Abstract
This study aimed to assess the balance function in children with sensorineural hearing loss (SNHL) using different tests to assess vestibulospinal pathway and tests to assess vestibular system and to compare the result obtained with those of children with normal hearing sensitivity. Detailed balance assessment was done for 15 children with severe to profound SNHL and 15 children with normal hearing sensitivity in the age range of 6–10 years. The audiological evaluation included pure-tone audiometry, speech audiometry, immittance evaluation, otoacoustic emission, vestibular evoked myogenic potential (cervical VEMP and ocular VEMP), and tests to assess vestibulospinal pathway and cerebellar function, such as Romberg test, Fukuda stepping test, Tandem gait test, and Finger-to-nose test. cVEMP and oVEMP were absent in 8 ears (27%) of a total of 30 ears with SNHL. Statistical analysis shows no significant difference between latency and amplitude of cVEMP peaks and latency of oVEMP peaks across groups. Significant reduction of oVEMP peaks amplitude was seen in children with SNHL compared to children with normal hearing. Fukuda stepping test showed an abnormal response in 2 children with SNHL (13%) and one child could not perform tandem gait test (7%). Children with SNHL showed an evident abnormality on the balance assessment test results. The abnormal function of the vestibular system and the vestibulospinal pathway can compromise the child’s motor development and thus needs investigation early in life.
Keywords: Vestibular evoked myogenic potential, Fukuda stepping test, Tandem gait test, Finger-to-nose test, Sensorineural hearing loss
Introduction
Maintenance of balance requires a coordinated action involving sensory information from the vestibular system, proprioceptive system, and visual system with the help of vestibular-ocular reflex, vestibule-colic reflex and vestibule-spinal reflex [1]. Since the cochlea and the vestibular system lies in close proximity to each other and also share the germ layers, it is not surprising to have some degree of abnormal vestibular symptoms in individuals with sensorineural hearing loss [2]. The prevalence of dizziness and balance problem was reported to be 5.7% [3] and 5.3% [4] in children without significant hearing loss and 38% had some degree of vestibular loss in 186 children with hearing loss [5]. The most frequent dizziness and balance symptoms reported by children were poor coordination in 46% of the group, light-headedness in 35.1%, poor balance in 30.9%, vertigo in 29% and frequent falls in 25% on the children [4]. The incidence of dizziness symptoms was found to increase with the increase in degree of hearing loss and dizziness symptoms also increased with increase in age [4]. This high prevalence of vestibular dysfunction in children with sensorineural hearing loss (SNHL) and its assessment has gained attention among the professionals over the decade [6–9]. The dizziness and the balance problem can be a consequence of abnormality in any of the system controlling balance, vestibular system, vestibulo-spinal, vestibulo-ocular and vestibulo-collic reflex pathways. The vestibular system is comprised of otolith organs, semicircular canals, and the neural pathway. The functioning of the otolith organs (the utricle and the saccule) and semicircular canals can be assessed using audiological tests such as Vestibular-evoked myogenic potential (VEMP), Electronystagmography (ENG)/Videonystagmography (VNG) test battery, Rotational chair test, Video Head impulse test (vHIT). Cervical vestibular evoked myogenic potential (cVEMP) and Ocular vestibular evoked myogenic potential (oVEMP) are commonly used tests for assessing the function of the otolith organ and vestibular nerves. cVEMP recorded from sternocleidomastoid (SCM) muscles, gives information about saccule and inferior vestibular nerve [10]. oVEMP recorded from extraocular muscle provides information about utricle and superior vestibular nerve [11].
There are a number of research studies discussing the audio-vestibular findings in individuals with normal hearing and with hearing loss [12, 13] but they have their limitations in terms of the study population they considered. Most of the researchers have considered adults with hearing loss for investigation and less attention was given to children with hearing loss. Children with vestibular problems show delayed development of motor milestones, as evident on standing and walking as compared to children without a vestibular problem [5, 14]. One group of researchers has investigated VEMP response in children with SNHL [6, 8]. But this study highlights only the findings of cVEMP in children with SNHL and lacks information about other systems responsible for maintaining postural control. Considering the close proximity of auditory and the vestibular system, there is a high probability of co-occurrence of auditory and the vestibular disorder in children with SNHL. So there was a need to assess both the auditory and the vestibular functions in children with SNHL. Along with the auditory and the vestibular system, the visual system and the proprioceptive system, which help in maintaining the postural stability in children with SNHL also needs investigation. Balance tests done together on the same child will give a holistic idea about the balance system and will also provide the data to the audiologist for counseling. Hence, the lack of information about the audio-vestibular reports gives rise to the need for the present study. So, the present study aimed to assess the balance function in children with SNHL and to compare the result obtained with typically developing children. The first objective of the study was to compare the cVEMP and the oVEMP results obtained from children with normal hearing and with SNHL. The second objective was to compare the results of vestibulospinal and cerebellar tests for both the groups of children with normal hearing and with SNHL.
Methods
Detailed balance assessment was done for 15 children with SNHL (8 males and 7 females) and 15 age-matched children (8 males and 7 females) with normal hearing sensitivity. All the children in the SNHL group had severe-to-profound hearing loss with varied etiology of hearing loss (hereditary, acquired and unknown). The age range of the participants was 6 years to 10 years with the mean age of 7.8 years. All the children with SNHL were recruited from the Audiology department of the city hospital and all the children were using digital behind-the-ear hearing aids binaurally. A detailed case history was taken from all the participants and the caregivers regarding their auditory, speech-language and motor development, their prenatal, natal and post-natal history, family history and academic performance in school. The neurologist examined the children for the presence of neural disorders and otorhinolaryngologist examined the children for the presence of any otological problem. The children with a complaint of any neurological or middle ear infection were excluded from the study. The audiological tests including pure-tone audiometry, speech audiometry, immittance evaluation, otoacoustic emission, and auditory brainstem response were administered on all the children and the test result from both the groups of children with normal hearing and with SNHL are shown in Table 1. Written informed consent was taken from the caregivers of all the children. Institutional ethical committee approval was taken prior to the commencement of the study. VEMP including both oVEMP and cVEMP were recorded to assess the status of the utriculo-ocular pathway and sacculo-collic pathway respectively. The test parameters used for recording cVEMP and oVEMP were the same as those used by Kumar and Apeksha [15]. The participants were seated upright on a straight back chair. The stimulus and the recording parameters for both cVEMP and oVEMP are provided in Table 2.
Table 1.
Audiological findings of children with normal hearing and with SNHL
| Audiological test | Children with normal hearing | Children with SNHL |
|---|---|---|
| Pure-tone average (PTA) | Less than or equal to 15 dB HL | Greater than 70 dB HL |
| Speech audiometry | Scores range from 90 to 100% | Scores range from 0 to 30% |
| Immittance evaluation | ‘A’ type tympanogram | ‘A’ type tympanogram |
| Distortion product otoacoustic emmission | Present | Absent |
| Auditory brainstem response | Present with latency and amplitude within normal range | Absent |
Table 2.
Stimulus and acquisition parameters for cVEMP and oVEMP
| Parameters | cVEMP | oVEMP |
|---|---|---|
| Electrode placement |
Non-inverting—sternocleidomastoid muscle Inverting—sterno-clavicular junction Ground—forehead |
Non-inverting—1 cm beneath the lower eyelid Inverting—2 cm below the non-inverting Ground—forehead |
| Stimuli | 500 Hz tone-burst | 500 Hz tone-burst |
| Rise/fall time | 2-1-2 ms | 2-1-2 ms |
| Stimulus intensity | 125 dB peSPL | 125 dB peSPL |
| Repetition rate | 5.1 Hz | 5.1 Hz |
| Filter | 10–1500 Hz | 10–1500 Hz |
| Epoch | 80 ms including 20 ms pre-stimulus | 64 ms including 10.5 ms pre-stimulus |
| Averages | 200 | 200 |
| Stimulation | Ipsilateral ear | Contralateral ear |
| Number of recording | 2 | 2 |
The vestibulospinal pathway was assessed using the Romberg test, Fukuda stepping test, Tandem gait tests, and cerebellar function was assessed using Finger-to-nose test. Romberg test is an assessment tool to diagnose sensory ataxia and is also sensitive means of measuring the disequilibrium caused by the vertigo of central or peripheral in origin [16]. For the Romberg test, the children were asked to stand in the center of a circle drawn on the floor with hands stretched horizontal to the ground and were asked to stand for 1 min with eyes closed. Activities like children opening their eyes, movement from the initial position, or tendency to fall as observed by the investigator or reported by the children, were noted positive and is suggestive of proprioceptive deficit. Fukuda stepping test helps to identify the weaker labyrinth. An angular deviation of greater than 30° about the vertical axis suggests asymmetry in the labyrinthine function with weaker side identified by the direction of rotation [17]. In Fukuda stepping test, the children were asked to stand at the center of a circle with hands stretched horizontal to the ground and was asked to march in the same place 50 times with eyes closed. Any movement, either in forwards-backward direction or right-left or angular shift about the vertical axis was noted. Tandem gait test is an important tool in the assessment of cerebellar disease, parkinsonism, peripheral neuropathies and vestibulopathies [18]. The inability to perform heel-to-toe walk with a tendency to fall, imbalance, or raising a hand to maintain balance was considered as an abnormal result [19]. In the Tandem gait test, the children were asked to walk heel-to-toe on a straight line and body sway, if present (front-back, right-left) was noted. In Finger-to-nose test, the children were asked to touch their nose and investigator’s index finger alternately for a number of trials. Overshooting and undershooting was noted.
Data Analyses
The data obtained from cVEMP and oVEMP were tabulated and analyzed using Statistical Package for the Social Sciences (SPSS Inc, Illinois, USA) software. Both groups were compared based on VEMP parameters and vestibulospinal and cerebellar test results. Shapiro-Wilks test of normality showed data were non-normally distributed (p < 0.05) and thus non-parametric tests were done. Wilcoxon signed-rank test was done to check for the ear difference for cVEMP and oVEMP latency and amplitude in both the groups.
Results
The VEMP responses showed clear, identifiable and replicable peaks for all the 15 children with normal hearing sensitivity whereas VEMP responses were present in only 11 children (73%) with SNHL. The results showed no ear difference (p > 0.05) for both cVEMP and oVEMP latency and amplitude data and thus the data from both the ears were combined making a total of 30 ears with normal hearing sensitivity and 22 ears with SNHL. Of the response obtained from 30 ears of children with SNHL, the response rate for cVEMP was 73% (response present in 22 ears) and the response rate for oVEMP was 73% (response present in 22 ears).
The mean and the standard deviation of the latency and the amplitude of cVEMP are given in Table 3 and Fig. 1. On visual inspection, it is evident from Fig. 1 that the amplitude of P13 and N23 showed more variability than the latency of P13 and N23 peaks. The variability was found to be more in children with SNHL compared to children with normal hearing sensitivity. The latency and amplitude values were similar for children with normal hearing and with SNHL. The mean and the standard deviation of the latency and the amplitude of oVEMP are given in Table 3 and Fig. 2. From Fig. 2 it is clear that the latency of n1 and p1 was similar for both the groups of children with normal hearing and with SNHL. In contrast to the latency of oVEMP, the amplitude of oVEMP showed a noticeable difference between both the groups of children with normal hearing and with SNHL.
Table 3.
Mean and standard deviation (SD) of the peak amplitude and peak latency of cVEMP and oVEMP obtained from children with normal hearing and with SNHL
| Children with normal hearing | Children with SNHL | ||||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| cVEMP | |||||
| Latency (ms) | P13 | 15.6 | 2.65 | 15.60 | 2.54 |
| N23 | 20.53 | 2.03 | 20.10 | 2.93 | |
| Amplitude (µV) | P13 | 14.53 | 9.91 | 12.05 | 10.99 |
| N23 | − 11.36 | 9.31 | − 9.89 | 8.56 | |
| oVEMP | |||||
| Latency (ms) | n1 | 12.90 | 3.41 | 12.40 | 3.55 |
| p1 | 16.27 | 3.31 | 15.19 | 2.92 | |
| Amplitude (µV) | n1 | − 1.62 | 1.31 | 0.58 | 0.37 |
| p1 | 1.21 | 0.83 | 0.39 | 0.33 | |
Fig. 1.
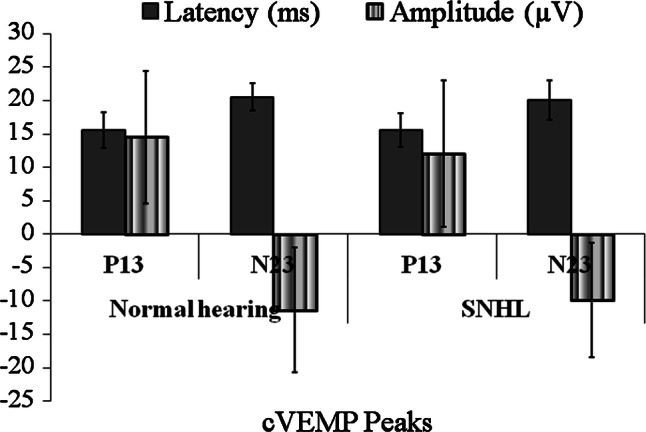
Mean and standard deviation of latency and amplitude of cVEMP peaks obtained from children with normal hearing and with SNHL. The error bar represents one standard error
Fig. 2.
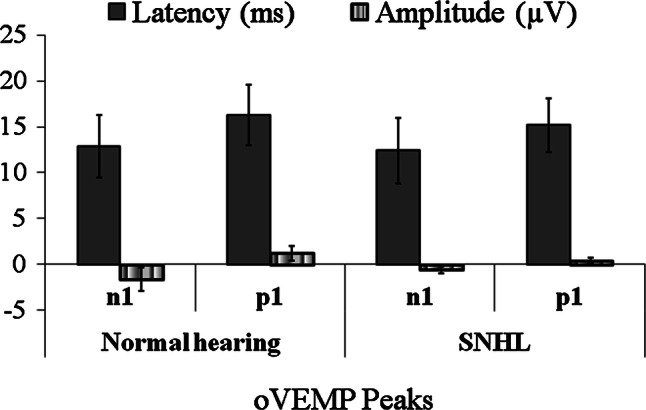
Mean and standard deviation of latency and amplitude of oVEMP peaks obtained from children with normal hearing and with SNHL. The error bar represents one standard error
Mann–Whitney U test was done to compare the response obtained from children with normal hearing and with SNHL. The result showed no statistically significant difference between the latency and amplitude of P13 and N23 of cVEMP and latency of n1 and p1 peaks of oVEMP across the groups (p > 0.05). The amplitude of n1 peak (z = − 3.66, p < 0.001), and p1 peak (z = − 3.34, p < 0.05) of oVEMP showed significant reduction in amplitudes in children with SNHL compared to children with normal hearing.
Romberg test—All the children with normal hearing and children with SNHL were able to stand for 1 min with their arm stretched and eyes closed. There was no significant abnormality seen in any of the children. Fukuda stepping test—all the children with normal hearing were able to step 50 times without any significant abnormality. Out of 15 children with SNHL, 12 (80%) of them moved in the forward direction (less than 1 m) without showing any significant angular deviation. One child (7%) deviated to 30° towards the side while performing the Fukuda stepping test, with the absence of cVEMP and oVEMP response on the same side. One of 15 children could not perform Fukuda stepping test, as was not able to March with eyes closed and also showed poor response on cVEMP and oVEMP. Tandem gait test—all the children with normal hearing were able to walk heel-to-toe without any significant abnormality. One of the children with SNHL was not able to walk heel-to-toe and also showed an abnormality on Fukuda stepping test. All the children with SNHL showed normal responses on Finger-to-nose test.
Discussion
From the test results, it is clear that the children with SNHL showed a significant abnormality on the cVEMP and oVEMP and also on behavioral balance tests. Except for the eight ears with the absent cVEMP response, children with SNHL showed cVEMP response similar to that of normal-hearing children, suggesting a normal sacculo-collic pathway in children in whom the response was present. The absence of cVEMP response in children with SNHL suggests an abnormal vestibular function in children with SNHL. These findings support the findings of the previous study by Zhou et al. [6], Singh et al. [8], Selim et al. [9] and Maes et al. [20]. Singh et al. [8] reported similar latency of cVEMP response in children with normal hearing and in children with severe to profound SNHL but the amplitude of cVEMP response was found to be significantly smaller in children with SNHL compared to children with normal hearing. The cVEMP response was also reported to be absent in two of the 15 children with SNHL. The authors suggested abnormality in sacculo-collic pathways in children with SNHL. In addition, Zhou et al. [6] showed abnormal cVEMP findings in 21 out of the 23 children with SNHL. The threshold of cVEMP was significantly higher and the amplitude of peaks was significantly lower in children with severe to profound hearing loss. Similar findings were reported by Selim et al. [9] on 30 children with different degrees of SNHL. In another study by Maes et al. [20], the vestibular evaluation was done for 39 children with bilateral SNHL using Rotational chair test and cVEMP. The result showed 79% of the children with SNHL showed some vestibular abnormality when examined with a combination of rotational chair test and cVEMP, whereas the sensitivity dropped to 60% with cVEMP alone and 49% with rotational chair test alone. The results of all the above-mentioned studies indicate an abnormal vestibular function in children with SNHL. Said [21] reported abnormal ENG findings for 64% of the children with SNHL and abnormal cVEMP findings for 72% of the children with SNHL. Based on all the above-mentioned reports, there is a significant vestibular abnormality seen in children with SNHL.
Absence of oVEMP response in 8 ears with SNHL and reduced mean amplitude of n1 and p1 in children with SNHL compared to children with normal hearing in the present study suggests dysfunction in the utriculo-ocular pathway in children with SNHL. These findings support the hypothesis that if there is any abnormality in the cochlea, there might be associated vestibular system abnormality. The probable reason for the dysfunction could be because of the close proximity of the cochlea to that of the vestibular system and also because it shares the same germ layers. Vestibulospinal tests, including the Fukuda stepping test and Tandem gait test, also showed the abnormal response for few of the children with SNHL. The abnormal response on the vestibulospinal tests along with absent/abnormal response of cVEMP and oVEMP response suggests an abnormal vestibular function in children with SNHL. This peripheral abnormality can result in overall poor development of motor milestones in children with SNHL [5, 22]. Inoue et al. [22] evaluated the function of superior and inferior vestibular nerve system using damped rotation test, caloric test, and cVEMP in children with profound SNHL and correlated the result with that of gross motor development in same children. Damped rotation test showed abnormality in 20% of the children, the caloric test showed abnormality in 41% of the children and cVEMP showed abnormality in 42% of the children with SNHL. The result also showed that the children with SNHL who showed an abnormality on the vestibular function test also showed significantly delayed acquisition of head control and independent walking suggesting that the normal vestibular function is required for the appropriate development of a gross motor function. Researchers opine that irrespective of the different vestibular tests administered on children with SNHL, the test result shows abnormal vestibular function in children with SNHL.
In spite of the abnormality seen on various vestibular and balance tests, the children with SNHL do not complain about the loss of balance or frequent fall when they are young. The probable reason could be because of the central compensation and the substitution of the vestibular system function by the other two systems, visual and proprioceptive system, involved in maintaining balance. Another reason could also be because of the less attention paid by the caregiver towards the symptoms, considering the symptoms as the normal developmental trend. Even though the child can manage their daily activities similar to that of children with normal hearing, they find it difficult in the challenging situation, like walking in the darkroom, walking on an uneven surface, swimming underwater. This study has limited implications as the other objective tests for balance assessment, such as the vHIT, ENG, Rotational chair test were not included in the present study. This study finding also lacks generalization as this study was done on a small group of population (15 children with SNHL and 15 children with normal hearing).
Summary and Conclusions
The children with SNHL show evident abnormality on the balance function tests which might compromise their gross and fine motor development and might also limit their performance in challenging situations. We advocate detailed balance assessment in children with SNHL, as it will help the professionals to counsel the caregiver about the problem early in life and will also help in rehabilitating the child with balance issues.
Acknowledgements
We would like to thank the Director and Principal, JSS Institute of Speech and Hearing, for allowing us to carry out this study. We would also like to thank all the participants of this study.
Funding
Not applicable.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Herdman SJ. Vestibular rehabilitation. 3. Philadelphia: F. A. Davis Company; 2007. [Google Scholar]
- 2.Northern JL, Downs MP. Hearing in children. Philadelphia: Lippincott Williams & Wilkins; 2002. [Google Scholar]
- 3.Humphriss RL, Hall AJ. Dizziness in 10 year old children: an epidemiological study. Int J Pediatr Otorhinolaryngol. 2011;75:395–400. doi: 10.1016/J.IJPORL.2010.12.015. [DOI] [PubMed] [Google Scholar]
- 4.Li CM, Hoffman HJ, Ward BK, et al. Epidemiology of dizziness and balance problems in children in the United States: a population-based study. J Pediatr. 2016;171:240–247. doi: 10.1016/j.jpeds.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 5.Janky KL, Thomas MLA, High RR, et al. Predictive factors for vestibular loss in children with hearing loss. Am J Audiol. 2018;27:137–146. doi: 10.1044/2017_AJA-17-0058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhou G, Kenna MA, Stevens K, Licameli G. Assessment of saccular function in children with sensorineural hearing loss. Arch Otolaryngol Neck Surg. 2009;135:40–44. doi: 10.1001/archoto.2008.508. [DOI] [PubMed] [Google Scholar]
- 7.Zhou G, Dargie J, Dornan B, Whittemore K. Clinical uses of cervical vestibular-evoked myogenic potential testing in pediatric patients. Medicine. 2014;93:1–6. doi: 10.1097/MD.0000000000000037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singh S, Gupta RK, Kumar P. Vestibular evoked myogenic potentials in children with sensorineural hearing loss. Int J Pediatr Otorhinolaryngol. 2012;76:1308–1311. doi: 10.1016/J.IJPORL.2012.05.025. [DOI] [PubMed] [Google Scholar]
- 9.Selim E-AS, El-Minawi MS, et al. Assessment of saccular function using cervical vestibular-evoked myogenic potentials in children with sensorineural hearing loss. Egypt J Otolaryngol. 2012;28:234–241. doi: 10.7123/01.EJO.0000418053.78780.0C. [DOI] [Google Scholar]
- 10.Isaradisaikul S, Navacharoen N, Hanprasertpong C, Kangsanarak J. Cervical vestibular-evoked myogenic potentials: norms and protocols. Int J Otolaryngol. 2012;2012:913515. doi: 10.1155/2012/913515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Welgampola MS, Carey JP. Waiting for the evidence: VEMP testing and the ability to differentiate utricular versus saccular function. Otolaryngol Neck Surg. 2010;143:281–283. doi: 10.1016/j.cortex.2009.08.003.Predictive. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Singh NK, Sinha SK, Govindaswamy R, Apeksha K. Are cervical vestibular evoked myogenic potentials sensitive to changes in the vestibular system associated with benign paroxysmal positional vertigo? Hear Balanc Commun. 2014;12:20–26. doi: 10.3109/21695717.2014.883208. [DOI] [Google Scholar]
- 13.Singh NK, Sinha SK, Rajeshwari G, et al. Frequency-amplitude ratio of cervical vestibular evoked myogenic potential for iden tifying meniere’ s disease. Int J Heal Sci Res. 2015;5:228–237. [Google Scholar]
- 14.Verbecque E, Marijnissen T, De Belder N, et al. Vestibular (dys)function in children with sensorineural hearing loss: a systematic review. Int J Audiol. 2017;56:361–381. doi: 10.1080/14992027.2017.1281444. [DOI] [PubMed] [Google Scholar]
- 15.Singh NK, Apeksha K. Efficacy of cervical and ocular vestibular-evoked myogenic potentials in evaluation of benign paroxysmal positional vertigo of posterior semicircular canal. Eur Arch Oto-Rhino-Laryngol. 2015;273:2523–2532. doi: 10.1007/s00405-015-3867-3. [DOI] [PubMed] [Google Scholar]
- 16.Galan-Mercant A, Cuesta-Vargas AI. Mobile Romberg test assessment (mRomberg) BMC Res Notes. 2014;7:640–647. doi: 10.1186/1756-0500-7-640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Honaker JA, Boismier TE, Shepard NP, Shepard NT. Fukuda stepping test: sensitivity and specificity. J Am Acad Audiol. 2009;20:311–314. doi: 10.3766/jaaa.20.5.4. [DOI] [PubMed] [Google Scholar]
- 18.Margolesky J, Singer C. How tandem gait stumbled into the neurological exam: a review. Neurol Sci. 2018;39:23–29. doi: 10.1007/s10072-017-3108-1. [DOI] [PubMed] [Google Scholar]
- 19.Rumalla K, Karim A, Hullar T. The effect of hearing aids on postural stability. Laryngoscope. 2015;125:720–723. doi: 10.1002/lary.24974. [DOI] [PubMed] [Google Scholar]
- 20.Maes L, De Kegel A, Van Waelvelde H, Dhooge I. Rotatory and collic vestibular evoked myogenic potential testing in normal-hearing and hearing-impaired children. Ear Hear. 2014;35:e21–e32. doi: 10.1097/AUD.0b013e3182a6ca91. [DOI] [PubMed] [Google Scholar]
- 21.Said E-F. Vestibular assessment in children with sensorineural hearing loss using both electronystagmography and vestibular-evoked myogenic potential. Egypt J Otolaryngol. 2014;30:43. doi: 10.4103/1012-5574.127203. [DOI] [Google Scholar]
- 22.Inoue A, Iwasaki S, Ushio M, et al. Effect of vestibular dysfunction on the development of gross motor function in children with profound hearing loss. Audiol Neurotol. 2013;18:143–151. doi: 10.1159/000346344. [DOI] [PubMed] [Google Scholar]


