumatoceles are benign lesions and most of them regress with symptomatic treatment and supportive therapy without any specific treatment.
Keywords: Cavitary lesion, Pulmonary pseudocyst, pneumatocele, thoracic trauma
Highlight key points.
Traumatic pneumatoceles do not contain prominent epithelial walls and form a small part of parenchymal injuries.
Trauma causes a sudden increase in pressure in a part of the peripheral airways and that the trapped air ruptures the alveolar wall.
Traumatic pneumatoceles are benign lesions and most of them regress with symptomatic treatment and supportive therapy without any specific treatment.
As a result of thoracic trauma, traumatic pulmonary pseudocyst (TPP), as also called traumatic lung cyst or traumatic pneumatocele and rarely seen cavitary lesions, may occur. TPPs are singular or multiple, unilateral or bilateral, oval or spherical, well-circumscribed lesions with air, fluid or blood in which. These cysts do not contain prominent epithelial walls and form a small part of parenchymal injuries that occur after blunt thoracic trauma. Traumatic pseudocyst does not have a membrane. They may occur at almost any age, but they are most common under the age of 30 years. These cysts can be detected on the chest X-ray, but thorax computed tomography (CT) is the best method in the diagnosis of these lesions [1–3].
MATERIALS AND METHODS
This retrospective clinical study was approved by the Local Ethics Committee (date: 07/11/2018, no: 2018/550). This study was conducted in accordance with the principles of the Declaration of Helsinki.
Between January 2014 and January 2017, 30 patients included in this study who were diagnosed with TPP, from 582 patients who were admitted to our hospital with blunt thoracic trauma. Patients with penetrating thoracic trauma were excluded from this study. To obtain data from the hospital information management system of patients included in this study, permission was obtained from the medical specialization board and the data were analyzed retrospectively. The cases were examined concerning gender, age, type and etiology of trauma, clinical findings, leukocyte count, concomitant intrathoracic and extrathoracic injuries, developing bone pathologies, surgical intervention, complications, mechanical ventilator requirement, intensive care unit requirement, total hospitalization period and mortality. TPPs were examined concerning diagnosis method (chest X-ray and/or CT), diagnosing period, TPP number, size, unilateral or bilateral occurence, localization, intraparenchymal or subpleural settling, and presence of contusion next to the pseudocyst, pseudocyst wall thickness and resolution time.
Statistical Analysis
The coding and statistical analysis of the data was performed with the SPSS for Windows version 22.0 software (SPSS Inc. Chicago, IL, USA). The numerical values obtained were expressed as mean±standard deviation (mean±SD) and categorical values were expressed as median±minimum maximum (median±min.–max.). Also, mean±SD and median±min.–max. values were visualized by a column or line graph. Means between groups were determined using an independent t-test and categorical data were evaluated using Chisquare tests. Significance was defined as p<0.05.
RESULTS
TPP was detected in 30 (5.2%) of 582 patients admitted to our hospital due to blunt thoracic trauma in this three-year period. Eight patients (26.7%) were female and 22 patients (73.3%) were male. The mean age of the patients with TPP was 40.8 years (range, 7–75 years), and 11 (36.7%) of the patients were under the age of thirty and 19 (63.3%) were over the age of thirty. Among the patients in this study, 16 patients had applied due to in-vehicle traffic accidents, seven patients falling from a height, five patients motorcycle accidents and one patient due to animal kicking. The other one patient was brought because he stayed under the demolished building after the bombing during the war. As admission symptoms, 29 patients (96.7%) had chest pain, 23 patients (76.7%) had dyspnea and seven patients (23.3%) had hemoptysis. Twenty-one (70%) patients had leukocytosis. Twenty-eight (93.3%) patients had lung contusion and among who has TPP diameter less than 2 cm, in 10 (33.3%) patients contusion was present. In 27 patients, TPP was seen in thoracic CT and diagnosed in the first 12 hours, but only in 10 of these patients, TPP was seen on chest x-ray. Twenty-three (76.7%) patients had a single TPP and seven (23.3%) had multiple TPPs. Twenty-nine (96.7%) patients had unilateral and one (3.3%) patients had bilateral lesions. TPP localization of the patients was 11 in the right upper lobe, three in the right middle lobe, six in the right lower lobe, seven in the left upper lobe and 11 in the left lower lobe. The mean wall thickness of the cyst was 2.1±0.33 (1–2.7) mm, the the mean vertical length was 18.3 (3.3–48) mm and the mean transfer length was 15.5 (4.3–42) mm. The air-fluid level image in the cyst was present in 6 (20%) patients. The extrathoracic injury was found in 15 (50%) patients (three radius fractures, one acetabular fracture, one subarachnoid hemorrhage, two pelvic fractures, three liver injuries, two spleen injuries, one vertebral fracture, one tibia fracture and one brain edema). The flail chest was detected in four patients (13.3%) and the costal fracture was detected in all 30 patients (one fracture in four patients, two fractures in seven patients, three fractures in nine patients, four fractures in three patients, five fractures in four patients, six fractures in one patient, seven fractures in one patient and eight fractures in one patient). One patient had a fracture of the sternum, four patients had a scapular fracture and three patients had a clavicle fracture. Twenty-two (73.3%) patients underwent tube thoracostomy. When the etiological factors in tube thoracostomy patients were examined, the findings showed that eight patients had a pneumothorax, five patients had hemothorax and nine patients had hemopneumothorax. No patient required a thoracotomy. Nine (30%) patients underwent the orthopedic procedure (surgery, gypsum, corset and bandage) and three (10%) patients underwent laparotomy (because of liver and spleen injury). The mean hospitalization period was 7.47±4.57 (2–25) days. Of the 11 patients under 30 years of age, 10 patients underwent tube thoracostomy and among these 10 patients, six of them had three or more costa fractures. 10 (33.3%) of the TPPs were subpleural and 20 (66.7%) were intraparenchymal. The mean age of the patients with subpleural TPP was 55.5±13.3 (38–75), and the mean age of the patients with intraparenchymal TPP was 29±17.2 (7–67). Tube thoracostomy was performed for only four of the patients (18.2%) with subpleural TPP and 18 of the patients (81.8%) with intraparenchymal TPP (Fig. 1) because of concomitant hemothorax, pneumothorax or hemopneumothorax (Fig. 2). Ten (33.3%) patients were followed up in the intensive care unit, and three patients required mechanical ventilation (two flail chest and one subarachnoid hemorrhage). One patient died on the 25th day of hospitalization. The patient who died had a pneumothorax, a costa fracture and a pseudocyst, with accompanying subarachnoid hemorrhage and extensive brain injury.
FIGURE 1.

X-ray findings in intraparenchymal traumatic pulmonary pseudocyst (posteroanterior radiograph).
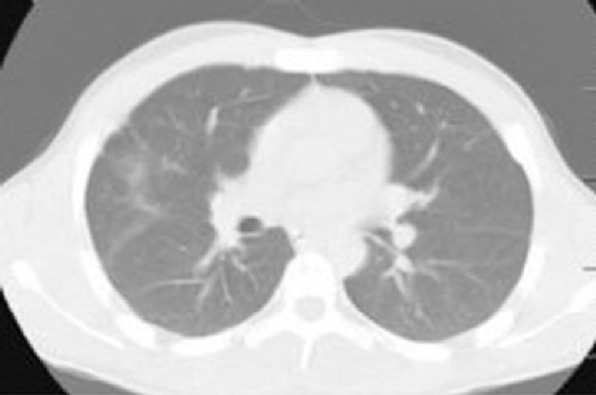
FIGURE 2.

Coexistence of Traumatic pulmonary pseudocyst and hemothorax.
DISCUSSION
While the walls of true cysts are surrounded by epithelial tissue, the walls of traumatic pulmonary pseudocysts are nonepithelial and are composed of interlobar interstitial connective tissue [4]. It was first described by Fallon in 1940 and the most common etiological factors are motor vehicle accidents and drops from height [5, 6]. Similarly, in our study, a motor vehicle accident with 53.3% and fall from height with 23.3% were the first two etiological factors. Sorsdahl and Powell [7] reported that most traumatic pulmonary pseudocysts occur in children and young adults, especially those under 30 years of age. Ulutaş et al. [3] reported that there is no significant difference below 30 years of age and above and may develop at any time in life. In our study, patients over 30 years of age (n=19, 63.3%) were significantly higher than those under the age of 30 years. Men have more motor vehicle accidents and fall more from a high distance. Therefore, they are reported to be more likely to be affected [8]. Similarly, in our study, most of the patients were male (n=22, 73.3%).
One of the mechanisms of TPP formation is that the trauma causes a sudden increase in pressure in a part of the peripheral airways and that the trapped air ruptures the alveolar wall. The other is that the jarring waves spreading through the lung parenchyma cause tears in the parenchyma [9].
Most traumatic pulmonary pseudocysts occur within 24–48 hours following blunt chest trauma [10, 11]. Symptoms are not specific to pseudocyst and are typical symptoms of lung parenchymal damage [12]. Although chest pain, dyspnea, cough and hemoptysis are common symptoms, asymptomatic cases are not few [13]. Our patients had complained of chest pain, dyspnea and hemoptysis.
Since most patients have additional pathologies to lung contusion, mild fever and leukocytosis are common. If the pulmonary contusion area is large and there is a multiple rib fracture or flail chest, acute respiratory failure may develop, and the need for a mechanical ventilator may occur. In our study, 70% of the patients (n=21) had leukocytosis.
Traumatic pulmonary pseudocysts may be single or multiple, unilateral or bilateral. They may be localized in any lobe of the lung. Although studies show that it is seen more frequently in the lower lobes, there are also studies showing that is seen more frequently in the upper lobes [2, 3, 14]. In 76.7% (n=23) of our patients, pseudocyst was single, and in 23.3% (n=7) were multiple. In 96.7% of our patients, TPPs (n=29) were unilateral and in 3.3% (n=1) were bilateral. The lower and upper lobe localization rates were close to each other and there was no significant difference.
In the literature, there are lesions ranging in diameter from 1–14 centimeters [15]. The wall thickness is between 1–7 mm and the average is 1.8 mm [16]. In our study, mean vertical length was 18.3 (3.3–48) mm, mean transfer length was 15.5 (4.3–42) mm, and mean pseudocyst wall thickness was 2.1 (1–2.7) mm.
The most important stage in the diagnosis of traumatic pulmonary pseudocyst is the patient’s history of thoracic trauma and the presence of thoracic graphy/thorax CT findings supporting this story. A history of trauma will get the clinicians away from other cavitary lesion causes and help them make the correct diagnosis. On the posteroanterior chest radiography, pseudocysts can be seen as round or oval, mostly surrounded by contusion, and as cavitary lesions containing air-fluid level or completely air [15]. By just chest X-ray, pseudocysts are seen in solely half of the patients [17]. In our study, only in 33.3% (n=10) patients, pseudocysts could be seen with chest radiography.
All of these lesions can be diagnosed by thorax CT and the sensitivity is 100% [15, 17]. Even in the post-traumatic early period, in CT, millimetric pseudocysts are diagnosed even if masked with a lung contusion. In the first 12 hours after the trauma, 90% (n=27) of our patients were diagnosed as pseudocyst by thorax CT.
In parallel with the development of technology, imaging systems have been widely used in our hospitals. In the 2000s, the incidence of traumatic pulmonary pseudocyst was reported to be 2%, whereas since the using of tomography is more widespread today, there are studies that report the incidence is 8% or even 10% [4, 12, 14, 15]. In our study, the rate of traumatic pulmonary pseudocyst was 5.2%. Our data and the data of three studies with the highest number of patients in the literature are presented in detail in Table 1 [3, 6, 18].
TABLE 1.
Our results and data from 3 studies with the highest number of patients
| Characteristics | Our results % | Ulutas et al. [3] % | Cho et al. [6] % | Luo et al. [18] % |
|---|---|---|---|---|
| Patients with TPP | 5.2 | 5.3 | 8.3 | 9.8 |
| Age (average) | 40.8 (7–75) | 33.1 (12–72) | 0–83 | 32.2 (7–70) |
| Age ≤30 | 36.7 | 53.8 | 29.6 | – |
| Age >30 | 63.3 | 46.2 | 70.4 | – |
| Gender | ||||
| Female | 26.7 | 19.2 | – | 84.8 |
| Male | 73.3 | 80.7 | – | 15.2 |
| Etiologies | ||||
| Motor vehicle | 70 | 87.8 | 65.5 | 60.6 |
| Fall | 23.3 | 12.1 | 29.6 | 27.3 |
| Crush | 3.3 | – | 2.5 | – |
| Animal crush | 3.3 | – | – | – |
| Assault | – | – | – | 12.1 |
| Slip | – | – | 2.5 | – |
| Symptom | ||||
| Chest pain | 96.7 | 100 | – | – |
| Dyspnea | 76.7 | 100 | – | – |
| Hemoptysis | 23.3 | – | – | – |
| Leucocytosis | 70 | 84.6 | – | – |
| Pseudocyst datas | ||||
| Single | 76.7 | 80.8 | – | (53 cysts) |
| Multiple | 23.3 | 19.2 | – | – |
| Unilateral | 96.7 | 92.3 | – | – |
| Bilateral | 3.3 | 7.7 | – | – |
| Subpleural | 33.3 | – | 49.4 | 67.9 |
| Intraparenchymal | 66.7 | – | 50.6 | 32.1 |
| Right upper lobe | 11 | 7 | – | 17 |
| Right middle lobe | 3 | – | – | 11.3 |
| Right lower lobe | 6 | 13 | – | 17 |
| Left upper lobe | 7 | 17 | – | 34 |
| Left lower lobe | 11 | 11 | – | 20.8 |
| Mean wall thickness | 2.1 (1–2.7 mm) | |||
| Mean maximal diameter (mm) | 18.3 (3.3–48) | 49 (10–150) | 23 (8–157) | 18 (4–65) |
| Intrathoracic injury | ||||
| Pneumothorax | 8 | 16 | – | |
| Haemothorax | 5 | 10 | – | 28 |
| Haemopneumothorax | 9 | 19 | – | |
| Rib fracture | 100 | 55.8 | 14.8 | 69.7 |
| Rib fracture (single) | 4 | – | – | – |
| Rib fracture (multiple) | 26 | – | – | 5 |
| Sternal fracture | 1 | – | – | 6 |
| Scapula fracture | 4 | – | – | – |
| Clavicula fracture | 3 | – | – | – |
| Flail chest | 13.3 | 7.7 | – | – |
| Extrathoracic injury | 50 | 51.9 | – | – |
| Extremity fractures | 7 | 12 | – | – |
| Subarachnoid hemorrhage | 1 | 3 | – | 4 head traumas |
| Intraabdominal injury | 5 | 7 | – | – |
| Vertebral fracture | 1 | 5 | – | 5 |
| Cerebral edema | 1 | – | – | – |
| Surgical intervention | ||||
| Tube thoracostomy | 73.4 | 86.5 | 58 | 36.4 |
| Thoracotomy | – | 15.4 | – | 15.2 |
| Laparatomy | 10 | 9.6 | – | – |
| Ortopedic procedure (surgery, plaster, splint) | 30 | 1.9 | – | – |
| Resolution time (month) | 1–4 (mean 3) | 1–5 | – | – |
| Duration of hospitalization (day) | 7.47 (2–25) | 8.8 (2–35) | ||
| Intensive care unit | 33.3 | – | – | – |
| Mechanical ventilator | 10 | – | 60.5 | – |
| Exitus | 3.3 | 1.9 | 21 | 9.1 |
In differential diagnosis, esophageal rupture, pulmonary sequestration, postpneumonic pneumatocele, bronchogenic cyst, lung abscess, tuberculosis cavity, cavitary bronchial carcinoma and cyst hydatid disease, especially in endemic areas, should be considered. The history of trauma of the patient, and the presence of contusion around the pseudocyst, removes the clinician from these diseases. Other causes should be investigated in patients with no regression in cavitary lesionsduring follow-up. Since the study area was an endemic region for hydatid cyst and there is a patient that previously had cyst hydatid history, this patient was carefully followed for four months. At the end of the follow-up, all of the cystic lesions disappeared and it was understood there was no hydatid cyst in our patient, and all of the lesions were traumatic pseudocysts. The thorax CT sections that were taken while this patient was discharged are presented in Figure 3, and the thorax CT sections taken four months after the discharge are presented in Figure 4.
FIGURE 3.

Thorax CT image taken on the 14th day of the patient.
FIGURE 4.
Thorax CT scan performed at the fourth month revealed that all cavitary lesions were lost and there was no concomitant hydatid cyst
TPP treatment is generally symptomatic and is intended for accompanying injury if present. Postural drainage and physiotherapy can be applied. If the patient cannot remove the secretion, bronchoscopy can be performed. There is still no consensus on the use of prophylactic antibiotics. However, if there is any concomitant other system injury, if a surgical procedure is to be performed, if the patient is to be followed in the intensive care unit, if there is a resistant fever, a prophylactic antibiotic can be administered [2, 3, 17, 19]. In our follow-up, all patients who had flail chest, abdominal injury, open fracture, a requirement of intensive care follow-up and who underwent thoracic surgery were treated with prophylactic antibiotics. Tube thoracostomy was performed in 22 (73.3%) patients as surgical intervention. Nine (30%) patients underwent the orthopedic procedure (surgery, gypsum, corset, bandage) and 3 (10%) patients underwent laparotomy (because of liver and spleen injury). Video-assisted thoracoscopic surgery or thoracotomy should be considered if the pseudocyst ruptures the pleural cavity and causes hemothorax or prolonged air leakage [1, 15, 19]. It should also be considered in cases where the functional parenchyma remains under pressure due to increased wall tension or progressive growth of the pseudocyst. All of the pseudocysts in our patients disappeared regressively at follow-up and none of them underwent thoracotomy/video-assisted thoracoscopic surgery.
Radiographic resolution of the pseudocyst is between one and six months, with an average of three months (1–3). In our study, the resolution time was between one and four months and the mean duration was three months.
Traumatic pulmonary pseudocyst, traumatic lung cyst or traumatic pneumatocele are different expressions of the same disease and are rarely seen cavitary lesions after thoracic trauma. Traumatic pneumatoceles are benign lesions and most of them regress with symptomatic treatment and supportive therapy without any specific treatment.
Footnotes
Ethics Committee Approval: The Erciyes University Clinical Research Ethics Committee granted approval for this study (date: 07.11.2018, number: 2018/550).
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
Authorship Contributions: Concept – IEO, MAT; Design – IEO, MAT; Supervision – IEO, MAT; Fundings – IEO, MAT; Materials – IEO, MAT; Data collection and/or processing – IEO, MAT; Analysis and/or interpretation – IEO, MAT; Literature review – IEO; Writing – IEO; Critical review – IEO.
REFERENCES
- 1.Kocer B, Gulbahar G, Gunal N, Dural K, Sakinci U. Traumatic pulmonary pseuodocysts:two case reports. J Med Case Rep. 2007;1:112. doi: 10.1186/1752-1947-1-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chon SH, Lee CB, Kim H, Chung WS, Kim YH. Diagnosis and prognosis of traumatic pulmonary psuedocysts:a review of 12 cases. Eur J Cardiothorac Surg. 2006;29:819–23. doi: 10.1016/j.ejcts.2006.01.054. [DOI] [PubMed] [Google Scholar]
- 3.Ulutas H, Celik MR, Ozgel M, Soysal O, Kuzucu A. Pulmonary pseudocyst secondary to blunt or penetrating chest trauma:clinical course and diagnostic issues. Eur J Trauma Emerg Surg. 2015;41:181–8. doi: 10.1007/s00068-014-0427-2. [DOI] [PubMed] [Google Scholar]
- 4.Santos GH, Mahendra T. Traumatic pulmonary pseudocysts. Ann Thorac Surg. 1979;27:359–62. doi: 10.1016/s0003-4975(10)63316-4. [DOI] [PubMed] [Google Scholar]
- 5.Gupta N, George J, Gupta RC, Dixit R. Traumatic pulmonary pseudocyst. Int J Crit Illn Inj Sci. 2013;3:155–8. doi: 10.4103/2229-5151.114276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cho HJ, Jeon YB, Ma DS, Lee JN, Chung M. Traumatic pulmonary pseudocysts after blunt chest trauma:Prevalence mechanisms of injury and computed tomography findings. J Trauma Acute Care Surg. 2015;79:425–30. doi: 10.1097/TA.0000000000000758. [DOI] [PubMed] [Google Scholar]
- 7.Sorsdahl OA, Powell JW. Cavitary pulmonary lesions following nonpenetrating chest trauma in children. Am J Roentgenol Radium Ther Nucl Med. 1965;95:118–24. doi: 10.2214/ajr.95.1.118. [DOI] [PubMed] [Google Scholar]
- 8.Fagkrezos D, Giannila M, Maniatis P, Papailiou J, Triantopoulou C. Post-traumatic pulmonary pseudocyst with hemopneumothorax following blunt chest trauma:a case report. J Med Case Rep. 2012;6:356. doi: 10.1186/1752-1947-6-356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.De A, Peden CJ, Nolan J. Traumatic pulmonary pseudocysts. Anaesthesia. 2007;62:409–11. doi: 10.1111/j.1365-2044.2007.05023.x. [DOI] [PubMed] [Google Scholar]
- 10.Stathopoulos G, Chrysikopoulou E, Kalogeromitros A, Papakonstantinou K, Poulakis N, Polyzogopoulos D, et al. Bilateral traumatic pulmonary pseudocysts:case report and literature review. J Trauma. 2002;53:993–6. doi: 10.1097/00005373-200211000-00031. [DOI] [PubMed] [Google Scholar]
- 11.Romero J, Velmahos GC. Giant posttraumatic hemopneumatocele:nonoperative management is safe. J Trauma. 2000;49:1132–4. doi: 10.1097/00005373-200012000-00028. [DOI] [PubMed] [Google Scholar]
- 12.Athanassiadi K, Gerazounis M, Kalantzi N, Kazakidis P, Fakou A, Kourousis D. Primary traumatic pulmonary pseudocysts:a rare entity. Eur J Cardiothorac Surg. 2003;23:43–5. doi: 10.1016/s1010-7940(02)00653-x. [DOI] [PubMed] [Google Scholar]
- 13.Yang PJ, Tsai IT, Liu TH. Traumatic Pulmonary Pseudocyst. J Pediatr. 2015;167:777.e1. doi: 10.1016/j.jpeds.2015.06.025. [DOI] [PubMed] [Google Scholar]
- 14.Hazer S, Orhan Söylemez UP. Clinical features diagnosis, and treatment of traumatic pulmonary pseudocysts. Ulus Travma Acil Cerrahi Derg. 2018;24:49–55. doi: 10.5505/tjtes.2017.56023. [DOI] [PubMed] [Google Scholar]
- 15.Melloni G, Cremona G, Ciriaco P, Pansera M, Carretta A, Negri G, et al. Diagnosis and treatment of traumatic pulmonary pseudocysts. J Trauma. 2003;54:737–43. doi: 10.1097/01.TA.0000022351.07179.D6. [DOI] [PubMed] [Google Scholar]
- 16.Tsitouridis I, Tsinoglou K, Tsandiridis C, Papastergiou C, Bintoudi A. Traumatic pulmonary pseudocysts:CT findings. J Thorac Imaging. 2007;22:247–51. doi: 10.1097/RTI.0b013e3180413e2a. [DOI] [PubMed] [Google Scholar]
- 17.Kato R, Horinouchi H, Maenaka Y. Traumatic pulmonary pseudocyst. Report of twelve cases. J Thorac Cardiovasc Surg. 1989;97:309–12. [PubMed] [Google Scholar]
- 18.Luo L, Yin L, Liu Z, Xiang Z. Posttraumatic pulmonary pseudocyst:computed tomography findings and management in 33 patients. J Trauma Acute Care Surg. 2012;73:1225–8. doi: 10.1097/TA.0b013e318265ccb9. [DOI] [PubMed] [Google Scholar]
- 19.Yazkan R, Ozpolat B, Sahinalp S. Diagnosis and management of post-traumatic pulmonary pseudocyst. Respir Care. 2009;54:538–41. [PubMed] [Google Scholar]


