Abstract
Background:
The changing prevalence and patterns of tobacco use, the advent of novel nicotine delivery devices, and the development of new biomarkers prompted an update of the 2002 Society for Research on Nicotine and Tobacco (SRNT) report on whether and how to apply biomarker verification for tobacco use and abstinence.
Methods:
The SRNT Treatment Research Network convened a group of investigators with expertise in tobacco biomarkers to update the recommendations of the 2002 SNRT Biochemical Verification Report.
Results:
Biochemical verification of tobacco use and abstinence increases scientific rigor and is recommended in clinical trials of smoking cessation, when feasible. Sources, appropriate biospecimens, cutpoints, time of detection windows and analytic methods for carbon monoxide, cotinine (including over the counter tests), total nicotine equivalents, minor tobacco alkaloids, and 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol are reviewed, as well as biochemical approaches to distinguishing cigarette smoking from use of electronic nicotine delivery devices (ENDS).
Conclusions:
Recommendations are provided for whether and how to use biochemical verification of tobacco use and abstinence. Guidelines are provided on which biomarkers to use, which biospecimens to use, optimal cutpoints, time windows to detection, and methodology for biochemical verifications. Use of combinations of biomarkers is recommended for assessment of ENDS use.
Implications:
Biochemical verification increases scientific rigor, but there are drawbacks that need to be assessed to determine whether the benefits of biochemical verification outweigh the costs, including the cost of the assays, the feasibility of sample collection, the ability to draw clear conclusions based on the duration of abstinence, and the variability of the assay within the study population. This paper provides updated recommendations from the 2002 SRNT report on whether and how to use biochemical markers in determining tobacco use and abstinence.
Introduction
Whether to employ biochemical verification of cigarette smoking (i.e., as a study inclusion criterion) or abstinence (i.e., as a treatment outcome) is a critical decision for tobacco researchers. The pros of biochemical verification include the potential for increased rigor and validity compared to self-reported smoking abstinence. However, biochemical verification has limitations, including the inability to confirm long-term abstinence, implementation challenges, cost, and the need for analysis plans to address missing verification data. The goal of this paper is to provide the necessary technical information regarding biochemical markers of various forms of tobacco use to allow researchers to make this important decision.
Is Bioverification of Baseline Smoking Status Necessary?
Smoking cessation clinical trials typically and laboratory studies sometimes require that participants report a minimal level of smoking exposure (e.g., 5 or 10 cigarettes per day). Researchers must decide whether biochemical verification of smoking status is necessary to ensure that participants are, indeed, smokers. This practice may be particularly important for trials that involve contingency management or trials involving switching to alternative tobacco products (e.g., electronic cigarettes) that require biochemical verification of reduced exposure. Thus, some researchers have included bioverification as an inclusion criterion.1,2
Is Bioverification of Quitters Necessary?
Identifying participants who have quit smoking is a critical smoking cessation clinical trial outcome. In the 2002 SRNT Subcommittee on Biochemical Verification paper, the authors stated that, “Biochemical verification has been generally recommended for clinic-based randomized trials.3 However, empirical data have been lacking to support this recommendation.” In the absence of special circumstances, self-report has often been considered adequate, especially in large trials. This practice has often been justified by a historically low rate of nonvalidation of self-reported abstinence in the general population of smokers, typically less than 5%.4-6 However, a 1994 meta-analysis of 51 comparisons between self-report and biochemical verification revealed a mean sensitivity of 89%, meaning 11% of participants were not able to biochemically confirm abstinence.7 The idea that 1 in 10 smokers report abstinence that cannot be biochemically verified would suggest the need for this additional step in validating the primary outcome of treatment studies. More recently, a clinical trial reported carbon monoxide (CO) verified abstinence rates that were less than half of the self-reported rates (e.g., 6.0% vs. 18.4%),8 suggesting that misreporting may be more common than previously thought.
Special attention to the need for validation has often been based on characteristics of the population being studied, the type of intervention (e.g., minimal contact vs. face-to-face clinical contact), and demand characteristics (e.g., bogus pipeline effects).9 For instance, biochemical verification is considered especially important for smokers who may be especially vulnerable to demand characteristics10 and those who have demonstrated high misclassification rates (smokers who are classified as nonsmokers), including smokers who have participated in an intensive cessation trial,8 those with medical conditions related to smoking, for example, those with cancer, respiratory disease, cardiovascular disease, women who are pregnant,11-16 veterans,17 hospitalized smokers,18,19 smokers with no more than a high school education, young smokers (both due to lighter smoking and tendency to misreport),20 smokers who are not White (vs. White), and those with incomes of less than $20 000.8 The growing number of specific treatment groups and other individual difference variables that are related to a lack of biochemical verification of abstinence lends further support to the recommendation to include biochemical verification of abstinence in treatment study protocols, whenever feasible. One option to reduce the burden on both research resources and participants is to attempt to collect biochemical verification data from a subsample of the participants rather than the entire sample. We recognize that in some research designs, such as quitline-based cessation trials, biochemical validation may not be feasible.
History of Biochemical Verification Recommendations
In 2002, the first SRNT Subcommittee on Biochemical Verification assessed the utility of biomarkers of tobacco use and cessation and made recommendations for their application in clinical trials.3 Since this report was published, the nicotine and tobacco landscape has changed greatly. The prevalence of cigarette smoking has continued its decline and the proportion of light smokers among active smokers has increased.21 Nonsmokers’ exposure to other people’s smoke has decreased substantially,22 reflecting policy changes on smoking in public places and the wider adoption of home smoking rules. Analytic sensitivity for some biomarkers has increased, and some new biomarkers have been developed. New analyses of the population distribution of some biomarkers have been performed, potentially leading to updated recommendations for cutpoints to discriminate smoking status.23 The advent of electronic nicotine delivery systems (ENDS), heat-not-burn and other novel nicotine consumer products, is transforming the ways nicotine is consumed across the world, leading to new challenges in ascertaining nicotine and tobacco use status. No longer will the question be simply: have people quit cigarettes (with or without the aid of nicotine replacement), but have they transitioned partially or completely to a noncombustible form of nicotine delivery, and how is that move reflected in exposure markers? Given these changes, it is timely to revisit these issues in an updated report.
This update of the 2002 paper, based on the authors’ review of relevant published literature through the end of 2018, discusses the recognized biomarkers of tobacco exposure, including their sources, selection of biofluids for testing and biospecimen handling, sources of interindividual variability and analytic chemistry considerations. We also review the time window within which each biomarker is able to assess tobacco use after cessation of such use. The window of detection depends on the initial biomarker level prior to cessation, the half-life of the biomarker, and the cutpoint that is used to determine nonsmoking. Half-life refers to the time it takes for blood levels of a biomarker to decline by 50%. Thus, after one, two, three, and four half-lives, the blood levels of a biomarker would be 50%, 25%, 12.5%, and 6.25%, respectively (Figure 1). Finally, we review biomarkers of noncombusted tobacco products, including ENDS. For a recent detailed review of biomarkers of tobacco exposure in general, the reader is referred to Schick et al.24
Figure 1.
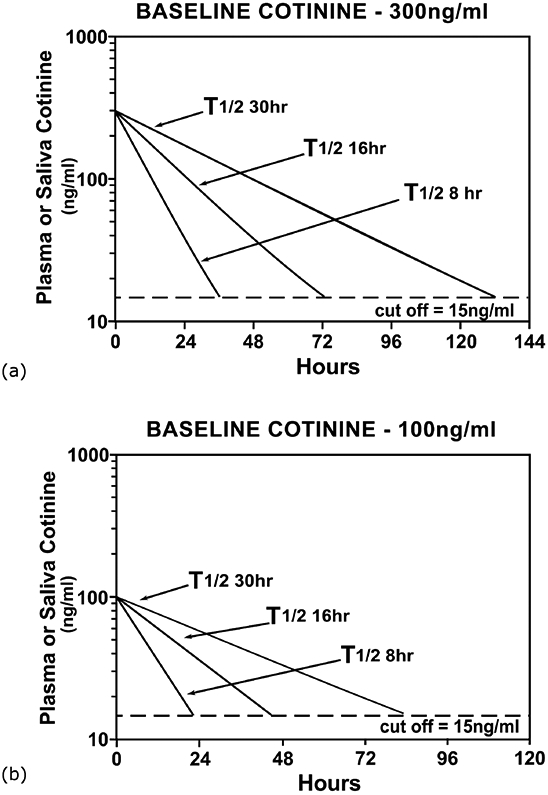
(a) Simulated blood or saliva cotinine concentrations over time, assuming an initial concentration of 300 ng/ml, and different half-lives. The dashed line represents a nonsmoking cotinine level cutoff of 15 ng/ml. Cutoff would be reached at 130, 70, and 35 hours if cotinine half-life was 30, 16, and 8 hours, respectively. (b) Similar simulation to (a) but starting from a baseline cotinine level of 100 ng/ml. Cutoff would be reached at 83, 44, and 22 hours if cotinine half-life was 30, 16, and 8 hours, respectively. Reprinted with permission from Benowitz N, Jacob P, Ahijevych K, et al. Biochemical verification of tobacco use and cessation. Nicotine and Tobacco Research. 2002; 4:149–159.
The authors also recommend optimal cutpoints to distinguish active smoking from not smoking, where possible, for each biomarker (Table 1). Cutpoints are informed by consideration of sensitivity (the ability of a test to correctly identify those who are smokers, i.e., true positive rate), specificity (the ability of the test to correctly identify nonsmokers, i.e., true negative rate), positive predictive value (the probability that smokers who exceed the cutpoint are indeed smoking), and negative predictive value (the probability that smokers who do not exceed the cutpoint are indeed abstinent). Ideally, data on sensitivity, specificity, and positive and negative predictive values would be used to estimate cutpoints but, unfortunately, such information is not always available. Thus, the term cutpoint is not as definitive as the name suggests, and data from a given study should be considered in the context of the study population and study limitations.
Table 1.
Cutpoints and time after smoking cessation to reach cutpoint to distinguish smokers and nonsmokers (based on average precessation levels, cigarette smoking, and U.S. population data)
| Detects | Cutpoint | Average half-life | Approximate time to cutpoint |
||
|---|---|---|---|---|---|
| Free cotinine plasma, saliva, and urinea | Exposure to nicotine from all sources (e.g., combustible, noncombustible, and NRT) | 3–10 ng/ml 30–50 ng/ml |
16 h | 80–100 h | |
| CO (exhaled air) | Consumption of combustible tobacco and nontobacco (e.g., marijuana) products | 5–6 ppmb | 2–8 h depends on physical activity level |
12–24 h | |
| Minor tobacco alkaloids (urine) | Exposure to tobacco-derived nicotine products (e.g., cigarettes, cigars, and smokeless) | Anabasine Anatabine Nicotelline |
2 ng/ml 2 ng/ml ? |
16 h 10 h 2–3 h |
80 h 50 h 10 h |
| NNAL (urine) | Exposure to cured tobacco (e.g., cigarrettes, cigars, and smokeless) | 10–40 pg/ml | 10–40 days | 2–3 months |
NNAL = 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol; NRT = nicotine replacement therapy.
Urine provides the highest concentration of cotinine and, thus, has the greatest sensitivity but also more between-sample variability. Plasma and saliva provide similar results, with lower concentrations, but with more between-sample stability.
At one end of the continuum (e.g., in a country with high smoking prevalence and relatively weak legislation requiring smoke-free public places in industrial cities with high levels of air pollution), we recommend that the previous cutpoint of <10 ppm to validate a self-report of smoking abstinence for at least 24 h may still be appropriate. At the other end of the continuum (e.g., in places with strong smoke-free legislation, low smoking prevalence and relatively low levels of air pollution), we recommend that a cutpoint as low as <5 ppm will be more appropriate. Investigators should select the appropriate cutpoint (from 4 to 10 ppm) for their research and clinical purposes bearing these known factors (as well as brand/model of monitor) in mind.25
Biochemical Verification of Tobacco Use and Cessation Using CO
Burning organic matter gives rise to CO as a byproduct of combustion. CO can be used as an indicator of recent smoke absorption from combustible tobacco products (cigarettes, cigars, pipes, and hookah) but not smokeless tobacco or most ENDS. The concentration of CO can be measured in exhaled breath (eCO) in parts per million (ppm) or in blood (carboxyhemoglobin in percent hemoglobin saturation). These two methods are very highly correlated (e.g., r = 0.95).26 Exhaled CO can be measured easily using a relatively inexpensive portable device and has become a widely used method for assessing tobacco smoke exposure and validating selfreports of smoking cessation.
CO is also present in ambient air that contains common pollutants (e.g., automobile exhaust and smoke from home barbeques). CO can also be produced in the human body (largely via hemeoxygenase-1); however, endogenous formation typically only contributes 1–2 ppm.27 Therefore, CO levels need to be assessed in the context of potential environmental exposures. In countries that largely ban smoking in public places and have relatively strong prohibitions on air pollution, nonsmokers typically have eCO in the lower part of the range 0–5 ppm.28 However, in large industrial cities in countries without comprehensive smoke-free air policies, neversmokers often have eCO readings in the range 2–8 ppm.29,30 Smoking marijuana is also a potential source, producing CO levels similar to tobacco smoking, and information on recent marijuana smoking should be elicited if possible when measuring CO levels in research studies.31 CO typically has a half-life of around 4 hours, but this half-life is influenced by pulmonary ventilation and, therefore, by exercise,32 with a half-life of 2 hours during exercise and as long as 8–10 hours during sleep.33 Thus, CO may reach a “nonsmoking” cutpoint in a regular smoker in 6–24 hours, depending on activity, and light and intermittent smokers will often have an exhaled CO level below 6 ppm.34
The 2002 SRNT Subcommittee on Biochemical Verification report recommended cutpoints for eCO to distinguish a smoker from someone who is abstinent in the range 8–10 ppm.3 Since that time, however, several studies have presented data suggesting that a lower eCO cutpoint would be more accurate. Perkins et al studied 261 adult smokers who attempted to quit smoking over 5 days on two separate occasions, with smoking and eCO being recorded on each day.35 A cutpoint of <5 ppm was able to detect smoking days with 83% sensitivity and verify nonsmoking days with 87% specificity, whereas a cutpoint of <9 ppm had only 60% sensitivity and 97% specificity to detect nonsmoking in the past 24 hours. This study used a BreathCO (MD Spiro, Lewiston, ME) CO monitor following a 20-second breath hold and did not include cotinine validation. A similar study by Javors et al using a Vitalograph CO monitor (Lenexa, KS) found the highest combined sensitivity and specificity with a CO criterion of <3 ppm. Other clinical trials using simultaneous cotinine validation also recommended reducing the CO cutpoint. Cropsey et al studied the relationship between eCO (using a Vitalograph monitor) and urine cotinine (using a qualitative OTC COT device)36 among 662 participants in a smoking cessation clinical trial, all under some form of criminal justice supervision in the community. This study found that a CO cutoff of <3 ppm most ac-curately distinguished smokers from nonsmokers (97% correct classification). Emery and Levine assessed eCO (using a Vitalograph monitor) and saliva cotinine (Salimetrics LLC; cutpoint of <15 ng/ mL) in a relapse prevention trial among 208 postpartum women and found that cutpoints of <2 ppm or <3 ppm (at different timepoints) had higher sensitivity plus specificity than higher eCO cutpoints when compared to saliva cotinine.37
Exhaled CO levels are influenced by breathing rate (minute ventilation); since minute ventilation increases in pregnancy, the optimal eCO cutpoint to verify abstinence might need to be lower in pregnancy. Higgins et al measured both eCO and urine cotinine at the same timepoints throughout a clinical trial.38 Classifications of smoking status based on eCO were in relatively poor agreement with cotinine (which has a much longer half-life than CO) at the same timepoints. Sensitivity and specificity (<87%) for eCO was best at 4 ppm. Another study comparing self-report status to eCO levels in pregnant women showed that, using a cutpoint of 8 ppm, only 1% of nonsmokers were incorrectly identified as smokers, but only 56% of smokers were identified as such.39 At 4 ppm, 8% of nonsmokers were identified as smokers but 90% of smokers were identified correctly.
One caveat in recommending a single “gold standard” cutpoint for eCO is that CO readings may differ when using different types of eCO monitors.25,40 Karelitz et al reported a literature search from 2004 to 2014 using keywords “CO monitor” and “smoking” and found that 58% of the studies did not report the type of CO monitor used. Of the 311 studies that disclosed the type of monitor, 61% used a Bedfont monitor and 35% used a Vitalograph. Karelitz et al studied 78 smokers who were attempting to abstain from smoking.25 Participants provided eCO samples using both the Bedfont piCO+ Smokerlyzer (Kent, UK) and the Vitalograph BreathCO monitors, collected 5–10 minutes apart, using the manufacturer’s in-structions, plus instructions to exhale slowly for consistency. The Bedfont monitor gave mean eCO readings 3.8 ppm higher than the Vitalograph monitor, although the difference was smaller (1.7 ppm) among those who reported abstaining in the prior 12–24 hours compared to those who were smoking regularly (mean difference = 5.6 ppm). Importantly, when the Vitalograph values were <5 ppm, only 48.5% of the Bedfont values were also <5 ppm. These differences may have related to the particular model of the Bedfont monitor. We recommend that different types of monitors should not be used interchangeably in the same study, and the optimal cutpoints from studies that used the Vitalograph CO monitor may not apply to other models of monitors as noted above for the Bedfont piCO model used in the Karelitz et al study.
Given the multiple factors influencing eCO in addition to recent tobacco smoking (e.g., environmental exposure and type of eCO monitor), rather than recommending a specific cutpoint for distinguishing recent tobacco smokers from nonsmokers, we prefer to recommend a range of reasonable cutpoints, along with suggestions of situations in which these cutpoints may be appropriate. The choice to use one cutoff over another will depend, in part, on the purpose of assessing smoking status. For example, it may be preferred to use a lower CO cutoff of <3 ppm when smoking is an important exclusion criterion (e.g., attempting to exclude pregnant smokers from a trial of a new drug). Alternatively, studies aimed at evaluating new smoking cessation interventions may prefer to use a higher CO cutoff (e.g., <6 ppm) to reduce the risk of incorrectly rejecting successful approaches.37 We also recommend that authors of research papers in which eCO is measured always report the brand and model of the monitor used in the study. See Table 1 for our range of recommendations.
Nicotine Metabolites: Cotinine and Total Nicotine Equivalents
All tobacco products deliver nicotine to the user, making nicotine a highly specific biomarker of use of tobacco products, ENDS, or nicotine replacement products. However, due to its relatively short half-life (about 2 hours), nicotine is not a very useful quantitative indicator of nicotine intake. Cotinine is the major proximate metabolite of nicotine and is the most widely used biomarker of nicotine intake.41 The half-life of cotinine can vary from 8 to 30+ hours due to genetic, hormonal, and other factors as discussed in detail later in this section. Assuming an initial cotinine blood level of 200 ng/mL, it would take five half-lives for the level to decline below 5 ng/ mL (Figure 1). For individuals with half-lives of 8, 16, or 30 hours, it would take 40, 90, and 150 hours to reach the cutpoint. Therefore, a smoker who has a short cotinine half-life could have a cotinine level below cutpoint in only 2 days but, given the potential for a long half-life, to minimize false positivity, it is reasonable to allow 6–7 days to assess compliance with nonsmoking.
Cotinine can be measured in a variety of biological fluids, including blood (serum, plasma, or whole blood), saliva, and urine. Cotinine is present in biological fluids as free cotinine and cotinine glucuronide. Serum and saliva levels are generally reported as free cotinine, while urine values may be reported as either free cotinine or the sum of the free and glucuronide forms, termed total cotinine. Serum levels of free cotinine in daily smokers typically average from 100 to 250 ng/mL, while levels in those exposed to secondhand smoke (SHS) are usually <3 ng/mL.23 Concentrations in saliva and blood are highly correlated; saliva/plasma ratios range from 1.04 to 1.27 in different studies.4,42-44 Saliva cotinine concentration is affected by salivary flow rate; higher flow rates result in lower concentrations. Urine and blood concentrations are also highly correlated but not as strongly as saliva and blood. The average urine/plasma ratio for urinary free cotinine to plasma cotinine is 4.6 (4.0–5.3), and the ratio is influenced by urine flow rate and urine pH.45 Thus, urine cotinine has a higher cutpoint than blood or saliva (see Table 1).
The optimal cutpoint to distinguish cigarette smokers from nonsmokers is influenced by the prevalence and intensity of SHS exposure and may also be affected by race and physiologically related metabolic differences. The most recent large-scale analysis of the optimal cutpoint in the United States was based on the participants in the National Health and Nutrition Examination Survey (NHANES) from 1990 to 2004.23 Data from 3078 smokers and 13 078 nonsmokers were analyzed using the receiver operator curve approach. Based on self-reported smoking status of cigarette smoking or not smoking, the optimal cutpoint for serum cotinine among adults was 3 ng/mL (sensitivity 96.3; specificity 97.4%). Racial/ethnic differences in cutpoints were observed: 5 ng/mL for non-Hispanic White individuals, 6 ng/mL for non-Hispanic Black individuals, and 1 ng/mL for Mexican-American individuals. For adolescents, the optimal cutpoints were 3, 3, and 1 ng/mL for the same racial-ethnic groups.
Another large population-based analysis of the optimal saliva cotinine cutpoint to discriminate cigarette smoking from nonsmoking was conducted in the United Kingdom on 58 971 people aged 4 or older between 1996 and 2004.46 The optimal cutpoint was determined to be 12 ng/mL (sensitivity 95.8%; specificity 96.9%). Of note, the optimal cutpoint was higher if there were other smokers in home or not (18 vs. 5 ng/mL) and progressively higher with increased social disadvantage (gradient 8 to 18 ng/mL). Most likely the differences in cutpoints between the U.S. and UK studies also relate to differences in heaviness of smoking (heavier in the United Kingdom based on higher cotinine levels) and levels of secondhand smoke exposure (higher in the United Kingdom).
The optimal cutpoint concentrations determined in the NHANES and UK studies were lower than the 15 ng/mL cited in the 2002 SRNT Working Group report. This cutpoint was based on a publication by Jarvis conducted in the United Kingdom in the 1980s, when the prevalence of active smoking and SHS exposure were much higher than at present.47 Fortunately, varying cutpoints within the range 3–15 ng/mL makes little difference to the classification of individuals as nonsmokers or smokers, since most self-reported nonsmokers who are classified as smokers have cotinine concentrations well above these levels.46
Cutpoints can be affected by physiological differences (e.g., pregnancy and disease states), race/ethnicity, genetic differences, and environmental factors (e.g., hormone status and drug interactions). Pregnancy is associated with changes in cigarette consumption, extent of secondhand smoke exposure, and physiological and metabolic changes that can affect optimal cutpoints for detection of smoking. For example, the metabolism of nicotine and cotinine are accelerated during pregnancy.48 When comparing “self-report” by pregnant women of smoking status to salivary or serum cotinine, studies evaluating optimal sensitivity and specificity have recommended cutpoints of 13,49 12.9,50 10,51 and 5.3 ng/mL.52 Another study in 377 Alaskan Native women showed that the sensitivity and specificity was best at 1.07 ng/mL.53 Together, these studies suggest that 5–10 ng/mL may be a reasonable cutoff for pregnant smokers, but this value may differ by population characteristics.
Cotinine is generated from nicotine primarily via the liver enzyme CYP2A6.41 This enzyme is subject to considerable genetic variability and is also influenced by hormonal, drug, and other environmental factors. Cotinine blood levels also depend on the rate of cotinine metabolism, driven by the enzymes CYP2A6 (to trans-3’ hydroxycotinine [3HC]) and UGT2B10 (to cotinine glucuronide), the latter of which is also genetically polymorphic.54 The prevalence of slow metabolism variants of the CYP2A6 gene is higher in Asians and African Americans, so these groups convert less nicotine to cotinine and do so more slowly than Caucasians, and these groups metabolize cotinine more slowly.55,56 Sex hormones also strongly influence cotinine levels. Estrogen induces CYP2A6 activity as well as cotinine glucuronidation.48 The same changes are produced by chronic alcohol abuse.57 Consequently, for these groups cotinine levels are lower for any given daily nicotine intake. These metabolic differences explain in part differences in cotinine cutpoints by race/ethnicity. Interpretation of nicotine metabolites as biomarkers of combusted tobacco use needs also to consider the use of blunts—hollowed out cigars filled with marijuana. Blunt use can result in cotinine levels consistent with active smoking or heavy secondhand smoke exposure. Some blunt users deny tobacco smoking in general, so the use of blunts should also be queried.
Cutpoints for saliva cotinine are typically similar to those of serum. Free cotinine urine cutpoints would be predicted to be on average 4.6 higher than serum cutpoints, corresponding to 23 ng/mL. Empirical studies of urine-free cotinine as a cutpoint have reported around 30 ng/mL as optimal, similar to that predicted from urine to plasma ratio data.58 The ratio for total urinary cotinine (which includes cotinine glucuronide) to plasma cotinine has not been evaluated in detail, but total cotinine is generally about 1.5–2 times higher than free cotinine, so the ratio can be adjusted accordingly.
Urine cotinine has been used as a biomarker with and without creatinine correction. Two studies suggest that creatinine corrected urine cotinine levels correlate better with plasma levels than do uncorrected values, but the difference is not large, and many researchers continue to use uncorrected urine cotinine values.45,59 Most urine cutpoints have been reported in uncorrected values.
In pregnant women, Straierowicz et al showed that urine-free cotinine levels of 42.3 ng/mL or 53.1 ug/g creatinine was the best cutoff.50 Higgins et al found that agreement between self-reported smoking and urine cotinine in 131 pregnant women enrolled in a smoking cessation study was best at 25 ng/mL.38 Changing the cutpoint to 12.5 ng/mL resulted in only a 1% difference in overall agreement. These studies suggest that the cutpoint of 25–50 ng/mL is appropriate to identify pregnant smokers.
Analytic methods for cotinine include immunoassay, gas chromatography (GC), GC–mass spectrometry (GC–MS), liquid chromatography (LC), and liquid chromatography coupled to tandem mass spectrometry (LC–MS/MS). Chromatographic assays are specific and more sensitive than immunoassays. Immunoassays often report higher levels of cotinine due to nonspecificity and, therefore, resulting cutpoints are higher. Chromatographic methods are preferred, and recommended cutpoints have been based on chromato-graphic method results.
Nicotine is metabolized to a number of metabolites in addition to cotinine, and the sum of most or all nicotine metabolites in urine (termed urine total nicotine equivalents, TNE) is another validated biomarker of nicotine intake.60,61 The full panel of TNE includes nicotine, nicotine glucuronide, cotinine, cotinine glucuronide, 3HC, 3HC-glucuronide, nicotine-N oxide, cotinine-N oxide, nornicotine, and norcotinine, commonly referred to as “TNE7.”62 Some researchers report only [total nicotine + total cotinine + total 3HC], referred to as “TNE3,” as the other metabolites are minor. TNE3 is highly correlated with the sum of all metabolites (r = 0.99), and the correlation is not affected by sex or race/ethnicity. TNE is less influenced by individual differences in nicotine metabolism pathways compared to cotinine, making TNE the gold standard for estimating daily intake of nicotine. Analysis of TNE is done by LC–MS/MS and is available from several laboratories. However, it is considerably more expensive than measuring cotinine alone, and optimal cutpoints to distinguish cigarette smoking from not smoking have not been reported. When measurement of TNE becomes more widely available and less expensive and the optimal cutpoints have been established, it should be the nicotine exposure biomarker of choice. For purposes of assessing daily intake of nicotine, such as for tobacco harm-reduction studies, TNE is the best available biomarker. Cotinine is less accurate across individuals due to metabolic differences but works well to assess changes in nicotine intake over time within subjects.
Over the Counter Cotinine
Over the counter (OTC) cotinine test strips can provide quick nicotine exposure data. These assays have the advantage of being inexpensive and easy to use, and provide results within minutes, enabling nearly immediate feedback. However, they have important limitations including the semiquantitative nature of the measurements and the limited sensitivity and precision of the results. They are not suitable for measuring low cotinine concentrations such as from SHS or thirdhand smoke (THS) exposures.
The two best established OTC assays are NicCheck63 and the Nymox NicAlert.64 NicCheck I is an older colorimetric urine test strip assay with relatively low sensitivity and specificity. Consequently, it has not often been used in recent research. NicAlert test kits are multilevel lateral flow immunoassays (LFIA) that have been evaluated and compared with alternative methodologies in several peerreviewed publications.65-71 Although urine is the preferred matrix because of its higher cotinine concentration, both urine and saliva samples have been examined, with the lower bands used as the cutoff for saliva samples. In general, published NicAlert evaluations have found good results for smoker versus nonuser discrimination but have not proven reliable for quantitative or SHS exposure analysis.
LFIA test strips with a single band at a given cutoff value have been developed and are now widely available on the Internet. These strips are typically designed for urine samples with a nominal 200 ng/mL cutoff to distinguish between tobacco users and nonusers, although versions with lower cutoffs and potentially useable with saliva are also available. These strips are quite inexpensive at USD $1–3 apiece and could prove useful for quick, on-the-spot testing. However, they provide only an initial qualitative estimate. A recent report evaluated two of these strips relative to LC–MS/MS quantitation of total cotinine in urine with good results.72 Since these cotinine strips provide high specificity for nicotine exposure, combining OTC strips with eCO measurements has the potential to provide confirmation of smoking for nicotine intake from the strips with the presence or absence of elevated eCO levels, which might aid in distinguishing between combustion and noncombustion sources of nicotine exposure.
Anabasine/Anatabine and Other “Minor” Tobacco Alkaloids
Nicotine and cotinine reflect exposure to nicotine regardless of its source. Minor tobacco alkaloids are chemicals that are structurally related to nicotine and are specific for tobacco-derived products (e.g., cigarettes, cigars, and smokeless tobacco). If detection of tobacco use is needed in people who are using nicotine replacement medications (e.g., gum and patches) or nicotine-containing ENDS, minor tobacco alkaloids can be used. Because they are present in negligible amounts in pharmaceutical grade nicotine (which is tobacco derived but more highly purified than that in many e-liquids), two of these alkaloids, anabasine and anatabine, were developed as biomarkers for tobacco use during nicotine replacement therapy (NRT).73-75 Nicotine used in nonpharmaceutical commercial products is almost always derived from tobacco and, if not sufficiently purified, could contain measurable amounts of minor alkaloids. An exception is some ENDS fluids that have been reported to contain synthetic nicotine.76,77
The half-lives of anabasine and anatabine based on urinary excretion data are about 16 and 10 hours, respectively.75 Anabasine and anatabine are measured in urine using chromatography–mass spectrometry methods.78,79
The specificity of anabasine and anatabine for tobacco use was verified by analysis of urine samples from 35 nonsmokers (confirmed by cotinine analysis). Using a cutpoint of 2 ng/mL for both alkaloids as the criterion, specificity for cigarette smoking was 100%.74 In cigarette smokers (N = 99), concentrations of anabasine and anatabine in urine were similar (M = 22 ng/mL for both). Comparing smokeless tobacco users to cigarette smokers (two studies, N = 100 and N = 105), concentrations of urine anabasine were similar, 24 and 23 ng/mL, respectively. In contrast, urine anatabine concentrations were significantly higher in smokeless tobacco users than in cigarette smokers, 43 and 22 ng/mL, respectively. There are no known stability issues for anabasine and anatabine, and urine specimens can be stored frozen for long periods.
Anabasine and anatabine are useful biomarkers for tobacco use in people consuming pharmaceutical grade nicotine, but they may not be as useful for detecting tobacco use in ENDS users because the nicotine used in some e-liquids may contain substantial amounts of the two minor alkaloids.80,81 However, another minor alkaloid, nicotelline, has not been found in significant amounts in e-liquids. Nicotelline can be measured in urine, it has a half-life of about 2–3 hours,82 and studies in progress have shown that it can detect recent tobacco product use in people also using ENDS.73 Other studies in progress indicate that measurement of anatalline, another tobacco alkaloid, in combination with nicotelline, may be able to distinguish smokeless tobacco use from combusted tobacco use.
4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol
4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol (NNAL) is a metabolite of the tobacco-specific lung carcinogen 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK).83,84 Five properties of NNAL make it a very attractive biomarker for studies of tobacco product exposure. First, since NNK is found only in cured tobacco, the presence of NNAL in urine specifically and conclusively demonstrates use of some form of tobacco and/or exposure to SHS. Second, NNAL is formed metabolically from NNK in virtually all humans and is excreted in urine in its free form and as glucuronide conjugates.85-87 Third, NNAL is not found in the urine of people who use NRT, and in only extremely low levels, or not at all, in people who use ENDS.88 Only trace amounts of NNK are present as a contaminant in the nicotine used in some e-liquids.89 Fourth, both NNK and NNAL are powerful lung carcinogens, producing lung tumors in rodents at low doses and independent of the route of administration and, thus, are believed to play an important role in lung cancer induction by tobacco products.90,91 Thus, NNAL serves as a biomarker of carcinogen exposure. Fifth, and perhaps most important, NNAL has a relatively long lifetime in humans.87,92 In contrast to the relatively short half-life of cotinine (16 hours), the half-life of NNAL in urine is estimated to be 10–45 days. Thus, when regular smokers stop smoking, 34.5% of the amount of NNAL plus NNAL glucuronides present in urine during regular smoking is detectable 1 week after cessation, whereas the corresponding value for cotinine is 1.1%. After 3 weeks of abstinence, levels of NNAL plus its glucuronides in urine are still 15.3% of levels during smoking, whereas cotinine is undetectable.87 This relatively long lifetime means that NNAL will also detect intermittent tobacco use, where cotinine levels may be below the cutpoint.
In NHANES, which quantified urinary NNAL, exclusive smokeless tobacco users had the highest geometric mean concentrations of total NNAL (2.79 pmol/mg creatinine) compared to exclusive cigarette smokers (0.625 pmol/mg creatinine).93 Other large studies of cigarette smokers found 1.12–1.65 pmol/mL urine total NNAL in adult smokers.94-96 In the 2011–2012 NHANES, among those exposed to SHS, the geometric mean for total NNAL in young children (age 6–11 years) was almost three times that of adult nonsmokers in the age range 21–59 years.97 All large studies demonstrate strong correlations between urinary total NNAL and cotinine.
Although analytic challenges remain, total NNAL is almost the ideal biomarker for studies of SHS exposure because of its complete tobacco specificity, relatively long lifetime, and detectability at very low levels with great sensitivity, accuracy, and precision using LC–MS/MS methods. Thus, nonsmokers’ exposure to NNK was demonstrated virtually throughout life by measurement of total NNAL (ranging from 0.018 to 0.090 pmol/mL) in the urine of infants,98 elementary school children,99,100 adolescents,101 women living with smokers,102 restaurant and bar workers,103 and casino patrons.104 Only a few studies have examined cutpoints for NNAL to distinguish active smoking from SHS exposure. In one recent study among adolescents, the optimal NNAL cutpoint to distinguish active cigarette smoking from not smoking was 9.6 pg/mL by latent class analysis and 14.4 pg/mL by receiver operating characteristic analysis.101 Another study estimated an optimal cutpoint to separate smokers from heavily SHS exposed individuals to be 47 pg/mL92.
Urine is by far the most common body fluid used for analysis of NNAL as concentrations are much higher in urine than in blood. First morning urine, spot urine, and 24-hour urine samples have all been used for NNAL measurements. Although NNAL is quite stable, urine samples should be refrigerated until they are aliquoted and stored at −20°C, conditions under which free and glucuronidated (NNAL-O-Gluc and NNAL-N-Gluc)105,106 NNAL are stable virtually indefinitely.107 Most studies use β-glucuronidase treatment of the urine to hydrolyze NNAL-O-Gluc and NNAL-N-Gluc to free NNAL, which is then analyzed. The results are reported as “total NNAL,” which is the sum of free NNAL, NNAL-O-Gluc, and NNAL-N-Gluc.108 Total NNAL has also been quantified in blood (both plasma and serum),109,110 toe nails,111 amniotic fluid,112 pancreatic juice,113 saliva,114 and hair115 but methods for the latter four media have not been extensively applied and validated.
All current analytic methods use LC–MS/MS, which has adequate sensitivity and absolute specificity to detect and quantify NNAL and its glucuronides in people who use tobacco products or are exposed to SHS.106,108 The cost of NNAL analysis is considerably higher than that for cotinine. There are no reliable immunoassays for NNAL, so there is no rapid spot test for quickly indicating exposure to NNK. Note that some studies report NNAL values as pmol/mL, while others report pg/mL. The conversion factor is 209 pg/pmol.
Electronic Nicotine Delivery Systems
At present, two types of ENDS are marketed around the world—electronic cigarettes (e-cigarettes) and heat-not-burn devices. E-cigarettes heat a solution of nicotine, propylene glycol, and/or vegetable glycerin and flavorants to generate an aerosol that is inhaled by the users (vapers).116 Heat-not-burn devices (e.g., IQOS) apply controlled heating to a cigarette-like product, with the intent of delivering nicotine and tobacco flavor while avoiding combustion.117 ENDS can deliver nicotine in levels that can be comparable to those from conventional cigarettes but much lower levels of combustion products compared to a burning cigarette. Heating of an e-liquid can convert propylene glycol, vegetable glycerin and some flavor chemicals to volatile and potentially toxic organic chemicals (e.g., acetaldehyde, formaldehyde, and acrolein) but does not generate CO.118 Nicotine in e-liquids is extracted from tobacco and, depending on the extraction and purification processes, can contain other tobacco alkaloids, like anabasine and anatabine and small amounts of NNK. Emissions from IQOS generate low levels of thermal breakdown products, such as acetaldehyde, formaldehyde, and acrolein, but generally lower levels than those in conventional cigarette emissions.119
To date, no biomarkers specific for e-cigarette use are available. Considering the biomarkers that might distinguish ENDS use from tobacco use, cotinine and TNE are not useful because ENDS are nicotine delivery devices. Cotinine levels are quite similar in regular vapers and cigarette smokers.120 Biomarkers that can distinguish recent cigarette smoking from vaping are products of combustion (e.g., CO) or tobacco-specific constituents such as minor tobacco alkaloids and NNAL. The minor alkaloids anabasine and anatabine may also be useful to distinguish cigarette smoking from vaping, depending on the e-liquid that is used. Some e-liquids contain relatively high levels of anabasine and anatabine (due to incomplete purification of nicotine), in which case these alkaloids are not useful discriminators. Nicotelline levels are extremely low in e-liquids and high in tobacco smoke, making it an excellent discriminator.
With respect to window of detection, various minor alkaloids and CO have half-lives from 2 to 16 hours. Thus, these biomarkers can detect smoking within the past 1–2 days, depending on intensity of smoking and activity level. For longer-term discrimination, NNAL is the best biomarker. NNAL can persist in the urine for 2 months or longer after stopped tobacco use. Urine NNAL is also useful in detecting low-level intermittent tobacco use. In trying to identify people who are exclusively e-cigarette users, as might be required in health effects epidemiology studies, urine NNAL should be measured to exclude concurrent tobacco use. Figure 2 shows the time course of change of various biomarkers in a person who has quit cigarette smoking and switched to e-cigarettes. The use of biomarkers to distinguish heat-not-burn use from cigarette smoking has not been examined.
Figure 2.
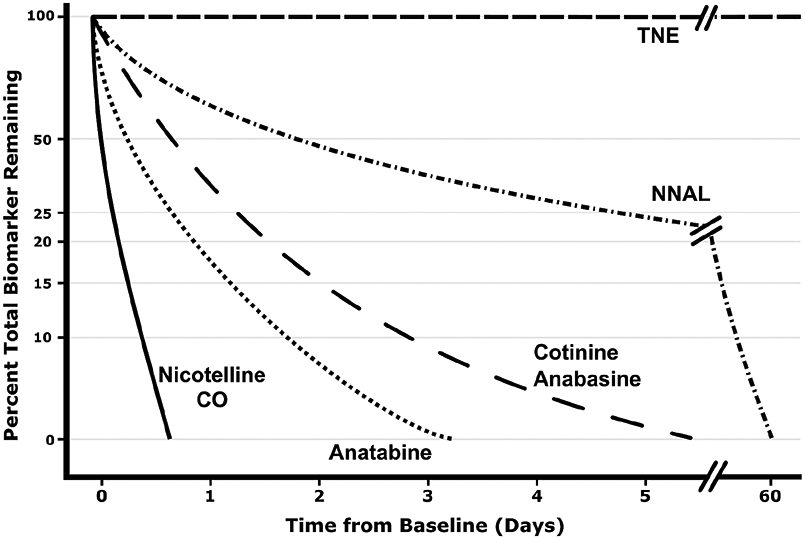
Biomarker elimination over time after switching from cigarettes to E-cigarettes (adapted from Jacob et al. 73, submitted for publication). Biomarkers other than CO are measured in urine. The time 0 value (100%) indicates levels that were present while smoking cigarettes. Values over time are shown as percent of baseline values. TNE = total nicotine equivalents. CO = carbon monoxide.
Summary and Recommendations
Biochemical verification of abstinence appears to be increasingly important, especially in clinical trials, as both social norms relating to smoking behavior and an increasing number of personal factors (e.g., age, pregnancy, hospitalization status, and socioeconomic status) are related to misreporting of smoking behavior.
Biochemical verification increases scientific rigor, but there are drawbacks that need to be assessed to determine whether the benefits of biochemical verification outweigh the costs, including the cost of the assays, the feasibility of sample collection, the ability to draw clear conclusions based on the duration of abstinence, and the variability of the assay within the study population.
If researchers opt to use biochemical verification, it is important to report details of sample collection and storage, analytic methodology including type of CO monitor used, limit of quantitation, the specific nature of the analytes (e.g., free vs. total cotinine, which metabolites are included for TNE), and the rationale for selecting specific cutpoints.
Researchers need to decide what biomarkers and biofluids are most appropriate for a given study (Table 2). If a marker of recent smoking abstinence is desired, then cotinine or CO are useful, while NNAL is preferred for assessment of long-term quitting. Cotinine can be measured in multiple biofluids; NNAL is most commonly measured in urine but can be measured in blood (plasma or serum), although concentrations are much lower in blood than in urine. Saliva or blood (serum, plasma, or whole blood) can be used interchangeably to measure cotinine, while whole blood is needed for carboxyhemoglobin.
A combination of biochemical assays, as well as clear assessment of what tobacco, nicotine, and combustible products a participant is using, may be necessary to biochemically verify product use or abstinence. For instance, to verify that a participant is using only e-cigarettes and no combustible cigarettes, the researcher needs self-report of e-cigarette use and denial of combustible cigarettes or other combustible product use (e.g., cigars, little cigars, and marijuana) and no use of NRT. In this case, a combination of eCO to rule out use of combustible products and a cotinine assay to detect the nicotine from the e-cigarettes would provide biochemical verification of e-cigarette but no combustible product use.
Table 2.
Biomarkers for use with various tobacco and nicotine products
| Product | Exhaled CO | Cotinine/TNE | Anabasine/anatabine | Nicotelline | NNAL |
|---|---|---|---|---|---|
| Cigarettes and other combusted tobacco products | + | + | + | + | + |
| Smokeless tobacco | − | + | + | + | + |
| ECIG | − | + | ± | − | − |
| NRT | − | + | − | − | − |
Note that evidence is not yet available on how best to assess heat-not-burn devices.
CO = carbon monoxide; ECIG = electronic cigarettes; NNAL = 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol; NRT = nicotine replacement therapy; TNE = urine total nicotine equivalents.
Acknowledgements
We would like to thank scientists who reviewed this paper prior to submission and offered their expert comments and suggestions: Andrea Weinberger and Steve Bernstein on behalf of the SRNT Treatment Research Network Advisory Committee and Benjamin Toll and Suzanne Colby on behalf of the SRNT Board. We thank Newton Addo for editorial assistance.
Funding
This work was not supported by external grant funding.
Footnotes
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily represent the views, official policy or position of the U.S. Department of Health and Human Services or any of its affiliated institutions or agencies. Use of trade names and commercial sources is for identification only and does not constitute endorsement by the U.S. Department of Health and Human Services, CDC, or FDA.
Declaration of Interests
Dr. Benowitz has been a paid consultant to Pfizer Inc. and Achieve Life Sciences, companies that market or are developing smoking cessation medications; and has been a paid expert witness in litigation against tobacco companies. Dr. Foulds has been a paid consultant to and has received grant support and product from Pfizer Inc. The other authors have no conflicts to declare. Dr. Oncken has received free nicotine and placebo inhalers from Pfizer Pharmaceuticals for an NIH funded smoking cessation study in pregnant women.
References
- 1.Anthenelli RM, Benowitz NL, West R, et al. Neuropsychiatric safety and efficacy of varenicline, bupropion, and nicotine patch in smokers with and without psychiatric disorders (EAGLES): a double-blind, randomised, placebo-controlled clinical trial. Lancet. 2016;387(10037):2507–2520. [DOI] [PubMed] [Google Scholar]
- 2.Lopez AA, Cobb CO, Yingst JM, et al. A transdisciplinary model to inform randomized clinical trial methods for electronic cigarette evaluation. BMC Public Health. 2016;16:217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Benowitz N, Jacob P, Ahijevych K, et al. Biochemical verification of tobacco use and cessation. Nicotine Tob Res. 2002;4:149–159. [DOI] [PubMed] [Google Scholar]
- 4.Jarvis MJ, Primatesta P, Erens B, Feyerabend C, Bryant A. Measuring nicotine intake in population surveys: comparability of saliva cotinine and plasma cotinine estimates. Nicotine Tob Res. 2003;5(3):349–355. [DOI] [PubMed] [Google Scholar]
- 5.Yeager DS, Krosnick JA. The validity of self-reported nicotine product use in the 2001–2008 national health and nutrition examination survey. Med Care. 2010;48(12):1128–1132. [DOI] [PubMed] [Google Scholar]
- 6.West R, Zatonski W, Przewozniak K, Jarvis MJ. Can we trust national smoking prevalence figures? Discrepancies between biochemically assessed and self-reported smoking rates in three countries. Cancer Epidemiol Biomarkers Prev. 2007;16(4):820–822. [DOI] [PubMed] [Google Scholar]
- 7.Patrick DL, Cheadle A, Thompson DC, Diehr P, Koepsell T, Kinne S. The validity of self-reported smoking: a review and meta-analysis. Am J Public Health. 1994;84(7):1086–1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Piper ME, Cook JW, Schlam TR, et al. A randomized controlled trial of an optimized smoking treatment delivered in primary care. Ann Behav Med. 2018;52(10):854–864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roese NJ, Jamieson DW. Twenty years of bogus pipeline research: a critical review and meta-analysis. Psychol Bull. 1993;114(2):363–375. [Google Scholar]
- 10.Nichols AL, Maner JK. The good-subject effect: investigating participant demand characteristics. J Gen Psychol. 2008;135(2):151–165. [DOI] [PubMed] [Google Scholar]
- 11.Martínez ME, Reid M, Jiang R, Einspahr J, Alberts DS. Accuracy of self-reported smoking status among participants in a chemoprevention trial. Prev Med. 2004;38(4):492–497. [DOI] [PubMed] [Google Scholar]
- 12.Spector LG, Murphy SE, Wickham KM, Lindgren B, Joseph AM. Prenatal tobacco exposure and cotinine in newborn dried blood spots. Pediatrics. 2014;133(6):e1632–e1638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lewis SJ, Cherry NM, McL Niven R, Barber PV, Wilde K, Povey AC. Cotinine levels and self-reported smoking status in patients attending a bronchoscopy clinic. Biomarkers. 2003;8(3-4):218–228. [DOI] [PubMed] [Google Scholar]
- 14.Pell JP, Haw SJ, Cobbe SM, et al. Validity of self-reported smoking status: comparison of patients admitted to hospital with acute coronary syndrome and the general population. Nicotine Tob Res. 2008;10(5):861–866. [DOI] [PubMed] [Google Scholar]
- 15.Monninkhof E, van der Valk P, van der Palen J, et al. The effect of a minimal contact smoking cessation programme in out-patients with chronic obstructive pulmonary disease: a pre-post-test study. Patient Educ Couns. 2004;52(3):231–236. [DOI] [PubMed] [Google Scholar]
- 16.Dietz PM, Homa D, England LJ, et al. Estimates of nondisclosure of cigarette smoking among pregnant and nonpregnant women of reproductive age in the United States. Am J Epidemiol. 2011;173(3):355–359. [DOI] [PubMed] [Google Scholar]
- 17.Noonan D, Jiang Y, Duffy SA. Utility of biochemical verification of tobacco cessation in the department of veterans affairs. Addict Behav. 2013;38(3):1792–1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Scheuermann TS, Richter KP, Rigotti NA, et al. ; Consortium of Hospitals Advancing Research on Tobacco (CHART). Accuracy of self-reported smoking abstinence in clinical trials of hospital-initiated smoking interventions. Addiction. 2017;112(12):2227–2236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hammett E, Veldheer S, Hrabovsky S, et al. TXT2STAYQUIT: pilot randomized trial of brief automated smoking cessation texting intervention for inpatient smokers discharged from the hospital. J Hosp Med. 2018;13(7):488–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lantini R, McGrath AC, Stein LA, Barnett NP, Monti PM, Colby SM. Misreporting in a randomized clinical trial for smoking cessation in adolescents. Addict Behav. 2015;45:57–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jamal A, King BA, Neff LJ, Whitmill J, Babb SD, Graffunder CM. Current cigarette smoking among adults—United States, 2005-2015. MMWR Morb Mortal Wkly Rep. 2016;65(44):1205–1211. [DOI] [PubMed] [Google Scholar]
- 22.Pirkle JL, Bernert JT, Caudill SP, Sosnoff CS, Pechacek TF. Trends in the exposure of nonsmokers in the U.S. population to secondhand smoke: 1988–2002. Environ Health Perspect. 2006;114(6):853–858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Benowitz NL, Bernert JT, Caraballo RS, Holiday DB, Wang J. Optimal serum cotinine levels for distinguishing cigarette smokers and nonsmokers within different racial/ethnic groups in the United States between 1999 and 2004. Am J Epidemiol. 2009;169(2):236–248. [DOI] [PubMed] [Google Scholar]
- 24.Schick SF, Blount BC, Jacob P 3rd, et al. Biomarkers of exposure to new and emerging tobacco delivery products. Am J Physiol Lung Cell Mol Physiol. 2017;313(3):L425–L452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Karelitz JL, Michael VC, Perkins KA. Analysis of agreement between expiredair carbon monoxide monitors. J Smok Cessat. 2017;12(2):105–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jarvis MJ, Belcher M, Vesey C, Hutchison DC. Low cost carbon monoxide monitors in smoking assessment. Thorax. 1986;41(11):886–887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shaoqing Y, Ruxin Z, Yingjian C, Jianqiu C, Yanshen W, Genhong L. A meta-analysis of the association of exhaled carbon monoxide on asthma and allergic rhinitis. Clin Rev Allergy Immunol. 2011;41(1):67–75. [DOI] [PubMed] [Google Scholar]
- 28.Tual S, Piau JP, Jarvis MJ, Dautzenberg B, Annesi-Maesano I. Impact of tobacco control policies on exhaled carbon monoxide in non-smokers. J Epidemiol Community Health. 2010;64(6):554–556. [DOI] [PubMed] [Google Scholar]
- 29.Maga M, Janik MK, Wachsmann A, et al. Influence of air pollution on exhaled carbon monoxide levels in smokers and non-smokers. A prospective cross-sectional study. Environ Res. 2017;152:496–502. [DOI] [PubMed] [Google Scholar]
- 30.Zhang Q, Li L, Smith M, et al. ; China Kadoorie Biobank study collaboration. Exhaled carbon monoxide and its associations with smoking, indoor household air pollution and chronic respiratory diseases among 512,000 Chinese adults. Int J Epidemiol. 2013;42(5):1464–1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moolchan ET, Zimmerman D, Sehnert SS, Zimmerman D, Huestis MA, Epstein DH. Recent marijuana blunt smoking impacts carbon monoxide as a measure of adolescent tobacco abstinence. Subst Use Misuse. 2005;40(2):231–240. [DOI] [PubMed] [Google Scholar]
- 32.Hawkins LH. Blood carbon monoxide levels as a function of daily cigarette consumption and physical activity. Br J Ind Med. 1976;33(2):123–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Castleden CM, Cole PV. Variations in carboxyhaemoglobin levels in smokers. Br Med J. 1974;4(5947):736–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Coburn RF, Forster RE, Kane PB. Considerations of the physiological variables that determine the blood carboxyhemoglobin concentration in man. J Clin Invest. 1965;44(11):1899–1910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Perkins KA, Karelitz JL, Jao NC. Optimal carbon monoxide criteria to confirm 24-hr smoking abstinence. Nicotine Tob Res. 2013;15(5):978–982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cropsey KL, Trent LR, Clark CB, Stevens EN, Lahti AC, Hendricks PS. How low should you go? Determining the optimal cutoff for exhaled carbon monoxide to confirm smoking abstinence when using cotinine as reference. Nicotine Tob Res. 2014;16(10):1348–1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Emery RL, Levine MD. Optimal carbon monoxide criteria to confirm smoking status among postpartum women. Nicotine Tob Res. 2016;18(5):966–970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Higgins ST, Heil SH, Badger GJ, et al. Biochemical verification of smoking status in pregnant and recently postpartum women. Exp Clin Psychopharmacol. 2007;15(1):58–66. [DOI] [PubMed] [Google Scholar]
- 39.Bailey BA. Using expired air carbon monoxide to determine smoking status during pregnancy: preliminary identification of an appropriately sensitive and specific cut-point. Addict Behav. 2013;38(10):2547–2550. [DOI] [PubMed] [Google Scholar]
- 40.Moscato U, Poscia A, Gargaruti R, Capelli G, Cavaliere F. Normal values of exhaled carbon monoxide in healthy subjects: comparison between two methods of assessment. BMC Pulm Med. 2014;14:204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hukkanen J, Jacob P 3rd, Benowitz NL. Metabolism and disposition kinetics of nicotine. Pharmacol Rev. 2005;57(1):79–115. [DOI] [PubMed] [Google Scholar]
- 42.Bernert JT Jr, McGuffey JE, Morrison MA, Pirkle JL. Comparison of serum and salivary cotinine measurements by a sensitive high-performance liquid chromatography-tandem mass spectrometry method as an indicator of exposure to tobacco smoke among smokers and nonsmokers. J Anal Toxicol. 2000;24(5):333–339. [DOI] [PubMed] [Google Scholar]
- 43.Simoni M, Baldacci S, Puntoni R, et al. Plasma, salivary and urinary cotinine in non-smoker Italian women exposed and unexposed to environmental tobacco smoking (SEASD study). Clin Chem Lab Med. 2006;44(5):632–638. [DOI] [PubMed] [Google Scholar]
- 44.St Helen G, Novalen M, Heitjan DF, et al. Reproducibility of the nicotine metabolite ratio in cigarette smokers. Cancer Epidemiol Biomarkers Prev. 2012;21(7):1105–1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Benowitz NL, Dains KM, Dempsey D, Herrera B, Yu L, Jacob P 3rd. Urine nicotine metabolite concentrations in relation to plasma cotinine during low-level nicotine exposure. Nicotine Tob Res. 2009;11(8):954–960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jarvis MJ, Fidler J, Mindell J, Feyerabend C, West R. Assessing smoking status in children, adolescents and adults: cotinine cut-points revisited. Addiction. 2008;103(9):1553–1561. [DOI] [PubMed] [Google Scholar]
- 47.Jarvis MJ, Tunstall-Pedoe H, Feyerabend C, Vesey C, Saloojee Y. Comparison of tests used to distinguish smokers from nonsmokers. Am J Public Health. 1987;77(11):1435–1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dempsey D, Jacob P 3rd, Benowitz NL. Accelerated metabolism of nicotine and cotinine in pregnant smokers. J Pharmacol Exp Ther. 2002;301(2):594–598. [DOI] [PubMed] [Google Scholar]
- 49.Hegaard HK, Kjaergaard H, Møller LF, Wachmann H, Ottesen B. Determination of a saliva cotinine cut-off to distinguish pregnant smokers from pregnant non-smokers. Acta Obstet Gynecol Scand. 2007;86(4):401–406. [DOI] [PubMed] [Google Scholar]
- 50.Stragierowicz J, Mikołajewska K, Zawadzka-Stolarz M, Polańska K, Ligocka D. Estimation of cutoff values of cotinine in urine and saliva for pregnant women in Poland. Biomed Res Int. 2013;2013:386784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Polanska K, Krol A, Kaluzny P, et al. Estimation of saliva cotinine cut-off points for active and passive smoking during pregnancy-polish mother and child cohort (REPRO_PL). Int J Environ Res Public Health. 2016;13(12):1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kvalvik LG, Nilsen RM, Skjœrven R, et al. Self-reported smoking status and plasma cotinine concentrations among pregnant women in the Norwegian mother and child cohort study. Pediatr Res. 2012;72(1):101–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Smith JJ, Robinson RF, Khan BA, Sosnoff CS, Dillard DA. Estimating cotinine associations and a saliva cotinine level to identify active cigarette smoking in alaska native pregnant women. Matern Child Health J. 2014;18(1):120–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Murphy SE, Park SS, Thompson EF, et al. Nicotine N-glucuronidation relative to N-oxidation and C-oxidation and UGT2B10 genotype in five ethnic/racial groups. Carcinogenesis. 2014;35(11):2526–2533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.McDonagh EM, Wassenaar C, David SP, et al. PharmGKB summary: very important pharmacogene information for cytochrome P-450, family 2, subfamily A, polypeptide 6. Pharmacogenet Genomics. 2012;22(9):695–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zhu AZ, Renner CC, Hatsukami DK, et al. The ability of plasma cotinine to predict nicotine and carcinogen exposure is altered by differences in CYP2A6: the influence of genetics, race, and sex. Cancer Epidemiol Biomarkers Prev. 2013;22(4):708–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gubner NR, Kozar-Konieczna A, Szoltysek-Boldys I, et al. Cessation of alcohol consumption decreases rate of nicotine metabolism in male alcoholdependent smokers. Drug Alcohol Depend. 2016;163:157–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Benowitz NL, Jain S, Dempsey DA, Nardone N, Helen GS, Jacob P 3rd. Urine cotinine screening detects nearly ubiquitous tobacco smoke exposure in urban adolescents. Nicotine Tob Res. 2017;19(9):1048–1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Thompson SG, Barlow RD, Wald NJ, Van Vunakis H. How should urinary cotinine concentrations be adjusted for urinary creatinine concentration? Clin Chim Acta. 1990;187(3):289–295. [DOI] [PubMed] [Google Scholar]
- 60.Benowitz NL, Dains KM, Dempsey D, Yu L, Jacob P 3rd. Estimation of nicotine dose after low-level exposure using plasma and urine nicotine metabolites. Cancer Epidemiol Biomarkers Prev. 2010;19(5):1160–1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Feng S, Kapur S, Sarkar M, et al. Respiratory retention of nicotine and urinary excretion of nicotine and its five major metabolites in adult male smokers. Toxicol Lett. 2007;173(2):101–106. [DOI] [PubMed] [Google Scholar]
- 62.Benowitz N, St Helen G, Nardone N, Sanderson Cox L, Jacob P. Urine metabolites for estimating daily intake of nicotine from cigarette smoking. Nicotine Tob Res. 2019: [epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mossman Associates. Nicotine. 2015; http://www.mossmanassociates.com/nicotine.html. Accessed December 12, 2017.
- 64.Nymox. Nymox—NicAlert(R). 2017; http://www.nymox.com/default.action?itemid=47. Accessed December 12, 2017.
- 65.Best D, Green EM, Smith JH, Perry DC. Dipstick tests for secondhand smoke exposure. Nicotine Tob Res. 2010;12(6):551–556. [DOI] [PubMed] [Google Scholar]
- 66.Cooke F, Bullen C, Whittaker R, McRobbie H, Chen MH, Walker N. Diagnostic accuracy of NicAlert cotinine test strips in saliva for verifying smoking status. Nicotine Tob Res. 2008;10(4):607–612. [DOI] [PubMed] [Google Scholar]
- 67.Marrone GF, Paulpillai M, Evans RJ, Singleton EG, Heishman SJ. Breath carbon monoxide and semiquantitative saliva cotinine as biomarkers for smoking. Hum Psychopharmacol. 2010;25(1):80–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Marrone GF, Shakleya DM, Scheidweiler KB, Singleton EG, Huestis MA, Heishman SJ. Relative performance of common biochemical indicators in detecting cigarette smoking. Addiction. 2011;106(7):1325–1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Montalto NJ, Wells WO. Validation of self-reported smoking status using saliva cotinine: a rapid semiquantitative dipstick method. Cancer Epidemiol Biomarkers Prev. 2007;16(9):1858–1862. [DOI] [PubMed] [Google Scholar]
- 70.Scheidweiler KB, Marrone GF, Shakleya DM, Singleton EG, Heishman SJ, Huestis MA. Oral fluid nicotine markers to assess smoking status and recency of use. Ther Drug Monit. 2011;33(5):609–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yeh E, Levasseur G, Kaiserman MJ. Evaluation of urinary cotinine immunoassay test strips used to assess smoking status. Nicotine Tob Res. 2011;13(11):1045–1051. [DOI] [PubMed] [Google Scholar]
- 72.Achilihu H, Feng J, Wang L, Bernert JT. Tobacco use classification by inexpensive urinary cotinine immunoassay test strips. J Anal Toxicol. 2019;43(2):149–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Jacob P, St Helen G, Yu L, et al. Biomarkers of Exposure for Dual Use of Electronic Cigarettes and Combustible Cigarettes: Nicotelline, NNAL, and Total Nicotine Equivalents. 2019. [Under Review] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jacob P 3rd, Hatsukami D, Severson H, Hall S, Yu L, Benowitz NL. Anabasine and anatabine as biomarkers for tobacco use during nicotine replacement therapy. Cancer Epidemiol Biomarkers Prev. 2002;11(12):1668–1673. [PubMed] [Google Scholar]
- 75.Jacob P 3rd, Yu L, Shulgin AT, Benowitz NL. Minor tobacco alkaloids as biomarkers for tobacco use: comparison of users of cigarettes, smokeless tobacco, cigars, and pipes. Am J Public Health. 1999;89(5):731–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Harlay J Nicotine E-juices: natural, tobacco-free or synthetic? 2016; https://www.vapingpost.com/2016/06/28/nicotine-e-juices-natural-tobacco-free-or-synthetic/. Accessed January 4, 2019.
- 77.Zettler PJ, Hemmerich N, Berman ML. Closing the regulatory gap for synthetic nicotine products. Boston Coll Law Rev. 2018;59(6):1933–1982. [PMC free article] [PubMed] [Google Scholar]
- 78.Jacob P 3rd, Yu L, Liang G, Shulgin AT, Benowitz NL. Gas chromatographicmass spectrometric method for determination of anabasine, anatabine and other tobacco alkaloids in urine of smokers and smokeless tobacco users. J Chromatogr. 1993;619(1):49–61. [DOI] [PubMed] [Google Scholar]
- 79.von Weymarn LB, Thomson NM, Donny EC, Hatsukami DK, Murphy SE. Quantitation of the minor tobacco alkaloids nornicotine, anatabine, and anabasine in smokers’ urine by high throughput liquid chromatographymass spectrometry. Chem Res Toxicol. 2016;29(3):390–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Etter JF, Zäther E, Svensson S. Analysis of refill liquids for electronic cigarettes. Addiction. 2013;108(9):1671–1679. [DOI] [PubMed] [Google Scholar]
- 81.Trehy ML, Ye W, Hadwiger ME, et al. Analysis of electronic cigarette cartridges, refill solutions, and smoke for nicotine and nicotine related impurities. J Liq Chromatogr Relat Technol. 2011;34(14):1442–1458. [Google Scholar]
- 82.Jacob P 3rd, Goniewicz ML, Havel CM, Schick SF, Benowitz NL. Nicotelline: a proposed biomarker and environmental tracer for particulate matter derived from tobacco smoke. Chem Res Toxicol. 2013;26(11):1615–1631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hecht SS, Stepanov I, Carmella SG. Exposure and metabolic activation biomarkers of carcinogenic tobacco-specific nitrosamines. Acc Chem Res. 2016;49(1):106–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hecht SS, Young R, Chen CB. Metabolism in the F344 rat of 4-(N-methyl-N-nitrosamino)-1-(3-pyridyl)-1-butanone, a tobacco-specific carcinogen. Cancer Res. 1980;40(11):4144–4150. [PubMed] [Google Scholar]
- 85.Appleton S, Olegario RM, Lipowicz PJ. TSNA levels in machine-generated mainstream cigarette smoke: 35 years of data. Regul Toxicol Pharmacol. 2013;66(2):197–207. [DOI] [PubMed] [Google Scholar]
- 86.Appleton S, Olegario RM, Lipowicz PJ. TSNA exposure from cigarette smoking: 18 years of urinary NNAL excretion data. Regul Toxicol Pharmacol. 2014;68(2):269–274. [DOI] [PubMed] [Google Scholar]
- 87.Hecht SS, Carmella SG, Chen M, et al. Quantitation of urinary metabolites of a tobacco-specific lung carcinogen after smoking cessation. Cancer Res. 1999;59(3):590–596. [PubMed] [Google Scholar]
- 88.Hecht SS, Carmella SG, Kotandeniya D, et al. Evaluation of toxicant and carcinogen metabolites in the urine of e-cigarette users versus cigarette smokers. Nicotine Tob Res. 2015;17(6):704–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kim HJ, Shin HS. Determination of tobacco-specific nitrosamines in replacement liquids of electronic cigarettes by liquid chromatography-tandem mass spectrometry. J Chromatogr A. 2013;1291:48–55. [DOI] [PubMed] [Google Scholar]
- 90.Balbo S, Johnson CS, Kovi RC, et al. Carcinogenicity and DNA adduct formation of 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone and enantiomers of its metabolite 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol in F-344 rats. Carcinogenesis. 2014;35(12):2798–2806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.International Agency for Research on Cancer. Smokeless tobacco and tobacco-specific nitrosamines In: Mitchell J, Perez E, eds. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Vol. 89 Lyon, France: IARC; 2007:41–583. [Google Scholar]
- 92.Goniewicz ML, Havel CM, Peng MW, et al. Elimination kinetics of the tobacco-specific biomarker and lung carcinogen 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol. Cancer Epidemiol Biomarkers Prev. 2009;18(12):3421–3425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Rostron BL, Chang CM, van Bemmel DM, Xia Y, Blount BC. Nicotine and toxicant exposure among U.S. smokeless tobacco users: results from 1999 to 2012 national health and nutrition examination survey data. Cancer Epidemiol Biomarkers Prev. 2015;24(12):1829–1837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Park SL, Carmella SG, Ming X, et al. Variation in levels of the lung carcinogen NNAL and its glucuronides in the urine of cigarette smokers from five ethnic groups with differing risks for lung cancer. Cancer Epidemiol Biomarkers Prev. 2015;24(3):561–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Roethig HJ, Munjal S, Feng S, et al. Population estimates for biomarkers of exposure to cigarette smoke in adult U.S. cigarette smokers. Nicotine Tob Res. 2009;11(10):1216–1225. [DOI] [PubMed] [Google Scholar]
- 96.Vogel RI, Carmella SG, Stepanov I, Hatsukami DK, Hecht SS. The ratio of a urinary tobacco-specific lung carcinogen metabolite to cotinine is significantly higher in passive than in active smokers. Biomarkers. 2011;16(6):491–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Wei B, Blount BC, Xia B, Wang L. Assessing exposure to tobacco-specific carcinogen NNK using its urinary metabolite NNAL measured in US population: 2011-2012. J Expo Sci Environ Epidemiol. 2016;26(3):249–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Hecht SS, Carmella SG, Le KA, et al. 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol and its glucuronides in the urine of infants exposed to environmental tobacco smoke. Cancer Epidemiol Biomarkers Prev. 2006;15(5):988–992. [DOI] [PubMed] [Google Scholar]
- 99.Hecht SS, Ye M, Carmella SG, et al. Metabolites of a tobacco-specific lung carcinogen in the urine of elementary school-aged children. Cancer Epidemiol Biomarkers Prev. 2001;10(11):1109–1116. [PubMed] [Google Scholar]
- 100.Stepanov I, Hecht SS, Duca G, Mardari I. Uptake of the tobacco-specific lung carcinogen 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone by Moldovan children. Cancer Epidemiol Biomarkers Prev. 2006;15(1):7–11. [DOI] [PubMed] [Google Scholar]
- 101.Benowitz NL, Nardone N, Jain S, et al. Comparison of urine 4-(Methylnitrosamino)-1-(3)Pyridyl-1-butanol and cotinine for assessment of active and passive smoke exposure in urban adolescents. Cancer Epidemiol Biomarkers Prev. 2018;27(3):254–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Anderson KE, Carmella SG, Ye M, et al. Metabolites of a tobacco-specific lung carcinogen in nonsmoking women exposed to environmental tobacco smoke. J Natl Cancer Inst. 2001;93(5):378–381. [DOI] [PubMed] [Google Scholar]
- 103.Tulunay OE, Hecht SS, Carmella SG, et al. Urinary metabolites of a tobacco-specific lung carcinogen in nonsmoking hospitality workers. Cancer Epidemiol Biomarkers Prev. 2005;14(5):1283–1286. [DOI] [PubMed] [Google Scholar]
- 104.Anderson KE, Kliris J, Murphy L, et al. Metabolites of a tobacco-specific lung carcinogen in nonsmoking casino patrons. Cancer Epidemiol Biomarkers Prev. 2003;12(12):1544–1546. [PubMed] [Google Scholar]
- 105.Hecht SS. Biochemistry, biology, and carcinogenicity of tobacco-specific N-nitrosamines. Chem Res Toxicol. 1998;11(6):559–603. [DOI] [PubMed] [Google Scholar]
- 106.Shah KA, Karnes HT. A review of the analysis of tobacco-specific nitrosamines in biological matrices. Crit Rev Toxicol. 2010;40(4):305–327. [DOI] [PubMed] [Google Scholar]
- 107.Xia Y, Bernert JT. Stability of the tobacco-specific nitrosamine 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol in urine samples stored at various temperatures. J Anal Toxicol. 2010;34(7):411–415. [DOI] [PubMed] [Google Scholar]
- 108.Carmella SG, Ming X, Olvera N, Brookmeyer C, Yoder A, Hecht SS. High throughput liquid and gas chromatography-tandem mass spectrometry assays for tobacco-specific nitrosamine and polycyclic aromatic hydrocarbon metabolites associated with lung cancer in smokers. Chem Res Toxicol. 2013;26(8):1209–1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Carmella SG, Han S, Villalta PW, Hecht SS. Analysis of total 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol in smokers’ blood. Cancer Epidemiol Biomarkers Prev. 2005;14(11 Pt 1):2669–2672. [DOI] [PubMed] [Google Scholar]
- 110.Church TR, Anderson KE, Caporaso NE, et al. A prospectively measured serum biomarker for a tobacco-specific carcinogen and lung cancer in smokers. Cancer Epidemiol Biomarkers Prev. 2009;18(1):260–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Stepanov I, Feuer R, Jensen J, Hatsukami D, Hecht SS. Mass spectrometric quantitation of nicotine, cotinine, and 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol in human toenails. Cancer Epidemiol Biomarkers Prev. 2006;15(12):2378–2383. [DOI] [PubMed] [Google Scholar]
- 112.Milunsky A, Carmella SG, Ye M, Hecht SS. A tobacco-specific carcinogen in the fetus. Prenat Diagn. 2000;20(4):307–310. [DOI] [PubMed] [Google Scholar]
- 113.Prokopczyk B, Hoffmann D, Bologna M, et al. Identification of tobacco-derived compounds in human pancreatic juice. Chem Res Toxicol. 2002;15(5):677–685. [DOI] [PubMed] [Google Scholar]
- 114.Idris AM, Nair J, Friesen M, et al. Carcinogenic tobacco-specific nitrosamines are present at unusually high levels in the saliva of oral snuff users in Sudan. Carcinogenesis. 1992;13(6):1001–1005. [DOI] [PubMed] [Google Scholar]
- 115.Yao L, Yang J, Guan YF, et al. Development, validation, and application of a liquid chromatography-tandem mass spectrometry method for the determination of 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol in human hair. Anal Bioanal Chem. 2012;404(8):2259–2266. [DOI] [PubMed] [Google Scholar]
- 116.Hajek P, Etter JF, Benowitz N, Eissenberg T, McRobbie H. Electronic cigarettes: review of use, content, safety, effects on smokers and potential for harm and benefit. Addiction. 2014; 109(11):1801–1810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Schorp MK, Tricker AR, Dempsey R. Reduced exposure evaluation of an electrically heated cigarette smoking system. Part 1: Nonclinical and clinical insights. Regul Toxicol Pharmacol. 2012;64 (2 Suppl):S1–10. [DOI] [PubMed] [Google Scholar]
- 118.Logue JM, Sleiman M, Montesinos VN, et al. Emissions from electronic cigarettes: assessing vapers’ intake of toxic compounds, secondhand exposures, and the associated health impacts. Environ Sci Technol. 2017;51(16):9271–9279. [DOI] [PubMed] [Google Scholar]
- 119.Auer R, Concha-Lozano N, Jacot-Sadowski I, Cornuz J, Berthet A. Heat-not-burn tobacco cigarettes: smoke by any other name. JAMA Intern Med. 2017;177(7):1050–1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Marsot A, Simon N. Nicotine and cotinine levels with electronic cigarette: a review. Int J Toxicol. 2016;35(2):179–185. [DOI] [PubMed] [Google Scholar]


