Sir,
The assessment of body temperature with thermal imaging scanners and/or non-contact infra-red thermometers to screen individuals for potential severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection is now widespread in most healthcare facilities, as well as in a vast array of other social environments. Nonetheless, the reliability of this strategy is plagued by biological [i.e. high rate of asymptomatic SARS-CoV-2 infection, prevalence of fever of approximately 80% in patients with coronavirus disease 2019 (COVID-19), antipyretic use] and practical (i.e. impact of environmental temperature, device accuracy) drawbacks [[1], [2], [3]]. In order to mitigate the frequent imprecision of infra-red forehead temperature devices, Hsiao et al. recently suggested that body temperature should be measured at least twice after subjects have acclimatized to the indoor environment [4]. To provide further evidence on this matter, this observational study aimed to compare forehead temperatures measured concomitantly with an infra-red thermometer and a thermal imaging scanner, both used routinely for personnel and outpatient screening before hospital access.
The study population consisted of 24 consecutive healthcare workers {16 women and eight men; mean age 42 [standard deviation (SD) 14] years, range 19–65 years} who underwent routine forehead temperature scanning before entering the University Hospital of Verona, Verona, Italy. As repeated body temperature screening with an infra-red thermometer and/or thermal imaging scanner is mandatory before hospital entry and when moving between wards or laboratories, there was no need for ethical approval or informed consent. Forehead temperature was measured 10 times on the same subject using the same thermal imaging scanner (Hikvision DS-2TD1217B-6/PA; Hikvision, Hangzhou, China; measurement range 30.0–45.0°C; mean declared inaccuracy ±0.5°C), and then, immediately afterwards, 10 times on the same subject using the same infra-red thermometer (Jumper JPD-FR300; non-contact dual mode FDA-cleared thermometer; Shenzhen Jumper Medical, Shenzhen, China; measurement range 35.0–42.2°C; mean declared inaccuracy ±0.2°C). Both devices were used in accordance with the manufacturers' instructions. All subjects were allowed to acclimatize inside the hospital building for 15 min (inside temperature 21.5–22.0°C) before temperature measurements were taken; this prevented any potential bias from outdoor air temperature on the repeated measures. Results of repeated temperature measurements obtained are expressed as mean ± SD. Individual forehead temperatures, calculated as the mean of 10 repeated measures obtained for each device, were compared using the Mann–Whitney test, Spearman's correlation [with 95% confidence interval (CI)] and Bland–Altman plots. Statistical analyses were carried out using Analyse-it (Analyse-it Software Ltd, Leeds, UK).
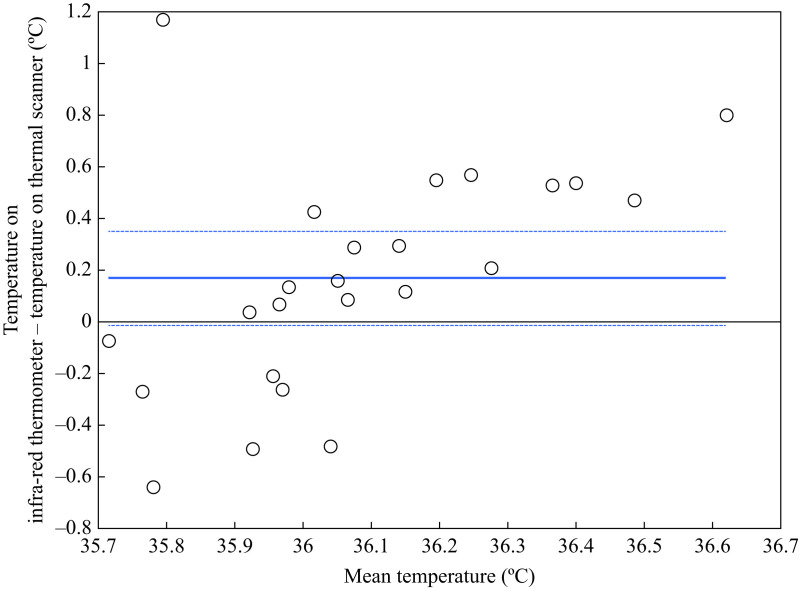
The mean imprecision of forehead temperature measurement, calculated from the mean imprecision of the 10 repeated measurements taken in each study subject and expressed as the coefficient of variation was 0.6±0.3% for the infra-red thermometer and 0.2±0.1% for the thermal imaging scanner, respectively. Correlation between values obtained with the two devices did not reach significance (r=0.19; 95% CI -23 to 0.55; P=0.382), and the mean forehead temperature recorded in all participants with the infra-red thermometer (36.2±0.4°C) was slightly but significantly higher than that measured with the thermal imaging scanner (36.0±0.2°C; P=0.034). Accordingly, Bland–Altman plot analysis revealed that the forehead temperature measured with the infra-red thermometer was, on average, 0.2°C higher (95% CI 0–0.04°C) than that measured with the thermal imaging scanner (Figure 1 ). Notably, the infra-red thermometer tended to underestimate forehead temperatures <36°C (mean bias −0.3°C; 95% CI −0.5 to −0.1°C; P=0.008), and significantly overestimated temperatures ≥36°C (mean bias 0.4°C; 95% CI 0.2–0.6; P<0.001).
Figure 1.
Bland–Altman plot of forehead temperature measured consecutively in 24 healthcare workers with an infra-red thermometer and a thermal imaging scanner upon hospital entry. The continuous line indicates mean bias, and the dashed lines indicate the 95% confidence interval.
Two important findings emerged from this study. First, although the cumulative imprecision of both devices was <1% and hence almost acceptable, the precision of the thermal imaging scanner used in this investigation was three-fold better than that of the infra-red thermometer (i.e. 0.2% vs 0.6%), such that the use of the thermal imaging scanner appears to be more precise for widespread body temperature screening, especially when testing people before accessing healthcare facilities. When thermal imaging scanners are not available, the present authors support the suggestion of Hsiao et al. [4] that repeated measurements of forehead temperature with an infra-red thermometer may be advisable to obtain a more precise measure. The second important aspect is that forehead temperature measured with the two devices did not appear to be well aligned, as attested by the poor correlation between respective values, and by the observation of a clear temperature-dependent bias (Figure 1). This implies that these two forehead temperature detectors should not be used interchangeably for systematic monitoring of body temperature of healthcare staff across an institution.
Acknowledgements
The authors wish to thank all the healthcare workers who participated in this study.
Conflict of interest statement
None declared.
Funding sources
None.
References
- 1.Oran D.P., Topol E.J. The proportion of SARS-CoV-2 infections that are asymptomatic: a systematic review. Ann Intern Med. 2021 doi: 10.7326/M20-6976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ng D.K., Chan C.H., Chan E.Y., Kwok K.L., Chow P.Y., Lau W.F. A brief report on the normal range of forehead temperature as determined by noncontact, handheld, infrared thermometer. Am J Infect Control. 2005;33:227–229. doi: 10.1016/j.ajic.2005.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Niven D.J., Gaudet J.E., Laupland K.B., Mrklas K.J., Roberts D.J., Stelfox H.T. Accuracy of peripheral thermometers for estimating temperature: a systematic review and meta-analysis. Ann Intern Med. 2015;163:768–777. doi: 10.7326/M15-1150. [DOI] [PubMed] [Google Scholar]
- 4.Hsiao S.H., Chen T.C., Chien H.C., Yang C.J., Chen Y.H. Measurement of body temperature to prevent pandemic COVID-19 in hospitals in Taiwan: repeated measurement is necessary. J Hosp Infect. 2020;105:360–361. doi: 10.1016/j.jhin.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]