Abstract
Although disasters such as pandemics are events that are random in nature, individuals’ vulnerability to natural disasters is inequitable and is shaped by their socioeconomic status (SES). This study examines health inequality by SES amid the COVID-19 pandemic and its underlying mechanisms in Wuhan, China’s epicenter. Using survey data collected in the city during the lockdown period from February 20 to March 6, 2020, we identify two ways in which SES shapes health inequalities—vulnerability and resilience to COVID-19. First, higher SES is associated with a lower risk of infection for both survey respondents and their family members. Second, higher SES reduces mental distress during the pandemic, and this protective effect is particularly strong for individuals who contract the virus or who have family members infected with the disease. Mediation analysis further illustrates that SES shapes the risk of infection and mental distress primarily through three channels: access to daily essential and protective supplies, employment status, and the community environment. These findings lend support to the fundamental cause theory that links socioeconomic differentials to health inequality in a unique context. The outbreak of COVID-19 magnifies pre-existing socioeconomic inequalities.
Keywords: COVID-19, Socioeconomic status (SES), Health inequality, Infection, Mental health
1. Introduction
The outbreak of COVID-19 has caused tens of millions of infections and triggered a global public health crisis. As of February 5, 2021, the COVID-19 pandemic had resulted in more than 104.17 million infections and 2,265,354 deaths across 219 countries and territories around the world (WHO, 2020). Previous studies of natural disasters, such as earthquakes, tsunamis, and forest fires, have demonstrated devastating short- and long-term effects on physical and psychological health (Briere & Elliott, 2000; Corrarino, 2008; Leon, 2004; Mills, Edmondson, & Park, 2007). The COVID-19 pandemic is no exception. In addition to the severe damage that the virus can do to the human body, the fear of infection (combined with economic lockdown and social isolation) has impaired individuals’ psychological well-being and social relationships (Brooks et al., 2020; Dubey et al., 2020; Recchi et al., 2020). For example, even as the pandemic gradually abated in China, many cities have witnessed soaring rates of divorce and suicide (Prasso, 2020; Zhou & Goh, 2020).
Against this backdrop, the present study investigates health disparities evidenced by COVID-19 in Wuhan, China’s epicenter. Previous studies have shown a high correlation between SES and health outcomes (e.g., self-rated health and chronic disease), but empirical studies during disasters or epidemics (e.g., mortality and infection risk) are rare. Of particular concern is the fact that the decision to lock down the city of Wuhan was an unexpected event for all social classes, and no one was adequately prepared in terms of protective or living materials. In this context, all people were affected by the city's closedown, regardless of their SES. As a result, did the association between SES and health inequalities persist during the 72-days lockdown of the city? Specifically, our key research question is: are there socioeconomic disparities in health outcomes associated with the pandemic, as measured by infection risks and mental health distresses? One line of arguments posits that a natural disaster is a potential equalizer because of its universal impact on the population at the same period in time (Aguilar, Pante, & Tugado, 2016; Saguin, 2016). COVID-19 substantially restricts the economic activities of almost everyone regardless of SES (Jones & Jones, 2020). Also, the coronavirus is a threat to every individual because of the natural properties of viral contagion.
Another strand of research, however, contends that natural disasters exacerbate fundamental inequalities due to marked differences in material and non-material resources across socioeconomic groups (Bolin & Kurtz, 2018), that lower SES individuals are less able to buffer themselves against the effects of a disaster than their higher SES counterparts. For example, during and after Hurricane Katrina in the United States, low-income individuals, as opposed to high-income individuals, were less likely to be rescued, more likely to lose their homes, and less likely to regain employment and housing (Brodie, Weltzien, Altman, Blendon, & Benson, 2006; Elliott & Pais, 2006; Elliott, Hite, & Devine, 2009; Fussell, Sastry, & VanLandingham, 2010; Lachlan, Burke, Spence, & Griffin, 2009; Sastry & VanLandingham, 2009). Similar processes will likely unfold during the COVID-19 pandemic, resulting in a heavier burden placed on the shoulders of the disadvantaged (Ahmed, Ahmed, Pissarides, & Stiglitz, 2020; Bowleg, 2020; Lamarque, 2020). Emerging evidence points to an SES-gradient in economic and health outcomes related to COVID-19, such that those on the bottom rungs of the hierarchy ladder are hardest hit (Buchanan, Patel, Rosenthal, & Singhvi, 2020; Finch & Hernández Finch, 2020; Lederer & Kurtenbach, 2020; Pickett, 2020; Recchi et al., 2020).
The fundamental cause theory addresses expectations as to how SES might affect the health outcomes of individuals affected by a disaster such as a pandemic (Link & Phelan, 1995; Lutfey & Freese, 2005). According to this theory, low SES individuals generally exhibit worse health status and higher mortality than their high SES counterparts at almost every stage of the life course (Lutfey & Freese, 2005). This is because SES shapes access to important resources that influence health, including income, knowledge, power, and beneficial social networks.. While it has been well documented that disparities in health outcomes and economic well-being (e.g., by gender, race, ethnicity, and geographic location) are found to be partially attributable to differences in SES across several countries in the current pandemic(Finch & Hernández Finch, 2020; Hu, 2020; Qian & Fan, 2020; Yaya, Yeboah, Charles, Otu, & Labonte, 2020), little empirical research has investigate the mechanism through which SES affects health disparities. The present study is to fill the void.
We proposed two stages in which SES affected health outcomes at the peak of the COVID-19 lockdown in Wuhan, China’s epicenter. In the first stage, we study differential vulnerability to COVID-19 by SES, as measured by infection risk. We speculate that high SES reduces the risk of infection because higher-status individuals are better able to secure resources to shield against viral infections. We specifically explore three underlying channels. First, SES affects access to daily essential and protective supplies, which helps individuals maintain normalcy and stay safe during the pandemic. Second, higher SES individuals tend to hold jobs with greater economic rewards, greater job security, and lower occupational hazards. During the pandemic, they are more likely to retain their jobs and be engaged in work remotely. These conditions reduce exposure to the infection. Finally, higher SES results in a more favorable living environment. Individuals with higher SES tend to live in communities with greater resources and networks, which ease access to supplies and information while minimizing contact with others and potential disease transmission. Taken together, these channels lower the risk of COVID-19 infection.
In the second stage, we examine differential resilience to COVID-19 by SES, as measured by mental health distress, which captures negative emotional effects such as depression, anxiety, or fear. We study the general role of SES in fostering resilience as well as how a protective effect of SES varies by infection status. We speculate a positive relationship between SES and resilience, which operates through three main channels. First, individuals of high SES tend to have greater access to daily essential and protective supplies. This brings a sense of normalcy and security and reduces fear and anxiety that can result from material shortages during the pandemic (Zhang et al., 2020). Second, higher status individuals tend to have greater employment stability and higher monetary rewards than their lower status counterparts, who are at a disproportionate risk for job loss and wage penalties (Hu, 2020; Qian & Fan, 2020). The more sufficient and stable the income, the lower the risk of depression and anxiety (Lei et al., 2020). High SES individuals are also more likely to hold jobs for which remote-work is feasible, which mitigates exposure to and concerns about infection. Finally, higher SES communities may provide more social support and cultivate collective efficacy (Cohen, Finch, Bower, & Sastry, 2006; Miao, Zeng, & Shi, 2021; Qian & Hanser, 2021; Wu, 2021). Such a social environment fosters mental health and resilience during a crisis. In sum, SES has a protective effect on mental health during the pandemic.
The protective effect of SES may be particularly strong among individuals who are infected or are exposed to heightened risks of infection. For those individuals, COVID-19 does take a toll on mental health. However, high-SES individuals are more likely to receive prompt, higher-quality treatment (Harris, 2020), which reduces their psychological distress. Also, these individuals have sufficient financial resources to cover medical and living expenses during hospitalization and quarantine, thereby mitigating financial insecurity. Moreover, high SES individuals tend to live in more spacious homes, thereby reducing the risk of within-family disease transmission and decreasing the mental health burdens of the infected. Therefore, we expect that there will be a larger protective effect of SES on mental health for those who are most vulnerable to mental distress. In other words, the mental distress posed by COVID-19 are greatest among individuals with low SES.
2. Data, variables, and methods
2.1. Data and the study setting
We study disparities in health by SES during the COVID-19 outbreak in Wuhan, where China’s first coronavirus case was confirmed. The government took extreme measures to lock down the entire city from January 23 until April 7. Our data are from the Life Experience and Community during the Covid-19 in Wuhan (LECC-Wuhan). Our survey follows network-based respondent-driven sampling methods. We first recruited 149 college students and faculty members from seven universities in Wuhan, who are referred as “seeds.” These seeds completed online questionnaires and were asked to recruit additional respondents via “one-on-one” private social networking; they were forbidden to recruit unknown others by posting the survey link on any online forum. To be eligible, respondents had to be residents of Wuhan at the time of the survey. To increase diversity, the seeds were asked to refer acquaintances of both sexes and individuals of all ages. Specifically, each seed had to refer the same number of males as females. These participants fell equally into three age categories: 30 years or younger, 30–50 years, and 50 years and older. All of the seeds received interviewer training to ensure that they could assist their recruits in completing the survey. The recruits were encouraged to contact the seeds with any questions during the survey.
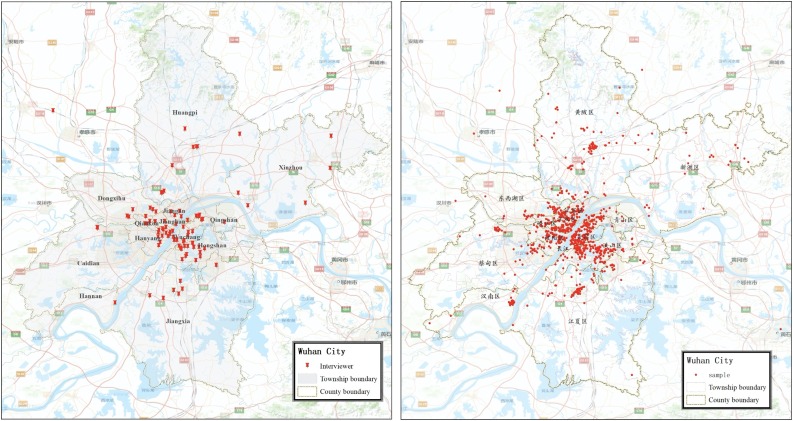
The survey successfully collected data from 4234 respondents. The spatial distribution of seeds and respondents are plotted in Fig. 1 (also see Miao et al., 2021). The timeliness of the survey and the prevalence of infection at the study site allows us to effectively investigate the key research questions. To minimize the potential sampling bias, we used sample weight and random iterative method (RIM) weighting (Miao et al., 2021) in the descriptive analysis (Table 1 ). RIM weighting allows researchers to weigh each variable as an individual entity to ensure that each data point is accurately represented, while keeping the characteristics proportionate as a whole (Miao et al., 2021). Our weighting procedure derives weight factors and applies them to the sample such that the weighted sample matches the two independent distributions, namely, age and education level. We weighted the data according to the demographic characteristics of the 2015 National 1% Population Sample Survey in Wuhan City, and yielded similar results.
Fig. 1.
Spatial Distribution of Interviewers and Interviewees in Wuhan.
Table 1.
Descriptive Statistics for Variables Used in the Analysis (N = 4234).
| Variables | Mean/percentage (unweighted) | Mean/percentage (weighted) |
|---|---|---|
| Tested positive and mental distress variables | ||
| Respondent confirmed/suspected COVID-19 | 1.39 % | 1.58 % |
| Coresident family members confirmed COVID-19 | 4.82% | 5.03 % |
| Respondent/Coresident family members confirmed COVID-19 | 5.22 % | 5.41 % |
| Mental distress | 11.95 (5.51) | 11.88 (5.66) |
| SES variables | ||
| SES | 5.45 (1.81) | 4.19 (1.83) |
| Indicators constructing SES | ||
| Educational attainment | ||
| Middle school and below | 10.20 % | 38.91 % |
| High school | 17.71 % | 23.80 % |
| 3-year college | 20.88 % | 15.43 % |
| Bachelor degree and above | 48.80 % | 21.86 % |
| Occupation | ||
| Managements | 10.68 % | 9.30 % |
| Professionals | 11.31 % | 5.79 % |
| Clerk and office | 5.20 % | 2.42 % |
| Sales and service | 10.53 % | 11.55 % |
| General unskilled workers | 13.89 % | 14.62 % |
| Unemployed/students/retired | 48.39 % | 56.33 % |
| Self-reported class | ||
| Upper class | 9.78 % | 15.40 % |
| Upper middle class | 32.88 % | 36.27 % |
| Middle class | 50.00 % | 42.82 % |
| Lower middle class | 6.75 % | 4.46 % |
| Lower class | 0.59 % | 1.05 % |
| Housing property ownership | 86.51 % | 80.65 % |
| Mediation variables | ||
| Access to daily essential supply | 83.82 % | 82.95 % |
| Access to protective gear supplies | 62.90 % | 63.56 % |
| Work type | ||
| Unemployed/students/retired | 48.39 % | 56.33 % |
| Have job and commute to work | 25.70 % | 27.65 % |
| Have job and work from home | 25.91 % | 16.02 % |
| Neighborhood mutual aid organization | 63.53 % | 62.34 % |
| Neighborhood WeChat group | 82.99 % | 79.43 % |
| Number of services of neighborhood committee | 4.23 (2.43) | 4.12 (2.50) |
| Control variables | ||
| Age | 37.77 (14.72) | 39.09 (16.77) |
| Female | 56.99 % | 47.72 % |
| Married | 57.58 % | 58.24 % |
| Household size | 3.47 (1.28) | 3.60 (1.44) |
| CCP membership | 23.48 % | 14.51 % |
| Wuhan Hukou | 90.41 % | 84.92 % |
| Community lockdown | 89.28 % | 90.51 % |
| Worried about contracting coronavirus | 3.05 (1.27) | 2.98 (1.35) |
Notes: Numbers in parentheses are standard deviations for continuous variables.
2.2. Variables
Health outcomes. The first set of outcome variables measures infection and infection risk. We ask whether respondents had confirmed or suspected COVID-19 infection or were exposed to significant risk of infection. Respondents were asked, "Which of the following categories do you currently belong to?" Choices include healthy, confirmed COVID-19 infection, suspected COVID-19 infection (i.e., individuals awaiting test results), symptomatic of COVID-19 and not ruled out for infection (i.e., individuals who have not yet been tested), and close contact with a confirmed COVID-19 patient. We code healthy respondents as 0 and all other categories as 1 to increase sample size for robust estimates (59 individuals, 1.39 %, are classified as 1).1 For simplicity, we use respondent confirmed/suspected infection to describe these scenarios. The descriptive statistics of all variables included in the analysis are presented in Table 1. In a sensitivity analysis, we restricted the sample to patients with confirmed or suspected infection or who are symptomatic, and we find similar results.
We then asked whether respondents had co-residing family members with confirmed COVID-19 infections; about 4.8 % of respondents reported that they did. Studying the infection of individuals and family members is meaningful because there is a high correlation between individual SES and coresident family members' infection risk. We finally combine the two measures to construct a variable of whether the individual has confirmed or suspected COVID-19 infection, and whether his or her co-residing family members are infected.2 This further increases the sample size as 5.2 % of the respondents or their co-residing family members were diagnosed with coronavirus.
The second outcome variable is mental distress, measured by the Hopkins Symptom Checklist (HSCL-5). HSCL-5 is a validated and widely used assessment of anxiety and depressive symptoms (Schmalbach et al., 2021). The scale consists of five questions about the frequency of several emotional affects in the past week: nervousness or shakiness inside, feeling fearful, feeling blue, worrying too much about things, and feeling hopeless about the future. The response categories are none or little (<1 day), not too much (1–2 days), sometimes (3–4 days), and most of the time (5–7 days). The HSCL-5 is a 5-point Likert scale consisting of five questions that measure two dimensions of mental distress: anxiety and depression. The Cronbach’s alpha of the five items was 0.91, suggesting high reliability. A total score was obtained by summing individual scores on the five items with higher values indicating more severe mental health problems.
Socioeconomic status (SES). We construct a composite measure that captures different aspects of socioeconomic resources: educational attainment, occupation, self-assessed socioeconomic position, and home ownership3 . Educational attainment is measured by the respondent's highest level of education. Occupation is classified into six categories according to 1-digit Chinese Standard Classification of Occupation (CSCO): management, professional, clerical and office, sales and service, general unskilled workers, and unemployed/student/retired. Self-assessed socioeconomic position is classified into five categories: upper class, upper middle class, middle class, lower middle class, and lower class, where respondent were asked directly, "In general, what class does your family's socio-economic status belong to in Wuhan?” Home ownership refers to whether a respondent owned the housing unit he or she occupied in Wuhan at the time of the survey. We use hybrid item response theory (IRT) model to construct an SES scale based on these variables (Ayala, 2009). The hybrid IRT model is used because it can incorporate different types of variables (binary for housing, ordinal for education and self-assessed SES, and nominal for occupation). The SES scale is then converted into a standardized scale with values from 0 to 10.
Mediation variables. We include three sets of mediating variables. The first set pertains to access to daily essential and protective supplies during the pandemic; both are dummy variables. Measures are based on answers to the questions, “Does your household have reliable sources of daily supplies (food, other daily essentials, etc.)?” and, "Does your household have reliable sources of protective gears (masks, disinfection products, etc.)?" The variables are coded 1 if the respondent answered "Yes," and 0 otherwise.
The second set of mediating variables measures the respondent's working status during the pandemic. We indicate whether the respondent has a job and whether he or she works remotely at the time of the interview: 1 represents "unemployed/student/retired," 2 represents "have job and commute to work," and 3 represents "have job and work from home."
The last set of mediating variables captures neighborhood characteristics. We first measure the presence of a residential mutual assistance organization in the respondent's community, which is true for 63 % of the respondents. We create a second variable indicating whether respondents or their family members have joined their community's WeChat online social networking group (83 % of the respondents). Finally, we include a variable measuring the number of services provided by the neighborhood organization, including dissemination of information on infection control, regular update on the number of confirmed cases in the community, daily disinfection reminders, body temperature monitoring, free distribution of supplies such as food and masks, assistance in buying food and medicines for residents in need, arrangements for medical treatment and hospitalization, and counseling services. This is a variable ranging from 0 to 8.
Covariates. We control for a series of covariates, as shown in weighted results in Table 1. The average age of respondents is 39.4 About 57 % of respondents are women, and 58 % of respondents are married. The average household size is 3.6. In addition, 15 % of the respondents are Chinese Communist Party members and 85 % of them have Wuhan hukou. Some 90 % of respondents lived in locked-down communities at the time of the survey. We control for whether the respondent was worried about contracting coronavirus in the mental distress models. This variable is measured by a 5-point Likert scale from least to most worried.
2.3. Empirical strategies
We first use logistic regression models to examine how SES is associated with COVID-19 infection and the risk of infection. We then use OLS linear regression models to study the socioeconomic disparities of individuals reporting mental distress during the pandemic. To address potential endogeneity bias, we conduct additional analyses using seemingly unrelated regressions (SUR) (Zellner, 1962) to jointly model SES and health outcomes, and we obtained similar findings. We report logistic and OLS for the main analyses because they are compatible with the mediation models. Specifically, for mediation analysis, we use the KHB method to decompose the total effect into direct effects and indirect (mediation) effects (Breen, Karlson, & Holm, 2013).
3. Results
3.1. SES disparities in vulnerability to COVID-19
Results are presented in Table 2 . Model 1 is based on whether the respondent was confirmed or suspected as having coronavirus or was exposed to significant risk of infection. We see that, net of the controls, for every unit increase on the SES scale (ranging from 0 to 10), the infection risk declines by 18 %. In principle it would be desirable to disaggregate confirmed or suspected as having coronavirus or was exposed to significant risk of infection, and then carry out a multinomial logistic regression to get more nuanced results but that the small fraction of positive cases (1.39 %) precludes this analysis. In Model 2, higher SES is also associated with a lower risk of infection for respondents' coresident family members (a 10 % reduction). When respondents and their family members are jointly considered (Model 3), the risk is reduced by 12 %. Hence, all three models confirm our hypothesis that SES reduces the risk of COVID-19 infection.
Table 2.
Logistic Regression Models Predicting Different Infection of COVID-19.
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| Respondent confirmed/suspected COVID-19 | Coresident family members confirmed COVID-19 | Respondent/Coresident family members confirmed COVID-19 | |
| SES | −0.199* | −0.107* | −0.130** |
| (0.080) | (0.043) | (0.042) | |
| Age | −0.104† | 0.014 | 0.008 |
| (0.056) | (0.035) | (0.034) | |
| Age2 | 1.049† | −0.160 | −0.148 |
| (0.570) | (0.374) | (0.368) | |
| Female | −0.489† | −0.280† | −0.362** |
| (0.267) | (0.146) | (0.140) | |
| Married | 0.542 | 0.177 | 0.263 |
| (0.456) | (0.251) | (0.243) | |
| Household size | −0.487*** | −0.042 | −0.087 |
| (0.133) | (0.060) | (0.059) | |
| CCP membership | 0.110 | 0.051 | 0.046 |
| (0.337) | (0.182) | (0.176) | |
| Wuhan Hukou | 0.599 | 0.500† | 0.619* |
| (0.530) | (0.286) | (0.286) | |
| Neighborhood lockdown | 0.068 | 0.340 | 0.189 |
| (0.438) | (0.267) | (0.241) | |
| Constant | −0.169 | −3.282*** | −2.689*** |
| (1.401) | (0.832) | (0.804) | |
| Observations | 4234 | 4234 | 4234 |
Notes: Standard errors in parentheses; *** p < 0.001, ** p < 0.01, * p < 0.05, † p < 0.1.
3.2. SES disparities in resilience to COVID-19
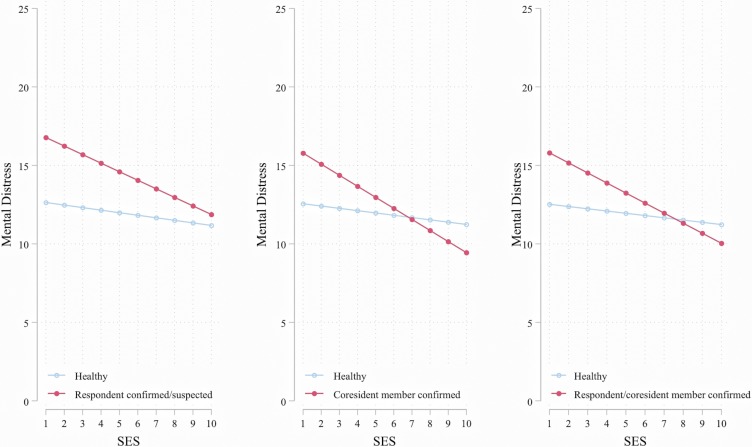
Table 3 presents the results regarding the protective role of SES for mental distress. Model 1 investigates the overall relationship. We see that, net of the other control variables, SES is associated with a large reduction in mental distress for the entire sample. Meanwhile, respondents confirmed or suspected of coronavirus infection experienced heightened anxiety and depression. Models 2–4 in Table 3 examine the moderating role of SES by including interaction terms between SES and infection risk for the respondent, family members, and both. The interaction term is negative for all but is significant for Models 3 and 4. In Model 2, the main effect of SES indicates that, among those who were uninfected or not exposed to heightened risk, the higher the SES, the lower the degree of mental distress. Those stricken with COVID-19 experienced more severe mental distress; among these respondents, the protective effect of SES for mental distress was similar to the effect on those who were healthy. The insignificant interaction may be partly due to the small sample size of respondents who had contracted the virus or were exposed to significant risk of infection (n = 59). Another possible explanation is that the toll a COVID-19 diagnosis takes on an individual’s mental health is so strong that it cannot be offset by greater socioeconomic resources.
Table 3.
Linear Regression Models Predicting Different Resilience to COVID-19.
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Mental Distress | Mental Distress | Mental Distress | Mental Distress | |
| SES | −0.167*** | −0.162** | −0.146** | −0.144** |
| (0.049) | (0.049) | (0.050) | (0.050) | |
| Respondent confirmed/suspected COVID-19 | 2.634*** | 4.525* | ||
| (0.686) | (2.107) | |||
| Respondent confirmed/suspected COVID-19*SES | −0.383 | |||
| (0.403) | ||||
| Coresiding family members confirmed COVID-19 | 3.782** | |||
| (1.173) | ||||
| Coresiding family members confirmed COVID-19*SES | −0.558* | |||
| (0.217) | ||||
| Respondent/Coresiding family members confirmed COVID-19 | 3.774*** | |||
| (1.128) | ||||
| Respondent/Coresiding family members confirmed COVID-19*SES | −0.497* | |||
| (0.210) | ||||
| Age | 0.160*** | 0.161*** | 0.155*** | 0.155*** |
| (0.039) | (0.039) | (0.039) | (0.039) | |
| Age2 | −1.838*** | −1.858*** | −1.792*** | −1.789*** |
| (0.419) | (0.420) | (0.419) | (0.419) | |
| Female | 0.891*** | 0.892*** | 0.887*** | 0.897*** |
| (0.164) | (0.164) | (0.164) | (0.164) | |
| Married | 0.057 | 0.049 | 0.086 | 0.071 |
| (0.278) | (0.278) | (0.278) | (0.278) | |
| Household size | 0.044 | 0.046 | 0.031 | 0.035 |
| (0.065) | (0.065) | (0.064) | (0.064) | |
| CCP membership | 0.205 | 0.199 | 0.215 | 0.213 |
| (0.205) | (0.205) | (0.205) | (0.205) | |
| Wuhan Hukou | 0.153 | 0.153 | 0.154 | 0.137 |
| (0.277) | (0.277) | (0.278) | (0.278) | |
| Neighborhood lockdown | −0.946*** | −0.943*** | −0.960*** | −0.954*** |
| (0.261) | (0.261) | (0.261) | (0.261) | |
| Worried about contracting coronavirus | 1.174*** | 1.175*** | 1.169*** | 1.168*** |
| (0.064) | (0.064) | (0.064) | (0.064) | |
| Constant | 6.197*** | 6.130*** | 6.242*** | 6.193*** |
| (0.911) | (0.914) | (0.911) | (0.911) | |
| Observations | 4234 | 4234 | 4234 | 4234 |
| R-squared | 0.106 | 0.106 | 0.106 | 0.107 |
Notes: Standard errors in parentheses. *** p < 0.001, ** p < 0.01, * p < 0.05, † p < 0.1.
Models 3 and 4 underscore the strong protective effect of SES against mental distress among respondents who tested positive for COVID-19 or had co-residing family members who did. The interaction term is negative and significant, suggesting that SES is particularly salient in buffering mental distress among individuals directly affected by COVID-19. These patterns are illustrated in Fig. 2 . While SES is negatively associated with mental health distress in general, the decline is more pronounced when the respondents or his or her family members are infected. This result points to a larger protective effect of SES on mental health for those who are most vulnerable to mental distress. An alternative way to interpret the interaction term is that the higher the SES, the lower the mental health problems caused by a COVID-19 infection. In other words, the mental health challenges posed by COVID-19 are greatest among individuals with low SES.
Fig. 2.
Predicted Mental Distress by Socioeconomic Status.
3.3. Mediation channels linking SES and COVID-19 risk
To assess the mechanisms through which SES shapes infection and mental health, we turn to the decomposition results in Table 4 . The upper panel corresponds to Model 1 in Table 2. The total effect is very close to Table 2 but not identical because the KHB method uses bootstrap steps. The total effect suggests that higher SES individuals are less likely to contract the virus or be exposed to significant risk of infection. A large proportion of the total effect is channeled through the mediating variables (42 %).
Table 4.
Decomposition of Total Effects into Direct Effect and Indirect Effect.
| Coefficient | Std. Err. | Mediation percentage | |
|---|---|---|---|
| Model 1: Effects of SES on Respondent confirmed/suspected COVID-19 (Logit Model) | |||
| Total effect | −0.196 | (0.082) | |
| Direct effect | −0.114 | (0.084) | |
| Indirect effect | −0.082 | (0.030) | 41.75 % |
| Indirect effect with Bootstrap Std. Err. | −0.081 | (0.032) | 41.75 % |
| via access to daily essential supply | −0.001 | (0.007) | 0.70 % |
| via access to protective gear supplies | −0.014 | (0.007) | 7.12 % |
| via unemployed/students/retired | 0.013 | (0.014) | −6.40% |
| via have job and work from home | −0.044 | (0.029) | 22.47 % |
| via number of services of neighborhood committee | −0.001 | (0.008) | 0.62 % |
| via neighborhood mutual aid organization | −0.014 | (0.008) | 7.15 % |
| via neighborhood WeChat group | −0.020 | (0.009) | 10.08 % |
| Model 2: Effects of SES on Mental Distress (OLS Model) | |||
| Total effect | −0.167 | (0.048) | |
| Direct effect | −0.090 | (0.051) | |
| Indirect effect | −0.078 | (0.019) | 46.44 % |
| Indirect effect with Bootstrap Std. Err. | −0.077 | (0.018) | 46.44 % |
| via access to daily essential supply | −0.020 | (0.006) | 12.23 % |
| via access to protective gear supplies | −0.022 | (0.006) | 13.14 % |
| via unemployed/students/retired | −0.009 | (0.009) | 5.32 % |
| via have job and work from home | −0.004 | (0.016) | 2.41 % |
| via number of services of neighborhood committee | −0.027 | (0.007) | 16.17 % |
| via neighborhood mutual aid organization | 0.005 | (0.005) | −2.77% |
| via neighborhood WeChat group | 0.000 | (0.006) | −0.06% |
We further analyze the respective contribution of each select mediating variable. The results point to three main channels. First, reliable access to daily supplies is an important mediator. This is particularly true for access to protective supplies (7.1 %) relative to access to daily essentials (0.7 %). The second mediating factor is working status. More than 22 % of the SES effect can be attributed to the tendency that high SES individuals are more likely to have a job and be able to work from home during the pandemic, therefore reducing their risk of infection. These individuals are also less likely to be in the unemployed/student/retired category, a group especially vulnerable to infection. But these effects are not statistically significant. Lastly, the effect of SES is channeled through the neighborhood environment (Miao et al., 2021). Higher SES individuals are more likely to have access to neighborhood aid organizations and online community social groups, which may reduce infection risk through resource sharing, information dissemination, and provision of tangible assistance. The number of community services has a relatively small effect.
The lower panel in Table 4 illustrates the mediating mechanisms for the SES effect on mental health. It corresponds to Model 1 in Table 3. The total effect suggests that higher SES individuals are less likely to experience mental health distress during the pandemic. Again, a large proportion of the total effect is channeled through the three domains of mediating factors (46 %). Specifically, about 12 % and 13 % of the effect of SES on mental health is explained, respectively, by more reliable access to daily essential supplies and to protective gear among high-SES individuals. In addition, the working status appears to contribute to 7.3 % of the SES effect on mental health, but it is not significant. Moreover, the neighborhood environment clearly matters. Higher SES individuals are more likely to live in neighborhoods offering a wide range of assistance and services, which in turn reduces mental distress. This pathway accounts for 16.2 % of the total effect. Neighborhood aid organizations and online social groups have relatively limited effects. The coefficients are small and insignificant. One possible explanation is that community networks and organizations may increase anxiety by spreading rumors and negative emotions.
4. Summary and conclusions
This research investigates the impact of SES disparities on infection and mental health during the COVID-19 pandemic in Wuhan, China’s epicenter. Results show that SES shapes both vulnerability and resilience to the pandemic. Higher SES is associated with a lower risk of infection for survey respondents and their co-residing family members. Also, SES shapes health disparities by conditioning mental distress in response to COVID-19 infection, and its role varies by the vulnerability of individuals. The protective effect is especially strong for the most vulnerable, that is, those who are diagnosed with coronavirus or have family members who are. Hence, when individuals of different SES contract the virus, their psychological responses vary substantially: the higher the SES, the better the adjustment and the less severe the emotional problems.
Another contribution of this study is to explore the mechanisms by which SES shapes health inequalities during the pandemic. Mediation analysis demonstrates that the effect of SES operates through three main channels: access to daily essential and protective supplies, job stability and mode of work, and community environment. The health premiums experienced by high SES individuals are largely explained by their more reliable access to daily supplies, greater job stability and flexibility, and greater access to communities that provide tangible and intangible resources and support. Overall, these findings provide further evidence for the fundamental cause theory during a pandemic.
Although a pandemic is random in nature, its impact is not universal. Indeed, natural disasters never play the role of an equalizer; instead, they exacerbate pre-existing social inequalities across class, race, and gender. One important reason is that valuable social resources are the primary way to reduce vulnerability and increase resilience, both in the moment of a natural disaster and in the post-disaster recovery and reconstruction process. But for vulnerable groups, they lack these resources to secure life and carry out post-disaster reconstruction. Therefore, in the aftermath of any disaster, it is necessary for governments to pay special attention to the situation of vulnerable social groups and provide them with sufficient valuable resources to ensure life safety and reduce social inequality. In sum, the outbreak of COVID-19 reproduces existing socioeconomic inequalities that manifest in the realm of health.
Declaration of Competing Interest
The authors report no declarations of interest.
Acknowledgments
The data are from the Life Experience and Community during COVID-19 in Wuhan (LECC-Wuhan), sponsored by the Center for Applied Social and Economic Research (CASER), Hong Kong University of Science and Technology. The authors would like to acknowledge support from the Collaborative Research Fund (C6011-16G) of the Hong Kong Research Grants Council. Direct correspondence to Dr. Xiaoguang Li (xiaoguangli@xjtu.edu.cn) or Dr. Xiaogang Wu (xw29@nyu.edu).
Footnotes
For these individuals, a questionnaire was filled out using a mobile phone in hospital or at home, as long as the person was willing to participate in the survey.
This variable only includes confirmed or suspected cases and does not count those respondent who closely contacted with confirmed cases.
In social stratification studies, education and occupation are the key determinants of an individual's socioeconomic status. Considering the rising importance of housing property in China's social stratification, we added property as an indicator. The inclusion of self-assessed socioeconomic position evaluations helps to further calibrate the socioeconomic status indicator.
For 351 respondents with missing value on the specific year of birth, we imputed age information by taking the midpoint of the cohort reported by the respondents.
References
- Aguilar F.V., Pante M.D., Tugado A.F. Disasters in history and the history of disaster: Some key issues. Philippine Studies Historical and Ethnographic Viewpoints. 2016;64(3–4):641–656. doi: 10.1353/phs.2016.0043. [DOI] [Google Scholar]
- Ahmed F., Ahmed N., Pissarides C., Stiglitz J. Why inequality could spread COVID-19. The Lancet Public Health. 2020;5(5):e240. doi: 10.1016/S2468-2667(20)30085-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayala R.J. Guilford Press; 2009. The theory and practice of item response theory. [Google Scholar]
- Bolin B., Kurtz L.C. Handbook of disaster research. Springer; Cham: 2018. Race, class, ethnicity, and disaster vulnerability; pp. 181–203. [DOI] [Google Scholar]
- Bowleg L. We’re not all in this together: On COVID-19, intersectionality, and structural inequality. American Journal of Public Health. 2020;110(7):917. doi: 10.2105/AJPH.2020.305766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breen R., Karlson K.B., Holm A. Total, direct, and indirect effects in logit and probit models. Sociological Methods & Research. 2013;42(2):164–191. doi: 10.1177/0049124113494572. [DOI] [Google Scholar]
- Briere J., Elliott D. Prevalence, characteristics, and long-term sequelae of natural disaster exposure in the general population. Journal of Traumatic Stress. 2000;13(4):661–679. doi: 10.1023/A:1007814301369. [DOI] [PubMed] [Google Scholar]
- Brodie M., Weltzien E., Altman D., Blendon R.J., Benson J.M. Experiences of Hurricane Katrina evacuees in Houston shelters: Implications for future planning. American Journal of Public Health. 2006;96(8):1402–1408. doi: 10.2105/AJPH.2005.084475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N.…Rubin G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchanan L., Patel J.K., Rosenthal B.M., Singhvi A. The New York Times; 2020. A month of coronavirus in New York City: See the hardest-hit areas. [Google Scholar]
- Cohen D.A., Finch B.K., Bower A., Sastry N. Collective efficacy and obesity: The potential influence of social factors on health. Social Science & Medicine. 2006;62(3):769–778. doi: 10.1016/j.socscimed.2005.06.033. [DOI] [PubMed] [Google Scholar]
- Corrarino J.E. Disaster-related mental health needs of women and children. MCN the American Journal of Maternal/Child Nursing. 2008;33(4):242–248. doi: 10.1097/01.NMC.0000326079.26870.e3. [DOI] [PubMed] [Google Scholar]
- Dubey S., Biswas P., Ghosh R., Chatterjee S., Dubey M.J., Chatterjee S.…Lavie C.J. Psychosocial impact of COVID-19. Diabetes and Metabolic Syndrome Clinical Research and Reviews. 2020;14(5):779–788. doi: 10.1016/j.dsx.2020.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott J.R., Pais J. Race, class, and Hurricane Katrina: Social differences in human responses to disaster. Social Science Research. 2006;35(2):295–321. doi: 10.1016/j.ssresearch.2006.02.003. [DOI] [Google Scholar]
- Elliott J.R., Hite A.B., Devine J.A. Unequal return: The uneven resettlements of New Orleans’ uptown neighborhoods. Organization & Environment. 2009;22(4):410–421. doi: 10.1177/1086026609347184. [DOI] [Google Scholar]
- Finch W.H., Hernández Finch M.E. Poverty and Covid-19: Rates of incidence and deaths in the United States during the first 10 weeks of the pandemic. Frontiers in Sociology. 2020;5(June):1–10. doi: 10.3389/fsoc.2020.00047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fussell E., Sastry N., VanLandingham M. Race, socioeconomic status, and return migration to New Orleans after Hurricane Katrina. Population and Environment. 2010;31(1):20–42. doi: 10.1038/jid.2014.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris A. The Atlantic; 2020. Coronavirus testing: Why rich people get tested.https://www.theatlantic.com/politics/archive/2020/03/coronavirus-testing-rich-people/608062/ March 15, Retrieved from. [Google Scholar]
- Hu Y. Intersecting ethnic and native–migrant inequalities in the economic impact of the COVID-19 pandemic in the UK. Research in Social Stratification and Mobility. 2020;68(June):100528. doi: 10.1016/j.rssm.2020.100528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones B.L., Jones J.S. The Washington Post; 2020. Gov. Cuomo is wrong, COVID-19 is anything but an equalizer.https://www.washingtonpost.com/outlook/2020/04/05/gov-cuomo-is-wrong-covid-19-is-anything-an-equalizer/ Retrieved from. [Google Scholar]
- Lachlan K.A., Burke J., Spence P.R., Griffin D. Risk perceptions, race, and hurricane katrina. Howard Journal of Communications. 2009;20(3):295–309. doi: 10.1080/10646170903070035. [DOI] [Google Scholar]
- Lamarque K. COVID-19 exacerbating inequalities in the US. Lancet. 2020;395(January):1243–1244. doi: 10.1016/S0140-6736(20)30893-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lederer E., Kurtenbach E. The Associated Press; 2020. Pandemic hits poorest hardest as India, Pakistan cases jump.https://www.citynews1130.com/2020/06/04/pandemic-hits-poorest-hardest-as-india-pakistan-cases-jump/ Retrieved from. [Google Scholar]
- Lei L., Huang X., Zhang S., Yang J., Yang L., Xu M. Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-19 epidemic in southwestern China. Medical Science Monitor. 2020;26:1–12. doi: 10.12659/MSM.924609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leon G.R. Overview of the psychosocial impact of disasters. Prehospital and Disaster Medicine. 2004;19(1):4–9. doi: 10.1017/S1049023X00001424. [DOI] [PubMed] [Google Scholar]
- Link B.G., Phelan J. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior. 1995;35(Special Extra Issue):80–94. [PubMed] [Google Scholar]
- Lutfey K., Freese J. Toward some fundamentals of fundamental causality: Socioeconomic status and health in the routine clinic visit for diabetes. The American Journal of Sociology. 2005;110(5):1326–1372. doi: 10.1086/428914. [DOI] [Google Scholar]
- Miao J., Zeng D., Shi Z. Can neighborhoods protect residents from mental distress during the COVID-19 pandemic? Evidence from Wuhan. Chinese Sociological Review. 2021;53(1):1–26. doi: 10.1080/21620555.2020.1820860. [DOI] [Google Scholar]
- Mills M.A., Edmondson D., Park C.L. Trauma and stress response among Hurricane Katrina evacuees. American Journal of Public Health. 2007;97 doi: 10.2105/AJPH.2006.086678. Suppl 1(May) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickett E. 2020. VitaMins: Socioeconomic effects of COVID-19.https://www.clubvita.us/news-and-insights/vitamins-socioeconomic-effects-of-covid-19 Retrieved from. [Google Scholar]
- Prasso S. Bloomberg Businessweek; 2020. China’s divorce spike is a warning to rest of locked-down world.https://www.bloomberg.com/news/articles/2020-03-31/divorces-spike-in-china-after-coronavirus-quarantines March 11, Retrieved from. [Google Scholar]
- Qian Y., Fan W. Who loses income during the COVID-19 outbreak? Evidence from China. Research in Social Stratification and Mobility. 2020;68(June):100522. doi: 10.1016/j.rssm.2020.100522. [DOI] [Google Scholar]
- Qian Y., Hanser A. How did Wuhan residents cope with a 76-day lockdown? Chinese Sociological Review. 2021;53(1):55–86. doi: 10.1080/21620555.2020.1820319. [DOI] [Google Scholar]
- Recchi E., Ferragina E., Helmeid E., Pauly S., Safi M., Sauger N.…Schradie J. The “eye of the hurricane” paradox: An unexpected and unequal rise of well-being during the Covid-19 lockdown in France. Research in Social Stratification and Mobility. 2020;68(May):100508. doi: 10.1016/j.rssm.2020.100508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saguin K.K. States of hazard: Aquaculture and narratives of typhoons and floods in laguna de bay. Philippine Studies Historical and Ethnographic Viewpoints. 2016;64(3–4):527–554. doi: 10.1353/phs.2016.0039. [DOI] [Google Scholar]
- Sastry N., VanLandingham M. One year later: Mental illness prevalence and disparities among New Orleans residents displaced by Hurricane Katrina. American Journal of Public Health. 2009;99(Suppl 3):725–731. doi: 10.2105/ajph.2009.174854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmalbach B., Zenger M., Tibubos A.N., Kliem S., Petrowski K., Brähler E. Psychometric properties of two brief versions of the Hopkins Symptom Checklist: HSCL-5 and HSCL-10. Assessment. 2021;28(2):617–631. doi: 10.1177/1073191119860910. [DOI] [PubMed] [Google Scholar]
- WHO . World Health Organization; 2020. WHO coronavirus disease (COVID-19) dashboard.https://covid19.who.int Retrieved from. [Google Scholar]
- Wu C. Social capital and COVID-19: A multidimensional and multilevel approach. Chinese Sociological Review. 2021;53(1):27–54. doi: 10.1080/21620555.2020.1814139. [DOI] [Google Scholar]
- Yaya S., Yeboah H., Charles C.H., Otu A., Labonte R. Ethnic and racial disparities in COVID-19-related deaths: Counting the trees, hiding the forest. BMJ Global Health. 2020;5(6) doi: 10.1136/bmjgh-2020-002913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zellner A. An efficient method of estimating seemingly unrelated regressions and tests for aggregation bias. Journal of the American Statistical Association. 1962;57(298):348–368. doi: 10.1080/01621459.1962.10480664. [DOI] [Google Scholar]
- Zhang S.X., Liu J., Afshar Jahanshahi A., Nawaser K., Yousefi A., Li J., Sun S. At the height of the storm: Healthcare staff’s health conditions and job satisfaction and their associated predictors during the epidemic peak of COVID-19. Brain, Behavior, and Immunity. 2020;87:144–146. doi: 10.1016/j.bbi.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou W., Goh B. In post-lockdown China, student mental health in focus amid reported jump in suicides. Reuters. 2020 https://www.reuters.com/article/us-health-coronavirus-china-mental-healt/in-post-lockdown-china-student-mental-health-in-focus-amid-reported-jump-in-suicides-idUSKBN23H3J3 June 11, Retrieved from. [Google Scholar]