Abstract
The descriptor “usual care” refers to standard or routine care. Yet, no formal definition exists. The need to define what constitutes usual care arises in clinical research. Often one arm in a trial represents usual care in comparison to a novel intervention. Accordingly, usual care in genetic counseling research appears predominantly in randomized controlled trials. Recent standards for reporting genetic counseling research call for standardization, but do not address usual care. We (1) inventoried all seven studies in the Clinical Sequencing Evidence-Generating Consortium (CSER) about how genetic counseling was conceptualized, conducted, and whether a usual care arm was involved; (2) conducted a review of published randomized control trials in genetic counseling, comparing how researchers describe usual care groups; (3) and reviewed existing professionally endorsed definitions and practice descriptions of genetic counseling. We found wide variation in the content and delivery of usual care. Descriptions frequently detailed the content of usual care, most often noting assessment of genetic risk factors, collecting family histories and offering testing. A minority included addressing psychological concerns or the risks versus benefits of testing. Descriptions of how care was delivered were vague except for mode and type of clinician, which varied. This significant variation, beyond differences expected among subspecialties, reduces the validity and generalizability of genetic counseling research. Ideally, research reflects clinical practice so that evidence generated can be used to improve clinical outcomes. To address this objective, we propose a definition of usual care in genetic counseling research that merges common elements from the National Society of Genetic Counselors’ practice definition, the Reciprocal Engagement Model, and the Accreditation Council for Genetic Counselors’ practice-based competencies. Promoting consistent execution of usual care in the design of genetic counseling trials can lead to more consistency in representing clinical care and facilitate the generation of evidence to improve it.
Keywords: Usual Care, Genetic counseling research, Randomized Controlled Trials, Genetic counseling interventions
1. Introduction
Research in genetic counseling includes process studies that examine communication approaches and content (e.g. Roter, 2006; Joseph, 2017 and 2019), and studies of genetic counseling outcomes that assess independent variables for their role in achieving targeted outcomes such as pursuit of follow up health care recommendations. Outcomes research also assesses the value of genetic counseling to end users (McAllister, 2011; Hippman, 2016; Ison, 2019), and compares alternative service delivery models that may be more efficient while also being effective (Schwartz, 2014 and 2018). Often such studies are conducted using a randomized controlled trial (RCT) design involving a control group to compare existing conditions to interventions, frequently using the descriptor “usual care” to refer to the standard care offered in such a control group. Yet, there exists no guidance on what constitutes usual care in genetic counseling research. Although Hooker and colleagues recently outlined standards for reporting genetic counseling research in the peer-reviewed literature (Hooker, 2017), defining usual care was notably absent from that effort, leaving an opportunity to address this shortfall.
While there have been many debates surrounding the selection of and the quality of usual care groups in behavioral research (Freedland, 2011; van der Graaf, 2009; Au, 2007), little has been published that seeks to describe or standardize usual care in clinical research, and none in the field of genetic counseling. Recent examples in clinical research include Young et. al (2020) who outlined the challenges of defining and measuring usual care in type 2 diabetes interventions with a focus on how usual care variability has implications for study quality, noting that the reproducibility of a study can be negatively impacted by omissions in descriptions of usual care. Similarly, Arch and Stanton (2019) reviewed the historical shifts in usual care within psychosocial oncology clinical trials, highlighting the difficulty of defining and interpreting usual care, and offering recommendations for psychosocial oncology research. The lack of precision in descriptions of usual care has also been noted in the context of type 1 diabetes interventions (Ayling, 2015), psychiatry (Gold, 2017; Mohr, 2014) and primary care (Smelt, 2010). In all these settings, minimal description of usual care arms made it hard to discern the essence of the differences between a proposed intervention and usual care. In response to these findings, Smelt et al. called for a systematic description of control groups or usual care arms (i.e., an extended CONSORT guideline), and Ayling et al. developed a checklist to code standard of care approaches. These research efforts demonstrate the cross disciplinary importance of addressing usual care and further encouraged our efforts to address the issue in genetic counseling research.
We are largely genetic counselors providing clinical care and, in some cases, interventions, in the Clinical Sequencing Evidence-Generating Research Consortium (CSER) studies (Amendola, 2018). Studies within the consortium are investigating the effectiveness of integrating genomic sequencing into the clinical care of diverse and medically underserved individuals at various clinical settings. This prompted our further exploration of how usual care is conducted across genetic counseling research more broadly. To achieve this, we (1) inventoried all seven CSER studies regarding how genetic counseling was conducted and whether a usual care arm was involved; (2) conducted a review of published RCTs in genetic counseling, comparing how investigators described the usual care groups, noting similarities and differences; and (3) reviewed existing professionally endorsed definitions and practice descriptions of genetic counseling. These efforts verified the current lack of standardization and led us to develop a definition of usual care in genetic counseling research to improve consistency in how usual care is conducted and described in research.
2. METHODS
2.1. Review of Consortium studies
Fifteen genetic counselors representing each of the seven CSER Consortium studies completed a set of open-ended questions that captured the scope and nature of the genetic counseling research being conducted. The responses were put in a table that displayed how usual care was defined in each RCT of a genetic counseling intervention. The responses were checked for completeness and any follow up questions were directed towards the genetic counselors. All CSER study responses were then collated into a larger table.
2.2. Review of published randomized genetic counseling clinical trials
To identify existing descriptions of genetic counseling usual care in the peer-reviewed literature, we reviewed U.S.-based studies from the most recent and comprehensive systematic review of genetic counseling RCTs (Athens et al., 2017) and eight U.S. RCTs published subsequently. The systematic review included English-language publications in peer-reviewed journals from 1990 to 2015 presenting findings from RCTs with at least one primary study aim referencing an outcome of genetic counseling. Two authors read the source manuscripts to abstract information on study design and methodology. We focused on the descriptions of usual care using two constructs: content and delivery. Content was defined as the main elements that made up the counseling aspect of usual care (e.g., genetic risk assessments; the benefits and risks of genetic testing). Delivery was defined as how participants received usual care (e.g., by phone vs. in-person) and by whom (e.g., a formally trained genetic counselor vs. another provider). Where needed, we supplemented our abstraction with protocol papers or previously published articles on the trials that were referred to in the papers’ methods sections.
2.3. Developing a definition of usual care in genetic counseling
To create a definition of usual care to promote standardization, we collated genetic counseling practice elements from the National Society of Genetic Counselors’ Definition of Genetic Counseling (National Society of Genetic Counselors’ Definition Task Force: Resta, 2006), the Reciprocal Engagement Model (Veach, 2007), the Central Tenets of Practice (Biesecker, 2020) and the Accreditation Council for Genetic Counseling (ACGC) Practice-Based Competencies for board certification (Accreditation Council for Genetic Counseling, 2019). These four competencies were chosen as most directly related to care delivery. Fifteen genetic counselors representing all seven CSER studies independently reviewed the competencies for those most relevant to our practice and most likely to be universal across subspecialties. In addition, we consulted guidelines for genetic counseling from related professional societies, including the American College of Medical Genetics and Genomics (https://www.acmg.net/), the American College of Obstetricians and Gynecologists (https://www.acog.org/), American Society of Clinical Oncology (https://www.asco.org/), National Comprehensive Cancer Network (https://www.nccn.org) and the American Society of Human Genetics (https://www.ashg.org). We limited our sources of genetic counseling practice elements to U.S. sources. It was sufficiently challenging to consider variation in care across subspecialties in the U.S., and we were initially skeptical we would arrive at a definition. What provided the opportunity was the consistency in the descriptions by the U.S. professional bodies. Further, there is significant variation in how genetic counseling is defined across international professional bodies and the training of counselors (Abacan, 2019). U.S. practices appear to be most similar to those in the United Kingdom and Australia, and divergent from European countries such as Italy and the Netherlands where physicians provide genetic counseling.
3. RESULTS
3.1. Usual care in the CSER Consortium
All seven CSER Consortium studies provided genetic counseling, but only four tested a genetic counseling intervention against a usual care arm in a randomized trial: Cancer Health Assessments Reaching Many (CHARM), NYCKidSeq, NCGENES, and SouthSeq (See Table 1). Usual care in each of these studies was meant to reflect clinical practice and was not standardized. The practice of usual care in genetic counseling varied in accordance with clinical practice at participating clinics, the aims of the specific CSER study, and the study design. In these four CSER studies, participants were recruited from multiple sites and clinics, with varied clinical practices. Thus, usual care reflected the varied clinical practice across the multiple clinical sites and genetic counselors within each CSER study. For example, in CHARM, counselors in both arms did not have access to medical records per study protocol, and, where appropriate, referred participants to follow-up clinical genetics visits rather than providing ongoing care themselves. In NYCKidSeq, the usual care arm is consistent with current pediatric genetic counseling practice at the two study institutions, apart from study counselors being unaccompanied by other genetics providers during counseling sessions. Study counselors also provide referrals to clinical pediatric genetics for appropriate follow-up care.
Table 1.
CSER Consortium studies with a usual care (UC) arm
| CSER Study | Study Aim (related to genetic counseling) | UC Content | UC Delivery |
|---|---|---|---|
| CHARM | Compare UC genetic counseling and a modified literacy-focused genetic counseling approach for adults at risk of hereditary cancer during disclosure of clinical exome sequencing results for hereditary cancer and secondary results. Counselors in the literacy-focused arm received in-depth training and ongoing support to use evidence-based techniques for effective communication with individuals of limited health literacy (e.g. plain language and teach back; Riddle; 2020); Outcomes include understanding of recommended care, satisfaction with visit, perception of communication, and extent of family communication. | UC defined as the absence of exposure to a GC training intervention on literacy-focused communication. UC included: • Contracting—introduction, establish purpose of call, set expectations for flow of discussion and length of call, review why patient was eligible for the test; • Family history—obtain 3 generation pedigree; • Education—provide background info on genes/inheritance/genetic testing; • Disclosure—disclose results, describe condition caused by gene change (if applicable), review medical management recommendations, create follow-up plan for referrals, outline implications for family members, discuss cascade screening; • Conclusion—review plan, remind patient that results will go into EMR/a summary letter. |
Delivered by telephone by a certified genetic counselor. |
| NYCKidsSeq | Compare traditional (usual care) genetic counseling and genetic counseling using a novel web-based communication tool, GUÍA (Genomic, Understanding, Information & Awareness application), to facilitate the delivery of genomic test results and medical management recommendations to parents of children with suspected neurologic, immunologic and cardiac genetic disorders. The study is investigating the impact of using GUÍA to enhance genetic counseling on participant outcomes (e.g., parental understanding, satisfaction, feelings about the results, and their subsequent behavior). | UC not defined and reflects clinical practice as conducted by the individual GCs, including: • Contracting • Review of pre-test counseling (test ordered, purpose of testing, possible result types); • Disclosure of primary results, including describing the condition, the natural history, inheritance, recurrence risk, impact on family members, treatment and management guidelines; • Disclosure of secondary findings, and targeted counseling as described for primary results disclosure; • Discuss next steps including referrals, medical management, sharing results with PCP and referring provider; Providing resources (e.g., support groups); Psychosocial counseling and support; • Discuss how patients’ genomic data may be used throughout the study. |
Delivered in-person by a certified genetic counselor. |
| SouthSeq | Compare genome sequencing results returned to parents of infants in the NICU with suspected genetic disorders by genetic counselors or trained non-genetics providers. Study genetic counselors developed and delivered training for NICU non-genetics providers on genome result disclosure based on personal experience disclosing genome results and the NSGC Practice Based Competencies (PBCs). The non-inferiority trial is using parental empowerment as the primary outcome. |
UC not defined; assumed GCs would practice within their published scope and competencies. Included: • Contracting: introduction, review purpose of interaction and why infant was enrolled in the study; • Disclosure: primary results (positive, uncertain, negative), secondary results, risk assessment, psychosocial assessment; • Education: explain relevant genetic concepts, context of results, and inheritance; • Conclusion: Recommend next steps, provide support resources. UC arm offers in-depth discussion of genetics concepts; expanded range of genetic counseling skills and models to facilitate adaptation to genetic risks and conditions. |
Delivered in-person when possible, or via phone and/or video. Delivered by a certified genetic counselor. |
| NCGENES | Compare UC in the pediatric genetics or pediatric neurology clinic with UC plus receipt of caregiver “pre-visit prep” materials on measures of caregiver-clinician engagement and caregiver efficacy. Intervention arm receives an educational booklet and question prompt list (QPL) prior to first appointment with pediatric genetics or pediatric neurology and another booklet and QPL prior to return of results. Materials are developed by a multidisciplinary team including parent and family advocates and genetic counselors. Outcomes include caregiver/family engagement, clinicians’ perception of family preparedness and engagement, and caregivers’ reported self-efficacy, satisfaction, and perception of the appointment’s patient-centeredness. | UC not defined, but assumed to be the customary care provided by the pediatric and neurology provider teams guided by their clinic leadership and within their scope of practice. This included MDs and GCs (genetics) and MDs (neurology). Content at discretion of providers and followed UC for the clinic. |
Pre-test: Delivered in person by GC or research associate. Post-test: Delivered according to clinicians’ usual practice. For neurology clinic may be in person or telephone by a neurologist. For genetics clinic, typically by phone with occasional in person disclosure by GC or geneticist. |
3.2. Usual care descriptions identified in published systematic review
We initially reviewed all genetic counseling RCTs in the 58 manuscripts presented in the systematic review (Athens, 2017) and summarized the descriptions of usual care. Most studies were conducted in the United States (n = 38), with International studies occurring most often in the United Kingdom (n = 6) and the Netherlands (n = 6). Given our domestic focus for sources of usual care practice, we excluded studies conducted outside the U.S (See full descriptions in Supplementary Table 1). The additional eight RCTs were all U.S.-based, for a total of 46 RCTs to review. Overall, the majority of the U.S.-based RCTs were in the cancer genetics context and focused on either a comparison of modes of genetic counseling delivery or a comparison of genetic counseling content. Almost all papers included at least some description of the usual care or, if they did not, provided a citation to a protocol article that more fully described the usual care arm. We found variation in descriptions of both content and delivery of usual care. Table 2 provides examples of the ways that usual care was presented among the RCTs. Our selected examples are trials in the cancer genetics setting that compared a single genetic counseling intervention to usual care and provided significant detail to illustrate the differences. These differences highlight the variability in how researchers describe usual care and underscore the importance of a consistent definition.
Table 2.
Descriptions of usual care (UC) in select RCTs in the cancer genetics setting
| 1st Author, Year | Study Aim | UC Content | UC Delivery |
|---|---|---|---|
| Charles, 2006 | Compare culturally tailored genetic counseling to standard genetic counseling for BRCA1/2 testing among African American women. | UC lasted 1.5 hours and included: 1) education about hereditary breast and ovarian cancer; 2) the risks associated with and the probability of having a BRCA1/2 mutation; 3) the process of genetic testing for BRCA1/2 mutations (including benefits, limitations, and risks of genetic testing); and 4) interpretation of genetic test results. | In-person delivery, semi-structured with visual aids, by a board-certified genetic counselor. |
| Graves, 2010 | Evaluate the impact of augmenting standard genetic counseling with a psychosocial counseling intervention, consisting of 5 weekly telephone sessions and a mailed booklet. | UC included: 1) a pre-test discussion about hereditary breast and ovarian cancer, mutation testing, and the potential benefits, limitations, and risks of genetic testing; 2) a disclosure session consisting of disclosure of test results, information about the risks of developing cancer, and individualized management strategies. | In-person delivery by genetic counselor. Summary letter and follow-up call 2 weeks post-disclosure. |
| Rousi, 2010 | Evaluate the impact of an enhanced counseling intervention on knowledge about the heritability of breast and ovarian cancer and distress, as a function of BRCA test result among high-risk women. | UC included: standard genetic counseling followed by a general health information session, including current recommendations for general health. | In-person delivery, 45-minutes led by a Health Educator. |
Content of Usual Care.
The descriptions of usual care frequently detailed the content of usual care, most often noting assessment of genetic risk factors, taking family histories, and/or offering testing. A minority included addressing psychological concerns or the risks versus benefits of testing. This element of usual care was typically found in a shared decision-making model of care.
Delivery of Usual Care.
The greatest variation in usual care descriptions was regarding care delivery. Aside from mode (phone/in-person) and type of clinician, descriptions were general and vague with regard to how the provider engaged with the patient/family (see Supplementary Table 1.) Although usual care was typically delivered in person, details such as how the GC approached the patient and how long counseling sessions lasted were sparse. There was wide variation in how usual care was described with no apparent effort to ensure standardization. This significant variation in usual care, beyond differences among subspecialties, threatens the validity and generalizability of genetic counseling research.
3.3. Development of Usual Care in Genetic Counseling Research Definition
While there were minor discrepancies among the core competencies we independently nominated as key to usual care in genetic counseling, there was unanimity in putting forth the items in the ACGC Domains I-III (Accreditation Council for Genetic Counseling, 2019). Domains I-III are topics of expertise needed: genetics expertise and analysis; interpersonal, psychosocial and counseling skills; and education abilities. We then compared the items in these domains to the NSGC Practice Definition (Resta, 2006) and found that the tasks listed in the definition were accounted for in the core competency items we identified. We next considered the Reciprocal Engagement Model (REM) as a practice model in which the relationship between the client and the genetic counselor is at the core and central practice tenets are described (Veach, 2007). The REM served as a framework to embody the tasks from the ACGC core competencies and NSGC definition. We also reviewed expanded practice tenets to ensure that they would be included in our definition (Biesecker, 2020). There was notable overlap in the concepts among these professional sources, such that they facilitated the drafting of a usual care definition of genetic counseling for research. Our review of genetic counseling descriptions from the American College of Medical Genetics and Genomics, the American College of Obstetricians and Gynecologists, the American Society of Clinical Oncology, the National Comprehensive Cancer Network and the American Society of Human Genetics addressed content to be discussed with patients, but not how it should be delivered within a relationship between the provider and patient. Importantly, the content was redundant with that identified in the NSGC practice definition and in the ACGC practice domains, and therefore did not further the usual care definition.
Proposed Definition
Our objective was to fill the need for a definition of usual care for genetic counseling research. We did this by developing a definition of usual care based on existing professionally endorsed resources and augmented by existing descriptors and definitions of clinical practice. The significant overlap across key practice elements led to the generation of a concise proposed definition of usual care for genetic counseling research:
Usual care in genetic counseling relies on a client-centered relationship that is respectful, culturally informed, and empathetic. Personal and family health information is obtained to determine genetic risks while understanding of genomic information is assessed to tailor education. Discussion of recommendations or options for testing and management provides guidance for follow-up. Facilitation of client-centered, value-based decision-making leads to informed choice and identification of coping resources to promote adaptation and psychological well-being.
4. DISCUSSION
Genetic counseling care models are evolving. The limited number of genetic counselors concurrent with the expansion of genomic medicine applications and increased access to genetics services has demanded creativity and experimentation in the development of new and adaptive delivery models of genetic counseling (Biesecker, 2018; Stoll, 2018; Schmidlen, 2019). The diversity of patients accessing clinical genetics care and the integration of genetics/genomics into a wide range of medical disciplines has implications for the variability of what may be considered usual care in genetic counseling.
Genetic counseling research, while going on for decades, remains limited. While randomized clinical trials exist, they have yielded insufficient evidence to adequately inform development of successful novel service delivery models to achieve expanded access and to meet the needs of a more diverse range of clients. The recent call for reporting standards in genetic counseling research represents an important advance for the profession (Hooker, 2017). One of the limitations has been a lack of consensus and reporting on what constitutes usual care in genetic counseling research. As studies expand to represent a wider range of research, consistency in what we mean by usual care will help to interpret the evidence and its implications for clinical practice. As is clear from our review, usual care clinical practice is varied, as is usual care as defined in clinical trials of genetic counseling interventions. This variance limits our ability to compare study outcomes and to gather sufficient consistent evidence that specific service delivery models are clearly more effective and efficient than others. Without more consistency in research questions, outcomes assessed (Athens, 2017), and in the definition of usual care in randomized control trials of genetic counseling interventions, the generation of useful evidence will lag.
The proposed usual care definition complements the NSGC practice definition. They differ in that the usual care definition is relationship-based (per the REM), while the NSGC definition emphasizes the main tasks of genetic counseling (Resta, 2006). Further, the usual care definition characterizes how the tasks in the NSGC definition are implemented. Similarities in the definitions are key if usual care in genetic counseling research is to represent clinical practice.
The process of standardizing delivery of usual care in genetic counseling research may be challenging given the variation in individual styles of genetic counselors, and care priorities that vary across clinical settings (i.e., cancer, prenatal, cardiac, pediatrics). Yet, genetic counseling process studies have suggested there is consistency across genetic counselors and contexts in terms of the proportion of time spent on education/provision of genetic information over psychological counseling, and the relatively high literacy level at which counseling is provided (e.g. Roter, 2006; Joseph, 2017, Ellington, 2011, 2006, and 2005; Meiser, 2008). Procedures to monitor and ensure fidelity to both the intervention and usual care genetic counseling arms of a randomized study could help to demystify usual care practices, and reporting on the processes as well as outcomes (e.g. using mixed methods study designs) could improve overall understanding of the scope of genetic counseling practice, how it is conducted, and its outcomes. Strategies used to provide consistency within each study arm (e.g. fidelity checklists, review of audio recordings etc.) could also provide more evidence on what researchers intend by usual care; however, caution is warranted. We do not want to suggest a scripted interaction that is likely to fail to address the individual client’s needs; however, implementing a minimum checklist could be valuable. Our usual care definition lends itself to a minimal checklist, shown in Figure 1. The National Institutes of Health’s 2021 commitment to fund extramural research in genetic counseling (see RFA-HG-20-048, ‘Investigator-Initiated Research on Genetic Counseling Processes and Practices’) confirmed that the time is right to design studies with attention to what counts as usual care in order to enhance how we evaluate new interventions.
Figure 1.
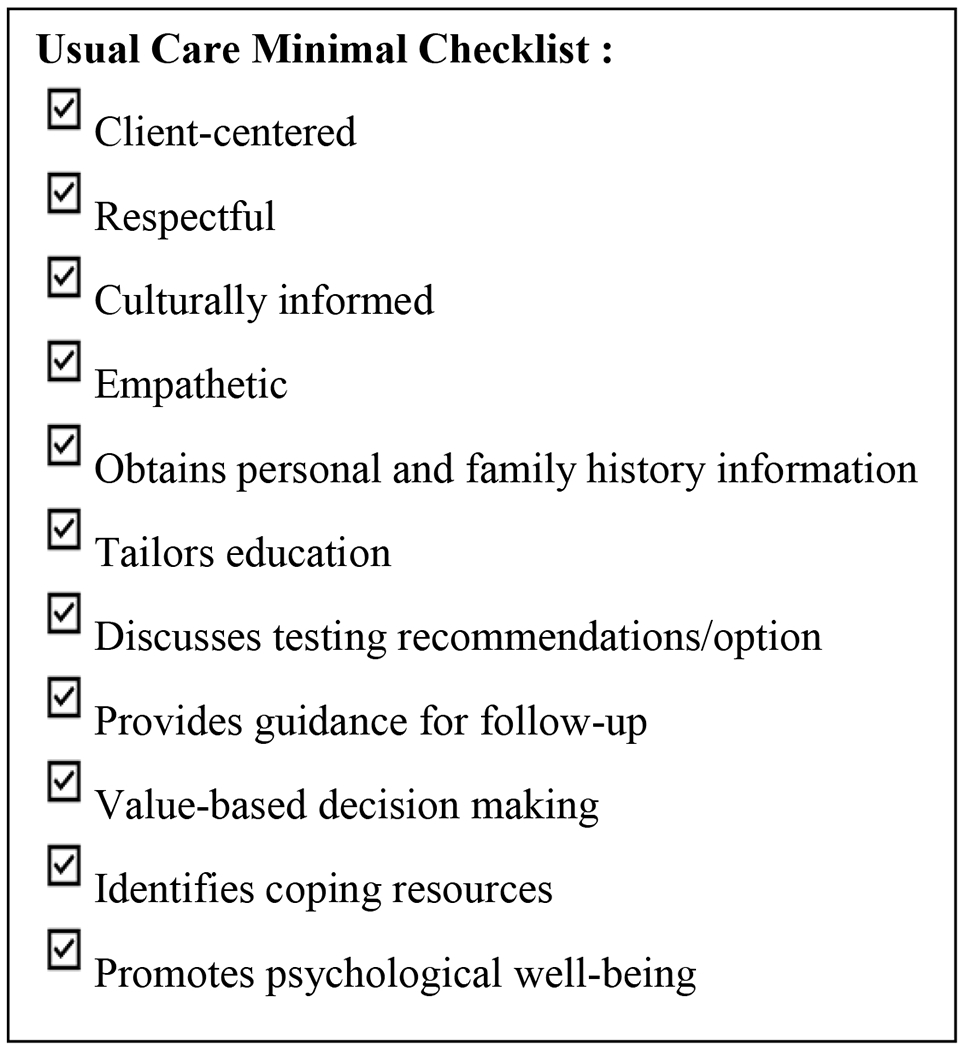
Minimal Checklist for Usual Care
4.1. Limitations
Our review is based on the RCTs in the CSER consortium, those previously identified by Athens et al. (2017) and eight subsequent RCTs. It was within the CSER consortium that the authors came to appreciate that what was referenced as ‘usual care’ differed significantly among our studies. This offered a contemporary example among genomic sequencing studies of evidence that usual care in genetic counseling research differed remarkably. We then searched the literature and found no definition of what constituted usual care in genetic counseling, identifying a research gap we aimed to address. The systematic literature review covering 25 years of RCTs provided further examples of the variation in usual care. This supported our observation among the CSER studies. We did not further investigate genomic consortia studies as we had a remarkable degree of variation between the CSER studies and the published RCTs. We anticipate that the definition will evolve over time as further research is needed to provide evidence of what is, or ought to be, most consistently actualized in usual care arms of genetic counseling. Although there have been more recent RCTs since the publication of the systematic review, using Athens et al. as our source allowed us to take a broad view of the literature. In order to address this limitation, we identified eight U.S.-based RCTs that have been published after the Athens review. These more recent RCTs followed the pattern of the RCTs identified previously; namely, variation in the descriptions of both content and delivery of usual care, highlighting the importance of a consistent definition (see Supplementary Table 1b for these additions). Additionally, we acknowledge that the rigor of the usual care descriptions found in published RCTs may have been constrained artificially by manuscript word limits.
4.2. Research Recommendations
As investigators from a variety of professional backgrounds design and conduct studies in genetic counseling, assumptions are made about what constitutes usual care that may or may not reflect clinical practice. Genetic counselors knowledgeable about practice elements are well-equipped to define usual care to inform genetic counseling research. With researchers turning their attention to interventions, using the proposed definition of usual care in genetic counseling research to inform the design of studies will help to ensure that practice elements in the study do not introduce threats to validity. Consistent use of usual care in the design of trials will further help genetic counseling research to more accurately represent clinical care and will facilitate the generation of evidence to improve this research, and ultimately the care of patients accessing genetics counseling services.
4.3. Practice Implications
This review identifies inconsistency in how usual care in genetic counseling is actualized in research. Since genetic counseling research is used to inform practice, care needs to be taken when incorporating interventions from research involving usual care. Our proposed definition of usual care in genetic counseling research will help to yield more consistency in the design of studies aimed at generating evidence to improve clinical care.
Supplementary Material
What is known about this topic?
Despite recent standards for reporting genetic counseling research in the peer-reviewed literature, there exists no guidance on what constitutes usual care in genetic counseling research.
What this paper adds to the topic:
We propose a definition of usual care in genetic counseling research. This definition is supported by our review of Clinical Sequencing Evidence-Generating Consortium studies and the published literature of randomized control trials in genetic counseling, and of existing professionally endorsed definitions and practice descriptions of genetic counseling.
Acknowledgements
Research reported in this publication was supported by the National Human Genome Research Institute, the National Cancer Institute and the National Institute on Minority Health and Health Disparities of the National Institutes of Health under Award Numbers U01 HG007301, U01 HG009599, U01 HG009610, U01 HG006487, U01 HG006485, and U24 HG007307. Funding was also provided by the NHGRI Intramural Research Program (KL) and RTI International (BBB, SL). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of Interest
Barbara B. Biesecker, Sarah E. Lillie, Laura M. Amendola, Katherine E. Donohue, Kelly M. East, Ann Katherine M. Foreman, Marian J. Gilmore, Veronica Greve, Billie Liangolou, Julianne M. O’Daniel, Jacqueline A. Odgis, Shannon Rego, Bradley Rolf, Sarah Scollon, Sabrina A. Suckiel, Jamilyn Zepp and Galen Joseph declare that they have no conflict of interest.
Human Studies and Informed Consent
No human studies were carried out by the authors for this article.
Animal Studies
No non-human animal studies were carried out by the authors for this article.
Data Availability
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
References
- Abacan M, Alsubaie L, Barlow-Stewart K, Caanen B, Cordier C, Courtney E, … Wicklund C (2019). The Global State of the Genetic Counseling Profession. European Journal of Human Genetics, 27, 183–197. 10.1038/s41431-018-0252-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Accreditation Council for Genetic Counseling Practice-Based Competencies for Genetic Counselors. (2019). Retrieved from https://www.gceducation.org/wp-content/uploads/2019/06/ACGC-Core-Competencies-Brochure_15_Web_REV-6-2019.pdf. [DOI] [PubMed]
- Athens BA, Caldwell SL, Umstead KL, Connors PD, Brenna E, & Biesecker BB (2017). A systematic review of randomized controlled trials to assess outcomes of genetic counseling. Journal of Genetic Counselling, 26, 902–933. doi: 10.1007/s10897-017-0082-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amendola LM, Berg JS, Horowitz CR, Angelo F, Bensen JT, Biesecker BB, … & Fullerton SM (2018). The clinical sequencing evidence-generating research consortium: integrating genomic sequencing in diverse and medically underserved populations. The American Journal of Human Genetics, 103, 319–327. doi: 10.1016/j.ajhg.2018.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arch JJ, & Stanton AL (2019). Examining the “usual” in usual care: a critical review and recommendations for usual care conditions in psycho-oncology. Supportive care in cancer: official journal of the Multinational Association of Supportive Care in Cancer, 27, 1591–1600. 10.1007/s00520-019-04677-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Au DH, Castro M, & Krishnan JA (2007). Selection of controls in clinical trials: introduction and conference summary. Proceedings of the American Thoracic Society, 4, 567–569. doi: 10.1513/pats.200707-099JK. [DOI] [PubMed] [Google Scholar]
- Ayling K, Brierley S, Johnson B, Heller S, & Eiser C (2015). How standard is standard care? Exploring control group outcomes in behaviour change interventions for young people with type 1 diabetes. Psychology & Health, 30, 85–103. doi: 10.1080/08870446.2014.953528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biesecker B (2020). Genetic counseling and the central tenets of practice. Cold Spring Harbor Perspectives in Medicine, 10, a038968. doi: 10.1101/cshperspect.a038968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biesecker BB, Lewis KL, Umstead KL, Johnston JJ, Turbitt E, Fishler KP, Patton JH, …& Biesecker LG (2018). Web platform vs in-person genetic counselor for return of carrier results from exome sequencing: A randomized clinical trial. JAMA Internal Medicine, 178, 338–346. doi: 10.1001/jamainternmed.2017.8049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charles S, Kessler L, Stopfer JE, Domchek S, & Halbert CH (2006). Satisfaction with genetic counseling for BRCA1 and BRCA2 mutations among African American women. Patient Education and Counseling, 63, 196–204. doi: 10.1016/j.pec.2005.10.007. [DOI] [PubMed] [Google Scholar]
- Ellington L, Kelly KM, Reblin M, Latimer S, & Roter D (2011). Communication in genetic counseling: cognitive and emotional processing. Health Communication, 26, 667–675. doi: 10.1080/10410236.2011.561921. [DOI] [PubMed] [Google Scholar]
- Ellington L, Baty BJ, McDonald J, Venne V, Musters A, Roter D, … & Croyle RT (2006). Exploring genetic counseling communication patterns: the role of teaching and counseling approaches. Journal of Genetic Counseling, 15, 179–189. doi: 10.1007/s10897-005-9011-6. [DOI] [PubMed] [Google Scholar]
- Ellington L, Roter D, Dudley WN, Baty BJ, Upchurch R, Larson S, …& Botkin JR (2005). Communication analysis of BRCA1 genetic counseling. Journal of Genetic Counseling, 14, 377–386. doi: 10.1007/s10897-005-3660-3. [DOI] [PubMed] [Google Scholar]
- Freedland KE, Mohr DC, Davidson KW, & Schwartz JE (2011). Usual and unusual care: existing practice control groups in randomized controlled trials of behavioral interventions. Psychosomatic Medicine, 73, 323–335. doi: 10.1097/PSY.0b013e318218e1fb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold SM, Enck P, Hasselmann H, Friede T, Hegerl U, Mohr DC, & Otte C (2017). Control conditions for randomised trials of behavioural interventions in psychiatry: a decision framework. The Lancet Psychiatry 4, 725–732. doi: 10.1016/S2215-0366(17)30153-0. [DOI] [PubMed] [Google Scholar]
- Graves KD,Wenzel L, Schwartz MD, Luta G,Wileyto P, Narod S,….& Halbert CH (2010). Randomized controlled trial of a psychosocial telephone counseling intervention in BRCA1 and BRCA2 mutation carriers. Cancer Epidemiology, Biomarkers & Prevention, 19, 648–654. doi: 10.1158/1055-9965.epi-09-0548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hippman C, Ringrose A, Inglis A, Cheek J, Albert AYK, Remick R, …& Austin JC (2016). A pilot randomized clinical trial evaluating the impact of genetic counseling for serious mental illnesses. Journal of Clinical Psychiatry, 77, e190–e198. doi: 10.4088/JCP.14m09710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooker GW, Babu D, Myers MF, Zierhut H & McAllister M (2017). Standards for the Reporting of Genetic Counseling Interventions in Research and Other Studies (GCIRS): an NSGC Task Force Report. Journal of Genetic Counseling, 26, 355–360. doi: 10.1007/s10897-017-0076-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ison HE, Ware SM, Schwantes-An TH, Freeze S, Elmore L, & Spoonamore KG (2019). The impact of cardiovascular genetic counseling on patient empowerment. Journal of Genetic Counseling, 28, 570–577. doi: 10.1002/jgc4.1050. [DOI] [PubMed] [Google Scholar]
- Joseph G, Pasick RJ, Schillinger D, Luce J, Guerra C, & Cheng JKY (2017). Information mismatch: cancer risk counseling with diverse underserved patients. Journal of Genetic Counseling, 26, 1090–1104. doi: 10.1007/s10897-017-0102-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph G, Lee R, Pasick RJ, Guerra C, Schillinger D, & Rubin S (2019). Effective communication in the era of precision medicine: A pilot intervention with low health literacy patients to improve genetic counseling communication. European Journal of Medical Genetics, 62, 357–367. doi: 10.1016/j.ejmg.2018.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinney AY, Steffen LE, Brumbach BH, Kohlmann W, Du R, Lee JH, … & Campo RA (2016). Randomized noninferiority trial of telephone delivery of BRCA1/2 genetic counseling compared with in-person counseling: 1-year follow-up. Journal of Clinical Oncology, 34, 2914. doi: 10.1200/JCO.2015.65.9557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAllister M, Wood AM, Dunn G, Shiloh S, & Todd C (2011). The Genetic Counseling Outcome Scale: a new patient-reported outcome measure for clinical genetics services. Clinical Genetics, 79, 413–424. 10.1111/j.1399-0004.2011.01636.x. [DOI] [PubMed] [Google Scholar]
- Meiser B, Irle J, Lobb E, & Barlow-Stewart K (2008). Assessment of the content and process of genetic counseling: a critical review of empirical studies. Journal of Genetic Counseling, 17, 434–451. doi: 10.1007/s10897-008-9173-0. [DOI] [PubMed] [Google Scholar]
- Mohr DC, Ho J, Hart TL, Baron KG, Berendsen M, Beckner V, … Kinsinger SW (2014). Control condition design and implementation features in controlled trials: a meta-analysis of trials evaluating psychotherapy for depression. Translational Behavioral Medicine 4, 407–423. doi: 10.1007/s13142-014-0262-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resta R, Biesecker BB, Bennett RL, Blum S, Hahn SE, Strecker MN, & Williams JL (2006). A new definition of Genetic Counseling: National Society of Genetic Counselors’ Task Force report. Journal of Genetic Counseling, 15, 77–83. doi: 10.1007/s10897-005-9014-3. [DOI] [PubMed] [Google Scholar]
- Riddle L, Amendola LM, Gilmore M, Guerra C, Biesecker BB, Kauffman TL, … & Goddard KAB Development and early implementation of a literacy-focused genetic counseling model for disclosure of clinical exome sequencing results. Patient Education and Counseling. [under review]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roter D, Ellington L, Erby LH, Larson S, & Dudley W (2006). The Genetic Counseling Video Project (GCVP): Models of practice. American Journal of Medical Genetics Part C: Seminars in Medical Genetics, 142C, 209–220. doi: 10.1002/ajmg.c.30094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidlen T, Schwartz M, DiLoreto K, Kirchner HL, & Sturm AC (2019). Patient assessment of chatbots for the scalable delivery of genetic counseling. Journal of Genetic Counseling, 28, 1166–1177. doi: 10.1002/jgc4.1169. [DOI] [PubMed] [Google Scholar]
- Schwartz MD, Peshkin BN, Isaacs C, Willey S, Valdimarsdottir HB, Nusbaum R, … & Heinzmann J (2018). Randomized trial of proactive rapid genetic counseling versus usual care for newly diagnosed breast cancer patients. Breast Cancer Research and Treatment, 170, 517–524. doi: 10.1007/s10549-018-4773-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz MD, Valdimarsdottir HB, Peshkin BN, Mandelblatt J, Nusbaum R, Huang AT, …& King L (2014). Randomized noninferiority trial of telephone versus in-person genetic counseling for hereditary breast and ovarian cancer. Journal of Clinical Oncology, 32, 618–626. doi: 10.1200/jco.2013.51.3226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smelt AF, van der Weele GM, Blom JW, Gussekloo J, & Assendelft WJ (2010). How usual is usual care in pragmatic intervention studies in primary care? An overview of recent trials. The British Journal of General Practice, 60, e305–e318. doi: 10.3399/bjgp10X514819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoll K, Kubendran S, & Cohen SA (2018). The past, present and future of service delivery in genetic counseling: keeping up in the era of precision medicine. American Journal of Medical Genetics Part C: Seminars in Medical Genetics, 178, 24–37. doi: 10.1002/ajmg.c.31602. [DOI] [PubMed] [Google Scholar]
- van der Graaf R, & van Delden JJ (2009). What is the best standard for the standard of care in clinical research? American Journal of Bioethics, 9, 35–43. doi: 10.1080/15265160802654129. [DOI] [PubMed] [Google Scholar]
- Veach PM, Bartels DM, & Leroy BS (2007). Coming full circle: a reciprocal-engagement model of genetic counseling practice. Journal of Genetic Counseling, 16, 713–728. doi: 10.1007/s10897-007-9113-4. [DOI] [PubMed] [Google Scholar]
- Young HM, Miyamoto S, Tang-Feldman Y, Dharmar M, Balsbaugh T, & Greenwood D (2020). Defining Usual Care in Clinical Trials. Research in Gerontological Nursing, 13, 125–129. doi: 10.3928/19404921-20191127-01. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


