Abstract
Objectives
This study reports on the readiness of Palestinian dentists to reopen their practices for routine care during the current coronavirus disease 2019 (COVID-19) pandemic.
Methods
A cross-sectional study targeted dentists in the West Bank area of Palestine using an online survey during the first 2 weeks of May 2020. Questions mainly asked about dentists’ perception of the risks of COVID-19, readiness to reopen their clinics for routine care, and the level of confidence in dealing with patients suspected of having COVID-19.
Results
A total of 488 dentists completed the survey. Almost 60% believed that they were not ready to reopen their practices. Almost 13% had “no confidence” in dealing with patients with COVID-19, while 64% had “little to moderate” confidence. Confidence was correlated negatively with increased fear of becoming infected (ρ = -0.317, P < .0001) and positively with years of practice (ρ = 1.7, P < .0001). Dentists who received updated training on infection control or on COVID-19 reported higher levels of confidence (χ2 = 53.8, P < .0001, χ2 = 26.8, P < .0001, respectively). Although 88% preferred not to treat patients with COVID-19, 40% were willing to provide care to them. Almost 75% reported that they were already facing financial hardships and could not survive financially until the end of the current month.
Conclusions
Ethical and financial reasons were the main drivers for dentists in this sample to reopen their practices for routine care. Data from this study highlights the fragility of private dental practice in emergency situations. Ethical, health, and financial challenges that emerged during COVID-19 require dentists to adapt and be better prepared to face future crises.
Key words: COVID-19, Practice management, Dentist, Infection, Coronavirus
Introduction
The world has changed dramatically since coronavirus disease 2019 (COVID-19), a pneumonia-like infectious disease caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was first described in December 2019.1 The COVID-19 outbreak has influenced every aspect of life.2 Within a few months, COVID-19 had spread globally and on March 11, 2020, the World Health Organization (WHO) declared it a pandemic disease.3,4 COVID-19 has the potential to cause severe acute respiratory tract infection in humans and is commonly transmitted from person to person via hands, saliva, nasal droplets, and surface contact.4,5 Common symptoms are those of upper respiratory tract infections but also include high-grade fever, a dry cough, and dyspnoea.6
Current estimates of COVID-19’s case fatality rate suggest that the novel coronavirus is less deadly than severe acute respiratory syndrome (SARS), Middle East respiratory syndrome (MERS), and Ebola.7 However, the infection seems to spread much faster than SARS, MERS, and seasonal influenza.7 The virus's basic reproduction number (R0)—the average number of people one infected person passes the virus to—is comparatively high, with the WHO estimating the R0 in the Middle East to be 2.5-4.5 based on early data.8
At the time of this writing, antiviral vaccines are beginning to become available; however, these are not widely available across the world.4 Therefore, patients have to rely on supportive therapy to relieve the symptoms of the disease until the body's immune system can eradicate the infection.9 Recommendations are that individuals suspected of having contact with an infected person be kept in isolation and under observation until tests for the virus, using real-time polymerase chain reaction (RT-PCR), determine if an infection is present.10
The Centers for Disease Control and Prevention (CDC) in the United States has indicated that certain health care workers, including dentists, are at a “very high” risk of exposure to SARSCoV-2.11 Dentists provide care in a close proximity with patients, and most of dental procedures generate aerosols and droplets.12,13 Dental team members are not only at high risk for infection but also can become potential carriers of the disease and potentially spread it to their peers, families, and other patients. Under these conditions, it is critical that dentists be well-prepared when reopening their dental practices for routine care.
In the Occupied Palestinian Territories (oPt), the first 4 cases of COVID-19 were identified in the Bethlehem area on March 4 after these infected individuals were in contact with a tourist group. At the time of writing, data from the WHO indicates that there have been a total of 1517 confirmed cases and 5 deaths in the oPt. These include 1239 cases and 2 deaths in the West Bank, 206 cases and 2 deaths in East Jerusalem, and 72 cases and 1 death in Gaza.14 Most of people who have been infected by the SARS-Cov-2 virus were males in the 18- to 39-year age bracket.15 The governorates most affected by COVID-19 have been Hebron, Jerusalem, inside and outside the Separating Wall, and followed by Ramallah and Bethlehem.14
The Palestinian government declared a 30-day state of emergency when the first cases were diagnosed early in March and then extended the state of emergency for another 30 days.15 Measures taken included closing schools and universities and establishing border checks for travellers. In a subsequent stage, starting March 22, the government imposed a complete quarantine for 14 days, prohibited movements within the West Bank governorates, and put restrictions of movement on Palestinian workers who entered the green line for work in historical Palestine.15
Based on recommendations from WHO16 and the US Centers for Disease Control and Prevention (CDC)17 and consistent with the practices in many other countries, the Ministry of Health (MOH) restricted the work in private dental clinics to only urgent care. The MOH also closed all of their dental clinics, which provide the majority of dental health services in the area. They deployed MOH dentists to the front lines of the pandemic response, where they provided testing and screening for COVID-19. On April 13, the MOH, in collaboration with the Palestinian Dental Association (PDA), the national professional dental association of dentists practicing in the West Bank area of oPt, released interim infection prevention and control guidelines to dentists working during the pandemic.
On May 28, 2020, after the numbers of infected persons had stabilised, the Palestinian government lifted many restrictions and reopened most aspects of life, including routine and elective care at dental clinics, provided that safety measures for staff and patients were strictly followed. Though dentists were able to provide urgent care during the pandemic, many dentists decided to close their practices on March 22, when the complete lockdown was imposed.15
Guidelines for practicing dentistry during the pandemic were amended for routine dental care by the MOH late in May 2020. These guidelines were tailored from those of the American Dental Association (ADA)18 and prescribed key steps to be taken by dentists to prevent the spread of COVID-19, in addition to the standard universal precautions. The guidelines included measures such as assessing patients’ recent travel history; assessing signs and symptoms of upper respiratory tract infections; recording patients’ body temperature; mouth rinsing with 1% hydrogen peroxide prior to any procedure; using a rubber dam and high volume suction during procedures; and frequently cleaning and disinfecting public contact areas including door handles, chairs, and washrooms.12
Although detailed guidelines were in place and personal protective equipment (PPE) were secured for the long term, many dentists expressed reluctance to practice in such a situation. Therefore, this study assessed Palestinian dentists’ readiness to reopen their clinics for routine care during the COVID-19 pandemic.
Specifically, this study assessed, (i) dentists’ perception of risk of COVID-19; (ii) dentists’ readiness to reopen their private clinics for routine care; and (iii) dentists’ level of confidence in dealing with patients suspected of having COVID-19 and factors related to this confidence level. Secondly, the study assessed (i) dentists’ satisfaction with the MOH's and PDA's role in this pandemic; (ii) dentists’ perception of their own role in pandemic response; and (iii) dentists’ perception of their financial stability during the COVID-19 pandemic. In addition, dentists’ knowledge about various practice modifications to combat the COVID-19 outbreak was evaluated.
Results from this study can be used to help dentists and dental organisations implement proper strategic and long-term measures that can prepare dentists to adapt to any future disruptions in health care practice.
Methods
Study population
The study population consisted of dentists who worked in the West Bank area of Palestine regardless of whether they worked in private clinics, governmental clinics, or other health centres. Due to the current political conditions in the occupied territories, dentists in Gaza were not registered in the MOH or PDA and were not included in this sample. An online questionnaire using Google forms was used to collect the data. The sample of dentists was selected through Facebook groups. Members of PDA created these dentist Facebook groups that were open only to dentists who worked in Palestine and their registration with the PDA and their places of work had to be confirmed to participate. Two main groups were selected: the formal PDA Facebook group that covers all dentists in the target population and the informal PDA Facebook group. Both groups cover all dentists in the West Bank area; however, other smaller dentists’ Facebook groups were also selected to make sure that all dentists were invited to complete the questionnaire. The cover letter accompanying the questionnaire only asked dentists who were still actively providing patient care in any dental settings in the West Bank area to complete the questionnaire.
There were 2700 dentists practicing dentistry in the West Bank area and registered in the Palestinian MOH. To calculate the minimum sample size needed to assess our main outcome variable – readiness of dentists to reopen their dental practices as measured by their level of confidence in treating patients during the pandemic – a margin of error of 5% and a confidence level of 95% were used. In this way, our calculations found that a minimum sample of 336 dentists was needed to adequately represent the population. Dentists were contacted through personal messages and through posts on the Facebook groups’ news feed. The questionnaire was posted on May 7 and stayed open until May 20. Two reminders were posted after 7 and 10 days from the initial contact and one messenger reminder was sent out after 10 days. Response bias was checked by comparing distributions of dentists’ demographic variables such as gender, specialty, and years since graduation between our sample and the whole population of dentists in Palestine based on data available at the MOH and the PDA.
The questionnaire was kept anonymous to maintain the privacy and confidentiality of participants and e-mail accounts were not recorded; and, the “Show link to submit another response” was disabled so as to not to encourage subjects to submit the questionnaire twice. All aspects of this study were approved by Al-Quds University Ethics Committee.
Study instrument
Questions included in the survey were developed after reviewing the relevant literature19,20 and the international guidelines for Infection Prevention and Control Guidance for Dental Settings During the COVID-19 Response.18 The questionnaire was designed in English and then translated to Arabic. The Arabic version was pilot-tested among 25 dentists who were not included in the current sample. The questionnaire was a structured multiple-choice questionnaire that included questions about:
-
1)
Sociodemographic characteristics (Table 1);
-
2)
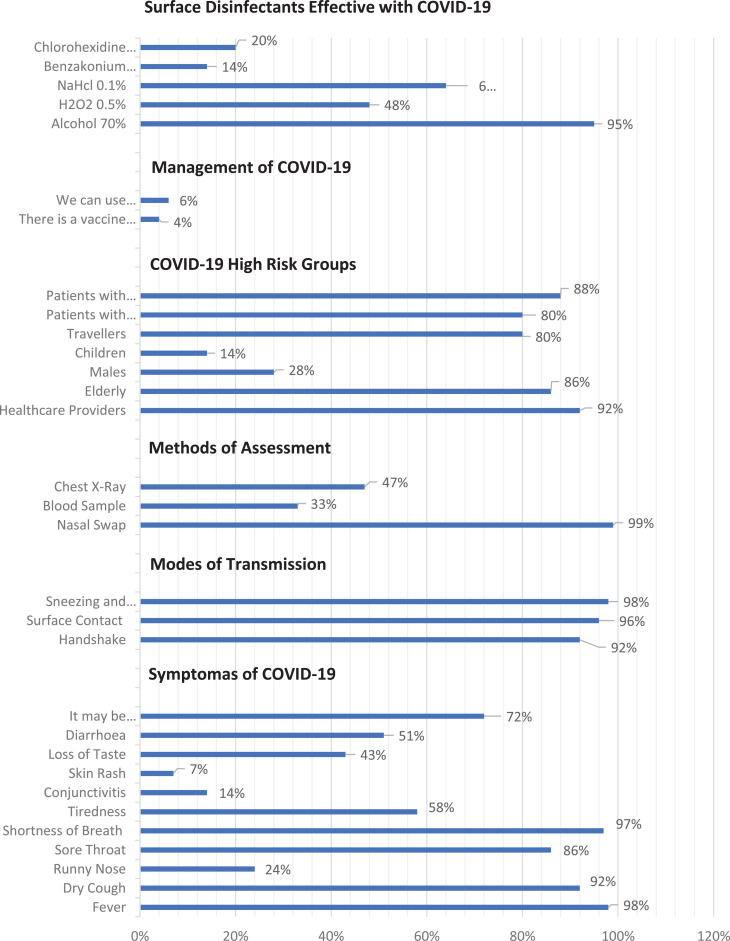
Dentists’ knowledge about COVID-19 (Figure 1);
-
3)
Perception of risk of COVID-19 (Table 2);
-
4)
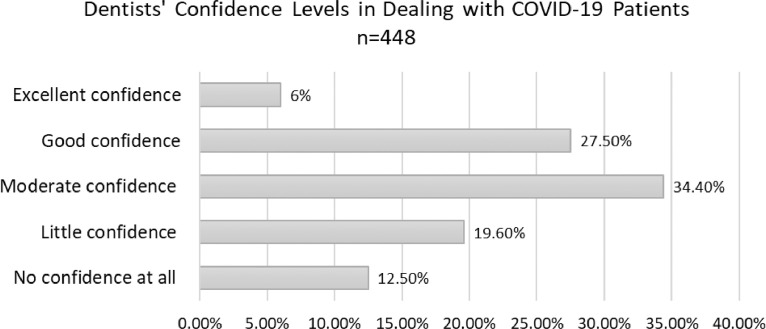
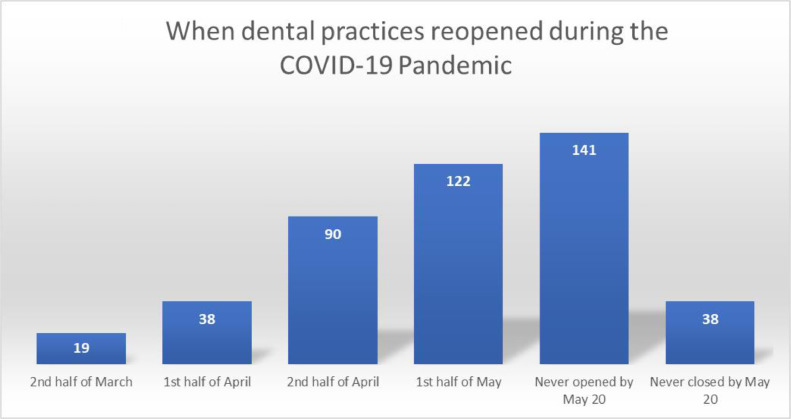
Readiness to reopen private clinics for routine care (Fig. 2, Fig. 3);
-
5)
Perception of MOH and PDA role in this pandemic (quantified by a 5-point scale: 0 = very unsatisfied to 5 = very satisfied);
-
6)
Perception of dentists’ own role in pandemic response, quantified by the 2 questions: (i) As a dentist your role in teaching others about COVID-19 (from 0 = not significant at all to 4 = very significant and (ii) Other than providing urgent care to patients, what role can a dentist play in this pandemic? (a) On the front line with other health care providers in testing and screening, (b) educating the public about COVID-19 and its preventive measure, (c) staying home, social distant, and plan how to practice dentistry safely in the future, and (d) others; and
-
7)
Dentists’ perception of their financial stability during the COVID-19 pandemic quantified by the question: How do you describe your financial status? (a) Stable for the next 6 months, (b) stable for the next 3 months, (c) stable for the next month, and (d) I already face financial problems.
Table 1.
Sample characteristics of dentists in this sample.
| Dentists, N = 448 | Frequency (%) |
|---|---|
| Gender | |
| Females | 197(44) |
| Males | 251(56) |
| Age | |
| ≤30 | 155 (34.6) |
| 30-39 | 207 (46.2) |
| 40-49 | 59(13.2) |
| ≥50 | 27(6) |
| Years of practice | |
| ≤5 years | 148 (33) |
| 6-10 years | 102 (22.8) |
| ≥10 years | 198 (44.2) |
| Type of work settings (check all that apply) | |
| Academics | 38 (8.5) |
| Private practice | 418 (93.3) |
| Government | 24 (5.4) |
| Military services | 5 (1.1) |
| UNRWA | 1 (0.2) |
| Nongovernmental | 14 (3.1) |
| Location of practice | |
| North (Nublus, Qalqilya, Tulkarem, Salfit, Tobas, Jenin) | 106 (23.6) |
| Middle (Jerusalem, Ramallah) | 191 (42.6) |
| South (Bethlehem, Hebron) | 151 (33.7) |
| Dentist education | |
| General | 332 (74.1) |
| Specialist | 116 (25.9) |
UNRWA = United Nations Relief and Works Agency for Palestine Refugees in the Near East.
Fig. 1.
Questions that assessed dentists’ knowledge about coronavirus disease 2019 (COVID-19).
Table 2.
Risk perception of COVID-19 among dentists in this sample.
| Risk perception questions | Frequency (%) |
|---|---|
| How do you perceive COVID-19? | |
| Very dangerous Moderately dangerous |
88 (19.6%) 271 (60.5% |
| Not dangerous | 66 (14.7%) |
| I don't know | 23 (5.1%) |
| How do you perceive COVID-19 compared to severe acute respiratory syndrome (SARS)? | |
| Less dangerous | 188 (42%) |
| More dangerous | 147 (32%) |
| The same | 67 (15%) |
| I don't know | 46 (10.3) |
| How do you perceive COVID-19 compared to Middle East respiratory syndrome (MERS)? | |
| Less dangerous | 146 (32.6%) |
| More dangerous | 128 (28.6) |
| The same | 66 (14.7%) |
| I don't know | 108 (24.1%) |
| COVID-19 symptoms often resolve with time and do not require any special treatment. | |
| Yes | 278 (62.1%) |
| No | 170 (37.9%) |
| I believe COVID-19 is not currently a serious public health issue. | |
| Yes | 355 (79.2%) |
| No | 93 (20.8%) |
COVID-19 = coronavirus disease 2019.
Fig. 2.
Dentists’ confidence level in dealing with patients with coronavirus disease 2019 (COVID-19) during the current pandemic.
Fig. 3.
When dental practices reopened during the coronavirus disease 2019 (COVID-19) pandemic.
Data analysis
Data were analysed using the Statistical Package for Social Sciences (SPSS) version 25.21 Descriptive statistical analysis was used to characterise responses to items included in the survey. Means and standard deviations were used to describe the continuous variables and percentages were used to describe the categorical data. Bivariable analyses using Pearson's χ2 and Spearman's correlation were conducted to relate different predictor variables with our main outcome variable, dentists’ level of confidence in treating patients during the pandemic. These associations were confirmed by using stepwise linear regression models to explain the variation found in our outcome variable. Level of confidence was measured on a 5-point scale, (1: no confidence at all to 5: excellent confidence).
Results
A total of 488 dentists completed the survey, 44% of whom were females (n = 197). Thirty-five percent of our sample (n = 155) were younger than 30 years of age and 44.2% (n = 198) had more than 10 years in dental practice. Ninety-three percent (n = 418) of our sample were dentists in private practice and 74 % (n = 332) were general dentists. Detailed information about the demographic characteristics of the respondents are presented in Table 1. No response bias was detected when demographic variables were compared between our sample and the dentist population working in the West Bank area of Palestine.
Thirty-nine percent (n = 173) of our sample recently received updated training in infection control and 26.6% (n = 119) received special training about COVID-19. The training was mainly online (68%). Fifty-five percent of our sample had this training before an outbreak or a health emergency response; however, only 18.1% (n = 81) had helped in a previous pandemic or health emergency.
At the time of completing the survey, 57% of our sample (n = 257) reported that they were open to treat urgent cases only, while 10.5% (n = 47) reported that they were open and worked as usual. Figure 3 shows the timeline of when the dental practices were planning to reopen.
When responding to questions that assessed dentists knowledge about COVID-19 symptoms and surface disinfection, 62% (n = 280) knew that 1-14 days was the reported incubation period of the virus and 71 (n = 321) knew that there were many cases that were asymptomatic. Ninety five percent (n = 426) thought that 70% alcohol was adequate to disinfect surfaces. Responses regarding dentists’ knowledge is presented in Figure 1.
Questions that assessed COVID-19 risk perception found that 19.6% (n = 88) perceived COVID-19 as very dangerous and 14.7% (n = 66) perceived COVID-19 as not dangerous at all. Almost 81% of our sample (n = 361) reported that they updated themselves regularly about new information. More about risk perception among this sample is found in Table 2.
At time of data collection, 60% of our sample (n = 270) believed that they were not ready to reopen their practices during the current COVID-19 outbreak and 68.5 % (n = 307) believed that their usual infection control practices in their own clinics were inadequate to receive patients in the pandemic. Almost 13% (n = 56) of dentists in our sample had no confidence at all in dealing with patients with COVID-19. Figure 2 shows the confidence level in dealing with COVID-19 patients in our sample.
Confidence level in dealing with patients suspected to have COVID-19 was negatively correlated with increased fear of becoming infected and transmitting the disease to family and friends, (ρ = -0.317, P < .0001). In addition, confidence levels increased in our sample with age (ρ = 1.18, P < .0001) and years of practice (ρ = 1.7, P < .0001). General practitioners and female practitioners had lower confidence levels than specialists and male colleagues (χ2 = 17.8, P = .001, χ2 = 10.1, P = .038, respectively). As expected, dentists who received updated training on infection control or special training on COVID-19 reported higher levels of confidence in dealing with patients suspected of having COVID-19 (χ2 = 53.8, P < .0001, χ2 = 26.8, P < .0001, respectively).
A final regression model (Table 3) explained 32% (R2 = 0.32) of the variation in dentists’ confidence level to treat patients during the pandemic. This model included the following significant predictor variables: having updated training in infection control, having specialised training on COVID-19, self-reported preparedness to the pandemic, fear of infection transmission to family and friends, dentists’ willingness to buy advanced PPE for their clinics, and their perception that their regular PEE is inadequate to treat patients during the pandemic.
Table 3.
Regression model of the outcome variable: dentists’ level of confidence in treating patients during the pandemic.
| Model | Standardized coefficients | t | Sig. |
|---|---|---|---|
| Beta | |||
| (Constant) | 20.00 | .000 | |
| I feel I am ready for COVID-19 pandemic. Yes: 1, No: 2 |
-.314 | -7.49 | .000 |
| I fear that I will transmit the infection to family and friends. (5-point scale, 1: strongly disagree to 5: strongly agree) |
-.223 | -5.49 | .000 |
| I participated in an updated infection control course. Yes: 1, No: 2 |
-.162 | -3.78 | .000 |
| I participated in a course about COVID-19. Yes: 1, No: 2 |
-.126 | -3.03 | .003 |
| I already planned to buy advanced PPE. Yes: 1, No: 2 |
-.107 | -2.71 | .007 |
| I think the regular PPE I used to use in my clinic is inadequate to treat patients during the pandemic. Yes: 1, No: 2 |
-.095 | -2.358 | .019 |
COVID-19 = coronavirus disease 2019; PPE = personal protective equipment.
*Dependent variable: dentists’ level of confidence.
Ninety four percent of our sample (n = 423) agreed that they were afraid of transmitting the infection to family members if they went back to practice. In addition, 88% of the sample preferred not to treat susceptible cases of COVID-19. When asked about treating patients with upper respiratory tract symptoms, 45.8% reported they would refer to the hospital without providing them dental care, 17.9% would treat them first then refer them to the hospital, 18.3% would treat them and then refer them to the closest preventive medicine department, and 18.3% refused to provide them with any care.
In general, 94% of our sample believed that COVID-19 increased the burden in dental practice. Seventy-five percent felt unsafe to use basic PPE during the pandemic and 93% of the dentists planned to purchase more advanced PPE.
At the time of completing the survey, 89.1% of our sample had read the MOH's protocol for providing dental care during the COVID-19 pandemic. Fifty-five percent thought that the protocol was adequate to practice dentistry safely and 56.7% thought it was applicable in their clinics. However, 61.2% agreed that they felt confused about the protocol's procedures. Therefore, 79% of dentists in our sample demanded the MOH and the PDA provide dentists with training on the new protocol, 85% asked for support in getting the right PPE, and 78% demanded updating of the current protocol to reopen dental clinics to routine care.
In the free comments, many dentists asked for better coordination and communication between the MOH, the PDA and the dentists, and many felt they needed some kind of financial support during the pandemic. Fifty-three percent of dentists in our sample reported that they were already facing financial troubles, 22.3% reported they were financially stable until the end of the current month, 13.6% for the next 3 months, and only 10.9% indicated that they could survive financially over the next 6 months.
In general, 90.6% of the dentists were not satisfied with the role of the MOH and the PDA in supporting the dental profession during the pandemic. Sixty-four percent did not agree with the decision of closing the governmental MOH dental clinics and thought clinics should have stayed open to provide urgent care during the pandemic (64%).
Most of the dentists thought that their role in the COVID-19 pandemic was to provide urgent dental care to patients (89.7%), educate others about COVID-19 (82.4%), or work on the front line with other health care providers (52%). Only 40% thought their role was like any other citizen (ie, to stay home and socially distance until they could return and practice safely).
Although there was no call for deployment for dentists at the time, 14% of our sample offered to volunteer with frontline health care providers, 18.8% offered help but there was no need, and 19% reported that they wanted to volunteer but they did not know where to go to offer help.
Discussion
During the pandemic, with some exceptions, all countries recommended that dental care should be limited to emergencies and urgent dental care. At the beginning of the pandemic in China, all 48 public tertiary dental hospitals suspended general nonemergency dental treatment while providing emergency dental services only.22 The British Dental Association (BDA) recommended avoiding all aerosol-generating procedures wherever possible to reduce staff and patient exposure to potential infection.23 The ADA provided a list of dental procedures that were to be considered urgent; these mainly refer to potentially serious conditions and dental or oral pain.18
In general, dentists globally were advised to avoid elective and nonurgent dental care and procedures that produced droplets and aerosols while local restrictive measures were in place. However, by the end of May, most countries, including Palestine, relieved the restrictive measures to allow for elective procedures to resume and dental offices to reopen with increased safety measures for staff and patients. Dentists in Palestine, as all over the world, prepared themselves to return to routine practice with little reliable data on work-related infection risk for dental personnel.
Private dentists constitute the majority of dental care providers in Palestine and they mainly practice in solo clinics located in the commercial centres of big cities.
The majority of dentists in our sample did not agree with closing all MOH dental clinics and felt that they were left isolated to face the ethical dilemma of providing the best possible care to patients while keeping themselves and their staffs safe in the workplace. At the same time, as business owners, they were facing a financial impact from loss of income resulting from service limitations. In general, dentists in this sample felt they needed more support from the government and their professional association, the PDA, to guide them through a period of uncertainty for which none of them were prepared.
In our sample, 47% of dental clinics reopened in the second half of April or first week of May and 31% were still closed. In the United Kingdom, dental clinics were informed by the BDA that they could reopen starting June 8, if appropriate safety measures were in place. A poll of 2053 practices in England suggested that slightly more than one-third (36%) planned to reopen on June 8.24 In the United States, 40 states had allowed for reopening for elective dental services by the week of May 18, and of these, 21 of the states reopened with no restrictions other than additional PPE. In the 27 states that had reopened by the end of April, the patient rebound reached 54% of pre-COVID-19 levels.25
In the current study, 75.4 % of dentists in our sample reported that they were already facing financial troubles or were able to maintain their financial stability only until the end of the current month. In a survey conducted by the BDA for UK dentists in mid-March, 70% of dental clinics reported they could only remain financial stable for 3 months or less.26 In Germany, an economic analysis showed that COVID-19 and associated policies had profound economic effect on dental practices and urged policy makers to consider dentists in governmental subsidy and safety net programs.27
In our sample, financial drivers seem to be strong motivators to reopen dental clinics. At the time of completing the survey, although 60.3% reported that they were not ready to address the COVID-19 outbreak and 76% had “no” or “little to moderate” confidence in their ability to deal with patients with COVID-19, more than half of the practices were open for urgent care and 10.5% were open for all types of care. Our data indicates that this low level of confidence was mainly related to dentists’ fear of becoming infected or transmitting the infection to family and friends.
In general, dentists in this sample preferred to refer patients with upper respiratory tract (URT) symptoms to the hospital, rather than treat them in their offices. Ninety-four percent of dentists in our sample were afraid of transmitting infection to family and friends. This was similar to how Turkish dentists felt when asked a similar question, where 95% were concerned about carrying the virus to their families.28 In Jordan, despite no local cases of COVID-19 at the time, the vast majority of dentists (82.6%) preferred to avoid working with a patient who was a suspected of having COVID-19.20 In general, studies across the world that assessed attitudes towards practicing dentistry during the COVID-19 pandemic reported overwhelming feelings of fear, confusion, and anxiety among dental professionals because dentistry was viewed as a high-risk profession for transmitting infection to family and friends.29, 30, 31, 32
An earlier clinical study from Wuhan, China, showed that 29% of 138 hospitalized patients with 2019-nCoV-infected pneumonia were health care team members.33 In the United States, an ADA bimonthly poll on May 18 indicated that among owner dentists whose practices were not open for elective care, 28% reported the reason was dental team members’ hesitation to return to practice and 34% reported unclear guidance for reopening their practices.25
In our sample, 69% agreed that they were not sure of how to implement the new MOH infection prevention and control protocol and 79% demanded the MOH and the PDA provide dentists with training on the new protocol. On the other hand, almost 18% of dentists took self-initiative and used online training materials on COVID-19 from international organisations to update their knowledge on this matter. This compared to 7.6% of Jordanian dentists21 and 26.6% among Turkish dentists.28 Training on updated infection control measures and COVID-19 response measures increased the level of confidence in this sample in dealing with patients suspected of having COVID-19. These results suggest that it is imperative that information sessions about COVID-19 and training on the new infection control protocols during the pandemic should be intensified and be the responsibility of the MOH and PDA.
The confusion about implementing the new protocol about providing dental care during the pandemic was evident in patients’ referral when suspected of having a URT infection. Although the MOH protocol clearly indicated that patients with URT infections need to be screened, and if symptoms conform with COVID-19, be referred to the department of preventive medicine rather than hospitals, 18% in our sample would provide patients with dental care and refer them to hospital afterwards, while 45.8% would refer to hospital without providing dental care. This is similar to Jordanian dentists, where 43.8% would refer the patient to the hospital without treating patients with URT symptoms.20
In the current study, although 88% preferred not to deal with patients with COVID-19, 40% indicated their willingness to provide dental care to patients with URT symptoms. This suggests that many dentists felt ethically obligated to offer help and guidance to those patients.
In general, despite the feeling of discomfort, fear, and the need for more training, almost all dentists in this sample were ready to adhere to the new guidelines and already planned the purchase of new necessary PPE.
The majority of dentists in this sample reported that they updated their information about COVID-19 regularly and 82% felt that they were obliged to educate their patients about COVID-19. This compared to 83% of Turkish dentists28 and 97.8% of Jordanian dentists20 who also thought that dentists were qualified and responsible for educating others about COVID-19 to prevent its spread.
Knowledge about COVID-19 among this sample was very good, with 60%-90% of dentists reporting the correct incubation period, COVID-19 symptoms, high-risk populations, and the best agents to disinfect surfaces in the dental clinic. This knowledge was developed over 50 days of quarantine in the months of March, April, and May, when more information about COVID-19 and how to minimise its transmission were emerging. There was, however, a lack of knowledge among the current sample in identifying loss of taste as a symptom of COVID-19 because only 43% indicated this among the symptoms list. This may be because that the first study to link loss of taste and smell to COVID-19, based on empirical data, was published in mid-April.34 In general, the literature found that knowledge about respiratory diseases and their causative agents was lower in dentists35 than other health care providers.19 In light of the current pandemic, this finding is alarming and suggests that efforts should be made to improve dentist's knowledge about respiratory diseases. Dental professionals spend most of their clinical encounters in close proximity to patients, and dental procedures are among the highest in generating aerosols.36
The dental literature indicates that many dental restorative procedures produce aerosols and droplets that are contaminated with disease causative agents that are considered potential routes for disease transmission.37 In addition to the routine use of standard barriers such as masks and gloves, rubber dams, preprocedural rinses, and high-volume evacuation, the philosophy of treatment needs to shift from heavily emphasising restorative care to focused on prevention. Focusing on educating patients to care for their teeth at home, wide use of fluorides, promotion of healthy diets, and regular visits the dentist would eventually minimise the need for emergency care in crisis times.37 Moreover, switching away from aerosol-generating procedures, such using nonrestorative treatment options to manage dental caries such as fissure sealants, fluoride varnish, resin infiltration, and silver diamine fluoride (SDF) for cavitated and noncavitated lesions may be an appropriate strategy to minimise the risk of infection in dental settings.38 Atraumatic restorative treatment (ART)39 and the Hall technique40 are also good candidates to minimise aerosol generation in dental settings.
Results of this study highlighted an important point about how dentistry works in isolation and is distant from other health care providers. A majority of dentists in this sample felt that their main role in the pandemic was providing urgent dental care to their patients, and they did not see themselves working on the front lines of the pandemic, nor were they were eager to volunteer to do so. Dentists in this sample rarely participated in any pandemic response efforts, did not attempt to update themselves regularly about emergency preparedness, and only 58% of them indicated that they referred to their medical colleagues as a source of information about COVID-19. Dentistry has traditionally focused almost exclusively on the restorative and rehabilitation model of care instead of promoting the health and the well-being of individuals, leaving dentists with limited ability to respond to or be fully used in a major health crisis.41
This study was a simple descriptive cross-sectional study that described dentists’ perception of their ability to deal with this pandemic at one point in time. Issues are changing dramatically in this pandemic as new information about the nature of this disease is emerging and the government's response, based on the number of new cases, is changing accordingly.
Although we believe that our sample was a good representation of the majority of dentists practicing dentistry in the West Bank area of Palestine, using social media groups and forums as sampling frame may bias our results because not all dentists were active on those platforms.
Although dentists in this sample were not confident of their readiness to go back to practice due to the COVID-19 pandemic, they already reopened, or were planning to reopen soon for routine dental care. Their ethical obligation to their patients and their financial situation pushed them to make such decisions. Dentists in this sample felt that more support from the government and their professional association were needed. Dentistry was not included in the first response preparedness for the pandemic, and it took some time before the government focused on issues related to dental clinics.
Conclusion
Although the main goal of this study was to assess readiness of dentists in our sample to return to dental practice, current data give us the chance to think about what we have learned about members of the dental profession, the system, and patients in this pandemic. Data in this study highlight the fragility of private dental practice in emergencies and the constrains that a restorative model of dental practice places on dentists in terms of working with other health workers.
Ethical, health, and financial challenges that emerged during COVID-19 require us to start a dialogue about these issues to be better prepared in the future. The future holds the challenge to better integrate dental care with primary and specialty medical care. Such integration will assure that oral health will be addressed as an important part of the overall health of individuals and will not be ignored. However, such integration will also require changes in the practice of dentistry, which may include more holistic approaches to patients’ overall and oral health and a willingness to consider alternative or nontraditional treatment modalities.
Data from this study should be used by dentists, their professional association, and governments to better address oral health as a priority that needs to be included in any crisis response and that dentists need to be supported to better provide optimum and safe care to their patients.
Acknowledgments
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
None disclosed.
References
- 1.World Health Organization (WHO). Coronavirus disease (COVID19) outbreak. Available from: https://www.who.int/emergencies/diseases/novelcoronavirus-2019. Accessed 30 May 2020.
- 2.Gralinski LE, Menachery VD. Return of the coronavirus: 2019-nCoV. Viruses. 2020;12:135. doi: 10.3390/v12020135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Neher RA, Dyrdak R, Druelle V. Potential impact of seasonal forcing on a SARS-CoV-2 pandemic. Swiss Med Wkly. 2020;150:w20224. doi: 10.4414/smw.2020.20224. [DOI] [PubMed] [Google Scholar]
- 4.Khurshid Z, Asiri FYI, Al Wadaani H. Human saliva: non-invasive fluid for detecting novel coronavirus (2019-nCoV) Int J Environ Res Public Health. 2020;17:2225. doi: 10.3390/ijerph17072225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peng X, Xu X, Li Y, et al. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020;12:1–6. doi: 10.1038/s41368-020-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guan W, Ni Z, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Callaway E, Cyranoski E, Mallapaty S. The coronavirus pandemic in five powerful charts. Nature. 2020;579:482–483. doi: 10.1038/d41586-020-00758-2. [DOI] [PubMed] [Google Scholar]
- 8.Ahmed A, Salam B, Mohammad M, et al. Analysis coronavirus disease (COVID-19) model using numerical approaches and logistic model. AIMS Bioengineering. 2020;7(3):130–146. doi: 10.3934/bioeng.2020013. [DOI] [Google Scholar]
- 9.Zhang L, Liu Y. Potential interventions for novel coronavirus in China: a systematic review. J Med Virol. 2020;92(5):479–490. doi: 10.1002/jmv.25707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Corman VM, Landt O, Kaiser M, et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020;25:1–8. doi: 10.2807/1560-7917.ES.2020.25.3.2000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ran L, Chen X, Wang Y, et al. Risk factors of healthcare workers with corona virus disease 2019: a retrospective cohort study in a designated Hospital of Wuhan in China. Clin Infect Dis. 2020;71(16):2218–2221. doi: 10.1093/cid/ciaa287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ather A, Patel B, Ruparel NB, et al. Coronavirus disease 19 (COVID-19): implications for clinical dental care. J Endod. 2020;46(5):584–595. doi: 10.1016/j.joen.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meng L, Hua F, Bian Z. Coronavirus disease 2019 (COVID-19): emerging and future challenges for dental and oral medicine. J Dent Res. 2020;99(5):481–487. doi: 10.1177/0022034520914246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization (WHO). Eastern Mediterranean regional office country reports. Updates on coronavirus disease 2019 (COVID-19) in oPt. Available from: http://www.emro.who.int/countries/pse/index.html. Accessed 20 May 2020.
- 15.Al Khaldi M, Kaloti R, Shella D, et al. Health system's response to the COVID-19 pandemic in conflict settings: policy reflections from Palestine. Glob Public Health. 2020;15(8):1244–1256. doi: 10.1080/17441692.2020.1781914. [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization (WHO). Infection prevention and control during health care when novel coronavirus (nCoV) infection is suspected. Interim guidance. Available from: https://www.who.int/publications/i/item/10665-331495. Accessed 30 May 2020.
- 17.Centers for Disease Control and Prevention (CDC). Interim infection prevention and control guidance for dental settings during the COVID-19 response. Available from:https://www.cdc.gov/coronavirus/2019-ncov/hcp/dental-settings.html. Accessed 20 June 2020.
- 18.American Dental Association. ADA interim guidance for management of emergency and urgent dental care. Available from:https://success.ada.org/en/practice-management/patients/safety-and-clinical?utm_source=cpsorg&utm_medium=covid-nav&utm_content=nav-safety-clinical&utm_campaign=COVID-19. Accessed 10 May 2020.
- 19.Abolfotouh MA, AlQarni AA, Al-Ghamdi SM, et al. An assessment of the level of concern among hospital-based health-care workers regarding MERS outbreaks in Saudi Arabia. BMC Infect Dis. 2017;17:4. doi: 10.1186/s12879-016-2096-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Khader Y, Al Nsour M, Al-Batayneh OB, et al. Dentists’ awareness, perception, and attitude regarding COVID-19 and infection control: cross-sectional study among Jordanian dentists. JMIR Public Health Surveill. 2020;6(2):e18798. doi: 10.2196/18798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.IBM Corp . IBM Corp; Armonk, NY: 2017. IBM SPSS statistics for Windows, version 25.0. [Google Scholar]
- 22.Yang Y, Zhou Y, Liu X, Tan J. Health services provision of 48 public tertiary dental hospitals during the COVID-19 epidemic in China. Clin Oral Investig. 2020;24(5):1861–1864. doi: 10.1007/s00784-020-03267-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.British Dental Association (BDA). BDA issues urgent advice to dentists. Available from: http://bda.org/advice/Coronavirus/Pages/latest-updates.aspx. Accessed 15 May 2020.
- 24.Tom Edgington. Coronavirus: no return to 'business as usual' for dentists. BBC News. Available from: https://www.bbc.com/news/health-52913826. Accessed 1 June 2020.
- 25.American Dental Association Health Policy Institute. COVID-19 economic impact on dental practices. Available from:https://www.ada.org/en/publications/ada-news/2020-archive/may/hpi-polling-shows-dental-practices-recovering-as-states-reopen?&utm_source=social&utm_medium=twitter&utm_content=cv-hpi-view-poll-results&utm_campaign=COVID-19. Accessed 7 June 2020.
- 26.British Dental Association (BDA). Practices weeks from collapse without rapid action from government. Available from:https://bda.org/news-centre/press-releases/Pages/Practices-months-from-collapse-without-rapid-action-from-UK-government.aspx. Accessed 10 May 2020.
- 27.Schwendicke F, Krois J, Gomez J. Impact of SARS-CoV2 (COVID-19) on dental practices: economic analysis. J Dent. 2020;99 doi: 10.1016/j.jdent.2020.103387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Duruk G, Gümüşboğa ZŞ, Çolak C. Investigation of Turkish dentists’ clinical attitudes and behaviors towards the COVID-19 pandemic: a survey study. Braz Oral Res. 2020;34:e054. doi: 10.1590/1807-3107bor-2020.vol34.0054. [DOI] [PubMed] [Google Scholar]
- 29.Mijiritsky E, Hamama-Raz Y, Liu F, et al. Subjective overload and psychological distress among dentists during COVID-19. Int J Environ Res Public Health. 2020;17(14):5074. doi: 10.3390/ijerph17145074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gambarini E, Galli M, Di Nardo D, et al. A survey on perceived COVID-19 risk in dentistry and the possible use of rapid tests. J Contemp Dent Pract. 2020;21(7):718–722. [PubMed] [Google Scholar]
- 31.Tysiąc-Miśta M, Dziedzic A. The Attitudes and professional approaches of dental practitioners during the COVID-19 outbreak in Poland: a cross-sectional survey. Int J Environ Res Public Health. 2020;17(13):4703. doi: 10.3390/ijerph17134703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Martina S, Amato A, Rongo R, Caggiano M, Amato M. The perception of COVID-19 among Italian dentists: an orthodontic point of view. Int J Environ Res Public Health. 2020;17(12):4384. doi: 10.3390/ijerph17124384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yan CH, Faraji F, Prajapati DP, et al. Association of chemosensory dysfunction and COVID-19 in patients presenting with influenza-like symptoms. Int Forum Allergy Rhinol. 2020;10(7):806–813. doi: 10.1002/alr.22579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Baseer M, Ansari S, AlShamrani S, et al. Awareness of droplet and airborne isolation precautions among dental health professionals during the outbreak of corona virus infection in Riyadh city, Saudi Arabia. J Clin Exp Dent. 2016;8(4):e379–e387. doi: 10.4317/jced.52811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Harrel SK, Molinari J. Aerosols and splatter in dentistry: a brief review of the literature and infection control implications. J Am Dent Assoc2004;135(4):429-37. [DOI] [PMC free article] [PubMed]
- 37.Sun BC, Chi DL, Schwarz E, et al. Emergency department visits for nontraumatic dental problems: a mixed-methods study. Am J Public Health. 2015;105(5):947–955. doi: 10.2105/AJPH.2014.302398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Slayton R, Urquhart O, Araujo MW, et al. Evidence-based clinical practice guideline on nonrestorative treatments for carious lesions: a report from the American Dental Association. J Am Dent Assoc. 2018;149(10) doi: 10.1016/j.adaj.2018.07.002. 837-49.e19. [DOI] [PubMed] [Google Scholar]
- 39.de Amorim RG, Frencken JE, Raggio DP, et al. Survival percentages of atraumatic restorative treatment (ART) restorations and sealants in posterior teeth: an updated systematic review and meta-analysis. Clin Oral Investig. 2018;22(8):2703–2725. doi: 10.1007/s00784-018-2625-5. [DOI] [PubMed] [Google Scholar]
- 40.Badar SB, Tabassum S, Khan FR, Ghafoor R. Effectiveness of Hall technique for primary carious molars: a systematic review and meta-analysis. Int J Clin Pediatr Dent. 2019;12(5):445–452. doi: 10.5005/jp-journals-10005-1666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ren YF, Rasibala L, Malmstrom H, Eliav E. Dental care and oral health under the clouds of COVID-19. JDR Clin Trans Res. 2020;5(3):202–210. doi: 10.1177/2380084420924385. [DOI] [PubMed] [Google Scholar]