Abstract
Consumer demand for organically produced foods is increasing in the United States as well as globally. Consumer perception often credits organic foods as being safer than conventionally produced foods, although organic standards do not directly address safety issues such as microbial or chemical hazards. We reviewed outbreaks reported to the Centers for Disease Control and Prevention’s Foodborne Disease Outbreak Surveillance System where the implicated food was reported to be organic. Information collected for each outbreak included the year, state, number of illnesses, pathogen, and implicated food. We identified 18 outbreaks caused by organic foods from 1992 to 2014, resulting in 779 illnesses, 258 hospitalizations, and 3 deaths; 56% of outbreaks occurred from 2010 to 2014. Nine outbreaks occurred in a single state, and nine outbreaks were multistate. Salmonella sp. (44% of outbreaks) and Escherichia coli O157:H7 (33%) were the most commonly occurring pathogens. Eight of the outbreaks were attributed to produce items, four to unpasteurized dairy products, two to eggs, two to nut and seed products, and two to multi-ingredient foods. Fifteen (83%) outbreaks were associated with foods that were definitely or likely U.S. Department of Agriculture certified. More foodborne outbreaks associated with organic foods in the United States have been reported in recent years, in parallel with increases in organic food production and consumption. We are unable to assess risk of outbreaks due to organic foods compared with conventional foods because foodborne outbreak surveillance does not systematically collect food production method. Food safety requires focused attention by consumers, regardless of whether foods are produced organically or conventionally. Consumers should be aware of the risk of milk and produce consumed raw, including organic.
Keywords: Disease outbreak, Foodborne illness, Organic
Consumer demand for organically produced goods in the United States has steadily increased over the past decade (Fig. 1). Retail sales of organic foods reached US$28 billion in 2012, up from US$11 billion in 2004 (22). Consumers cite many reasons for purchasing organic foods including, in part, health consciousness, environmental concerns, better taste, and food safety (9). Although producer marketing and consumer perception may credit organic foods as meeting stringent food safety standards, consumers are often not aware that organic standards do not directly address food safety considerations such as microbial or chemical hazards (2). Studies suggest however that consumption of organic foods may reduce exposure to pesticide residues and antibiotic-resistant bacteria (1, 12, 20).
FIGURE 1.
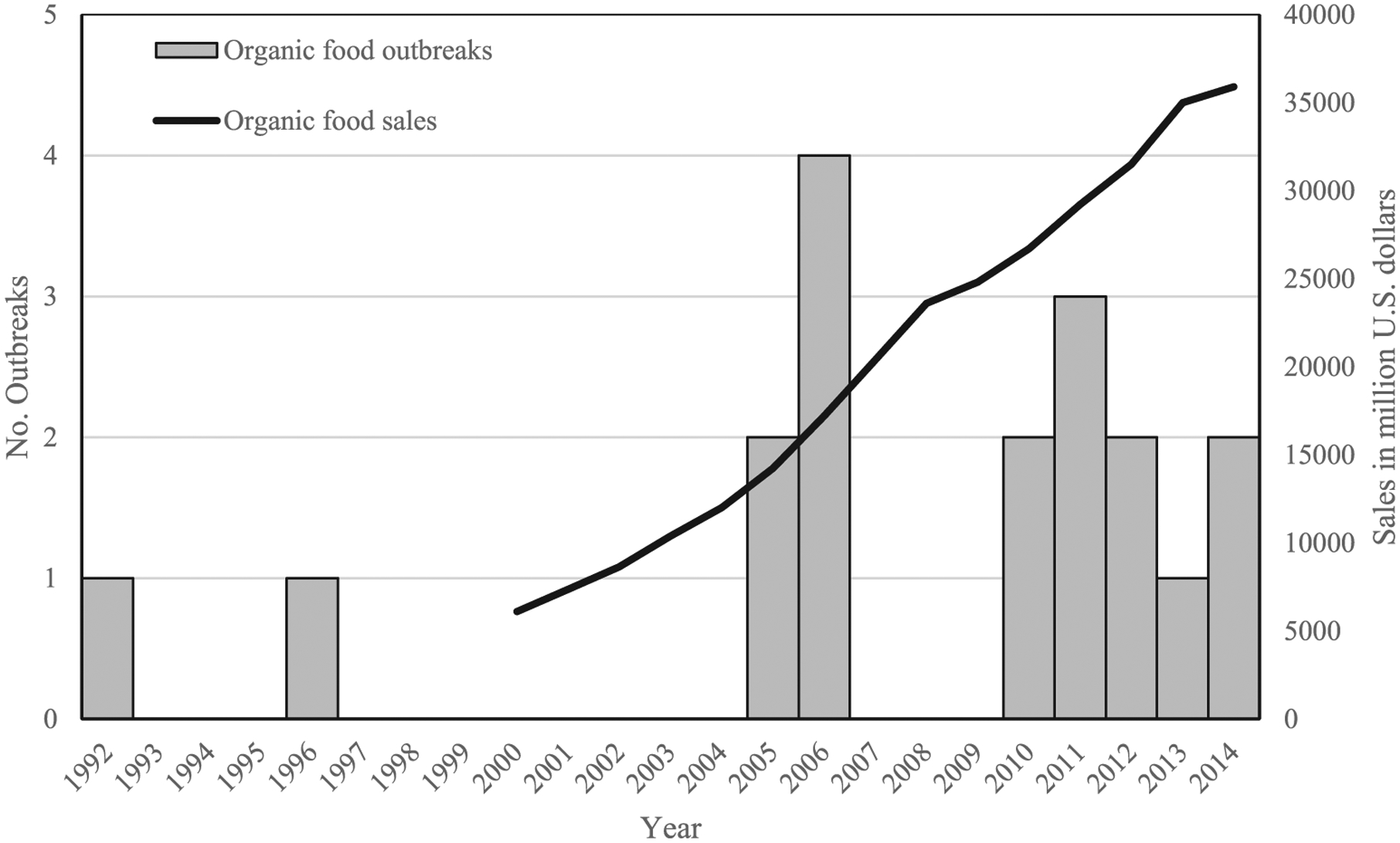
Outbreaks attributed to organic food (1992 to 2014) and organic food sales (2000 to 2014) by year (21), in the United States.
The term “organic,” as defined in 2002 by the U.S. Department of Agriculture (USDA), National Organic Program of the Agriculture Marketing Service, applies to specific methods of production of crops and livestock aimed to protect natural resources and conserve biodiversity. Crops are verified as organic when certain agricultural practices are not performed or specific compounds or products are not used, including sewage sludge, synthetic fertilizers, genetically modified organisms, and prohibited pesticides. Generally, organic livestock practices require that producers meet defined animal health and welfare standards, administer no antibiotics or growth hormones, and use organic feed (23).
We use data from a national surveillance system to summarize and describe reported outbreaks caused by organic foods in the United States from 1992 to 2014.
MATERIALS AND METHODS
The Centers for Disease Control and Prevention collects reports of foodborne disease outbreaks voluntarily reported by state, local, and territorial health departments through the Foodborne Disease Outbreak Surveillance System. Information collected for each outbreak includes the year, state, number of illnesses, pathogen, and implicated food. Information on whether a food is produced using conventional or organic methods is not explicitly collected, although it can be included as part of a food’s description or noted in the remarks accompanying a report. We queried outbreaks reported from 1973, when the system was created, through the most recent year for which data were available, 2014, for any mention of “organic”: variables searched included implicated food, recalled product, traceback facility, and report comments. Additional information was also obtained from an online search for news reports and press releases describing outbreaks implicating organic foods by using the Foodborne Illness Outbreak Database (6) compiled by a law firm that includes outbreaks beginning in 1984, and Google News Search that queries news articles beginning in 2003.
We identified outbreaks where the implicated food was reported as organic. USDA organic certification was not necessary for inclusion in the analysis; outbreaks where the food was reported as organic and certification was likely, but insufficient details were available to confirm certification and those where the food was represented or self-reported as organic by the producer or grower were also included.
RESULTS
We identified 18 foodborne disease outbreaks associated with organic foods, resulting in 779 illnesses, 258 hospitalizations, and 3 deaths (Table 1). The first identified outbreak caused by an organic food occurred in 1992; 56% of outbreaks occurred from 2010 to 2014 (Fig. 1). Nine outbreaks occurred in a single state (California, three outbreaks; Minnesota, three outbreaks; Maine, one outbreak; Florida, one outbreak; Michigan, one outbreak), and nine outbreaks were multistate (i.e., exposure to the implicated food occurred in more than one state).
TABLE 1.
Outbreaks caused by organic foods 1992 to 2014 in the United States
| Year | Month of first illness onset | State(s) | No. ill | No. hospitalized | No. died | Food name | Pathogen(s) | USDA-certified statusa |
|---|---|---|---|---|---|---|---|---|
| 1992 | Unknown | Maine | 4 | 1 | 1 | Produce | E. coli O157:H7 | Not certified |
| 1996 | Unknown | Multistate | 61 | 21 | 0 | Mesclun lettuce | E. coli O157:H7 | Not certified |
| 2005 | November | Florida | 10 | — | — | Sweet potato dish | Salmonella sp. | Likely certified |
| 2005 | July | Multistate | 23 | 5 | 0 | Eggs | Salmonella Enteritidis | Certified |
| 2006 | June | Minnesota | 50 | 6 | 0 | Vegetable-based soup | Salmonella Typhimurium | Certified (cross-contamination) |
| 2006 | September | Multistate | 4 | 4 | 1 | Carrot juice, pasteurized | Clostridium botulinum | Certified |
| 2006 | September | California | 6 | 3 | 0 | Raw milk and cream | E. coli O157:H7 | Certified |
| 2006 | September | Multistate | 183 | 95 | 1 | Spinach | E. coli O157:H7 | Likely certified |
| 2010 | May | Minnesota | 7 | 0 | 0 | Raw milk | E. coli O157, Campylobacter jejuni, Cryptosporidium parvum | Not certified |
| 2010 | November | Multistate | 140 | 31 | 0 | Alfalfa sprouts | Salmonella I 4,[5],12:i:– | Likely certified |
| 2011 | August | Minnesota | 8 | 3 | 0 | Eggs | Salmonella Enteritidis | Certified |
| 2011 | September | Michigan | 33 | 1 | 0 | Grape tomatoes | Salmonella sp. | Certified |
| 2011 | August | California | 5 | 3 | 0 | Raw milk | E. coli O157:H7 | Certified |
| 2012 | October | Multistate | 33 | 10 | 0 | Spinach and spring mix | E. coli O157:H7 | Likely certified |
| 2012 | January | California | 10 | 0 | 0 | Raw milk and cream | Campylobacter sp. | Certified |
| 2013 | March | Multistate | 165 | 69 | 0 | Pomegranate seeds | Hepatitis A | Certified |
| 2014 | January | Multistate | 31 | 5 | 0 | Chia seed powder | Salmonella Newport, Hartford, and Oranieburg | Certified |
| 2014 | January | Multistate | 6 | 1 | 0 | Nut butter | Salmonella Braenderup | Certified |
The USDA National Organic Program was established in 2002.
The most commonly occurring pathogens were Salmonella sp. (eight outbreaks, 44%) and Escherichia coli O157:H7 (six outbreaks, 33%), followed by Campylobacter (one outbreak, 6%), Clostridium botulinum (one outbreak, 6%), and hepatitis A virus (one outbreak, 6%). One outbreak involved Escherichia coli O157:H7, Campylobacter, and Cryptosporidium.
Nearly half (44%) of the outbreaks were attributed to produce items (alfalfa sprouts, carrot juice, grape tomatoes, mesclun lettuce, pomegranate seeds, spinach, spinach and spring mix, and an unspecified produce item), four outbreaks to unpasteurized dairy products, two outbreaks to eggs, two outbreaks to nut and seed products, and two outbreaks to multi-ingredient foods (vegetable-based soup and sweet potato casserole). Three of four outbreaks caused by unpasteurized milk and cream were associated with a single California producer. Five (63%) of eight outbreaks associated with produce with known month of illness onset occurred from August to November.
Fifteen (83%) outbreaks were associated with foods that were definitely or likely USDA certified. Our supplemental online search confirmed USDA certification for 11 of these outbreaks; the other 4 outbreaks were likely USDA certified, although we were unable to confirm this through our supplemental search. These foods were alfalfa sprouts, carrot juice, chia seed powder, eggs (twice), grape tomatoes, nut butter, pomegranate seeds, soup, spinach, spinach and spring mix, sweet potato casserole, and unpasteurized milk and cream (three times). Two outbreaks (11%) were associated with foods marketed as organic that were not USDA certified: one outbreak involved unpasteurized milk that used the word “organic” in the product name and the other outbreak was associated with mesclun lettuce that preceded the establishment of the National Organic Program. The remaining outbreak involved produce grown in a home garden that was self-reported as organic by the owner.
DISCUSSION
We identified 18 outbreaks caused by organic foods, with more outbreaks reported in recent years. This increase in outbreaks is consistent with increasing sales and consumption of organic foods in the United States (Fig. 1) and creation of the National Organic Program in 2002. Although our study cannot ascribe risk of foodborne outbreaks based on production method, these data provide a first step toward comparing foodborne disease outbreaks associated with organically and conventionally produced foods in the future, and they highlight the possible benefits of systematically collecting more information about production practices associated with foods implicated in outbreaks.
Nearly half of the organic food outbreaks were associated with produce. Several factors probably contribute to this finding, some of which are independent of production method. Produce is the most purchased organic food, accounting for 43% of organic food sales in the United States in 2012 (22). Outbreaks associated with produce are increasing in general, regardless of production method (14). From 1998 to 2008, an estimated 46% of foodborne illnesses were attributed to produce (18). It is possible that some farming methods common in organic production might allow for a higher pathogen load for certain foods (15). For example, synthetic fertilizers cannot be used in organic production; therefore, composted manure or raw manure, spread at least 90 to 120 days before harvesting, is commonly applied to soil as fertilizer (17). Composting and the required elapsed time between raw manure application and harvesting are intended to eliminate harmful microbes, but some studies have found that bacteria in composted soil, including Salmonella sp. and E. coli, can survive much longer than 120 days (10). In a laboratory, pathogens including Salmonella sp. and E. coli were capable of regrowth in finished compost, suggesting the use of compost might present a risk for produce contamination when spread or applied to agricultural fields (25). In addition, a recent study found that produce from organic farms using manure for fertilization was more likely to be contaminated with E. coli than was produce from organic farms not using manure (16). More research is needed to determine the best period between manure application and harvest, to better characterize the regrowth potential of pathogens in finished compost, and to better describe pathogen growth in different types of compost.
Together, produce and unpasteurized dairy products accounted for 78% of the organic food outbreaks identified. These foods are generally consumed without further processing (e.g., cooking) that reduces the risk of foodborne illness. Washing produce can reduce, but not eliminate, bacterial contamination, emphasizing the importance of production and processing methods designed to minimize pathogens present in finished produce (19). Consumption of unpasteurized dairy products is inherently risky and pasteurization is the most effective method of enhancing the safety of dairy products (13). Although most (89%) of the outbreaks identified were associated with single food products, two outbreaks were associated with multi-ingredient foods. For such foods, ingredients other than those organically produced could have been contaminated and thus responsible for the outbreak. In fact, cross-contamination from raw eggs was a likely cause of the 2006 outbreak associated with organic vegetable–based soup.
Our study did not identify any outbreaks associated with organic meats; however, studies suggest that meat produced under organic conditions might be more likely to be contaminated with foodborne pathogens than meat from conventionally produced animals (7, 24). At the same time, because antimicrobial treatment is prohibited for organically raised animals, it has been found that organically produced meats have a lower prevalence of contamination with antimicrobial resistant bacteria (24). Although additional research is needed to characterize risk of foodborne illness as it relates to contamination with pathogens of varied antimicrobial resistance profiles, most studies suggest bacteria recovered from organically produced meat are less likely to develop antimicrobial resistance than those from conventionally raised meat.
Organic certification requirements and farming practices vary worldwide, but the principal tenants are generally consistent in that organic foods are grown without synthetic pesticides or fertilizers or routine use of antibiotics or growth hormones, and outbreaks associated with organic foods have also been reported from other countries. For example, in 2007, organic fermented beef sausage was associated with an outbreak of Shiga toxin–producing E. coli (STEC) O26:H11 infections in Denmark (5). In 2011, organic fenugreek sprouts were associated with an international outbreak of STEC O104:H4 infections (3). Although the global demand for organically produced foods has led to increasing amounts of agricultural land dedicated to organic food production (11), relatively few outbreaks associated with organic foods internationally are recorded in the literature, possibly due to the lack of systematic collection of information on production methods during outbreak investigation. As such, those reported probably underestimate the true burden of outbreaks associated with organic foods due to data collection methods as well as the varied certification requirements. As the food industry continues to globalize, shelf-stable organic foods are more likely to be distributed internationally. For example, the outbreak associated with organic chia seed powder occurred in both the United States and Canada, and recalled products were distributed to at least 14 other countries (Centers for Disease Control and Prevention, unpublished data).
In the United States, businesses and farms must be certified by a USDA-accredited certifying agent to label a product organic; the Code of Federal Regulation (7 CFR Part 205) codifies organic standards that are established and regulated by the USDA National Organic Program. For products to be labeled organic, they must adhere to these USDA-regulated standards, and the use of these labels is regulated and enforced by USDA to ensure validity. Certain exemptions exist that allow products to be labeled organic without certification. For example, small farms or operations with less than US$5,000 in annual sales are exempt according to 7 CFR Part 205.101. Categories of organic products include “100% organic,” “organic,” “made with organic,” and “specified organic ingredients”; the similarities and differences among these labeling categories and their accompanying technical definitions might confuse consumers. Similarly, variations in the use of the term organic could influence consumer perception. Most of the outbreaks attributed to organic produce were probably included in the National Organic Program; however, we identified at least one outbreak where the food was sold as organic based on the name of the establishment, but was not actually certified.
Consumer perception tends to view organic farming methods as safer than conventional production methods (9,26). Studies in Europe suggest many consumers have heard of the term organic and are aware of its central features (i.e., chemical free), yet most are unfamiliar with organic farming standards and practices, and considerable confusion surrounding the term organic still exists (4, 8). This is probably the case in the United States as well, not from a regulatory viewpoint as the standards are clearly defined, but from that of consumers who might not be familiar with the technical definitions of National Organic Program labeling and exemptions. Although interpretation of the term organic may vary based on consumer knowledge, attitude, and practices, organic production methods should not be viewed as a replacement for other food safety practices.
Our study has several limitations. First, the Foodborne Disease Outbreak Surveillance System outbreak report form does not explicitly collect information on production methods (e.g., organic). Therefore, we cannot compare outbreaks caused by organic foods with those caused by foods grown using other methods. It is possible that we underestimated the true number of outbreaks caused by organic foods because we lacked details on the foods implicated in some outbreaks. It is also possible we misclassified some foods as organic that were not certified. Better methods for gathering accurate information on production methods, including organic, are needed. This includes updated data collection methods to systematically assess production techniques in the context of outbreak investigations. Considerations such as USDA certification status must be taken into account before methodologic changes are made, and our hope is that this research note will highlight these gaps to ultimately improve data collection. There may also be other mechanisms to collect this information, such as better linkage between Centers for Disease Control and Prevention and traceback databases managed by the U.S. Food and Drug Administration and USDA for foods under their respective regulatory authority. In addition to increasing sales of organic foods in the United States, outbreak reporting has been enhanced in recent years, so it is possible that the increased number of outbreaks in recent years reflects improvements in surveillance rather than a true increase in the number of outbreaks. Similarly, our supplementary Internet search for additional details was probably biased toward the more recent past.
Our findings emphasize the need to continually improve data collection to be able to accurately describe the causes of foodborne disease outbreaks. Consumers should not assume organic foods to be more or less safe than foods produced by conventional methods. Proper handling, preparation, and storage of foods, regardless of production method, are necessary to prevent foodborne illness.
REFERENCES
- 1.Bourn D, and Prescott J. 2002. A comparison of the nutritional value, sensory qualities, and food safety of organically and conventionally produced foods. Crit. Rev. Food Sci. Nutr 42:1–34. [DOI] [PubMed] [Google Scholar]
- 2.Brennan C, Gallagher K, and McEachern M. 2003. A review of the “consumer interest” in organic meat. Int. J. Consum. Stud 27:381–394. [Google Scholar]
- 3.Buchholz U, Bernard H, Werber D, Bohmer MM, Remschmidt C, Wilking H, Delere Y, an der Heiden M, Adlhoch C, Dreesman J, Ehlers J, Ethelberg S, Faber M, Frank C, Fricke G, Greiner M, Hohle M, Ivarsson S, Jark U, Kirchner M, Koch J, Krause G, Luber P, Rosner B, Stark K, and Kuhne M. 2011. German outbreak of Escherichia coli O104:H4 associated with sprouts. N. Engl. J. Med 365:1763–1770. [DOI] [PubMed] [Google Scholar]
- 4.Chryssochoidis G 2000. Repercussions of consumer confusion for late introduced differentiated products. Eur. J. Mark 34:705–722. [Google Scholar]
- 5.Ethelberg S, Smith B, Torpdahl M, Lisby M, Boel J, Jensen T, Nielsen EM, and Molbak K. 2009. Outbreak of non-O157 Shiga toxin-producing Escherichia coli infection from consumption of beef sausage. Clin. Infect. Dis 48:e78–81. [DOI] [PubMed] [Google Scholar]
- 6.Foodborne Illness Outbreak Database. 2016. Marler Clark. Available at: http://outbreakdatabase.com/. Accessed 6 May 2014.
- 7.Hardy B, Crilly N, Pendleton S, Andino A, Wallis A, Zhang N, and Hanning I. 2013. Impact of rearing conditions on the microbiological quality of raw retail poultry meat. J. Food Sci 78:M1232–1235. [DOI] [PubMed] [Google Scholar]
- 8.Harper G, and Makatouni A. 2002. Consumer perception of organic food production and farm animal welfare. Br. Food J 104:287–299. [Google Scholar]
- 9.Hughner R, McDonagh P, Prothero A, Shultz C, and Stanton F. 2007. Who are organic food consumers? A compilation and review of why people purchase organic food. J. Consum. Behav 6:94–110. [Google Scholar]
- 10.Ingram D 2009. Assessment of foodborne pathogen survival during production and pre-harvest application of compost and compost tea Ph.D. dissertation University of Maryland, College Park: Available at: http://drum.lib.umd.edu/bitstream/1903/9137/1/Ingram_umd_0117E_10231.pdf. Accessed 6 May 2014. [Google Scholar]
- 11.Kearney J 2010. Food consumption trends and drivers. Philos. Trans. R. Soc. Lond. B Biol. Sci 365:2793–807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim S, and Woo GJ. 2014. Prevalence and characterization of antimicrobial-resistant Escherichia coli isolated from conventional and organic vegetables. Foodborne Pathog. Dis 11:815–821. [DOI] [PubMed] [Google Scholar]
- 13.Lejeune JT, and Rajala-Schultz PJ. 2009. Food safety: unpasteurized milk: a continued public health threat. Clin. Infect. Dis 48:93–100. [DOI] [PubMed] [Google Scholar]
- 14.Lynch MF, Tauxe RV, and Hedberg CW. 2009. The growing burden of foodborne outbreaks due to contaminated fresh produce: risks and opportunities. Epidemiol. Infect 137:307–315. [DOI] [PubMed] [Google Scholar]
- 15.Miranda JM, Guarddon M, Mondragon A, Vazquez BI, Fente CA, Cepeda A, and Franco CM. 2007. Antimicrobial resistance in Enterococcus spp. strains isolated from organic chicken, conventional chicken, and turkey meat: a comparative survey. J. Food Prot 70:1021–1024. [DOI] [PubMed] [Google Scholar]
- 16.Mukherjee A, Speh D, and Diez-Gonzalez F. 2007. Association of farm management practices with risk of Escherichia coli contamination in pre-harvest produce grown in Minnesota and Wisconsin. Int. J. Food Microbiol 120:296–302. [DOI] [PubMed] [Google Scholar]
- 17.Organic Trade Association. 2007. Organic Trade Association: manure facts. Available at: http://www.ota.com/organic/foodsafety/manure.html. Accessed 15 April 2014.
- 18.Painter JA, Hoekstra RM, Ayers T, Tauxe RV, Braden CR, Angulo FJ, and Griffin PM. 2013. Attribution of foodborne illnesses, hospitalizations, and deaths to food commodities by using outbreak data, United States, 1998–2008. Emerg. Infect. Dis 19:407–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sapers G 2001. Efficacy of washing and sanitizing methods for disinfection of fresh fruit and vegetable products. J. Food Technol. Biotechnol 39:305–311. [Google Scholar]
- 20.Smith-Spangler C, Brandeau ML, Olkin I, and Bravata DM. 2013. Are organic foods safer or healthier? Ann. Intern. Med 158:297–300. [DOI] [PubMed] [Google Scholar]
- 21.Statista. 2016. Organic food sales in the Unites States from 2000 to 2014 (in million U.S. dollars) Available at: http://www.statista.com/statistics/196952/organic-food-sales-in-the-us-since-2000/. Accessed 6 May 2014.
- 22.U.S. Department of Agriculture. 2012. USDA Economic Research Service: organic market overview. Available at: http://www.ers.usda.gov/topics/natural-resources-environment/organic-agriculture/organic-market-overview.aspx. Accessed 9 May 2014.
- 23.U.S. Department of Agriculture. 2013. USDA Agricultural Marketing Service: National Organic Program. Available at: http://www.ams.usda.gov/AMSv1.0/ams.fetchTemplateData.do?template=TemplateN&navID=OrganicStandardslinkNOPConsumers&rightNav1=OrganicStandardslinkNOPConsumers&topNav=&leftNav=&page=NOPOrganicStandards&resultType&acct=nopgeninfo. Accessed 25 April 2014.
- 24.Van Loo EJ, Alali W, and Ricke SC. 2012. Food safety and organic meats. Annu. Rev. Food Sci. Technol 3:203–225. [DOI] [PubMed] [Google Scholar]
- 25.Wichuk K, and McCartney D. 2007. A review of the effectiveness of current time-temperature regulations on pathogen inactivation during composting. J. Environ. Eng. Sci 6:573–586. [Google Scholar]
- 26.Williams PR, and Hammitt JK. 2001. Perceived risks of conventional and organic produce: pesticides, pathogens, and natural toxins. Risk Anal. 21:319–330. [DOI] [PubMed] [Google Scholar]


