Abstract
Infectious diseases and human behavior are intertwined. On one side, our movements and interactions are the engines of transmission. On the other, the unfolding of viruses might induce changes to our daily activities. While intuitive, our understanding of such feedback loop is still limited. Before COVID-19 the literature on the subject was mainly theoretical and largely missed validation. The main issue was the lack of empirical data capturing behavioral change induced by diseases. Things have dramatically changed in 2020. Non-pharmaceutical interventions (NPIs) have been the key weapon against the SARS-CoV-2 virus and affected virtually any societal process. Travel bans, events cancellation, social distancing, curfews, and lockdowns have become unfortunately very familiar. The scale of the emergency, the ease of survey as well as crowdsourcing deployment guaranteed by the latest technology, several Data for Good programs developed by tech giants, major mobile phone providers, and other companies have allowed unprecedented access to data describing behavioral changes induced by the pandemic.
Here, I review some of the vast literature written on the subject of NPIs during the COVID-19 pandemic. In doing so, I analyze 348 articles written by more than 2518 authors in the first 12 months of the emergency. While the large majority of the sample was obtained by querying PubMed, it includes also a hand-curated list. Considering the focus, and methodology I have classified the sample into seven main categories: epidemic models, surveys, comments/perspectives, papers aiming to quantify the effects of NPIs, reviews, articles using data proxies to measure NPIs, and publicly available datasets describing NPIs. I summarize the methodology, data used, findings of the articles in each category and provide an outlook highlighting future challenges as well as opportunities.
Keywords: Non-pharmaceutical interventions, COVID-19, SARS-CoV-2, Behavioral changes
1. Introduction
Our interactions, movements, and behavior affect the spreading of infectious diseases. The unfolding of such illnesses, in turn, might drastically affect our actions. Although obvious, particularly during a pandemic, we still do not have a well understood and developed theory or even an accepted standardized approach to account for this observation. Capturing the feedback loop between human behavior and infectious diseases is one of the key challenges in epidemiology [1]. Arguably, it can be considered as the hard problem of epidemiology.
Even before the COVID-19 pandemic, the literature tackling this issue was vast [2], [3]. One of the reviews on the subject noted a key challenge: only 15% of the papers are based on empirical data, most models being “purely theoretical and lack[ing] representative data and a validation process” [2]. In the small set of papers informed, at least partially, by empirical data we find interesting approaches. Researchers have designed games [4], [5], surveys, and used datasets (e.g., television viewing) to infer social-distancing as well as attitudes, altruism and self-interest in the context of vaccinations [6], [7], [8], [9], [10], [11]. Others have used surveys to measure risk perception during the H1N1 2009 pandemic [12], [13], to estimate the perceived severity of the SARS outbreak [14], or characterize behavioral changes induced by the seasonal flu [15]. Data from social media have been used to estimate the spread of awareness in the population during the H1N1 2009 pandemic [16], [17], [18]. Another type of approach used epidemiological data (such as incidence) to calibrate diseases and behavioral models [19], [20]. A notable example of this method is Ref. [21] where the authors used historical records from the 1918 influenza pandemic to fit three different models, one of which included behavioral responses, to determine the origins of the multiple epidemic waves observed.
Despite these efforts, the scarcity of direct observational data describing the feedback between human behavior and diseases represented a major obstacle. The reader might have noted the use of the past tense which is not, like many others in the text, a grammatical mistake. In fact, in the last year or so, things have dramatically changed. The COVID-19 pandemic took over the world and unfortunately, non-pharmaceutical interventions (NPIs) have been one of the only weapons against the disease in the first months of the emergency. NPIs refers to a wide range of both top-down (i.e., governmental) and bottom-up (i.e., self-initiated) measures aimed at interrupting infection chains by altering key aspects of our behavior. Travel bans, curfews, social distancing, bans of social gathering, face masks, increased hygiene, remote working, school closures, and lockdowns are examples. The heterogeneity of such measures across space and time as well as the magnitude of the changes they induced offer an unprecedented opportunity to understand, measure, and model the link between human behavior and infectious diseases. Modern technology and many Data for Good programs created by tech giants such as Google, Apple, Facebook by major mobile phone operators such as Vodafone, Telefonica, Orange and by smaller companies such as Cuebiq, SafeGraph, Unacast have provided unparalleled lenses to capture the effects of both top-down and bottom-up NPIs. In this background, I aim to summarize some key observations, data produced, approaches, and knowledge developed in the first turbulent year of the COVID-19 pandemic.
The incredible work of the research community makes it extremely hard to review manually all papers related to COVID-19. Just to give an idea of the scale, a query on PubMed for “COVID” returns more than 71,000 results. On Google Scholar we can find instead more than 135,000 matches. Within this large body of work, some lines of research are smaller than others. However, NPIs have virtually affected all aspects of human activity. Consequently, we can expect the research on the subject to be vast and diversified across many communities. As I write we are in the middle of the second wave in Europe. A new, potentially more transmissible, variant has emerged in the UK. Hence, many more papers are being started, finalized, and published. Considering my research interests and expertise the focus of this work is directed mainly towards the epidemiological implications of NPIs. From the development of epidemic models to surveys aimed at quantifying awareness and their adoption. Hence, I have opted for PubMed to gather a big part of the papers in the sample. Inevitably, this introduced a bias towards interdisciplinary, biomedical, and life science journals. Surely a search on the ISI Web of Knowledge would provide a more exhaustive picture of the implementation and effect of non-pharmaceutical interventions during the pandemic. As described below, I have not done a systematic search on PubMed by, for example, carefully crafting a set of target keywords via an iterative or a consultation process. Hence, it is important to stress how this review is not systematic nor complete. Furthermore, as described in details below, this review is not the first attempting to describe the research centered around NPIs induced by COVID-19. However, it offers some novel contributions. First of all, it is not focused on a particular subject such as for example epidemic models or data driven approaches to measure NPIs. The group of papers that are considered here cover different areas that range from epidemic models and surveys to comments/perspectives and articles aimed at quantify the effects of NPIs. Hence, the review provides an overview of many different, often complementary, disciplines and methodologies. The review is organized around a taxonomy that classifies the research in seven main categories and many more sub-categories. The classification has been developed to facilitate the narrative flow and to help readers navigating the large body of reviewed articles potentially jumping directly to particular aspects, topics, of interest. All papers together with some of their key features such as sample size, geographical targets of the research, modeling approach used, and type of data adopted are showcased in several tables aimed to simplify access and navigability for the interested readers. Furthermore, the review offers some scientometric analyses that highlight the impact of the articles reviewed (in terms of citations), showcase the scale of the research efforts across fields (in terms of number of authors and countries involved), accent the global focus of the research providing information about the geographical targets (if any) of the studies, and identify the broad set of journals that published the papers matter of review. Overall, this review covers a large and diverse body of research providing a glimpse of the breadth in the area and highlights key results as well as the interdisciplinary range of approaches used.
2. Data collection, inclusion principles, annotation, and classification
Since the beginning of the pandemic, I have been following the research aimed at modeling the unfolding of the virus and at characterizing its societal effects. In doing so, I have compiled a list1 of influential papers that have shaped the research in the area and that, I believe, everyone would expect to see. Clearly, this list is biased by the research communities I am part of, those I follow, and my perception. Thus, I have thought to drastically extend the list using PubMed. To this end, on November 10th I have submitted the following query: ((non-pharmaceutical intervention) OR (non pharmaceutical intervention)) AND (COVID). The query targeted papers that mention explicitly NPIs and returned results. After some thinking on November 11th I have further extend the search querying PubMed for: (behavioral changes) AND (COVID). The idea was to expand even more the corpus by including papers that studied the impact of COVID-19 on our behaviors without mentioning explicitly NPIs. The second search returned results. In both cases the query was run without any particular other specification such as constraining the search to titles or abstracts. I have scanned titles and abstracts of these papers manually eliminating those referring to drugs trails, drugs development, clinical trials, clinical procedures and research protocols. I have removed duplications and papers outside the scope. Furthermore, I have kept only articles written in English. At the end of the process, and considering the initial list, I was left with papers which constitute the corpus of this review.
It is important to stress one more time how this is just a small subset of all related work. For example searchers in PudMed for restrictions AND COVID, lockdown AND COVID, (control measures) AND COVID and (social distancing) AND COVID return more than , , and results respectively. Furthermore, any systematic review should play with synonymous and similar words. This monumental work, which would end up with well more than fifteen thousand papers is left for the future and it would benefit from a large collaboration.
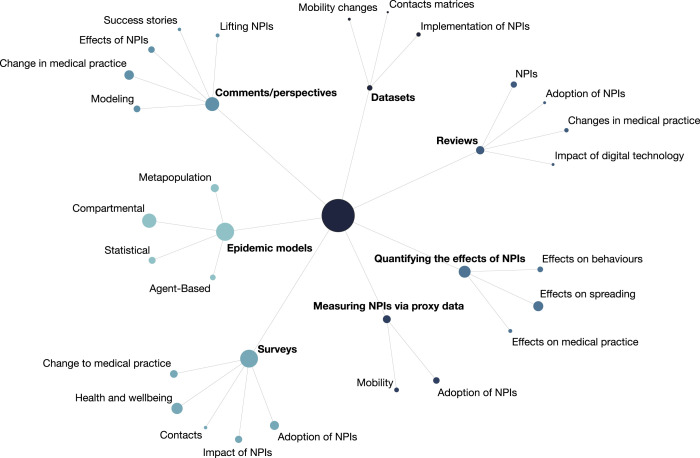
For each paper, I have manually extracted the following information: DOI, countries from author’s affiliations, countries focus of the study (if any), journal and month of publication. Furthermore, I added annotations to describe which method was used (i.e., survey) and other relevant information (i.e., sample size, type of data used). After a first sweep, I have done several others to classify the corpus and create a personal, machine readable, taxonomy reported in Fig. 1.
Fig. 1.
Schematic representation of the classification scheme. The central node describes all articles. The size of each node (i.e., category) is proportional to the number of articles.
At the higher level, by considering the most representative methodology and/or aim of each paper, we find categories:
-
1.
Epidemic models (29%): papers aimed at describing the unfolding of COVID-19 via epidemic models;
-
2.
Surveys (28%): papers aimed at characterizing the impact of NPIs on several areas of human activity and/or their adoption via surveys;
-
3.
Comments and/or perspectives (17%): papers that offer a reflection/perspective on NPIs in particular contexts;
-
4.
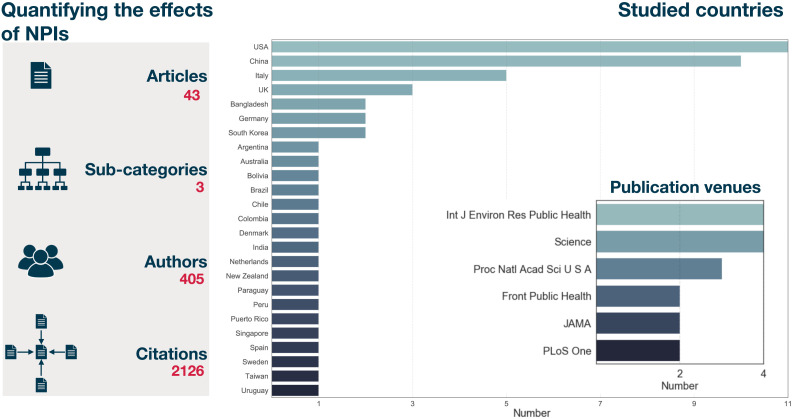
Quantifying the effects of NPIs (12%): papers aimed at characterizing the effects of NPIs on epidemic indicators, behaviors and activities;
-
5.
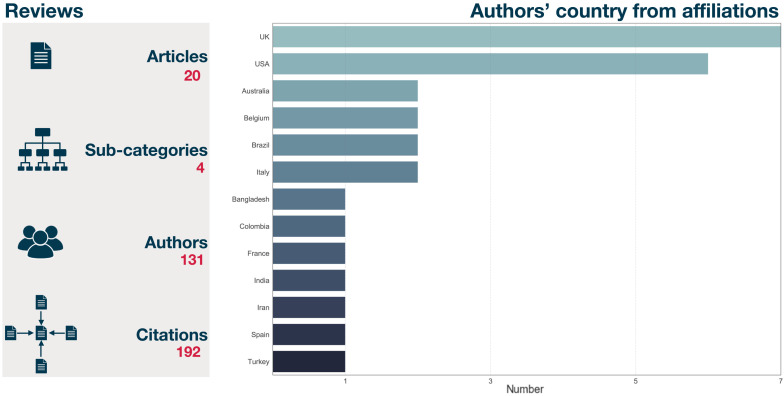
Reviews (6%): papers presenting a summary of the literature about NPIs in different contexts and areas;
-
6.
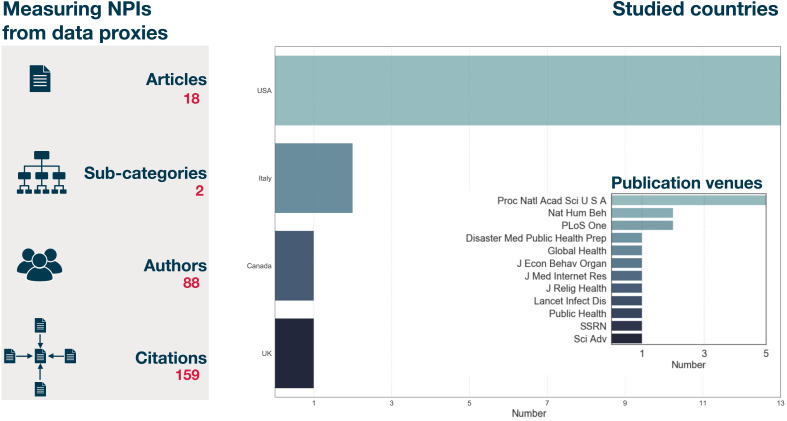
Measuring NPIs via proxy data (5%): papers monitoring and measuring NPIs via data proxies;
-
7.
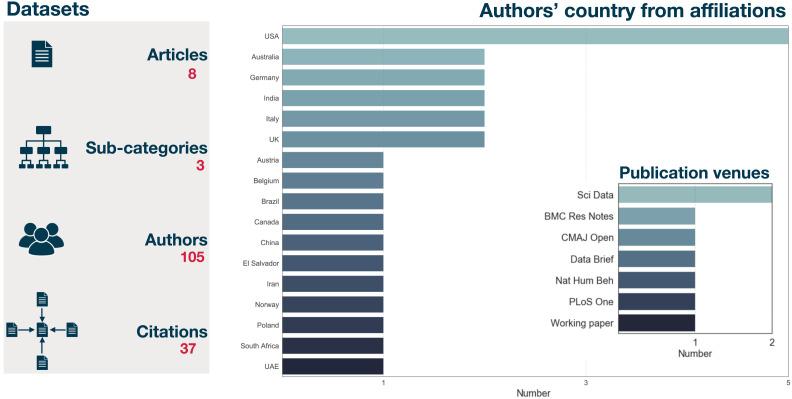
Datasets (2%): papers describing and sharing data collections relevant for the study of NPIs.
As in any classification scheme not all cases are clear cuts and there is some overlap. To simplify the analysis, I have assigned each paper to one and one only main category. Clearly, this implies same level of arbitrary in the classification.
By using Semantic Scholar 2 I have also extracted information about the authors and citations of each paper. Remarkably, these papers have been written by more than authors (note that some were not indexed) and accumulated more than citations.3 In Table 1, I provide the breakdown of number of authors, citations, median of citations and the top three articles (per number of citations) in each category. Epidemic models are the most cited category in the sample both for total number and median of citations. Surveys are the least cited considering the median of citations of the articles in the group. It is important to stress how this literature is very recent. Some papers have been published just one or two months ago hence they did not have enough time to accrue citations.
Table 1.
Number of authors, total number of citations, median number of citations, and top three papers for citation for each of the categories. Citations and authors names have been extracted via Semantic Scholar on December 19th, 2020.
| Category | Authors | Total Citations | Median citations | Top three articles for citations |
|---|---|---|---|---|
| Epidemic models | 774 | 4859 | 5 | 1st [22], 2nd [23], 3rd [24] |
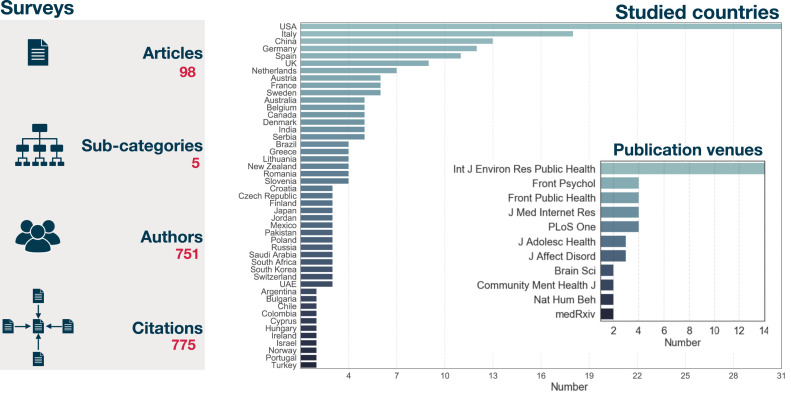
| Surveys | 751 | 775 | 1 | 1st [25], 2nd [26], 3rd [27] |
| Comments and/or | ||||
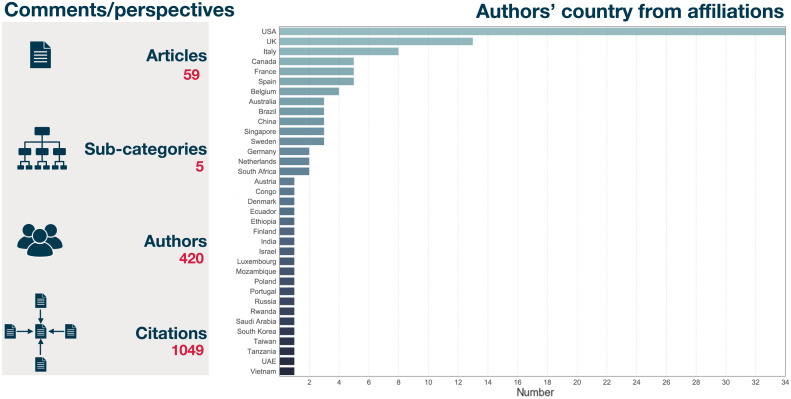
| perspectives | 420 | 1049 | 4 | 1st [28], 2nd [29], 3rd [30] |
| Quantifying the effects of NPIs | 405 | 2126 | 2 | 1st [31], 2nd [32], 3rd [33] |
| Reviews | 131 | 192 | 3.5 | 1st [34], 2nd [35], 3rd [36] |
| Measuring NPIs with proxy data | 88 | 159 | 2 | 1st [37], 2nd [38], 3rd [39] |
| Datasets | 105 | 37 | 1.5 | 1st [40], 2nd [41], 3rd [42] |
3. Epidemic models
After the first suspicious cases of pneumonia in Wuhan were linked to a new virus, a set of key questions rapidly emerged. How infectious and fatal is it? How does it transmit? How many people are already sick? Can it be contained? What are the chances of importation in other countries? Is this the start of a new pandemic? When the virus was detected in Singapore, South Korea, France, UK, Italy, USA answers to many of these questions were still unclear. However, it did not take long to understand that widespread community transmission was probably taking place. Testing was initially targeted towards symptomatic individuals with travel history in China and the virus was spreading undetected via what is called cryptic transmission. Cases, deaths and hospitalizations started to double at increasing pace in many countries. Asian states took draconian measures early. Europe reacted too late. Despite concerning news coming for Asia, the first European countries hit by waves of deaths and hospitalizations assumed, just days before, to be in perfect control. Emblematic is what the major of London declared the same days when Italy started a national lockdown: “we should carry on doing what we have been doing” [43]. Things escalated quickly and in one week also the UK entered in a national lockdown. After the efforts and unprecedented NPIs put in place around the world, epidemic curves started to level off and also thanks to the good weather COVID hospitals started to empty, deaths rapidly decreased, and number of cases showed clear downwards trends. At this stage, the key questions revolved around how to relax the measures and reopen society. Should we keep the schools closed? Restaurants and pubs? What about international borders? Should face masks be mandatory? Summer , in the northern hemisphere, has been extremely better than the dark months of spring. However, the infections started to ramp-up quite quickly in September and October. While countries have developed quite different strategies to manage winter, it became unfortunately clear that the virus was winning one more time. As I write these words, we are in the second national lockdown in England and from tomorrow some of the restrictions will be lifted. The questions now revolve around the Christmas break. What should people be allowed to do? How many people should meet during the holidays? What about Christmas shopping? One more time we are all facing a very challenging act balancing risks with hopes to go back to semi-normal life.
Although, the set of questions during the different phases of the pandemic changed many of the answers have been provided and/or informed by epidemic models. Not all suggestions coming from the Science, as they say here in the UK, have been followed by our leaders, but it is clear that forecasts, predictions, scenario analyses coming from a variety of models were key to inform response strategies. In this section, I will revise some of the literature produced in the area. All models target the same virus, but the type of approach, data used, assumptions, how NPIs are modeled, limitations, strengths, predictive power or predictive ambitions are extremely diverse.
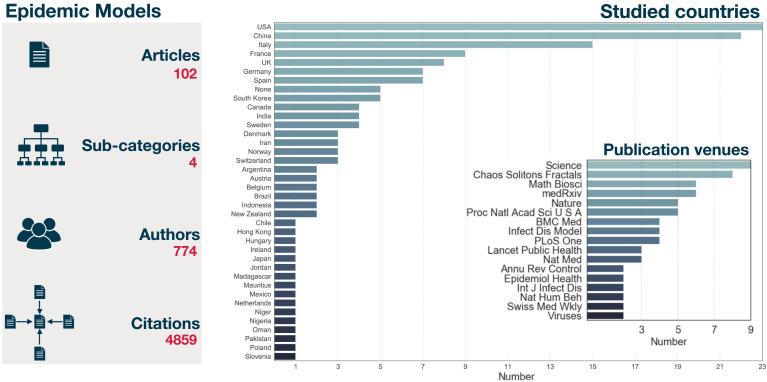
Before diving into the details, few words about the subset of research I will be reviewing. First of all, the large majority of models was tested or motivated by observations in one single country. USA, China, Italy, France and the UK are the most commonly used countries (see Fig. 2). The list does not come as surprise considering the epicenter of the pandemic, data availability as well as the evolution of the pandemic in USA and Europe. However, few models in the sample consider hundreds of countries [22], [44], [45], [45], [46], [47]. Second, this body of research has been published by authors with affiliations in countries. USA, UK, China, and Italy are the top of the list. Third, there is a large variety also in terms of publication venues (see Fig. 2). In fact, the sample of epidemic models has been published in venues (including papers in medRxiv). Science, Chaos Solitons Fractals, Mathematical Biosciences, medRxiv, Nature, and PNAS are at the top of the list. Finally, these papers have been written by more than authors and received more than citations. A median of citations per article.
Fig. 2.
Total number of authors and citations of the papers in this category on the left. Note that these numbers are estimated from Semantic Scholar. On the right (top) histogram describing the number of countries subject of study in this category. Note how few papers that studied hundreds of countries are not counted in the histogram. On the right (bottom) most represented publication venues of the category. To improve visibility I am showing only journals featuring at least two articles.
3.1. Classification
After analyzing the whole subset of papers and considering the typology of model adopted, I have identified categories. In particular:
-
1.
Compartmental models: consider a single population divided according to health statuses and in some cases age structure;
-
2.
Metapopulation models: are based on a network of subpopulations (i.e., cities, regions, countries) connected by mobility;
-
3.
Statistical models: capture the evolution of the epidemic inferring key parameters and behaviors from data;
-
4.
Agent-based models: capture the spreading patterns at the level of single individuals.
In Table 2 I present the full set of articles grouped according to the categories and in some cases sub-categories. I also report the country or countries used, if any. Here, same papers might be present in multiple categories. In fact, some of them adopted, often compare, different methods.
Table 2.
Summary of the epidemic models in the sample. The first column describes the main categories, the second the sub-categories, the last the country/countries focus of each study and the references.
| Category | Subcategory | Country/countries of study and reference |
|---|---|---|
| Compartmental | SIR-like |
Brazil, China [48]; China [49], [50], [51]; China, Italy [52]; China, France, Iran, Italy, South Korea, USA [53]; France, Iran, Italy [54]; Germany [55]; India [56]; Italy [57]; USA [58]; 187 countries [45]; several European countries [44], [59] |
| SIR-like age structured |
China [60], Italy [61], 143 countries [47] |
|
| SEIR-like |
Argentina, Japan, Indonesia, New Zealand, Spain, USA [62]; Canada [63], [64]; Canada, Germany, Italy [65]; China [66], [67], [68], [69]; China, Italy [70]; China, UK [71]; Germany [72]; India [73], [74]; Indonesia [75]; Ireland [76]; Mexico [77]; Pakistan [78]; South Korea [79], [80]; Switzerland [81]; USA [82], [83], [84], [85], [86], [87], [88], [89], [90]; Theoretical [91], [92] |
|
| SEIR-like age structure |
China [23]; UK [93], [94], [95]; France [96], [97]; Germany [98]; Madagascar [99]; Mauritius, Niger, Nigeria [100]; South Korea [101]; UK, USA [102]; USA [103]; Theoretical [104] |
|
| SEIRS-like | USA [105] | |
| Metapopulation | Age unstructured |
Canada [106]; China [107], [108], [109], [110]; France, Poland, Spain [111], [112]; Jordan [113]; Italy [114], [115]; USA [116], [117]; Europe [118] |
| Age structured | Chile [119]; Hungary [120]; Spain [121]; Sweden [122]; USA [123], 200+ countries [22] |
|
| Statistical | NA | Austria, Belgium, Denmark, France, Germany, Italy, Norway, Spain, Sweden, Switzerland, UK [124]; Brazil [125] China [126], [127]; China, Iran, Italy, South Korea [128]; Hong Kong [129]; India [130]; Oman [131]; Slovenia [132]; USA [133]; 190 [46]; 11 European countries [24]; 41 countries [134] |
| Agent-based | NA | China [66]; China, Italy, USA [135]; Canada [63]; Italy [136]; USA [137], [138]; Theoretical [139], [140] |
3.2. Compartmental models
Compartmental models are the most common in the category. Probably this does not come as surprise since they require the least amount of data about the population under study. Nevertheless, they are a proven and powerful tool for describing the evolution of infectious diseases. It is important to note how compartmental models are featured also in other categories of models discussed below. In fact, it is extremely common to describe individuals’ progression in the different phases of a disease (i.e., natural history of the disease) via compartments, each one representing health statuses. Susceptible, infectious, asymptomatic infectious, hospitalized, and recovered are classic examples. Other modeling approaches use a compartmentalization of the target population as one of the elements of the theoretical construct. Explicit social contacts structures, travel patterns and other features are added to describe key epidemiologically behaviors. In the category discussed here instead, these other details are simplified and expressed via effective functions, contact matrices, and rescaling of parameters.
As mentioned, compartmental models split the population according to health statuses. The number and type of compartments change as function of the disease under study, according to the hypotheses about the mechanisms driving the spreading of the virus and the behavior of the population. All compartmental models in the sample, and there are many, are a variation of two basic archetypes: SIR or SEIR. The sequence of letters, describing each compartments, captures the natural history of the disease. In SIR models susceptible individuals, in contact with infectious, develop the disease and move from to . This transition is often written as where is the transmission rate. The compartment describes recovered individuals that are removed from the disease dynamics. The transition from to is spontaneous and can be written as where is the recovery rate. is the infectious period. In SEIR models, we have another compartment describing individuals that were exposed to the virus but not yet infected. Thus the transmission of the disease can be written as . As soon as the viral load reach certain levels exposed become infected . The sum of and is called generation time, defined as the average time from an infection to the next. In these archetypes, the per-capita rate at which susceptible contract the infection, the force of infection, is often written as . Hence, it is proportional to the transmission rate and to the probability of meeting an infectious individual in a homogeneously mixed population. These models are characterized by another key quantity called basic reproductive number, , defined as the number of secondary infections generated by an index case in an otherwise fully susceptible population. In case is above one the disease is able to spread and affect a finite fraction of the population. In SIR and SEIR models it is simple to show how . In more complex models with several types of infectious compartments the expression is generally different but it can be calculated via the so called next generation matrix approach. See Ref. [141] for a very accessible and clear review.
The majority of models is the sample follow the SEIR archetype thus can be classified as SEIR-like models. If you ever had to quarantine after crossing a border, you have experienced first hand the reason why including the compartment of exposed is important: the incubation period peaks within few days but it has been reported to possibly extend for more than one week. As we will see below, the general structure of these models is that of a simple SEIR model but typically several other compartments are added to account for individuals that are hospitalized, different types of manifestation of the disease (i.e., symptomatic, asymptomatic, pauci-symptomatic), as well as behavioral classes (i.e., individuals wearing face masks, reducing their contacts because concerned). COVID-19 is a quite complex disease with a wide range of manifestations that affects people’s health and behaviors in different ways.
A subset of both SEIR and SIR like models includes another important element: the age-structure of the population. In fact, COVID-19 does not affect age classes homogeneously. Older individuals have a much higher risk of hospitalization and mortality [142]. Furthermore, stratifying the population for age classes allows to account for the fact that contacts are not homogenous across age brackets. Including empirical contact matrices, which describe the rate of contacts within and across age classes, allows to move towards a more precise representation of the spreading of the virus and to account, explicitly, for different infection fatality rates (IFRs). Furthermore, the ability to include contacts patterns across age groups allows to split contacts taking place at school, work, and in other contexts. This is particularly important for models which aim to measure the impact of school closure, remote working, and other NPIs. After this general prelude, let us dive into the research that adopts compartmental models to study the spreading of COVID-19.
We start considering the body of modeling work based on SIR-like models. This subset of papers studies the effects of isolation and quarantine policies [49], models NPIs as effective changes of the parameters [44], [45], [48], [50], [52], [54], [55], [56], [57], [59], investigates the impact of different policies [53], [58], and defines the conditions for the optimal control of the spreading [51]. In the following, I will highlight some of these approaches.
Ref. [49] presents a modification of the SIR scheme including a compartment to account for the portion of infectious individuals that are either quarantined or adopt other forms of NPIs, which effectively nullifying their ability to spread the virus. Furthermore, the model also considers that a portion of susceptible adopts NPIs and as result is removed from the epidemic dynamics. Interestingly, these two relatively simple modifications of the classic SIR model are enough to explain the sub-exponential growth observed in China. In fact, without any interventions a SIR model would imply an exponential growth in the early phases of the epidemic which is not what has been empirically observed in the Chinese context. A number of papers propose approaches to account for NPIs as effective variation or modulation of key SIR parameters such as the transmission rate and recovery rate which are either fitted from data or set a priory in scenario analyses. Two papers focusing on India [56], Italy and China [52] extended the force of infection including a time-varying parameter to modulate the bare transmission rate . The modulation is function of the NPIs put in place to curb the spreading of the virus. By fitting the model to epidemic indicators Ref. [52] estimated a for Italy above and in Hunan around in the early phases of the pandemic. A similar model has been proposed to infer the impact of NPIs on the epidemic evolution in Germany [55]. The author extended the SIR archetype considering that the transmission rate can change at certain points , with , from to over days. Hence, the index runs over the possible change points, each covering several days. For simplicity they assume a linear variation. The parameters , , among others are obtained via a Bayesian Markov Chain Monte Carlo (MCMC) comparing each potential model with real data. Interestingly, they observed that only the compound effects of NPIs, put in place at different moments, was enough to bring the reproductive number below one. A similar estimation framework has been used to model the pandemic in Brazil and China [48]. In this paper however, authors impose a precise functional form of the variation of the transmission rate: for where is the value in absence of any interventions, is the modulation introduced by NPIs and is the time in which the interventions are put in place. A Bayesian framework is also used in Ref. [44]. Here authors provide a picture of key epidemic indicators such as for countries which can be explored via a dashboard.4 In this model the transmission rate is written as (remember that is the recovery rate). The reproductive number is considered to go from to with as function of the time due to NPIs implementation. The results indicate that the timing of NPIs is key for an effective suppression of the virus. Ref. [45] adopts an extension of the SIR archetype, considering time-varying recovery and infection rates, to model the spreading of COVID-19 in countries. The results, that can be explored via an interactive tool,5 are obtained fitting the parameters to the real epidemic data. The comparison between different countries highlights the heterogeneity in the response. For example Iceland was able to drastically reduce since early April thus suppressing the spread with efficacy. Sweden in contrast, opted for a mitigation strategy, and as result the decrease of was much slower. In Ref. [57] authors extend the basic SIR model including, among other things, deaths and writing the transmission rate as thus as a linear combination of two basic rates. The first weights more in the early phases of the spreading. The second kicks in when the NPIs are in full swing. Similarly they consider the recovery and mortality rates as linear combinations of so called basis functions. A key point of the methodology is defining the shape of such functions. Interestingly the authors adopt sparse identification techniques applied to the real epidemic data finding a combination of exponentials and polynomials to be the best fit. The model, applied both to national and regional data in Italy, show the effectiveness of the first lockdown (that was implemented in the first half of March 2020) especially in the regions more affected. In Ref. [53] authors use a mix of econometric and epidemiological methods to quantify the effect of a NPIs policies on the evolution of the pandemic. The problem formulation is similar to those linking economical policies to economic growth. The first are substitute by NPIs. The second, by the epidemic growth. In the early stage of an epidemic it is easy to show that, according to an SIR model, where is . The authors link this observable to the set of NPIs policies implemented by the country , in subnational unit , in day as:
| (1) |
is the growth rate in absence of any policy, accounts for weekly patterns in data reporting, accounts for variations in reporting methods, which might induce jumps in the data, describes the policy adopted, the impact of each policy in the growth rate and is the classic error term. In other words, the growth rate is assumed to be a linear combination of each policy implemented. By fitting the model to data from China, South Korea, Iran, Italy, France and USA, the authors establish that the portfolio of measures implemented in these countries was enough to reduce the transmission and were beneficial in terms of health outcomes. The results also show the heterogeneous impact of the measures across countries. For example the impact of school closures on daily growth rate appear to be higher in Italy than France. Ref. [58] used online searches and mobility data to estimate the effect of heterogenous implementation of NPIs in the USA. Interestingly, they found that some specific locations (such as churches) saw an increase in attendance locally while, as result of stay home orders, they decrease nationally. This counterintuitive observation shows the effect of heterogeneity in NPIs. Local closure might induce some individuals to travel further for the same activity. The effect of this type of adaptive behavior might increase the number of cases. In fact, the changes in mobility might induce mixing of otherwise separated groups, thus accelerating the spreading. They confirm this intuition with a simple model that divides a population of individuals in gatherings. They assume that a fraction closes at time due to the implementation of NPIs. As result, a fraction of the population does not complies with the measures and visit the gatherings still open. In these settings, the dynamics of the disease split at time in two. On one side, the open gatherings are still participating to the spreading of the virus. On the other, closed gatherings can just recover the individuals infected before. The results clearly show that the patchy adoption of NPIs induces worse health outcomes and highlights the negative effects of inconsistent geographical implementation of NPIs.
Three articles expanded the SIR modeling framework considering age structure and contact matrices [47], [60], [61], [102]. In Ref. [47] authors study the impact of COVID-19 and the effects of different NPIs strategies in low and middle income countries. Including age brackets and the share of contacts within/across them allows to account explicitly for the demographic distribution and mixing patterns of the population under consideration. This becomes very important when comparing the spreading of COVID-19 in different socio-economic contexts. In fact, low and middle income countries are typically younger populations, thus less at risk of serious forms of COVID-19. However, the social stratification is such that older individuals have higher contacts with other age brackets respect to what happens in higher income settings [47]. Hence, there is smaller fraction of the population at high risk, but that fraction is more intensely connected with younger individuals thus more prone to be exposed to the virus. This interplay is fully explored by the authors which also consider a range of comorbidities, healthcare availability and quality. Furthermore, the authors consider two possible approaches in the management of the pandemic. The first is suppression of the first wave by strict NPIs which pushes below one. The second instead is mitigation, which reduces to values close to one. Suppression drastically limits the burden in the short run, but comes with high socio-economic costs and since it limits the spreading does not form the necessary immunity to avoid multiple peaks. Mitigation, allows for less stringent NPIs but is linked to a much higher number of cases/deaths and pressure to the healthcare system. While younger demographic structures might suggest that mitigation in low and middle income settings might be a more suitable strategy respect to high income contexts, the higher levels of intergenerational mixing, limited resources in terms of healthcare facilities, and comorbidities impose great deal of caution. It is interesting to notice how the response of these group of countries has been put in place early respect to the local circulation of the virus. The paper also point out the challenges and different angles governments have to consider when developing a strategy against COVID-19. Authors in Ref. [102] consider two different strategies to curb the spreading of COVID-19 in schools. In doing so, they consider a stratification of the population (i.e., school) considering different cohorts (i.e., classes), day of infection (to account for different viral loads) and study the effects of NPIs that (i) isolate students with fever (ii) reduce the school week to four days. After fitting the model to the spreading of ILIs and COVID-19 in school settings, the authors found that, in the context of COVID-19, reducing the school week is more efficient measure.
The body of modeling work based on the SEIR scheme touches similar themes to those just mentioned, but due to the larger number of articles, there are also some new interesting angles. In particular, we find papers focusing, among other things, on the effects of face masks [82], [85], [86], [87], [89], capturing different aspects of NPIs [64], [67], [69], [70], [71], [73], [74], [75], [77], [79], [80], [81], [83], [84], [90], studying the problem of optimal control of the pandemic [72], [76], [78], [88], investigating approaches to lift measures put in place in the first wave [62], [63], [65], model the possible exposure to the virus via droplets or fomites [91], [92], and consider the impact on the health care infrastructure of COVID-19 and seasonal flu in the winter [68].
In Ref. [85] authors present a detailed scenario analysis of the winter season in each US state. Interestingly, in their model not only is considered function of time, but the force of infection is modulated by a mixing parameter defined in such a way that where and describe pre-symptomatic and symptomatic individuals. Furthermore, they develop a pipeline modeling the link between the transmission rate and cases, deaths as well as a range of covariates such as mobility indicators, population density, smoking rates, masks use via a regression. In doing so, they build a linear regression model to link the implementation of different NPIs (e.g., school closures, stay home orders) on mobility considering data from Google mobility reports,6 Facebook data for good,7 SafeGraph8 and Descartes laboratories.9 Using the observations for all these variables in the first wave, they study the possible scenarios in the winter considering an adaptive strategy where NPIs are reinstated if a certain threshold of mortality rates is reached. The results confirm the effectiveness of NPIs and show that a 95% adoption rate of mask covering could be crucial to mitigate the effects of disease resurgence. Furthermore, they estimate that universal face covering could help save more than hundred thousands of lives. The importance of face masks has been also shown in Refs. [82], [86], [87], [89]. In more details, authors in Ref. [86] consider a model featuring susceptible, exposed, infectious, asymptomatic, critical (ICU), and recovered individuals. Furthermore, they split the population separating susceptible and exposed individuals under quarantine, as well as isolated infectious people. In doing so, they also assume that a fraction of the population adopts face masks that have an efficacy modeled as a free parameter. Interestingly, they apply the model to the US and New York state observing that, within the assumptions made, an adoption rate of 70% in New York state and 80% in the USA of mask with efficacy above 70% could lead to an elimination of the virus. Ref. [87] proposes a different methodology by modeling the adoption of face masks splitting the population and compartments (susceptible, exposed, symptomatic infectious, asymptomatic, hospitalized, recovered and dead) in two: those wearing face masks and those not wearing them. Using data and observations from New York and Washington state their model suggests that high adoption rates (80%) even of moderately effective masks (50%) could seriously impact the spreading of COVID-19 by reducing projected deaths by over a two months period. Authors in Ref. [83] manage to account super-spreading events and thus study the effects of NPIs aimed at chopping off the tails of transmission rates. Typically, models that consider this aspect are based on explicit contact networks capturing the heterogeneity of social interactions. Compartmental models are typically based on the assumption of homogenous mixing which by definition neglect the features of real contact patterns. The authors propose accounting for the heterogeneity in transmission rates by considering the effective (population-wide) effect of having individual transmission rates following a gamma distribution. In doing so, they are able to model the effect of NPIs targeting super-spreading events, by affecting the aforementioned distribution. Furthermore, they assume a time varying where modulates the implementation of NPIs. Such measures induce variations in the transmission rate distribution. The model, fitted to data from several counties across USA, shows that targeted NPIs that cut the right tail of transmission rates distribution are more efficient than social distancing measures at the population level (affecting the average rather than the extreme values). This result is in line with classic results from epidemic spreading on heterogenous networks which show that targeted measures aimed at isolating few central individuals are much more efficient than average measures across the whole system [143], [144]. Two papers based on data and observations in South Korea model NPIs considering that susceptible individuals might adopt protective behaviors as function of the number of infected individuals in the population [79], [80]. In particular, they adapt the model proposed in Ref. [145] where there are two classes of susceptible: and . The latter describes scared individuals (F stands for feared) of infection that change behaviors to reduce their risks. The transmission rate for these individuals becomes where is the protection gained. People join the compartment as function of the number of individuals in self-isolation. This transition is not modeled as mass-action. Thus it is not driven by the fraction of individuals in self-isolation but by their absolute number. In fact, in a context such as South Korea, where the extinction efforts have been quite successful, the news of few cases might induce behavioral changes. Feared individuals might move back as function of the fraction susceptible (not scared) and recovered individuals. The authors fit the model to the epidemic curves at the country and/or regional level to estimate the extent to which behavioral changes, as modeled, have been adopted. They show that, as expected, regions with more cases are compatible with a lower adoption. A similar model has been proposed in Ref. [75] in the context of Indonesia. Here, susceptible individuals are split in two: unaware and aware of the risks of infection. People move in the aware compartment with a constant rate which models a media effect. Aware individuals are characterized by a lower transmission rate and might relax their behavior spontaneously. The model includes also undetected and detected infectious compartments. People in the first might be tested and transition in the second compartment. The results show how a combination of effective media campaigns and aggressive testing might reduce drastically the burden of the disease. Ref. [77] proposes similar approach. In fact, the authors assume that a fraction of the population adopts NPIs while does not. The split takes place at the time when the measures are put in place. The transmission rate is modeled as linear decreasing function of time, which goes from to within a certain time window after the start of NPIs. The authors fit the model to the epidemic data from Mexico City finding that NPIs were critical to contain the first wave and that the data is compatible with high level of adoption rates. Ref. [64] proposes a SIER-like model splitting compartments in two accounting for those adopting physical distancing and those that do not. By using a Bayesian approach the model is fitted to the evolution of the first pandemic wave in British Columbia (Canada), few US States and New Zealand. The results for Canada suggest a widely adoption of physical distancing in the Canadian province and indicate that NPIs have reduced by about 80% social contacts bringing the below its critical threshold. Similar results are found for New Zealand. In the USA the results suggest a reduction in New York, Florida, and Washington but not in California. In Ref. [67] authors study the pandemic in Wuhan with the aim to reconstruct its progression as function of the interventions. In doing so, they propose an extension of the classic SEIR model considering individuals traveling in and out the population under study (note that this is modeled as an effective in–out flow) before the cordon sanitarie. The initial ascertainment rate is estimated considering the cases imported from Wuhan to Singapore which, due to aggressive surveillance, is assumed to have detected them all. Furthermore, the infectiousness of unascertained cases is considered to be 55% respect to infectious individuals. The incubation period is set to be 5.2 days and the pre-symptomatic infectious period 2.3 days implying a latent period of 2.9 days. Finally, they consider the transmission and ascertainment rates possibly different in four time periods describing the different phases of the pandemic. The values of these rates are estimated from data using Markov Chain Monte Carlo methods. The results highlight the features of the pandemic: high covertness (87% of infectious were unascertained) and transmissibility ().
Several papers studied the implementation of NPIs as an optimal control problem [72], [76], [78], [88]. Authors in Ref. [76] consider as optimal strategies that reduce the disease burden as well as their socio-economic costs. It is interesting to notice how the structure and weight of the different components of the cost function are arbitrary and dependent on the ultimate goals. The authors propose one that puts high value to human lives and assumes that economic activity, similarly to the transmission rate, is proportional to the number of contacts. This assumption allows to simply link NPIs to economic costs. Using data and observations from Ireland the authors found that disease suppression is preferable to mitigation. Ref. [72] confirms that balancing economic costs of NPIs and avoiding the overflow of health care facilities in an optimal mitigation strategy might be a “tightrope walk close to the stability boundary of the system”. Furthermore, authors of Ref. [88] points to the fact that the effectiveness of optimal mitigation strategies depends on the details of key epidemiological parameters and on the exact impact of NPIs. Hence confirming the challenges linked to the definition of optimal mitigation strategies.
A set of papers focus on the effects of relaxing NPIs after the first wave [62], [63], [65]. Authors in Ref. [62] consider an extension of the SEIR model including confined susceptible, quarantined and deceased individuals. They model recovery and transmission rates as function of time fitted to the data from the first wave in different countries (Argentina, Indonesia, Japan, New Zealand, Spain, and USA). They then explore different reopening scenarios finding that lockdowns of two months would be ideal to prevent disease resurgence and that effective social distancing as well as other NPIs adopted by a larger fraction of the population could avoid the need for other lockdowns. Authors in Ref. [65] focus on data from Canada, Germany and Italy and used a neural network approach to fit an extended SEIR model that accounts for asymptomatic, symptomatic, hospitalized, and deceased individuals to real epidemic data. Their results suggest that reopening strategies should be gradual and stage-wise to avoid quick disease resurgence.
Two theoretical approaches consider explicitly the presence of the virus in the compartmental structure [91], [92]. In particular, authors of Ref. [91] split a population in two: those wearing masks and those that do not. Then they consider that asymptomatic and symptomatic individuals create the inoculum in form of droplets. These are described by a compartment and move with a certain rate into the fomite compartment capturing the virus presence in contaminated surfaces. Finally, fomites decay. Interestingly, the transmission rates are driven by the interactions of susceptible with the and compartments. This allows to model more explicitly the role of face masks which offer some protection from droplets but not from fomites. Ref. [68] focuses on the possible impact of the seasonal flu in the management of the COVID-19 pandemic. In fact, flu symptoms might be confused with those of COVID-19. As result resources, key for the fight against the current pandemic, such as tests, might be diverted towards the flu. The authors propose to capture this possible negative interaction by extending the classic SEIR model to account for asymptomatic, symptomatic, as well as susceptible, exposed, and infected quarantined. Furthermore, they consider the possibility of having individuals with the flu in the pool of people to quarantine and subject to COVID-19 tests. They consider a transmission rate explicitly function of contacts that due to NPIs go from to a exponentially as function of time. Their results show how an uptake of the flu vaccine could help the depletion of resources necessary to contain COVID-19.
Several articles adopted SEIR-like models with age-structures to study the impact of different NPIs in countries [23], [93], [96], [97], [98], [101], reopening scenarios [95], [103], investigate herd immunity [94], [104], and consider particular contexts such as African countries [99], [100].
Two articles modeled the impact of the NPIs in the first wave in France and studied different reopening scenarios [96], [97]. In particular, Ref. [97] considers an extended SEIR model with contact matrices and age structure fitting the transmission rate before and during the lockdown from data. They studied different contact matrices during the lockdown (not estimating them from data). The baseline for the lockdown considers no contacts in school, a reduction of 80% of work contacts, and 90% in other locations. The results suggest that about 3% of infected individuals was hospitalized (by May 11), and an average 0.5% died across the board. The IFR for individual was found to be 8.3% while 0.001% for those or younger. Furthermore, the results indicated that was reduced from 2.9 to 0.67 and 5.3% of the population is considered to be infected by mid May. Ref. [96] considers a similar model (though with a broader range of compartments to account for asymptomatic, pauci-symptomatic, mild, and severe infectious) for the Il̂e de France, region where the capital is located. They consider a range of NPIs such as remote working, school closure, case isolation, banning of social events, and senior isolation that study them as single or as portfolio of interventions. Each NPIs affects the contact matrices. The lockdown is for example modeled considering a complete removal of contacts in school, remote working at 70%, 90% of senior isolation, closure of all non essential activities but no case isolation. Fitting the model via a maximum likelihood approach to hospital admission data, the authors estimate an that was effectively reduced to 0.68 by the lockdown. Furthermore, estimates for the IFR are in between 0.7%–1.2%. These figures are a bit higher than those mentioned above. It is important to stress how this paper focuses on one of the most afflicted region of France while the first considered the entire country thus averaging with less affected areas. A similar approach, though with a simpler compartmental structure and no fit with real data but a scenario analysis informed by observations from Wuhan, has been proposed also in Ref. [23]. The results, published at the end of March, indicate the impact of school closures and remote working on the mixing patterns, thus on the disease and the risks of lifting the restrictions too early. Authors of Ref. [93] consider instead the case of UK and study the impact of several NPIs such as school closure, social distancing, shielding, self-isolation and different portfolios of them on the burden of the disease. They use a simpler age-stratified SEIR model for each of the counties in the UK and model the variation of the contact matrices induced by NPIs. Interestingly, the results show that moderate levels of interventions (i.e., school closure, self-isolation, or shielding) even in combination would not be enough to avoid exceeding healthcare capabilities. The authors suggest that only more strict measures, such as lockdown, implemented for shorter periods in a background of general social distancing might be enough to avoid crushing the health system.
Authors of Ref. [95] model different reopening scenarios after the first lockdown in London, UK. In doing so, they extend the SEIR model to account for age-structure, contact matrices and other compartments such as asymptomatic, symptomatic and isolated infectious individuals. They study different scenarios: citywide extended lockdown, universal testing in a background of less stringent social distancing, shielding people , universal testing and face coverings, universal testing isolation of cases and their contacts and face coverings during the lockdown. The model confirms also in this context how strategies that combine a range of NPIs are the most efficient and offer alternatives to extended lockdowns.
Two articles tackle the issue of herd immunity. Ref. [94] adopts an SEIR model with age structure and contact matrices fitted to the UK to investigate the feasibility of dynamic mitigation strategies that reduce the reproductive number in such a way to avoid overflowing the healthcare system. In other words, when the infections are decreasing some measures might be lifted until certain warning levels are reached. This implies the ability to modify the contact matrices as function of the disease progression. In doing so, hypothetically, the impact of the virus can be mitigated with less stringent measures. The authors show how, even in simple modeling settings, such dynamic mitigation strategies require an unpractical balancing of several poorly defined indicators. It is important to notice how mitigation and not suppression was the initial strategy proposed by the government in mid March, before a drastic u-turn towards disease suppression induced by a tsunami of hospitalizations. Authors in Ref. [104] investigate the herd immunity threshold. This is the fraction of the population with immunity needed to avoid disease resurgence. In a homogeneously mixed population this fraction can be computed as . Assuming a in the range of 2.5 the herd immunity would be reached at 60%. The authors show that this threshold can be as low as 42% considering heterogeneity in contact matrices and infection rates across age-brackets.
Two articles studied NPIs in the context of African countries [99], [100]. Ref. [99] investigates possible explanations behind the relative lack of COVID-19 cases in sub-Saharan Africa. Using data and observations in Madagascar, which had a moderate peak in mid July, they considered three competing explanations: (i) low case detection (ii) epidemiological differences due to climate, younger population, lower population density and transportation infrastructure in rural areas (iii) effective NPIs. Interestingly, the results, obtained via an age-stratified SEIR model, suggest that the epidemiological markers of COVID-19 are consistent with those observed in other countries and that the observed pattern is compatible with a low case detection, late case importation, and effective NPIs. Authors in Ref. [100] study the evolution of COVID-19 and the effects of different types of NPIs in three African countries selected from youngest to oldest average age: Niger, Nigeria, Mauritius. In doing so, they adopt an age-stratified SEIR model modifying some of the parameters to better match the African context. In particular, they shifted case severity and IFR to younger ages. The results show how general physical distancing and self-isolation of symptomatic individuals, although important, might not be enough to contain the virus without lockdown levels. Furthermore, shielding of high risk people is key to avoid overflow of healthcare facilities.
Finally, one article investigates the possibility of waning immunity [105]. The compartmental structure follows the SEIRS archetype where recovered might loose immunity and move back to the susceptible compartment. The authors consider also the effects of NPIs by using time-varying transmission and mortality rates. Furthermore they introduce a compartment to account for individuals that protect themselves from infection by adopting and complying with NPIs. They assume that susceptible move to this compartment with a time-varying rate which is fitted and move out with another time-varying parameter. The model is applied and fitted to the data from New York state. The results confirm the efficacy of the NPIs put in place and warn about the possibility of endemic infections in case of wining immunity.
3.3. Metapopulation models
Metapopulation models consider a number of sub-populations connected by means of human mobility. In doing so, the disease dynamics inside each patch (i.e., sub-population) follow a compartmental model like those described in the previous section. However sub-populations are now coupled by mobility flows. Thus, these types of models allow to capture the geo-spatial spreading of a disease which is defined by the dynamics within and across patches. In particular, metapopulation models represent socio-technical systems as networks in which nodes describe sub-populations and links the mobility flows between them. The spreading of a virus is locally driven by the which is function of the reaction dynamics within each subpopulation. However, the global spreading is also dependent on the features of the mobility flows. This introduces another threshold typically called invasion threshold [146]. Considering explicitly the coupling between subpopulations allows to tackle broader set of questions with respect to those amenable in single populations. What are the effects of national and international travel bans? When and from where the first cases have been imported? Local lockdowns are a good alternative with respect to nation-wide measures? What is the chance of international importation of cases? What are the most affected sub-population and why? Furthermore, they allow to use importation and seeding events to estimate initially unknown epidemic parameters such as or the number of unascertained cases. These capabilities come with some costs. Access to mobility data and increase of computational complexity of the model are the two main aspects to consider. However, as we already saw data capturing historic as well as in near real time human mobility are readily available at different geographical scales and the use of compartmental models inside each subpopulation allows to scale up the models to hundreds of countries. On this point, it is important to mention how the definition of subpopulations is highly variable according to the data available or the goal of the research. They can describe neighborhoods of a city, cities, regions, countries etc.
The papers that used a metapopulation approach in the sample under investigation here cover several important angles such as the spatial heterogeneity of the pandemic due to local differences in the implementation of NPIs and/or features of population distributions [107], [116], [117], the first pandemic wave and the efficacy of the measures put in place [108], [109], [110], [111], [112], [113], [121], and reopening scenarios [106], [114], [115], [118]. Let us dive in some details.
Ref. [117] proposes a metapopulation model in which subpopulations are the neighborhoods of the ten largest metropolitan areas in the USA. The million people in these can interact within each node and/or visit a point of interest (POI) which might be a bar, hotel, gym etc. The system is modeled as a bi-partite network in which the two types of nodes are neighborhoods and POI. The authors built the model leveraging hourly data extracted from mobile phone of users in the area (via SafeGraph). The data is used to construct the mobility flows and coupling in the system. The resolution of the data allows to factor in behavioral changes induced by the spreading of the virus. The model is fitted considering real data from the area under investigation. The model includes only three free parameters: (i) transmission rates at POIs, (ii) transmission rates in the neighborhoods and (iii) the initial proportion of exposed individuals. The authors assume that disease dynamic follows a SEIR compartmental model. Interestingly, the transition from S to E in each neighborhood is modeled as follows:
| (2) |
where is the rate of infection in POI , the number of individuals from neighborhood visiting POI at time t, and the infection rate in that neighborhood at time . Note how the authors divided the infection dynamics explicitly considering events taking place in POIs and within each census area. Notably, the rate of infection in each POI is written as where the denominator is the total number of visitors in at each time and as usual is the transmission rate. The authors provide an expression for this rate considering it a function of the disease (which is one of the parameter fitted), and the contacts within each POIs. The latter is modeled accounting for the physical area and the average time people spend there. The rate of infection in each neighborhood is modeled similarly via the force of infection. The results indicate that a small set of POIs are responsible for the large majority of infections. Full served restaurants and hotels are on the top of the list. Furthermore, the model suggests that reducing the time spent in POIs is more efficient that reducing the mobility across the board. The authors find also heterogeneity in terms of infection rates in disadvantaged socio-economic groups which are not able to reduce their mobility as others. In Ref. [116] authors built a metapopulation model for US counties. The mobility flows up to mid March are taken from the official statistics while those after are estimated from inter county mobility towards POIs from SafeGraph. In fact, historical data is far from representative when top-down and bottom-up behavioral changes started to take off. Interestingly, the infection dynamics are split between day and night time. The model, fitted from the epidemic data of the counties more affected, shows a large heterogeneity in terms of the reduction of the reproductive number across counties. Among several others, the different extent of NPIs implementation is an explaining factor. Ref. [107] uses detailed cases data from China to study the link between the shape of the epidemic curve and spatial features of cities. Interestingly, they found that the peakedness of the epidemic is affected by population aggregation and heterogeneity in such as way that crowded cities are affected by higher attack rates and longer epidemics. The observations can be explained by considering the hierarchical structure of social contacts which are stratified in households, neighborhoods, cities, prefectures etc. Densely populated areas have higher rates of connections across households hence, given a level of NPIs aimed to cut such contacts, more dense areas will retain more connections across subpopulations which will result in higher attack rates and longer epidemics. Authors of Ref. [108] develop a metapopulation model at the level of prefectures in China. In doing so, they use a range of datasets from Baidu to estimate mobility across subpopulations and contacts within them. The goal is to quantify the effects of NPIs in the country. Interestingly, the model suggests that without interventions the number of cases would have been 67-fold. Early detection and isolation of cases is more efficient than overall travel restrictions and social distancing. Similar results, data and models in the context of China have been obtained also in Refs. [109], [110]. Authors of Ref. [113] use the Global Epidemic and Mobility model10 to simulate the spreading of COVID-19 and quantify the impact of NPIs in Jordan. Details of the model are reported below. Ref. [111] studies the case of France, Poland and Spain dividing the countries in cells and adopting a cellular automata to model the transitions within and the movements between cells. By considering time-varying transmission and mobility rate the authors confirm the efficacy of the NPIs put in place in the countries, though they estimate a very large . Authors of Ref. [112] study the very early phases of the outbreak in Spain. They use an SEIR metapopulation model fed with a multitude of datasets capturing the mobility patterns across sub-populations. Interestingly, the authors consider mobility by planes, buses, trains, cars, and ferries. In doing so, they aimed to characterize the spreading potential and patterns of SARS-CoV-2 in the first wave. They also quantified the efficacy of different control measures. Their results point to the importance of aggressive cases detection and isolation for disease eradication.
Ref. [118] tackles the issue of reopening strategies after the first wave in Europe. In doing so, they augment the mobility data reports from Google via much higher resolution mobility flows obtained considering CDRs (call details records) from Vodafone in Spain and Italy. In particular, they develop a linear model to rescale the data from Google considering CDRs to better capture key epidemiological behaviors. Using such augmentation process across all countries in Europe they built a metapopulation model at the NUTS3 (Nomenclature of Territorial Units for Statistics) resolution. The results indicate that a coordinated relaxation strategy is more beneficial than an uncoordinated approach. Interestingly, coordinated intermittent lockdowns are found to reduce by half the periods of stricter restrictions needed in case of isolated implementations. Ref. [114] investigates the reopening scenario in Italy. In doing so, they built a metapopulation model at the level of provinces. The mobility flows are taken from official statistics and are modified according to the estimate obtained and shared in Ref. [40]. The dataset will be described in more details below. Accounting for the NPIs put in place in Italy, they consider three values of . The first two are constant across the country, the last is allowed to be region dependent. Using a hierarchical framework they fit the model to the epidemic data and then consider different reopening scenarios. The results show how an increase of 40% in the effective rate, after the lockdown, would be enough to induce a disease resurgence and that detecting and isolating around 5% of the daily exposed via aggressive testing would be enough to avoid a rebound of the disease even relaxing NPIs. Ref. [106] uses a metapopulation approach considering all counties of Ontario Canada. Mobility across subpopulation is estimated via a survey that mapped commuters in the region. They consider different transmission rates according to the health status (asymptomatic, pre-symptomatic, symptomatic) and allow a variability across subpopulations. The model is fitted to the data and used to investigate different reopening approaches after the first wave. Interestingly, the results show that local reopening are better. As cost function they use the person days of closure and number of cases. They also observe that local measures might be better in the early stages of the epidemic if testing rates are high and the threshold that triggers them is set to be low. Authors of Ref. [115] propose a theoretical framework in which the transmission within, and reduction of mobility rates across, subpopulations of a metapopulation network are obtained solving an optimal control problem where a possible goal could be to avoid overflowing the healthcare system.
A subsets of papers use a metapopulation approach accounting also for the age-stratification and contact matrices within each subpopulation. In this group we find papers that evaluate the risks of importation of cases from China in the early phases of the pandemic [22], model the first wave [119], [121], [122], [123], [147] and investigate reopening scenarios [106], [120].
Ref. [22] is an emblematic example of the types of questions a metapopulation model can answer during the very uncertain initial phases of a pandemic. The authors used the Global Epidemic and Mobility model [148], [149], [150], [151] to understand the risk of importations of cases from China, estimate key epidemiological parameters, and provide a more precise picture of the epidemic in the epicenter. The model is based on three layers. The first describes the population distribution. The world is divided into over subpopulations constructed using a Voronoi tessellation of the Earth’s surface. Subpopulations are centered around major transportation hubs (e.g., airports). They consist of cells with a resolution of arc minutes (approximately Km). The population is estimated via high resolution data [152]. The model accounts for other features of individual subpopulations, such as age specific contact patterns, health infrastructure if available [153]. The second layer describes the mobility flows across subpopulations. These are split in two: short-range (i.e., commuting patterns) and long-range (i.e., air transportation). The final layer is the epidemic layer which is a compartmental model applied to each subpopulation. The authors used an age-stratified SEIR model and adopted an Approximated Bayesian Computation to estimate the posterior distribution of given the observations of international case importation from China. In other words, the authors used the cases that were popping out around the world in the very early phase of the pandemic to define compatible with such observations. After fitting the model, the authors were also able to estimate the effects of NPIs on the pandemic. The results indicate a (CI 2.37–2.78) and suggest that the travel ban from/to Wuhan delayed the unfolding of the epidemic in China of only 3–5 days. More significant were the estimated effects internationally, though the model suggests an intense seeding that took place from Wuhan and other Chinese cities after the travel ban. The results also indicate that features of the disease and the air transportation network are such that a strong travel ban from/to China is not effective without sustained social distancing. It is important to note how a first draft of this paper was posted on medrxiv in mid of February 2020. At the moment the discussion outside China revolved around the possibility of containment, and on the risk of a global pandemic. The metapopulation approach and the real data used to fed it allowed the authors to provide a picture of the spatio-temporal diffusion and diffusion potential of the virus which at that time was still highly debated. A similar model, without long-range mobility, has been proposed to describe the first wave and the impact of NPIs in the metropolitan area of Santiago de Chile [119]. The model considers as subpopulation the municipalities of the capital of Chile and adopts data from mobile phones to estimate the mobility flows as well as their changes induced by NPIs. The model suggests that only the compound effects of subsequent measures was enough to suppress the epidemic. Furthermore, the results confirm how even in this country individuals from municipalities characterized by low Human Development Index (HDI) were not able to reduce their mobility as those living in high HDI locations. As result of these socio-economic factors poor areas registered higher cases and deaths. Authors of Ref. [122] built an age-structured metapopulation model for Sweden at the municipality level. In doing so, they adopt the radiation model to estimate the mobility between subpopulations [154] before and during the pandemic. They investigate different scenarios considering moderate to strong physical distancing. The results indicate that the scenario closer to the observation is the one with moderated physical distancing of people younger than 60, very strong distancing of those older than 60 as well as a general awareness and compliance to home isolation if symptomatic. Hence, this confirms how despite the lack of strict top-down NPIs respect to many other countries the Swedish population did change behavior. Unfortunately the health outcome was still much worse than other nordic countries which took a suppression rather than a mitigation approach. Ref. [123] proposes another age-stratified metapopulation model for Georgia state (USA). The authors consider the state divided in small cells (m m) which are the nodes of the metapopulation system. Mobility is modeled considering a density function. The reduction of normal mobility due COVID-19 is estimated using the Facebook data. While typically metapopulation models consider mobility at the aggregated level of compartment (e.g., how many exposed from node travel to node ), authors here consider individual based travels and infections. In doing so, they are able to study the role of super-spreaders events. The model, fitted to the epidemic data via Bayesian inference, indicates that 2% of cases are responsible for 20% of infections and that the reproductive number was reduced below the critical value after two weeks of the shelter in place order. Also, infected non-elderly might be about three times more infectious than elderly thus driving the super-spreading events. Authors in Ref. [121] introduce an age-stratified metapopulation model for Spain. By using an Markov chain approach the authors are able to derive analytical expressions for the reproductive number as function of different types of NPIs. Furthermore, they show how the model can be calibrated to reproduce the observed evolution of the pandemic in the country.
3.4. Statistical models
The approaches described above model the spreading of infectious diseases mechanistically. Real epidemiological data is then used to constrain the phase space of parameters. Statistical models use assumptions about the progression of the disease to write down mathematical expression linking, for example, the number of cases at time with those a time . Statistical inference approaches are then used to determine the parameters modulating such relationships. A classic example is the statistical estimation of and/or . While in compartmental models is estimated looking at the difference between observed cases/deaths and those simulated by the model, statistical approaches target directly the data estimating the parameters necessary to match the expected mathematical evolution of cases/deaths.
These approaches have been applied to the COVID-19 pandemic to gather information about the key epidemiological parameters and quantify the effects of NPIs by looking at deviations from expected and/or initial trends [24], [46], [124], [125], [126], [127], [129], [130], [131], [132], [133], [134]. Let us dive into some details.
Ref. [24] uses a discrete renewal process to estimate in countries in Europe (Austria, Belgium, Denmark, France, Germany, Italy, Norway, Spain, Sweden, Switzerland, the UK) and the effects of NPIs of its evolution. The authors assume that the number of infections in a country at time can be written as:
| (3) |
where the first term on the r.h.s. estimates the fraction of the population still available for infection (not already immune, or removed), is the reproductive number regulating the growth of infections, and is the generation distribution describing the time between being infected and infecting. Hence, the new number of infected individuals is function of how many have been infected in the past modulated by the generation distribution and the average number of infections each of these is able to produce. The authors consider six types of NPIs: school closures, self-isolation of symptomatic, banning of public events, partial or complete lockdown, social distancing, and any other government intervention. They then assume the effect of such interventions to be multiplicative and such that:
| (4) |
where indicates whether each intervention is in place, is the effect of each intervention, is a country specific error term on the last intervention put in place by each country . The parameters are fitted for all countries in a single hierarchical model. The results show that the portfolio of measures put in place was enough to suppress the epidemic. Lockdowns are found to be the most significant NPIs in terms of variations to the . Furthermore, the models suggest that across all those countries a 3%–4% of the population has been infected up to early May. The same model, extended to consider more data such as hospitalizations and ICU patients, has been proposed for Slovenia [132]. The results suggest that the country has the smallest attack rate in Europe (0.3% of infected population) and point to an IFR of 1.56%. A similar model has been also applied to the case of Brazil [125]. The estimation of the points to the fact that the measures put in place were not enough to suppress the spreading, but were able to mitigate it. The authors consider also genomic data to shed light on the start of the local epidemic. The results point to the fact that the majority of importations in the genomic sample are linked to Europe and the local spreading was in place before the implementation of travels bans. A model with the same approach has been also proposed in Ref. [134] to infer the effects of NPIs in countries in Europe as well as in other continents. Interestingly the results show how across the board reduction of gatherings to ten or less, school closure and remote working had the largest impact on the reproductive number. A model based on a renewal process has been also proposed in Ref. [124]. Authors define the reproductive number at time for country as:
| (5) |
where here the describes the mobility index linked to type of places (e.g., retail and recreation, grocery and pharmacy, public transport, workplaces, home) at time for country estimated from the Google mobility reports, and is the effects of movements and interactions in each type of place on the disease spreading. The model is applied to European countries and confirms the importance of NPIs in the mitigation and suppression efforts. Interestingly, the model suggests that most significant variations in mobility are linked to groceries and pharmacies. However, variations of mobility to all categories of place are shown to be highly correlated with disease burden (measured in terms of deaths) with a delay of one month. Authors in Refs. [46], [126], [129], [131] adopt and/or extend the approach developed in [155], [156] to estimate . This method is readily available in Python and R and is called EpiEstim. In short, the total number of infectious at time can be written as where, as above, is the discrete serial distribution. The expected number of infected can be written as . Without going to the details, the approach assumes that the number of case is extracted from a Poisson distribution providing an expression linking the probability of observing a number of cases in a time window given the . This allows to apply Bayesian inference from data having as target . Ref. [46] applies the approach to data from countries and estimates the effects of different NPIs. Interestingly they found social distancing to be the most efficient in reducing the reproductive number followed by mandatory masks. Furthermore, they confirm that a portfolio of measures is required to suppress the spreading. Similar results have been reported in Ref. [129] in the context of Hong Kong. Beside estimating the effects of NPIs the authors report also the result of three surveys which show high level of awareness and adoption of NPIs such as face mask and avoid crowded places. Finally, EpiEstim has been used also to model the impact of NPIs in several cities in China [126]. The results highlight the effectiveness of the aggressive NPIs strategy put in place and point to a very different confirmed case fatality ratio in Hubei and outside. In the epicenter of the pandemic it appears to be five times higher than outside. Authors in Ref. [128] adopt a state transfer matrix model, which similarly to compartmental models, to describe the different states of individuals that got in contact with the virus. Hence, this model could be classified as a compartmental model. However as it does not match directly any archetype I opted to add it to this category. The model is fitted to data from China, Iran, Italy and South Korea with the aim to characterize the impact of NPIs in those countries and project possible attack rates.
3.5. Agent-based models
Agent-based models push the mechanistic approach to its limit. In fact, they simulate the spreading of disease reproducing, to different extents, key aspects of the society where the disease is spreading. In particular, classic epidemiological agent-based models are based on a synthetic population that is built considering empirical socio-demographic features such as households sizes and compositions. A key aspect for the spreading of diseases are social contacts which are built accounting for socio-economic activities such as school, work places, and other types of activities. The nature of agent-based models requires a much wider range of data necessary to build the synthetic population and its interactions. The computational costs associated are also much more significative. A large body of literature has been devoted to study the effects of considering real social contact networks on the spreading of infectious diseases [143], [144]. These agent-based models do not typically account for all societal details such as households, schools and work places. As such they are not typically used to make accurate predictions but rather to develop a better understanding of how the features of real contact networks might affect the unfolding of a virus. They have been used to quantify the effects of contact tracing, isolation, vaccination campaigns among other things.
In the sample of papers under review here, we find full fledged agent-based models used to model the COVID-19 and the effects of NPIs at the levels of countries, regions, or cities [63], [66], [135], [137], [138], [157]. We also find more theoretical approaches modeling particular aspects of NPIs such as different strategies for isolation [136], [139], [140].
Authors in Ref. [157] propose an agent-based model for France with the aim to understand the efficiency of different NPIs in the reopening phases after the first wave. This is a text book example of this category of models. The first important point to mention is the complexity of the approach which is exemplified by the number of parameters: in total. The majority () are to describe the socio-demographic features of the french population, are to model the contact networks, to describe the features of the virus. were obtained either from the literature or from sensible assumptions. The two remaining, which describe the contamination risk per minute per of contact and the fraction of undiagnosed cases, have been fitted to mortality data. In the model households are assigned to a square grid. These are built considering a stratification which include age and gender to reproduce the french population. Furthermore, comorbidities (e.g., diabetes, obesity, different chronic diseases) are also taken into account. The contact network is built taking into consideration several types of interactions taking place at home, in school, work, as well as during other locations such as groceries. The construction of such synthetic population allows to model with high resolution several NPIs such as reopening of particular activities or isolation approaches. The results, which where published in July, paint quite a grim picture which unfortunately has been later confirmed: measures in place after the strict lockdown is lifted are not enough to avoid the overwhelming of the healthcare system. A similar approach has been proposed in Ref. [137]. The authors use high resolution data describing the movements and potential interactions of people in Boston. They build a multilayer synthetic population which models the socio-demographic features of Bostonians, their movements and possible interactions in different locations (i.e., households, workplaces, schools etc.). The authors use the model to investigate the impact of different reopening scenarios. The results suggest that aggressive testing and household isolation could allow to reopen economic activities while keeping the health care facilities protected from overflow of cases. Ref. [138] presents an agent-based model for the metropolitan areas of New York and Seattle. They model is informed with mobile phone data collected from about 700,000 users by Cuebiq. The authors, similar to what done for Boston, built a weighted layered network capturing interactions in the community, schools, work places, and households. Furthermore, they use foursquare data to identify POIs. The results show the impact of NPIs in the two cities, provide information about the risk of infection according to the type of locations visited and estimate the size of transmission chains. In the same line with what reported above, the results suggest that the large majority of infections (80%) are due to a small minority of individuals (27%). Despite the big role played by large social event, the authors found that work places, restaurants, and grocery stores are the main drivers of the observed patterns. Authors of Ref. [135] propose an agent-based model to study the spreading of COVID-19 in Hubei, Lombardy (Italy), and New York City. The model nicely show how the details can be adapted to the goal and data available. The authors built synthetic populations form by individuals stratified for age, comorbidities and assigned to a household. Contacts are divided in two category: inside and outside households. Contacts in different contexts than home are modeled via contact matrices. The free parameters are fitted to data using a Bayesian framework. The results show how the efficacy of NPIs aimed at limiting contacts across age brackets vary according to the location under study. This suggests how a one fit all strategy might not be optimal and measures should be tailored to the specific socio-demographic features of each populations. Authors in Ref. [66] use a network-based model where a representative sample of different cities interacts via a contact network. The authors model interactions within and across cities. These are modeled as clustered networks. Links inside each community are extracted from a configuration model. Links across communities assume an homogenous random graph. Connections between cities are built considering real data from Baidu. Since the units of the model are individuals, the number of travelers from city and are assigned randomly to nodes in . These form a number of connections, which is the average in the system, with random nodes in . The population is scaled down to reduce the computational costs. This model does not consider explicitly the stratification of individuals in households, school or work locations. The results obtained confirm the importance of NPIs in controlling the pandemic in China. Authors in Ref. [140] propose an agent-based framework where beside individuals, agents describe houses, business, government, and the health care system. Each type of agent is assigned with a set of features and enabled to take a set of actions. The framework allows for the implementation of a range of NPIs and measure the impact in terms of disease and economic burden.
4. Surveys
The seismic impact of COVID-19 on our society has dramatically boosted the study of non-pharmaceutical interventions via explicit observations: surveys. This methodology allows to gather ground truth data by asking specific questions to a sample of the population rather than inferring answers from proxy data. Hence, they are a powerful tool to understand and measure causal links. In the era of big-data surveys might look old fashion and surpassed. However they are still an invaluable approach to characterize complex processes. The sample size is typically an issue castings doubts about the external validity of the findings. However, modern technology and having a larger part of the population stuck at home in front of a screen due to lockdowns offered the opportunity to reach large numbers of participants quite easily.
Before diving into the observations and results of this large body of research, let me spend few words to characterize the subset. First of all, it is interesting to notice how the surveys have been answered by participants in countries. While in the large majority of cases the survey targeted a specific country, four surveys were done in two countries, two in five, one was extended to participants in countries. Second, the most represented country is USA, followed by Italy and China. This top three is not surprising. China was the epicenter of the pandemic. Italy was the first country in Europe to be affected by the virus. USA is a powerhouse of scientific production and one of the most affected countries in the pandemic. In Fig. 3 I report a histogram considering, to improve the readability, just countries featured in more than one single study. All continents, except Antarctica, are represented. Third, countries are found in the affiliations of this group of papers. USA, Italy, China and the UK are at the top of the list. Fourth, the research has been published in different journals (including preprint in the medRxiv not yet published elsewhere). The most represented journals are International Journal of Environmental Research and Public Health, Frontiers in Psychology, Frontiers in Public Health, PLoS ONE and the Journal of Medical Internet Research (see Fig. 3). It is interesting to stress the diversity of the set of publication venues that ranges from Nature Human Behavior and Science to Journal of Medical Internet Research and Seizure. This, still limited sample, highlights the breadth of research on the subject. Finally, these papers have been written by more than authors and, as of December 19th they received citations. See Fig. 3 for more details.
Fig. 3.
Total number of articles, sub-categories, authors, and citations of the papers in this category on the left. Note that these numbers are estimated from Semantic Scholar. On the right (main panel) histogram describing the number of countries subject of study in this category. On the right (in-set) most represented publication venues of the category. To improve visibility I am showing only countries featured at least in two studied and journals featuring at least two articles.
4.1. Classification
After inspecting all the articles and considering their focus, I have assigned each survey to one of five categories. In particular:
-
1.
Health and wellbeing indicators: surveys aimed at monitoring, measuring or access the impact of NPIs on health and wellbeing;
-
2.
Adoption and awareness of NPI: surveys aimed characterizing the adoption of NPIs identifying the key factors influencing changes in behaviors;
-
3.
Changes in medical practice: describes studies focused on accessing the impact of NPIs on patients and health care;
-
4.
Effects of NPI: surveys set out to understand the impact of NPIs on a range of human activities;
-
5.
Contacts: surveys aimed at quantifying the effects of NPIs on human contacts.
It is important to mention that similar topics will be found also in other types of study described in other sections. However, those do not rely on primary data collection methods but on data proxies. In other words, they use data that have been collected for other uses as proxy for behavioral markers.
In Table 3 I report the full list of references organized according the taxonomy I have created. Furthermore, I have grouped the research considering the sample size and the country or countries from where the participants where recruited. Now, we are ready to dive into each subcategory.
Table 3.
Summary of the surveys in the sample of papers. The first column describes the main topic of each survey, the second the subcategory, if any. The third the sample size. Note that for simplicity I have group them in brackets. The last column describes the country or countries focus of the survey and/or the location of the participants.
| Category | Subcategory | Sample size | Country and Reference |
|---|---|---|---|
| Health and wellbeing indicators | Mental Health and wellbeing |
|
Italy [158], 59 countries [159] |
|
|
Bangladesh [160], China [161], [162], USA [163], [164], [165], Serbia [166] |
||
|
|
Canada [167], China [168], Ghana [169], Jordan [170], Italy [171], Russia and Belarus [26], USA [172], [173], [174] |
||
|
|
USA [175] |
||
|
|
Netherlands [176] |
||
| Health Behaviors |
|
China [177], Spain [178], UK [179], USA [180], [181], [182] |
|
|
|
Australia [183], USA [184] |
||
|
|
Spain [185], [186], USA [187] |
||
| Effects on patients |
|
Germany [188] |
|
|
|
Germany [189], Japan [190], Italy [191], [192] |
||
| Brazil [193], USA [194] | |||
| Adoption and awareness of NPI | NA |
|
Australia, Austria, France, Germany, Italy, New Zealand, UK, USA [195], [196], Japan [197] |
|
|
China [198], [199],Germany [200], Jordan [201] India [202], [203], Saudi Arabia [204], Slovenia [205], New Zealand [206], Taiwan [207]; UK [179], USA [208], [209], [210], [211] |
||
|
|
Serbia [212], Pakistan [213] |
||
| India [214],Pakistan [215], Saudi Arabia [216], South Korea [217], USA [218] |
|||
| Changes in medical practice | Mental Health |
|
Austria [219] |
|
|
Italy [220], 29 countries [221] |
||
|
|
Austria and Germany [222] India [223], USA [224] |
||
|
|
Australia, Canada, Netherlands, UK, USA [225], Germany [226], Italy [227], [228] |
||
| Oncology |
|
Italy [229] |
|
|
|
Austria, Belgium, France, Germany, Italy, Luxembourg, Netherlands, Spain, Switzerland, USA [230] |
||
| Other care |
|
USA [231] |
|
|
|
China [232], Italy and Saudi Arabia [233] |
||
| UAE [234], USA [235] | |||
| Effect of NPIs | Leisure |
|
USA [236], Sweden [237], 12 countries [238], 24 countries [239] |
|
|
Sweden [240] |
||
|
|
South Korea [241], Sweden [242], USA [243] |
||
| Education |
|
China [244], Jordan [245], 32 countries [246] |
|
| Mobility |
|
Germany [247], Denmark, Netherlands, Italy, Spain, UK [248] |
|
| Consumption |
|
China [249] |
|
| Romania [250], Tunisia [251] | |||
| Contacts | NA |
|
China [252], UK [27] |
| China [25] | |||
4.2. Health and wellbeing indicators
This body of research aims to characterize the effects of NPIs on (i) mental health, (ii) health behaviors, and (iii) patients. These constitute three subcategories. Let us discuss them in order.
It interesting to notice the variety of angles and aspects covered in the surveys on mental health. In fact, they consider loneliness [164], [172], [174], domestic abuse [170], psychological mindset [26], [158], [159], [160], [163], [165], [166], [168], [169], as well as particular groups of the population studying the toll on frontline workers [161], students [173], [175], parents and children [162], [167], [171], [176]. Several common themes as well as some conflicting results emerged from this research. When it comes to loneliness age, gender, and perceived concerns about the pandemic appear to be important factors. In particular, younger individuals, especially female, reported a larger increase in loneliness respect to adults [174]. However, a direct comparison between participants in the 60–70 and age brackets show that the older group felt more lonely [172]. Hence, loneliness appears not to be a monotone function of age. Very young and older age classes are more affected by it. Furthermore, loneliness increases more for those reporting greater concerns about the pandemic. However, it is important to notice that while two surveys found an increase of loneliness during the first wave [172], [174], another reported no significant variations from January to April [164]. One survey focused on the effect of NPIs on domestic abuse [170]. The study considers a sample of women living in Jordan contacted via WhatsApp. Tragically 40% reported same level of domestic abuse during the health emergency. Being unemployed and married were the most important features linked to abuse. In terms of psychological mindset of participants living under some type of NPIs country of residence, age, gender relationship status, living arrangements, income, and education are important factors [26], [158], [159], [160], [163], [166], [168], [169]. In fact, a study conducted by recruiting participants in countries reports that socio-demographic features, having had symptoms, mobility restrictions, and having had issues transitioning to remote work or an increase of conflict at home explain around 20% of the variance in depression and anxiety [159]. Another survey estimates panic in 79% of participants and found being older than , educated, married, and living with a joint family to be predictors of it [160]. In contrast, a survey conducted in Serbia found that worry, fear, boredom, anger, and annoyance decreased in time during the first wave [166]. Adherence to NPIs and exposure to media were linked to positive effects on worry and fear. Similarly, a survey aimed at capturing the effect of NPIs on five factor personality traits found that during the crisis neuroticism went down [163]. The authors speculate that this trend is due to the progression of the pandemic rather than to peoples’ personality.
The second subcategory describes surveys aimed at capturing the impact of NPIs on a range of health behaviors such as sleep, physical activity, sex, and substance use. Two studies on children noted how COVID-19 restrictions led to less physical activity and sleep disturbances but to more screen and sleeping time [177], [185]. The findings hint to a complex picture with some positive and negative effects of home confinement. Physical activity and changes in sleeping patterns have been reported also in the adult population [178], [179], [180], [181], [186]. A sample of more than participants in the UK provides some hints about the magnitude of physical activity variation before and during the lockdown [179]. While 64% reported to have kept similar levels of activity, 25% did less and 11% increased. Overall, the surveys on the subject highlight high BMI, depression, health conditions, gender (being female), and high risk perception as features connected to larger decrease of physical activity [179], [180]. Being an essential worker negatively impacted lifestyle [186]. Social distancing and stay home orders affected also other health behaviors such as sex and substance use. Two surveys done in Australia and USA show how NPIs have led to drastic reduction of sex with occasional partners and an increase of porn consumption [183], [187]. Alcohol consumption, above the drinking limits, has reported to increase during NPIs [184]. Similarly, medicinal use of cannabis has increased among individuals with mental health conditions and 16% affirmed to have changed to route of administration shifting away from smoking [182].
The tsunami of COVID-19 cases that flooded health care facilities had a drastic impact also on patients affected by other conditions. Several surveys aimed at providing a better understanding of this unfortunate phenomenon. They considered patients affected by diabetes, cancer, ALS, hypertension, mental or substance abuse disorders [188], [189], [190], [191], [192], [193], [194]. Admittedly, the research focused on short term effects and on the shift towards telemedicine (i.e., remote care). A study conducted in Italy on diabetic patients revealed their good resilience and adaptation to technology [191]. However, a similar research done in Japan hints to a negative impact of reduced physical activity on glycemic control [190]. A cohort of patients affected by cancer in Germany showed levels of stress and anxiety similar to a control [189]. Drastic reduction of physical activity, with potentially detrimental effects, has been reported for adults with hypertension [193].
4.3. Adoption of NPIs
Several interesting themes emerge from the surveys aimed at understanding the factors driving the adoption of NPIs. First of all, across several countries and in different studies gender appears to be a key factor. In fact, female respondents are found more likely to perceive COVID-19 as a risk, agree and comply with NPIs [195], [197], [200], [212], [218]. Similar trends are observed for individuals with high level of education [200], [215]. Age again does not appear to be a monotonic function: very young and old individuals share similar trends. In fact, young adults have reported a smaller decrease in mobility and old individuals less compliance to NPIs (especially if male) [212], [218]. It is important to mention that age was not a relevant factor in a survey conducted in Germany [200]. The research points also to a big urban–rural division and thus to the importance of socio-economic factors when it comes to compliance. In fact, several barriers to NPIs have been reported in peri-urban and rural areas in India [202], [203], [214]. Individuals living in urban settings report a better knowledge about COVID-19 and better opportunities to adopt hygienic behaviors. The country of residence also seems to play a role when it comes to the trust level towards media during the emergency which might influence adoption. A cohort in Jordan reported a positive influence, especially on the awareness levels [201]. However, a survey in Slovenia, done with of the first confirmed case, points to low level of trust of the media and shows that perceived credibility of information linked to lower levels of negative emotional response and higher adherence to NPIs [205]. A survey conducted in South Korea compared the adoption of NPIs during COVID-19 with results obtained during the spread of MERS-CoV [217]. Interestingly social distancing and practicing other transmission reducing behaviors increased significantly during the COVID-19 pandemic. The subset of participants with a higher perception of risk was found to be more likely to adopt NPIs in both. Interestingly, several surveys confirm the expectation coming from the health belief model pointing to the fact that knowledge about the disease and perceived risks are predictors behavioral changes [198], [204], [206], [208], [214], [215], [216]. The adoption of face masks has been found to be negatively affected by perception of shortage in New Zealand [206], and positively influenced by national guidelines in the USA [211]. Ref. [196] analyzes the dataset collected from half millions of users that installed the platform for digital surveillance called How We Feel. The app collects a range of demographic, symptoms, and behavioral data such as use of masks and social distancing practices. Though the aim of the paper is to investigate whether the data collected can be used to estimate risk factors and exposure to the virus, it provides interesting insights about the behavior of the sample in terms of NPIs. The majority (61%) of users reported to have left home despite the stay at home orders. Only 19% of these attributed to work the reason to leave home. Of this subset of people that left home the majority reported to practice social distancing and wearing face masks. Though still a significant fraction did not. A minority of users reported that, despite testing positive, they went to work sometime without wearing a mask. Healthcare and essential workers were more likely to go to work after testing positive. Though, people who tested positive, reported a clear reduction of contacts with respect to those that were untested or tested positive.
4.4. Changes on medical practice
How did medical practice change to cope with NPIs and COVID-19? A very interesting subset of surveys provides some answers from both patients and doctors. I have identified three subcategories which refer to mental health, oncology and other medical specialties.
A survey among psychotherapists in Austria revels that the decrease of face-to-face appointments was not necessarily linked to an increase of remote sessions [219]. Similarly, another in Italy reports the needs for more health care support [220]. Even more concerning are the results of a survey that pooled participants in countries [221]. These are the caregivers of individuals with intellectual and developmental disabilities. The majority, 74%, reported that they lost access to at least one therapy. The majority nevertheless, 56%, was able to keep services though 36% reported to have lost healthcare provider. Across several surveys, telemedicine has been found to be useful [221], [223], [227]. Though, socio-economic disparities, linguistic disadvantage, and health issues have been reported as challenges of remote care. It is also interesting to notice the perception of telemedicine among practitioners [222], [224]. Rapid transitions towards it, reduce revenue and modification of communication linked to it have been reported as challenges [224]. Furthermore, the judgment of the transition appears to be function of the number of patients supported [222].
In the second subcategory we have two surveys dealing with changes in oncology care. The first used WhatsApp to explore the topic covered in discussions between patients and doctors. The most common themes that emerged cover delays with care, queries about immunosuppression, and variation of lifestyle or activities [229]. The second survey was conducted in oncological care institutions in countries. Remote triage before visits was implemented by 90% of centers. Adoption of PPE was used across the board and only few clinical instrumental examination were performed. Telemedicine was adopted by 76% and separated pathways for COVID-19 positive and negative patients were put in place. Return to work policies required a negative test in 76% of centers.
In the third and final subcategory we find surveys targeting both patients and practitioners in a variety of specializations. From remote management of geriatric patients with heart conditions [232] and the effects of NPIs on transplant recipients/donors [233] to the changes adopted by several hospitals in academic centers [235], hearing and emergency care [231], [234]. Overall the observations on patients point to the interim efficacy of telemedicine and to high level of awareness about the risk of infection. The findings on medical practices highlight the drastic changes and adaption put in place to cope with the pandemic. Marked reduction of in person visits, stockpile of PPE and use of respiratory isolation units have been reported. Remarkably, in one study 46% of practitioners reported examples of non-COVID-19 diagnoses in patients admitted for COVID-19 evaluation and vice versa highlighting the challenges induced by the virus to the health care system [235].
4.5. Effect of NPIs
This group of surveys captures the impact of NPIs of a range of human activities such as (i) leisure, (ii) education, (iii) mobility, and (iv) consumption.
Due to social distancing, travel limitation, and stay home orders the possibility for leisure has been dramatically reduced. A survey done in a cohort of around participants in countries investigates the impact on bird watchers [239]. A large majority, 85%, changed behavior reducing traveling and targeting local spots. They reported also a significant change in social interactions. The increase of time spent inside has induced variations in the locations selected when going outside [238]. Walking paths have been changed to include urban gardens, tree lined streets and traveling by car in green areas. In others words, the confinement has boosted the interest and value of nature. The stop of many sport events and leagues has impacted also gambling [240]. While sport gambling has dropped, the attention has been shifted towards other forms. The gambling habits of the majority of respondents to another survey reported did not report a change in gambling habit [237]. However, the minority that did was affected by gambling problems and reported an increase in alcohol consumption. The toll of NPIs on sport activities has been quite significant for elite athletes [242], [243]. Level of stress and anxiety have been observed, especially among women, and linked to worries about the future of the sport. A survey conducted in South Korea links the tendencies towards keeping practicing sport with the perception of risk and worry about getting infected [241]. Age and the type of sport were found to play a modulating role.
Educational activities have been also altered. Like in many other sectors the need for physical distancing required drastic shifts in the delivery of classes as well as on research production. A survey conducted in China extended to parents, students and teachers point to the fact that while online teaching was positively valued, parents and teachers were found to be more concerned about the possible side effects [244]. A survey delivered in a cohort of students in Jordan aimed to understand the impact of remote learning and in particular on online exams [245]. A sizable fraction of students (32%) reported more stress linked to this exam mode. Navigation of questions and technical issues were reported to be main drivers of stress. Furthermore, online exams appeared to affect negatively eating habits, sleep, physical activity and led to increase in smoking. A study conducted on principal investigators in USA and Europe, point how NPIs, despite the reduction of activities outside home, have reduced the time spent doing research especially for female scientists, those in experimental fields and with young children [246].
As we will see in more details later, one of the most explored aspect of non-pharmaceutical interventions is mobility. Beside the interest in the way population adapted movements/travels, characterizing variations in mobility is key to model the spreading of the virus. As result, we will speak about NPIs and mobility in several sections. Though the aim will be the same, what changes is the methodology used to characterize changes in mobility. Here, we report two studies done with cohort of individuals in Germany [247] and more than people in five European countries [248]. In both cases, smartphone apps were used to collected information about mobility (distance traveled, steps count) as well as other indicators (heart rate, sleep duration, bedtime, social app use). The results point to a drastic reduction of distance traveled (more than half in the lockdown period) [247]. The reduction did not cease immediately after the end of lockdown. Age and gender groups behaved similarly, reporting a consistent relative variation respect to pre lockdown period. Reduction of steps and increase homestay have been reported also outside Germany [248]. Furthermore, use of phone and social media apps have increased. Consistently with what mentioned above, sleeping patterns have been altered. More sleep and later bed time have been reported [248].
4.6. Contacts
NPIs are designed to reduce transmission chains. Hence, several targeted directly or indirectly social contacts. Different surveys have been designed and deployed to capture the effect of NPIs on contacts and thus estimating the impact on the disease spreading. A survey conducted in Wuhan and Shanghai during the outbreak revealed a reduction of factor 7–8 of social contacts [25]. Using this data together with information about contact tracing the authors estimated, via an epidemic model, this reduction was enough to contain the spreading. Another survey conducted, considering also data after the end of the lockdown in China, shows that the relaxation of NPIs brought an 5%–17% increase in social contacts which are anyway 3–7 times lower than pre-pandemic values and still below the levels associated to disease resurgence. A similar study conducted during the lockdown in the UK report consistent, though smaller, reduction contacts (a factor 4) [27]. Nevertheless the change was enough to push the below the critical threshold of one.
5. Comments and/or perspectives
A significative fraction of the sample can be classified as comments and/or perspectives. Here researchers reflect on future challenges, point out opportunities, summarize findings and approaches developed in the fight against COVID-19. In doing so, they do not necessarily present new analysis or findings. Rather, the goal is to highlight key aspects, draw the attention to specific points, critically discuss evidence, questions assumptions as experts in the field.
Before summarizing this body of work, let me spend few words to provide a general description of it. While the large majority of articles provide a general outlook to a specific topic, some draw from a specific context. In fact, we find comments focused from observations in USA [253], [254], [255], [256], [257], [258], in Italy [259], [260], [261], in Canada [262], [263] and the UK [264], [265]. We have then articles that focus on Africa [266], China [267], Ethiopia [268] , France [260], Poland [269], Taiwan [270], Vietnam [271], South Korea [272] and Singapore [273]. Comments and perspectives have been written by researchers with affiliations in countries (see Fig. 4). The most represented countries are USA, UK, and Italy. Finally, this research has been published in journals (including one preprint in medrxiv). Really a wide range of publication avenues ranging from journals focusing on pediatric psychology to interdisciplinary journals such as Science Advances. The most representative journals, each with two comments/perspectives, are BMC Medicine, Journal of Addiction Medicine, Journal of Travel Medicine and Science. These papers have been written by more than authors and received more than citations. A median of citations per article.
Fig. 4.
Total number of authors and citations of the papers in this category on the left. Note that these numbers are estimated from Semantic Scholar. On the right histogram describing the number of countries considering authors’ affiliations.
5.1. Classification
Considering their topics, comments and/or perspectives can be classified in five categories (see Table 4):
Table 4.
Summary of the comments and/or perspective in the sample. The first column describes the category of each article in this group. The second, the topics and references.
| Category | Topic and references |
|---|---|
| Change to medical practice | Mental health care [254], [257], [261], [273], [274], [275]; Emergency care [276], [277]; Substance abuse [253], [263], [278], [279], [280]; Oncological care [264], [281] Health care practices [255], [259], [262], [282], [283], [284]; Pediatric care [283], [285] Other care [256], [260], [268], [286], [287], [288] |
| Modeling | Modeling approaches [28], [265], [289], [290], [291], [292], [293]; Transmission dynamics [294], [295], [296], [297], [298] Mobile phone data [29]; estimation [258] |
| Effect of NPIs | Effects on: children [30], [299]; education [269], [300]; gambling [301] other diseases [267]; the environment [302], [303]; food consumption [304]; corporate world [305]; porn consumption [306] |
| Lifting NPIs | African context [266]; Vietnamese context [271]; Preventing second wave [307] Effects on children back to school [308] |
| Success story | South Korea [272], Taiwan [270] |
-
1.
Change to medical practice: describe articles that analyze challenges and changes to medical procedures made necessary by NPIs;
-
2.
Modeling: refers to comments and/or perspectives discussing different aspects, challenges, approaches, and opportunities to model the unfolding of COVID-19;
-
3.
Effect of NPIs: captures articles reflecting on the changes induced by NPIs on a range of activities;
-
4.
Lifting NPIs: describes the set of articles about different strategies and challenges to tackle when relaxing NPIs;
-
5.
Success stories: describes comments and/or perspectives about lessons learnt in countries that manage to successfully suppress COVID-19;
5.2. Change to medical practice
This is the largest group of comments and/or perspectives. We find articles focused on a range of medical specialties: mental health care [254], [257], [261], [273], [274], [275], emergency care [276], [277], substance abuse [253], [263], [278], [279], [280], oncological care [264], [281], health care practices [255], [259], [262], [282], [283], [284], pediatric care [283], [285], and other care [256], [260], [268], [286], [287], [288].
Ref. [257] draws on the experience developed when counseling patients suffering from anxiety disorders in one of the worst hit region in the USA during the first wave: New York City. The observations highlight how the changes in behaviors induced by NPIs shifted the sense of familiarity, predictability or daily activities towards the unknown and drastically limited social support. The variation of ordinary routine is linked to increase distress. Social support, which is one of the key pillars of well-being, has been also challenged by the closure of activities, and social distancing. The article calls for establishing new routines and to make efforts to keep high level of social engagements. Authors in Ref. [275] reflect on the challenges linked to mental health care delivery in the context of social distancing. While the needs to move a portion of the services remotely are clear, the authors call for a diversification of the offer that includes in-person visits for patients that might lack the technology required for tele-health, digital interventions, community outreach, family support and national warm lines. Authors in Ref. [277] tackle the practical issues of social distancing in the challenging context of emergency departments. A wide range of standard procedures and workflows have been drastically changed to limit the changes of transmission between patients and health workers. Authors in Ref. [278] highlight the opportunities of digital phenotyping via smartphones to reduce the limitations induced by NPIs during the pandemic in substance abuse care. The authors point to the use of such technology, which can be used at scale, for early detection of possible issues thus targeting the limited resources and reducing risks. In the context of oncologic care (in particular pancreatic cancer) Ref. [264] presents a discussion of the variations put in place by UK clinicians. The article, recommends for prioritization of specific treatments, strategies to postpone surgical procedures, and for approaches that limit hospital visits. Ref. [259] proposes a set of measures in hospitals to reduce the risks of infection in patients and health workers. Authors call for aggressive and periodic testing of practitioners, use of appropriate PPE and air filtering systems, suspensions of surgical training and experimental treatments among other things. Authors in Ref. [283] discuss the changes to care in pediatric settings. They acknowledge the key role of telemedicine, discuss the opportunities, barriers, and call for future research aimed at characterizing the possible short and long term effects of this change in care. Finally, Ref. [268] describes the effects of NPIs on veteran care in the USA. Thanks to the efforts already in place, the transition to telemedicine in this context has been reported to be quick and efficient. Nevertheless, also in this case, the authors call for future studies aimed at measuring the short and long term effects of such variation in care especially in mental health.
5.3. Modeling
Several comments and/or perspectives focus on different aspects of modeling COVID-19 dynamics and NPIs. In particular, we find articles discussing epidemic modeling efforts [28], [265], [289], [290], [291], [292], [293], analyzing knowns and unknowns of transmission dynamics [294], [295], [296], [297], [298], presenting opportunities to model and control the spreading of COVID-19 enabled by novel data streams such as mobile phone data [29], and discussing the challenges in estimation [258].
Ref. [291] discusses the main challenges in developing epidemic models for COVID-19. From highlighting the differences between “peace” and “war” modeling due to lack of data and a fluid landscape of knowledge about the virus under study in the middle of a pandemic, to the importance and challenges of considering super-spreading events. Authors in Ref. [292] reflect on the key role played by predictive modeling in the emergency stressing the wide range of methodologies that have been put in place as well as the key challenges ahead to develop standard metrics to measure their performance. Authors in Ref. [294] provide an overview of the engines responsible for the spreading of SARS-CoV-2. Contacts in households, presence of asymptomatic and pre-symptomatic transmission as well as super-spreading events are considered as key factors. The importance of understanding and capturing super-spreading events to accurately model and suppress COVID-19 is also matter of discussion in Ref. [296]. Ref. [29] discusses the opportunities and challenges offered by mobile phone data to inform, guide, and help designing NPIs policies during the different phases of a pandemic. In the early phases, mobile phone data can be fundamental to help standard surveillance efforts aimed at fast detection of cases and possible exposed contacts. During the exponential growth phase, when the shields of NPIs are lifted as response, mobile phone data can be crucial to monitor mobility reduction at the population level thus quantifying the effectiveness of the measures as well as to inform realistic epidemic models (as we saw in previous sections). After the peak, this type of data can be crucial to help contact tracing, identify with the help of epidemic models risks of hotspots of local disease resurgence. While these opportunities are real and they come with serious challenges. In fact, the authors note how the lack of a widespread use of this data as a go-to tool to face epidemic spreading is linked to several problems. Lack of a “digital mindset” of key institutions, reluctance of corporations collecting the data to share it, privacy concerns, the “academic mindset” which often does not allow to formulate solutions in relevant actionable terms, remain challenges for to tackle in the future. Finally, as we saw in the section about statistical epidemic model, the estimation of is a classic approach to characterize the unfolding of infectious diseases. The authors of Ref. [258] discuss several methods and, by using synthetic data, present possible practical challenges that might bias the results. Interestingly, they suggest the adoption of EpiEstim (which we discussed above) and recommend against other methods which either use data after the time (so can be used only retrospectively) or are prone to biased estimates if the underlying assumptions do not hold.
5.4. Effect of NPIs
This category captures comments and/or perspectives discussing the effects of non-pharmaceutical interventions on specific groups such as children [30], [299], on education [269], [300] or other activities such as gambling [301] and food [304], on other diseases [267], the environment [302], [303], the corporate world [305] and porn consumption [306].
Ref. [299] discusses the issues children face while confined at home during lockdowns. The authors suggest parenting strategies that structure the day in a set of activities with assigned roles and adopt technology to keep them socially connected. Authors in Ref. [30] highlight the behavioral and emotional disorders in children as result of the pandemic. Ref. [269] addresses the effectiveness of e-learning for medical students. The observations from a cohort of students in Poland showcase the effectiveness of the technology that allows to meet several learning outcomes but point out the limitations to reach others linked to practical skill development which is key for doctors. Authors of Ref. [304] reflect on the effects of NPIs, in particular those that increase the time spent at home and limit physical activities, on food consumption. The authors introduce the concept of covibesity to highlight the possible negative consequences of home confinement: increase of take away orders, food and alcohol consumption. They also reflect on the marketing shifts of the food industry which has leveraged the increased time spent online boosting online advertising in particular for children. Authors in Ref. [267] discuss how the strict NPIs put in place in China have also reduced the burden of influenza. In fact, social distancing and increase hygiene are key factors which might interrupt transmission chains of a range of viruses beside COVID-19. Ref. [302] highlights one of the silverlining of NPIs put in place to curb the spreading of COVID-19: global reduction of mobility and thus a much smaller fingerprint on the environment. The authors point to the fact that positive change to the environment is proven to be possible and hope for behavioral changes in this direction even after the end of the pandemic. Ref. [305] discusses the reaction of leadership in the corporate world to systemic crises such as COVID-19. The results from interviews and observations highlight how in crisis times leaders tend to be guided by compassion and how the scale of the crisis might help leaders to question what really matters which might help them to better capture the ethos of the company. Finally Ref. [306] reflects on the increase in porn consumption due to NPIs, the possible negative effects associated with it and call for future studies investigating this phenomenon.
5.5. Lifting NPIs
Four articles provide a perspective about the relaxation of NPIs in different countries and contexts [266], [271], reflecting on the risks of a second wave [307], and on the challenges children going back to school after a long period of isolation face [308].
Ref. [266] details the challenges faced by African countries when relaxing NPIs. In fact, the limited resources and the specific contexts of each country in the continent might impede adequate testing, contact tracing, and adoption of NPIs to avoid a rebound of infections. The authors warn about the grim consequences of other COVID-19 waves and call for efforts similar to those in place to flight HIV, TB, and malaria. Authors in Ref. [307] discuss the differences between mitigation and suppression which we have presented above. They argue that suppression approaches based on lockdowns are to be preferred to mitigation strategies and how they might provide the time necessary to build up the testing and contact tracing infrastructure to avoid disease resurgence. The article published in July warned about the lack of such infrastructure despite the relaxation of measures in most countries and how this might lead to a second wave. The warning unfortunately manifested to be a well poised concern.
5.6. Success stories
While most of the countries in the world have not met the challenges posed by COVID-19 and saw multiple significant waves of infection as well as lockdowns, few managed to suppress the virus effectively. South Korea and Taiwan are examples. Their experience and lessons learnt have been focussed in two perspectives [270], [272]. In both cases the strategy revolved on early actions, rapid development of testing capabilities, aggressive contact tracing, social distancing and high adoption of face masks.
6. Quantifying the effects on NPIs
Non-pharmaceutical interventions are not a monolith. By now it should be clear how they refer to a wide range of measures. A first binary classification can be used to split them according to whether they emerge bottom-up as voluntary reactions of the population or whether they are pushed top-down by authorities. In the first class, we find spontaneous use of face covering, increased hygiene, changes of diet, avoidance of transportation, social gatherings and more in general social distancing. In the second we find border closures, travel constraints, school closures, curfews, lockdowns, stay at home orders, the mandate use of face covering among others. While we were quite familiar with the first type, for example during a particularly aggressive seasonal flu, the second, often draconian, measures came as a surprise for many since they are real social and economical nuclear options. It is important to mention how in reality the difference between the two is not a clear cut and, in a complex landscape as the COVID-19 emergency, they might be concurrent. Furthermore, the spatio-temporal unfolding of the virus, the sequence of events, economic and social pressure, political ideologies, and past experiences with similar health emergencies induced high level of heterogeneities in the response, visible not only across but within countries. As mentioned above, while Italy was shutting down in an unprecedented national lockdown, the UK was opting for a mitigation strategy (to develop herd immunity) rather that acting to suppress the virus. The subsequent wave of hospitalizations and deaths forced a u-turn. New Zealand, Singapore, Taiwan, Vietnam, and South Korea are all countries that acted early and aggressively. Many of them did not even had the luxury of being affected later respect to others.
The articles in this section aim to understand, measure and quantify the efficacy of different NPIs in the mitigation/suppression of COVID-19. Some investigate their impact on the unfolding of COVID-19. Others focus on a range of behaviors beside those directly targeted by the interventions, variations induced on medical practice, and financial markets (see Table 5). It is important to mention how a large part of the first subgroup could be also classified as epidemic models. In fact, some measure the evolution of and others use compartmental models. These papers however aim at singling out the impact on NPIs on the spreading, thus I thought to highlight them here.
As usual, before diving in the research, let me say few words about the sample of papers. They report analysis and observations from countries. In fact, while many of them focus on a particular country, others consider a wide range of them. USA, China and Italy are again at the top of the list (see Fig. 5). The authors of the articles in this category are affiliated with institutions from countries. USA, China, and the UK are the most represented. Furthermore, the research has been published in journals ranging from PNAS and Nature Human behavior to Lancet Oncology and JAMA. The most represented journals are the International Journal of Environmental Research and Public Health and Science. As of December 19th these paper received citations.
Fig. 5.
Total number of authors and citations of the papers in this category on the left. Note that these numbers are estimated from Semantic Scholar. On the right (top) histogram describing the number of countries subject of study in this category. Note how I have removed from the count, few papers that studied hundreds of countries as I could not find machine readable lists. On the right (bottom) most represented publication venues of the category. To improve visibility I am showing only journals featuring at least two articles.
6.1. Classification
The sample of papers studying the impact of NPIs can be further classified in three main categories:
-
1.
Effects on spreading: describes papers that quantify the impact of NPIs on COVID-19 spreading;
-
2.
Effects on behaviors: describes articles aiming to characterize how NPIs have affected a range of behaviors and activities;
-
3.
Effects on medical practice: describes research efforts quantifying the impact of NPIs on health care
Let us dive into the details.
Table 5.
Summary of the articles aimed at measuring the effects of NPIs. The left column describes the main categories in this group of articles.
| Subcategory | Country and references |
|---|---|
| Effects on spreading | Argentina, Bolivia, Brazil, Chile, Colombia, Paraguay, Peru, and Uruguay [309]; Australia [310] Bangladesh [311]; China [31], [32], [33], [312], [313], [314], [315]; China, Germany, India, Italy, Singapore, South Korea, Spain, UK, USA [316]; Italy [317], [318]; New Zealand [319]; Puerto Rico [320]; South Korea [321]; Taiwan [322]; USA [323], [324], [325], [326], [327], [328]; 44 countries [329]; 53 countries [330]; 56 countries [331]; 142 countries [332]; 149 countries [333] |
| Effects on behaviors | China [334]; China, Italy [335]; Denmark, Sweden [336]; Germany [337] USA [338], [339], [340], [341]; 20 countries [342]; 67 countries [343] |
| Effects on medical practice | Italy [344]; Netherlands [345]; UK [346], [347] |
6.2. Effects on spreading
These articles study the impact on the unfolding of the disease focusing on the measures adopted in a specific country [31], [32], [33], [309], [310], [311], [312], [313], [315], [317], [318], [319], [320], [322], [323], [324], [325], [326], [327], proposing multi country analyses [316], [329], [330], [331], [332], [333], and characterizing the effects of NPIs on other diseases [314], [321], [328].
Ref. [310] studies the impact of travel bans in Australia from China. In doing so, authors use historical data describing the mobility flows from China to Australia, the evolution of the epidemic in China and developed an age-structured SIER-like model to describe the unfolding of the local pandemic given importations from the epicenter of the outbreak. The analysis of the initial phases of the spread suggests that the travel ban has been effective in reducing the number of infected seeds coming in the country which might have resulted in faster local growth of cases. Authors of Ref. [312] use publicly available data to create a database capturing transmission pairs outside Hubei province. These describe the onset of symptoms and, for about half, the social relationships, infector and infectee pairs in the first month of the emergency. The analysis of the data suggests how the implementation of NPIs was key to shorten the serial interval from 7.8 days, in the early phases of the spreading, to 2.2 days. As more cases were promptly identified and isolated the opportunities for the virus to start new infection chains decreased drastically. From a methodological stand point the authors suggest the use of time-varying estimates of serial interval in the computation of key epidemic indicators such as the reproductive number to avoid biased results. In Ref. [32] authors analyzed the features of 32,583 cases in Wuhan. They considered as set of features such as socio-demographic, occupation and severity of illness. Their analysis confirms the strong impact of NPIs which in about two months were able to bring the reproductive from values above to values well below one. Health workers have been affected at higher rates respect to the general population (more than 3 times), and the portion of the severe cases drastically reduced from the initial phases to over the intervention period. Authors in Ref. [315] study more than infected individuals and their close contacts (more than 15,000). The dataset captures almost 20,000 exposure events in Hunan (China) from mid January to early April 2020. The primary infections have been identified by the surveillance network, their closed contacts have been followed for at least two weeks and some of them were tested if developed symptoms before February 7. After this date all contacts were required to be tested even if asymptomatic. The authors studied the transmission risks according to the type (i.e., household, social, community, family, healthcare), duration, timing of exposure and as function of the NPIs put in place. By using a logistic regression model they find that household contacts are the most risky type of exposures. Extended family, social and community contacts followed. Interestingly, contacts in healthcare settings have been found to have the lowest risk, hinting to the efficacy of protective equipment and measures put place in those settings. The results show that the effects of NPIs varies as function of the type of contact. In fact, the lockdown increased household contacts increasing the risk for further transmission at home. The same measure instead drastically reduced community and social contacts. Longer exposures increase the risk of infection and transmission risk was found to be higher around the time of first symptoms. Children were confirmed to be less susceptible than individuals with age between and . People older than was found significantly more susceptible. The data allowed the authors to study serial intervals and the impact of NPIs on their distribution. Consistently with other observations, the serial interval decreased from 7.3 days for individuals isolated more than days after symptoms to 1.7 days for those isolated days after showing signs of the disease. Interestingly, the authors are able to describe the type of case detection (passive or active surveillance) as the pandemic unfolded and NPIs strategies adapted. While in the early phases (before January ) about 80% of cases were detected and isolated only after showing symptoms, thus via passive surveillance, with a median time from onset to isolation of more than 5 days, after the 4th of February this time difference become negative ( days) thanks to active contact tracing. This clearly shows the key role of aggressive testing and tracing strategies to reduce the chances of further transmission. Ref. [31] uses real-time mobility data, case and travel history across China to access the impact of NPIs in the country. The authors show how in the early phases the spatial distribution of cases is captured by and highly correlated with mobility data. The correlation drops significantly soon as after the implementation of NPIs (in particular travel restrictions). The results point also to clear decrease in the serial distribution showing the impact of strict surveillance and highlighting the effectiveness of the implemented measures to suppress the spreading of COVID-19. Ref. [33] analyzes epidemic and mobility data across China to describe the impact and effect of NPIs during the first days of the pandemic. The mobility data was constructed aggregating information from location-based services (i.e., mobile apps), migration and Baidu datasets. The authors use a linear regression model to link the arrival of cases in other cities with the travel bans in Wuhan. The results show a very high correlation (0.98) and that cities with larger populations and more connected with Wuhan had earlier importations. The authors build also a linear regression model the link the timing and type of NPIs implemented in cities and the number of cases in the first week of local outbreak. The results suggest how cities that acted early had a lower burden and that stopping intracity transportation, entertainment venues, and banning public gatherings are the NPIs more associated with reductions in cases. Interestingly, the results show also that the cordon sanitaire in Wuhan, though important for the suppression of the disease, induced only a delay of about days in the arrival of the disease in other cities. Ref. [313] uses detailed data from contact tracing in China to estimate the transmission patterns in households settings. The results suggest higher infectivity during the pre-symptomatic phase, higher susceptibility for people , and highlight the importance of case isolation and aggressive contact tracing of close contacts. Similar conclusions have been drawn in the context Vó, a small municipality in Veneto (Italy) [318]. The city has been the first to report a confirmed COVID-19 death in Italian soil and was one of the first hotspots of the pandemic in the country. The authors conduced two surveys collecting demographic, clinical, and contact network information as well as testing the presence of infection in a large fraction of the population (85.9% and 71.5% respectively). The results show how when the lockdown was put in place (first survey) the prevalence was about 1%. After the lockdown (second survey) the prevalence was slightly smaller than 3%. Remarkably, about 42% of cases were asymptomatic. The results informed the local policy makers and, due to the high number of asymptomatic, testing has been conducted to all contacts of positive individuals in the region of Veneto. This approach has been critical to suppress effectively the virus during the first wave. Authors in Ref. [319] present an analysis of all confirmed cases in New Zealand. The country is often considered as one of the models for COVID-19 suppression. In fact, the early and strong implementation of NPIs has resulted in (almost) disease elimination. The authors study a range of features for each subject: demographic, health outcomes, transmission patterns, serial intervals, and testing coverage across the different phases of the response. The results show how the implementation of NPIs reduced the serial intervals and isolation times. Testing increased across time and the response has shown to limit disparities across socio-economic groups. Ref. [320] presents the analysis of NPIs in the context of Puerto Rico. The results, which focused on the initial phases of the outbreak, suggest a high efficacy of the measures. The authors estimate that without interventions the death toll could have been three times higher. Authors of Ref. [323] study the differences of disease burden across US States linking them with the heterogenous implementation and adoption of NPIs. In doing so, they included a wide range of correlates such as population density, fraction of population above , life expectancy, years of schooling, income, vaccination rate and testing rates. Furthermore, they adopted two indexes proxies of the tendency of each subpopulation to adopt measures which might benefit the community and the tendency to follow rules. Though in the USA NPIs widely varied across states the authors identified five which are the most adopted: declaration of state-emergency, limit size of social gatherings, school closure, strict restaurant operations, and stay at home orders. In the early phases of the pandemic lower density and higher vaccination rates were significantly associated with slower growth rates. Restricting restaurant was the only variable predictive of doubling time. However, the authors note how states that implemented more actions earlier have been more effective in reducing the growth. In Ref. [324] authors use an econometric approach to correlate policies, informations about the spreading, behavioral changes measured as variation in mobility from the Google mobility reports, with disease progression in the USA. The findings confirm both top-down and bottom-up NPIs had an impact in the mitigation effort. Ref. [325] presents a statistical analysis of the effect of school closures on the progression of the disease in the USA. In doing so, they consider a range of covariates such as other NPIs, demographic and socio-economic informations. The results show that closures of school were linked, temporally, with a reduced disease burden measured both in terms of cases and deaths. Interestingly, they observe that the effectiveness of school closures has been higher when they were implemented earlier. The authors note how measuring the effect of a single NPIs when several are in place is particular hard. Finally, authors in Ref. [326] study a population of pregnant women in New York City that shared information about their residence (borough), age and SARS-CoV-2 test outcomes. Authors adopt a Bayesian approach to quantify the prevalence in each borough from the sample. Furthermore they consider general mobility data captured from Facebook to study the link between prevalence and adoption of NPIs (estimated from the mobility data). The results suggest a city-wide prevalence of 15.6% up to early May which however varied from 11% in Manhattan to 26% in South Queens. Interestingly, prevalence was low in borough with higher reduction in morning traffic out and evening traffic into them.
Authors in Ref. [333] analyze the impact of NPIs in countries. In doing so, they built a linear regression model where the dependent variable is the logarithm of the number of cases at time and the independent variables describe the days since the first confirmed case, a dummy variable describing the present or absence of interventions, the days since the start of the interventions, and the population size. They assume a week delay from the implementation of NPIs to their effect. They also consider a range of other covariates such as different demographic and socio-economic indicators. Furthermore, they consider five NPIs: school closure, remote working, limits on social gatherings, closure of public transportation, and lockdown. Interestingly, in the period between 1st of January and 30th of May, the authors observe that at least one of those NPIs was put in place in all countries. All five have been put in place in countries, at least four in and just three in . Tanzania put in place two (school closure and limits on social gatherings) and Belarus only one (school closure). These observations clearly show the global impact of the COVID-19 pandemic. The results suggest how the implementation of any NPIs is linked to a decrease of 13% in incidence. Higher GDP per capita, higher percentage of population about and country security index were associated with stronger reductions. The effects of implementing all five rather than four measures are found to be similar. A smaller reduction was found in countries implementing only three of them. Combinations of school closures, remote working and limits on mass gatherings with or without closure of public transport was linked to decreases in disease burden. Early implementation of lockdowns has been found associated with large reduction of incidence. Authors of Ref. [331] aim to estimate the impact of NPIs in countries by looking at the variations of . In particular, they studied the dataset discussed in details below, which provides a taxonomy and temporal information about the range of NPIs implemented across the globe. Interestingly, they compute the ranking of effectiveness considering four different methods: linear regression where each NPIs together with other covariates is used to estimate the variation of , lasso regression done assuming that without intervention would be constant and that variations are linked to the implementation of NPIs, random forest considering the variation of and neural networks that approximate taking as input the set of NPIs and . The estimation of is done using EpiEstim which we have discussed above. The results suggest how lockdowns, limits on social gathering, remote working and school closures are the most effective NPIs. Border restrictions are also found to have a significant impact. Other less costly measures such as risk communication strategies that promote healthy behaviors are found to be important. It is interesting to note how food programs and financial support are also significant as they help people to adopt NPIs without the risk of harsh economic consequences. Ref. [332] investigates the impact of NPIs in countries. In doing so, they link, via a regression model, the variations of with NPIs considering also several country specific covariates. The results confirm the effectiveness of lockdowns and travel bans. Furthermore they suggest that partial lockdowns might be as effective as full lockdowns if implemented earlier. Authors in Ref. [330] combine data from the Oxford COVID-19 Government Response Tracker (which is discussed below) [348], epidemiological indicators, Google mobility reports, and socio-economic data from the World Bank to study the impact of NPIs in countries. Differently from the other approaches mentioned above, here the authors use a compartmental SIR model with time-varying parameters and link the logarithm of the transmission rate for each country to the NPIs and other covariates via a regression model. Their findings suggest that the impact of school closures and remote working decreases with employment rate, portion of elderly, country extension, population density and increase of GDP per capita as well as expenditure in health care. The authors reflect on the fact that adoption rates of NPIs could be less pronounced in case of low risk perception, younger population, and a stronger health care system. Authors in Ref. [316] study the time series of the cumulative number of cases in a range of countries such as India, USA, and Singapore. They study variance, autocorrelation, skewness and other indicators to capture signals of slow down linked to implementation of NPIs. The results confirm how the timing of intervention is a key variable that might explain successful suppression strategies.
Authors in Ref. [314] investigate the effects of NPIs induced by COVID-19 on the seasonal flu in China. The drastic measures put in place to hamper the spreading of SARS-CoV-2 were extremely efficient to stop transmission chains also of the flu. The findings suggest a reduction of 64% respect compared with previous years. In the context of South Korea and with a wider range of diseases (i.e., chickenpox, mumps, invasive pneumococcal disease, scarlet fever and pertussis) Ref. [321] estimates the impact of NPIs put in place in response of COVID-19 on these diseases. They use an ARIMA (autoregressive integrated moving average) model built considering historical data to compare estimated incidence of each disease with observations. The results suggest a large reduction (36%) for chickenpox. For mumps they observe a marginal reduction only in the young population ( years old). Reductions of about 80% were reported for respiratory viruses. Ref. [328] investigates the effects of NPIs on two endemic infections in the USA: respiratory syncytial virus and seasonal influenza. By studying detailed surveillance data and using an epidemic model, the authors note how behavioral changes induced by COVID-19 have reduced their transmission by at least 20%. As a result of the increased fraction of susceptible population the results indicate the chances of large future outbreaks.
6.3. Effects on behaviors
Within this category we find articles exploring the impact of NPIs on online activities [334], [335], [341], [342], health [338], [339], [340], mobility [337], spending [336], and performance of financial markets [343].
Authors in Ref. [335] study the effect of the lockdown in Twitter and Weibo users in Lombardy and Wuhan. The first is the most affected Italian region in the first wave. The second is the epicenter of the pandemic. In doing so, they mined content posted two weeks before and after the lockdowns. They extracted psycholinguistic features from the posts. The results suggest that in Wuhan the attention shifted towards religion, emotions and social groups. In posts written in Lombardy the authors noted a decrease of stress and an increase of topics related to leisure. Ref. [342] studies data from Google Trends in European countries to investigate possible shifts in attention towards nature and environmental topics during the pandemic. Their findings suggest that, since the beginning of the COVID-19 crisis and the implementation of strict NPIs, interest towards nature increased significantly. The effect is not so visible for environmental topics instead. Ref. [334] studies the link between posts and mobility from Sina Weibo in Sichuan, China. In more details, authors investigate variations in the overall content posted and mobility (proxy of behavioral changes) as function of the different NPIs and COVID-19 phases. Initially the increase of cases is linked to increase of negative emotions and decrease of mobility. As the number of cases kept increasing the authors observe a decrease in negative sentiments posted and a stabilization of mobility. After the peak decrease of negative posts and increase of mobility is reported. Overall the results show how the peak of negative emotion proceeded the epidemic peak as well as the variation of mobility patterns thus hinting to a significant bottom-up reaction in the population. Ref. [341] investigates the increase of anti-asian sentiments expressed on Twitter as result of the pandemic. Unfortunately, even political leaders publicly referred to COVID-19 as the chinese virus. The authors mined about three million tweets from USA and used SVM (support vector machine) to estimate the sentiment associated to them. The collection considered a dictionary of more than keywords defined in previous race-related studies and a database of racial slurs. Unfortunately, the authors detect an increase of anti-asian posts by 67% comparing pre and post-COVID-19 posts.
Ref. [338] studies the runs of emergency medical services for opioid overdose in Kentucky (USA) before and after the state of emergency declaration in the state. In a background of decrease of runs for other conditions the authors observed an increase of calls for opioid overdose by 17%, and an increase of 50% in calls for suspected overdose with deaths at the scene. Overall the results are tragic, alarming and highlight the possible consequence of health emergencies that drastically modify societal activities. Authors in Ref. [339] study the variations in Google searches related with mental health before and after the stay at home order declaration in several US states. The results indicate that searches linked to negative thoughts, anxiety, suicidal ideation among others increased before the stay at home order and level off at the time of the announcements. Despite the research is based on a very large number of searches, the period of analysis covers only one week. Hence, more work is needed to investigate these trends, potentially considering second/third waves and subsequent NPIs.
Ref. [337] uses mobile phone data to study the changes in mobility patterns in Germany. Interestingly, they investigate a time period covering the first lockdown and the relaxation of NPIs put in place. The results suggest a long lasting variation in the mobility patterns that remained in place despite the lifting of top-down constraints. In fact, the authors show how long range movements across the country have been considerably reduced and as consequence the mobility network in the new normal is considerably more local and clustered.
Authors in Ref. [336] use real-time transactions data in Sweden and Denmark to understand the effects of COVID-19 and different NPIs strategies on consumer spending. The results suggest how during the emergency spending dropped on average by 25% in Sweden and by 29% in Denmark. The small differences is particularly interesting considering that Denmark adopted a suppression strategy with a lockdown rather than a mitigation strategies with general social distancing and other restrictions without the social nuclear option of a shutdown. The findings suggest how the reduction in spending is largely caused by the virus. Considering the much higher disease burden in Sweden these results highlight how suppression strategies are a better control method when considering also economic factors. Finally, authors in Ref. [343] study the link between performance of financial markets and NPIs in countries. They consider stock returns volatility and study their association with NPIs. The results suggest higher volatility (which might induce large-scale sale of risky assets and higher cost of capital) in countries that implemented stricter NPIs policies. Interestingly, information campaigns and events cancellations are found to be the major contributors of volatility.
6.4. Effects on medical practice
Here we find four articles investigating and estimating the effects of NPIs on medical practice. Authors in Ref. [346] use historical data to estimate the effects of diagnostic delays for breast, colorectal, esophageal and lung cancer in the UK. In fact, NPIs limited drastically visits, specialistic follow-up and routine screenings. The results paint a very grim picture with a projected increase of avoidable cancer deaths. These go from 8%–10% for breast cancer to 15%–17% for lung cancer. The authors call for urgent policy interventions to mitigate these tragic losses. In the context of a cohort of patients living with HIV in Italy, Ref. [344] highlights the negative impact of the pandemic and NPIs. Visits missed, decrease of new diagnosis respect of historical baselines, and a drop of antiretroviral therapy dispensation paint a grim picture even in this case. Ref. [347] aims to characterize the increase in ICU deaths linked to limited capacity. In the context of the UK, the modeling scenarios developed by the authors suggest that a significant impact could be obtained doubling beds and reducing length of stay by 25%. Finally, Ref. [345] studies the effect of NPIs in a long term care institution in the Netherlands specialized on intellectual disabilities. The authors focused on incidents reported during the emergency respect to historical data. The lockdown has caused a reduction across all types of incidents however, those linked with aggression spiked up quickly soon after highlighting the need for developing specific protocols which are better suited for patients with intellectual disabilities.
7. Reviews
Not surprisingly, I am not the first to think about writing a review about NPIs during the COVID-19 pandemic. In fact, the sample of papers I am analyzing here contains articles which can be classified as reviews. Some of them could be also considered as perspectives and/or comments, but I opted to include them here as they provide a broad overview of a particular topic or context. This section will be much shorter than the others. In fact, considering the nature of these articles, providing a summary of them is probably more appropriate for meta-analyses.
The efforts behind the compilation of these articles come from more than authors with affiliations in countries (see Fig. 6). The UK and USA are at the top of the list. Furthermore, in terms of publication venues, we find journals that range from interdisciplinary domains such as Nature Communications to more specialized such as BMC Oral Health. These articles already received citations.
Fig. 6.
Total number of authors and citations of the papers in this category on the left. Note that these numbers are estimated from Semantic Scholar. On the right histogram describing the number of countries representing authors’ affiliations.
7.1. Classification
By looking at the angle and focus, the sample of reviews can be further grouped in categories (see Table 6):
-
1.
Non-pharmaceutical interventions: describes articles which focus on different aspects of NPIs such as types, effectiveness, and their modeling;
-
2.
Change in medical practice: captures articles summarizing approaches, results, and success stories about the adaptation of medical practices to NPIs;
-
3.
Adoption of NPIs: considers articles discussing the issues and challenges linked to adoption of NPIs in different contexts;
-
4.
Impact of digital technologies: describes reviews summarizing the opportunities and challenges that new technologies (such as mobile phones) offer in the fight against COVID-19
Table 6.
Summary of reviews articles in the sample. The first column describe the categories. The second instead, the topic and references.
| Category | Topic and references |
|---|---|
| Non-pharmaceutical interventions | Effectiveness of NPIs [36], [349], [350], [351], [352]; Effects of NPIs [353], [354], [355], [356], [357]; Epidemic modeling [358] |
| Change in medical practice | Surgery [34], [359]; Ophthalmology [35]; Disease control [360]; Dentistry [361] |
| Adoption of NPIs | [362], [363] |
| Impact of digital technology | [364], [365] |
7.2. Non-pharmaceutical interventions
In this category we find reviews that discuss the effectiveness of NPIs [36], [298], [349], [350], [351], [352], their effects [353], [354], [355], [356], [357] and modeling [358].
In particular, Ref. [349] reviews the modeling efforts measuring the effects of NPIs in the Indian context. Authors in Ref. [350] summarize the evidences about NPIs efficacy and approaches adopted across the globe. They highlight how portfolios of measures appear to be more effective than single interventions. Similar conclusions are drawn in Ref. [36] where the authors also stress the key importance of right timing in the implementation of NPIs. Ref. [352] reviews the evidence about the efficacy and challenges of both pharmaceutical and non-pharmaceutical interventions.
Ref. [353] reviews the literature focused on the psychological impacts of NPIs with particular attention to minorities and disadvantaged groups, which unfortunately have been more affected by both disease and NPIs. Authors in Ref. [354] review the evidences about the impact of NPIs on education. They highlight the importance of considering the ripple effects that school closures have on students, parents, economy, and mental health. Ref. [355] analyzes the literature focused on the effects of NPIs on eating disorders. In doing so, it provides a range of suggestions and approaches to tackle the issue. Authors in Ref. [356] study the literature about the psychological impact of the pandemic on pregnant women highlighting the particular needs of this high-risk group. In the same spirit of considering a particular group of individuals, Ref [357] investigates the effects of NPIs and COVID-19 on professional drivers pointing out how the emergency has introduced a wide range of new stressors that sum up to those already in place. Finally, Ref. [358] provides a summary of the modeling approaches put forward to model COVID-19 and capture NPIs.
7.3. Change in medical practice
In this category we find articles that summarize the evidence, approaches and suggestions on how to adapt medical practice in the middle of the COVID-19 pandemic. We find articles focused on surgery [34], [359], ophthalmology [35], disease control (routine vaccination campaigns) [360] and dentistry [361].
7.4. Adoption of NPIs
Here we find two articles that provide a summary about the factors influencing the adoption of NPIs. Ref. [363] confirms how adoption of health behaviors is linked to a range of factors, form socio-economic to psychological. Authors in Ref. [362] summarize the practical issues linked to NPIs adoption in several African countries where lack of water and soap are unfortunately widespread.
7.5. Impact of digital technology
Here, we find two reviews that highlight the incredible opportunities offered by digital technologies to capture behaviors, their changes and inform modeling as well as policies [364], [365]. Interestingly, they also discuss the issues linked to privacy, legal, ethical concerns and biases in the data.
8. Measuring NPIs via proxy data
Every call we make or receive, every time we connect to internet via our mobile phones, all posts we leave on social media platforms, all queries we submit in search engines and all the times we swipe our credit cards are just few examples of our daily activities that leave digital traces. The data is recorded and stored by a wide range of companies to enable services, meet legal obligations, and billing purposes. However, such data offers unprecedented opportunities to measure and understand a variety of human behaviors which are of epidemiological relevance [366]. Information about which cell towers we are connected to when making a call or surfing the web can be used to infer our location and movements. The content, topic, and other meta data linked to our posts on Twitter, Facebook or online searches might be studied to estimate our health status, our concerns about a health emergency, judge our level of exposition to low quality information or our mobility. Our digital payments might be used to detect life changing moments (i.e., pregnancies), infer our mobility patterns, or gathering socio-economic information about people similar to us, people living in our neighborhoods, city or country. In general, this data offers high-resolution proxies for many societal activity and behaviors. Due to serious privacy risks and concerns such data is stored in what we can call digital vaults. Luckily, over the last few years corporations, academia, and institutions at various levels have been working to unleash the potential hidden in these proxies while taking all the necessary steps to preserve privacy and to respect stringent regulations. In fact, a range of so called Data for Good initiatives have been put in place with the aim of leveraging high-resolution datasets collected by companies in non-for-profit applications. I said luckily because these ecosystems, their success, and great potential were in places before the COVID-19 pandemic. This, together with the scale and magnitude of the emergency, has allow tech giants such as Google, Apple, Facebook and large mobile phone operators such as Telefonica, Vodafone, Orange as well as smaller companies such as SafeGraph, Cuebiq among others to promptly step-up and provide invaluable data to the scientific community. It is hard to imagine these efforts put in place so quickly, safely, and extensively just five–ten years ago. COVID-19 is probably the largest data for good effort ever assembled.
In this category, we find articles aiming to measure, quantify, monitor and capture NPIs via data proxies. It is interesting to stress the range of data types and sources used. From information collected via mobile phone apps, services, GPS, and wifi connections to posts on Twitter, Reddit, views of Wikipedia pages or credit card records.
Though the large majority of studies in the sample are based on data collected in the USA, the penetration of mobile phones allowed researchers to mine data from nearly all countries in the world (see Fig. 7). These research efforts have been produced by more than authors, affiliated with institutions from countries. Again USA, Italy and UK are on the top of the list. In terms of publication venues, this sample has been published in journals. PNAS, Nature Human behavior and PLoS One are in the top of the list. It is not surprising to see these interdisciplinary journals in this category. In fact, the research efforts are based on a fusion of different approaches and techniques which are not bounded by specific scientific domains. In terms of citations, this sample collected (as of Dec 19) citations.
Fig. 7.
Total number of authors and citations of the papers in this category on the left. Note that these numbers are estimated from Semantic Scholar. On the right (top) histogram describing the number of countries subject of study in this category. Note how few papers using data from hundreds of countries are not counted in the histogram. On the right (bottom) most represented publication venues of the category.
8.1. Classification
Considering their topics and aims these articles can be classified in two categories (see Table 7):
-
1.
Adoption of NPI: describes articles that tackle the issue of NPIs adoption;
-
2.
Mobility changes: are papers that study the effects of NPIs on human mobility
Let us dive in some details.
Table 7.
Summary of the articles measuring NPIs via proxy data. The first column describes the main categories. The second the type of data used. The third, the country of study and the references.
| Category | Proxy data type | Country and reference |
|---|---|---|
| Adoption of NPI | Mobile phones and/or vehicles through location intelligence and measurement platforms |
USA [367], [368], [369], [370], [371], [372] |
| Twitter |
Twitter population [373], [374] |
|
| Wikipedia and Reddit |
Canada, Italy, USA, UK [375] |
|
| Google |
USA [376]; 130 countries [377] |
|
| TV | USA [378] | |
| Mobility changes | Mobile phones and/or vehicles through location intelligence and measurement platforms |
USA [37], [38], [379], [380] |
| Facebook |
Italy [39] |
|
| Citymapper app | 22 countries [381] | |
8.2. Adoption of NPIs
Here, we find articles aimed at quantifying the adoption of NPIs via proxy data such as mobile phones collected by location intelligence companies [367], [368], [369], [370], [371], [372], Twitter [373], [374], COVID-19 ad-hoc apps [196], Wikipedia and Reddit [375], Google [376], [377], and TV viewings [378].
Authors in Ref. [367] use data from SafeGraph and Facebook to quantify social distancing at the county level in the USA. In particular, SafeGraph provides information about access to locations and POIs. Home locations are obtained considering the typical position of each phone in the night. Work locations are inferred considering where phones spend three (i.e., part-time) or six (i.e., full-time) hours outside home. These locations are identified using data from January, hence pre-NPIs. Aggregating all the observations at the county level the authors identified a social distancing index for each county in day defined as:
| (6) |
where describes individuals that appear not to have left home in day , those that appear to have gone at work, and the total number of devices in county . The authors measured also the (online) social connectedness of each county considering Facebook friendship data as:
| (7) |
where is the number of social connections in Facebook between county and county or country (if outside USA) , is the number of Facebook users in each considered location. They also study the timeline of NPIs put in place, epidemic indicators and built a regression model to find the association between social distancing with social connectedness, NPIs, and cases. The results show that counties with higher online social ties with China and Italy where more likely to comply with NPIs. This points to the fact that being exposed to informations from highly affected areas might influence risk perception and thus behavior change. Furthermore, the results show differences between political leanings, education levels, and stands about climate changes. The link between political affiliations and NPIs adoption is studied also in Ref. [369]. Here, authors use mobile phone data to test whether aggregated variation in mobility are associated with political leanings at the state level. By using a regression model the authors find a significant negative correlation between fraction of republicans and NPIs adherence (measured in terms of mobility reduction). This link was found to be significant adjusting for population, poverty rates, Gini index, urbanization levels, and portion of essential workers. Similarly authors in Ref. [370] study mobile data collected by SafeGraph to measure the association between political views and mobility reductions. In doing so, they considered behaviors, aggregated at the level of counties, after governors issued recommendations to physical distance. These typically preceded stay at home orders or other top-down restrictions. By using a regression model, built considering a wide range of covariates, the author confirms the role of political leanings in response to such recommendation thus in self-initiated behavioral changes. The recommendations had a significant effect on overall mobility, comparable to the stay at home orders. The effects are found to be stronger in democratic counties and even stronger in case of republican governors. The link between mobility reduction and political affiliation is studied also in Ref. [371]. Here, the authors used mobile phone data collected by Unacast from about M users in the USA as well as consumption levels of conservative traditional media (i.e., TV). Their results confirm a correlation between adherence to NPIs and political leanings at the level of counties. In fact, counties that in 2016 voted for Trump show, on average, 14% less mobility reduction and those that went to Hillary Clinton. Also in this case, political affiliation was found to be a stronger predictor of mobility variation than other variables such as density, income, and demographic informations. The authors point out how counties that voted for Trump have been hit harder by the virus and show higher infections and fatality rates. Authors of Ref. [368] use mobile phone data collected by Cuebiq to investigate the possible association between adoption of NPIs (proxied as mobility reduction) and religiosity of US states (measured via six indexes). The results from a regression analysis suggest that states classified as more religious showed a lower and slower reduction of mobility. Furthermore, stay at home orders appear to have weaker effects in such states. The results highlight once again how adoption of behavioral changes is a multifaceted problem linked to a wide range of perceptions and beliefs. Authors in Ref. [372] use mobile phone data collected by Unacast to study the socio-economic factors influencing adherence to NPIs, measured as variation in mobility following stay at home orders, in the USA. By using a regression approach the authors confirm how low income counties complied less with the orders than high income ones. These effects are visible considering confounding factors as political leanings, population density, unemployment rates among others.
Authors in Ref. [373] tackle a key issue which might have dire consequence in adoption of protective behaviors: the spreading of mis-information on social media. Focusing on Twitter, they collected and mined Millions of tweets and develop a Infodemic Risk Index to monitor the exposure to low quality information of users across countries. Their results show that the spread of unreliable information typically precedes the local rise of cases potentially affecting adoption to NPIs. Interestingly however, after the initial phases reliable information seems to take over. Ref. [374] studies the communication strategies of official accounts (i.e., public health, emergency services, officials) on Twitter during the evolution of the emergency. In fact, the ability to reach effectively a large user base to promote safe and verified recommendation as well as explaining measures and regulations in place is key. The results show how the inclusion of engaging content such as videos/photos and hashtags increases sharing. Posts with content linked to epidemic indicators, technical information, content related to measures to contain the spreading and flatten the curve were re-shared more widely. Authors in Ref. [375] study users attention to the COVID-19 emergency considering as proxy Wikipedia page views and discussion on Reddit. The results show how these were initially driven by media coverage (traditional media such as news articles and YouTube videos published by news organization). However, while media coverage remained high, the authors found evidence of decline in public attention raising questions about risk perception and COVID-19 fatigue on NPIs compliance. Authors of Ref. [376] study the association between NPIs related keywords on Google Trends and disease burden in each US state. Using a regression model they find that attention towards NPIs related keywords, measured using proxy queries in Google, is associated (0.42) with higher deaths per capita and case-fatality (0.60). They also confirm the association between political leanings. Ref. [377] studies the association between mobility changes measured via the Google mobility reports and economic, social and governmental features in countries. The results indicate a reduction of mobility across the board with patterns which are specific to the evolution of the epidemic in each location. Countries with more authoritarian governments (where Google is however less likely to have access) were found to be more responsive to changes of mobility as cases increased. This points to another dimension of compliance to NPIs. Finally, Ref. [378] studies local television coverage and survey data in rural settings in the USA. The results suggest that despite local news tend to be urban-centric they can still affect adoption of NPIs. In fact, the authors find that rural residents are more likely to adopt social distancing if they live in a media market more affected by the disease, which is driven by close by cities. The survey data allowed the authors to confirm, at least for a sample, that these effects are linked to local news viewings. The authors note how though significant these effects are about half respect to those driven by partisanship.
8.3. Mobility changes
About half of the papers that measured NPIs via proxy data focused on the changes in mobility that travel bans, school closure, remote working, local and national lockdowns have induced in the population. While there is rich variety of data sources used, this data is collected via mobile phones by location intelligence and measurement platforms [37], [38], [368], [369], [379], [380], tech giants such as Facebook [39], [367] and Google [377], [382], as well as other mobile apps [381]. Indeed the high penetration of smart phones, their portability, the vital role they took in our daily lives, the popularity of some apps and services make them the perfect tool to infer high-resolution data about our movements and their possible changes.
Ref. [379] studies data collected via mobile phone as well as vehicles to characterize the variations of aggregated mobility in the USA during the early phases of the pandemic (January–April). The results indicate how the overall mobility decreased markably following the national emergency declaration. Interestingly, the results confirm how the population reacted before the stay at home mandates by reducing their mobility voluntarily maybe nudged by news and increase risk perception. The observed patterns however shows high levels of spatial heterogeneity linked to income and population density. Authors in Ref. [380] study the data collected from more than M users in the USA from third party data providers. They focused on county level mobility patterns. The data can be explored via an interactive dashboard https://data.covid.umd.edu/. The observations show how travels outside counties decreased by 35% when the national emergency was declared. The reduction however did not last long. By using a simultaneous equations model, they investigated the link between the inflow in each county and the number of infections. The model is based on two expressions. One for the number of cases in county in a day , . To limit fluctuations this number is computed considering , thus a seven day window. The second is an expression for the inflow in the same county. In this case where is a lag period. In both expressions they include autoregressive terms, as well as county and temporal covariates. Using this approach, they observed a particularly strong association between the mobility and infections in states that relaxed the NPIs. Ref. [38] adopts a range of datasets: exposure indexes (which effectively estimate the number of devices in contact in 14-days periods, as done by many contact tracing apps) computed by PlaceIQ [383], Google mobility reports and data from SafeGraph. Their observations indicated how poorer areas decrease mobility less than wealthier. Even more, they observed a reversal: wealthier areas were more mobile than poorer before the emergency. This findings confirm observations from many other articles and, considering that low income neighborhoods are affected by low access to health care and higher level of preexisting conditions, point to the fact that NPIs and the pandemic are affecting society heterogeneously, targeting disproportionally already challenged groups. Authors of Ref. [37] use mobile phone data collected by Teralytics, a location intelligence company, describing the mobility across and within counties in the USA. They defined a mobility ratio (MR) metric to measure the variations of mobility patterns in each county at time as:
| (8) |
where describes the number of trips from county to at time and is the baseline values before the emergency thus in absence of NPIs. Note how in both numerator and denominator the second and third terms are not the same quantity repeated but consider in and out flow for each county. They then computed the growth rate ratio for epidemiological data. They compare the moving average of the number of cases in each and days periods. They studied the association between the two metrics in counties. The results show a correlation between variation of mobility (induced by NPIs) and disease growth ratio above 0.7 in out of counties. The changes in mobility however are not visible in the progress of the disease before 9–12 days and up to three weeks, which is compatible with generation times. Furthermore, they confirm how changes in mobility preceded official restrictions. Authors in Ref. [39] use Facebook mobility data to study the impact of strict NPIs put in place in the first wave in Italy. They also consider socio-economic data. Their results confirm, also in the Italian context, how individuals living in cities with higher fiscal capacity where able to reduce more mobility. Furthermore, they observe stronger reductions in municipalities with higher levels of inequalities. Authors in Ref. [381] use data from cities in countries collected via the transportation app Citymapper. They study the association between mobility and NPIs policies. Across the board they find a strong correlation between the decline in mobility and the COVID-19 Government Response Stringency Index [348]. The variation of mobility linked to a specific NPIs is stronger for closing public transport (18%) probably due to the nature of the data, workplace closure (15%), restriction of internal movement (13%), school closure (10%) and borders restrictions (5%).
9. Datasets
The last category describes publicly available datasets capturing different aspects of NPIs. Here, I am considering only datasets that have been featured in publications and shared with the community. There are many popular others that we mentioned several times above such as Google mobility reports, Apple mobility reports, and Facebook Data for Good datasets which have been put forward by the corporate world through their data for good initiatives.
The datasets, especially those describing the timeline of NPIs, cover large part of the countries in the world. They have been shared thanks to the work of more than authors affiliated in institutions from countries (see Fig. 8). In terms of publication venues, we find six journals. The most represented, with two publications, is Scientific Data which is a journal from the Springer Nature family dedicated to description and sharing of datasets. Others journals we find are Nature Human Behavior and PloS One. As of December 19th these articles received citations, with a median of 1.5.
Fig. 8.
Total number of authors and citations of the papers in this category on the left. Note that these numbers are estimated from Semantic Scholar. On the right (top) histogram describing the number of countries describing authors’ affiliations. On the right (bottom) most represented publication venues of the category.
9.1. Classification
The datasets in the sample can be divided in three categories (see Table 8):
-
1.
Implementation of NPIs: describes datasets providing detailed information about the timelines and typology of NPIs;
-
2.
Mobility: captures variations to human mobility induced by NPIs;
-
3.
Contacts: describes datasets providing information about physical contacts which can be used to feed many of the age-structured epidemic models discussed above
Let us dive into some details.
Table 8.
Summary of the articles presenting a dataset relevant for NPIs. The first column is the main category. The second provides information about country/countries of study and references.
| Category | Country and references |
|---|---|
| Implementation of NPIs | Government response trackers: Canada [384], 195 countries [385], 180 countries [348], 56 countries [42]; Universities response in USA [386] |
| Mobility | Australia, Brazil, China, Ghana, India, Iran, Italy, Norway, South Africa, USA [387]; Italy [40] |
| Contacts | Belgium, China, Finland, France, Germany, Italy, Hong Kong, Luxembourg, Netherlands, Poland, Peru, Russia, South Africa, UK, Vietnam, Zambia, Zimbabwe [41] |
9.2. Implementation of NPIs
Here we find datasets describing institutional interventions. The majority of them focused on governmental responses. One considered the specific context of Universities.
Ref. [348] describes the Oxford COVID-19 Government Response Tracker. The data can be downloaded and explored via this url: https://ourworldindata.org/policy-responses-covid. The dataset provides information about indicators capturing governmental responses. The taxonomy is organized in four main categories. The first is containment and closure which is further divided in school closures, workplace closures, public event bans, restrictions of social gathering size, closure of public transport, stay at home requirements, national and international travel restrictions. The second type is economic response which is divided in income support, debt/contract relief for households, fiscal measures, giving international support. The third category is health systems which captures public information campaign, testing policies, contact tracing, emergency investments in health care as well as vaccines, facial coverings and vaccination policies. The fourth describes other responses. Some of the variables are ordinal, others are numerical. Furthermore, variables provide information at a geographical level. The resolution can go from country to city. Beside the data, the authors provide ready to use indexes that can be readily adopted in modeling efforts. These are: (1) the overall governmental response index, (2) the stringency index, (3) the containment and health index, (4) the economic support index.
Ref. [42] provides data describing the implementation of NPIs in countries that can be downloaded form this url: https://github.com/amel-github/covid19-interventionmeasures. The taxonomy created is organized in four levels. The first is divided in (1) case identification, contact tracing and related measures, (2) environmental measures, (3) healthcare and public health capacity, (4) resource allocation, (5) risk communication, (6) social distancing, (7) travel restriction, and (8) returning to normal life. The other levels provide finer and finer description of each measure. The data comes as a timeline of events. Each one with a specific ID, country, state, region, date, classification in the four levels, status (which describe whether the measure is an extension of an old measure), comments, and source of information.
Authors in Ref. [385] present the CoronaNet dataset with the timeline of NPIs implemented in countries. The dataset is available here https://www.coronanet-project.org/. The data is organized in a taxonomy that provides information about (i) type of NPIs implemented (16 in total) (ii) the type of government implementing the intervention (i.e., national or provincial) (iii) geographical target of the measure (i.e., national, provincial) (iv) the human or material target of the NPI (i.e., face masks, travelers) (v) the directionality of the policy (i.e., outbound, inbound) (vi) the mechanism of travel targeted by the measure (i.e., trains, flights), (vii) whether the measure is mandatory or voluntary, (viii) the nature of the enforcer (i.e., government, military) (ix) the timing of the policy (i.e., date of announcement and/or implementation). Besides the description of the dataset, Ref. [385] applies a Bayesian approach to study the evolution of NPIs strategies across countries. They observe a clear acceleration of more costly measures in mid-March 2020, when indeed we observed a rapid escalation as mentioned above.
Authors in Ref [384] apply the taxonomy defined by the Oxford COVID-19 Government Response Tracker to the case of Canada. The data, together with many other relevant datasets from Canada and other countries, can be found here: https://howsmyflattening.ca/#/data.
Finally, authors in Ref. [386] describe a dataset describing the strategies adopted by US universities. The data can be explored here: https://covidtracking.com/. By looking at official COVID-19 pages created by Universities, which describe the portfolio of measures put in place, the authors studied five (binary) variables: (1) remote learning (2) discourage campus housing (3) travel bans (4) close campus (5) remote working. It is interesting to note how the analysis of the data, points out very high heterogeneity in terms of NPIs in the country.
9.3. Mobility
In this category we find datasets describing the effects of NPIs on human mobility.
Ref. [40] provides information about the mobility of more than 80,000 users in Italy, estimated via mobile phones by Cuebiq, a location intelligence and measurement platform. The data covers the period from January 18 to April 17 and is available here: https://data.humdata.org/dataset/covid-19-mobility-italy. The dataset provides different indicators. The first is the daily origin–destination matrices between Italian provinces. These are normalized directed flows computed by tracing the movements across provinces of the users. The authors count as a stop only the locations where users stay for more than one hour. In doing so, transits are discounted. The second measure is the radius of gyration of users which provides information about their range of mobility. This metric is computed weekly. The third metric is the proximity network which provides information about the possible social contacts between users. These are relevant for modeling the transmission dynamics of the virus. To build this network, authors consider time windows of one hour and connect all users within a radium of .
Ref. [387] describes a survey conducted among more than 9,000 individuals in Australia, Brazil, China, Ghana, India, Iran, Italy, Norway, South Africa, USA. The answers are made available here: https://doi.org/10.7910/dvn/eiquga. The data provides demographic information and answers to several questions about the transportation modes before and after the start of the pandemic. Furthermore, the authors queried participants about their perception about COVID-19 related risks in transportation system.
9.4. Contacts
In this category we find a research project called SOcial Contact RATES (Socrates) [41]. The authors assembled a range of contact matrices, across different countries (Belgium, China, Finland, France, Germany, Italy, Hong Kong, Luxembourg, Netherlands, Poland, Peru, Russia, South Africa, UK, Vietnam, Zambia, Zimbabwe), both in pre and post COVID-19 periods. The data and interactive tool to explore and extract it in ready to use format is available here: http://www.socialcontactdata.org/.
10. Conclusions and outlook
What are the main take-home messages from the sample of the literature considered?
Many articles helped to define the features of the virus and its transmission. SARS-CoV-2 is characterized by large . The majority of models estimate values in the 3–4 range, depending on the region/country. Due to lack of adequate testing (especially in the early phases) and a large fraction of asymptomatic infections the virus spread largely undetected. Several data-driven modeling efforts show heterogeneity in disease transmission. A minority of cases is responsible for a large fraction of infections. Furthermore, some locations such as restaurants, hotels, workplaces are risker locations for infections. Detailed analysis of confirmed cases and their contacts show how household contacts are also responsible for a large fraction of infections (especially during lockdowns) followed by extended family interactions. Children are found to be less susceptible and less at risk of severe outcomes. On the contrary, individuals older than are found to be more susceptible and at higher risk of death. Crowded cities are affected by higher attack rates and longer epidemic waves.
Many articles aimed to measure the effects of NPIs. Across the board, the modeling efforts unanimously show the importance and effectiveness of NPIs in slowing down the spread of COVID-19. Interestingly, the timing of their implementation is a critical variable. Countries that acted early, with respect to the local spread, were most successful in controlling the spread and reported markedly lower death tolls. In several contexts, only a staggered NPI strategy was enough to bring the below the critical value. A range of articles highlights how a patchy and inconsistent geographical NPI strategy is linked to worst health outcomes. It might induce behavioral changes, such as travel further for an activity, which ultimately might accelerate the spreading. The study of the conditions necessary to reach herd immunity, without overflowing the health care system, point out that dynamic mitigation strategies are unrealistic and unpractical. Even more, several articles, some factoring in also economic metrics, point to the fact that suppression is preferable to mitigation in the long run. Many research efforts show the large impact of one of the simpler and less costly NPIs: face masks. Analyses of NPIs adopted across many countries as well as data-driven epidemic models highlight how banning public gatherings, limiting social gatherings, school closures, remote working, and lockdowns are the most efficient top-down measures. It is important to notice, how the heterogeneity of infection outcomes as function of age, the difference in socio-demographic stratifications, and intergenerational contacts across different countries suggest that one-fits-all NPIs strategy might be far from optimal. Measures should be custom-tailored to the specific context of each population.
Despite their efficacy NPIs came with high societal costs. Several articles in the sample highlight the impact on mental health, loneliness, domestic abuse, sex, food consumption, and substance abuse among others. The way health care facilities operated had to drastically change. The quick shift towards telemedicine and remote care allowed to provide help to a countless number of patients. However, several surveys highlight the challenges that this induced. From lack of enough support and socio-economic disparities to the tragic increase of preventable deaths for several types of cancers due to reduction of screening. Also the education sector had to adapt drastically. The results point to the effectiveness of remote learning as well as the challenges that it entails which go from the lack of social interactions, the key to the development of children, to the impossibility of meeting some learning outcomes linked to practical skills. Even though strict NPIs have increased the time spent at home, a large survey conducted among scientists in the USA and Europe points to the fact that female scientists, those in experimental fields and with young children had to reduce the time spent doing research.
When it comes to adoption and adherence to NPIs a range of articles paint a very complex picture pointing out several factors influencing behavioral changes. Gender, education, age, and political leanings are examples. Several surveys suggest that women are more likely to comply with NPIs and to consider COVID-19 as a real risk. Similar patterns are observed in individuals with higher education levels. When it comes to age, the results indicate how young and older adults are less likely to comply with NPIs. Few articles, in the context of the USA, indicate how republican leaning counties were less likely to reduce mobility and were associated with a higher impact of the disease. The research points also to a big urban–rural divide and the importance of socio-economic factors. People living in urban settings were found more informed, and in the context of the developing world, more equipped to adopt protective behaviors. Across the board, thus also in the richest countries, adoption of NPIs is linked to socio-economic indicators: individuals in high-income brackets are able to drastically reduce their mobility with respect to low-income brackets. Heterogeneity in terms of infection rates in disadvantaged socio-economic groups is also reported. These effects, together with the worst access to health care and higher levels of comorbidities, induced disproportionally higher disease burden in low-income groups. There is evidence suggesting that food programs and financial support, implemented as part of containment strategies, help NPIs adoption. Several articles point to the fact that, though many NPIs were imposed top-down, big variations in mobility patterns were observed before official orders. This suggests that bottom-up, spontaneous, behavioral changes took place in several contexts.
Despite the incredible effort of many scientific communities, there are still open questions and challenges for future work.
We do not have a validated theory to describe the feedback loop between behaviors and diseases. Before COVID-19 the research on NPIs was mainly theoretical. Lack of empirical data describing behavioral changes was the main limitation. During the COVID-19 pandemic unprecedented high-resolution datasets, capturing different aspects of NPIs, have been collected and shared. The large majority of models used them as input. Thus, we transitioned from theoretical approaches in the pre-COVID-19 world to data-driven modeling post-COVID-19. In fact, with few exceptions, the vast theoretical literature on the subject has been neglected during the pandemic. As mentioned in one of the perspectives [291], pandemics are a war period for modelers. Information is sparse, knowledge limited, answers a real commodity. Access to data has allowed the luxury to avoid developing (or adapting) models of behavioral changes and focus on other aspects. As result, despite great progress, we still do not have a validated theory to describe NPIs. It is important to mention how there are very popular and successful approaches, such as the health belief model [388], [389], [390], which allow us to understand the drivers of behavioral changes, but we still lack a practical, solid, and well validated theoretical framework to readily model the feedback loop between diseases and behaviors. The data collected during the COVID-19 pandemic will be of crucial importance to tackle this challenge in the future.
We do not have standardized metrics to compare or judge epidemic models. Epidemic models are the most represented category in the sample of papers considered here. We find a wide range of approaches and methodologies. While they all seem to do a decent job in reproducing the epidemic patterns, it is far from clear how to compare them or how to judge their efficacy. As noted in one of the perspectives [292], going forward the challenge is to define standard metrics to evaluate their performance. Competition is not the goal. The aim is to compare their predictive power, quantify their reliability and sensitivity to assumptions.
We need to strengthen Data for Good initiatives. Many companies have provided unprecedented datasets to estimate the effects of NPIs on our behaviors. The data have been shared thanks to several Data for Good programs. Their value and impact in the fight against COVID-19 cannot be overstated. As we move towards the end of the pandemic, I hope these initiatives will become even more popular rather than shrink dramatically. Extensions, definition of standard metrics, and privacy concerns are key challenges for future work.
We need to improve availability and accessibility of public health data. Within few months, we saw incredible progresses on this front. Many health agencies, organizations and initiatives created APIs that allow to download official cases and death counts at different geographical resolutions. However, much more work is needed. Some countries still do not share all the data collected. For example, detailed information about onset of symptoms, and breakdown of data per age-bracket are often not shared or provided by regional initiatives in very unhelpful formats (i.e., pdfs). In other cases, we see still long delays before the data is shared. The new SARS-CoV-2 variant spreading in the UK is an example. After several weeks, data is still spread across sources and sparse. One of the major challenges going forward is to improve data access and sharing standards.
We do not know much about the long terms of NPIs. NPIs have affected virtually any activity and societal process. As noted in many articles, especially those written in the context of health care, going forward key challenges are linked to study their long-term effects and to develop strategies/policies to cope with them.
Promoting high quality information is key. The adoption of health promoting behaviors is a complex phenomenon affected by many variables. In the current landscape access to information and misinformation is critical. As we transition towards the largest vaccination campaign ever attempted and as we prepare for future health emergencies, understanding how to promote high-quality information and demote misinformation is a key challenge for future work.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Editor: I. Procaccia
Footnotes
Until December 18th, .
As of December 19th .
References
- 1.Vespignani Alessandro. Predicting the behavior of techno-social systems. Science. 2009;325(5939):425–428. doi: 10.1126/science.1171990. [DOI] [PubMed] [Google Scholar]
- 2.Verelst Frederik, Willem Lander, Beutels Philippe. Behavioural change models for infectious disease transmission: a systematic review (2010–2015) J. R. Soc. Interface. 2016;13(125) doi: 10.1098/rsif.2016.0820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Funk Sebastian, Salathé Marcel, Jansen Vincent A.A. Modelling the influence of human behaviour on the spread of infectious diseases: a review. J. R. Soc. Interface. 2010;7(50):1247–1256. doi: 10.1098/rsif.2010.0142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Savi Maharaj, Tamsin McCaldin, Adam Kleczkowski, A participatory simulation model for studying attitudes to infection risk, in: Proceedings of the 2011 Summer Computer Simulation Conference, 2011, pp. 8–13.
- 5.Chen Frederick, Griffith Amanda, Cottrell Allin, Wong Yue-Ling. Behavioral responses to epidemics in an online experiment: using virtual diseases to study human behavior. PLoS One. 2013;8(1) doi: 10.1371/journal.pone.0052814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhong Wei, Kim Yushim, Jehn Megan. Modeling dynamics of an influenza pandemic with heterogeneous coping behaviors: case study of a 2009 H1N1 outbreak in Arizona. Comput. Math. Organ. Theory. 2013;19(4):622–645. [Google Scholar]
- 7.Gray Richard T., Hoare Alexander, McCann Pol Dominic, Bradley Jack, Down Ian, Donovan Basil, Prestage Garrett, Wilson David P. Will changes in gay men’s sexual behavior reduce syphilis rates? Sex Transm. Dis. 2011;38(12):1151–1158. doi: 10.1097/OLQ.0b013e318238b85d. [DOI] [PubMed] [Google Scholar]
- 8.Rubin G. James, Amlôt Richard, Page Lisa, Wessely Simon. Public perceptions, anxiety, and behaviour change in relation to the swine flu outbreak: cross sectional telephone survey. Bmj. 2009;339:b2651. doi: 10.1136/bmj.b2651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rubin G. James, Bakhshi Savita, Amlôt Richard, Fear Nicola, Potts Henry W.W., Michie Susan. The design of a survey questionnaire to measure perceptions and behaviour during an influenza pandemic: the flu telephone survey template (flutest) NIHR J. Library. 2014 [PubMed] [Google Scholar]
- 10.Shim Eunha, Chapman Gretchen B., Townsend Jeffrey P., Galvani Alison P. The influence of altruism on influenza vaccination decisions. J. R. Soc. Interface. 2012;9(74):2234–2243. doi: 10.1098/rsif.2012.0115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bayham Jude, Kuminoff Nicolai V., Gunn Quentin, Fenichel Eli P. Measured voluntary avoidance behaviour during the 2009 A/H1N1 epidemic. Proc. R Soc. Lond. 2015;282(1818) doi: 10.1098/rspb.2015.0814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cohen Matan J., Brezis Mayer, Block Colin, Diederich Adele, Chinitz David. Vaccination, herd behavior, and herd immunity. Med. Decis. Making. 2013;33(8):1026–1038. doi: 10.1177/0272989X13487946. [DOI] [PubMed] [Google Scholar]
- 13.Fierro Annalisa, Liccardo Antonella. Lattice model for influenza spreading with spontaneous behavioral changes. PloS One. 2013;8(12) doi: 10.1371/journal.pone.0083641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Durham David P., Casman Elizabeth A. Incorporating individual health-protective decisions into disease transmission models: a mathematical framework. J. R. Soc. Interface. 2012;9(68):562–570. doi: 10.1098/rsif.2011.0325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gozzi Nicolò, Perrotta Daniela, Paolotti Daniela, Perra Nicola. Towards a data-driven characterization of behavioral changes induced by the seasonal flu. PLoS Comput. Biol. 2020;16(5) doi: 10.1371/journal.pcbi.1007879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pawelek Kasia A., Oeldorf-Hirsch Anne, Rong Libin. Modeling the impact of twitter on influenza epidemics. Math. Biosci. Eng. 2014;11(6):1337. doi: 10.3934/mbe.2014.11.1337. [DOI] [PubMed] [Google Scholar]
- 17.Collinson Shannon, Khan Kamran, Heffernan Jane M. The effects of media reports on disease spread and important public health measurements. PLoS One. 2015;10(11) doi: 10.1371/journal.pone.0141423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xiao Yanni, Tang Sanyi, Wu Jianhong. Media impact switching surface during an infectious disease outbreak. Sci. Rep. 2015;5:7838. doi: 10.1038/srep07838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Poletti Piero, Ajelli Marco, Merler Stefano. The effect of risk perception on the 2009 H1N1 pandemic influenza dynamics. PLoS One. 2011;6(2) doi: 10.1371/journal.pone.0016460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Funk Sebastian, Gilad Erez, Watkins Chris, Jansen Vincent A.A. The spread of awareness and its impact on epidemic outbreaks. Proc. Natl. Acad. Sci. 2009;106(16):6872–6877. doi: 10.1073/pnas.0810762106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.He Daihai, Dushoff Jonathan, Day Troy, Ma Junling, Earn David J.D. Inferring the causes of the three waves of the 1918 influenza pandemic in England and Wales. Proc. R Soc. Lond. 2013;280(1766) doi: 10.1098/rspb.2013.1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chinazzi Matteo, Davis Jessica T., Ajelli Marco, Gioannini Corrado, Litvinova Maria, Merler Stefano, y Piontti Ana Pastore, Mu Kunpeng, Rossi Luca, Sun Kaiyuan, Viboud Cécile, Xiong Xinyue, Yu Hongjie, Halloran M. Elizabeth, Longini Ira M., Vespignani Alessandro. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020;368(6489):395–400. doi: 10.1126/science.aba9757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Prem Kiesha, Liu Yang, Russell Timothy W., Kucharski Adam J., Eggo Rosalind M., Davies Nicholas, Jit Mark, Klepac Petra, Flasche Stefan, Clifford Samuel, Pearson Carl A.B., Munday James D., Abbott Sam, Gibbs Hamish, Rosello Alicia, Quilty Billy J., Jombart Thibaut, Sun Fiona, Diamond Charlie, Gimma Amy, van Zandvoort Kevin, Funk Sebastian, Jarvis Christopher I., Edmunds W. John, Bosse Nikos I., Hellewell Joel. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study. Lancet Public Health. 2020;5(5):e261–e270. doi: 10.1016/S2468-2667(20)30073-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Flaxman Seth, Mishra Swapnil, Gandy Axel, Unwin H. Juliette T., Mellan Thomas A., Coupland Helen, Whittaker Charles, Zhu Harrison, Berah Tresnia, Eaton Jeffrey W., Monod Mélodie, Ghani Azra C., Donnelly Christl A., Riley Steven, Vollmer Michaela A.C., Ferguson Neil M., Okell Lucy C., Bhatt Samir. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020;584(7820):257–261. doi: 10.1038/s41586-020-2405-7. [DOI] [PubMed] [Google Scholar]
- 25.Zhang Juanjuan, Litvinova Maria, Liang Yuxia, Wang Yan, Wang Wei, Zhao Shanlu, Wu Qianhui, Merler Stefano, Viboud Cécile, Vespignani Alessandro, Ajelli Marco, Yu Hongjie. Changes in contact patterns shape the dynamics of the COVID-19 outbreak in China. Science. 2020;368(6498):1481–1486. doi: 10.1126/science.abb8001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reznik Alexander, Gritsenko Valentina, Konstantinov Vsevolod, Khamenka Natallia, Isralowitz Richard. COVID-19 fear in eastern europe: Validation of the fear of COVID-19 scale. Int. J. Ment. Health Addict. 2020 doi: 10.1007/s11469-020-00283-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jarvis Christopher I., Zandvoort Kevin Van, Gimma Amy, Prem Kiesha, Klepac Petra, Rubin G. James, Edmunds W. John. Quantifying the impact of physical distance measures on the transmission of COVID-19 in the UK. BMC Med. 2020;18(1) doi: 10.1186/s12916-020-01597-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eubank S., Eckstrand I., Lewis B., Venkatramanan S., Marathe M., Barrett C.L. Commentary on ferguson, et al., impact of non-pharmaceutical interventions (NPIs) to reduce COVID-19 mortality and healthcare demand. Bull. Math. Biol. 2020;82(4) doi: 10.1007/s11538-020-00726-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Oliver Nuria, Lepri Bruno, Sterly Harald, Lambiotte Renaud, Deletaille Sébastien, Nadai Marco De, Letouzé Emmanuel, Salah Albert Ali, Benjamins Richard, Cattuto Ciro, Colizza Vittoria, de Cordes Nicolas, Fraiberger Samuel P., Koebe Till, Lehmann Sune, Murillo Juan, Pentland Alex, Pham Phuong N., Pivetta Frédéric, Saramäki Jari, Scarpino Samuel V., Tizzoni Michele, Verhulst Stefaan, Vinck Patrick. Mobile phone data for informing public health actions across the COVID-19 pandemic life cycle. Sci. Adv. 2020;6(23):eabc0764. doi: 10.1126/sciadv.abc0764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jiao Wen Yan, Wang Lin Na, Liu Juan, Fang Shuan Feng, Jiao Fu Yong, Pettoello-Mantovani Massimo, Somekh Eli. Behavioral and emotional disorders in children during the COVID-19 epidemic. J. Pediatr. 2020;221:264–266.e1. doi: 10.1016/j.jpeds.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kraemer Moritz U.G., Yang Chia-Hung, Gutierrez Bernardo, Wu Chieh-Hsi, Klein Brennan, Pigott David M., du Plessis Louis, Faria Nuno R., Li Ruoran, Hanage William P., Brownstein John S., Layan Maylis, Vespignani Alessandro, Tian Huaiyu, Dye Christopher, Pybus Oliver G., Scarpino Samuel V. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science. 2020;368(6490):493–497. doi: 10.1126/science.abb4218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pan An, Liu Li, Wang Chaolong, Guo Huan, Hao Xingjie, Wang Qi, Huang Jiao, He Na, Yu Hongjie, Lin Xihong, Wei Sheng, Wu Tangchun. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. JAMA. 2020;323(19):1915. doi: 10.1001/jama.2020.6130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tian Huaiyu, Liu Yonghong, Li Yidan, Wu Chieh-Hsi, Chen Bin, Kraemer Moritz U.G., Li Bingying, Cai Jun, Xu Bo, Yang Qiqi, Wang Ben, Yang Peng, Cui Yujun, Song Yimeng, Zheng Pai, Wang Quanyi, Bjornstad Ottar N., Yang Ruifu, Grenfell Bryan T., Pybus Oliver G., Dye Christopher. An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science. 2020;368(6491):638–642. doi: 10.1126/science.abb6105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Simone B. De, Chouillard E., Saverio S. Di, Pagani L., Sartelli M., Biffl W.L., Coccolini F., Pieri A., Khan M., Borzellino G., Campanile F.C., Ansaloni L., Catena F. Emergency surgery during the COVID-19 pandemic: what you need to know for practice. Annals. 2020;102(5):323–332. doi: 10.1308/rcsann.2020.0097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Romano Mario R., Montericcio Alessio, Montalbano Clara, Raimondi Raffaele, Allegrini Davide, Ricciardelli Gabriella, Angi Martina, Pagano Luca, Romano Vito. Facing COVID-19 in ophthalmology department. Curr. Eye Res. 2020;45(6):653–658. doi: 10.1080/02713683.2020.1752737. [DOI] [PubMed] [Google Scholar]
- 36.Imai Natsuko, Gaythorpe Katy A.M., Abbott Sam, Bhatia Sangeeta, van Elsland Sabine, Prem Kiesha, Liu Yang, Ferguson Neil M. Adoption and impact of non-pharmaceutical interventions for COVID-19. Wellcome Open Res. 2020;5:59. doi: 10.12688/wellcomeopenres.15808.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Badr Hamada S., Du Hongru, Marshall Maximilian, Dong Ensheng, Squire Marietta M., Gardner Lauren M. Association between mobility patterns and COVID-19 transmission in the USA: a mathematical modelling study. Lancet Infect. Dis. 2020;20(11):1247–1254. doi: 10.1016/S1473-3099(20)30553-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Weill Joakim A., Stigler Matthieu, Deschenes Olivier, Springborn Michael R. Social distancing responses to COVID-19 emergency declarations strongly differentiated by income. Proc. Natl. Acad. Sci. USA. 2020;117(33):19658–19660. doi: 10.1073/pnas.2009412117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bonaccorsi Giovanni, Pierri Francesco, Cinelli Matteo, Flori Andrea, Galeazzi Alessandro, Porcelli Francesco, Schmidt Ana Lucia, Valensise Carlo Michele, Scala Antonio, Quattrociocchi Walter, Pammolli Fabio. Economic and social consequences of human mobility restrictions under COVID-19. Proc. Natl. Acad. Sci. USA. 2020;117(27):15530–15535. doi: 10.1073/pnas.2007658117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pepe Emanuele, Bajardi Paolo, Gauvin Laetitia, Privitera Filippo, Lake Brennan, Cattuto Ciro, Tizzoni Michele. COVID-19 outbreak response, a dataset to assess mobility changes in Italy following national lockdown. Sci. Data. 2020;7(1) doi: 10.1038/s41597-020-00575-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Willem Lander, Hoang Thang Van, Funk Sebastian, Coletti Pietro, Beutels Philippe, Hens Niel. SOCRATES: an online tool leveraging a social contact data sharing initiative to assess mitigation strategies for COVID-19. BMC Res. Notes. 2020;13(1) doi: 10.1186/s13104-020-05136-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Desvars-Larrive Améie, Dervic Elma, Haug Nils, Niederkrotenthaler Thomas, Chen Jiaying, Natale Anna Di, Lasser Jana, Gliga Diana S., Roux Alexandra, Sorger Johannes, Chakraborty Abhijit, Ten Alexandr, Dervic Alija, Pacheco Andrea, Jurczak Ania, Cserjan David, Lederhilger Diana, Bulska Dominika, Berishaj Dorontinë, Tames Erwin Flores, Ávarez Francisco S., Takriti Huda, Korbel Jan, Reddish Jenny, Grzymala-Moszczyńska Joanna, Stangl Johannes, Hadziavdic Lamija, Stoeger Laura, Gooriah Leana, Geyrhofer Lukas, Ferreira Marcia R., Bartoszek Marta, Vierlinger Rainer, Holder Samantha, Haberfellner Simon, Ahne Verena, Reisch Viktoria, Servedio Vito D.P., Chen Xiao, Pocasangre-Orellana Xochilt María, Garncarek Zuzanna, Garcia David, Thurner Stefan. A structured open dataset of government interventions in response to COVID-19. Sci. Data. 2020;7(1) doi: 10.1038/s41597-020-00609-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mayor of London announcement March 11th. https://www.facebook.com/sadiqforlondon/posts/3025766374142796, Accessed: 2020-05-11.
- 44.Karnakov Petr, Arampatzis Georgios, Kii Ivica, Wermelinger Fabian, Wlchli Daniel, Papadimitriou Costas, Koumoutsakos Petros. Data-driven inference of the reproduction number for COVID-19 before and after interventions for 51 European countries. Swiss Med. Wkly. 2020 doi: 10.4414/smw.2020.20313. [DOI] [PubMed] [Google Scholar]
- 45.Loeffler-Wirth Henry, Schmidt Maria, Binder Hans. Covid-19 transmission trajectories–monitoring the pandemic in the worldwide context. Viruses. 2020;12(7):777. doi: 10.3390/v12070777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bo Yacong, Guo Cui, Lin Changqing, Zeng Yiqian, Li Hao Bi, Zhang Yumiao, Hossain Md Shakhaoat, Chan Jimmy W.M., Yeung David W., Kwok Kin On, Wong Samuel Y.S., Lau Alexis K.H., Lao Xiang Qian. Effectiveness of non-pharmaceutical interventions on COVID-19 transmission in 190 countries from 23 January to 13 April 2020. Int. J. Infect. Dis. 2021;102:247–253. doi: 10.1016/j.ijid.2020.10.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Walker Patrick G.T., Whittaker Charles, Watson Oliver J., Baguelin Marc, Winskill Peter, Hamlet Arran, Djafaara Bimandra A., Cucunubá Zulma, Mesa Daniela Olivera, Green Will, Thompson Hayley, Nayagam Shevanthi, Ainslie Kylie E.C., Bhatia Sangeeta, Bhatt Samir, Boonyasiri Adhiratha, Boyd Olivia, Brazeau Nicholas F., Cattarino Lorenzo, Cuomo-Dannenburg Gina, Dighe Amy, Donnelly Christl A., Dorigatti Ilaria, van Elsland Sabine L., FitzJohn Rich, Fu Han, Gaythorpe Katy A.M., Geidelberg Lily, Grassly Nicholas, Haw David, Hayes Sarah, Hinsley Wes, Imai Natsuko, Jorgensen David, Knock Edward, Laydon Daniel, Mishra Swapnil, Nedjati-Gilani Gemma, Okell Lucy C., Unwin H. Juliette, Verity Robert, Vollmer Michaela, Walters Caroline E., Wang Haowei, Wang Yuanrong, Xi Xiaoyue, Lalloo David G., Ferguson Neil M., Ghani Azra C. The impact of COVID-19 and strategies for mitigation and suppression in low- and middle-income countries. Science. 2020:eabc0035. doi: 10.1126/science.abc0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cotta Renato M., Naveira-Cotta Carolina P., Magal Pierre. Mathematical parameters of the COVID-19 epidemic in Brazil and evaluation of the impact of different public health measures. Biology. 2020;9(8):220. doi: 10.3390/biology9080220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Maier Benjamin F., Brockmann Dirk. Effective containment explains subexponential growth in recent confirmed COVID-19 cases in China. Science. 2020;368(6492):742–746. doi: 10.1126/science.abb4557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lobato Fran Sérgio, Libotte Gustavo Barbosa, Platt Gustavo Mendes. Identification of an epidemiological model to simulate the COVID-19 epidemic using robust multiobjective optimization and stochastic fractal search. Comput. Math. Methods Med. 2020;2020:1–8. doi: 10.1155/2020/9214159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Din Anwarud, Li Yongjin, Khan Tahir, Zaman Gul. Mathematical analysis of spread and control of the novel corona virus (COVID-19) in China. Chaos Solitons Fractals. 2020;141 doi: 10.1016/j.chaos.2020.110286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wangping Jia, Ke Han, Yang Song, Wenzhe Cao, Shengshu Wang, Shanshan Yang, Jianwei Wang, Fuyin Kou, Penggang Tai, Jing Li, Miao Liu, Yao He. Extended SIR prediction of the epidemics trend of COVID-19 in Italy and compared with Hunan, China. Front. Med. 2020;7 doi: 10.3389/fmed.2020.00169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hsiang Solomon, Allen Daniel, Annan-Phan Sébastien, Bell Kendon, Bolliger Ian, Chong Trinetta, Druckenmiller Hannah, Huang Luna Yue, Hultgren Andrew, Krasovich Emma, Lau Peiley, Lee Jaecheol, Rolf Esther, Tseng Jeanette, Wu Tiffany. The effect of large-scale anti-contagion policies on the COVID-19 pandemic. Nature. 2020;584(7820):262–267. doi: 10.1038/s41586-020-2404-8. [DOI] [PubMed] [Google Scholar]
- 54.Visscher Alex De. The COVID-19 pandemic: model-based evaluation of non-pharmaceutical interventions and prognoses. Nonlinear Dyn. 2020;101(3):1871–1887. doi: 10.1007/s11071-020-05861-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dehning Jonas, Zierenberg Johannes, Spitzner F. Paul, Wibral Michael, Neto Joao Pinheiro, Wilczek Michael, Priesemann Viola. Inferring change points in the spread of COVID-19 reveals the effectiveness of interventions. Science. 2020;369(6500):eabb9789. doi: 10.1126/science.abb9789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ray Debashree, Salvatore Maxwell, Bhattacharyya Rupam, Wang Lili, Du Jiacong, Mohammed Shariq, Purkayastha Soumik, Halder Aritra, Rix Alexander, Barker Daniel, et al. Predictions, role of interventions and effects of a historic national lockdown in India’s response to the the COVID-19 pandemic: Data science call to arms. Harv. Data Sci. Rev. 2020 doi: 10.1162/99608f92.60e08ed5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Calafiore Giuseppe C., Novara Carlo, Possieri Corrado. A time-varying SIRD model for the COVID-19 contagion in Italy. Annu. Rev. Control. 2020 doi: 10.1016/j.arcontrol.2020.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Althouse Benjamin M., Wallace Brendan, Case Brendan, Scarpino Samuel V., Allard Antoine, Berdahl Andrew M., White Easton R., Hébert-Dufresne Laurent. The unintended consequences of inconsistent pandemic control policies. medRxiv. 2020 doi: 10.1186/s44263-023-00028-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bhanot Gyan, DeLisi Charles. 2020. Analysis of Covid-19 data for eight European countries and the United Kingdom using a simplified SIR model. [Google Scholar]
- 60.Lei Hao, Wu Xifeng, Wang Xiao, Xu Modi, Xie Yu, Du Xiangjun, Cowling Benjamin J., Li Yuguo, Shu Yuelong. Different transmission dynamics of COVID-19 and influenza suggest the relative efficiency of isolation/quarantine and social distancing against COVID-19 in China. Clin. Infect. Dis. 2020 doi: 10.1093/cid/ciaa1584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Scala Antonio, Flori Andrea, Spelta Alessandro, Brugnoli Emanuele, Cinelli Matteo, Quattrociocchi Walter, Pammolli Fabio. Time, space and social interactions: exit mechanisms for the Covid-19 epidemics. Sci. Rep. 2020;10(1) doi: 10.1038/s41598-020-70631-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.López Leonardo, Rodó Xavier. The end of social confinement and COVID-19 re-emergence risk. Nat. Hum. Behav. 2020;4(7):746–755. doi: 10.1038/s41562-020-0908-8. [DOI] [PubMed] [Google Scholar]
- 63.Ogden Nick H., Fazil Aamir, Arino Julien, Berthiaume Philippe, Fisman David N., Greer Amy L., Ludwig Antoinette, Ng Victoria, Tuite Ashleigh R., Turgeon Patricia, Waddell Lisa A. Modelling scenarios of the epidemic of COVID-19 in Canada. CCDR. 2020:198–204. doi: 10.14745/ccdr.v46i06a08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Anderson Sean C., Edwards Andrew M., Yerlanov Madi, Mulberry Nicola, Stockdale Jessica E., Iyaniwura Sarafa A., Falcao Rebeca C., Otterstatter Michael C., Irvine Michael A., Janjua Naveed Z., Coombs Daniel, Colijn Caroline. Quantifying the impact of COVID-19 control measures using a Bayesian model of physical distancing. PLoS Comput. Biol. 2020;16(12) doi: 10.1371/journal.pcbi.1008274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Alauddin Md, Khan Md Aminul Islam, Khan Faisal, Imtiaz Syed, Ahmed Salim, Amyotte Paul. How can process safety and a risk management approach guide pandemic risk management? J. Loss Prev. Process Ind. 2020;68 doi: 10.1016/j.jlp.2020.104310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Yang Qihui, Yi Chunlin, Vajdi Aram, Cohnstaedt Lee W., Wu Hongyu, Guo Xiaolong, Scoglio Caterina M. Short-term forecasts and long-term mitigation evaluations for the COVID-19 epidemic in Hubei Province, China. Infect. Dis. Model. 2020;5:563–574. doi: 10.1016/j.idm.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hao Xingjie, Cheng Shanshan, Wu Degang, Wu Tangchun, Lin Xihong, Wang Chaolong. Reconstruction of the full transmission dynamics of COVID-19 in Wuhan. Nature. 2020;584(7821):420–424. doi: 10.1038/s41586-020-2554-8. [DOI] [PubMed] [Google Scholar]
- 68.Li Qian, Tang Biao, Bragazzi Nicola Luigi, Xiao Yanni, Wu Jianhong. Modeling the impact of mass influenza vaccination and public health interventions on COVID-19 epidemics with limited detection capability. Math. Biosci. 2020;325 doi: 10.1016/j.mbs.2020.108378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Yan Qinling, Tang Yingling, Yan Dingding, Wang Jiaying, Yang Linqian, Yang Xinpei, Tang Sanyi. Impact of media reports on the early spread of COVID-19 epidemic. J. Theoret. Biol. 2020;502 doi: 10.1016/j.jtbi.2020.110385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Liu Pei-Yu, He Sha, Rong Li-Bin, Tang San-Yi. The effect of control measures on COVID-19 transmission in Italy: Comparison with Guangdong province in China. Infect Dis. Poverty. 2020;9(1) doi: 10.1186/s40249-020-00730-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Overton Christopher E., Stage Helena B., Ahmad Shazaad, Curran-Sebastian Jacob, Dark Paul, Das Rajenki, Fearon Elizabeth, Felton Timothy, Fyles Martyn, Gent Nick, Hall Ian, House Thomas, Lewkowicz Hugo, Pang Xiaoxi, Pellis Lorenzo, Sawko Robert, Ustianowski Andrew, Vekaria Bindu, Webb Luke. Using statistics and mathematical modelling to understand infectious disease outbreaks: COVID-19 as an example. Infect. Dis. Model. 2020;5:409–441. doi: 10.1016/j.idm.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kantner Markus, Koprucki Thomas. Beyond just flattening the curve: Optimal control of epidemics with purely non-pharmaceutical interventions. J. Math. Industry. 2020;10(1) doi: 10.1186/s13362-020-00091-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mondal Chittaranjan, Adak Debadatta, Majumder Abhijit, Bairagi Nandadulal. Mitigating the transmission of infection and death due to SARS-CoV-2 through non-pharmaceutical interventions and repurposing drugs. ISA Trans. 2020 doi: 10.1016/j.isatra.2020.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mandal Manotosh, Jana Soovoojeet, Nandi Swapan Kumar, Khatua Anupam, Adak Sayani, Kar T.K. A model based study on the dynamics of COVID-19: Prediction and control. Chaos Solitons Fractals. 2020;136 doi: 10.1016/j.chaos.2020.109889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Aldila Dipo. Analyzing the impact of the media campaign and rapid testing for COVID-19 as an optimal control problem in East Java, Indonesia. Chaos Solitons Fractals. 2020;141 doi: 10.1016/j.chaos.2020.110364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Náraigh Lennon Ó., Byrne Áine. Piecewise-constant optimal control strategies for controlling the outbreak of COVID-19 in the Irish population. Math. Biosci. 2020;330 doi: 10.1016/j.mbs.2020.108496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Acuña-Zegarra Manuel Adrian, Santana-Cibrian Mario, Velasco-Hernandez Jorge X. Modeling behavioral change and COVID-19 containment in Mexico: A trade-off between lockdown and compliance. Math. Biosci. 2020;325 doi: 10.1016/j.mbs.2020.108370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ullah Saif, Khan Muhammad Altaf. Modeling the impact of non-pharmaceutical interventions on the dynamics of novel coronavirus with optimal control analysis with a case study. Chaos Solitons Fractals. 2020;139 doi: 10.1016/j.chaos.2020.110075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kim Soyoung, Seo Yu Bin, Jung Eunok. Prediction of COVID-19 transmission dynamics using a mathematical model considering behavior changes. Epidemiol Health. 2020 doi: 10.4178/epih.e2020026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kim Soyoung, Ko Youngsuk, Kim Yae-Jean, Jung Eunok. The impact of social distancing and public behavior changes on COVIDCOVID-19 transmission dynamics in the Republic of Korea. PLoS ONE. 2020;15(9) doi: 10.1371/journal.pone.0238684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Lemaitre Joseph C., Perez-Saez Javier, Azman Andrew S., Rinaldo Andrea, Fellay Jacques. Assessing the impact of non-pharmaceutical interventions on SARS-CoV-2 transmission in Switzerland. Swiss Med. Wkly. 2020 doi: 10.4414/smw.2020.20295. [DOI] [PubMed] [Google Scholar]
- 82.Li Tom, Liu Yan, Li Man, Qian Xiaoning, Dai Susie Y. Mask or no mask for COVID-19: A public health and market study. PLoS ONE. 2020;15(8) doi: 10.1371/journal.pone.0237691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kain Morgan P., Childs Marissa L., Becker Alexander D., Mordecai Erin A. Chopping the tail: how preventing superspreading can help to maintain COVID-19 control. medRxiv. 2020 doi: 10.1016/j.epidem.2020.100430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Childs Marissa L., Kain Morgan P., Kirk Devin, Harris Mallory, Couper Lisa, Nova Nicole, Delwel Isabel, Ritchie Jacob, Mordecai Erin A. The impact of long-term non-pharmaceutical interventions on COVID-19 epidemic dynamics and control. medRxiv. 2020 doi: 10.1098/rspb.2021.0811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Reiner Robert C., Barber Ryan M., Collins James K., Zheng Peng, Adolph Christopher, Albright James, Antony Catherine M., Aravkin Aleksandr Y., Bachmeier Steven D., Bang-Jensen Bree, et al. Modeling COVID-19 scenarios for the United States. Nat. Med. 2020 doi: 10.1038/s41591-020-1132-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ngonghala Calistus N., Iboi Enahoro, Eikenberry Steffen, Scotch Matthew, MacIntyre Chandini Raina, Bonds Matthew H., Gumel Abba B. Mathematical assessment of the impact of non-pharmaceutical interventions on curtailing the 2019 novel coronavirus. Math. Biosci. 2020;325 doi: 10.1016/j.mbs.2020.108364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Eikenberry Steffen E., Mancuso Marina, Iboi Enahoro, Phan Tin, Eikenberry Keenan, Kuang Yang, Kostelich Eric, Gumel Abba B. To mask or not to mask: Modeling the potential for face mask use by the general public to curtail the COVID-19 pandemic. Infect. Dis. Model. 2020;5:293–308. doi: 10.1016/j.idm.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Perkins T. Alex, España Guido. Optimal control of the COVID-19 pandemic with non-pharmaceutical interventions. Bull. Math. Biol. 2020;82(9) doi: 10.1007/s11538-020-00795-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Iboi Enahoro A., Ngonghala Calistus N., Gumel Abba B. Will an imperfect vaccine curtail the COVID-19 pandemic in the U.S.? Infect. Dis. Model. 2020;5:510–524. doi: 10.1016/j.idm.2020.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Weitz Joshua S., Park Sang Woo, Eksin Ceyhun, Dushoff Jonathan. Awareness-driven behavior changes can shift the shape of epidemics away from peaks and toward plateaus, shoulders, and oscillations. Proc. Natl. Acad. Sci. USA. 2020 doi: 10.1073/pnas.2009911117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Stutt Richard O.J.H., Retkute Renata, Bradley Michael, Gilligan Christopher A., Colvin John. A modelling framework to assess the likely effectiveness of facemasks in combination with ‘lock-down’ in managing the COVID-19 pandemic. Proc. R. Soc. A. 2020;476(2238) doi: 10.1098/rspa.2020.0376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Zamir Muhmmad, Shah Zahir, Nadeem Fawad, Memood Arif, Alrabaiah Hussam, Kumam Poom. Non pharmaceutical interventions for optimal control of COVID-19. Comput. Methods Programs Biomed. 2020;196 doi: 10.1016/j.cmpb.2020.105642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Davies Nicholas G., Kucharski Adam J., Eggo Rosalind M., Gimma Amy, Edmunds W. John, Jombart Thibaut, Reilly Kathleen O., Endo Akira, Hellewell Joel, Nightingale Emily S., Quilty Billy J., Jarvis Christopher I., Russell Timothy W., Klepac Petra, Bosse Nikos I., Funk Sebastian, Abbott Sam, Medley Graham F., Gibbs Hamish, Pearson Carl A.B., Flasche Stefan, Jit Mark, Clifford Samuel, Prem Kiesha, Diamond Charlie, Emery Jon, Deol Arminder K., Procter Simon R., van Zandvoort Kevin, Sun Yueqian Fiona, Munday James D., Rosello Alicia, Auzenbergs Megan, Knight Gwen, Houben Rein M.G.J., Liu Yang. Effects of non-pharmaceutical interventions on COVID-19 cases, deaths, and demand for hospital services in the UK: a modelling study. Lancet Public Health. 2020;5(7):e375–e385. doi: 10.1016/S2468-2667(20)30133-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Brett Tobias S., Rohani Pejman. Transmission dynamics reveal the impracticality of COVID-19 herd immunity strategies. Proc. Natl. Acad. Sci. USA. 2020;117(41):25897–25903. doi: 10.1073/pnas.2008087117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Goscé Lara, Phillips Professor Andrew, Spinola P., Gupta Dr Rishi K., Abubakar Professor Ibrahim. Modelling SARS-COV2 spread in London: Approaches to lift the lockdown. J. Infect. 2020;81(2):260–265. doi: 10.1016/j.jinf.2020.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Domenico Laura Di, Pullano Giulia, Sabbatini Chiara E., Boëlle Pierre-Yves, Colizza Vittoria. Impact of lockdown on COVID-19 epidemic in Île-de-France and possible exit strategies. BMC Med. 2020;18(1) doi: 10.1186/s12916-020-01698-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Salje Henrik, Kiem Cécile Tran, Lefrancq Noémie, Courtejoie Noémie, Bosetti Paolo, Paireau Juliette, Andronico Alessio, Hozé Nathanaël, Richet Jehanne, Dubost Claire-Lise, Strat Yann Le, Lessler Justin, Levy-Bruhl Daniel, Fontanet Arnaud, Opatowski Lulla, Boelle Pierre-Yves, Cauchemez Simon. Estimating the burden of SARS-CoV-2 in France. Science. 2020;369(6500):208–211. doi: 10.1126/science.abc3517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Barbarossa Maria Vittoria, Fuhrmann Jan, Meinke Jan H., Krieg Stefan, Varma Hridya Vinod, Castelletti Noemi, Lippert Thomas. Modeling the spread of COVID-19 in Germany: Early assessment and possible scenarios. PLoS ONE. 2020;15(9) doi: 10.1371/journal.pone.0238559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Evans Michelle V., Garchitorena Andres, Rakotonanahary Rado J.L., Drake John M., Andriamihaja Benjamin, Rajaonarifara Elinambinina, Ngonghala Calistus N., Roche Benjamin, Bonds Matthew H., Rakotonirina Julio. Reconciling model predictions with low reported cases of COVID-19 in Sub-Saharan Africa: insights from Madagascar. Glob. Health Action. 2020;13(1) doi: 10.1080/16549716.2020.1816044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.van Zandvoort Kevin, Jarvis Christopher I., Pearson Carl A.B., Davies Nicholas G., Ratnayake Ruwan, Russell Timothy W., Kucharski Adam J., Jit Mark, Flasche Stefan, Eggo Rosalind M., Checchi Francesco. Response strategies for COVID-19 epidemics in african settings: a mathematical modelling study. BMC Med. 2020;18(1) doi: 10.1186/s12916-020-01789-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Min Kyung-Duk, Kang Heewon, Lee Ju-Yeun, Jeon Seonghee, il Cho Sung. Estimating the effectiveness of non-pharmaceutical interventions on COVID-19 control in Korea. J. Korean Med. Sci. 2020;35(35) doi: 10.3346/jkms.2020.35.e321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Burns Adam A.C., Gutfraind Alexander. Effectiveness of isolation policies in schools: Evidence from a mathematical model of influenza and COVID-19. medRxiv. 2020 doi: 10.7717/peerj.11211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Matrajt Laura, Leung Tiffany. Evaluating the effectiveness of social distancing interventions to delay or flatten the epidemic curve of coronavirus disease. Emerg. Infect. Diseases. 2020;26(8):1740–1748. doi: 10.3201/eid2608.201093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Britton Tom, Ball Frank, Trapman Pieter. A mathematical model reveals the influence of population heterogeneity on herd immunity to SARS-CoV-2. Science. 2020;369(6505):846–849. doi: 10.1126/science.abc6810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Hoffman Benjamin U. Significant relaxation of SARS-CoV-2-targeted non-pharmaceutical interventions may result in profound mortality: A new york state modelling study. PLoS ONE. 2020;15(9) doi: 10.1371/journal.pone.0239647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Karatayev Vadim A., Anand Madhur, Bauch Chris T. Local lockdowns outperform global lockdown on the far side of the COVID-19 epidemic curve. Proc. Natl. Acad. Sci. USA. 2020;117(39):24575–24580. doi: 10.1073/pnas.2014385117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Rader Benjamin, Scarpino Samuel V., Nande Anjalika, Hill Alison L., Adlam Ben, Reiner Robert C., Pigott David M., Gutierrez Bernardo, Zarebski Alexander E., Shrestha Munik, Brownstein John S., Castro Marcia C., Dye Christopher, Tian Huaiyu, Pybus Oliver G., Kraemer Moritz U.G. Crowding and the shape of COVID-19 epidemics. Nat. Med. 2020 doi: 10.1038/s41591-020-1104-0. [DOI] [PubMed] [Google Scholar]
- 108.Lai Shengjie, Ruktanonchai Nick W., Zhou Liangcai, Prosper Olivia, Luo Wei, Floyd Jessica R., Wesolowski Amy, Santillana Mauricio, Zhang Chi, Du Xiangjun, Yu Hongjie, Tatem Andrew J. Effect of non-pharmaceutical interventions to contain COVID-19 in China. Nature. 2020;585(7825):410–413. doi: 10.1038/s41586-020-2293-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ge Jing, He Daihai, Lin Zhigui, Zhu Huaiping, Zhuang Zian. Four-tier response system and spatial propagation of COVID-19 in China by a network model. Math. Biosci. 2020;330 doi: 10.1016/j.mbs.2020.108484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Aleta Alberto, Hu Qitong, Ye Jiachen, Ji Peng, Moreno Yamir. A data-driven assessment of early travel restrictions related to the spreading of the novel COVID-19 within mainland China. Chaos Solitons Fractals. 2020;139 doi: 10.1016/j.chaos.2020.110068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Medrek M., Pastuszak Z. Numerical simulation of the novel coronavirus spreading. Expert Syst. Appl. 2021;166 doi: 10.1016/j.eswa.2020.114109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Aleta Alberto, Moreno Yamir. Evaluation of the potential incidence of COVID-19 and effectiveness of containment measures in Spain: a data-driven approach. BMC Med. 2020;18:1–12. doi: 10.1186/s12916-020-01619-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Kheirallah Khalid A., Alsinglawi Belal, Alzoubi Abdallah, Saidan Motasem N., Mubin Omar, Alorjani Mohammed S., Mzayek Fawaz. The effect of strict state measures on the epidemiologic curve of COVID-19 infection in the context of a developing country: A simulation from Jordan. IJERPH. 2020;17(18):6530. doi: 10.3390/ijerph17186530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Bertuzzo Enrico, Mari Lorenzo, Pasetto Damiano, Miccoli Stefano, Casagrandi Renato, Gatto Marino, Rinaldo Andrea. The geography of COVID-19 spread in Italy and implications for the relaxation of confinement measures. Nature Commun. 2020;11(1) doi: 10.1038/s41467-020-18050-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Carli Raffaele, Cavone Graziana, Epicoco Nicola, Scarabaggio Paolo, Dotoli Mariagrazia. Model predictive control to mitigate the COVID-19 outbreak in a multi-region scenario. Annu. Rev. Control. 2020 doi: 10.1016/j.arcontrol.2020.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Pei Sen, Kandula Sasikiran, Shaman Jeffrey. Differential effects of intervention timing on COVID-19 spread in the United States. medRxiv. 2020 doi: 10.1126/sciadv.abd6370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Chang Serina, Pierson Emma, Koh Pang Wei, Gerardin Jaline, Redbird Beth, Grusky David, Leskovec Jure. Mobility network models of COVID-19 explain inequities and inform reopening. Nature. 2020 doi: 10.1038/s41586-020-2923-3. [DOI] [PubMed] [Google Scholar]
- 118.Ruktanonchai N.W., Floyd J.R., Lai S., Ruktanonchai C.W., Sadilek A., Rente-Lourenco P., Ben X., Carioli A., Gwinn J., Steele J.E., Prosper O., Schneider A., Oplinger A., Eastham P., Tatem A.J. Assessing the impact of coordinated COVID-19 exit strategies across europe. Science. 2020;369(6510):1465–1470. doi: 10.1126/science.abc5096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Gozzi Nicolò, Tizzoni Michele, Chinazzi Matteo, Ferres Leo, Vespignani Alessandro, Perra Nicola. Estimating the effect of social inequalities in the mitigation of COVID-19 across communities in Santiago de Chile. medRxiv. 2020 doi: 10.1038/s41467-021-22601-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Röst Gergely, Bartha Ferenc A., Bogya Norbert, Boldog Péter, Dénes Attila, Ferenci Tamás, Horváth Krisztina J., Juhász Attila, Nagy Csilla, Tekeli Tamás, Vizi Zsolt, Oroszi Beatrix. Early phase of the COVID-19 outbreak in Hungary and post-lockdown scenarios. Viruses. 2020;12(7):708. doi: 10.3390/v12070708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Arenas Alex, Cota Wesley, Gómez-Gardeñes Jesús, Gómez Sergio, Granell Clara, Matamalas Joan T., Soriano-Paños David, Steinegger Benjamin. Modeling the spatiotemporal epidemic spreading of COVID-19 and the impact of mobility and social distancing interventions. Phys. Rev. X. 2020;10(4) [Google Scholar]
- 122.Sjödin Henrik, Johansson Anders F., Brännström Ake, Farooq Zia, Kriit Hedi Katre, Wilder-Smith Annelies, Åström Christofer, Thunberg Johan, Söderquist Mårten, Rocklöv Joacim. COVID-19 healthcare demand and mortality in Sweden in response to non-pharmaceutical mitigation and suppression scenarios. Int. J. Epidemiol. 2020 doi: 10.1093/ije/dyaa121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Lau Max S.Y., Grenfell Bryan, Thomas Michael, Bryan Michael, Nelson Kristin, Lopman Ben. Characterizing superspreading events and age-specific infectiousness of SARS-CoV-2 transmission in Georgia, USA. Proc. Natl. Acad. Sci. USA. 2020;117(36):22430–22435. doi: 10.1073/pnas.2011802117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Bryant Patrick, Elofsson Arne. Estimating the impact of mobility patterns on COVID-19 infection rates in 11 European countries. PeerJ. 2020;8 doi: 10.7717/peerj.9879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Candido Darlan S., Claro Ingra M., de Jesus Jaqueline G., Souza William M., Moreira Filipe R.R., Dellicour Simon, Mellan Thomas A., du Plessis Louis, Pereira Rafael H.M., Sales Flavia C.S., Manuli Erika R., Thézé Julien, Almeida Luiz, Menezes Mariane T., Voloch Carolina M., Fumagalli Marcilio J., Coletti Thaís M., da Silva Camila A.M., Ramundo Mariana S., Amorim Mariene R., Hoeltgebaum Henrique H., Mishra Swapnil, Gill Mandev S., Carvalho Luiz M., Buss Lewis F., Prete Carlos A., Ashworth Jordan, Nakaya Helder I., Peixoto Pedro S., Brady Oliver J., Nicholls Samuel M., Tanuri Amilcar, Rossi Átila D., Braga Carlos K.V., Gerber Alexandra L., de C. Guimarães Ana Paula, Gaburo Nelson, Alencar Cecila Salete, Ferreira Alessandro C.S., Lima Cristiano X., Levi José Eduardo, Granato Celso, Ferreira Giulia M., Francisco Ronaldo S., Granja Fabiana, Garcia Marcia T., Moretti Maria Luiza, Perroud Mauricio W., Castiñeiras Terezinha M.P.P., Lazari Carolina S., Hill Sarah C., de Souza Santos Andreza Aruska, Simeoni Camila L., Forato Julia, Sposito Andrei C., Schreiber Angelica Z., Santos Magnun N.N., de Sá Camila Zolini, Souza Renan P., Resende-Moreira Luciana C., Teixeira Mauro M., Hubner Josy, Leme Patricia A.F., Moreira Rennan G., Nogueira Maurício L., Ferguson Neil M., Costa Silvia F., Proenca-Modena José Luiz, Vasconcelos Ana Tereza R., Bhatt Samir, Lemey Philippe, Wu Chieh-Hsi, Rambaut Andrew, Loman Nick J., Aguiar Renato S., Pybus Oliver G., Sabino Ester C., Faria Nuno Rodrigues. Evolution and epidemic spread of SARS-CoV-2 in Brazil. Science. 2020;369(6508):1255–1260. doi: 10.1126/science.abd2161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Leung Kathy, Wu Joseph T., Liu Di, Leung Gabriel M. First-wave COVID-19 transmissibility and severity in China outside hubei after control measures, and second-wave scenario planning: a modelling impact assessment. Lancet. 2020;395(10233):1382–1393. doi: 10.1016/S0140-6736(20)30746-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Quilty Billy J., Diamond Charlie, Liu Yang, Gibbs Hamish, Russell Timothy W., Jarvis Christopher I., Prem Kiesha, Pearson Carl A.B., Clifford Samuel, Flasche Stefan, Klepac Petra, Eggo Rosalind M., Jit Mark. The effect of travel restrictions on the geographical spread of COVID-19 between large cities in China: a modelling study. BMC Med. 2020;18(1) doi: 10.1186/s12916-020-01712-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Zheng Zhong, Wu Ke, Yao Zhixian, Zheng Xinyi, Zheng Junhua, Chen Jian. The prediction for development of COVID-19 in global major epidemic areas through empirical trends in China by utilizing state transition matrix model. BMC Infect. Dis. 2020;20(1) doi: 10.1186/s12879-020-05417-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Cowling Benjamin J., Ali Sheikh Taslim, Ng Tiffany W.Y., Tsang Tim K., Li Julian C.M., Fong Min Whui, Liao Qiuyan, Kwan Mike Y.W., Lee So Lun, Chiu Susan S., Wu Joseph T., Wu Peng, Leung Gabriel M. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. Lancet Public Health. 2020;5(5):e279–e288. doi: 10.1016/S2468-2667(20)30090-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Basu Deepankar, Salvatore Maxwell, Ray Debashree, Kleinsasser Michael, Purkayastha Soumik, Bhattacharyya Rupam, Mukherjee Bhramar. A comprehensive public health evaluation of lockdown as a non-pharmaceutical intervention on COVID-19 spread in India: National trends masking state level variations. medRxiv. 2020 doi: 10.1136/bmjopen-2020-041778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Wahaibi Adil Al, Manji Abdullah Al, Maani Amal Al, Rawahi Bader Al, Harthy Khalid Al, Alyaquobi Fatma, Al-Jardani Amina, Petersen Eskild, Abri Seif Al. COVID-19 epidemic monitoring after non-pharmaceutical interventions: The use of time-varying reproduction number in a country with a large migrant population. Int. J. Infect. Dis. 2020;99:466–472. doi: 10.1016/j.ijid.2020.08.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Manevski Damjan, Gorenjec Nina Ružić, Kejžar Nataša, Blagus Rok. Modeling COVID-19 pandemic using Bayesian analysis with application to slovene data. Math. Biosci. 2020;329 doi: 10.1016/j.mbs.2020.108466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Morley Christopher P., Anderson Kathryn B., Shaw Jana, Stewart Telisa, Thomas Stephen J., Wang Dongliang. Social distancing metrics and estimates of SARS-CoV-2 transmission rates: Associations between mobile telephone data tracking and r. J. Public Health Manag. Pract. 2020;26(6):606–612. doi: 10.1097/PHH.0000000000001240. [DOI] [PubMed] [Google Scholar]
- 134.Brauner Jan M., Mindermann Sören, Sharma Mrinank, Johnston David, Salvatier John, Gavenčiak Tomáš, Stephenson Anna B., Leech Gavin, Altman George, Mikulik Vladimir, Norman Alexander John, Monrad Joshua Teperowski, Besiroglu Tamay, Ge Hong, Hartwick Meghan A., Teh Yee Whye, Chindelevitch Leonid, Gal Yarin, Kulveit Jan. Inferring the effectiveness of government interventions against COVID-19. Science. 2020 doi: 10.1126/science.abd9338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Wilder Bryan, Charpignon Marie, Killian Jackson A., Ou Han-Ching, Mate Aditya, Jabbari Shahin, Perrault Andrew, Desai Angel N., Tambe Milind, Majumder Maimuna S. Modeling between-population variation in COVID-19 dynamics in Hubei, Lombardy, and New York City. Proc. Natl. Acad. Sci. USA. 2020;117(41):25904–25910. doi: 10.1073/pnas.2010651117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Bouchnita Anass, Jebrane Aissam. A hybrid multi-scale model of COVID-19 transmission dynamics to assess the potential of non-pharmaceutical interventions. Chaos Solitons Fractals. 2020;138 doi: 10.1016/j.chaos.2020.109941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Aleta Alberto, Martín-Corral David, y Piontti Ana Pastore, Ajelli Marco, Litvinova Maria, Chinazzi Matteo, Dean Natalie E., Halloran M. Elizabeth, Jr Ira M. Longini, Merler Stefano, Pentland Alex, Vespignani Alessandro, Moro Esteban, Moreno Yamir. Modelling the impact of testing, contact tracing and household quarantine on second waves of COVID-19. Nat. Hum. Behav. 2020;4(9):964–971. doi: 10.1038/s41562-020-0931-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Aleta Alberto, Martín-Corral David, Bakker Michiel A., Piontti Ana Pastore y, Ajelli Marco, Litvinova Maria, Chinazzi Matteo, Dean Natalie E., Halloran M. Elizabeth, Longini Ira M., Pentland Alex, Vespignani Alessandro, Moreno Yamir, Moro Esteban. Quantifying the importance and location of SARS-CoV-2 transmission events in large metropolitan areas. medRxiv. 2020 doi: 10.1073/pnas.2112182119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Kwon Okyu, Son Woo-Sik, Kim Jin Yong, Kim Jong-Hun. Intervention effects in the transmission of COVID-19 depending on the detection rate and extent of isolation. Epidemiol Health. 2020 doi: 10.4178/epih.e2020045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Silva Petrônio C.L., Batista Paulo V.C., Lima Hélder S., Alves Marcos A., Guimarães Frederico G., Silva Rodrigo C.P. COVID-ABS: An agent-based model of COVID-19 epidemic to simulate health and economic effects of social distancing interventions. Chaos Solitons Fractals. 2020;139 doi: 10.1016/j.chaos.2020.110088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Blackwood Julie C., Childs Lauren M. An introduction to compartmental modeling for the budding infectious disease modeler. Lett. Biomath. 2018;5(1):195–221. [Google Scholar]
- 142.Verity Robert, Okell Lucy C., Dorigatti Ilaria, Winskill Peter, Whittaker Charles, Imai Natsuko, Cuomo-Dannenburg Gina, Thompson Hayley, Walker Patrick G.T., Fu Han, et al. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect. Dis. 2020 doi: 10.1016/S1473-3099(20)30243-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Barrat Alain, Barthelemy Marc, Vespignani Alessandro. Cambridge university press; 2008. Dynamical Processes on Complex Networks. [Google Scholar]
- 144.Barabási Albert-László, et al. Cambridge university press; 2016. Network Science. [Google Scholar]
- 145.Perra Nicola, Balcan Duygu, Gonçalves Bruno, Vespignani Alessandro. Towards a characterization of behavior-disease models. PLoS One. 2011;6(8) doi: 10.1371/journal.pone.0023084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Colizza Vittoria, Vespignani Alessandro. Epidemic modeling in metapopulation systems with heterogeneous coupling pattern: Theory and simulations. J. Theoret. Biol. 2008;251(3):450–467. doi: 10.1016/j.jtbi.2007.11.028. [DOI] [PubMed] [Google Scholar]
- 147.Tagliazucchi E., Balenzuela P., Travizano M., Mindlin G.B., Mininni P.D. Lessons from being challenged by COVID-19. Chaos Solitons Fractals. 2020;137 doi: 10.1016/j.chaos.2020.109923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Balcan Duygu, Gonçalves Bruno, Hu Hao, Ramasco José J., Colizza Vittoria, Vespignani Alessandro. Modeling the spatial spread of infectious diseases: The global epidemic and mobility computational model. J. Comput. Sci. 2010;1(3):132–145. doi: 10.1016/j.jocs.2010.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Balcan Duygu, Hu Hao, GonΩ CÇcalves Bruno, Bajardi Paolo, Poletto Chiara, Ramasco Jose Javier, Paolotti Daniela, Perra Nicola, Tizzoni Michele, Van den Broeck Wouter, Colizza Vittoria, Vespignani Alessandro. Seasonal transmission potential and activity peaks of the new influenza a(h1n1): A Monte Carlo likelihood analysis based on human mobility. BMC Med. 2009;7:45. doi: 10.1186/1741-7015-7-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.y Piontti Ana Pastore, Perra Nicola, Rossi Luca, Samay Nicole, Vespignani Alessandro. Springer; 2018. Charting the Next Pandemic: Modeling Infectious Disease Spreading in the Data Science Age. [Google Scholar]
- 151.Balcan Duygu, Colizza Vittoria, Goncalves Bruno, Hu Hao, Ramasco José J., Vespignani Alessandro. Multiscale mobility networks and the spatial spreading of infectious diseases. Proc. Natl. Acad. Sci. 2009;106(51):21484–21489. doi: 10.1073/pnas.0906910106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Socioeconomic Data and Applications Center (SEDAC), Columbia University http://sedac.ciesin.columbia.edu/gpw.
- 153.Mistry Dina, Litvinova Maria, Chinazzi Matteo, Fumanelli Laura, Gomes Marcelo F.C., Haque Syed A., Liu Quan-Hui, Mu Kunpeng, Xiong Xinyue, Halloran M. Elizabeth, et al. 2020. Inferring high-resolution human mixing patterns for disease modeling. arXiv preprint arXiv:2003.01214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Simini Filippo, González Marta C., Maritan Amos, Barabási Albert-László. A universal model for mobility and migration patterns. Nature. 2012;484(7392):96–100. doi: 10.1038/nature10856. [DOI] [PubMed] [Google Scholar]
- 155.Cori Anne, Ferguson Neil M., Fraser Christophe, Cauchemez Simon. A new framework and software to estimate time-varying reproduction numbers during epidemics. Am. J. Epidemiol. 2013;178(9):1505–1512. doi: 10.1093/aje/kwt133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Thompson R.N., Stockwin J.E., van Gaalen Rolina D., Polonsky J.A., Kamvar Z.N., Demarsh P.A., Dahlqwist Elisabeth, Li Siyang, Miguel Eve, Jombart Thibaut, et al. Improved inference of time-varying reproduction numbers during infectious disease outbreaks. Epidemics. 2019;29 doi: 10.1016/j.epidem.2019.100356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Hoertel Nicolas, Blachier Martin, Blanco Carlos, Olfson Mark, Massetti Marc, Rico Marina Sánchez, Limosin Frédéric, Leleu Henri. A stochastic agent-based model of the SARS-CoV-2 epidemic in France. Nat. Med. 2020;26(9):1417–1421. doi: 10.1038/s41591-020-1001-6. [DOI] [PubMed] [Google Scholar]
- 158.Tintori A., Cerbara L., Ciancimino G., Crescimbene M., La Longa F., Versari A. Adaptive behavioural coping strategies as reaction to COVID-19 social distancing in Italy. Eur. Rev. Med. Pharmacol. Sci. 2020;24(20):10860–10866. doi: 10.26355/eurrev_202010_23449. [DOI] [PubMed] [Google Scholar]
- 159.Alzueta Elisabet, Perrin Paul, Baker Fiona C., Caffarra Sendy, Ramos-Usuga Daniela, Yuksel Dilara, Arango-Lasprilla Juan Carlos. How the COVID-19 pandemic has changed our lives: A study of psychological correlates across 59 countries. J. Clin. Psychol. 2020 doi: 10.1002/jclp.23082. [DOI] [PubMed] [Google Scholar]
- 160.Islam Md. Saiful, Ferdous Most Zannatul, Potenza Marc N. Panic and generalized anxiety during the COVID-19 pandemic among Bangladeshi people: An online pilot survey early in the outbreak. J. Affect. Disord. 2020;276:30–37. doi: 10.1016/j.jad.2020.06.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Cai Qi, Feng Hongliang, Huang Jing, Wang Meiyao, Wang Qunfeng, Lu Xuanzhen, Xie Yu, Wang Xing, Liu Zhenxing, Hou Botong, Ouyang Keni, Pan Jing, Li Qin, Fu Beibei, Deng Yongchao, Liu Yumin. The mental health of frontline and non-frontline medical workers during the coronavirus disease 2019 (COVID-19) outbreak in China: A case-control study. J. Affect. Disord. 2020;275:210–215. doi: 10.1016/j.jad.2020.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Liu Qi, Zhou Yu, Xie Xinyan, Xue Qi, Zhu Kaiheng, Wan Zihao, Wu Hao, Zhang Jiajia, Song Ranran. The prevalence of behavioral problems among school-aged children in home quarantine during the COVID-19 pandemic in China. J. Affect. Disord. 2021;279:412–416. doi: 10.1016/j.jad.2020.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Sutin Angelina R., Luchetti Martina, Aschwanden Damaris, Lee Ji Hyun, Sesker Amanda A., Strickhouser Jason E., Stephan Yannick, Terracciano Antonio. Change in five-factor model personality traits during the acute phase of the coronavirus pandemic. PLoS ONE. 2020;15(8) doi: 10.1371/journal.pone.0237056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Luchetti Martina, Lee Ji Hyun, Aschwanden Damaris, Sesker Amanda, Strickhouser Jason E., Terracciano Antonio, Sutin Angelina R. The trajectory of loneliness in response to COVID-19. Am. Psychol. 2020;75(7):897–908. doi: 10.1037/amp0000690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Patrick Stephen W., Henkhaus Laura E., Zickafoose Joseph S., Lovell Kim, Halvorson Alese, Loch Sarah, Letterie Mia, Davis Matthew M. Well-being of parents and children during the COVID-19 pandemic: A national survey. Pediatrics. 2020;146(4) doi: 10.1542/peds.2020-016824. [DOI] [PubMed] [Google Scholar]
- 166.Sadiković Selka, Branovački Bojan, Oljača Milan, Mitrović Dušanka, Pajić Dejan, Smederevac Snežana. Daily monitoring of emotional responses to the coronavirus pandemic in Serbia: A citizen science approach. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.02133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Trougakos John P., Chawla Nitya, McCarthy Julie M. Working in a pandemic: Exploring the impact of COVID-19 health anxiety on work, family, and health outcomes. J. Appl. Psychol. 2020;105(11):1234–1245. doi: 10.1037/apl0000739. [DOI] [PubMed] [Google Scholar]
- 168.Song Lili, Wang Yong, Li ZhengLin, Yang Ying, Li Hao. Mental health and work attitudes among people resuming work during the COVID-19 pandemic: A cross-sectional study in China. IJERPH. 2020;17(14):5059. doi: 10.3390/ijerph17145059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Asiamah Nestor, Opuni Frank Frimpong, Mends-Brew Edwin, Mensah Samuel Worlanyo, Mensah Henry Kofi, Quansah Fidelis. Short-term changes in behaviors resulting from COVID-19-related social isolation and their influences on mental health in ghana. Community Ment. Health J. 2020 doi: 10.1007/s10597-020-00722-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Abuhammad Sawsan. Violence against Jordanian Women during COVID-19 outbreak. Int. J. Clin. Pract. 2020 doi: 10.1111/ijcp.13824. [DOI] [PubMed] [Google Scholar]
- 171.Mazza Cristina, Ricci Eleonora, Marchetti Daniela, Fontanesi Lilybeth, Giandomenico Serena Di, Verrocchio Maria Cristina, Roma Paolo. How personality relates to distress in parents during the Covid-19 lockdown: The mediating role of child’s emotional and behavioral difficulties and the moderating effect of living with other people. IJERPH. 2020;17(17):6236. doi: 10.3390/ijerph17176236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Emerson Kerstin Gerst. Coping with being cooped up: Social distancing during COVID-19 among 60+ in the United States. Revis. Panam. de Salud Publica. 2020;44:1. doi: 10.26633/RPSP.2020.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Copeland William E., McGinnis Ellen, Bai Yang, Adams Zoe, Nardone Hilary, Devadanam Vinay, Rettew Jeffrey, Hudziak Jim J. Impact of COVID on college student mental health and wellness. J. Am. Acad Child Adolesc. Psychiatry. 2020 doi: 10.1016/j.jaac.2020.08.466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Lee Christine M., Cadigan Jennifer M., Rhew Isaac C. Increases in loneliness among Young adults during the COVID-19 pandemic and association with increases in mental health problems. J. Adolesc. Health. 2020;67(5):714–717. doi: 10.1016/j.jadohealth.2020.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Huckins Jeremy F., DaSilva Alex W., Wang Weichen, Hedlund Elin, Rogers Courtney, Nepal Subigya K., Wu Jialing, Obuchi Mikio, Murphy Eilis I., Meyer Meghan L., Wagner Dylan D., Holtzheimer Paul E., Campbell Andrew T. Mental health and behavior during the early phases of the COVID-19 pandemic: A longitudinal mobile smartphone and ecological momentary assessment study in college students (preprint) J. Med. Internet Res. 2020 doi: 10.2196/20185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.van de Groep Suzanne, Zanolie Kiki, Green Kayla H., Sweijen Sophie W., Crone Eveline A. A daily diary study on adolescents’ mood, empathy, and prosocial behavior during the COVID-19 pandemic. PLoS ONE. 2020;15(10) doi: 10.1371/journal.pone.0240349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Liu Zhijun, Tang Hui, Jin Qiyun, Wang Guanghai, Yang Zixin, Chen Hongyan, Yan Hongxia, Rao Wenjie, Owens Judith. Sleep of preschoolers during the coronavirus disease 2019 (COVID-19) outbreak. J. Sleep Res. 2020 doi: 10.1111/jsr.13142. [DOI] [PubMed] [Google Scholar]
- 178.Balanzá-Martínez Vicent, Kapczinski Flavio, de Azevedo Cardoso Taiane, Atienza-Carbonell Beatriz, Rosa Adriane R., Mota Jurema C., Boni Raquel B. De. The assessment of lifestyle changes during the COVID-19 pandemic using a multidimensional scale. Revista de Psiquiatría y Salud Mental. 2020 doi: 10.1016/j.rpsm.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Rogers Nina Trivedy, Waterlow Naomi R., Brindle Hannah, Enria Luisa, Eggo Rosalind M., Lees Shelley, h. Roberts Chrissy. Behavioral change towards reduced intensity physical activity is disproportionately prevalent among adults with serious health issues or self-perception of high risk during the UK COVID-19 lockdown. Front. Public Health. 2020;8 doi: 10.3389/fpubh.2020.575091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Bourassa Kyle J., Sbarra David A., Caspi Avshalom, Moffitt Terrie E. Social distancing as a health behavior: County-level movement in the United States during the COVID-19 pandemic is associated with conventional health behaviors. Ann. Behav. Med. 2020;54(8):548–556. doi: 10.1093/abm/kaaa049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Knell Gregory, Robertson Michael C., Dooley Erin E., Burford Katie, Mendez Karla S. Health behavior changes during COVID-19 pandemic and subsequent stay-at-home orders. IJERPH. 2020;17(17):6268. doi: 10.3390/ijerph17176268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Vidot Denise C., Islam Jessica Y., Camacho-Rivera Marlene, Harrell Melissa B., Rao Devika R., Chavez Jennifer V., Ochoa Lucas G., Hlaing WayWay M., Weiner Michelle, Messiah Sarah E. The COVID-19 cannabis health study: Results from an epidemiologic assessment of adults who use cannabis for medicinal reasons in the united states. J. Addictive Dis. 2020:1–11. doi: 10.1080/10550887.2020.1811455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Hammoud Mohamed A., Maher Lisa, Holt Martin, Degenhardt Louisa, Jin Fengyi, Murphy Dean, Bavinton Benjamin, Grulich Andrew, Lea Toby, Haire Bridget, Bourne Adam, Saxton Peter, Vaccher Stefanie, Ellard Jeanne, Mackie Brent, Batrouney Colin, Bath Nicky, Prestage Garrett. Physical distancing due to COVID-19 disrupts sexual behaviors among gay and bisexual men in Australia: Implications for trends in HIV and other sexually transmissible infections. JAIDS J. Acquir. Immune Defic. Syndr. 2020;85(3):309–315. doi: 10.1097/QAI.0000000000002462. [DOI] [PubMed] [Google Scholar]
- 184.Barbosa Carolina, Cowell Alexander J., Dowd William N. Alcohol consumption in response to the COVID-19 pandemic in the United States. J. Addict. Med. 2020;Publish Ahead of Print doi: 10.1097/ADM.0000000000000767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Medrano María, Cadenas-Sanchez Cristina, Oses Maddi, Arenaza Lide, Amasene Maria, Labayen Idoia. Changes in lifestyle behaviours during the COVID -19 confinement in spanish children: A longitudinal analysis from the MUGI project. Pediatric. Obesity. 2020 doi: 10.1111/ijpo.12731. [DOI] [PubMed] [Google Scholar]
- 186.Romero-Blanco Cristina, Rodríguez-Almagro Julián, Onieva-Zafra María Dolores, Parra-Fernández María Laura, del Carmen Prado-Laguna María, Hernández-Martínez Antonio. Sleep pattern changes in nursing students during the COVID-19 lockdown. IJERPH. 2020;17(14):5222. doi: 10.3390/ijerph17145222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Nelson Kimberly M., Gordon Allegra R., John Steven A., Stout Claire D., Macapagal Katharyn. Physical sex is over for now: Impact of COVID-19 on the well-being and sexual health of adolescent sexual minority males in the U.S. J. Adolesc. Health. 2020;67(6):756–762. doi: 10.1016/j.jadohealth.2020.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Schäfer Sarah K., Sopp M. Roxanne, Schanz Christian G., Staginnus Marlene, Göritz Anja S., Michael Tanja. Impact of COVID-19 on public mental health and the buffering effect of a sense of coherence. Psychother. Psychosom. 2020:1–7. doi: 10.1159/000510752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Musche Venja, Bäuerle Alexander, Steinbach Jasmin, Schweda Adam, Hetkamp Madeleine, Weismüller Benjamin, Kohler Hannah, Beckmann Mingo, Herrmann Ken, Tewes Mitra, Schadendorf Dirk, Skoda Eva-Maria, Teufel Martin. COVID-19-related fear and health-related safety behavior in oncological patients. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.01984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Kishimoto Miyako, Ishikawa Takuya, Odawara Masato. Behavioral changes in patients with diabetes during the COVID-19 pandemic. Diabetol. Int. 2020 doi: 10.1007/s13340-020-00467-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Passanisi Stefano, Pecoraro Maria, Pira Francesco, Alibrandi Angela, Donia Vittoria, Lonia Paola, Pajno Giovanni Battista, Salzano Giuseppina, Lombardo Fortunato. Quarantine due to the COVID-19 pandemic from the perspective of pediatric patients with type 1 diabetes: A web-based survey. Front. Pediatr. 2020;8 doi: 10.3389/fped.2020.00491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Martinotti Giovanni, Alessi Maria Chiara, Natale Chiara Di, Sociali Antonella, Ceci Franca, Lucidi Lorenza, Picutti Elena, Carlo Francesco Di, Corbo Mariangela, Vellante Federica, Fiori Federica, Tourjansky Gaia, Catalano Gabriella, Carenti Maria Luisa, Incerti Chiara Concetta, Bartoletti Luigi, Barlati Stefano, Romeo Vincenzo Maria, Verrastro Valeria, Giorgio Fabio De, Valchera Alessandro, Sepede Gianna, Casella Pietro, Pettorruso Mauro, di Giannantonio Massimo. Psychopathological burden and quality of life in substance users during the COVID-19 lockdown period in Italy. Front. Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.572245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Browne Rodrigo A.V., Macêdo Geovani A.D., Cabral Ludmila L.P., Oliveira Gledson T.A., Vivas Andrés, Fontes Eduardo B., Elsangedy Hassan M., Costa Eduardo C. Initial impact of the COVID-19 pandemic on physical activity and sedentary behavior in hypertensive older adults: An accelerometer-based analysis. Exp. Geront. 2020;142 doi: 10.1016/j.exger.2020.111121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Beukenhorst Anna L., Collins Ella, Burke Katherine M., Rahman Syed Minhajur, Clapp Margaret, Konanki Sai Charan, Paganoni Sabrina, Miller Timothy M., Chan James, Onnela Jukka-Pekka, Berry James D. Smartphone data during the COVID -19 pandemic can quantify behavioral changes in people with ALS. Muscle Nerve. 2020 doi: 10.1002/mus.27110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Galasso Vincenzo, Pons Vincent, Profeta Paola, Becher Michael, Brouard Sylvain, Foucault Martial. Gender differences in COVID-19 attitudes and behavior: Panel evidence from eight countries. Proc. Natl. Acad. Sci. USA. 2020;117(44):27285–27291. doi: 10.1073/pnas.2012520117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Allen William E., Altae-Tran Han, Briggs James, Jin Xin, McGee Glen, Shi Andy, Raghavan Rumya, Kamariza Mireille, Nova Nicole, Pereta Albert, Danford Chris, Kamel Amine, Gothe Patrik, Milam Evrhet, Aurambault Jean, Primke Thorben, Li Weijie, Inkenbrandt Josh, Huynh Tuan, Chen Evan, Lee Christina, Croatto Michael, Bentley Helen, Lu Wendy, Murray Robert, Travassos Mark, Coull Brent A., Openshaw John, Greene Casey S., Shalem Ophir, King Gary, Probasco Ryan, Cheng David R., Silbermann Ben, Zhang Feng, Lin Xihong. Population-scale longitudinal mapping of COVID-19 symptoms, behaviour and testing. Nat. Hum. Behav. 2020;4(9):972–982. doi: 10.1038/s41562-020-00944-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Muto Kaori, Yamamoto Isamu, Nagasu Miwako, Tanaka Mikihito, Wada Koji. Japanese citizens behavioral changes and preparedness against COVID-19: An online survey during the early phase of the pandemic. PLoS ONE. 2020;15(6) doi: 10.1371/journal.pone.0234292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Xu Hong, Gan Yong, Zheng Daikun, Wu Bo, Zhu Xian, Xu Chang, Liu Chenglu, Tao Zhou, Hu Yaoyue, Chen Min, Li Mingjing, Lu Zuxun, Chen Jack. Relationship between COVID-19 infection and risk perception, knowledge, attitude, and four nonpharmaceutical interventions during the late period of the COVID-19 epidemic in China: Online cross-sectional survey of 8158 adults. J. Med. Internet Res. 2020;22(11) doi: 10.2196/21372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Wei Lifeng, Sha Zhuowa, Wang Ying, Zhang Gangyu, Jia Haonan, Zhou Shuang, Li Yuanheng, Wang Yameng, Liu Chao, Jiao Mingli, Sun Shufan, Wu Qunhong. Willingness and beliefs associated with reporting travel history to high-risk coronavirus disease 2019 epidemic regions among the chinese public: a cross-sectional study. BMC Public Health. 2020;20(1) doi: 10.1186/s12889-020-09282-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Lüdecke Daniel, von dem Knesebeck Olaf. Protective behavior in course of the COVID-19 outbreak. Survey results from Germany. Front. Public Health. 2020;8 doi: 10.3389/fpubh.2020.572561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Al-Dmour Hani, Masadeh Raed, Salman Amer, Abuhashesh Mohammad, Al-Dmour Rand. Influence of social media platforms on public health protection against the COVID-19 pandemic via the mediating effects of public health awareness and behavioral changes: Integrated model. J. Med. Internet Res. 2020;22(8) doi: 10.2196/19996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Ashraf Sania, Kuang Jinyi, Das Upasak, Bicchieri Cristina. Sanitation practices during early phases of COVID-19 lockdown in peri-urban communities in Tamil Nadu, India. Am. J. Trop. Med. Hyg. 2020;103(5):2012–2018. doi: 10.4269/ajtmh.20-0830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Kuang Jinyi, Ashraf Sania, Das Upasak, Bicchieri Cristina. Awareness, risk perception, and stress during the COVID-19 pandemic in communities of Tamil Nadu, India. IJERPH. 2020;17(19):7177. doi: 10.3390/ijerph17197177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Tripathi Rina, Alqahtani Saad S., Albarraq Ahmed A., Meraya Abdulkarim M., Tripathi Pankaj, Banji David, Alshahrani Saeed, Ahsan Waquar, Alnakhli Fatimah M. Awareness and preparedness of COVID-19 outbreak among healthcare workers and other residents of south-west Saudi Arabia: A cross-sectional survey. Front. Public Health. 2020;8 doi: 10.3389/fpubh.2020.00482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Lep Žan, Babnik Katarina, Beyazoglu Kaja Hacin. Emotional responses and self-protective behavior within days of the COVID-19 outbreak: The promoting role of information credibility. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.01846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Gray Lesley, MacDonald Carol, Tassell-Matamua Natasha, Stanley James, Kvalsvig Amanda, Zhang Jane, Murton Samantha, Wiles Siouxsie, Puloka Viliami, Becker Julia, Johnston David, Baker Michael G. Wearing one for the team: views and attitudes to face covering in new Zealand/Aotearoa during COVID-19 Alert Level 4 lockdown. J. Prim Health Care. 2020;12(3):199. doi: 10.1071/HC20089. [DOI] [PubMed] [Google Scholar]
- 207.Wang Peng-Wei, Lu Wei-Hsin, Ko Nai-Ying, Chen Yi-Lung, Li Dian-Jeng, Chang Yu-Ping, Yen Cheng-Fang. Covid-19-related information sources and the relationship with confidence in people coping with COVID-19: Facebook survey study in Taiwan. J. Med. Internet Res. 2020;22(6) doi: 10.2196/20021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Kasting Monica L., Head Katharine J., Hartsock Jane A., Sturm Lynne, Zimet Gregory D. Public perceptions of the effectiveness of recommended non-pharmaceutical intervention behaviors to mitigate the spread of SARS-CoV-2. PLoS ONE. 2020;15(11) doi: 10.1371/journal.pone.0241662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Arp Nicholas L., Nguyen Tung H., Linck Emma J. Graham, Feeney Austin K., Schrope Jonathan H., Ruedinger Katrina L., Gao Anqi, Miranda-Katz Margot, Kates Ashley E., Safdar Nasia. Use of face coverings by the public during the COVID-19 pandemic: an observational study. medRxiv. 2020 [Google Scholar]
- 210.Clipman Steven J., Wesolowski Amy P., Gibson Dustin G., Agarwal Smisha, Lambrou Anastasia S., Kirk Gregory D., Labrique Alain B., Mehta Shruti H., Solomon Sunil S. Rapid real-time tracking of nonpharmaceutical interventions and their association with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) positivity: The coronavirus disease 2019 (COVID-19) pandemic pulse study. Clin. Infect. Dis. 2020 doi: 10.1093/cid/ciaa1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Fisher Kiva A., Barile John P., Guerin Rebecca J., Esschert Kayla L. Vanden, Jeffers Alexiss, Tian Lin H., Garcia-Williams Amanda, Gurbaxani Brian, Thompson William W., Prue Christine E. Factors associated with cloth face covering use among adults during the COVID-19 pandemic — United States, april and may 2020. MMWR Morb. Mortal. Wkly. Rep. Morbidity and Mortality Weekly Report. 2020;69(28):933–937. doi: 10.15585/mmwr.mm6928e3. [DOI] [PubMed] [Google Scholar]
- 212.Cvetković Vladimir M., Nikolić Neda, Nenadić Una Radovanović, Öcal Adem, Noji Eric K., Zečević Miodrag. Preparedness and preventive behaviors for a pandemic disaster caused by COVID-19 in Serbia. IJERPH. 2020;17(11):4124. doi: 10.3390/ijerph17114124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Haque Ayesha, Mumtaz Sadaf, Khattak Osama, Mumtaz Rafia, Ahmed Amal. Comparing the preventive behavior of medical students and physicians in the era of COVID-19: Novel medical problems demand novel curricular interventions. Biochem. Mol. Biol. Educ. 2020;48(5):473–481. doi: 10.1002/bmb.21406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.ul Haq Shamsheer, Shahbaz Pomi, Boz Ismet. Knowledge, behavior and precautionary measures related to COVID-19 pandemic among the general public of Punjab province, Pakistan. J. Infect. Dev. Ctries. 2020;14(08):823–835. doi: 10.3855/jidc.12851. [DOI] [PubMed] [Google Scholar]
- 215.Balkhi Fizra, Nasir Aamna, Zehra Arhama, Riaz Ramsha. Psychological and behavioral response to the coronavirus (COVID-19) pandemic. Cureus. 2020 doi: 10.7759/cureus.7923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Siddiqui Ammar Ahmed, Alshammary Freah, Amin Junaid, Rathore Hassaan Anwer, Hassan Ibne, Ilyas Muhammad, Alam Mohammad Khursheed. Knowledge and practice regarding prevention of COVID-19 among the Saudi Arabian population. WOR. 2020;66(4):767–775. doi: 10.3233/WOR-203223. [DOI] [PubMed] [Google Scholar]
- 217.Jang Won Mo, Jang Deok Hyun, Lee Jin Yong. Social distancing and transmission-reducing practices during the 2019 coronavirus disease and 2015 middle east respiratory syndrome coronavirus outbreaks in Korea. J. Korean Med. Sci. 2020;35(23) doi: 10.3346/jkms.2020.35.e220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Barber Sarah J., Kim Hyunji. COVID-19 worries and behavior changes in older and Younger men and women. J Gerontol. 2020 doi: 10.1093/geronb/gbaa068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Probst Thomas, Stippl Peter, Pieh Christoph. Changes in provision of psychotherapy in the early weeks of the COVID-19 lockdown in Austria. IJERPH. 2020;17(11):3815. doi: 10.3390/ijerph17113815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Colizzi Marco, Sironi Elena, Antonini Federico, Ciceri Marco Luigi, Bovo Chiara, Zoccante Leonardo. Psychosocial and behavioral impact of COVID-19 in autism spectrum disorder: An online parent survey. Brain Sci. 2020;10(6):341. doi: 10.3390/brainsci10060341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Jeste S., Hyde C., Distefano C., Halladay A., Ray S., Porath M., Wilson R.B., Thurm A. Changes in access to educational and healthcare services for individuals with intellectual and developmental disabilities during COVID-19 restrictions. J. Intellectual. Disabil. Res. 2020;64(11):825–833. doi: 10.1111/jir.12776. [DOI] [PubMed] [Google Scholar]
- 222.Korecka Nicole, Rabenstein Rafael, Pieh Christoph, Stippl Peter, Barke Antonia, Doering Bettina, Gossmann Katharina, Humer Elke, Probst Thomas. Psychotherapy by telephone or internet in Austria and Germany which CBT psychotherapists rate it more comparable to face-to-face psychotherapy in personal contact and have more positive actual experiences compared to previous expectations? IJERPH. 2020;17(21):7756. doi: 10.3390/ijerph17217756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Panda Prateek Kumar, Dawman Lesa, Panda Pragnya, Sharawat Indar Kumar. Feasibility and effectiveness of teleconsultation in children with epilepsy amidst the ongoing COVID-19 pandemic in a resource-limited country. Seizure. 2020;81:29–35. doi: 10.1016/j.seizure.2020.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Murphy Ann A., Karyczak Sean, Dolce Joni N., Zechner Michelle, Bates Francine, Gill Kenneth J., Rothpletz-Puglia Pamela. Challenges experienced by behavioral health organizations in new york resulting from COVID-19: A qualitative analysis. Community Ment Health J. 2020 doi: 10.1007/s10597-020-00731-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Waller Glenn, Pugh Matthew, Mulkens Sandra, Moore Elana, Mountford Victoria A., Carter Jacqueline, Wicksteed Amy, Maharaj Aryel, Wade Tracey D., Wisniewski Lucene, Farrell Nicholas R., Raykos Bronwyn, Jorgensen Susanne, Evans Jane, Thomas Jennifer J., Osenk Ivana, Paddock Carolyn, Bohrer Brittany, Anderson Kristen, Turner Hannah, Hildebrandt Tom, Xanidis Nikos, Smit Vera. Cognitive-behavioral therapy in the time of coronavirus: Clinician tips for working with eating disorders via telehealth when face-to-face meetings are not possible. Int. J. Eat. Disord. 2020;53(7):1132–1141. doi: 10.1002/eat.23289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Kersebaum Dilara, Fabig Sophie-Charlotte, Sendel Manon, Sachau Juliane, Lassen Josephine, Rehm Stefanie, Hüllemann Philipp, Baron Ralf, Gierthmühlen Janne. The early influence of COVID-19 pandemic-associated restrictions on pain, mood, and everyday life of patients with painful polyneuropathy. PR9 Reports. 2020;5(6) doi: 10.1097/PR9.0000000000000858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Taddei Matilde, Bulgheroni Sara. Facing the real time challenges of the COVID-19 emergency for child neuropsychology service in Milan. Res. Dev. Disabil. 2020;107 doi: 10.1016/j.ridd.2020.103786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Brondino Natascia, Damiani Stefano, Politi Pierluigi. Effective strategies for managing COVID-19 emergency restrictions for adults with severe ASD in a daycare center in Italy. Brain Sci. 2020;10(7):436. doi: 10.3390/brainsci10070436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Gebbia Vittorio, Piazza Dario, Valerio Maria Rosaria, Borsellino Nicolo, Firenze Alberto. Patients with cancer and COVID-19: A whatsapp messenger-based survey of patients’ queries, needs, fears, and actions taken. JCO Glob. Oncol. 2020;(6):722–729. doi: 10.1200/GO.20.00118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Onesti Concetta Elisa, Rugo Hope S., Generali Daniele, Peeters Marc, Zaman Khalil, Wildiers Hans, Harbeck Nadia, Martin Miguel, Cristofanilli Massimo, Cortes Javier, Tjan-Heijnen Vivianne, Hurvitz Sara A., Berchem Guy, Tagliamento Marco, Campone Mario, Bartsch Rupert, Placido Sabino De, Puglisi Fabio, Rottey Sylvie, Müller Volkmar, Ruhstaller Thomas, Machiels Jean-Pascal, Conte PierFranco, Awada Ahmad, Jerusalem Guy. Oncological care organisation during COVID-19 outbreak. ESMO Open. 2020;5(4) doi: 10.1136/esmoopen-2020-000853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Palinkas Lawrence A., Whiteside Lauren, Nehra Deepika, Engstrom Allison, Taylor Mark, Moloney Kathleen, Zatzick Douglas F. Rapid ethnographic assessment of the COVID-19 pandemic april 2020 ‘surge’ and its impact on service delivery in an acute care medical emergency department and trauma center. BMJ Open. 2020;10(10) doi: 10.1136/bmjopen-2020-041772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Li Xiaoye, Zuo Chengchun, Lu Wenjing, Zou Ye, Xu Qing, Li Xiaoyu, Lv Qianzhou. Evaluation of remote pharmacist-led outpatient service for geriatric patients on rivaroxaban for nonvalvular atrial fibrillation during the COVID-19 pandemic. Front. Pharmacol. 2020;11 doi: 10.3389/fphar.2020.01275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Monaco Andrea, Manzia Tommaso Maria, Angelico Roberta, Iaria Giuseppe, Gazia Carlo, Alawi Yousef Al, Fourtounas Konstantinos, Tisone Giuseppe, Cacciola Roberto. Awareness and impact of non-pharmaceutical interventions during coronavirus disease 2019 pandemic in renal transplant recipients. Transplant. Proc. 2020;52(9):2607–2613. doi: 10.1016/j.transproceed.2020.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Ayas Mohammed, Amadi Ahmad Mohd Haider Ali Al, Khaled Duaa, Alwaa Ahmad Munzer. Impact of COVID-19 on the access to hearing health care services for children with cochlear implants: a survey of parents. F1000Res. 2020;9:690. doi: 10.12688/f1000research.24915.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Auerbach Andrew, Leary Kevin J.O., Greysen S. Ryan, Harrison James D., Kripalani Sunil, Ruhnke Gregory W., Vasilevskis Eduard E., Maselli Judith, Fang Margaret C., Herzig Shoshana J., Lee Tiffany, Schnipper Jeffrey. Hospital ward adaptation during the COVID-19 pandemic: A national survey of academic medical centers. J. Hosp. Med. 2020;15(8):483–488. doi: 10.12788/jhm.3476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Applebaum Jennifer W., Tomlinson Camie A., Matijczak Angela, McDonald Shelby E., Zsembik Barbara A. The concerns, difficulties, and stressors of caring for pets during COVID-19: Results from a large survey of U.S. pet owners. Animals. 2020;10(10):1882. doi: 10.3390/ani10101882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Haakansson Anders. Changes in gambling behavior during the COVID-19 pandemic. a web survey study in Sweden. IJERPH. 2020;17(11):4013. doi: 10.3390/ijerph17114013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Ugolini Francesca, Massetti Luciano, Calaza-Martínez Pedro, Cariñanos Paloma, Dobbs Cynnamon, Ostoić Silvija Krajter, Marin Ana Marija, Pearlmutter David, Saaroni Hadas, Šaulienė Ingrida, Simoneti Maja, Verlič Andrej, Vuletić Dijana, Sanesi Giovanni. Effects of the COVID-19 pandemic on the use and perceptions of urban green space: An international exploratory study. Urban For. Urban Green. 2020;56 doi: 10.1016/j.ufug.2020.126888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Randler Christoph, Tryjanowski Piotr, Jokimäki Jukka, Kaisanlahti-Jokimäki Marja-Liisa, Staller Naomi. SARS-CoV2 (COVID-19) pandemic lockdown influences nature-based recreational activity: The case of birders. IJERPH. 2020;17(19):7310. doi: 10.3390/ijerph17197310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Håkansson Anders. Impact of COVID-19 on online gambling - a general population survey during the pandemic. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.568543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Choi Chulhwan, Bum Chul-Ho. Changes in the type of sports activity due to COVID-19: Hypochondriasis and the intention of continuous participation in sports. IJERPH. 2020;17(13):4871. doi: 10.3390/ijerph17134871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Håkansson Anders, Jönsson Caroline, Kenttä Göran. Psychological distress and problem gambling in elite athletes during COVID-19 restrictions - a web survey in top leagues of three sports during the pandemic. IJERPH. 2020;17(18):6693. doi: 10.3390/ijerph17186693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Graupensperger Scott, Benson Alex J., Kilmer Jason R., Evans M. Blair. Social (un)distancing: Teammate interactions, athletic identity, and mental health of student-athletes during the COVID-19 pandemic. J. Adolesc. Health. 2020;67(5):662–670. doi: 10.1016/j.jadohealth.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Zhao Ying, Guo Yong, Xiao Yu, Zhu Ranke, Sun Wei, Huang Weiyong, Liang Deyi, Tang Liuying, Zhang Fan, Zhu Dongsheng, et al. The effects of online homeschooling on children, parents, and teachers of grades 1–9 during the COVID-19 pandemic. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2020;26:e925591–1. doi: 10.12659/MSM.925591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Elsalem Lina, Al-Azzam Nosayba, Jumah Ahmad A., Obeidat Nail, Sindiani Amer Mahmoud, Kheirallah Khalid A. Stress and behavioral changes with remote E-exams during the Covid-19 pandemic: A cross-sectional study among undergraduates of medical sciences. Ann. Med. Surg. 2020;60:271–279. doi: 10.1016/j.amsu.2020.10.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Myers Kyle R., Tham Wei Yang, Yin Yian, Cohodes Nina, Thursby Jerry G., Thursby Marie C., Schiffer Peter, Walsh Joseph T., Lakhani Karim R., Wang Dashun. Unequal effects of the COVID-19 pandemic on scientists. Nat. Hum. Behav. 2020;4(9):880–883. doi: 10.1038/s41562-020-0921-y. [DOI] [PubMed] [Google Scholar]
- 247.Bönisch Sebastian, Wegscheider Karl, Krause Linda, Sehner Susanne, Wiegel Sarah, Zapf Antonia, Moser Silke, Becher Heiko. Effects of coronavirus disease (COVID-19) related contact restrictions in Germany, march to may 2020, on the mobility and relation to infection patterns. Front. Public Health. 2020;8 doi: 10.3389/fpubh.2020.568287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Sun Shaoxiong, Folarin Amos A., Ranjan Yatharth, Rashid Zulqarnain, Conde Pauline, Stewart Callum, Cummins Nicholas, Matcham Faith, Costa Gloria Dalla, Simblett Sara, Leocani Letizia, Lamers Femke, Sorensen Per Soelberg, Buron Mathias, Zabalza Ana, Pérez Ana Isabel Guerrero, Penninx Brenda W.J.H., Siddi Sara, Haro Josep Maria, Myin-Germeys Inez, Rintala Aki, Wykes Til, Narayan Vaibhav A., Comi Giancarlo, Hotopf Matthew, Dobson Richard J.B. Using smartphones and wearable devices to monitor behavioral changes during COVID-19. J. Med. Int. Res. 2020;22(9) doi: 10.2196/19992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Song Wei, Jin Xiaotong, Gao Jian, Zhao Taiyang. Will buying follow others ease their threat of death? An analysis of consumer data during the period of COVID-19 in China. IJERPH. 2020;17(9):3215. doi: 10.3390/ijerph17093215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Butu Alina, Brumă Ioan Sebastian, Tanasă Lucian, Rodino Steliana, Vasiliu Codrin Dinu, Dobos Sebastian, Butu Marian. The impact of COVID-19 crisis upon the consumer buying behavior of fresh vegetables directly from local producers. Case study: The quarantined area of suceava county, Romania. IJERPH. 2020;17(15):5485. doi: 10.3390/ijerph17155485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Jribi Sarra, Ismail Hanen Ben, Doggui Darine, Debbabi Hajer. COVID-19 virus outbreak lockdown: What impacts on household food wastage? Environ. Dev. Sustain. 2020;22(5):3939–3955. doi: 10.1007/s10668-020-00740-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Zhang Juanjuan, Litvinova Maria, Liang Yuxia, Zheng Wen, Shi Huilin, Vespignani Alessandro, Viboud Cecile, Ajelli Marco, Yu Hongjie. The impact of relaxing interventions on human contact patterns and SARS-CoV-2 transmission in China. medRxiv. 2020 doi: 10.1126/sciadv.abe2584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Samuels Elizabeth A., Clark Seth A., Wunsch Caroline, Keeler Lee Ann Jordison, Reddy Neha, Vanjani Rahul, Wightman Rachel S. Innovation during COVID-19: Improving addiction treatment access. J. Addict. Med. 2020;14(4):e8–e9. doi: 10.1097/ADM.0000000000000685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Goldman Matthew L., Druss Benjamin G., Horvitz-Lennon Marcela, Norquist Grayson S., Ptakowski Kristin Kroeger, Brinkley Amy, Greiner Miranda, Hayes Heath, Hepburn Brian, Jorgensen Shea, Swartz Marvin S., Dixon Lisa B. Mental health policy in the era of COVID-19. PS. 2020;71(11):1158–1162. doi: 10.1176/appi.ps.202000219. [DOI] [PubMed] [Google Scholar]
- 255.Lau Jen, Knudsen Janine, Jackson Hannah, Wallach Andrew B., Bouton Michael, Natsui Shaw, Philippou Christopher, Karim Erfan, Silvestri David M., Avalone Lynsey, Zaurova Milana, Schatz Daniel, Sun Vivian, Chokshi Dave A. Staying connected in the COVID-19 pandemic: Telehealth at the largest safety-net system in the United States. Health Affairs. 2020;39(8):1437–1442. doi: 10.1377/hlthaff.2020.00903. [DOI] [PubMed] [Google Scholar]
- 256.Connolly Samantha L., Stolzmann Kelly L., Heyworth Leonie, Weaver Kendra R., Bauer Mark S., Miller Christopher J. Rapid increase in telemental health within the department of veterans affairs during the COVID-19 pandemic. Telemedicine e-Health. 2020 doi: 10.1089/tmj.2020.0233. [DOI] [PubMed] [Google Scholar]
- 257.Sweeney M. Counseling clients during New York City’s COVID-19 pandemic: observations on fundamental elements of emotions management. Ir. j. psychol. Med. 2020;37(3):212–213. doi: 10.1017/ipm.2020.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Gostic Katelyn M., McGough Lauren, Baskerville Edward, Abbott Sam, Joshi Keya, Tedijanto Christine, Kahn Rebecca, Niehus Rene, Hay James A., Salazar Pablo M. De, Hellewell Joel, Meakin Sophie, Munday James, Bosse Nikos, Sherratt Katharine, Thompson Robin M., White Laura F., Huisman Jana, Scire Jérémie, Bonhoeffer Sebastian, Stadler Tanja, Wallinga Jacco, Funk Sebastian, Lipsitch Marc, Cobey Sarah. Practical considerations for measuring the effective reproductive number, rt. medRxiv. 2020 doi: 10.1371/journal.pcbi.1008409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Leonardi Rosario, Bellinzoni Piera, Broglia Luigi, Colombo Renzo, Marchi Davide De, Falcone Lorenzo, Giusti Guido, Grasso Vincenzo, Mantica Guglielmo, Passaretti Giovanni, Proietti Silvia, Russo Antonio, Saitta Giuseppe, Smelzo Salvatore, Suardi Nazareno, Gaboardi Franco. Hospital care in departments defined as COVID-free: A proposal for a safe hospitalization protecting healthcare professionals and patients not affected by COVID-19. Arch. Ital. Urol. Androl. 2020;92(2) doi: 10.4081/aiua.2020.2.67. [DOI] [PubMed] [Google Scholar]
- 260.Furfaro Federica, Vuitton Lucine, Fiorino Gionata, Koch Stephane, Allocca Mariangela, Gilardi Daniela, Zilli Alessandra, D’Amico Ferdinando, Radice Simona, Chevaux Jean-Baptiste, Schaefer Marion, Chaussade Stanislas, Danese Silvio, Peyrin-Biroulet Laurent. SFED recommendations for IBD endoscopy during COVID-19 pandemic: Italian and french experience. Nat. Rev. Gastroenterol. Hepatol. 2020;17(8):507–516. doi: 10.1038/s41575-020-0319-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Gualano Maria Rosaria, Moro Giuseppina Lo, Voglino Gianluca, Bert Fabrizio, Siliquini Roberta. Monitoring the impact of COVID-19 pandemic on mental health: a public health challenge? Reflection on Italian data. Soc. Psychiatry Psychiatr Epidemiol. 2020 doi: 10.1007/s00127-020-01971-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Elbeddini Ali, Prabaharan Thulasika, Almasalkhi Sarah, Tran Cindy, Zhou Yueyang. Barriers to conducting deprescribing in the elderly population amid the COVID-19 pandemic. Res. Soc. Adm. Pharm. 2020 doi: 10.1016/j.sapharm.2020.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Zastepa Evelyn, Sun Jane C., Clune Jennifer, Mathew Nickie. Adaptation of contingency management for stimulant use disorder during the COVID-19 pandemic. J. Subst. Abuse. Treat. 2020;118 doi: 10.1016/j.jsat.2020.108102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Jones Christopher M., Radhakrishna Ganesh, Aitken Katharine, Bridgewater John, Corrie Pippa, Eatock Martin, Goody Rebecca, Ghaneh Paula, Good James, Grose Derek, Holyoake Daniel, Hunt Arabella, Jamieson Nigel B., Palmer Daniel H., Soonawalla Zahir, Valle Juan W., Hawkins Maria A., Mukherjee Somnath. Considerations for the treatment of pancreatic cancer during the COVID-19 pandemic: the UK consensus position. Br. J. Cancer. 2020;123(5):709–713. doi: 10.1038/s41416-020-0980-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Thompson Robin N. Epidemiological models are important tools for guiding COVID-19 interventions. BMC Med. 2020;18(1) doi: 10.1186/s12916-020-01628-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Nachega Jean B., Grimwood Ashraf, Mahomed Hassan, Fatti Geoffrey, Preiser Wolfgang, Kallay Oscar, Mbala Placide K., Muyembe Jean-Jacques T., Rwagasore Edson, Nsanzimana Sabin, Ngamije Daniel, Condo Jeanine, Sidat Mohsin, Noormahomed Emilia V., Reid Michael, Lukeni Beatrice, Suleman Fatima, Mteta Alfred, Zumla Alimuddin. From easing lockdowns to scaling up community-based coronavirus disease 2019 screening, testing, and contact tracing in africa. Shared approaches, innovations, and challenges to minimize morbidity and mortality. Clin. Infect. Dis. 2020 doi: 10.1093/cid/ciaa695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Sun Jing, Shi Zhanli, Xu Hong. Non-pharmaceutical interventions used for COVID-19 had a major impact on reducing influenza in China in 2020. J. Travel Med. 2020 doi: 10.1093/jtm/taaa064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Mohammed Hussen, Oljira Lemessa, Roba Kedir Teji, Yimer Getnet, Fekadu Abebaw, Manyazewal Tsegahun. Containment of COVID-19 in Ethiopia and implications for tuberculosis care and research. Infect. Dis. Poverty. 2020;9(1) doi: 10.1186/s40249-020-00753-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Torres Anna, Domańska-Glonek Ewa, Dzikowski Wojciech, Korulczyk Jan, Torres Kamil. Transition to online is possible: Solution for simulation-based teaching during the COVID-19 pandemic. Med. Educ. 2020;54(9):858–859. doi: 10.1111/medu.14245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Chien Li-Chien, Beÿ Christian K., Koenig Kristi L. Taiwan’s successful COVID-19 mitigation and containment strategy: Achieving quasi population immunity. Disaster Med. Public Health Prep. 2020:1–4. doi: 10.1017/dmp.2020.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Nong Vuong Minh, Nguyen Quyen Le Thi, Doan Tra Thu, Do Thanh Van, Nguyen Tuan Quang, Dao Co Xuan, Nguyen Trang Huyen Thi, Do Cuong Duy. The second wave of COVID-19 in a tourist hotspot in Vietnam. J. Travel Med. 2020 doi: 10.1093/jtm/taaa174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Oh Juhwan, Lee Jong-Koo, Schwarz Dan, Ratcliffe Hannah L., Markuns Jeffrey F., Hirschhorn Lisa R. National response to COVID-19 in the Republic of Korea and lessons learned for other countries. Health Syst. Reform. 2020;6(1) doi: 10.1080/23288604.2020.1753464. [DOI] [PubMed] [Google Scholar]
- 273.Lateef Fatimah. Face to face with coronavirus disease 19: Maintaining motivation, psychological safety, and wellness. J. Emerg. Trauma Shock. 2020;13(2):116. doi: 10.4103/JETS.JETS_27_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Anmella G., Arbelo N., Fico G., Murru A., Llach C.D., Madero S., da Costa S. Gomes, Imaz M.L., López-Pelayo H., Vieta E., Pintor L. COVID-19 inpatients with psychiatric disorders: Real-world clinical recommendations from an expert team in consultation-liaison psychiatry. J. Affect. Disord. 2020;274:1062–1067. doi: 10.1016/j.jad.2020.05.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Kopelovich Sarah L., Monroe-DeVita Maria, Buck Benjamin E., Brenner Carolyn, Moser Lorna, Jarskog L. Fredrik, Harker Steve, Chwastiak Lydia A. Community mental health care delivery during the COVID-19 pandemic: Practical strategies for improving care for people with serious mental illness. Community Ment. Health J. 2020 doi: 10.1007/s10597-020-00662-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Wong Ambrose, Roppolo Lynn, Chang Bernard, Yonkers Kimberly, Wilson Michael, Powsner Seth, Rozel John. Management of agitation during the COVID-19 pandemic. WestJEM. 2020;21(4) doi: 10.5811/westjem.2020.5.47789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Sangal Rohit B., Scofi Jean E., Parwani Vivek, Pickens Andrew T., Ulrich Andrew, Venkatesh Arjun K. Less social emergency departments: implementation of workplace contact reduction during COVID-19. Emerg. Med. J. 2020:emermed–2020–209826. doi: 10.1136/emermed-2020-209826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Hsu Michael, Ahern David K., Suzuki Joji. Digital phenotyping to enhance substance use treatment during the COVID-19 pandemic. JMIR Ment. Health. 2020;7(10) doi: 10.2196/21814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.López-Pelayo Hugo, Aubin Henri-Jean, Drummond Colin, Dom Geert, Pascual Francisco, Rehm Jürgen, Saitz Richard, Scafato Emanuele, Gual Antoni. The post-COVID era: challenges in the treatment of substance use disorder (SUD) after the pandemic. BMC Med. 2020;18(1) doi: 10.1186/s12916-020-01693-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Ornell Felipe, Moura Helena Ferreira, Scherer Juliana Nichterwitz, Pechansky Flavio, Kessler Felix Henrique Paim, von Diemen Lisia. The COVID-19 pandemic and its impact on substance use: Implications for prevention and treatment. Psychiatry Res. 2020;289 doi: 10.1016/j.psychres.2020.113096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Pothuri Bhavana, Secord Angeles Alvarez, Armstrong Deborah K., Chan John, Fader Amanda N., Huh Warner, Kesterson Joshua, Liu Joyce F., Moore Kathleen, Westin Shannon N., Naumann R. Wendel. Anti-cancer therapy and clinical trial considerations for gynecologic oncology patients during the COVID-19 pandemic crisis. Gynecol. Oncol. 2020;158(1):16–24. doi: 10.1016/j.ygyno.2020.04.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Baweja Raman, Verma Shikha, Pathak Meenal, Waxmonsky James G. Development of a child and adolescent tele-partial hospitalization program (tele-PHP) in response to the COVID-19 pandemic. Prim. Care Companion CNS Disord. 2020;22(5) doi: 10.4088/PCC.20m02743. [DOI] [PubMed] [Google Scholar]
- 283.Plevinsky Jill M., Young Melissa A., Carmody Julia K., Durkin Lindsay K., Gamwell Kaitlyn L., Klages Kimberly L., Ghosh Shweta, Hommel Kevin A. The impact of COVID-19 on pediatric adherence and self-management. J. Pediatr. Psychol. 2020;45(9):977–982. doi: 10.1093/jpepsy/jsaa079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Correia G., Rodrigues L., da Silva M. Gameiro, Gonçalves T. Airborne route and bad use of ventilation systems as non-negligible factors in SARS-CoV-2 transmission. Med. Hypotheses. 2020;141 doi: 10.1016/j.mehy.2020.109781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Pritchard Alison E., Sweeney Kristie, Salorio Cynthia F., Jacobson Lisa A. Pediatric neuropsychological evaluation via telehealth: Novel models of care. Clin. Neuropsychol. 2020;34(7–8):1367–1379. doi: 10.1080/13854046.2020.1806359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Bartolo Michelangelo, Intiso Domenico, Lentino Carmelo, Sandrini Giorgio, Paolucci Stefano, Zampolini Mauro. Urgent measures for the containment of the coronavirus (Covid-19) epidemic in the neurorehabilitation/rehabilitation departments in the phase of maximum expansion of the epidemic. Front. Neurol. 2020;11 doi: 10.3389/fneur.2020.00423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Lapid Maria I., Seiner Stephen, Heintz Hannah, Hermida Adriana P., Nykamp Louis, Sanghani Sohag N., Mueller Martina, Petrides Georgios, Forester Brent P. Electroconvulsive therapy practice changes in older individuals due to COVID-19: Expert consensus statement. Am. J. Geriatr. Psychiatry. 2020;28(11):1133–1145. doi: 10.1016/j.jagp.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Halliwell-Ewen M., Atkin B., Huins C.T., Dalton C.L. Restructuring ENT out-patient services during the coronavirus disease 2019 pandemic–an iterative approach. J. Laryngol. Otol. 2020;134(8):670–679. doi: 10.1017/S0022215120001450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Cobey Sarah. Modeling infectious disease dynamics. Science. 2020;368(6492):713–714. doi: 10.1126/science.abb5659. [DOI] [PubMed] [Google Scholar]
- 290.Thompson Robin N., Hollingsworth T. Déirdre, Isham Valerie, Arribas-Bel Daniel, Ashby Ben, Britton Tom, Challenor Peter, Chappell Lauren H.K., Clapham Hannah, Cunniffe Nik J., Dawid A. Philip, Donnelly Christl A., Eggo Rosalind M., Funk Sebastian, Gilbert Nigel, Glendinning Paul, Gog Julia R., Hart William S., Heesterbeek Hans, House Thomas, Keeling Matt, Kiss István Z., Kretzschmar Mirjam E., Lloyd Alun L., McBryde Emma S., McCaw James M., McKinley Trevelyan J., Miller Joel C., Morris Martina, Neill Philip D.O., Parag Kris V., Pearson Carl A.B., Pellis Lorenzo, Pulliam Juliet R.C., Ross Joshua V., Tomba Gianpaolo Scalia, Silverman Bernard W., Struchiner Claudio J., Tildesley Michael J., Trapman Pieter, Webb Cerian R., Mollison Denis, Restif Olivier. Key questions for modelling COVID-19 exit strategies. Proc. R. Soc. B. 2020;287(1932) doi: 10.1098/rspb.2020.1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Vespignani Alessandro, Tian Huaiyu, Dye Christopher, Lloyd-Smith James O., Eggo Rosalind M., Shrestha Munik, Scarpino Samuel V., Gutierrez Bernardo, Kraemer Moritz U.G., Wu Joseph, Leung Kathy, Leung Gabriel M. Modelling COVID-19. Nat. Rev. Phys. 2020;2(6):279–281. doi: 10.1038/s42254-020-0178-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Poletto Chiara, Scarpino Samuel V., Volz Erik M. Applications of predictive modelling early in the COVID-19 epidemic. Lancet Digit. Health. 2020;2(10):e498–e499. doi: 10.1016/S2589-7500(20)30196-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Panovska-Griffiths Jasmina. Can mathematical modelling solve the current Covid-19 crisis? BMC Public Health. 2020;20(1) doi: 10.1186/s12889-020-08671-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Lee Elizabeth C., Wada Nikolas I., Grabowski M. Kate, Gurley Emily S., Lessler Justin. The engines of SARS-CoV-2 spread. Science. 2020;370(6515):406–407. doi: 10.1126/science.abd8755. [DOI] [PubMed] [Google Scholar]
- 295.Colebunders Robert, Fodjo Joseph Nelson Siewe, Vanham Guido, den Bergh Rafael Van. A call for strengthened evidence on targeted, non-pharmaceutical interventions against COVID-19 for the protection of vulnerable individuals in sub-Saharan Africa. Int. J. Infect. Dis. 2020;99:482–484. doi: 10.1016/j.ijid.2020.08.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Althouse Benjamin M., Wenger Edward A., Miller Joel C., Scarpino Samuel V., Allard Antoine, Hébert-Dufresne Laurent, Hu Hao. Superspreading events in the transmission dynamics of SARS-CoV-2: Opportunities for interventions and control. PLoS Biol. 2020;18(11) doi: 10.1371/journal.pbio.3000897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Bouayed Jaouad, Bohn Torsten. Behavioral manipulation key to the successful global spread of the new coronavirus SARS-CoV-2? J. Med. Virol. 2020 doi: 10.1002/jmv.26446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Feng Zhilan, Glasser John W., Hill Andrew N. On the benefits of flattening the curve: A perspective. Math. Biosci. 2020;326 doi: 10.1016/j.mbs.2020.108389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Lambrese Jason V. Helping children cope with the COVID-19 pandemic. CCJM. 2020 doi: 10.3949/ccjm.87a.ccc010. [DOI] [PubMed] [Google Scholar]
- 300.Pacheco Lílian Fernanda, Noll Matias, Mendonça Carolina Rodrigues. Challenges in teaching human anatomy to students with intellectual disabilities during the Covid-19 pandemic. Anat. Sci. Educ. 2020;13(5):556–557. doi: 10.1002/ase.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Håkansson Anders, Fernández-Aranda Fernando, Menchón Jose M., Potenza Marc N., Jiménez-Murcia Susana. Gambling during the COVID-19 crisis. a cause for concern. J. Addict. Med. 2020;14(4):e10–e12. doi: 10.1097/ADM.0000000000000690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Zowalaty Mohamed E. El, Young Sean G., Järhult Josef D. Environmental impact of the COVID-19 pandemic a lesson for the future. Infect. Ecol. Epidemiol. 2020;10(1) doi: 10.1080/20008686.2020.1768023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Vanapalli Kumar Raja, Sharma Hari Bhakta, Ranjan Ved Prakash, Samal Biswajit, Bhattacharya Jayanta, Dubey Brajesh K., Goel Sudha. Challenges and strategies for effective plastic waste management during and post COVID-19 pandemic. Sci. Total Environ. 2021;750 doi: 10.1016/j.scitotenv.2020.141514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Khan Moien A.B., Smith Jane Elizabeth Moverley. Covibesity, a new pandemic. Obesity Med. 2020;19 doi: 10.1016/j.obmed.2020.100282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Yeo Roland K. Know thyself. Organ. Dyn. 2020 doi: 10.1016/j.orgdyn.2020.100800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Mestre-Bach Gemma, Blycker Gretchen R., Potenza Marc N. Pornography use in the setting of the COVID-19 pandemic. J. Behav. Addict. 2020;9(2):181–183. doi: 10.1556/2006.2020.00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Wilder-Smith Annelies, Bar-Yam Yaneer, Fisher Dale. Lockdown to contain COVID-19 is a window of opportunity to prevent the second wave. J. Travel Med. 2020;27(5) doi: 10.1093/jtm/taaa091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Pelaez Martha, Novak Gary. Returning to school: Separation problems and anxiety in the age of pandemics. Behav. Anal. Pract. 2020;13(3):521–526. doi: 10.1007/s40617-020-00467-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.González-Bustamante Bastián. Evolution and early government responses to COVID-19 in south america. World Dev. 2021;137 doi: 10.1016/j.worlddev.2020.105180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Costantino Valentina, Heslop David J., MacIntyre C. Raina. The effectiveness of full and partial travel bans against COVID-19 spread in Australia for travellers from China during and after the epidemic peak in China. J. Travel Med. 2020;27(5) doi: 10.1093/jtm/taaa081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Rahman Md. Rejaur, Islam A.H.M. Hedayutul, Islam Md. Nazrul. Geospatial modelling on the spread and dynamics of 154 day outbreak of the novel coronavirus (COVID-19) pandemic in Bangladesh towards vulnerability zoning and management approaches. Model. Earth Syst. Environ. 2020 doi: 10.1007/s40808-020-00962-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Ali Sheikh Taslim, Wang Lin, Lau Eric H.Y., Xu Xiao-Ke, Du Zhanwei, Wu Ye, Leung Gabriel M., Cowling Benjamin J. Serial interval of SARS-CoV-2 was shortened over time by nonpharmaceutical interventions. Science. 2020;369(6507):1106–1109. doi: 10.1126/science.abc9004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Jing Qin-Long, Liu Ming-Jin, Zhang Zhou-Bin, Fang Li-Qun, Yuan Jun, Zhang An-Ran, Dean Natalie E, Luo Lei, Ma Meng-Meng, Longini Ira, Kenah Eben, Lu Ying, Ma Yu, Jalali Neda, Yang Zhi-Cong, Yang Yang. Household secondary attack rate of COVID-19 and associated determinants in Guangzhou, China: a retrospective cohort study. Lancet Infect. Dis. 2020;20(10):1141–1150. doi: 10.1016/S1473-3099(20)30471-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Lei Hao, Xu Modi, Wang Xiao, Xie Yu, Du Xiangjun, Chen Tao, Yang Lei, Wang Dayan, Shu Yuelong. Nonpharmaceutical interventions used to control COVID-19 reduced seasonal influenza transmission in China. J. Infect. Dis. 2020;222(11):1780–1783. doi: 10.1093/infdis/jiaa570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Sun Kaiyuan, Wang Wei, Gao Lidong, Wang Yan, Luo Kaiwei, Ren Lingshuang, Zhan Zhifei, Chen Xinghui, Zhao Shanlu, Huang Yiwei, Sun Qianlai, Liu Ziyan, Litvinova Maria, Vespignani Alessandro, Ajelli Marco, Viboud Cécile, Yu Hongjie. Transmission heterogeneities, kinetics, and controllability of SARS-CoV-2. Science. 2020:eabe2424. doi: 10.1126/science.abe2424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Kaur Taranjot, Sarkar Sukanta, Chowdhury Sourangsu, Sinha Sudipta Kumar, Jolly Mohit Kumar, Dutta Partha Sharathi. Anticipating the novel coronavirus disease (COVID-19) pandemic. Front. Public Health. 2020;8 doi: 10.3389/fpubh.2020.569669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Guzzetta Giorgio, Riccardo Flavia, Marziano Valentina, Poletti Piero, Trentini Filippo, Bella Antonino, Andrianou Xanthi, Manso Martina Del, Fabiani Massimo, Bellino Stefania, Boros Stefano, Urdiales Alberto Mateo, Vescio Maria Fenicia, Piccioli Andrea, Brusaferro Silvio, Rezza Giovanni, Pezzotti Patrizio, Ajelli Marco, Merler Stefano. Impact of a nationwide lockdown on SARS-CoV-2 transmissibility, Italy. Emerg. Infect. Diseases. 2021;27(1) doi: 10.3201/eid2701.202114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Lavezzo Enrico, Franchin Elisa, Ciavarella Constanze, Cuomo-Dannenburg Gina, Barzon Luisa, Vecchio Claudia Del, Rossi Lucia, Manganelli Riccardo, Loregian Arianna, Navarin Nicolò, Abate Davide, Sciro Manuela, Merigliano Stefano, Canale Ettore De, Vanuzzo Maria Cristina, Besutti Valeria, Saluzzo Francesca, Onelia Francesco, Pacenti Monia, Parisi Saverio G., Carretta Giovanni, Donato Daniele, Flor Luciano, Cocchio Silvia, Masi Giulia, Sperduti Alessandro, Cattarino Lorenzo, Salvador Renato, Nicoletti Michele, Caldart Federico, Castelli Gioele, Nieddu Eleonora, Labella Beatrice, Fava Ludovico, Drigo Matteo, Gaythorpe Katy A.M., Brazzale Alessandra R., Toppo Stefano, Trevisan Marta, Baldo Vincenzo, Donnelly Christl A., Ferguson Neil M., Dorigatti Ilaria, Crisanti Andrea. Suppression of a SARS-CoV-2 outbreak in the Italian municipality of vo’. Nature. 2020;584(7821):425–429. doi: 10.1038/s41586-020-2488-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Jefferies Sarah, French Nigel, Gilkison Charlotte, Graham Giles, Hope Virginia, Marshall Jonathan, McElnay Caroline, McNeill Andrea, Muellner Petra, Paine Shevaun, Prasad Namrata, Scott Julia, Sherwood Jillian, Yang Liang, Priest Patricia. COVID-19 in New Zealand and the impact of the national response: a descriptive epidemiological study. Lancet Public Health. 2020;5(11):e612–e623. doi: 10.1016/S2468-2667(20)30225-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Valencia Miguel, Becerra José E., Reyes Juan C., Castro Kenneth G. Assessment of early mitigation measures against COVID-19 in Puerto Rico: March 15-may 15, 2020. PLoS ONE. 2020;15(10) doi: 10.1371/journal.pone.0240013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Huh Kyungmin, Jung Jaehun, Hong Jinwook, Kim MinYoung, Ahn Jong Gyun, Kim Jong-Hun, Kang Ji-Man. Impact of nonpharmaceutical interventions on the incidence of respiratory infections during the coronavirus disease 2019 (COVID-19) outbreak in Korea: A nationwide surveillance study. Clin. Infect. Dis. 2020 doi: 10.1093/cid/ciaa1682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Hsieh Chih-Chia, Lin Chih-Hao, Wang William Yu Chung, Pauleen David J., Chen Jengchung Victor. The outcome and implications of public precautionary measures in Taiwan - declining respiratory disease cases in the COVID-19 pandemic. IJERPH. 2020;17(13):4877. doi: 10.3390/ijerph17134877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.White Easton R., Hébert-Dufresne Laurent. State-level variation of initial COVID-19 dynamics in the United States. PLoS ONE. 2020;15(10) doi: 10.1371/journal.pone.0240648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Chernozhukov Victor, Kasahara Hiroyuki, Schrimpf Paul. Causal impact of masks, policies, behavior on early covid-19 pandemic in the U.S. J. Econometrics. 2020 doi: 10.1016/j.jeconom.2020.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Auger Katherine A., Shah Samir S., Richardson Troy, Hartley David, Hall Matthew, Warniment Amanda, Timmons Kristen, Bosse Dianna, Ferris Sarah A., Brady Patrick W., Schondelmeyer Amanda C., Thomson Joanna E. Association between statewide school closure and COVID-19 incidence and mortality in the US. JAMA. 2020;324(9):859. doi: 10.1001/jama.2020.14348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Kissler Stephen M., Kishore Nishant, Prabhu Malavika, Goffman Dena, Beilin Yaakov, Landau Ruth, Gyamfi-Bannerman Cynthia, Bateman Brian T., Snyder Jon, Razavi Armin S., Katz Daniel, Gal Jonathan, Bianco Angela, Stone Joanne, Larremore Daniel, Buckee Caroline O., Grad Yonatan H. Reductions in commuting mobility correlate with geographic differences in SARS-CoV-2 prevalence in New York City. Nature Commun. 2020;11(1) doi: 10.1038/s41467-020-18271-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Jalali Aliea M., Peterson Brent M., Galbadage Thushara. Early COVID-19 interventions failed to replicate 1918 st. Louis vs. philadelphia outcomes in the United States. Front. Public Health. 2020;8 doi: 10.3389/fpubh.2020.579559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Baker Rachel E., Park Sang Woo, Yang Wenchang, Vecchi Gabriel A., Metcalf C. Jessica E., Grenfell Bryan T. The impact of COVID-19 nonpharmaceutical interventions on the future dynamics of endemic infections. Proc. Natl. Acad. Sci. USA. 2020;117(48):30547–30553. doi: 10.1073/pnas.2013182117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329.Jardine Rachel, Wright James, Samad Zainab, Bhutta Zulfiqar A. Analysis of COVID-19 burden, epidemiology and mitigation strategies in Muslim majority countries. East Mediterr Health J. 2020;26(10):1173–1183. doi: 10.26719/emhj.20.120. [DOI] [PubMed] [Google Scholar]
- 330.Castex Gonzalo, Dechter Evgenia, Lorca Miguel. COVID-19: The impact of social distancing policies, cross-country analysis. EconDisCliCha. 2020 doi: 10.1007/s41885-020-00076-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.Haug Nils, Geyrhofer Lukas, Londei Alessandro, Dervic Elma, Desvars-Larrive Amélie, Loreto Vittorio, Pinior Beate, Thurner Stefan, Klimek Peter. Ranking the effectiveness of worldwide COVID-19 government interventions. Nat. Hum. Behav. 2020;4(12):1303–1312. doi: 10.1038/s41562-020-01009-0. [DOI] [PubMed] [Google Scholar]
- 332.Koh Wee Chian, Naing Lin, Wong Justin. Estimating the impact of physical distancing measures in containing COVID-19: an empirical analysis. Int. J. Infect. Dis. 2020;100:42–49. doi: 10.1016/j.ijid.2020.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333.Islam Nazrul, Sharp Stephen J., Chowell Gerardo, Shabnam Sharmin, Kawachi Ichiro, Lacey Ben, Massaro Joseph M., D’Agostino Ralph B., White Martin. Physical distancing interventions and incidence of coronavirus disease 2019: natural experiment in 149 countries. BMJ. 2020:m2743. doi: 10.1136/bmj.m2743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334.Li Yuchen, Zeng Yu, Liu Guangdi, Lu Donghao, Yang Huazhen, Ying Zhiye, Hu Yao, Qiu Jianqing, Zhang Chao, Fall Katja, Fang Fang, Valdimarsdóttir Unnur A., Zhang Wei, Song Huan. Public awareness, emotional reactions and human mobility in response to the COVID-19 outbreak in China a population-based ecological study. Psychol. Med. 2020:1–8. doi: 10.1017/S003329172000375X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Su Yue, Xue Jia, Liu Xiaoqian, Wu Peijing, Chen Junxiang, Chen Chen, Liu Tianli, Gong Weigang, Zhu Tingshao. Examining the impact of COVID-19 lockdown in wuhan and lombardy: A psycholinguistic analysis on weibo and Twitter. IJERPH. 2020;17(12):4552. doi: 10.3390/ijerph17124552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336.Sheridan Adam, Andersen Asger Lau, Hansen Emil Toft, Johannesen Niels. Social distancing laws cause only small losses of economic activity during the COVID-19 pandemic in Scandinavia. Proc. Natl. Acad. Sci. USA. 2020;117(34):20468–20473. doi: 10.1073/pnas.2010068117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337.Schlosser Frank, Maier Benjamin F., Jack Olivia, Hinrichs David, Zachariae Adrian, Brockmann Dirk. COVID-19 lockdown induces disease-mitigating structural changes in mobility networks. Proc. Natl. Acad. Sci. USA. 2020 doi: 10.1073/pnas.2012326117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Slavova Svetla, Rock Peter, Bush Heather M., Quesinberry Dana, Walsh Sharon L. Signal of increased opioid overdose during COVID-19 from emergency medical services data. Drug Alcohol Depend. 2020;214 doi: 10.1016/j.drugalcdep.2020.108176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Jacobson Nicholas C., Lekkas Damien, Price George, Heinz Michael V., Song Minkeun, O’Malley A. James, Barr Paul J. Flattening the mental health curve: COVID-19 stay-at-home orders are associated with alterations in mental health search behavior in the united states. JMIR Ment. Health. 2020;7(6) doi: 10.2196/19347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Ward Rose Marie, Riordan Benjamin C., Merrill Jennifer E., Raubenheimer Jacques. Describing the impact of the COVID-19 pandemic on alcohol-induced blackout tweets. Drug Alcohol Rev. 2020 doi: 10.1111/dar.13186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Nguyen Thu T., Criss Shaniece, Dwivedi Pallavi, Huang Dina, Keralis Jessica, Hsu Erica, Phan Lynn, Nguyen Leah H., Yardi Isha, Glymour M. Maria, Allen Amani M., Chae David H., Gee Gilbert C., Nguyen Quynh C. Exploring U.S. shifts in anti-Asian sentiment with the emergence of COVID-19. IJERPH. 2020;17(19):7032. doi: 10.3390/ijerph17197032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Rousseau Sandra, Deschacht Nick. Public awareness of nature and the environment during the COVID-19 crisis. Environ. Res. Econ. 2020;76(4):1149–1159. doi: 10.1007/s10640-020-00445-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.Zaremba Adam, Kizys Renatas, Aharon David Y., Demir Ender. Infected markets: Novel coronavirus, government interventions, and stock return volatility around the globe. Finance Res. Lett. 2020;35 doi: 10.1016/j.frl.2020.101597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Quiros-Roldan Eugenia, Magro Paola, Carriero Canio, Chiesa Annacarla, Hamad Issa El, Tratta Elena, Fazio Raffaella, Formenti Beatrice, Castelli Francesco. Consequences of the COVID-19 pandemic on the continuum of care in a cohort of people living with HIV followed in a single center of Northern Italy. AIDS Res. Ther. 2020;17(1) doi: 10.1186/s12981-020-00314-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345.Schuengel C., Tummers J., Embregts P.J.C.M., Leusink G.L. Impact of the initial response to COVID-19 on long-term care for people with intellectual disability: an interrupted time series analysis of incident reports. J. Intellectual Disabil. Res. 2020;64(11):817–824. doi: 10.1111/jir.12778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Maringe Camille, Spicer James, Morris Melanie, Purushotham Arnie, Nolte Ellen, Sullivan Richard, Rachet Bernard, Aggarwal Ajay. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol. 2020;21(8):1023–1034. doi: 10.1016/S1470-2045(20)30388-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347.Wood Richard M., McWilliams Christopher J., Thomas Matthew J., Bourdeaux Christopher P., Vasilakis Christos. COVID-19 scenario modelling for the mitigation of capacity-dependent deaths in intensive care. Health Care Manag Sci. 2020;23(3):315–324. doi: 10.1007/s10729-020-09511-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348.Hale Thomas, Petherick Anna, Phillips Toby, Webster Samuel. Variation in government responses to COVID-19. Blavatnik Sch. Gov. Work. Pap. 2020;31 [Google Scholar]
- 349.Ray Soumalya, Lahiri Arista, Jha SweetySuman, Bhattacharya Saikat, Chakraborty Arup. Effectiveness of preventive measures against COVID-19: A systematic review of in silico modeling studies in indian context. Indian J. Public Health. 2020;64(6):156. doi: 10.4103/ijph.IJPH_464_20. [DOI] [PubMed] [Google Scholar]
- 350.Patiño-Lugo Daniel F., Velez Marcela, Salazar Pamela Velásquez, Vera-Giraldo Claudia Yaneth, Veéz Viviana, Mariń Isabel Cristina, Ramiŕez Paola Andrea, Quintero Sebastián Pemberthy, Martínez Esteban Castrillón, Higuita Daniel Andrés Pineda, Herrera Gilma Norela Henandez. Non-pharmaceutical interventions for containment, mitigation and suppression of COVID-19 infection. Colombia Medica. 2020:1–25. doi: 10.25100/cm.v51i2.4266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Hens Niel, Vranck Pascal, Molenberghs Geert. The COVID-19 epidemic, its mortality, and the role of non-pharmaceutical interventions. Eur. Heart J. 2020;9(3):204–208. doi: 10.1177/2048872620924922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352.Alvi Mohammed M., Sivasankaran Sowmya, Singh Mahima. Pharmacological and non-pharmacological efforts at prevention, mitigation, and treatment for COVID-19. J. Drug Target. 2020;28(7–8):742–754. doi: 10.1080/1061186X.2020.1793990. [DOI] [PubMed] [Google Scholar]
- 353.Pedrosa Ana Luisa, Bitencourt Letícia, Fróes Ana Claudia Fontoura, Cazumbá Maria Luíza Barreto, Campos Ramon Gustavo Bernardino, de Brito Stephanie Bruna Camilo Soares, e Silva Ana Cristina Simões. Emotional, behavioral, and psychological impact of the COVID-19 pandemic. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.566212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 354.Kneale Dylan, Mara-Eves Alison O., Rees Rebecca, Thomas James. School closure in response to epidemic outbreaks: Systems-based logic model of downstream impacts. F1000Res. 2020;9:352. doi: 10.12688/f1000research.23631.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Cooper Marita, Reilly Erin E., Siegel Jaclyn A., Coniglio Kathryn, Sadeh-Sharvit Shiri, Pisetsky Emily M., Anderson Lisa M. Eating disorders during the COVID-19 pandemic and quarantine: an overview of risks and recommendations for treatment and early intervention. Eat. Disord. 2020:1–23. doi: 10.1080/10640266.2020.1790271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356.Brooks S.K., Weston D., Greenberg N. Psychological impact of infectious disease outbreaks on pregnant women: rapid evidence review. Public Health. 2020;189:26–36. doi: 10.1016/j.puhe.2020.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 357.Lemke Michael Kenneth, Apostolopoulos Yorghos, Sönmez Sevil. Syndemic frameworks to understand the effects of COVID-19 on commercial driver stress, health, and safety. J. Transp. Health. 2020;18 doi: 10.1016/j.jth.2020.100877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 358.Estrada Ernesto. COVID-19 and SARS-CoV-2. Modeling the present, looking at the future. Phys. Rep. 2020;869:1–51. doi: 10.1016/j.physrep.2020.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359.Wall Chris, Johnson Theresa, de Steiger Richard. Symptom management for patients awaiting joint replacement surgery. Aust. J. Gen. Pract. 2020;49(7):444–446. doi: 10.31128/AJGP-03-20-5286. [DOI] [PubMed] [Google Scholar]
- 360.Dinleyici Ener Cagri, Borrow Ray, Safadi Marco Aurélio Palazzi, van Damme Pierre, Munoz Flor M. Vaccines and routine immunization strategies during the COVID-19 pandemic. Hum. Vaccin. Immunother. 2020:1–8. doi: 10.1080/21645515.2020.1804776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361.Banakar Morteza, Lankarani Kamran Bagheri, Jafarpour Dana, Moayedi Sedigheh, Banakar Mohammad Hasan, MohammadSadeghi Ashkan. COVID-19 transmission risk and protective protocols in dentistry: a systematic review. BMC Oral. Health. 2020;20(1) doi: 10.1186/s12903-020-01270-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362.Jiwani Safia S., Antiporta Daniel A. Inequalities in access to water and soap matter for the COVID-19 response in sub-Saharan Africa. Int. J. Equity Health. 2020;19(1) doi: 10.1186/s12939-020-01199-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 363.Seale Holly, Dyer Clare E.F., Abdi Ikram, Rahman Kazi M., Sun Yanni, Qureshi Mohammed O., Dowell-Day Alexander, Sward Jonathon, Islam M. Saiful. Improving the impact of non-pharmaceutical interventions during COVID-19: examining the factors that influence engagement and the impact on individuals. BMC Infect. Dis. 2020;20(1) doi: 10.1186/s12879-020-05340-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 364.Budd Jobie, Miller Benjamin S., Manning Erin M., Lampos Vasileios, Zhuang Mengdie, Edelstein Michael, Rees Geraint, Emery Vincent C., Stevens Molly M., Keegan Neil, Short Michael J., Pillay Deenan, Manley Ed, Cox Ingemar J., Heymann David, Johnson Anne M., McKendry Rachel A. Digital technologies in the public-health response to COVID-19. Nat. Med. 2020;26(8):1183–1192. doi: 10.1038/s41591-020-1011-4. [DOI] [PubMed] [Google Scholar]
- 365.Grantz Kyra H., Meredith Hannah R., Cummings Derek A.T., Metcalf C. Jessica E., Grenfell Bryan T., Giles John R., Mehta Shruti, Solomon Sunil, Labrique Alain, Kishore Nishant, Buckee Caroline O., Wesolowski Amy. The use of mobile phone data to inform analysis of COVID-19 pandemic epidemiology. Nature Commun. 2020;11(1) doi: 10.1038/s41467-020-18190-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 366.Salathe Marcel, Bengtsson Linus, Bodnar Todd J., Brewer Devon D., Brownstein John S., Buckee Caroline, Campbell Ellsworth M., Cattuto Ciro, Khandelwal Shashank, Mabry Patricia L., et al. Digital epidemiology. PLoS Comput. Biol. 2012;8(7) doi: 10.1371/journal.pcbi.1002616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367.Charoenwong Ben, Kwan Alan, Pursiainen Vesa. Social connections with COVID-19 affected areas increase compliance with mobility restrictions. Sci. Adv. 2020;6(47):eabc3054. doi: 10.1126/sciadv.abc3054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 368.Hill Terrence D., Gonzalez Kelsey, Burdette Amy M. The blood of christ compels them: State religiosity and state population mobility during the coronavirus (COVID-19) pandemic. J. Relig. Health. 2020;59(5):2229–2242. doi: 10.1007/s10943-020-01058-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369.Hsiehchen D., Espinoza M., Slovic P. Political partisanship and mobility restriction during the COVID-19 pandemic. Public Health. 2020;187:111–114. doi: 10.1016/j.puhe.2020.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 370.Grossman Guy, Kim Soojong, Rexer Jonah M., Thirumurthy Harsha. Political partisanship influences behavioral responses to governors’ recommendations for COVID-19 prevention in the United States. Proc. Natl. Acad. Sci. USA. 2020;117(39):24144–24153. doi: 10.1073/pnas.2007835117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 371.Gollwitzer Anton, Martel Cameron, Brady William J., Pärnamets Philip, Freedman Isaac G., Knowles Eric D., Bavel Jay J. Van. Partisan differences in physical distancing are linked to health outcomes during the COVID-19 pandemic. Nat. Hum. Behav. 2020;4(11):1186–1197. doi: 10.1038/s41562-020-00977-7. [DOI] [PubMed] [Google Scholar]
- 372.Wright Austin L., Sonin Konstantin, Driscoll Jesse, Wilson Jarnickae. Poverty and economic dislocation reduce compliance with COVID-19 shelter-in-place protocols. J. Econ. Behav. Organ. 2020;180:544–554. doi: 10.1016/j.jebo.2020.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 373.Gallotti Riccardo, Valle Francesco, Castaldo Nicola, Sacco Pierluigi, Domenico Manlio De. Assessing the risks of ‘infodemics’ in response to COVID-19 epidemics. Nat. Hum. Behav. 2020 doi: 10.1038/s41562-020-00994-6. [DOI] [PubMed] [Google Scholar]
- 374.Sutton Jeannette, Renshaw Scott L., Butts Carter T. COVID-19: Retransmission of official communications in an emerging pandemic. PLoS ONE. 2020;15(9) doi: 10.1371/journal.pone.0238491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 375.Gozzi Nicolò, Tizzani Michele, Starnini Michele, Ciulla Fabio, Paolotti Daniela, Panisson André, Perra Nicola. Collective response to media coverage of the COVID-19 pandemic on reddit and wikipedia: Mixed-methods analysis. J. Med. Internet Res. 2020;22(10) doi: 10.2196/21597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 376.Hartwell Micah, Greiner Benjamin, Kilburn Zach, Ottwell Ryan. Association of public interest in preventive measures and increased COVID-19 cases after the expiration of stay-at-home orders: A cross-sectional study. Disaster medicine and public health preparedness. 2020:1–5. doi: 10.1017/dmp.2020.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 377.Herren Cristina M., Brownwright Tenley K., Liu Erin Y., Amiri Nisrine El, Majumder Maimuna. Democracy and mobility: A preliminary analysis of global adherence to non-pharmaceutical interventions for COVID-19. SSRN J. 2020 [Google Scholar]
- 378.Kim Eunji, Shepherd Michael E., Clinton Joshua D. The effect of big-city news on rural America during the COVID-19 pandemic. Proc. Natl. Acad. Sci. USA. 2020;117(36):22009–22014. doi: 10.1073/pnas.2009384117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 379.Lee Minha, Zhao Jun, Sun Qianqian, Pan Yixuan, Zhou Weiyi, Xiong Chenfeng, Zhang Lei. Human mobility trends during the early stage of the COVID-19 pandemic in the United States. PLoS One. 2020;15(11) doi: 10.1371/journal.pone.0241468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 380.Xiong Chenfeng, Hu Songhua, Yang Mofeng, Luo Weiyu, Zhang Lei. Mobile device data reveal the dynamics in a positive relationship between human mobility and COVID-19 infections. Proc. Natl. Acad. Sci. USA. 2020;117(44):27087–27089. doi: 10.1073/pnas.2010836117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 381.Vannoni Matia, McKee Martin, Semenza Jan C., Bonell Chris, Stuckler David. Using volunteered geographic information to assess mobility in the early phases of the COVID-19 pandemic: a cross-city time series analysis of 41 cities in 22 countries from March 2nd to 26th 2020. Glob. Health. 2020;16(1) doi: 10.1186/s12992-020-00598-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 382.Kraemer Moritz U.G., Sadilek Adam, Zhang Qian, Marchal Nahema A., Tuli Gaurav, Cohn Emily L., Hswen Yulin, Perkins T. Alex, Smith David L., Reiner Robert C., Brownstein John S. Mapping global variation in human mobility. Nat. Hum. Behav. 2020;4(8):800–810. doi: 10.1038/s41562-020-0875-0. [DOI] [PubMed] [Google Scholar]
- 383.Couture Victor, Dingel AGJH Jonathan, Williams K. 2020. Exposure indices derived from PlaceIQ movement data. [Google Scholar]
- 384.McCoy Liam G., Smith Jonathan, Anchuri Kavya, Berry Isha, Pineda Joanna, Harish Vinyas, Lam Andrew T., Yi Seung Eun, Hu Sophie, Rosella Laura, Fine Benjamin. Characterizing early Canadian federal, provincial, territorial and municipal nonpharmaceutical interventions in response to COVID-19: a descriptive analysis. cmajo Open. 2020;8(3):E545–E553. doi: 10.9778/cmajo.20200100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 385.Cheng Cindy, Barceló Joan, Hartnett Allison Spencer, Kubinec Robert, Messerschmidt Luca. COVID-19 government response event dataset (coronanet v.1.0) Nat. Hum. Behav. 2020;4(7):756–768. doi: 10.1038/s41562-020-0909-7. [DOI] [PubMed] [Google Scholar]
- 386.Cevasco Kevin E., North Hayley M., Zeitoun Sheryne A., Wofford Rachel N., Matulis Graham A., Gregory Abigail F., Hassan Maha H., Abdo Aya D., Farris David, Roess Amira A., von Fricken Michael E. COVID-19 observations and accompanying dataset of non-pharmaceutical interventions across U.S. universities, March 2020. PLoS ONE. 2020;15(10) doi: 10.1371/journal.pone.0240786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 387.Barbieri Diego Maria, Lou Baowen, Passavanti Marco, Hui Cang, Lessa Daniela Antunes, Maharaj Brij, Banerjee Arunabha, Wang Fusong, Chang Kevin, Naik Bhaven, Yu Lei, Liu Zhuangzhuang, Sikka Gaurav, Tucker Andrew, Mirhosseini Ali Foroutan, Naseri Sahra, Qiao Yaning, Gupta Akshay, Abbas Montasir, Fang Kevin, Ghasemi Navid, Peprah Prince, Goswami Shubham, Hessami Amir, Agarwal Nithin, Lam Louisa, Adomako Solomon. A survey dataset to evaluate the changes in mobility and transportation due to COVID-19 travel restrictions in Australia, Brazil, China, ghana, India, Iran, Italy, Norway, South Africa, United States. Data Brief. 2020;33 doi: 10.1016/j.dib.2020.106459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 388.Rosenstock Irwin M. The health belief model and preventive health behavior. Health Educ. Monogr. 1974;2(4):354–386. doi: 10.1177/109019817800600406. [DOI] [PubMed] [Google Scholar]
- 389.Hochbaum G.M. Public Health Service publication, U.S. Department of Health, Education, and Welfare, Public Health Service, Bureau of State Services, Division of Special Health Services, Tuberculosis Program; 1958. Public Participation in Medical Screening Programs: A Socio-psychological Study. [Google Scholar]
- 390.Hayden J. Jones & Bartlett Learning; 2013. Introduction to Health Behavior Theory. [Google Scholar]