Abstract
Objectives:
This in-vitro study aimed to evaluate the effect of cavity disinfection with chlorhexidine (CHX) on marginal gaps of Class V composite resin restorations bonded with a universal adhesive using self-etch and etch-and-rinse bonding strategy.
Materials and Methods:
Sixty sound human premolars were randomly assigned to two groups (n=30): group 1 (CHX) and group 2 (no CHX). Each group was divided into two subgroups (n=15) according to the bonding strategy of the universal adhesive (self-etch or etch-and-rinse). Class V cavities were prepared on the buccal surfaces of the teeth. The occlusal and gingival margins of the cavities were placed in enamel and dentin, respectively. In the first and second subgroups of both groups, the All-Bond Universal adhesive was applied with self-etch and etch-and-rinse bonding strategy, respectively. After restoration and thermocycling, the samples were sectioned, and marginal gaps at the gingival margins were measured in micrometer (μm) under a stereomicroscope. Two-way analysis of variance (ANOVA) was used to compare marginal gaps between the groups and the subgroups.
Results:
The mean marginal gap size was significantly affected by cavity disinfection (P=0.001) and bonding strategy (P=0.002). However, the interaction effect of these two factors on the mean marginal gap size was not significant (P=0.79).
Conclusion:
The use of CHX resulted in larger marginal gaps at the gingival margins of Class V composite resin restorations. Irrespective of disinfection, the self-etch bonding strategy resulted in larger marginal gaps compared to the etch-and-rinse bonding strategy.
Keywords: Adhesives, Chlorhexidine, Dental Bonding, Dental Restoration, Disinfection, Dental Marginal Adaptations
INTRODUCTION
Polymerization shrinkage of composite resins and the resultant gaps at the tooth-composite resin interface is the most important problem in composite resin restorations. These gaps can lead to microleakage, recurrent caries, dental hypersensitivity, discoloration, pulpitis, and finally, bond failure [1]. The problems mentioned above can be aggravated in the presence of viable microorganisms that remain after cavity preparation [1]. It has been reported that only a small part of the cavity is sterile after cavity preparation [2], and the residual bacteria can maintain their activity for some time (more than a year) in dentin [3,4]. Various antibacterial solutions, including chlorhexidine (CHX), sodium hypochlorite (NaOCl), and benzalkonium chloride, have been introduced for cavity disinfection [5]. Different studies have introduced CHX as an effective agent for cavity disinfection [1,6]. CHX is soluble in water and has a physiological pH. It inhibits bacterial adhesion by bonding to Ca 2+ [7]. However, some studies have shown that the use of disinfecting agents can affect the bonding ability and seal of bonded restorations to dentin, leading to increased microleakage [1,8, 9]. Previous studies have evaluated the effect of cavity disinfecting agents on the bonding of composite resin restorations, and different results have been reported in terms of the type of disinfecting agents and bonding systems [10–14]. Some studies have demonstrated an increase in the marginal gap [7] and microleakage [1] and a decrease in the dentin bond strength of composite resins [10–12]. However, some other studies have reported no change in the dentin bond strength of composite resins after the use of CHX [9,13, 14].
Recently, a new generation of adhesive systems, referred to as universal adhesives, has been introduced, which consists of one bottle and can bond to tooth structure through the acid-etching and self-etching techniques [14,15]. In addition, universal adhesives can form a bond with different substrates, such as metals and ceramics [14]. Limited data are available on the efficacy of these adhesives [14]. One study has shown that the use of the All-Bond Universal and Single Bond Universal adhesives results in a higher microtensile bond strength with the etch-and-rinse strategy compared to the self-etch strategy [16]. Another study evaluated the bonding properties of three universal adhesives (All-Bond Universal Adhesive, Scotchbond Universal Adhesive, and Peak Universal Adhesive) [17]. The results showed that the microtensile bond strength of the three adhesives was higher with the etch-and-rinse strategy compared to the self-etch strategy [17]. However, some other studies have shown the same microtensile bond strength to dentin with the application of mild universal adhesives using the etch-and-rinse and self-etch bonding strategy [18].
Since little information is available on the effect of cavity disinfecting agents on the marginal gaps of composite resin restorations bonded with universal adhesives, this in-vitro study aimed to evaluate the effect of cavity disinfection with CHX on the marginal gaps of Class V composite resin restorations bonded with universal adhesives using the self-etch and etch-and-rinse bonding strategy.
MATERIALS AND METHODS
The protocol of the current study has been approved by the Regional Medical Research Ethics Committee (reference number: IR.TBZMED.REC.1397.874). Sixty sound human extracted premolars were selected for this in-vitro study. The teeth had been extracted for orthodontic treatment and had no cracks, fractures, or structural defects in the visual examination and under a stereomicroscope (Nikon, SMZ1000, Tokyo, Japan).
Sample size determination:
The sample size was determined to be 13 in each subgroup by considering use or non-use of CHX, α=0.05, a study power of 80%, and a difference of 3 units in the mean marginal gaps between the groups based on the mean marginal gap sizes in a previous study [7]. However, the sample size was increased to 15 in each subgroup (60 samples) to increase the validity of the study.
The samples were immersed in a 0.5% Chloramine-T solution (Merck KGaA, Darmstadt, Germany) for disinfection for seven days, followed by storage in distilled water in a refrigerator at 4ºC. The storage solution was renewed regularly. After 24 hours, before undertaking the procedural steps, the samples were conditioned by being transferred into distilled water at 23±2ºC.
Class V cavities, measuring 3×2×2 mm 3 , were prepared on the buccal surfaces of the teeth with the occlusal margin of the cavity located 1 mm above the cementoenamel junction (CEJ) and the gingival margin located 1 mm below the CEJ. Before the preparation of the cavities, the dimensions of the cavity were drawn on each tooth using a standard template. The depth of each cavity was measured using a probe [19]. The cavities were prepared using a #01 diamond fissure bur (Diatech Dental AG, Heerbrugg, Switzerland) mounted on a high-speed handpiece under air and water cooling. A new bur was used after every five preparations. All the cavity margins were butt joint (90º) with no bevel. The teeth were divided into two groups (n=30) according to the use or non-use of the CHX disinfecting agent. In each group, the teeth were subdivided into two subgroups (n=15) according to the use of the universal bonding agent with the self-etch or etch-and-rinse strategy.
In subgroup 1 of group 1 (no CHX), the All-Bond Universal adhesive (Bisco Inc., Schaumburg, IL, USA) was used with the self-etch bonding strategy according to the manufacturer’s instructions. Two layers of the adhesive were applied, and each layer was rubbed for 10–15 seconds using a microbrush. The excess solvent was evaporated using airstream for 10 seconds, and the adhesive was light-cured for 10 seconds using a light-curing unit (Dentamerica Inc., City of Industry, CA, USA) at a light intensity of 400 mW/cm 2 perpendicular to the surface according to the manufacturer’s instructions. The Aelite All-Purpose Body composite resin (A2 shade; Bisco Inc., Schaumburg, IL, USA) was used to restore the cavities with the horizontal incremental technique (two 1mm layers). After the restorative procedures, the samples were polished with diamond polishing burs (Diamant GmbH, D&Z, Berlin, Germany) and disks (Sof-Lex TM , 3M ESPE Dental Products, St. Paul, MN, USA). Then, the samples were incubated in distilled water at 37ºC for 24 hours. To simulate the oral condition, the teeth underwent a thermocycling procedure consisting of 500 cycles at 5±2ºC/55±2ºC with a dwell time of 30 seconds and a transfer time of 10 seconds in a water bath. Then, the samples were sectioned at the middle of the restoration in a buccolingual direction using a diamond disk (Diamant GmbH, D&Z, Berlin, Germany). Next, the gingival marginal gaps of the restorations were measured in micrometer (μm) under the stereomicroscope at ×40 magnification.
Some selected areas underwent digital photography using a DS-L2 control unit (Nikon, Tokyo, Japan) to measure the gap size. The built-in software program was used to measure the gaps. A tangential line on the tooth-side vector was used to determine the distance between the points on the restoration-side vector and the line above. The outer, middle, and inner portions of the gingival margins underwent repeated measurements. The mean of the marginal gap sizes at the three sites was calculated in μm in the study groups [20].
In the second subgroup of group 1, all the procedures were similar to those in subgroup 1, except that the universal adhesive was applied with the etch-and-rinse bonding strategy according to the manufacturer’s instructions. The enamel and dentin were etched for 15 seconds with 35% phosphoric acid gel (Bisco Inc., Schaumburg, IL, USA) followed by rinsing and elimination of excess water with an air spray for 1–2 seconds. Two layers of the adhesive were applied, and each layer was rubbed for 10–15 seconds with an airstream for 10 seconds. The adhesive was light-cured for 10 seconds.
In the first and second subgroups of group 2 (CHX), all the procedures were similar to subgroups 1 and 2 of group 1, respectively, except that after the preparation of the cavity and before the bonding process, 2% CHX gluconate disinfecting solution (Consepsis, Ultradent Products Inc., South Jordan, UT, USA) was used to disinfect the cavity. A microbrush was used to apply the 2% CHX solution to the cavity walls. CHX remained in contact with the cavity walls for 20 seconds followed by drying with an air syringe for 15 seconds [7].
Data were analyzed with two-way analysis of variance (ANOVA) using SPSS version 16 (SPSS Inc. Chicago, IL, USA). Kolmogorov-Smirnov test was used to evaluate the normal distribution of data. The statistical significance was defined as P<0.05.
RESULTS
Table 1 shows the descriptive statistics [means and standard deviations (SD)] of marginal gaps of the groups and subgroups of the study.
Table 1.
Means and standard deviations (SD) of marginal gap size (μm) in the study groups and subgroups (N=15)
| Cavity disinfection | Bonding strategy | Min | Max | Mean±SD |
|---|---|---|---|---|
| No use of chlorhexidine | Self-etch | 4.31 | 7.20 | 5.77±0.98 |
| Etch and rinse | 2.97 | 7.07 | 4.74±1.25 | |
| Use of chlorhexidine | Self-etch | 3.60 | 9.79 | 7.07±1.62 |
| Etch and rinse | 4.49 | 9.17 | 5.86±1.47 |
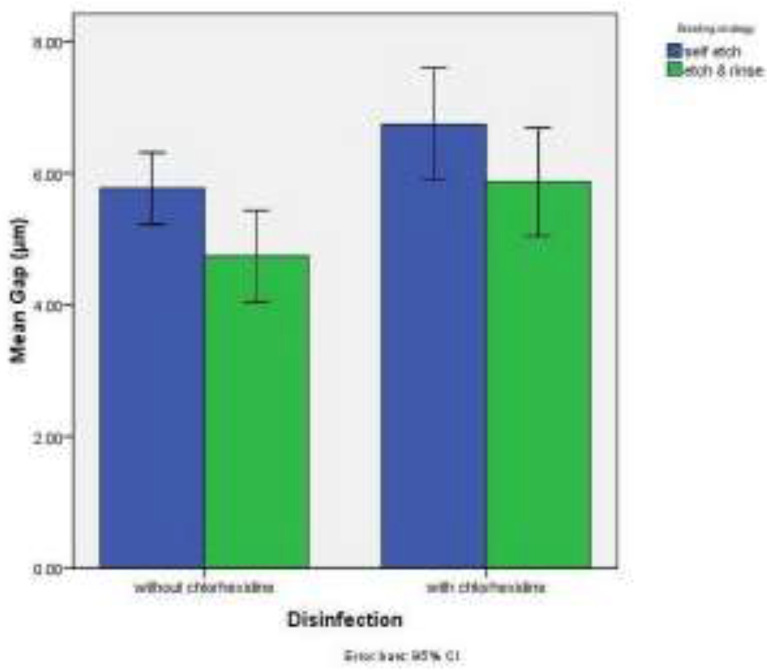
Figure 1 presents the error-bar graph of the mean marginal gaps in the study groups and subgroups according to cavity disinfection (use or non-use of CHX).
Fig. 1.
Error-bar graph of mean marginal gap size (μm) in the study groups and subgroups according to cavity disinfection
The results of two-way ANOVA showed that the difference in the mean marginal gap size was significant between the CHX and non-CHX groups (F 1,56 =12.09, P=0.001). The marginal gap sizes in the CHX groups were significantly larger compared to the non-CHX groups (P<0.001).
The difference in the mean marginal gap size was significant between the self-etch and etch-and-rinse groups (F 1,56 =10.21, P=0.002). The marginal gaps were significantly larger with the self-etch bonding strategy compared to the etch-and-rinse bonding strategy (P<0.001).
However, the interaction effect of these two factors (cavity disinfection and bonding strategy) on the mean marginal gap was not significant (F 1,56 =0.06, P=0.79).
DISCUSSION
Microorganisms that remain beneath restorative materials might lead to recurrent caries, negatively affecting the durability of the restorations [12]. Therefore, the use of cavity disinfecting agents has been recommended after the preparation of the cavity to decrease the counts of residual bacteria [1].
The present study evaluated the effect of cavity disinfection with CHX on the marginal gaps of Class V cavities restored with a composite resin bonded with a universal adhesive using the self-etch and etch-and-rinse bonding strategy. The results showed that CHX resulted in a significant increase in marginal gaps, irrespective of the bonding strategy used. In this context, Kimyai et al [7] showed that CHX increases the marginal gaps of Class V giomer restorations bonded with the BeautiBond self-etch adhesive. Singla et al [1] reported that the use of CHX in Class II composite resin restorations bonded with the Adper™ Easy One Self-Etch adhesive resulted in an increase in microleakage at the gingival margins. Suma et al [10] concluded that CHX results in a decrease in the shear bond strength of composite resins boned with the Adper™ Prompt self-etch adhesive to dentin [10]. In a study by Reddy et al [11], the use of CHX resulted in a decrease in the shear bond strength of composite resins bonded to dentin with the Adper™ Easy One and Adper™ SE Plus self-etch adhesives. Vieira Rde and da Silva [12] reported that CHX resulted in a decrease in the shear bond strength of composite resins bonded to the dentin of deciduous teeth with the Single Bond total-etch adhesive.
The adhesive used in the present study was the All-Bond Universal adhesive, which is considered an ultra-mild adhesive (pH=3.1) based on the pH value classification [18]. A scanning electron microscopic (SEM) evaluation of the dentin surface has shown some precipitates on the surface after exposure to 2% CHX [21]. The symmetrical CHX molecule has two positive charges that mediate electrostatic attraction to the phosphate anions in the hydroxyapatite structure to form crystals that serve as mechanical barriers to the formation of an effective hybrid layer [22]. Furthermore, it has been speculated that dentin is rendered resistant to acid conditioning because of CHX residues [7]. It appears that the presence of an acid-resistant layer in combination with weak acidity (a high pH) of the All-Bond Universal adhesive has an inhibitory effect on the demineralization of dentin surfaces, which might result in inadequate bonding and an increase in marginal gaps. In addition, it has been stated that the acid-resistant layer prevents the penetration of hydrophilic resin into dentin. The remnants of CHX can react with the calcium and the phosphate of dentin, decreasing the bonding ability [10,21, 22]. The All-Bond Universal adhesive contains 10-MDP (10-Methacryloyloxydecyl dihydrogen phos-phate) [16], which can form a chemical bond with the calcium of hydroxyapatite remaining around collagen fibers [19]. It appears that the reaction of CHX with the calcium of dentin results in lower levels of calcium available for bonding with the 10-MDP; therefore, the adhesive cannot form a proper bond to tooth structures [19]. Another study has shown that CHX compromises the bond of the adhesive by decreasing the wettability of dentin [11].
However, in two previous studies, the use of CHX did not result in any change in the shear bond strength of composite to dentin with the use of the Clearfil Protect Bond and Clearfil SE Bond self-etch adhesives [9] or with the use of the Prime & Bond NT etch-and-rinse adhesive [13]. The differences between the results of the present study and those of the studies above [9,13] might be attributed to differences in the adhesives used, their different pH, and the dependent variables evaluated in different studies (bond strength and/or gap).
Another finding of the present study was the fact that irrespective of disinfection with CHX, marginal gaps at the gingival margins (in dentin) were significantly larger with the use of universal adhesives and the self-etch strategy compared to the etch-and-rinse strategy. In this context, it has been reported that the dentin bond strength of the All-Bond Universal adhesive (an ultra-mild adhesive) improves with a separate acid-etching procedure before the application of the adhesive, which might be attributed to the high pH and weak acidity of this adhesive as it cannot properly condition and prime the dentin. However, with other universal adhesives, which are mild according to the pH classification, the dentin bond showed similar strengths with both etch-and-rinse and self-etch bonding strategies [18].
The smear layer is considered a barrier against the penetration of acidic monomers. A separate acid-etching procedure might increase the penetration of monomers and the formation of an integrated hybrid layer with dentin [18,23]. A SEM study showed that the use of the All-Bond Universal adhesive with the self-etch bonding strategy renders a hybrid layer devoid of resin tags whereas, with the etch-and-rinse bonding strategy, the hybrid layer is associated with well-formed, funnel-shaped, and long resin tags within the dentinal tubules [16]. Regarding the marginal gap, the results of one study showed that the etch-and-rinse bonding protocol exhibits significantly smaller marginal gaps for tested universal adhesives compared to the self-etch bonding protocol [24]. It has been stated that the application of universal adhesives with the self-etch protocol does not modify the smear layer or penetrate the dentinal tubules; subsequently, a very thin hybrid layer is formed [24]. The oral cavity conditions always differ from the outside environment; this difference is attributed to different physical and chemical factors [16,18]; therefore, it is necessary to carry out long-term studies by simulating the oral cavity conditions to more properly evaluate the adhesive interface. Moreover, the adhesive interface can be evaluated using SEM and confocal laser scanning microscopy (CLSM) to achieve valid results. In addition, it is advisable to evaluate the effect of CHX and other cavity disinfecting agents on the dentin bond of universal adhesives with different acidity.
CONCLUSION
Under the limitations of the present study, it can be concluded that the use of CHX disinfecting agent increases the size of the gingival margin gaps, irrespective of the bonding strategy applied. Regardless of cavity disinfection, the self-etch bonding strategy renders larger marginal gaps.
ACKNOWLEDGMENTS
The authors extend their gratitude to the Vice Chancellor for Research at Tabriz University of Medical Sciences for their financial support. Furthermore, the authors would like to thank Dr. Majid Abdolrahimi (D.D.S.), who edited the English manuscript of this article.
Footnotes
CONFLICT OF INTEREST STATEMENT
None declared
REFERENCES
- 1.Singla M, Aggarwal V, Kumar N. Effect of chlorhexidine cavity disinfection on microleakage in cavities restored with composite using a self-etching single bottle adhesive. J Conserv Dent. 2011. Oct;14(4):374–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brännström M. The cause of postrestorative sensitivity and its prevention. J Endod. 1986. Oct;12(10):475–81. [DOI] [PubMed] [Google Scholar]
- 3.Yip HK, Stevenson AG, Beeley JA. The specificity of caries detector dyes in cavity preparation. Br Dent J. 1994. Jun;176(11):417–21. [DOI] [PubMed] [Google Scholar]
- 4.Gürgan S, Bolay S, Kiremitçi A. Effect of disinfectant application methods on the bond strength of composite to dentin. J Oral Rehabil. 1999. Oct;26(10):836–40. [DOI] [PubMed] [Google Scholar]
- 5.Turkun M, Ozata F, Uzer E, Ates M. Antimicrobial substantivity of cavity disinfectants. Gen Dent. 2005. May–Jun;53(3):182–6. [PubMed] [Google Scholar]
- 6.Ersin NK, Aykut A, Candan U, Onçağ O, Eronat C, Kose T. The effect of a chlorhexidine containing cavity disinfectant on the clinical performance of high-viscosity glass-ionomer cement following ART: 24-month results. Am J Dent. 2008. Feb;21(1):39–43. [PubMed] [Google Scholar]
- 7.Kimyai S, Pournaghi-Azar F, Naser-Alavi F, Salari A. Effect of disinfecting the cavity with chlorhexidine on the marginal gaps of Cl V giomer restorations. J Clin Exp Dent. 2017. Feb 1;9(2):e202–e206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tulunoglu O, Ayhan H, Olmez A, Bodur H. The effect of cavity disinfectants on microleakage in dentin bonding systems. J Clin Pediatr Dent. 1998. Summer;22(4):299–305. [PubMed] [Google Scholar]
- 9.Sacramento PA, de Castilho AR, Banzi EC, Puppi-Rontani RM. Influence of cavity disinfectant and adhesive systems on the bonding procedure in demineralized dentin - a one-year in vitro evaluation. J Adhes Dent. 2012. Dec;14(6):575–83. [DOI] [PubMed] [Google Scholar]
- 10.Suma NK, Shashibhushan KK, Subba Reddy VV. Effect of dentin disinfection with 2% chlorhexidine gluconate and 0.3% iodine on dentin bond strength: an in vitro study. Int J Clin Pediatr Dent. 2017. Jul–Sep;10(3):223–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reddy MS, Mahesh MC, Bhandary S, Pramod J, Shetty A, Prashanth MB. Evaluation of effect of different cavity disinfectants on shear bond strength of composite resin to dentin using two-step self-etch and one-step self-etch bonding systems: a comparative in vitro study. J Contemp Dent Pract. 2013. Mar;14(2):275–80. [DOI] [PubMed] [Google Scholar]
- 12.Vieira Rde S, da Silva IA, Jr.. Bond strength to primary tooth dentin following disinfection with a chlorhexidine solution: an in vitro study. Pediatr Dent. 2003. Jan–Feb;25(1):49–52. [PubMed] [Google Scholar]
- 13.Ercan E, Erdemir A, Zorba YO, Eldeniz AU, Dalli M, Ince B, et al. Effect of different cavity disinfectants on shear bond strength of composite resin to dentin. J Adhes Dent. 2009. Oct;11(5):343–6. [PubMed] [Google Scholar]
- 14.Dos Santos RA, de Lima EA, Montes MAJR, Braz R. Pre-treating dentin with chlorhexadine and CPP-ACP: self-etching and universal adhesive systems. Acta Biomater Odontol Scand. 2016. Jul 1;2(1):79–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shadman N, Farzin-Ebrahimi S, Mortazavi-Lahijani E, Jalali Z. Effect of chlorhexidine on the durability of a new universal adhesive system. J Clin Exp Dent. 2018. Sep 1;10(9):e921–e926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tekçe N, Tuncer S, Demirci M, Balci S. Do matrix metalloproteinase inhibitors improve the bond durability of universal dental adhesives? Scanning. 2016. Nov;38(6):535–44. [DOI] [PubMed] [Google Scholar]
- 17.Muñoz MA, Luque I, Hass V, Reis A, Loguercio AD, Bombarda NH. Immediate bonding properties of universal adhesives to dentine. J Dent. 2013. May;41(5):404–11. [DOI] [PubMed] [Google Scholar]
- 18.Rosa WL, Piva E, Silva AF. Bond strength of universal adhesives: A systematic review and meta-analysis. J Dent. 2015. Jul;43(7):765–76. [DOI] [PubMed] [Google Scholar]
- 19.Kimyai S, Ajami AA, Chaharom ME, Oskoee JS. Comparison of microleakage of three adhesive systems in class V composite restorations prepared with Er, Cr:YSGG laser. Photomed Laser Surg. 2010. Aug;28(4):505–10. [DOI] [PubMed] [Google Scholar]
- 20.Oskoee PA, Kimyai S, Ebrahimi Chaharom ME, Rikhtegaran S, Pournaghi-Azar F. Cervical margin integrity of Class II resin composite restorations in laser- and bur-prepared cavities using three different adhesive systems. Oper Dent. 2012. May–Jun;37(3):316–23. [DOI] [PubMed] [Google Scholar]
- 21.Di Hipólito V, Rodrigues FP, Piveta FB, Azevedo Lda C, Bruschi Alonso RC, Silikas N, et al. Effectiveness of self-adhesive luting cements in bonding to chlorhexidine-treated dentin. Dent Mater. 2012. May;28(5):495–501. [DOI] [PubMed] [Google Scholar]
- 22.Lima JFM, Wajngarten D, Islam F, Clifford J, Botta AC. Effect of adhesive mode and chlorhexidine on microtensile strength of universal bonding agent to sound and caries-affected dentins. Eur J Dent. 2018. Oct–Dec;12(4):553–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.De Munck J, Van Landuyt K, Peumans M, Poitevin A, Lambrechts P, Braem M, et al. A critical review of the durability of adhesion to tooth tissue: methods and results. J Dent Res. 2005. Feb;84(2):118–32. [DOI] [PubMed] [Google Scholar]
- 24.Al-Qrimli AF, Al-Shamma AMW. Comparative evaluation of the effect of different universal adhesives and bonding techniques on the marginal gap of class I composite restoration (a SEM study). J Bagh Coll Dent. 2016. Dec;28(4):34–42. [Google Scholar]