Abstract
Background:
Melanocytomas are rare pigmented tumors of the central nervous system (CNS). They are more frequent in females in their fifties and are typically benign, but locally aggressive lesions that very are rarely found in the spine. They can occur in all the age groups.
Case Description:
A 62-year-old male presented with acute paraplegia a attributed to a C7-T1 intradural extramedullary melanocytoma. Urgent surgery, consisting of subtotal removal of the lesion, resulted in subtotal recovery of motor function with full resolution of his sensory deficit. Histologically, the lesion proved to be a melanocytoma.
Conclusion:
Rarely, patients with intradural extramedullary melanocytomas of the spine may present with acute paralytic deficits warranting emergent surgical intervention.
Keywords: Melanocytoma, Paraplegia, Primary spinal tumor, Spinal cord

INTRODUCTION
Melanocytomas are rare pigmented tumors originating from leptomeningeal melanocytes. They are benign lesions that infrequently occur in the spine, where they may cause acute radiculopathy and/or myelopathy. In this case, a 62-year-old male acutely presented with paraplegia attributed to a C7-T1 intradural extramedullary anterior melanocytoma.
CASE PRESENTATION
Clinical and surgical history
A 62-years-old male, with a 2 months history of interscapular pain, presented with acute T2-level paraplegia. The MRI showed an intradural extramedullary well-defined mass at the C7-T1 level located anterior to the spinal cord. The T2-weighted image demonstrated an isointense lesion with a wide dural attachment while the enhanced study demonstrated heterogeneous enhancement with compression and posterior displacement of the cord [Figure 1].
Figure 1:

Sagittal T2-weighted image showing an isointense extramedullary mass with dural attachment.
An emergent decompressive C7-T1 laminectomy was performed and achieved subtotal tumor removal. Intraoperatively, the cervicodorsal dura was blackened, and the lesion was firm.
Histopathology
The histopathologic examination revealed large cells, oval to polygonal in shape with prominent nucleoli, and eosinophilic cytoplasm filled with melanin pigment. There was no significant increase in mitosis (1/10 HPF and low proliferation index Ki 67: 2%). On immunohistochemistry tumor cells showed positivity with S100, Vimentin and HBM45 and negativity for EMA (which is an indicator of meningioma), thus confirming the diagnosis of melanocytoma [Figure 2].
Figure 2:
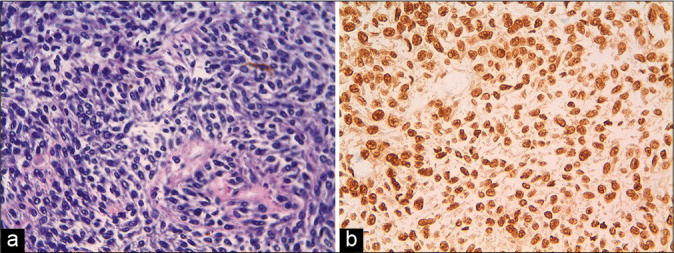
(a) Spindle-shaped cells with focal melanin pigmentation (b) immunohistochemical positivity for S100.
Postoperative course
The 1 day post-operative MRI revealed removal of the 90% of the lesion and no residual compression of the cervicothoracic cord at the same level. After the 1st postoperative week, he demonstrated subtotal recovery of motor (4/5 BMRC grade) and total sensory recovery of function. He was discharged in a rehabilitation unit. Three months later, the patient’s neurological status was improved (5/5 BMRC) and he is being referred for radiation therapy.
DISCUSSION
The World Health Organization’s classification classifies primary melanocytic lesions into four categories; meningeal melanocytosis, meningeal melanocytoma, meningeal melanoma, and meningeal melanomatosis.[3,6] Melanocytoma commonly presents in posterior fossa and foramen magnum, but only rarely in the spine.[2] Due to the benign nature of these tumors, and their typical slow growth, spinal symptoms/signs have a slow onset, and reflect the location of the lesion; acute paraplegia is very rare.[4] We treated this lesion as an acute spinal cord compression to grant the total neurological recovery of the patient, giving priority to clinical status with respect to complete removal of the tumor; although these are benign tumors, for gross total, subtotal or partial excision, the risk of recurrence is sufficiently high to warrant adjuvant radiation therapy.[1,5]
CONCLUSION
In the presence of spinal cord compression due to intradural extramedullary lesion with acute neurological onset, the surgical decompression and the removal of the lesion, despite subtotal, are necessary to achieve a good neurological outcome.
Footnotes
How to cite this article: Nigro R, Scogna AA, Intraina D, Toccaceli G, Ieraci A, Zotta DC. Acute onset of paraplegia due to melanocytic cervicodorsal lesion. Surg Neurol Int 2021;12:21.
Contributor Information
Raffaele Nigro, Email: raffaele.nigro1983@gmail.com.
Antonio Alessandro Scogna, Email: antonioalessandro.scogna@ausl.pe.it.
Daniele Intraina, Email: intraina@ausl.pe.it.
Giada Toccaceli, Email: toccaceli.giada@gmail.com.
Alfio Ieraci, Email: alfio.ieraci@ausl.pe.it.
Donato Carlo Zotta, Email: donatocarlo.zotta@ausl.pe.it.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Eskandari R, Schmidt MH. Intramedullary spinal melanocytoma. Rare Tumors. 2010;2:e24. doi: 10.4081/rt.2010.e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jayamma SS, Sud S, Buxi T, Madan VS, Goyal A, Dhawan S. Cervical spinal meningeal melanocytoma presenting as intracranial superficial siderosis. Case Rep Radiol. 2015;2015:674868. doi: 10.1155/2015/674868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Louis DN, Perry A, Reifenberger G, von Deimling A, FigarellaBranger D, Cavenee WK, et al. The 2016 World Health Organization classification of tumors of the central nervous system: A summary. Acta Neuropathol. 2016;131:803–20. doi: 10.1007/s00401-016-1545-1. [DOI] [PubMed] [Google Scholar]
- 4.Sen R, Sethi D, Goyal V, Duhan A, Modi S. Spinal meningeal melanocytoma. Asian J Neurosurg. 2011;6:110–2. doi: 10.4103/1793-5482.92176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tateyama M, Fujimoto T, Nakamura T, Miyamoto T. Meningeal melanocytoma occurring at epidural region of the cervical spine. Spine Surg Relat Res. 2020;4:377–9. doi: 10.22603/ssrr.2020-0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xie S, Jiang Z. Primary spinal cord melanocytoma: A case report and review of literature. Int J Clin Exp Pathol. 2019;12:669–73. [PMC free article] [PubMed] [Google Scholar]


