Abstract
Knowledge of lateral nasal wall landmarks in relation to lacrimal apparatus is essential for successful endoscopic dacryocystorhinostomy. This descriptive study of right and left sagittally sectioned ten adult cadaver head specimens was done measuring various lateral nasal wall anatomical landmarks including lacrimal apparatus with digital calipers. Maxillary line was identified in 75%, majority overlapping lacrimal sac. Genu of middle turbinate was at or posterior to nasolacrimal duct. Mean distance of superior end of sac was 8.88 mm above axilla, between its anterior edge and axilla was 10.58 mm and its length was 11.72 mm. Considering above measurements, ‘Rule of 10’ can be applied for nasal mucosal incision. A “Three Tier Approach” to overcome mucosal (nasal), bony (lacrimal and frontal process of maxilla) and mucosal (sac) boundaries exposes lacrimal sac up to its inferior limit ensuring successful endonasal endoscopic dacryocystorhinostomy.
Keywords: Dacryocystorhinostomy, Lacrimal apparatus, Nasolacrimal duct, Cadaver, Lacrimal apparatus diseases
Introduction
The knowledge of the intranasal anatomy relating to the lacrimal apparatus is fundamental to a successful dacryocystorhinostomy (DCR) [1]. Precise placement of initial mucosal incision followed by lacrimal osteotomy is of prime importance. A comprehensive knowledge of the surgical anatomy of lateral nasal wall and adjoining lacrimal system is mandatory [2].
The landmarks reported in the lateral nasal wall as guide for endonasal DCR are axilla, maxillary line and M point. Axilla which is the anterior most attachment of the middle turbinate to the lateral nasal wall is reported as one of the most relevant reference landmark. The maxillary line a curvilinear, mucosal eminence from axilla to dorsum of inferior turbinate [3, 4]. M point which is the midpoint of the maxillary line in the axial plane, marks the level of the superior aspect of the maxillary sinus ostium posteriorly, and the junction of the lacrimal sac and the nasolacrimal duct (NLD) anteriorly [3].
This manuscript describes the anatomy of nasolacrimal apparatus in relation to these landmarks in the lateral nasal wall by cadaveric dissection, so as to facilitate the surgeon a simple and systematic approach to lacrimal sac with a three-dimensional anatomy of the nasolacrimal system as a prelude to endoscopic DCR.
Materials and Methods
Study Design
It was a descriptive study of cadaver dissection in which data collection was done by measurement of anatomical landmarks in cadaver sagittal head sections. It was done following clearance from Institutional Review Board (IRB Min. No. 7339, Christian Medical College, Vellore, Tamil Nadu, India).
Participants
Ten Indian adult cadaver’s head sections (10 right and 10 left sagittally sectioned specimens) fixed with 10% formaldehyde solution.
Setting
Anatomy and ENT departments of a tertiary hospital.
Methods
Ten adult cadaver’s head sections were sagittally sectioned. This was followed by dissection of nasolacrimal system on each sagittal head section. Digital calliper (Fig. 1) was used to measure distances on dissection. During the dissection, the maxillary line was determined by retraction of the middle turbinate superiorly. An incision was made and mucoperiosteal flap elevated to expose the lacrimomaxillary suture. The relation between the maxillary line and lacrimomaxillary suture was noted. As a next step, NLD and lacrimal sac (LS) were dissected by the removal of the lacrimal bone (posterior to the lacrimomaxillary suture) and the frontal process of maxilla (anterior to the lacrimomaxillary suture). The relation of lacrimal bone to the LS was also noted. In cadavers’ heads agger nasi were noted and had to be excised to expose LS. The maxillary sinus ostium was then exposed by removing the uncinate process. Part of inferior turbinate was excised to expose NLD. This completed exposure of the nasolacrimal system.
Fig. 1.

Digital calliper
The features/dimensions noted on cadaveric dissection were tabulated in Tables 1 and 2, Fig. 2.
Table 1.
Relations
| Maxillary line | Clear | Not clear |
| 15(75%) | 5(25%) |
| Relation of maxillary line to lacrimomaxillary suture line: (anterior/posterior/over) | ||
| Anterior | Posterior | Over |
| 9 | 3 | 8 |
| After removal of lacrimal bone-lacrimal sac seen: (less than half/not seen) | |
| Less than half | Not seen |
| 19(95%) | 1(5%) |
| Superior end of sac: (at/below/above axilla) | |
| More than half above the axilla | Less than half above the axilla |
| 12(60%) | 8(40%) |
| The relation between the lacrimal sac and the maxillary line (more than half anterior to maxillary line/less than half anterior to maxillary line/full anterior) | ||
| Less than half | More than half | Anterior |
| 7(35%) | 12(60%) | 1(5%) |
| Relation of Genu of middle turbinate to nasolacrimal duct: (at/anterior/posterior) | ||
| Anterior | At | Posterior |
| 1(5%) | 9(45%) | 10(50%) |
Table 2.
Measurements
| Measurements | Side | Length-mean (SD) mm | Range (in mm) | P value | Clinical significance |
|---|---|---|---|---|---|
| Length of maxillary line | Right (n = 10) | 12.69 (2.33) | 9.59–15.82 | 0.580 | |
| Left (n = 10) | 12.38(2.76) | 8.09–16.79 | |||
| Total (n = 20) | 12.54(2.49) | 8.09–16.79 | |||
| Anterior nasal spine to genu | Right (n = 10) | 27.99(4.97) | 21.8–35.98 | 0.806 | Working area of the surgeon approximately 2–4.5 cm from anterior nasal spine |
| Left (n = 10) | 28.29(5.08) | 19.98–37.21 | |||
| Total (n = 20) | 28.15(4.89) | 19.98–37.21 | |||
| Anterior nasal spine to axilla | Right (n = 10) | 34.86(5.31) | 27.55–44.40 | 0.962 | |
| Left (n = 10) | 34.91(5.21) | 23.64–42.97 | |||
| Total (n = 20) | 34.89(5.11) | 23.64–44.40 | |||
| Nasolacrimal duct to the maxillary sinus ostium | Right (n = 10) | 3.97(1.16) | 2.0–5.51 | 0.734 | Care should be taken while enlarging maxillary sinus ostium anteriorly. |
| Left (n = 10) | 4.11(1.08) | 2.0–5.3 | |||
| Total | 4.042(1.09) | 2–5.51 | |||
| Anterior edge of lacrimal sac to axilla | Right (n = 10) | 10.84(1.88) | 6.33–13.44 | 0.255 | Anterior extent of incision; 10 mm anterior to axilla and maxillary line |
| Left (n = 10) | 10.31(1.13) | 7.65–12 | |||
| Total (n = 20) | 10.58(1.54) | 6.33–13.44 | |||
| Length of lacrimal sac | Right (n = 10) | 11.27(1.62) | 7.48–13.53 | 0.123 | Vertical incision to be approximately 10 mm to M point |
| Left (n = 10) | 12.17(2.58) | 6.98–15.54 | |||
| Total | 11.72(2.145) | 6.98–15.54 | |||
| Distance between fornix of LS and axilla of MT | Right (n = 10) | 8.48(2.17) | 5.43–12.20 | 0.394 | The incision to be approximately 10 mm above axilla |
| Left (n = 10) | 9.29(2.27) | 5.97–13.32 | |||
| Total | 8.88(2.2) | 5.43–13.32 |
Fig. 2.

The features/dimensions noted on cadaveric dissection: MSO-maxillary sinus ostium, IT-inferior turbinate, NF-nasal floor, ANS-anterior nasal spine
Statistical Analysis
SPSS version 16.0 was used for statistics. Mean, standard deviation and the minimum and maximum values of all measurements were determined, the values being rounded into having two digits after the points. Paired T test was done to detect whether a statistically significant difference existed in all the measurements between the right and left parts of the specimen.
Results
Maxillary line was clearly identified in 15 (75%) and not clear in five (25%) cadavers heads. The lacrimomaxillary suture was seen posterior to maxillary line in nine (45%); at maxillary line in eight (40%) and anterior to maxillary line in three (15%) of the cadavers. Line overlapped the LS in 95% cadavers (19/20) and in one cadaver the LS was completely anterior to the maxillary line. Following removal of lacrimal bone, the lower part of LS was seen in 19 cadavers (95%). More than half of the LS was above the axilla in 60% and less than half above the axilla in 40% of cadavers. Genu of middle turbinate was noted at NLD in 45% of cadavers, posterior to in 50% of cadavers and anterior in 1 cadaver (presence of concha bullosa). In our study agger nasi was noted in 16 cadavers (80%), adjacent to the lacrimal fossa. The various relations and measurements are given in Tables 1 and 2. There was no statistically significant difference between right and left parts of specimen.
Discussion
Endonasal endoscopic DCR for surgical treatment for epiphora has become preferred alternative to external DCR [5–7]. In ENDO-DCR the initial landmarks reported are axilla, maxillary line and M point [3, 4].
Axilla, the fixed bony reference point is the most relevant landmark as it is the basis of the other two landmarks. In our study maxillary line was clearly identified in 75%. This was similar to findings of Chastain et al. [3] who reported that the maxillary line could be identified in 88% of their cadaveric study. We also noted that in the cadavers, where maxillary line was not clear, a ridge was always present on the superior surface of inferior turbinate, near its medial border (Fig. 3). An imaginary line can be drawn from anterior end of this ridge to the axilla which could represent the maxillary line and assist the surgeon to initiate the ENDO-DCR. This has not been previously reported. The maxillary line overlapped the LS in 95% cadavers in our study, similar to the report of Orhan et al. [2]. In one cadaver the LS was completely anterior to the maxillary line. The maxillary line was anterior to (45%), at (40%) and posterior to (15%) the lacrimomaxillary suture (Table 2). Orhan et al. [2] reported that in 69% cadavers, maxillary line lay over lacrimomaxillary suture and in 31% it was anterior [2]. Considering these, incising the mucosa anterior to maxillary line and elevating it ensures exposure of the lacrimomaxillary suture line and the LS in majority of cases.
Fig. 3.

Maxillary line (pointer) and ridge (broken arrows) on the superior surface of inferior turbinate
M point, the midpoint of the maxillary line was noted in all the cadavers in our study at the level of the superior aspect of the maxillary sinus ostium posteriorly, and the junction of the LS and the NLD anteriorly as reported earlier [3]. NLD was about 4.04 mm anterior to maxillary sinus ostium in our study (Fig. 4). Tatlisumak et al. reported this distance to be an average of 3.9 mm [8].
Fig. 4.

Nearest distance between NLD to Maxillary sinus ostium (arrow)
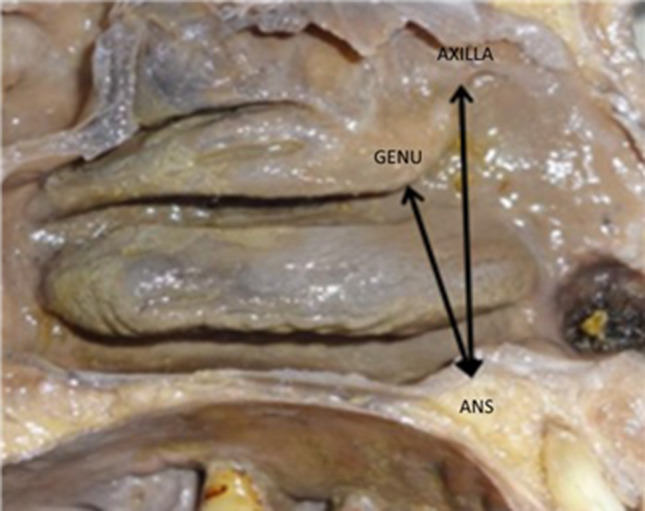
Genu (junction between the anterior most and lower most free part of the middle turbinate) in our study was noted at NLD in 45% (Fig. 5a), posterior to in 50% (Fig. 5b) and anterior in 1 (Fig. 5c, concha bullosa noted in this cadaver). Using this as a landmark, an incision anterior and just superior to level of the genu is sufficient to expose the inferior most aspect of LS in ENDO-DCR. Unlike the maxillary line and M point, the genu is not located over the frontal process of maxilla and lacrimal bone. Hence this landmark is useful to locate the NLD in revision DCR, where there is a paucity of lateral nasal wall landmarks. The emergence of prelacrimal approaches for the maxillary sinus is a recent surgical development [9, 10]. Partial removal of the lateral nasal wall with preservation of the NLD and the inferior turbinate in this approach, results in better access to the anterior half of the maxillary sinus and reduces the morbidity in medial maxillectomy. Genu of the middle turbinate is a useful land mark in the prelacrimal approach for the early localisation of NLD, which is a critical step in this approach. The surgeon also needs to rule out a concha bullosa as that can cause the genu to be anterior to the NLD.
Fig. 5.

Relation of genu with NLD. a Genu at NLD. b Genu posterior to NLD. c Genu anterior to NLD
In our study the distances between the anterior nasal spine to genu and axilla were noted on an average of 28.15 mm and 34.89 mm respectively. As an endoscopic surgeon considering ENDO–DCR, these two measurements would be helpful for understanding 3-dimensional anatomy. The surgeon would have to work in an area 2–4.5 cm (considering the range of both the measurements) from the anterior nasal spine (Fig. 6). This has not been previously reported.
Fig. 6.
Surgeon’s working area; ANS-anterior nasal spine 2–4.5 cm
Thickness of lacrimal bone was found to be 0.25 mm in our study. Other studies have reported mean thickness 0.106 mm and 0.057 mm [11, 12]. The lacrimal bone is thin and can be easily penetrated with most surgical instruments. Following removal of lacrimal bone, the lower part of LS (less than half) was seen in 95% of specimens in our study. This was also noted by Yung et al. [12]. In our study we noted the distance between anterior edge of LS and axilla being an average of 10.58 mm (Table 2). Orhan et al. reported the distance to be 3.67 mm [2]. The reasons for greater distance in our study could be due to the anatomical variation in the Indian population and presence of agger nasi. The length of LS in our study was an average of 11.72 mm, similar to other reports [2, 13].
Wormald and colleagues in 2000 evaluated CT scans and CT-Dacryocystograms (CT-DCG) of 47 cases and demonstrated that the LS extends a significant distance (average of 8 mm) above the axilla of the middle turbinate [1]. However, in our study the distance between fornix (superior end) of LS and axilla was 8.88 mm (Fig. 7). More than half of the LS was above the axilla in 60% (Table 1). This is similar to studies done by various authors [1, 2].
Fig. 7.

Distance between axilla to fornix of lacrimal sac; A—fornix of lacrimal sac, B—axilla
In another cadaveric study it was reported that majority of the LS (2/3) was located below the entry point of the common lacrimal canaliculus [14]. The common canaliculus thus provides a valuable landmark. If the common canaliculus can be viewed through the open sac it can be assumed that the dissection and bone removal are sufficiently high. However, the sac has to still be opened below to the midpoint of the anterior end of the middle turbinate to prevent sump formation [1]. A large opening into the sac extended inferiorly to level of M point resist stenosis and may also avoid lacrimal sump syndrome [3].
In our study agger nasi was noted in 16 cases (80%), adjacent to the lacrimal fossa similar to Woo et al. [15]. Agger nasi is encountered anterior to middle turbinate and might lead to difficulty in locating LS [16]. Preoperative endoscopic evaluation is essential to identify its presence in addition to other intranasal findings.
A ‘Rule of 10’ can be considered for nasal mucosal incision in view of the relationship between LS and maxillary line, length of the LS, distance between the axilla to fornix and anterior border of LS and LS-NLD junction. This incision can be approximately 10 mm above axilla, 10 mm anterior to maxillary line and genu and 10 mm long to M point (just above level of genu) to sufficiently expose the lacrimal sac up to its inferior limit (Fig. 8).
Fig. 8.

Mucosal incision of approximately 10 mm above axilla, 10 mm anterior to maxillary line and genu and 10 mm long to M point (above level of genu)
A Three Tier Approach concept can also be considered where the three boundaries are overcome in DCR. These are first mucosal boundary where initial above mentioned nasal incision is done and elevated, next being bony where lacrimal bone & frontal process of maxilla removed with the third being mucosal where incision is made to open and evert medial wall of the lacrimal sac.
Conclusion
This study highlights the various measurements of the LS and NLD in the Indian population. The description of Genu of middle turbinate as a landmark for the NLD is an important finding of our study. This is useful in revision DCR and in the prelacrimal approach to the maxillary sinus where an early localisation of the NLD is necessary. Preoperative nasal endoscopy is to be done to identify the presence of Aggar nasi as this would increase the distance between the anterior end of the sac and axilla. Application of “Rule of 10” for initial mucosal incision along with a “Three Tier Approach to the Lacrimal Sac” is suggested for a successful endonasal endoscopic DCR.
Summary
The lateral nasal wall landmarks reported as guide for endonasal DCR are axilla, maxillary line and M point
This descriptive anatomical study revealed that Genu of middle turbinate is an additional lateral nasal wall landmark to locate the inferior most aspect of LS in addition to locating NLD in revision DCR and prelacrimal approach to the maxillary sinus
Presence of Agger nasi is to be identified by preoperative endoscopy as this increases the distance of anterior end of LS from the axilla which could lead to difficulty in locating LS.
- To facilitate the surgeon for a simple and systematic approach to lacrimal sac for a successful endonasal endoscopic DCR, the following are suggested:
- ‘Rule of 10’ for initial intranasal mucosal incision
- “Three Tier Approach” concept to overcome the three boundaries: medial nasal mucosal, intermediate bony (lacrimal and frontal process of maxilla) and lateral mucosal (lacrimal sac).
Acknowledgements
This study was partially supported by Institutional Fluid Research Grant, Christian Medical College, Vellore, India (Grant No. IRB Min. No. 7339).
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Amit Kumar Tyagi: Previously Department of ENT, Speech and Hearing, Head and Neck Surgery, Christian Medical College, Vellore, Tamilnadu, India. Mary Kurien: Previously Department of ENT, Christian Medical College, Vellore, India.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wormald PJ, Kew J, Van Hasselt A. Intranasal anatomy of the nasolacrimal sac in endoscopic dacryocystorhinostomy. Otolaryngol Head Neck Surg. 2000;123(3):307–310. doi: 10.1067/mhn.2000.105416. [DOI] [PubMed] [Google Scholar]
- 2.Orhan M, Saylam CY, Midilli R. Intranasal localization of the lacrimal sac. Arch Otolaryngol Head Neck Surg. 2009;135(8):764–770. doi: 10.1001/archoto.2009.94. [DOI] [PubMed] [Google Scholar]
- 3.Chastain JB, Cooper MH, Sindwani R. The maxillary line: anatomic characterization and clinical utility of an important surgical landmark. Laryngoscope. 2005;115(6):990–992. doi: 10.1097/01.MLG.0000163764.01776.10. [DOI] [PubMed] [Google Scholar]
- 4.Ralph M. Endoscopic dacryocystorhinostomy—an update on techniques. Oper Tech Otolaryngol Head Neck Surg. 1995;6(3):217–220. doi: 10.1016/S1043-1810(06)80016-3. [DOI] [Google Scholar]
- 5.Metson R. Endoscopic surgery for lacrimal obstruction. Otolaryngol Head Neck Surg. 1991;104(4):473–479. doi: 10.1177/019459989110400408. [DOI] [PubMed] [Google Scholar]
- 6.Ben Simon GJ, Joseph J, Lee S, et al. External versus endoscopic dacryocystorhinostomy for acquired nasolacrimal duct obstruction in a tertiary referral center. Ophthalmology. 2005;112(8):1463–1468. doi: 10.1016/j.ophtha.2005.03.015. [DOI] [PubMed] [Google Scholar]
- 7.Cokkeser Y, Evereklioglu C, Er H. Comparative external versus endoscopic dacryocystorhinostomy: results in 115 patients (130 eyes) Otolaryngol Head Neck Surg. 2000;123(4):488–491. doi: 10.1067/mhn.2000.105470. [DOI] [PubMed] [Google Scholar]
- 8.Tatlisumak E, Aslan A, Cömert A, et al. Surgical anatomy of the nasolacrimal duct on the lateral nasal wall as revealed by serial dissections. Anat Sci Int. 2009;15(85):8–12. doi: 10.1007/s12565-009-0044-z. [DOI] [PubMed] [Google Scholar]
- 9.Morrissey DK, Wormald PJ, Psaltis AJ. Prelacrimal approach to the maxillary sinus. Int Forum Allergy Rhinol. 2015 doi: 10.1002/alr.21640. [DOI] [PubMed] [Google Scholar]
- 10.Zhou B, Han DM, Cui S-J, et al. Intranasal endoscopic prelacrimal recess approach to maxillary sinus. Chin Med J Engl. 2013;126(7):1276–1280. [PubMed] [Google Scholar]
- 11.Hartikainen J, Aho HJ, Seppä H, et al. Lacrimal bone thickness at the lacrimal sac fossa. Ophthalmic Surg Lasers. 1996;27(8):679–684. [PubMed] [Google Scholar]
- 12.Yung MW, Logan BM. The anatomy of the lacrimal bone at the lateral wall of the nose: its significance to the lacrimal surgeon. Clin Otolaryngol Allied Sci. 1999;24(4):262–265. doi: 10.1046/j.1365-2273.1999.00235.x. [DOI] [PubMed] [Google Scholar]
- 13.Groell R, Schaffler GJ, Uggowitzer M, et al. CT-anatomy of the nasolacrimal sac and duct. Surg Radiol Anat. 1997;19(3):189–191. doi: 10.1007/BF01627974. [DOI] [PubMed] [Google Scholar]
- 14.Zhang S-Q, Jia P-L, Tang H-H, et al. Endonasal anatomy of lacrimal sac and its clinical significance in dacryocystorhinostomy. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2006;41(7):506–509. [PubMed] [Google Scholar]
- 15.Woo KI, Maeng H-S, Kim Y-D. Characteristics of intranasal structures for endonasal dacryocystorhinostomy in Asians. Am J Ophthalmol. 2011;152(3):491.e1–498.e1. doi: 10.1016/j.ajo.2011.02.019. [DOI] [PubMed] [Google Scholar]
- 16.Wormald PJ. The agger nasi cell: the key to understanding the anatomy of the frontal recess. Otolaryngol Head Neck Surg. 2003;129(5):497–507. doi: 10.1016/S0194-5998(03)01581-X. [DOI] [PubMed] [Google Scholar]


