Abstract
Objectives:
Fracture of endodontically treated restored teeth is a common concern. Premolars are subjected to high shear and tensile forces. This study aimed to assess the fracture resistance and fracture mode of endodontically treated premolars restored with direct and indirect onlay restorations.
Materials and Methods:
In this in-vitro experimental study, 45 human maxillary premolars were divided into three groups (n=15) of control (sound teeth), direct onlay, and indirect onlay. In groups 2 and 3, the teeth underwent endodontic treatment. Mesio-occluso-distal cavities were prepared and restored with direct composite (P60) and indirect IPS e.max ceramic onlays, respectively. The teeth were subjected to vertical forces after cyclic loading. The maximum load causing fracture was recorded in Newtons. Data were analyzed using analysis of variance, chi-square test, and Tukey’s test.
Results:
The highest and the lowest fracture resistances were noted in sound teeth and direct onlay restorations, respectively. The difference in fracture resistance was significant among the three groups (P<0.001). Pairwise comparisons revealed a significant difference in the fracture resistance of sound teeth and the two restoration groups (P<0.001). However, the difference in the fracture resistance of direct and indirect onlay restorations was not significant (P=0.6). Chi-square test showed a significantly higher frequency of irreparable fractures in the indirect onlay group (P=0.005).
Conclusion:
Direct and indirect onlay restorations were not significantly different in terms of the fracture resistance but the frequency of irreparable fractures was higher in indirect restorations.
Keywords: Ceramics, Composite Resins, Dental Onlay, Endodontically-Treated Teeth
INTRODUCTION
Fracture of endodontically treated restored teeth is a common concern [1]. Endodontic treatment is known to decreases the elasticity and subsequently the fracture resistance of teeth [2].
It happens as the result of dehydration of tooth structure and loss of a great portion of dentin and important anatomical structures such as cusps, marginal ridges, and the roof of pulp chamber during access cavity preparation and endodontic treatment [3]. Survival of endodontically treated teeth depends on the amount of remaining tooth structure, type of restorative material, the technique of tooth restoration, and interactions between teeth, restorative materials, and the oral environment [4]. Many dental clinicians have often recommended complete coverage of endodontically treated teeth by prosthetic crowns [5]. However, inlay and onlay restorations can also be used in certain cases. Indirect restorative materials commonly used for the fabrication of inlays, onlays, and crowns include lithium disilicate, which has a high translucency and a wide color spectrum, as well as indirect composite resins, which have been proven to increase the fracture resistance of teeth [5].
Some researchers believe that large cavities in endodontically treated teeth require cuspal coverage to decrease the risk of fracture. Although both onlay restorations and full crowns protect teeth against fracture, onlay is a more conservative restoration than a full crown [4].
Despite the availability of many restorative materials for the restoration of endodontically treated teeth, composite resins and ceramics are more commonly used for this purpose due to their excellent esthetic properties [6]. The main advantage of using composite resins is the maximum preservation of tooth structure. On the other hand, ceramics have higher compressive resistance and durability than composite restorations in the oral cavity [6]. However, there are some controversies in this respect [5].
Premolars are subjected to high shear and tensile forces due to their particular position in the dental arch, and considering their unique anatomy, some considerations must be taken into account for their restoration following endodontic treatment to minimize their risk of fracture [1]. Considering the gap of information in this respect and lack of a consensus regarding an ideal protocol for the restoration of endodontically treated premolars, this study aimed to compare the fracture resistance of endodontically treated maxillary premolars restored with direct and indirect onlay restorations.
MATERIALS AND METHODS
This in-vitro experimental study was conducted on 45 sound human premolars extracted for orthodontic treatment or due to advanced periodontitis. The study was approved by the ethics committee of our university. The teeth were selected using convenience sampling.
The inclusion criteria were sound maxillary premolars of 18- to 25-year-old patients with complete roots and mature apices. All teeth were inspected under a stereomicroscope (SMZ 100, Nikon, Japan) at ×25 magnification to ensure the absence of cracks or caries. All teeth had normal anatomy without any anomaly. Also, the root length and the mesiodistal width of the teeth were measured using a caliper (Guilin Guanglu Measuring Instrument Co., Ltd., Guilin, China), and teeth with similar size and shape were chosen for the study. Soft tissue residues and dental calculi were removed using a scaler, and the teeth were immersed in a 0.5% chloramine-T solution at 23°C and used for this study within three months [7,8].
Grouping:
The teeth were first categorized based on their size. To calculate the size of teeth according to Eakle et al [9], the maximum buccolingual and mesiodistal dimensions of the teeth at the occlusal third were measured using the caliper, and the obtained two numbers were multiplied. The resultant number served as the tooth size. Accordingly, the teeth were randomly divided into three groups (n=15) using block randomization such that the three groups had an equal number of teeth with different sizes. This was done to eliminate the effect of tooth size and morphology as a confounder of the results. To standardize the intercuspal angle and the morphology of the restored teeth, an over-impression was made of the teeth using a vacuum-formed resin sheet to standardize the restorations. These molds were used to mimic the occlusal morphology of sound premolars in direct restorations [1,10].
The study groups were as follows:
Group 1. Sound maxillary premolars served as the control group.
Group 2. Endodontically treated maxillary premolars with mesio-occluso-distal (MOD) cavities and reduced buccal and palatal cusps for composite onlay restoration (P60; 3M ESPE, St. Paul, MN, USA).
Group 3. Endodontically treated maxillary premolars with MOD cavities and reduced buccal and palatal cusps for onlay restoration with IPS e.max Press lithium disilicate ceramic (Ivoclar Vivadent, Oklahoma City, OK, USA).
Endodontic treatment of teeth:
Teeth in groups 2 and 3 underwent endodontic treatment as follows: an access cavity, measuring 3×2 mm 2 , was prepared using a fissure diamond bur (Dentsply Sirona Endodontics, Tulsa, OK, USA) [11]. Then, a #15 K-file (Mani Inc., Tochigi, Japan) was introduced into the canal until its tip was visible at the apex. Next, 1 mm was subtracted from this length to determine the working length (WL). The canal was shaped using the step-back technique up to #30 K-file. The canals were flared using #1, #2, and #3 Gates-Glidden drills (Mani Inc., Tochigi, Japan). The canals were rinsed with saline between filings [7]. The canals were then dried with paper points. A #30 gutta-percha point (Meta, Wisconsin, USA) dipped in AH-26 sealer (Dentsply Maillefer, Tulsa, OK, USA) was placed in the canal as the master cone. Using a #2 spreader (Mani Inc., Tochigi, Japan) and #20 accessory gutta-percha points, the canals were filled with the lateral compaction technique. Excess gutta-percha was removed with a hot instrument at 0.5 mm below the cementoenamel junction (CEJ). Gutta-percha was condensed in the canal using a plugger [7]. In groups 2 and 3, the pulp chamber was etched with 37% phosphoric acid (SDI, Bayswater, VIC, Australia) for 20 seconds. The entire area was rinsed for 10 seconds. After drying, the All-Bond Universal adhesive (Bisco Dental Products, Schaumburg, IL, USA) was applied to the cavity and cured for 20 seconds with an overlapping curing procedure using a light-emitting diode (LED) light-curing unit (Radii Plus, SDI; Bayswater, VIC, Australia) at a light intensity of 1,500 mW/cm 2 . The first layer of the P60 composite was applied at 2 mm from the orifice and cured for 20 seconds. Then, the composite was incrementally applied and cured for 20 seconds with an overlapping curing procedure in the pulp chamber as shown in Figure 1 [2,5].
Fig. 1.
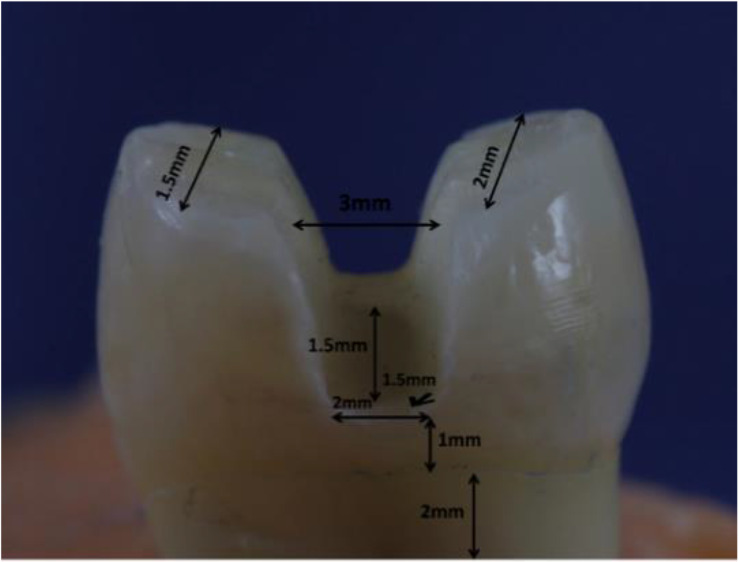
Tooth preparation
Using a high-speed handpiece and a diamond bur with a 1mm diameter (Dentsply Sirona Endodontics, Tulsa, OK, USA), MOD cavities were prepared under water coolant in all groups [1]. The buccolingual width of the MOD cavities was 3 mm at the occlusal surface. The height of the axial wall of the proximal boxes was 1.5 mm, and the depth of the gingival floor was 1.5 mm [2] such that the gingival floor of the proximal boxes was 1 mm above the CEJ [1].
After the preparation of MOD cavities, the buccal and palatal cusps were reduced by 1.5 mm and 2 mm, respectively, in all three groups according to the cuspal slope [5–8]. The diameter of the bur was used as a guide for adequate depth of cusp reduction such that two guiding grooves were created at the two sides of the cusp tip, and then, the grooves were connected and the cusps were reduced (Fig. 1) [1].
Restoration of teeth:
In group 2, the entire cavity was etched with 37% phosphoric acid for 20 seconds. The entire area was rinsed for 10 seconds. After drying, the All-Bond Universal adhesive was applied to the cavity and cured for 20 seconds with an overlapping curing procedure using the LED light-curing unit at a light intensity of 1,500 mW/cm 2 . The P60 composite was incrementally applied and cured for 20 seconds with an overlapping curing procedure for the restoration of the teeth. The occlusal surface was formed using the mold fabricated earlier and cured [1].
In group 3, an IPS e.max Press onlay was fabricated for each tooth. The internal surface of e.max restorations was etched with 9.5% hydrofluoric acid (Bisco Dental Products, Schaumburg, IL, USA) for 20 seconds. After rinsing and drying, silane (Bisco Dental Products, Schaumburg, IL, USA) was applied to the internal surface for 40 seconds. The teeth were then etched with 37% phosphoric acid for 15 seconds [4]. The All-Bond Universal adhesive was applied to the cavity and cured for 20 seconds [1]. The Dou-Link cement (Bisco Dental Products, Schaumburg, IL, USA) was mixed and applied to the tooth and the restoration. Excess cement was removed. Each sample was light-cured from the occlusal, buccal, and palatal aspects for 40 seconds [4].
Fracture mode:
The teeth were mounted in cylindrical molds with a 3cm height and a 2.5cm diameter containing autopolymerizing red acrylic resin to 2 mm below their CEJ [1].
The teeth were then placed in a chewing simulator (Mechatronik GmbH, Feldkirchen- Westerham, Germany) and subjected to 100,000 cycles under a 30N load to simulate horizontal and vertical masticatory forces applied to teeth in the oral cavity [12,13]. After cyclic loading, the teeth were transferred to a universal testing machine (Zwick/Roell, Ulm, Germany), and the load was applied along the longitudinal axes of the teeth by a conical steel cylinder with a 4mm diameter at a crosshead speed of 1 mm/minute. The load was increased until fracture. The maximum load causing fracture was recorded in Newtons (N) [1]. After the fracture, the teeth were inspected under the stereomicroscope at ×25 magnification to determine the failure mode as repairable or irreparable (Fig. 2 and 3).
Fig. 2.
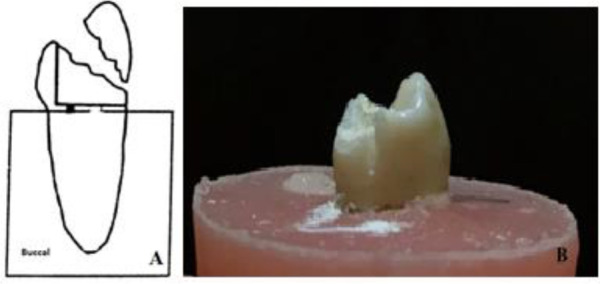
Schematic (A) and actual (B) reparable mode of failure
Fig. 3.
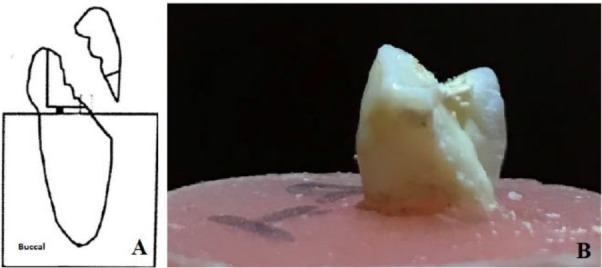
Schematic (A) and actual (B) irreparable mode of failure
Statistical analysis:
The mean, standard deviation (SD), and maximum and minimum fracture resistances were reported. The Kolmogorov-Smirnov test was used to assess the normal distribution of data, which showed that the data were normally distributed. Thus, the three groups were compared regarding their fracture resistance using analysis of variance (ANOVA). Pairwise comparisons were made using Tukey’s test. Chi-square test was used to compare the groups in terms of the fracture mode. All statistical analyses were carried out using SPSS version 22 (SPSS Inc., Chicago, IL, USA). P<0.05 was considered statistically significant.
RESULTS
Table 1 shows the fracture resistance of the three groups.
Table 1.
Fracture resistance in all groups (n=15)
| Group | Mean±SD | Min | Max | CV |
|---|---|---|---|---|
| Control | 1423±611 | 675 | 2507 | 43 |
| Direct onlay | 1008±399 | 606 | 2028 | 40 |
| Indirect onlay | 1080±487 | 474 | 1878 | 45 |
SD: Standard Deviation; CV: Coefficient of Variation; Min: Minimum; Max: Maximum
According to ANOVA, the difference in fracture resistance was significant among the three groups (P<0.001). Pairwise comparisons revealed that the difference between the control group and the two experimental groups was significant (P<0.001) but the difference between direct and indirect onlay restorations was not significant regarding the fracture resistance (P=0.6).
Regarding the mode of failure (Table 2), 26.7% (n=4) of fractures in the control group, 53.3% (n=8) of fractures in the direct onlay group, and 92.8% (n=13) of fractures in the indirect onlay group were irreparable.
Table 2.
Frequency of fracture modes in the three groups
| Group | Repairable N(%) | Irreparable N(%) |
|---|---|---|
| Control | 11(73.3) | 4(26.7) |
| Direct onlay | 7(46.7) | 8(53.3) |
| Indirect onlay | 1(7.2) | 13(92.8) |
According to the chi-square test, the percentage of irreparable fractures was significantly higher in the indirect onlay group (P<0.005).
DISCUSSION
This study assessed the fracture resistance and mode of failure of endodontically treated premolars restored with direct and indirect onlays. The results showed that sound teeth had the highest and direct onlay restorations had the lowest fracture resistance but no significant difference was noted in the fracture resistance of direct and indirect onlay groups. Evidence shows that the maximum masticatory force applied to the posterior teeth is 725 N in the clinical setting [14]. Thus, all teeth in our study, after cyclic loading for 100,000 cycles, could resist functional and parafunctional masticatory loads. According to the results, indirect onlay restorations provided 75% of the fracture resistance of sound teeth while this rate was 70% for direct restorations.
The selection of maxillary premolars for this study was due to their small volume of the crown and inappropriate crown/root ratio, which makes them more susceptible to cusp fracture compared to molars [4]. The fracture resistance of teeth directly depends on the amount of remaining sound tooth structure. Removal of the marginal ridge, increased isthmus width, and deep cavities are the main factors decreasing the fracture resistance of teeth [6]. Thus, endodontic treatment compromises the fracture resistance of teeth due to the removal of a large portion of tooth structure [6]. After endodontic treatment, the tendency for cuspal flexure under masticatory loads increases. Over time, frequent periodic stresses decrease the fracture resistance and result in tooth fracture under lower than normal loads [6]. Also, evidence shows that the protective mechanism of teeth against forces is no longer present following the removal of the pulp. On the other hand, the preparation of an MOD cavity creates long cusps that decrease the fracture resistance of teeth [2]. Thus, cuspal coverage is a major criterion for the clinical success of endodontically treated restored teeth. Takahashi et al [15] indicated that cuspal coverage increases the fracture resistance of endodontically treated teeth. Moreover, Fennis et al [16] revealed that premolars restored with onlay restorations could better tolerate cyclic loading. Seow et al [8], in 2015, stated that full-ceramic restorations, inlays, and onlays with cuspal coverage are the best options for the restoration of endodontically treated premolars.
Direct composite restorations have an easy application, excellent esthetics, and optimal mechanical properties; they reinforce the remaining tooth structure [14]. Bonding agents provide adequate retention for composite resins, serve as a bridge, and splint the buccal and lingual cusps [17]. However, technical sensitivity, polymerization shrinkage, postoperative tooth hypersensitivity, and low wear resistance are among the drawbacks of composite resins. Ceramic restorations have superior esthetics and better biocompatibility and are more resistant to wear. They have a coefficient of thermal expansion similar to that of the enamel. On the other hand, they are fragile and expensive and their fabrication is time-consuming [14]. It has been shown that cemented and bonded restorations decrease cuspal flexure and increase the fracture resistance of endodontically treated teeth [6].
In our study, sound teeth showed fracture resistance up to 1,423 N, which was similar to the findings of other studies [2,6,14,18]. Bianchi E Silva et al [6] evaluated the effect of direct and indirect composite restorations and ceramics on the fracture resistance of endodontically treated premolars and found no significant difference in the fracture resistance of the three groups, which was in agreement with our results. The fracture resistance of teeth restored with ceramic restorations was slightly but not significantly higher but this group had a higher frequency of irreparable fractures as well. This is due to the higher modulus of elasticity of ceramic than composite. Thus, a lower amount of load is absorbed by ceramics, compared to composite resins, and ceramics transfer a greater load to the underlying tooth structure, resulting in more severe fractures. They explained that the use of indirect restorations for the protection of teeth against fracture is not justifiable because direct restorations are as efficient as indirect restorations in this respect [6]. Jiang et al [19] showed that the level of stress applied to teeth increases with an increase in the modulus of elasticity of restorative materials, and composite onlays, compared to gold and ceramic, have the best performance in decreasing the internal stresses. Since internal stresses are the primary cause of restoration fracture, composite resins can better restore the structural integrity of teeth [19]. Rezvani et al [17] compared the fracture resistance of maxillary premolars restored with direct and indirect composite restorations and showed that both types of restoration increase the fracture resistance of teeth and are suitable for the reinforcement of compromised teeth. Xie et al [7] demonstrated that the fracture resistance of teeth restored with composites with coverage of both cusps was almost similar to that of sound teeth. However, coverage of all cusps increases the risk of irreparable fractures due to the accumulation of stress in the intercuspal groove. Santos and Bezerra [20] compared direct composite and indirect ceramic restorations of premolars with MOD cavities and found no significant difference between the two in terms of the fracture resistance, which was in line with our results.
However, some studies have reported results in contrast to our findings. For instance, Al Amri et al [21] compared the effect of amalgam restorations, composite restorations, ceramic inlays and onlays, and zirconia crowns on the fracture resistance of first molars and found that composite restorations and zirconia crowns yielded the highest fracture resistance with no significant difference between them. However, composite samples showed unfavorable fractures due to the strong bond of the composite to tooth structure [21]. Type of tooth, the technique of storage of samples, type of composite, and angle of load application can explain the difference in the results.
Sarabi et al [4] compared the fracture resistance of sound teeth, indirect composite and ceramic, and direct composite restorations and found that the fracture resistance of teeth restored with direct composites was higher than that of teeth restored with indirect composite and ceramic restorations. In addition, most direct composite fractures occurred below the CEJ while the most frequent mode of failure of ceramic onlays was the cohesive type. They stated that due to the similar modulus of elasticity of dentin and composite, stress is applied to the dentin in the root and the crown, causing root fracture. Cohesive fracture of ceramic was attributed to its brittleness and accumulation of stress in its structure [4]. The difference between their findings and ours may be due to the method of storage of teeth. Also, they only reduced the palatal cusps. They used different types of composite and ceramic. Furthermore, we applied the load with a ball-shaped tool while they used a crosshead with a sharp tip for load application. The crosshead speed was also different in the two studies.
In our study, the indirect onlay group showed a significantly higher frequency of irreparable fractures. Ragauska et al [14] showed a higher frequency of irreparable fractures in composites compared to ceramics and attributed it to the similar modulus of elasticity of teeth and composites and the strong bond between them. They simulated the periodontal ligament (PDL) with low-viscosity polyvinyl siloxane, which was not performed in our study. Moreover, they applied the load with a cylindrical tool at a different crosshead speed compared to our study, which may explain the difference in the results. Brunton et al [22] discussed that the higher the hardness of the restorative material, the more severe the fracture in the underlying tooth structure would be. This finding confirms our results.
In previous studies, the load was applied at a 45° angle relative to the longitudinal axis of the tooth to better simulate masticatory loads applied to teeth in the oral environment [1,23]. However, this could not be done in our study because if we had mounted the teeth at a 45° angle for cyclic loading, we had to remount them for fracture resistance testing in the universal testing machine, and therefore, we might have lost some samples.
Dynamic fatigue tests are efficient tools for the assessment of the long-term stability of materials under frequent stresses. A restored molar tolerates 60–200 N of masticatory loads. This load may increase to 500–800 N in bruxism. There are 800–1400 cycles of mastication per day. Thus, 500,000 cycles correspond to one year of mastication [24]. In the current study, 100,000 cycles of a 30N load were applied. Evidence shows that 100,000 cycles of a 30N load may have no significant effect on the fracture resistance of teeth while 500,000 cycles of a 250N load decrease the fracture resistance of teeth by 20–30% [25].
In-vitro tests cannot well simulate the clinical setting, and the generalization of their findings to the clinical setting must be done with caution. Future studies with a higher frequency of load cycles and better simulation of clinical settings are required to obtain accurate results.
CONCLUSION
Direct and indirect onlay restorations cannot increase the fracture resistance of endodontically treated premolars as high as that of sound teeth. Direct and indirect onlay restorations provide almost equal fracture resistances but the frequency of irreparable fractures is significantly higher in indirect onlay restorations.
ACKNOWLEDGMENTS
We would like to express our special appreciation to Mr. Naser Valaei for his sincere advice on statistical analysis of this research. We would also like to show gratitude to Dental Research Center, Dentistry Research Institute, Tehran University of Medical Sciences for their supportive cooperation.
Footnotes
CONFLICT OF INTEREST STATEMENT
None declared
REFERENCES
- 1.Kazemi Yazdi H, Aryan N, Shahbazi moghadam M. A comparison of the effect of three direct composite restoration techniques on the fracture resistance of endodontically treated maxillary premolars. J Res Dent Maxillofac Sci. 2014;11(4):199–208. [Google Scholar]
- 2.Alshiddi IF, Aljinbaz A. Fracture resistance of endodontically treated teeth restored with indirect composite inlay and onlay restorations - An in vitro study. Saudi Dent J. 2016. Jan;28(1):49–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Monga P, Sharma V, Kumar S. Comparison of fracture resistance of endodontically treated teeth using different coronal restorative materials: An in vitro study. J Conserv Dent. 2009. Oct;12(4):154–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sarabi N, Taji H, Jalayer J, Ghaffari N, Forghani M. Fracture resistance and failure mode of endodontically treated premolars restored with different adhesive restorations. J Dent Mater Tech. 2015. Mar;4(1):13–20. [Google Scholar]
- 5.Mynampati P, Babu MR, Saraswathi DD, Kumar JR, Gudugunta L, Gaddam D. Comparison of fracture resistance and failure pattern of endodontically treated premolars with different esthetic onlay systems: An in vitro study. J Conserv Dent. 2015. Mar–Apr;18(2):140–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bianchi E Silva AA, Ghiggi PC, Mota EG, Borges GA, Burnett LH, Jr, Spohr AM. Influence of restorative techniques on fracture load of endodontically treated premolars. Stomatologija. 2013;15(4):123–8. [PubMed] [Google Scholar]
- 7.Xie KX, Wang XY, Gao XJ, Yuan CY, Li JX, Chu CH. Fracture resistance of root filled premolar teeth restored with direct composite resin with or without cusp coverage. Int Endod J. 2012. Jun;45(6):524–9. [DOI] [PubMed] [Google Scholar]
- 8.Seow LL, Toh CG, Wilson NH. Strain measurements and fracture resistance of endodontically treated premolars restored with all-ceramic restorations. J Dent. 2015. Jan;43(1):126–32. [DOI] [PubMed] [Google Scholar]
- 9.Eakle WS, Maxwell EH, Braly BV. Fractures of posterior teeth in adults. J Am Dent Assoc. 1986. Feb;112(2):215–8. [DOI] [PubMed] [Google Scholar]
- 10.Fennis WM, Tezvergil A, Kuijs RH, Lassila LV, Kreulen CM, Creugers NH, et al. In vitro fracture resistance of fiber reinforced cusp-replacing composite restorations. Dent Mater. 2005. Jun;21(6):565–72. [DOI] [PubMed] [Google Scholar]
- 11.Kivanç BH, Alaçam T, Görgül G. Fracture resistance of premolars with one remaining cavity wall restored using different techniques. Dent Mater J. 2010. May;29(3):262–7. [DOI] [PubMed] [Google Scholar]
- 12.Heydecke G, Butz F, Strub JR. Fracture strength and survival rate of endodontically treated maxillary incisors with approximal cavities after restoration with different post and core systems: an in-vitro study. J Dent. 2001. Aug;29(6):427–33. [DOI] [PubMed] [Google Scholar]
- 13.Yamada Y, Tsubota Y, Fukushima S. Effect of restoration method on fracture resistance of endodontically treated maxillary premolars. Int J Prosthodont. 2004. Jan–Feb;17(1):94–8. [PubMed] [Google Scholar]
- 14.Ragauska A, Apse P, Kasjanovs V, Berzina-Cimdina L. Influence of ceramic inlays and composite fillings on fracture resistance of premolars in vitro. Stomatologija. 2008;10(4):121–6. [PubMed] [Google Scholar]
- 15.Takahashi CU, De Cara AA, Cotin I. [Resistance to fracture of direct restorations with cuspal coverage in endodontically treated upper bicuspids]. [Article in Portuguese]. Pesqui Odontol Bras. 2001. Jul–Sep;15(3):247–51. [DOI] [PubMed] [Google Scholar]
- 16.Fennis WM, Kuijs RH, Kreulen CM, Verdonschot N, Creugers NH. Fatigue resistance of teeth restored with cuspal-coverage composite restorations. Int J Prosthodont. 2004. May–Jun;17(3):313–7. [PubMed] [Google Scholar]
- 17.Rezvani MB, Mohammadi Basir M, Mollaverdi F, Moradi Z, Soboot AR. Comparison of direct and indirect composite resin restorations effect on the fracture resistance of maxillary premolars: An in vitro study. J Dent Sch Shahid Beheshti Univ Med Sci. 2012. Winter;29(5):299–305. [Google Scholar]
- 18.Moezizadeh M, Mokhtari N. Fracture resistance of endodontically treated premolars with direct composite restorations. J Conserv Dent. 2011. Jul;14(3):277–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jiang W, Bo H, Yongchun G, LongXing N. Stress distribution in molars restored with inlays or onlays with or without endodontic treatment: a three-dimensional finite element analysis. J Prosthet Dent. 2010. Jan;103(1):6–12. [DOI] [PubMed] [Google Scholar]
- 20.Santos MJ, Bezerra RB. Fracture resistance of maxillary premolars restored with direct and indirect adhesive techniques. J Can Dent Assoc. 2005. Sep;71(8):585. [PubMed] [Google Scholar]
- 21.Al Amri MD, Al-Johany S, Sherfudhin H, Al Shammari B, Al Mohefer S, Al Saloum M, et al. Fracture resistance of endodontically treated mandibular first molars with conservative access cavity and different restorative techniques: An in vitro study. Aust Endod J. 2016. Dec;42(3):124–131. [DOI] [PubMed] [Google Scholar]
- 22.Brunton PA, Cattell P, Burke FJ, Wilson NH. Fracture resistance of teeth restored with onlays of three contemporary tooth-colored resin-bonded restorative materials. J Prosthet Dent. 1999. Aug;82(2):167–71. [DOI] [PubMed] [Google Scholar]
- 23.Taha NA, Palamara JE, Messer HH. Fracture strength and fracture patterns of root-filled teeth restored with direct resin composite restorations under static and fatigue loading. Oper Dent. 2014. Mar–Apr;39(2):181–8. [DOI] [PubMed] [Google Scholar]
- 24.Wang RR, Lu CL, Wang G, Zhang DS. Influence of cyclic loading on the fracture toughness and load bearing capacities of all-ceramic crowns. Int J Oral Sci. 2014. Jun;6(2):99–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xible AA, de Jesus Tavarez RR, de Araujo Cdos R, Conti PC, Bonachella WC. Effect of cyclic loading on fracture strength of endodontically treated teeth restored with conventional and esthetic posts. J Appl Oral Sci. 2006. Aug;14(4):297–303. [DOI] [PMC free article] [PubMed] [Google Scholar]


