ABSTRACT
Background:
Hip prostheses are generally avoided in elderly patients because of cognitive decline and/or reduced muscle strength. The present report describes the case of an elderly woman who regained gait using a prosthesis prescribed during the early postoperative phase following hip disarticulation.
Case:
A 78-year-old woman suffered from a pathological fracture caused by liposarcoma of the left thigh. Before hospitalization, the patient was fully independent in her activities of daily living, including gait. The right and left handgrip strengths were 12.9 and 14.2 kg, respectively, and the patient had no signs of cognitive decline. Radical treatment involving hip disarticulation was scheduled. Before surgery, the possibility of fitting a hip prothesis that would allow the patient to walk was discussed, to which she consented. On postoperative day 23, the patient was fitted with a hip prosthesis and began gait training. On day 31, she was able to walk using a fixed walker and, eventually, using a crutch.
Discussion:
The present case demonstrated the successful reacquisition of gait using a hip prothesis prescribed during the early postoperative phase after amputation, suggesting that the applicability of hip prostheses may be widely considered even for elderly patients.
Keywords: elderly, hip disarticulation, prosthesis
INTRODUCTION
Regaining gait is a major target of rehabilitative treatments for patients who undergo lower-extremity amputation. For such patients, a prosthesis has generally been prescribed for regaining gait. Previous studies have indicated that among elderly patients who had undergone lower-leg amputation, only 34%–47.2% were able to regain gait. However, such numbers dropped to 9%–20% among those who had undergone thigh amputation,1,2,3) possibly because prostheses for those undergoing thigh amputation have to be made to individual specifications. Moreover, such prostheses require sufficient muscle strength in the non-amputated lower extremity and skills for controlling the knee joint.
Hip disarticulation is one of the most invasive surgical procedures for lower-extremity amputation. Compared with thigh and lower-leg amputation, a considerably smaller number of individuals undergo hip disarticulation, partially because of the causative diseases.4,5) The major causative disease for thigh and lower-leg amputation among elderly individuals, both of which procedures are prevalent in most advanced countries, was found to be arteriosclerosis obliterans.1) However, more recent case reports on hip disarticulation have indicated that the majority of patients who undergo hip disarticulation suffer rare malignant tumors.4) Unfortunately, only a limited number of studies have focused on regaining gait after hip disarticulation.
A prosthesis for hip disarticulation consists of a complex structure that includes a hip socket, hip joint, thigh pylon, knee joint, lower-leg pylon, and foot parts. Rehabilitative training for gait using such a prosthesis is challenging and is dependent on residual physical and cognitive functions. Consequently, the application of prostheses in real-world clinical settings is not widely accepted for elderly individuals who undergo hip disarticulation. Nonetheless, here we present the case of a 78-year-old woman who underwent hip disarticulation surgery and successfully regained gait using a hip prosthesis fitted during the early postoperative phase.
CASE REPORT
A 78-year-old woman, who underwent a major resection of a left femoral liposarcoma and chemotherapy at our hospital 8 years ago, developed a athological fracture due to tumor invasion into her femur. Before the fracture, the patient was fully independent in her activities of daily living (ADL), was capable of walking without a cane, and could manage household chores, including shopping. She did not engage in any sporting activities, such as tennis, swimming, and/or jogging, implying that she possessed typical physical fitness for her age group. The patient was 1.44 m tall, weighed 48.3 kg, and presented with comorbidities including idiopathic thrombocytopenic purpura (for which she was taking 5 mg of prednisolone) and hypothyroidism. Informed consent for inclusion in this case report was obtained from the patient in writing.
Hip disarticulation was chosen as a radical treatment because major blood vessels and nerves, such as the femoral artery, femoral nerve, and sciatic nerve, were involved in the tumor. Rehabilitative treatment was started 5 days before the surgery. Initial evaluations for rehabilitative treatment included the following: the range of motion was full in both upper and right lower extremities; the manual muscle test result was 4 in the right lower extremity; and the grip strengths were 12.9 and 14.2 kg for the right and left hands. Respiratory function was normal, with a vital capacity of 99.5% of the predicted value and a forced expiratory volume in 1 s/forced vital capacity ratio of 79.8%. Echocardiography findings were within normal limits. Cognitive function was screened using the Mini-Mental State Examination (MMSE) and Hasegawa Dementia Scale-Revised (HDS-R). Scores for both cognitive function tests suggested no signs of cognitive decline. The patient had a total Functional Independence Measure (FIM) score of 66 points, with the motor and cognitive components being 31 and 35 points, respectively. The patient underwent muscle strengthening training of the unaffected right lower extremity and upper extremities before surgery while ensuring that bed rest prior to surgery was not compromised.
Considering the patient’s normal cognitive function and maintained muscle strength in the unaffected extremities, medical staff, including orthopedic surgeons and physiatrists, discussed with the patient the prescription of a prosthesis aimed at recovering gait. Given the patient’s strong motivation to recover gait, she subsequently consented to the prescription of a prosthesis and rehabilitative training.
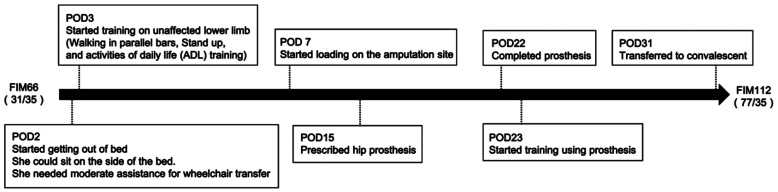
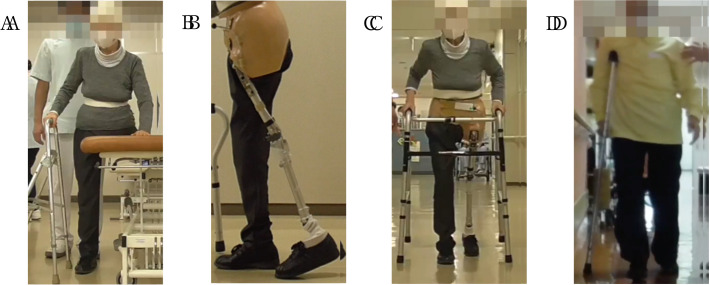
Figure 1 schematically illustrates the patient’s clinical course. During the postoperative period, the patient underwent muscle strength training for the upper and lower extremities at our acute care hospital. On postoperative day (POD) 2, the patient started getting out of bed and could sit on the side of the bed. On POD 3, training of the unaffected lower limb, including standing up and ADLs, was started. It is worthy of note that the patient was eventually able to walk between parallel bars with the healthy lower extremity at this point. By POD 7, the patient was able to load the amputation site (Fig. 2A). No abnormalities in the surgical wound were noted, indicating an uneventful healing process. A hip prosthesis (Fig. 2B), consisting of a Canadian socket, a modular single-centered hip with extension assistance, modular single axis knee joint with lock and extension assist, and energy-storage foot parts, was prescribed on POD 15. On POD 23, the hip prosthesis was fitted and gait training was initiated. On transferring to a convalescent rehabilitation hospital on POD 31, the patient was able to walk continuously for 60 m with a fixed walker (Fig. 2C). Her total FIM score increased to 108 points, with the motor and cognitive components being 78 and 35 points, respectively (Fig. 1).
Fig. 1.
Schematic of the patient’s clinical course. FIM, functional independence measure; POD, postoperative day. FIM scores are presented as motor/cognition subscales.
Fig. 2.
(A) Image obtained on postoperative day (POD) 7. The patient was able to load the amputation site. This meant that even before the prosthetic leg was made, the patient was able to train in a walking style to generate an awareness of walking with a prosthetic leg. (B) Image of the hip prosthesis. (C) Image obtained on POD 30. The patient was able to walk with a fixed walker. (D) Image obtained at discharge from the convalescent rehabilitation hospital. The patient was able to walk with a single crutch.
On discharge from the convalescent rehabilitation hospital, the patient was able to walk using a single crutch and could walk up and down stairs (Fig. 2D). Thereafter, the patient could successfully use her prosthesis daily, wearing it for approximate 3 h a day for walking on sidewalks and prolonged standing in the kitchen.
DISCUSSION
The present report describes the case of an elderly woman who was able to regain gait using a prosthesis prescribed during the early postoperative phase following hip disarticulation for radical cure of a neoplastic lesion. Prior to hospitalization, the patient was fully independent in ADLs and maintained good muscle strength in the healthy lower extremity and bilateral upper extremities. No evidence of cognitive decline was observed, and the patient was highly motivated to walk despite the scheduled amputation. The wound healing process was uneventful, and this subsequently facilitated the fitting of the hip prosthesis during the early postoperative phase. To the best of our knowledge, this is the first report of a case involving an elderly patient who regained gait using a hip prosthesis prescribed during the early postoperative phrase.
Cognitive impairment can negatively impact successful prosthesis use in elderly patients after lower-extremity amputation. In particular, dementia has been identified as a significant predictor of prosthesis utilization.6) Therefore, cognitive function assessment is critical for elderly patients scheduled for lower-extremity amputation. In the current case, the scores for the MMSE, HDS-R, and the cognitive FIM component were impeccable. After admission to our acute hospital, the patient was able to appropriately respond to various consent forms for medical treatment. Moreover, she consented to the prescription of a hip prosthesis aimed at regaining gait, which highly motivated her to undergo training after the amputation. Based on the screening test scores and clinical observations, we determined that the patient had sufficient cognitive function to use a hip prothesis. Although the patient’s cognitive level was well-preserved, we chose a fixed knee joint for simplicity of motor control and to take account of the predicted postoperative levels of daily activity considering her age, which is important for successful training.
In the current case, the hip prothesis was applied 3 weeks after surgery, and the prosthesis was fitted on day 23. Scheduling the prescription of a prosthesis at a later phase may have allowed the development of muscle atrophy in the unaffected extremities, at which point gait training using a hip prosthesis may no longer have been indicated. Previous studies have reported that patients generally received a hip prosthesis 3.3–7 months following surgery,5,7) with the earliest case being 7 weeks after surgery. However, the current patient was fitted with a hip prosthesis and started gait training at a much earlier period, which may have promoted a better outcome by avoiding muscle atrophy in the unaffected lower and upper extremities, which are critically important for gait training.
One factor for the successful early fitting of the prosthesis was the uneventful wound-healing process. Denes et al.,5) who studied 63 patients with hip disarticulation, showed that patients with malignant tumors had higher prosthesis fitting success rates than those with vascular disease. Patients with vascular disease have high rates of wound complications, which often preclude the eventual fitting of the prosthesis.4) The aforementioned findings imply that the success of prothesis fitting may be dependent on the type of underlying disease. Given that the primary disease in our case was a malignant tumor, for which wound complications are uncommon, the situation was favorable for the early initiation of prosthesis fitting.
Studies have shown that the use of a hip prosthesis requires more energy expenditure than walking with crutches or wheelchair locomotion.5) Although few reports have investigated the gait pattern of those using a hip prosthesis,8) the swinging of the hip prosthesis is often practiced on the pelvic gait pattern. Accordingly, a pelvic gait pattern requires more strength in the unaffected lower extremity and trunk muscles than a normal gait pattern. A good ADL index before the onset of disease and good balance during single-leg standing are excellent indicators of muscle strength in the unaffected lower extremity.9) We believe that one of the reasons for the success observed in the current case was the patient’s preoperative ability to independently perform ADLs and household chores, including shopping. Given that our patient developed a thigh fracture because of a malignant tumor, her physical fitness (e.g., the 6-min walking distance) could not be systematically evaluated. Notably, she had not engaged in any specific sporting activities, implying that her physical fitness was typical for her age. In such cases, ADL assessment may be essential for determining the applicability of a hip prosthesis.
This case report has several limitations worth noting. First, cognitive function was not systematically and comprehensively assessed using a battery of neuropsychological tests. In addition to the scores of the MMSE, HDS-R, and the cognitive component of the FIM, we relied on clinical observation during hospitalization. Second, because of the left lower-extremity fracture, we could not perform systematic physical fitness evaluation, such as respiratory gas assessment on a bicycle ergometer. Third, given the nature of a case report, we could not set any numerical cutoff points for age or cognitive or physical functions for the application of a hip prosthesis. Despite these limitations, the present case report indicates that a hip prosthesis can be successfully indicated for regaining gait in an elderly patient based on simple clinical observations. This case report suggests some key points for the successful prescription of a hip prosthesis in elderly patients. The current patient was independent in ADL, and the functions of the unaffected extremities were sound. Cardiac and respiratory functions were well preserved, and there were no signs of cognitive decline. The causative disease of disarticulation was unlikely to cause trouble with wound healing. These factors, together with the patient’s motivation to walk, may be important factors in determining the prescription of a hip prosthesis in the elderly.
ACKNOWLEDGMENTS
The authors would like to thank Kei Setogawa, RPT, and Ken Sato, OTR. We are also grateful to Shinichi Tanaka, PO, for making and fitting the prosthesis. We also thank Dwayne from Enago (www.enago.jp) for English language review.
Footnotes
CONFLICTS OF INTEREST: The authors declare that there are no conflict of interests.
REFERENCES
- 1.Fletcher DD,Andrews KL,Hallett JW Jr,Butters MA,Rowland CM,Jacobsen SJ: Trends in rehabilitation after amputation for geriatric patients with vascular disease: implications for future health resource allocation. Arch Phys Med Rehabil 2002;83:1389–1393. 10.1053/apmr.2002.34605 [DOI] [PubMed] [Google Scholar]
- 2.Peng CW,Tan SG: Perioperative and rehabilitative outcomes after amputation for ischaemic leg gangrene. Ann Acad Med Singapore 2000;29:168–172. [PubMed] [Google Scholar]
- 3.Toursarkissian B,Shireman PK,Harrison A,D’Ayala M,Schoolfield J,Sykes MT: Major lower-extremity amputation: contemporary experience in a single Veterans Affairs institution. Am Surg 2002;68:606–610. [PubMed] [Google Scholar]
- 4.Moura DL,Garruço A: Hip disarticulation – case series analysis and literature review. Rev Bras Ortop Engl Ed 2017;52:154–158. 10.1016/j.rboe.2016.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dénes Z,Till A: Rehabilitation of patients after hip disarticulation. Arch Orthop Trauma Surg 1997;116:498–499. 10.1007/BF00387586 [DOI] [PubMed] [Google Scholar]
- 6.Lee DJ,Costello MC: The effect of cognitive impairment on prosthesis use in older adults who underwent amputation due to vascular-related etiology: a systematic review of the literature. Prosthet Orthot Int 2018;42:144–152. 10.1177/0309364617695883 [DOI] [PubMed] [Google Scholar]
- 7.Chin T,Kuroda R,Akisue T,Iguchi T,Kurosaka M: Energy consumption during prosthetic walking and physical fitness in older hip disarticulation amputees. J Rehabil Res Dev 2012;49:1255–1260. 10.1682/JRRD.2011.04.0067 [DOI] [PubMed] [Google Scholar]
- 8.Radcliffe CW: The biomechanics of the Canadian-type hip-disarticulation prosthesis. Artif Limbs 1957;4:29–38. [PubMed] [Google Scholar]
- 9.Eijk MS,van der Linde H,Buijck BI,Zuidema SU,Koopmans RT: Geriatric rehabilitation of lower limb amputees: a multicenter study. Disabil Rehabil 2012;34:145–150. 10.3109/09638288.2011.591888 [DOI] [PubMed] [Google Scholar]