Abstract
Background
India has the second largest COVID-19 epidemic in the world as per current estimates. Central and peripheral nervous system involvement in COVID-19 (Neuro COVID-19) has been increasingly identified and reported. This letter is the first report of the spectrum of neurological disorders observed in patients with severe COVID-19 from a resource limited setting like India. Till October 30th 2020, Noble hospital and research center, Pune, India has admitted 2631 patients of COVID-19. Out of these, 423 patients had severe COVID-19.
Neurologic complications in severe COVID-19 in Pune, India
Of the 423 patients with severe COVID-19, 20 (4.7%) had pre-existing neurologic co-morbidities, with cerebrovascular disease (8 patients) being the most common. Poliomyelitis (4 patients) was also an important co-morbidity associated with severe COVID-19. Bodyache or myalgia (207/423, 49 %) and headache (59/423, 13.9 %) were the most common neurologic symptoms observed in patients. Encephalopathy (22/423, 5.2 %) and new onset large vessel ischemic stroke secondary to cerebral artery thrombosis (5/423, 1.1%) were the most common secondary neurologic complications noted in our cohort.
Two cases of COVID-19/central nervous system tuberculosis co-infection were also identified.
Challenges in management of Neuro COVID-19 in India
Various challenges like an overwhelmed health care system, inadequate workforce, lack of exhaustive reporting of symptoms and poor availability of neuroimaging in ventilated COVID-19 patients leads to underestimation of Neuro COVID-19 in resource limited settings like India.
Keywords: Neuro COVID-19, India, Cerebrovascular disease, Large vessel ischemic stroke, Encephalopathy, Myalgia, Anosmia, Dysgeusia, Poliomyelitis, COVID-19/Central nervous system tuberculosis co-infection
1. Background
The disease caused by severe acute respiratory syndrome coronavirus 2 was designated as coronavirus disease-2019 (COVID-19) in February 2020, by World Health Organization (WHO) [1]. COVID-19 spread rapidly worldwide, and India was no exception. As of October 30, 2020, there have been more than 8 million confirmed cases and 0.12 million deaths due to COVID-19 in India [2]. India is a lower middle income country, but lags behind only the United States of America (USA) in total COVID-19 case count.
Central and peripheral nervous system involvement in COVID-19 (Neuro COVID-19) has been increasingly identified and reported [[3], [4], [5], [6], [7], [8], [9]]. In this letter, we elucidate unique characteristics and challenges encountered in the management of Neuro COVID-19 by physicians in a tertiary level private hospital in Pune, Western India. Noble hospital and Research Centre (NHRC), Pune provides clinical care, diagnostic, and treatment services to COVID-19 patients since April 2, 2020. Pune is located in the State of Maharashtra and is one of the epicenters of the COVID-19 pandemic in India [2]. Data of all hospitalized patients are entered real time into an electronic database (Lifeline electronic database, Manorama infosystems, Kolhapur, India). It includes hospitalization dates, demographics, co-morbidities, presenting symptoms, clinical examination data, laboratory data, microbiology reports, imaging reports, data on the use of supplemental oxygen, ventilation parameters (noninvasive or invasive ventilation), and hospital outcomes. Till October 30, 2020, NHRC had admitted 2631 patients of COVID-19. Out of these, 423 patients had severe COVID-19. Severe COVID-19 was defined as the presence of clinical signs of pneumonia (fever, cough, dyspnea, and fast breathing) plus one of the following: respiratory rate > 30 breaths/min, severe respiratory distress, or SpO2 < 90% in room air, or acute life-threatening organ dysfunction [10]. Data on neurological comorbidities, neurological symptoms, and secondary complications were obtained from the electronic health record and inpatient case files of each patient by manual abstraction.
2. Neurological comorbidities and neurological symptoms associated with COVID-19
Of the 423 patients with severe COVID-19, 20 (4.7%) had preexisting neurological co-morbidities, with cerebrovascular disease (8 patients) being the most common. Preexisting cerebrovascular disease has been associated with a more severe form of COVID-19 and an increased risk of invasive mechanical ventilation and death [11,12]. Poliomyelitis was the second most common neurological co-morbidity associated with severe COVID-19 (4 patients). The association between preexisting poliomyelitis and severe COVID-19 has not been reported earlier. Alzheimer’s disease (1 patient), Parkinson’s disease (2 patients), psychiatric disorders like Schizophrenia (2 patients), Cerebral palsy (1 patient), Myasthenia Gravis (1 patient), and Epilepsy (1 patient) were the other neurological co-morbidities noted in our cohort. Body ache or myalgia (207/423, 49%), headache (59/423, 13.9%), anosmia (12/423, 2.8%), dysgeusia or hypogeusia (35/423, 8.3%), and lightheadedness or unsteadiness during walking (7/423, 1.65%) were the most commonly observed neurological symptoms in our cohort.
3. Incidence of secondary neurological disease or neurological complications after COVID-19
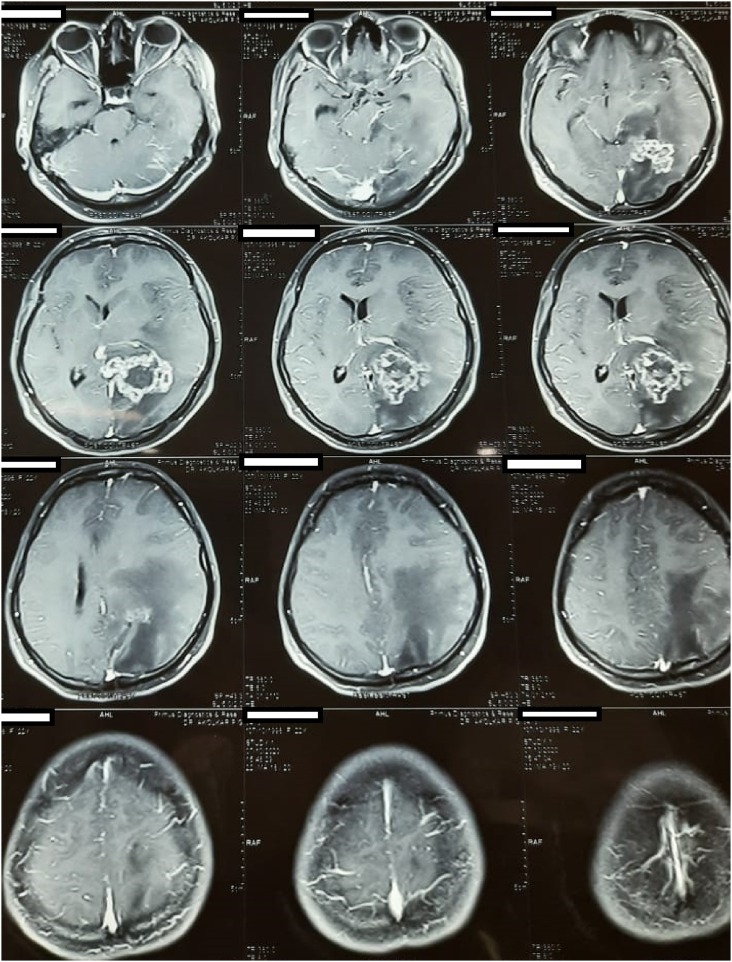
The most common secondary neurological complication seen in patients was Encephalopathy (22/423, 5.2%). Encephalopathy was defined as change in personality, behavior, cognition, or consciousness (including clinical presentations of delirium or coma) in patients without the evidence of brain inflammation [13,14]. A wide variety of causative agents could be responsible for encephalopathy, including the virus, hypoxia, drugs, and metabolic derangements [13]. Out of the 22 patients who developed encephalopathy during hospital admission, only 4 (18.2%) survived. Acute disseminated meningoencephalitis (ADEM, 1/423, 0.2%), large vessel ischemic stroke secondary to cerebral artery thrombosis (5/423, 1.1%), seizures (2/423, 0.4%), intracranial hemorrhage (2/423, 0.4%), acute transverse myelitis (1/423, 0.2%), and Guillain-Barre syndrome (GBS, 1/423, 0.2%) were the other neurological complications observed in our cohort. In addition, two cases of central nervous system tuberculosis (CNS TB) and COVID 19 co-infection have also been identified (Fig. 1 ). Both the patients presented with symptoms of fever, headache, vomiting, and altered sensorium and were found to have COVID-19/CNS TB co-infection. Both of them had mild COVID disease, no evidence of pulmonary involvement due to tuberculosis, and tested seronegative for HIV infection. Cerebrospinal fluid (CSF) examination revealed an elevated protein level, low glucose level (< 40 mg/dL), and lymphocytic pleocytosis. Mycobacterium tuberculosis was identified in the CSF sample of both the patients (Cartridge-based Nucleic acid Amplification test (CB-NAAT), Xpert MTB/RIF Ultra, Cepheid, USA). CSF was not evaluated for COVID-19 in both the instances. The authors believe that the cases of COVID-19/CNS TB co-infection were incidental in a high COVID-19/high TB burden setting [15]. One patient progressed to coma and died, while the other made a complete neurological recovery. There was an association between the development of secondary neurological complications during hospital admission and mechanical ventilation and death, although the direction of this association cannot be determined from the cross-sectional nature of this study.
Fig. 1.
An MRI of the brain (plain plus contrast) showing central nervous system tuberculomas with associated perilesional edema and meningitis in a patient with COVID-19 infection.
4. Challenges associated with the management of neurological complications in COVID-19
An overwhelmed health care system, inadequate workforce, and the lack of exhaustive reporting of symptoms due to relentless pressure to triage patients with severe COVID-19, could be responsible for the lower incidence of neurological symptoms and co-morbidities reported in our cohort. Infrastructure required for the rapid diagnosis of secondary neurological complications like neuroimaging (Magnetic resonance imaging of the brain and spinal cord), nerve conduction studies, and CSF examination is not routinely available in resource limited settings like India, particularly in patients on noninvasive or invasive ventilation leading to the underestimation of the problem. In addition, the availability of a neurologist for bedside or remote assessment through telemedicine is not routinely available for patients admitted in rural settings. Treatment modalities for the management of ADEM and GBS like intravenous immunoglobulin and plasmapheresis are also not routinely available in India.
References
- 1.World health organization (WHO): Available at https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it.
- 2.World health organization (WHO) Coronavirus disease (COVID-19) dashboard. Available at: https://covid19.who.int.
- 3.Beyrouti R., Adams M.E., Benjamin L., Cohen H., Farmer S.F., Goh Y.Y., et al. Characteristics of ischaemic stroke associated with COVID-19. J. Neurol. Neurosurg. Psychiatry. 2020;91(August 8):889–891. doi: 10.1136/jnnp-2020-323586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Varatharaj A., Thomas N., Ellul M.A., Davies N.W.S., Pollak T.A., Tenorio E.L., et al. Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study. Lancet Psychiatry. 2020;7(October 10):875–882. doi: 10.1016/S2215-0366(20)30287-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dixon L., Varley J., Gontsarova A., Mallon D., Tona F., Muir D., et al. COVID-19-related acute necrotizing encephalopathy with brain stem involvement in a patient with aplastic anemia. Neurol. Neuroimmunol. Neuroinflamm. 2020;7(May 5):e789. doi: 10.1212/NXI.0000000000000789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hayashi M., Sahashi Y., Baba Y., Okura H., Shimohata T. COVID-19-associated mild encephalitis/encephalopathy with a reversible splenial lesion. J. Neurol. Sci. 2020;415(August):116941. doi: 10.1016/j.jns.2020.116941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Helms J., Kremer S., Merdji H., Clere-Jehl R., Schenck M., Kummerlen C., et al. Neurologic features in severe SARS-CoV-2 infection. N. Engl. J. Med. 2020;382(June 23):2268–2270. doi: 10.1056/NEJMc2008597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Paterson R.W., Brown R.L., Benjamin L., Nortley R., Wiethoff S., Bharucha T., et al. The emerging spectrum of COVID-19 neurology: clinical, radiological and laboratory findings. Brain. 2020;143(October 10):3104–3120. doi: 10.1093/brain/awaa240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ahmad I., Rathore F.A. Neurological manifestations and complications of COVID-19: a literature review. J. Clin. Neurosci. 2020;77(July):8–12. doi: 10.1016/j.jocn.2020.05.017. Epub 2020 May 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World health organization . 2020. Clinical Management of COVID-19. Interim Guidance.http://WHO-2019-nCoV-clinical-2020.5-eng%20(1)%20(1).pdf 27th May 2020. Available at: [Google Scholar]
- 11.Herman C., Mayer K., Sarwal A. Scoping review of prevalence of neurologic comorbidities in patients hospitalized for COVID-19. Neurology. 2020;95(July 2):77–84. doi: 10.1212/WNL.0000000000009673. [DOI] [PubMed] [Google Scholar]
- 12.Romagnolo A., Balestrino R., Imbalzano G., Ciccone G., Riccardini F., Artusi C.A., et al. Neurological comorbidity and severity of COVID-19. J. Neurol. 2020;4(August):1–8. doi: 10.1007/s00415-020-10123-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berger J.R. COVID-19 and the nervous system. J. Neurovirol. 2020;26(April 2):143–148. doi: 10.1007/s13365-020-00840-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ellul M.A., Benjamin L., Singh B., Lant S., Michael B.D., Easton A., et al. Neurological associations of COVID-19. Lancet Neurol. 2020;19(September 9):767–783. doi: 10.1016/S1474-4422(20)30221-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Prasad R., Singh A., Gupta N. Tuberculosis and COVID-19 in India: challenges and opportunities. Lung India. 2020;37(July-August 4):292–294. doi: 10.4103/lungindia.lungindia_260_20. [DOI] [PMC free article] [PubMed] [Google Scholar]