Abstract
Background and Objective
Community mitigation strategies could help reduce COVID-19 incidence, but there are few studies that explore associations nationally and by urbanicity. In a national county-level analysis, we examined the probability of being identified as a county with rapidly increasing COVID-19 incidence (rapid riser identification) during the summer of 2020 by implementation of mitigation policies prior to the summer, overall and by urbanicity.
Methods
We analyzed county-level data on rapid riser identification during June 1–September 30, 2020 and statewide closures and statewide mask mandates starting March 19 (obtained from state government websites). Poisson regression models with robust standard error estimation were used to examine differences in the probability of rapid riser identification by implementation of mitigation policies (P-value< .05); associations were adjusted for county population size.
Results
Counties in states that closed for 0–59 days were more likely to become a rapid riser county than those that closed for >59 days, particularly in nonmetropolitan areas. The probability of becoming a rapid riser county was 43% lower among counties that had statewide mask mandates at reopening (adjusted prevalence ratio = 0.57; 95% confidence intervals = 0.51–0.63); when stratified by urbanicity, associations were more pronounced in nonmetropolitan areas.
Conclusions
These results underscore the potential value of community mitigation strategies in limiting the COVID-19 spread, especially in nonmetropolitan areas.
Keywords: COVID-19, Closures, Mask mandates, Mitigation strategies
Introduction
To date, nearly 29 million people have been diagnosed with coronavirus disease 2019 (COVID-19) in the United States, of whom over 500,000 persons have died [1]. In addition, there has been increased spread of the B.1.1.7 SARS-CoV-2 variant in the United States that has been shown to be more transmissible than other variants [2], [3]. Community mitigation strategies, including staying home and wearing masks in public, can reduce the spread of SARS-CoV-2 [4]. Studies have shown that countries that implemented earlier and longer closures and stay-at-home orders had decreases in COVID-19 incidence and mortality [5], [6]. In the spring of 2020, the majority of U.S. states implemented mandatory stay-at-home orders [7], which can help reduce activities associated with community spread of COVID-19 — including limiting population movement and close person-to-person contact outside the household. A modeling framework study showed that facemask use by the public, when used in combination with periods of closure, may help in managing the COVID-19 pandemic and re-opening economic activity [8].
The evidence of the positive impact of the community mitigation policies on the burden of COVID-19 is increasing. For instance, several individual state- or county-level investigations have shown the efficacy of mask mandates in reducing COVID-19 transmission [9], [10], [11], [12], [13]. However, no studies have systematically examined the effect of community mitigation measures on rapid increases in COVID-19 incidence across the entire nation. Further, associations have not been examined by urbanicity, which may be of strong interest given the differences in COVID-19 incidence over time by urbanicity [14]. Specifically, although metropolitan counties were strongly affected by the pandemic during the spring and much of the summer of 2020, COVID-19 incidence began rapidly increasing in nonmetropolitan counties, eventually exceeding that of metropolitan areas starting in August; this trajectory continued through much of the fall and winter [1], [15], [16]. In addition, because social vulnerabilities may be higher among less urban areas [17], examining associations between community mitigation policies and COVID-19 incidence by urbanicity might be important in informing public health action, particularly during periods of high COVID-19 incidence.
Since March 8, 2020, CDC has used county-level case counts and standard criteria to identify counties with rapidly increasing COVID-19 incidence, known as rapid riser counties (previously referred to as “hotspot” counties [18]), on a daily basis; rapid riser identification has been used to focus public health efforts in these communities with disproportionately high COVID-19 rates. In this study, we conducted a national analysis of county-level data to examined the probability of being identified as a county with rapidly increasing COVID-19 incidence (rapid riser identification) during the summer of 2020 by implementation of mitigation policies prior to the summer, overall and by urbanicity.
Materials and methods
Daily county-level COVID-19 case counts for all U.S. counties were obtained through USAFacts [19], which compiles data reported by state and local health departments. Rapid riser counties were defined as those that met the following criteria: (1) >100 new cases in the last 7 days, (2) >0% change in the 7-day incidence, (3) a decrease of no more than 60% or an increase in the most recent 3-day COVID-19 incidence over the preceding 3-day incidence, and (4) a 7-day incidence/30-day incidence ratio >0.31. In addition, rapid riser counties met one or both of the following triggering criteria: (1) >60% change in 3-day incidence, or (2) >60% change in 7-day incidence. These standardized criteria were developed through a collaborative process involving multiple federal agencies.
CDC and the University of Nevada, Las Vegas obtained data on statewide closures and mask mandates from state government websites containing executive and administrative orders. The date of the statewide closure was the earlier of either (1) the date that persons were required to stay home or (2) the date that both restaurants were required to cease any on-premises dining and nonessential retail businesses were ordered to close. The date of the statewide reopening was the earlier of either (1) the date the stay-at-home order was lifted or (2) the date that both restaurants were allowed to resume any on-premises dining and nonessential retail businesses were permitted to reopen. The start date of statewide public mask mandate was defined as the date persons operating in a personal capacity were required to wear masks (1) anywhere outside the home or (2) both in retail businesses and in restaurants/food establishments. Each order was analyzed and coded based on the effective start and end date of the mitigation measure. For counties in states with no statewide closure, the assigned date of reference was April 24, 2020 (the date of the first statewide reopening (Alaska [20]). All coding underwent secondary review and quality assurance checks.
Based on the distribution of length of closure and natural breaks in the data, statewide closures were categorized into five groups: 0 days, 1–29 days, 30–50 days, 51–59 days, and >59 days. States that did not close at all were categorized separately because we hypothesized that they may be different from states that closed for any length of time. States were also categorized according to whether a statewide mask mandate was in effect on the reopening date. Urbanicity of counties was based on the National Center for Health Statistics 2013 urban-rural classification scheme [21]. For this analysis, results were presented in three categories: large metropolitan (large central metropolitan and large fringe metropolitan); medium and small metropolitan; and nonmetropolitan (micropolitan and noncore areas).
All U.S. counties were categorized based on statewide closure and mask mandate data. The distribution of counties by length of statewide closures and implementation of mask mandates was described overall and by urbanicity. Comparisons between urbanicity groups were assessed using chi-squared tests or Fisher's exact tests (for comparisons with at least one cell with <5 observations).
Using Poisson regression models with robust standard error estimation, prevalence ratios (PR) with 95% confidence intervals (CI) were calculated to examine associations between implementation of community mitigation policies and identification of a county as a rapid riser one or more times during June 1–September 30, overall and by urbanicity. All associations were adjusted (aPR) for county population size (log population size) since population size was independently associated with rapid riser identification, and thus, might have confounded associations between mitigation strategies and rapid riser identification. All analyses were conducted using SAS (version 9.4; SAS Institute). P-values <.05 were considered statistically significant.
Results
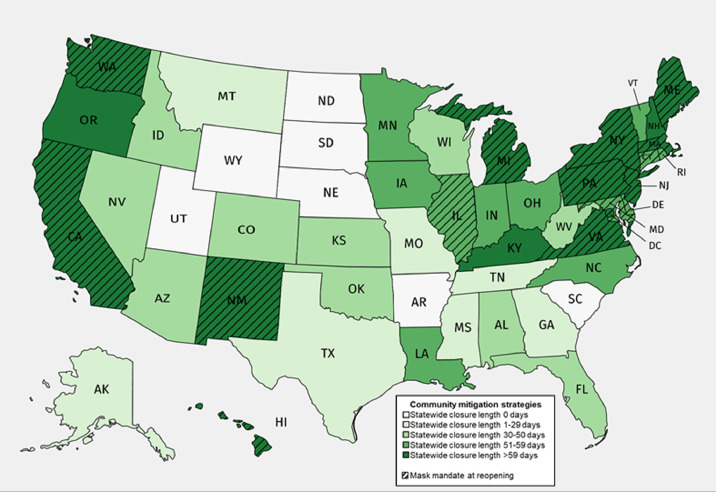
Among all U.S. counties, 2803 (89%) were in states with statewide closure orders. For counties in states that closed, statewide closure lengths ranged from 27 to 116 days; all closures began during March 19–April 7, 2020 (Figure 1 , Table A.1).
Fig. 1.
Length of statewide closures and states with mask mandates in place at reopening United States, March 19September 30, 2020*
*The length of statewide closure was defined as starting on the earlier of either 1) the date persons in all counties were required to stay home or 2) the date both restaurants were required to cease any on-premises dining and nonessential retail businesses were ordered to close in all counties; the earliest date one of these restrictions were lifted for all counties was defined as the statewide reopening. The start date of statewide mask mandate was defined as the date that persons operating in a personal capacity were required to wear masks 1) anywhere outside the home or 2) both in retail businesses and in restaurants/food establishments. (created with mapchart.net)
Overall, 339 counties did not have a statewide closure in place, 280 (83%) of which were nonmetropolitan counties (Table 1). Among 674 (22%) counties in states with statewide mask mandates at reopening, distribution varied significantly by urbanicity: 40% were large metropolitan counties, 26% were medium/small metropolitan counties, and 16% were nonmetropolitan counties. There was substantial overlap between statewide closures and mask mandates. Counties in states with statewide closures of >59 days were more likely to have a statewide mask mandate at reopening (79%) than were those in states closed for 51–59 days (7%), 30–50 days (1%), 1–29 days (0%), and 0 days (0%).
Table 1.
Distribution of community mitigation measures in all U.S. counties (n=3142), overall and by urbanicity — United States, March 19–September 30, 2020.
| No. (column%) |
|||||
|---|---|---|---|---|---|
| Mitigation measures | All counties | Large metropolitan counties | Medium and small metropolitan counties | Nonmetropolitan counties | P-value† |
| Overall | 3142 | 436 | 730 | 1976 | — |
| U.S. population represented, n (row%) | 328,239,523 | 183,480,600 (56) | 98,695,862 (30) | 46,063,061 (14) | — |
| Length of closure, days | <0.0001 | ||||
| 0 days of closure | 339 (10.8) | 3 (0.7) | 56 (7.7) | 280 (14.2) | |
| 1–29 days of closure | 836 (26.6) | 105 (24.1) | 178 (24.4) | 553 (28.0) | |
| 30–50 days of closure | 687 (21.9) | 61 (14.0) | 163 (22.3) | 463 (23.4) | |
| 51–59 days of closure | 480 (15.3) | 94 (21.6) | 128 (17.5) | 258 (13.1) | |
| >59 days of closure | 800 (25.5) | 173 (39.7) | 205 (28.1) | 422 (21.4) | |
| Mask mandate at reopening* | <0.0001 | ||||
| Yes | 674 (21.5) | 174 (39.9) | 187 (25.6) | 313 (15.8) | |
| No | 2468 (78.5) | 262 (60.1) | 543 (74.4) | 1663 (84.2) | |
| Mask mandate by length of closure* | |||||
| 0 days of closure | |||||
| Mask mandate | 0 | 0 | 0 | 0 | — |
| No mask mandate | 339 (100) | 3 (100) | 56 (100) | 280 (100) | |
| 1–29 days of closure | |||||
| Mask mandate | 0 | 0 | 0 | 0 | — |
| No mask mandate | 836 (100) | 105 (100) | 178 (100) | 553 (100) | |
| 30–50 days of closure | |||||
| Mask mandate | 5 (0.7) | 5 (8.2) | 0 | 0 | <0.0001 |
| No mask mandate | 682 (99.3) | 56 (91.8) | 163 (100.0) | 463 (100.0) | |
| 51–59 days of closure | |||||
| Mask mandate | 35 (7.3) | 17 (18.1) | 12 (9.4) | 6 (2.3) | <0.0001 |
| No mask mandate | 445 (92.7) | 77 (81.9) | 116 (90.6) | 252 (97.7) | |
| >59 days of closure | |||||
| Mask mandate | 634 (79.3) | 152 (87.9) | 175 (85.4) | 307 (72.7) | <0.0001 |
| No mask mandate | 166 (20.8) | 21 (12.1) | 30 (14.6) | 115 (27.3) | |
For counties in states that did not close, a reference date of April 24, 2020 was used.
P-value < .05 were considered statistically significant based on results from chi-squared tests or Fisher's exact tests (for comparisons with at least one cell with <5 observations).
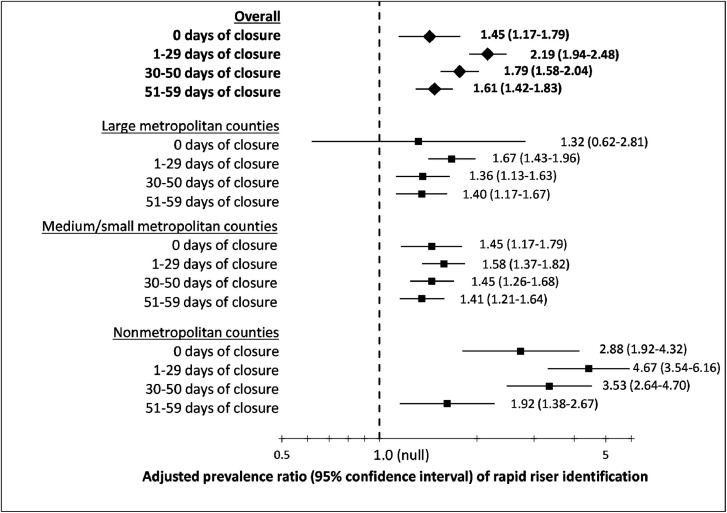
During June 1–September 30, 1112 (35%) counties were identified as rapid risers. After adjustment for county population size, counties in states that closed between 0 and 59 days were more likely to become rapid riser counties compared with those that closed for >59 days (0 days: adjusted prevalence ratio [aPR] = 1.45, 95% confidence interval [CI] = 1.17–1.79; 1–29 days: aPR = 2.19, 95% CI = 1.94–2.48; 30–50 days: aPR = 1.79, 95% CI = 1.58–2.04; 51–59 days: aPR = 1.61, 95% CI = 1.42–1.83) (Figure 2 , Table A.2). These associations were more pronounced in nonmetropolitan counties (0 days: aPR = 2.88, 95% CI = 1.92–4.32; 1–29 days: aPR = 4.67, 95% CI = 3.54–6.16; 30–50 days: aPR = 3.53, 95% CI = 2.64–4.70; 51–59 days: aPR = 1.92, 95% CI = 1.38–2.67).
Fig. 2.
Adjusted^ prevalence ratios and 95% confidence intervals comparing rapid riser* identification during June 1–September 30, 2020 by length of statewide closure (days)+, stratified by urbanicity.
Figure 2 Footnotes: ^Adjusted for population size; * Rapid riser counties were defined as those that met the following criteria: 1) >100 new cases in the last 7 days, 2) >0% change in the 7-day incidence, 3) a decrease of no more than 60% or an increase in the most recent 3-day COVID-19 incidence over the preceding 3-day incidence, and 4) a 7-day incidence/30-day incidence ratio >0.31. In addition, rapid riser counties met one or both of the following triggering criteria: 1) >60% change in 3-day incidence, or 2) >60% change in 7-day incidence. +Each statewide closure length category compared to reference category of statewide closure >59 days.
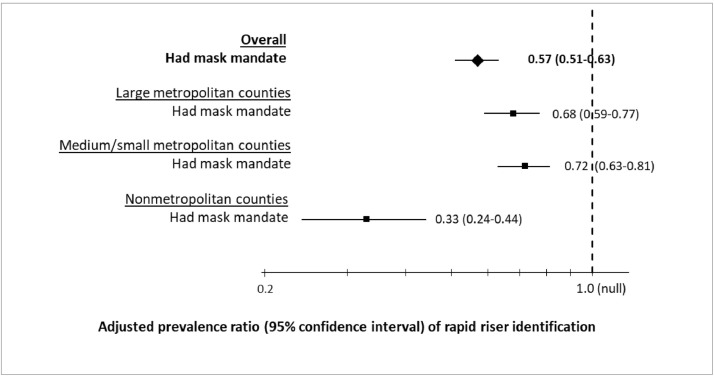
The probability of a county becoming a rapid riser during the summer months was 43% lower among counties in states with statewide mask mandates at reopening (aPR = 0.57; 95% CI = 0.51–0.63); this association was more pronounced in nonmetropolitan areas (aPR = 0.33, 95% CI = 0.24–0.44) (Figure 3 , Table A.2).
Fig. 3.
Adjusted^ prevalence ratios and 95% confidence intervals comparing rapid riser* identification during June 1–September 30, 2020 by statewide mask mandate upon statewide reopening, stratified by urbanicity.
Figure 3 Footnotes: ^Adjusted for population size. *Rapid riser counties were defined as those that met the following criteria: (1) >100 new cases in the last 7 days, (2) >0% change in the 7-day incidence, (3) a decrease of no more than 60% or an increase in the most recent 3-day COVID-19 incidence over the preceding 3-day incidence, and (4) a 7-day incidence/30-day incidence ratio >0.31. In addition, rapid riser counties met one or both of the following triggering criteria: (1) >60% change in 3-day incidence, or (2) >60% change in 7-day incidence.
Discussion
After adjustment for county population size, counties in states with lack of, or shorter, closure periods or without statewide mask mandates at reopening were more likely to experience sharp increases in COVID-19 incidence during June 1–September 30, 2020. These findings are consistent with other studies that have demonstrated the effect of community mitigation policies in reducing the spread of COVID-19 [9], [11], [12], [22], [23]. In addition, this analysis demonstrated that longer statewide closures and mask mandates might have had an even greater impact on slowing the acceleration of COVID-19 incidence in nonmetropolitan counties.
Among all 3142 U.S. counties, 89% were in states with statewide closures; 22% were in states with statewide mask mandates at reopening. Differences in the distribution of community mitigation policies by urbanicity could reflect a higher COVID-19 incidence in large metropolitan areas during the spring of 2020 that necessitated mitigation measures. With lower COVID-19 incidence among nonmetropolitan areas before the summer [1], increased incidence in these areas during the summer could be attributed to lack of community mitigation strategies, such as stay-at-home orders, closing restaurants and nonessential businesses, and mask mandates.
Differences in associations between community mitigation policies and rapid riser identification by urbanicity might also reflect variability in awareness of and adherence to mitigation policies. Previous studies have shown differences in mask-wearing behavior and other mitigation behaviors by gender, age, ethnicity, and urbanicity [24], [25], [26], [27]. Further, inherent differences in structural and social factors of counties could have influenced both statewide mitigation policies and individual behavior, and thus, may also have contributed to differences in observed associations by urbanicity [17], [28].
Counties in states with statewide closure periods >59 days had a significantly lower probability of rapid riser identification when adjusted by county population size, particularly in nonmetropolitan areas. By limiting population movement, statewide closures can be an important strategy to reduce COVID-19 transmission in areas with high incidence [7], [8]. In addition, there was a 43% reduction in the probability of becoming a rapid riser county among counties in states with a statewide mask mandate at reopening; associations between mask mandates and rapid riser identification differed by urbanicity, with the strongest association observed in nonmetropolitan areas. Mask mandates can play a critical role in preventing COVID-19 and could be especially important for persons who are required to work in-person, including essential workers and those working in crowded conditions, particularly in nonmetropolitan areas. Although it was not possible to ascertain the individual contribution of each mitigation strategy in reducing the probability of rapid riser identification, combining multiple mitigation strategies is recommended to reduce transmission [4], [29].
Associations between statewide mitigation policies and rapid riser identification were confounded by county population size. Confounding may have been, in part, due to the fact that larger counties may have been more substantially affected by COVID-19 during the summer. In addition, one of the criteria of the rapid riser definition was that counties had to have >100 new cases in the last 7 days, which might decrease the likelihood that small counties (specifically those with <20,000 population) would meet the definition. However, in a sensitivity analysis, even restricting the dataset to counties with ≥20,000 population yielded similar findings to the adjusted estimates presented in this study.
The findings in this report are subject to several limitations. First, policy data were limited to mandatory statewide mitigation measures; therefore, data did not account for county-specific variability or nonmandatory recommendations [30]. For example, some states issued orders that applied to certain counties, and others authorized counties to receive variances if certain thresholds are met (e.g., low COVID-19 test percent positivity). Second, heterogeneity in implementing mandatory mitigation measures were not incorporated in this study; thus, some states not meeting the definition of a closure state may have still implemented some mitigation measures. Further, this study could not assess motivations for implementation of community mitigation policies; states may have chosen not to implement policies despite high incidence, or because of lower baseline incidence [31]. Future studies assessing temporal associations between implementation of mitigation strategies and changes in COVID-19 incidence could account for factors (e.g., baseline incidence) that may have influenced decisions around community mitigation policies. Also, because of natural variations in national COVID-19 incidence and a wide range of reopening dates over time, rapid riser identification was examined based on a fixed period (summer months) and not on time since reopening; therefore, some states may have reopened during the rapid riser identification period. Examining the identification of rapid riser counties during summer, however, was important to assess the potential effect of mitigation measures implemented in the spring. Finally, universal compliance with mandatory statewide mitigation measures was not likely [28]. Although statewide mandates may not be consistently applied or complied with throughout an entire state, several studies have shown that governmental mitigation mandates, even at a national level, can have an impact on COVID-19 morbidity and mortality [5], [6], [29]. In addition, statewide mitigation mandates may be important from the standpoint of signaling and communicating a consistent and cohesive statewide policy and public health message as well as expected behaviors and social norms within a state.
Conclusions
Statewide closures and mask mandates might have reduced COVID-19 transmission during June 1–September 30. These results underscore the value of community mitigation strategies in limiting the spread of COVID-19, especially in nonmetropolitan areas, and particularly with continued high COVID-19 incidence and increased transmission risk associated with the B.1.1.7 variant [1], [3], [32]. Federal, state, and local partners should work together to monitor COVID-19 incidence and establish a threshold for implementing closures and mask mandates, if needed, to prevent increases in COVID-19 incidence.
Acknowledgments
Margaret Honein, Joanna Prasher, Henry Baggett, Angela Werner, Robert Daniels, Lee Warner, CDC COVID-19 Response Team; Timmy Pierce, Nicholas Skaff, CDC National Center for Environment Health; Matthew Penn, CDC Public Health Law Program.
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflicts of interest were disclosed.
This activity was reviewed by the Centers for Disease Control and Prevention and was conducted consistent with applicable federal law and CDC policy (45 C.F.R. part 46, 21 C.F.R. part 56; 42 U.S.C. §241(d); 5 U.S.C. §552a; 44 U.S.C. §3501 et seq.).
The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention/the Agency for Toxic Substances and Disease Registry.
Footnotes
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Appendix
Table A.1.
Statewide closure, reopening, and mask mandate effective dates — United States, March 19–September 30, 2020.
| State | Date of Statewide Closure* | Date of Statewide Reopening† | Number of days between statewide closure and statewide reopening | Date of Statewide Mask Mandate‡ |
|---|---|---|---|---|
| Alabama | 3/28/2020 | 4/30/2020 | 33 | 7/16/2020 |
| Alaska | 3/28/2020 | 4/24/2020 | 27 | NA |
| Arizona | 3/31/2020 | 5/16/2020 | 46 | NA |
| Arkansas | NA | NA | 0 | 7/20/2020 |
| California | 3/19/2020 | 7/13/2020 | 116 | 6/18/2020§ |
| Colorado | 3/26/2020 | 4/27/2020 | 32 | 7/16/2020 |
| Connecticut | 3/22/2020 | 5/20/2020 | 59 | 4/20/2020§ |
| Delaware | 3/24/2020 | 5/22/2020 | 59 | 4/28/2020§ |
| District of Columbia | 3/25/2020 | 5/29/2020 | 65 | 5/16/2020§ |
| Florida | 4/3/2020 | 5/4/2020 | 31 | NA |
| Georgia | 4/3/2020 | 4/30/2020 | 27 | NA |
| Hawaii | 3/25/2020 | 6/10/2020 | 77 | 4/17/2020§ |
| Idaho | 3/25/2020 | 5/1/2020 | 37 | NA |
| Illinois | 3/21/2020 | 5/29/2020 | 69 | 5/1/2020§ |
| Indiana | 3/24/2020 | 5/18/2020 | 55 | 7/27/2020 |
| Iowa | 3/26/2020 | 5/15/2020 | 50 | NA |
| Kansas | 3/30/2020 | 5/4/2020 | 35 | 7/3/2020 |
| Kentucky | 3/23/2020 | 5/22/2020 | 60 | 7/10/2020 |
| Louisiana | 3/23/2020 | 5/15/2020 | 53 | 7/13/2020 |
| Maine | 3/25/2020 | 5/31/2020 | 67 | 5/1/2020§ |
| Maryland | 3/23/2020 | 5/13/2020 | 51 | 4/18/2020§ |
| Massachusetts | 3/24/2020 | 6/8/2020 | 76 | 5/6/2020§ |
| Michigan | 3/24/2020 | 6/1/2020 | 69 | 4/26/2020§ |
| Minnesota | 3/27/2020 | 5/17/2020 | 51 | 7/24/2020 |
| Mississippi | 3/31/2020 | 4/27/2020 | 27 | 8/5/2020 |
| Missouri | 4/6/2020 | 5/4/2020 | 28 | NA |
| Montana | 3/28/2020 | 4/26/2020 | 29 | 7/15/2020 |
| Nebraska | NA | NA | 0 | NA |
| Nevada | 3/20/2020 | 5/9/2020 | 50 | 6/24/2020 |
| New Hampshire | 3/27/2020 | 6/16/2020 | 81 | NA |
| New Jersey | 3/21/2020 | 6/9/2020 | 80 | 4/10/2020§ |
| New Mexico | 3/24/2020 | 6/1/2020 | 69 | 6/1/2020§ |
| New York | 3/19/2020 | 6/6/2020 | 79 | 4/17/2020§ |
| North Carolina | 3/30/2020 | 5/22/2020 | 53 | 6/26/2020 |
| North Dakota | NA | NA | 0 | NA |
| Ohio | 3/23/2020 | 5/15/2020 | 53 | 7/23/2020 |
| Oklahoma | 3/25/2020 | 5/1/2020 | 37 | NA |
| Oregon | 3/23/2020 | 6/19/2020 | 88 | 7/1/2020 |
| Pennsylvania | 3/19/2020 | 6/5/2020 | 78 | 4/19/2020§ |
| Rhode Island | 3/28/2020 | 5/9/2020 | 42 | 5/8/2020§ |
| South Carolina | 4/7/2020 | 5/4/2020 | 27 | NA |
| South Dakota | NA | NA | 0 | NA |
| Tennessee | 3/31/2020 | 4/29/2020 | 29 | NA |
| Texas | 4/2/2020 | 5/1/2020 | 29 | 7/3/2020 |
| Utah | NA | NA | 0 | NA |
| Vermont | 3/24/2020 | 5/15/2020 | 52 | 8/1/2020 |
| Virginia | 3/30/2020 | 5/29/2020 | 60 | 5/29/2020§ |
| Washington | 3/23/2020 | 7/3/2020 | 102 | 6/26/2020§ |
| West Virginia | 3/24/2020 | 5/4/2020 | 41 | 7/7/2020 |
| Wisconsin | 3/25/2020 | 5/13/2020 | 49 | 8/1/2020 |
| Wyoming | NA | NA | 0 | NA |
Abbreviation: NA = No applicable statewide closure or mask mandate during the study period
The date of the statewide closure was the earlier of either 1) the date persons were required to stay home or 2) the date both restaurants were required to cease any on-premises dining and nonessential retail businesses were ordered to close.
The date of the statewide reopening was the earlier of either 1) the date the stay-at-home order was lifted or 2) the date both restaurants were allowed to resume any on-premises consumption and nonessential retail businesses were permitted to reopen.
The start date of statewide public mask mandate was defined as the date that persons operating in a personal capacity were required to wear masks 1) anywhere outside the home or 2) both in retail businesses and in restaurants/food establishments.
Indicates a statewide mask mandate that was implemented on or before the statewide reopening.
Table A.2.
Associations* between community mitigation measures and rapid riser counties identification, overall and by urbanicity (n = 3142 U.S. counties) — United States, June 1–September 30, 2020.
| Urbanicity category | Characteristics | Length of closure (days) |
Mask mandate at reopening |
||||||
|---|---|---|---|---|---|---|---|---|---|
| 0 | 1–29 | 30–50 | 51–59 | >59 | Yes | No | |||
| All | Total, No. | 3,142 (100) | 339 | 836 | 687 | 480 | 800 | 674 | 2,468 |
| Rapid riser (% of total) | 1,112 (35.4) | 59 (17.4) | 351 (42.0) | 258 (37.6) | 201 (41.9) | 243 (30.4) | 240 (35.6) | 872 (35.3) | |
| aPR† (95% CI)P-value | 1.45 (1.17 - 1.79)0.0005 | 2.19 (1.94 - 2.48)<0.0001 | 1.79 (1.58 - 2.04)<0.0001 | 1.61 (1.42 - 1.83)<0.0001 | Ref | 0.57 (0.51–0.63)<0.0001 | Ref | ||
| Large metropolitan |
Total, No. (%) | 436 (13.9) | 3 | 105 | 61 | 94 | 173 | 174 | 262 |
| Rapid riser (% of total) | 277 (63.5) | 2 (66.7) | 78 (74.3) | 44 (72.1) | 60 (63.8) | 93 (53.8) | 98 (56.3) | 179 (68.3) | |
| aPR† (95% CI)P-value | 1.32 (0.62 - 2.81)0.4719 | 1.67 (1.43 - 1.96)<0.0001 | 1.36 (1.13 - 1.63) | 1.40 (1.17 - 1.67)0.0002 | Ref | 0.68 (0.59–0.77)<0.0001 | Ref | ||
| Medium/small metropolitan |
Total, No. (%) | 730 (23.2) | 56 | 178 | 163 | 128 | 205 | 187 | 543 |
| Rapid riser (% of total) | 431 (59.0) | 30 (53.6) | 108 (60.7) | 108 (66.3) | 82 (64.1) | 103 (50.2) | 103 (55.1) | 328 (60.4) | |
| aPR† (95% CI)P-value | 1.45 (1.17 - 1.79)0.0006 | 1.58 (1.37 - 1.82)<0.0001 | 1.45 (1.26 - 1.68)<0.0001 | 1.41 (1.21 - 1.64)<0.0001 | Ref | 0.72 (0.63–0.81)<0.0001 | Ref | ||
| Nonmetropolitan | Total, No. (%) | 1,976 (62.9) | 280 | 553 | 463 | 258 | 422 | 313 | 1663 |
| Rapid riser (% of total) | 404 (20.4) | 27 (9.6) | 165 (29.8) | 106 (22.9) | 59 (22.9) | 47 (11.1) | 39 (12.5) | 365 (21.9) | |
| aPR† (95% CI)P-value | 2.88 (1.92 - 4.32)<0.0001 | 4.67 (3.54 - 6.16)<0.0001 | 3.53 (2.64 - 4.70)<0.0001 | 1.92 (1.38 - 2.67) | Ref | 0.33 (0.24–0.44)<0.0001 | Ref | ||
* Associations adjusted for county population size
§ P-value< .05 determined statistical significance
aPR = adjusted prevalence ratio; CI = confidence interval
References
- 1.COVID data tracker. Centers for Disease Control and Prevention. https://covid.cdc.gov/covid-data-tracker/#datatracker-home. [Accessed 4 March 2021].
- 2.U.S. COVID-19 cases caused by variants. [Accessed 4 March 2021].
- 3.Public Health England. Investigation of novel SARS-COV-2 variant: variant of concern 202012/01. London, United Kingdom: Public Health England; 2020. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/947048/Technical_Briefing_VOC_SH_NJL2_SH2.pdf
- 4.Community mitigation framework: Implementation of mitigation strategies for communities with local COVID-19 transmission. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/community/community-mitigation.html. [Accessed 5 March 2021].
- 5.Alfano V., Ercolano S. The efficacy of lockdown against COVID-19: a cross-country panel analysis. Appl Health Econ Health Policy. 2020;18(4):509–517. doi: 10.1007/s40258-020-00596-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fuller J.A., Hakim A., Victory K.R., Date K., Lynch M., Dahl B., et al. Mitigation policies and COVID-19-associated mortality - 37 European Countries, January 23-June 30, 2020. MMWR Morb Mortal Wkly Rep. 2021;70(2):58–62. doi: 10.15585/mmwr.mm7002e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moreland A., Herlihy C., Tynan M.A., Sunshine G., McCord R.F., Hilton C., et al. Timing of state and territorial COVID-19 stay-at-home orders and changes in population movement - United States, March 1-May 31, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(35):1198–1203. doi: 10.15585/mmwr.mm6935a2. March 1-May 31, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stutt R., Retkute R., Bradley M., Gilligan C.A., Colvin J. A modelling framework to assess the likely effectiveness of facemasks in combination with ‘lock-down’ in managing the COVID-19 pandemic. Proc R Soc A. 2020;476(2238) doi: 10.1098/rspa.2020.0376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kanu F.A., Smith E.E., Offutt-Powell T., Hong R., Delaware Case I., Contact Tracing T., et al. Declines in SARS-CoV-2 transmission, hospitalizations, and mortality after implementation of mitigation measures - Delaware, March-June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(45):1691–1694. doi: 10.15585/mmwr.mm6945e1. March-June 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lasry A., Kidder D., Hast M., Poovey J., Sunshine G., Winglee K., et al. Timing of community mitigation and changes in reported COVID-19 and community mobility - Four U.S. metropolitan areas, February 26-April 1, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(15):451–457. doi: 10.15585/mmwr.mm6915e2. February 26-April 1, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Padalabalanarayanan S., Hanumanthu V.S., Sen B. Association of state stay-at-home orders and state-level African American population with COVID-19 case rates. JAMA Network Open. 2020;3(10) doi: 10.1001/jamanetworkopen.2020.26010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Van Dyke M.E., Rogers T.M., Pevzner E., Satterwhite C.L., Shah H.B., Beckman W.J., et al. Trends in county-level COVID-19 incidence in counties with and without a mask mandate - Kansas, June 1-August 23, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(47):1777–1781. doi: 10.15585/mmwr.mm6947e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Joo H., Miller G., Sunshine G., Gakh M., Pike J., Havers M.P., et al. Decline in COVID-19 hospitalization growth rates associated with statewide mask mandates — 10 States, March–October 2020. MMWR Morb Mortal Wkly Rep. 2021;70:212–216. doi: 10.15585/mmwr.mm7006e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Paul R., Arif A.A., Adeyemi O., Ghosh S., Han D. Progression of COVID-19 from urban to rural areas in the United States: a spatiotemporal analysis of prevalence rates. J Rural Health. 2020;36(4):591–601. doi: 10.1111/jrh.12486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oster A.M., Caruso E., DeVies J., Hartnett K.P., Boehmer T.K. Transmission dynamics by age group in COVID-19 hotspot counties - United States, April-September 2020. MMWR Morb Mortal Wkly Rep. 2020;69(41):1494–1496. doi: 10.15585/mmwr.mm6941e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.COVID-19 Stats: COVID-19 Incidence, by Urban-Rural Classification - United States, January 22-October 31, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(46):1753. doi: 10.15585/mmwr.mm6946a6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dasgupta S., Bowen V.B., Leidner A., Fletcher K., Musial T., Rose C., et al. Association between social vulnerability and a county’s risk for becoming a COVID-19 hotspot - United States, June 1-July 25, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(42):1535–1541. doi: 10.15585/mmwr.mm6942a3. June 1-July 25, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oster A.M., Kang G.J., Cha A.E., Beresovsky V., Rose C.E., Rainisch G., et al. Trends in number and distribution of COVID-19 hotspot counties - United States, March 8-July 15, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(33):1127–1132. doi: 10.15585/mmwr.mm6933e2. March 8-July 15, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.USAFacts. Coronavirus stats & data. https://usafacts.org/issues/coronavirus. [Accessed 18 February 2021].
- 20.State of Alaska. Health mandate 016 – reopen Alaska responsibly PLAN- PHASE I-A 2020. https://covid19.alaska.gov/wp-content/uploads/2020/05/Mandate-016-and-Attachments-D-through-T.pdf. [Accessed 18 February 2021].
- 21.Ingram D.D., Franco S.J. 2013 NCHS urban-rural classification scheme for counties. Vital Health Stat. 2014;2(166):1–73. [PubMed] [Google Scholar]
- 22.Gallaway M.S., Rigler J., Robinson S., Herrick K., Livar E., Komatsu K.K., et al. Trends in COVID-19 incidence after implementation of mitigation measures - Arizona, January 22-August 7, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(40):1460–1463. doi: 10.15585/mmwr.mm6940e3. January 22-August 7, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lyu W., Wehby G.L. Community use of face masks And COVID-19: evidence from a natural experiment of state mandates in the US. Health Aff. 2020;39(8):1419–1425. doi: 10.1377/hlthaff.2020.00818. [DOI] [PubMed] [Google Scholar]
- 24.Haischer M.H., Beilfuss R., Hart M.R., Opielinski L., Wrucke D., Zirgaitis G., et al. Who is wearing a mask? Gender-, age-, and location-related differences during the COVID-19 pandemic. PLoS ONE. 2020;15(10) doi: 10.1371/journal.pone.0240785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Prichard E.C., Christman S.D. Authoritarianism, conspiracy beliefs, gender and COVID-19: links between individual differences and concern about COVID-19, mask wearing behaviors, and the tendency to blame China for the virus. Front Psychol. 2020;11 doi: 10.3389/fpsyg.2020.597671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hearne B.N., Nino M.D. Understanding how race, ethnicity, and gender shape mask-wearing adherence during the COVID-19 pandemic: evidence from the COVID impact survey. J Racial Ethn Health Disparities. 2021 doi: 10.1007/s40615-020-00941-1. online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hutchins H.J., Wolff B., Leeb R., Ko J.Y., Odom E., Willey J., et al. COVID-19 mitigation behaviors by age group - United States, April-June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(43):1584–1590. doi: 10.15585/mmwr.mm6943e4. April-June 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Papageorge N.W., Zahn M.V., Belot M., van den Broek-Altenburg E., Choi S., Jameson J.C., et al. Socio-demographic factors associated with self-protecting behavior during the COVID-19 pandemic. J Popul Econ. 2021;34:691–738. doi: 10.1007/s00148-020-00818-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Haug N., Geyrhofer L., Londei A., Dervic E., Desvars-Larrive A., Loreto V., et al. Ranking the effectiveness of worldwide COVID-19 government interventions. Nat Hum Behav. 2020;4(12):1303–1312. doi: 10.1038/s41562-020-01009-0. [DOI] [PubMed] [Google Scholar]
- 30.Ebrahim S., Ashworth H., Noah C., Kadambi A., Toumi A., Chhatwal J. Reduction of COVID-19 incidence and nonpharmacologic interventions: analysis using a US county-level policy data set. J Med Internet Res. 2020;22(12):e24614. doi: 10.2196/24614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Adolph C., Amano K., Bang-Jensen B., Fullman N., Wilkerson J. Pandemic politics: timing state-level social distancing responses to COVID-19. J Health Polit Policy Law. 2021;46(2):211–233. doi: 10.1215/03616878-8802162. [DOI] [PubMed] [Google Scholar]
- 32.Galloway S.E., Paul P., MacCannell D.R., Johansson M.A., Brooks J.T., MacNeil A, et al. Emergence of SARS-CoV-2 B.1.1.7 lineage — United States, December 29, 2020–January 12, 2021. MMWR Morb Mortal Wkly Rep. 2021;70:95–99. doi: 10.15585/mmwr.mm7003e2. [DOI] [PMC free article] [PubMed] [Google Scholar]