Abstract
Background
Patients often perceive a lumbar puncture (LP) as an invasive procedure. We aimed to evaluate the impact of a 3‐minute educational animation‐video explaining the LP procedure, on patients’ knowledge, uncertainty, anxiety, and post‐LP complications.
Methods
We included 203 newly referred memory clinic patients, who were randomly assigned to one of three conditions: (1) home viewing of the video, (2) clinic viewing of the video, or (3) control condition (care as usual). Participants completed questionnaires measuring knowledge as information recall, uncertainty, anxiety, and post‐LP complications, the latter when patients underwent an LP procedure (n = 145).
Results
Viewing the video increased information recall for both home (P < .001), and clinic viewers (P < .001) compared to controls. Levels of uncertainty decreased after viewing (Pfor interaction = .044), particularly for clinic viewers. Viewing the video or not did not affect anxiety and post‐LP complications.
Discussion
Preparing individuals for an LP by means of an educational video can help to increase knowledge about the procedure and reduce feelings of uncertainty.
Keywords: Alzheimer's disease, educational animation‐video, information provision, lumbar puncture, memory clinics, patient education, post‐lumbar puncture complications
1. BACKGROUND
Cerebrospinal fluid (CSF) analysis is an important diagnostic tool in many neurological diseases, including Alzheimer's disease (AD). Biomarkers that are analyzed in CSF obtained via lumbar puncture (LP) play a crucial role in diagnosis of AD with very high sensitivity and specificity, 1 , 2 , 3 and will likely play an important role in the future of disease‐modifying treatments. Despite the diagnostic relevance of CSF analysis, it is still underused. On the one hand, physicians are often reluctant to use CSF biomarkers in daily practice, due to the invasive nature of the LP. On the other hand, patients can be reluctant to undergo an LP. This may be due to uncertainty and/or anxiety regarding the LP procedure itself, concerns about possible complications afterward, or due to a lack of knowledge—for example, they are not sufficiently aware of what the procedure entails, or the reasons to perform an LP. 4 , 5 In reality, severe complications associated with LPs are rare (ie, requiring hospitalization = 0.9%). 6 , 7 We previously found that feelings of anxiety concerning the LP increase the actual risk for complications, such as atypical post‐LP headache and local back pain. 6 A lack of (accurate) information prior to the LP may negatively affect patients’ anxiety and expectations regarding the LP procedure, which in turn increase the risk of complications. 7
Results obtained in different settings, such as prior to a colonoscopy, or during genetic counseling, showed that information about a medical procedure or health risk can reduce uncertainty and anxiety. 8 , 9 , 10 , 11 , 12 , 13 Audiovisual materials, like educational patient videos, are an effective method to inform patients. 14 , 15 Informing patients through audiovisual materials has been found to be more effective than by verbal or written methods as videos can better satisfy a patient's needs, and aid in information uptake and recall. 16 , 17
In co‐creation with stakeholders, we recently developed an animation‐video to inform and prepare patients and caregivers for the LP procedure in the context of AD diagnosis 18 (Figure A.1 in supporting information). In the current randomized controlled trial (RCT), we evaluated the effectiveness of the video for improving knowledge of the LP procedure, decreasing feelings of uncertainty and anxiety, and reducing the occurrence of post‐LP complications.
RESEARCH IN CONTEXT
Systematic review: The authors searched PubMed for relevant literature. Previous literature has established that cerebrospinal fluid analysis obtained via lumbar puncture (LP) is an important tool in the diagnosis of Alzheimer's disease. Despite the diagnostic utility it is often not implemented in daily clinical practice, due to its perceived invasiveness and patients’ uncertainty and anxiety toward the procedure. To date, empirical studies on how to optimally inform patients about the LP procedure are lacking completely. Previous studies in other medical fields have shown that audiovisual information provided to patients may reduce uncertainty and anxiety, and benefit medical outcomes. These relevant publications are appropriately cited.
Interpretation: We previously developed an educational animation‐video to inform patients about the LP procedure. To evaluate the effect of the animation‐video on patients’ knowledge, experienced uncertainty and anxiety, and post‐LP complications, we included 203 newly referred memory clinic patients in a randomized controlled trial. Patients were randomly assigned in one of three conditions: (1) home viewing, (2) clinic viewing, or (3) control condition. They completed questionnaires measuring knowledge, uncertainty, anxiety, and post‐LP complications at timepoints prior to and after undergoing an LP.
Future directions: The results reported on in this article can be used in clinical practice to improve patient education regarding an LP procedure. With this study we show that implementing the video in daily practice is beneficial for patients. These results support the development of similar videos for other diagnostic modalities, such as a positron emission tomography or magnetic resonance imaging scan. In addition, our study shows that improving patient information provision can be achieved using empirical research. This type of empirical research can also be applied to optimize information provision for individuals with low health literacy or other underrepresented populations.
2. METHODS
2.1. Participants and design
This study entails an RCT for which we consecutively invited all newly referred patients visiting the memory clinic of the Alzheimer Center Amsterdam for standardized dementia screening 19 between April 2019 and March 2020. Participants were recruited by telephone by the researchers prior to their visit to the outpatient clinic. Participants were excluded when they had audiovisual impairments, did not master the Dutch language, or if an e‐mail address was unavailable. Of the 203 consenting participants, 145 received a lumbar puncture and were available for follow‐up on post‐LP complications (Figure 1).
FIGURE 1.
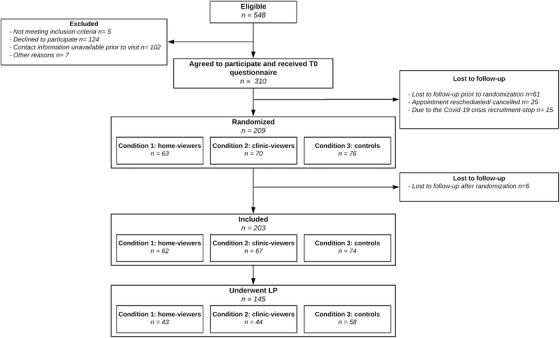
Study population flowchart. Abbreviations: Covid‐19, corona virus disease 2019; LP, lumbar puncture
All participants gave informed consent prior to participation. The study was reviewed and the need for formal approval was waived by the local medical ethical committee. The RCT was registered prior to the start at trialregister.nl, the Dutch Trial Registry (Trial NL7725).
Questionnaires were issued at four timepoints (Figure 2). Upon consent, participants received the baseline questionnaire (timepoint 1; T1), approximately 1 week prior to their visit. After completion of the T1 questionnaire, participants were randomly assigned to one of three conditions, by means of simple randomization: (1) home viewing, (2) clinic viewing, and (3) control condition. The study was embedded in the extensive routine work‐up in the outpatient clinic, and all participants received care as usual (ie, verbal information and an informational folder on the LP procedure) regardless of the study condition. The information provided in the video closely resembled the standard verbal and written information, which included information regarding the LP procedure and the most common complications. 18 Once a condition was assigned, condition 1 (home viewing) received a link to the video via e‐mail up to 1 week prior to their visit, allowing participants to watch the video as often as desired. Condition 2 (clinic viewing) viewed the video in the waiting room using headphones at the start of their visit to the outpatient clinic, prior to medical consultations. All participants received the second questionnaire at the start of their visit to the outpatient clinic at timepoint 2 (T2; clinic viewing first watched the video). In addition, participants received the third questionnaire at the end of the screening day (T3). Finally, participants were contacted by phone within 2 weeks after the LP by a physician, who asked about any post‐LP complications that occurred (T4).
FIGURE 2.
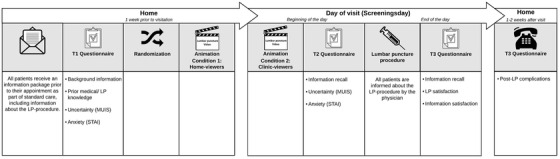
Schematic overview of the study
Highlights
We used a randomized controlled trial to improve information for patients about the lumbar puncture (LP) procedure.
Viewing our informative video improves knowledge and reduces uncertainty.
Viewing the animation or not did increase anxiety levels.
Providing the video can help prepare patients for an LP.
Both home viewing and integrating the video in the diagnostic visit is beneficial.
2.2. Measures
We assessed four main outcomes: patients’ recall of information, feelings of uncertainty and anxiety, and post‐LP complications. Additional outcomes of interest included patients’ satisfaction with the information and with the LP procedure.
2.2.1. Knowledge
Based on the information provided through standard care, we developed a questionnaire measuring knowledge as information recall. This questionnaire was pilot tested among six individuals to test clarity of questions and variation in responses. Participants were provided with eight multiple‐choice questions and were instructed to select the correct answer out of four. Sum scores for information recall were calculated after assigning one point for each correct answer. Information recall was assessed at T2 and T3.
2.2.2. Uncertainty and anxiety
Uncertainty levels were reported by participants at T1 and T2 using a selection of five relevant items from the Mishel Uncertainty in Illness Scale (MUIS), 20 answered on a five‐point Likert scale (1 = strongly disagree and 5 = strongly agree; Cronbach's α T1 = .71; Cronbach's α T2 = .65). An example of a question was: “the goal of the lumbar puncture is clear to me.”
State anxiety levels were assessed using a Dutch six‐item version of the State‐Trait Anxiety Inventory (S‐STAI‐S) at T1 and T2. 21 The items could be answered on a four‐point Likert scale ranging from 1 = not at all to 4 = very much so. 21 , 22
Higher scores indicated greater uncertainty and anxiety. Primary outcome measures were change over time as indicated by a comparison of uncertainty and anxiety levels reported at T1 and T2.
2.2.3. Post‐LP complications
Approximately 2 weeks after their visit (T4), participants were asked by telephone in a structured interview about the occurrence of post‐LP complications, previously described in Duits et al. 6 In brief, participants reported: (1) headache (yes/no), which in case of a positive answer was next specified as typical post‐LP headache or atypical headache, (2) local back pain (yes/no), or (3) severe complications (yes/no). Typical post‐LP headache was defined according to the International Classification of Headache Disorders (ICHD). 23 Severe complications were defined as complications serious enough to require hospitalization or an epidural blood patch.
2.2.4. Additional items
At baseline (T1), questions addressed patient demographics (eg, age, level of education). Additionally, baseline medical knowledge and knowledge about an LP procedure were both measured using a Visual Analog Scale (VAS; eg, “How much knowledge do you think you have about an LP procedure?”) ranging from zero (no knowledge at all) to ten (a lot of knowledge). Further, all participants were asked whether they had already seen an educational LP video prior to their visit to the outpatient clinic. At T2, home viewers were asked how often they had watched the video, and both home and clinic viewers were asked with whom they had watched the video. Moreover, at T3, all participants could indicate their satisfaction with the provision of information about the LP, and the LP procedure itself on VAS scales ranging from 1 = not at all to 10 = very much so.
2.3. Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics 24 (IBM Corp., Armonk, New York, USA). Demographic characteristics were compared between condition using chi‐squared tests, analysis of variance (ANOVA), or Kruskal‐Wallis test where appropriate; based on continuous, categorical, or ordinal scale of the variable. Intention to treat analysis included all 203 participants who were randomized, irrespective of whether they eventually underwent an LP. Changes in mean scores of self‐reported uncertainty and anxiety between conditions over time (T1 vs T2) were analyzed using repeated measures ANOVAs with Bonferroni post hoc tests. Information recall sum scores and patients’ information‐ and LP‐satisfaction scores were compared between conditions using univariate ANOVAs with Bonferroni post hoc test. Reported post‐LP complications were compared between conditions using chi‐squared tests. All analyses were corrected for sex and age, based on the study population of cognitively impaired individuals with a broad age range, and differences between conditions on demographic characteristics. Analyses for information recall were additionally corrected for prior LP knowledge. Next, we performed a per‐protocol analysis by repeating all analyses in participants who underwent an LP (n = 145). Finally, for exploratory reasons, we calculated Spearman correlations between the different outcome variables (uncertainty, anxiety, information recall, information satisfaction, and LP procedure satisfaction), and between patient‐related factors (ie, age, Mini‐Mental State Examination [MMSE], years of education, and prior LP knowledge) and outcome variables. A P < 0.05 was considered significant.
3. RESULTS
3.1. Demographics
We included 203 participants, with an average age of 63 ± 9 years; 72 (36%) were female, and the average MMSE was 25 ± 4. Sixty‐six (33%) participants received a dementia diagnosis, of which 48 (24%) were diagnosed as AD. Participants with a non‐dementia diagnosis included; subjective cognitive decline (SCD) 52 (26%), mild cognitive impairment (MCI) 14 (7%), and other diagnoses, such as other neurological disorders, 71 (34%). Participant characteristics are listed in Table 1. Participant distribution across conditions resulted in 62 in the home‐viewing condition, 67 in the clinic‐viewing condition, and 74 in the control condition. No differences were found across conditions in age, MMSE, years of education, diagnosis, and prior medical and LP knowledge. There was a trend toward more females in condition 1 (home viewing; Table 1).
TABLE 1.
Participant characteristics
| Total group | C1: Home viewing | C2: Clinic viewing | C3: Control condition | |
|---|---|---|---|---|
| n = 203 | n = 62 | n = 67 | n = 74 | |
| Age (years) | 63 ± 9, range 38 to 81 | 61 ± 8, range 46 to 81 | 64 ± 10, range 40 to 80 | 64 ± 9, range 38 to 79 |
| Sex, F(%) | 72 (36%) | 29 (47%) † | 21 (31%) | 22 (30%) |
| MMSE (n = 199) | 25 ± 4, range 11 to 30 | 25 ± 4, range 16 to 30 | 26 ± 4, range 11 to 30 | 25 ± 4, range 11 to 30 |
| Years of education | 12 ± 3, range 6 to 17 | 12 ± 3, range 6 to 17 | 13 ± 3, range 6 to 17 | 12 ± 3, range 8 to 17 |
| Diagnosis | ||||
| Dementia | 66 (33%) | 16 (26%) | 23 (34%) | 27 (37%) |
| AD | 48 (24%) | 11 (18%) | 17 (25%) | 20 (27%) |
| Non‐AD | 20 (9%) | 2 (3%) | 3 (5%) | 2 (3%) |
| Non‐dementia | 137 (68%) | 46 (74%) | 44 (66%) | 47 (64%) |
| SCD | 52 (26%) | 23 (37%) | 14 (21%) | 15 (20%) |
| MCI | 14 (7%) | 4 (7%) | 5 (8%) | 5 (7%) |
| Other | 71 (34%) | 8 (13%) | 13 (20%) | 12 (16%) |
| Prior medical knowledge | 4 ± 2 | 4 ± 2 | 4 ± 2 | 4 ± 2 |
| Prior LP knowledge | 4 ± 3 | 4 ± 3 | 4 ± 2 | 5 ± 3 |
| Help with questionnaire, n (%) | 128 (63%) | 45 (73%) | 40 (60%) | 43 (58%) |
| Times video viewed | n.a. | 1 ± 1, range 0 to 2 | 1 | 0 |
| Time since video (d) | n.a. | 3 ± 2, range 0 to 7 | 0 | n.a. |
| Primary language (n = 196) | ||||
| Dutch | 189 (93%) | 57 (92%) | 61 (94%) | 71 (97%) |
| Other | 11 (5%) | 5 (8%) | 4 (6%) | 2 (3%) |
NOTE: Table shows mean (SD), unless otherwise specified. Analyses of variance or Kruskal‐Wallis tests were applied where applicable. † = P < 0.10. Non‐AD includes: Lewy body disease, vascular dementia, frontotemporal dementia, and primary progressive aphasia. Other includes: psychiatry, other neurological disorders, and a postponed diagnosis.
Abbreviations: AD, Alzheimer's disease; LP, lumbar puncture; MCI, mild cognitive impairment; MMSE, Mini‐Mental State Exam; SCD, subjective cognitive decline; SD, standard deviation.
3.2. Information recall
We found differences in information recall between conditions at T2 (F[2, 170] = 23.16, P < .001) and T3 (F[2, 170] = 14.18, P < .001). At T2, both home and clinic viewing recalled more information, compared to the control condition (P < .001). This difference remained until the end of the day (T3, P < .001). There was no difference in information recall between home and clinic viewing at either T2 or T3. When restricting analyses to participants who underwent an LP (ie, per‐protocol analyses), results were similar (Table A.2 in supporting information). Likewise, results for uncorrected analyses are comparable (Table A.3 in supporting information).
3.3. Uncertainty and anxiety
ANOVA for repeated measures showed an effect of the intervention on the decrease in uncertainty (F[2, 183] = 5.02, Pfor interaction = .008). Here, clinic viewing showed the strongest decline in uncertainty over time, compared to both home viewing, and the control condition (Figure 3), though post hoc analyses did not yield significant differences between conditions. Results were largely comparable for uncorrected analyses (Table A.3), and after restricting analyses to participants who underwent an LP (ie, per‐protocol analyses; Table A.2).
FIGURE 3.
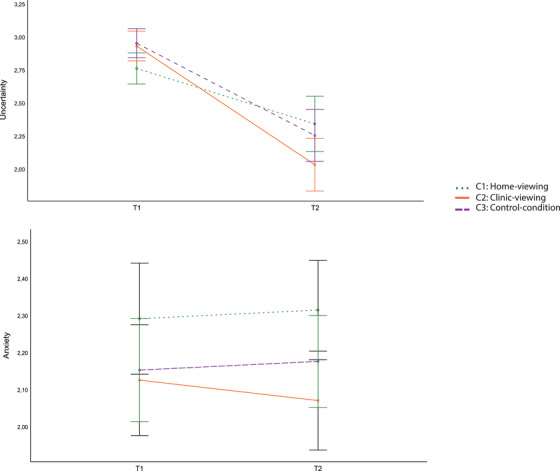
Estimated marginal means for uncertainty (Mishel Uncertainty in Illness Scale; A) and anxiety (State‐Trait Anxiety Inventory; B) at T1 and T2, with 95% confidence intervals. Analysis of variance (ANOVA) for repeated measures showed an effect of the intervention on the decrease in uncertainty (F[2, 183] = 5.02, Pfor interaction = .008). Here, clinic viewing showed the strongest decline in uncertainty over time, compared to both home viewing, and the control condition, though post hoc analyses did not yield significant differences between conditions. ANOVA for repeated measures for anxiety did not show an effect of the intervention on anxiety over time (F[2, 185] = .44, Pfor interaction = .64). Green dotted line = C1: home viewing, orange line = C2: clinic viewing, and purple dashed line = C3: control condition
With respect to anxiety, ANOVA for repeated measures did not show an effect of the intervention on anxiety over time (F[2, 185] = .44, Pfor interaction = .64). Next, analyses were repeated in participants who underwent an LP (n = 145). These per‐protocol analyses revealed similar results (Table A.2), as did uncorrected analyses (Table A.3).
3.4. Post‐LP complications
All reported post‐LP complications for participants who underwent an LP are listed in Table 2. Of all participants who underwent an LP, none reported a severe complication. Minor complications were quite common, as 67 (46%) reported one or two. We did not find any differences between conditions in the reported occurrence of non‐specific headache, typical post‐LP headache, or back pain.
TABLE 2.
Reported post‐LP complications
| Complication | Total group (T3) | C1: Home viewing | C2: Clinic viewing | C3: Control condition |
|---|---|---|---|---|
| n = 145 | n = 43 | n = 44 | n = 57 | |
| Typical post‐LP headache | 13 (9%) | 4 (9%) | 3 (7%) | 6 (11%) |
| Atypical post‐LP headache | 32 (22%) | 8 (19%) | 9 (21%) | 15 (26%) |
| Local back pain | 38 (26%) | 14 (33%) | 10 (23%) | 14 (25%) |
| Severe complications | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
NOTE: Table shows frequencies of post‐LP complications per condition, and in total, as reported by participants; (1) in case of reported headache (yes/no) this was specified as typical post‐LP headache or atypical headache, (2) local back pain (yes/no), or (3) severe complications (yes/no). Post‐LP complications were asked by telephone in a structured interview, previously described in Duits et al. 6
3.5. Exploratory analyses
Next, we compared information satisfaction and LP procedure satisfaction across conditions. Both the home‐ (8.9 ± 0.19), and clinic‐viewing conditions (8.8 ± 0.18) were slightly more satisfied with the information received regarding the LP compared to control condition (8.4 ± 0.17), although this effect did not reach significance (F[2, 176] = 2.24, P = .11). There was no difference in satisfaction with the LP procedure across conditions (F[2, 147] = .41, P = .66).
Subsequently, we explored associations between patient‐related factors and outcome measures. A decrease in uncertainty was associated with a decrease in anxiety (ρ = 0.25, P = .001). Further, patients who had greater LP information recall, experienced a stronger decrease in uncertainty (ρ = 0.23, P = .002) and anxiety over time (ρ = 0.16, P = .037). Finally, patients who had experienced a stronger decrease in uncertainty over time were more satisfied with the information received about the LP procedure (ρ = 0.28, P < .000), and with the LP procedure itself (ρ = 0.25, P = .003).
In addition, we found an association between age and change in uncertainty over time (ρ = –0.28, P < .001), as younger patients level of uncertainty decreased more over time (Figure 4). Further, we found that patients with higher MMSE had better information recall scores (ρ = 0.29, P < .001; Figure 4), and a larger decrease in uncertainty over time (ρ = 0.31, P < .001; Figure 4). In addition, patients with more years of education experienced a greater reduction in uncertainty over time (ρ = 0.21, P = .004; Figure 4). Additionally, patients who reported to have more knowledge regarding the LP procedure at baseline experienced a greater decrease in uncertainty over time (ρ = 0.32, P < .001; Figure 4).
FIGURE 4.
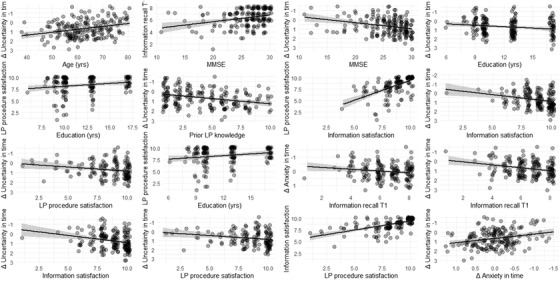
Scatterplots present the association between outcome measures, and outcome measures and patient‐related factors. Of note, a positive Δ uncertainty or Δ anxiety over time (eg, +1) equals a decrease in uncertainty or anxiety over time, and vice versa
4. DISCUSSION
The main finding of this randomized controlled trial on the effectiveness of an educational video as an adjunct to standard information was an improvement in knowledge and a reduction in level of uncertainty. Hence, our study suggests that a simple video is an effective tool for preparing individuals for a lumbar puncture in the context of AD diagnostics. Importantly, such a video is equally effective when offered at home or in the clinic.
As expected, the video increased patients’ knowledge about the LP procedure, compared to care as usual. This increase in patients’ procedural knowledge may be a result of repeating the information. Nevertheless, previous literature showed that the use of audiovisual information was associated with increased procedural knowledge, compared to solely verbal and written information. 11 , 14 , 16 , 24 , 25 , 26 , 27 Therefore, our finding may also be explained by having provided the information in an audiovisual format. Accurate knowledge about the diagnostic procedure may benefit patients and clinicians in several ways. First, in a former study, we found that memory clinic patients highly value procedural information about diagnostic tests. 28 Second, information fosters realistic patient expectations regarding the procedure and post‐LP complications. Third, procedural information allows patients to consider the relevance for their personal situation and preferences, and thus, empowers them to address such issues during patient–clinician interactions. Finally, using a video as a vehicle for patient education has the advantage of providing the same information to each patient, thus reducing unwarranted practice variation. This standardized information provision might also result in a reduction of consultation time. 26 Future work could assess potential benefits of the video regarding patient expectations and participation in patient–clinician interactions.
Watching the video also contributed to a reduction in uncertainty in patients who viewed the video at the day of the LP procedure (condition 2: clinic viewing). These findings are in line with two former studies, which reported reduced procedural uncertainty after audiovisual information provision on bariatric surgery and cardiac catheterization. 12 , 13 In addition, our explorative association analyses showed that the video appeared to reduce uncertainty most in younger participants, those with a higher MMSE, more years of education, or more prior self‐reported LP knowledge. It should be noted that self‐reported LP knowledge might not represent factual knowledge, but LP knowledge based on hearsay. This might explain why uncertainty could decrease strongly in patients with more prior LP knowledge. Contrary to our expectation, we did not detect any effects of the intervention on patients’ level of anxiety. Former studies in other fields, such as ophthalmology or anesthesia, have reported a decrease in anxiety after audiovisual information aids. 9 , 11 , 15 , 29 , 30 , 31 , 32 However, our results showed that patients experienced a relatively low level of anxiety, leaving little room for improvement. Therefore, a reduction in anxiety over time might have been too small to detect. In addition, physicians in our center are well educated and highly experienced in performing an LP. This has led us to develop an educational video on performing an LP procedure for professionals. 33 Because the LP is part of the routine diagnostic work‐up and performed on a daily basis, patients might feel more at ease as a result. Alternatively, while the STAI‐S is an extensively validated questionnaire, 21 , 22 it might not be sensitive enough to detect subtle changes in anxiety in a population including cognitively impaired individuals, as this has not been tested in this population. The video did not result in an increase in anxiety prior to the procedure, or an increase in post‐LP complications, and thus did not have any harmful effects.
Watching the educational video had no effect on post‐LP complications, whereas previously, we found a higher risk for post‐LP complications in patients who were anxious regarding post‐LP complications. 6 According to our hypothesis, the video would reduce anxiety, and as a result post‐LP complications. It is likely that compared to Duits et al. 6 the sample size was too small to detect small differences in post‐LP complications (3868 vs 145 participants, respectively). To effectively draw conclusions about the effect of information provision on the occurrence of post‐LP complications, this should be assessed using a larger sample. Therefore, even without an effect on post‐LP complications, the video effectively contributes to patient preparation.
Based on our findings, we recommend embedding the video in clinical practice in addition to routine care, as our results show that clinic viewers appear to benefit most from the video. Embedding the video in routine care facilitates health‐care providers as it is more efficient than sending it to each patient individually. Moreover, it ensures all patients see the video, and that any questions can be answered immediately. In addition, providing the video in routine clinical care makes it more accessible for every patient. For example, not all patients are able to view a video at home due to technological or cognitive disadvantages, such as cognitive impairment or illiteracy. Nevertheless, home viewers also benefit from the video in terms of increasing their knowledge, which may help them prepare for the LP procedure. Therefore, we would advise providing the video both prior to the visitation day and in the clinic, for example by placing the video on the website or showing it in the waiting area. If it is not feasible to embed the video in routine clinical practice, providing the video solely prior to the visitation day is a good alternative. Moreover, the video was developed specifically for cognitively impaired individuals. 18 Therefore, the information is presented in an easily understandable way. This might make the video as a medium of information provision especially suitable for individuals with low health literacy, as this concerns 12% of the European population. 34
This study has some limitations. First, the baseline questionnaire had to be filled in online, which may be more difficult for individuals with cognitive impairment. However, partners were allowed to assist the patient with filling in patients’ answers to the questionnaire. In addition, this was a single‐center study in a tertiary memory clinic, resulting in a relatively highly educated and young population. Of note, particularly the young and highly educated patients were most likely to benefit from the intervention. Second, inclusion was terminated prematurely due to SARS‐CoV‐2, the coronavirus that caused the COVID‐19 pandemic. 35 This resulted in a somewhat smaller sample size than envisioned, and may have led to loss of power, particularly with respect to the post‐LP complications analysis. Nevertheless, for this type of study, we were able to achieve a relatively large sample size.
A major strength of this study is the RCT design, which allowed us to establish the effectiveness of the video compared to standard information provision. In addition, this study was embedded into daily clinical routine, and therefore, it was designed to mimic the use of the video in a real clinical setting. Thus, our results translate directly to clinical practice, and show that it is feasible to implement the video in daily routine.
4.1. CONCLUSIONS
In conclusion, this RCT shows that a brief educational video increased patients’ knowledge, and decreased uncertainty in a large memory clinic cohort. This suggests that the video is of value for individuals undergoing an LP procedure, by helping them to prepare for the procedure in daily clinical practice. These results support the development of similar videos for other diagnostic modalities, such as a positron emission tomography or magnetic resonance imaging scan. This type of empirical research can also be applied to optimize information provision for individuals with low health literacy or other underrepresented populations.
CONFLICTS OF INTEREST
The authors have declared no conflicts of interest for this article.
Supporting information
Supporting Information
Supporting Information
Supporting Information
ACKNOWLEDGMENTS
The authors would like to thank all participants and the following people for their contribution to this study: Dr. Mathilde Verdam and Astrid Vark‐de Groot. The chair of Prof. Wiesje van der Flier is supported by the Pasman stichting and research of the Alzheimer Center Amsterdam is part of the neurodegeneration research program of Amsterdam Neuroscience. The Alzheimer Center Amsterdam is supported by Stichting Alzheimer Nederland and Stichting VUmc fonds and the clinical database structure was developed with funding from Stichting Dioraphte. This study was funded by Stichting LSH‐TKI (ABIDE‐communication: LSHM16025), a collaboration project co‐financed by Alzheimer Nederland, Piramal Neuroimaging, VU University Medical Center, and Amsterdam Medical Center, and financed by the Ministry of Economic Affairs and Climate Policy by means of the PPP Allowance made available by the Top Sector Life Sciences & Health to stimulate public–private partnerships (http://www.health-holland.com/). These funding sources were not involved in study design; in the collection, analysis, and interpretation of data; in writing of the manuscript; and the decision to submit the article for publication.
Babapour Mofrad R, Fruijtier AD, Visser LN, et al. Lumbar puncture patient video increases knowledge and reduces uncertainty: An RCT. Alzheimer's Dement. 2021;7:e12127 10.1002/trc2.12127
Rosha Babapour Mofrad and Agnetha D. Fruijtier contributed equally to this manuscript.
REFERENCES
- 1. Blennow K, Hampel H. CSF markers for incipient Alzheimer's disease. The Lancet Neurology. 2003;2:605‐613. [DOI] [PubMed] [Google Scholar]
- 2. Hulstaert F, Blennow K, Ivanoiu A, et al. Improved discrimination of AD patients using b‐amyloid(1‐42) and tau levels in CSF. Neurology. 1999;52:1555‐1576. [DOI] [PubMed] [Google Scholar]
- 3. Mulder C, Verwey NA, van der Flier WM, et al. Amyloid‐beta(1‐42), total tau, and phosphorylated tau as cerebrospinal fluid biomarkers for the diagnosis of Alzheimer disease. Clin Chem. 2010;56:248‐253. [DOI] [PubMed] [Google Scholar]
- 4. Blennow K, Dubois B, Fagan AM, Lewczuk P, de Leon MJ, Hampel H. Clinical utility of cerebrospinal fluid biomarkers in the diagnosis of early Alzheimer's disease. Alzheimers Dement. 2015;11:58‐69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zetterberg H, Tullhog K, Hansson O, Minthon L, Londos E, Blennow K. Low incidence of post‐lumbar puncture headache in 1,089 consecutive memory clinic patients. Eur Neurol. 2010;63:326‐330. [DOI] [PubMed] [Google Scholar]
- 6. Duits FH, Martinez‐Lage P, Paquet C, et al. Performance and complications of lumbar puncture in memory clinics: results of the multicenter lumbar puncture feasibility study. Alzheimers Dement. 2016;12:154‐163. [DOI] [PubMed] [Google Scholar]
- 7. Engelborghs S, Niemantsverdriet E, Struyfs H, et al. Consensus guidelines for lumbar puncture in patients with neurological diseases. Alzheimers Dement. 2017;8:111‐126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Scott A. Managing anxiety in ICU patients: the role of pre‐operative information provision. Nursing in Critical Care. 2004;9:72‐79. [DOI] [PubMed] [Google Scholar]
- 9. Freeman‐Wang T, Walker P, Linehan J, Coffey C, Glasser B, Sherr L. Anxiety levels in women attending colposcopy clinics for treatment for cervical intraepithelial neoplasia: a randomized trial of written and video information. Br J Obstet Gynaecol. 2001;108:482‐484. [DOI] [PubMed] [Google Scholar]
- 10. Lobb EA, Butow PN, Barratt A, et al. Communication and information‐giving in high‐risk breast cancer consultations: influence on patient outcomes. Br J Cancer. 2004;90:321‐327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Luck A, Pearson S, Maddem G, Hewett P. Effects of video information on precolonoscopy anxiety and knowledge: a randomised trial. The Lancet. 1999;354:2032‐2035. [DOI] [PubMed] [Google Scholar]
- 12. Arterburn DE, Westbrook EO, Bogart TA, Sepucha KR, Bock SN, Weppner WG. Randomized trial of a video‐based patient decision aid for bariatric surgery. Obesity (Silver Spring). 2011;19:1669‐1675. [DOI] [PubMed] [Google Scholar]
- 13. Chair SY, Chau MY, Sit JW, Wong EM, Chan AW. The psychological effects of a videotape educational intervention on cardiac catheterization patients. Contemp Nurse. 2012;40:225‐233. [DOI] [PubMed] [Google Scholar]
- 14. Snyder‐Ramos SA, Seintsch H, Bottiger BW, Motsch J, Martin E, Bauer M. Patient satisfaction and information gain after the preanesthetic visit: a comparison of face‐to‐face interview, brochure, and video. Anesth Analg. 2005;100:1753‐1758. [DOI] [PubMed] [Google Scholar]
- 15. Soydas Yesilyurt D, Yildiz Findik U. Effect of preoperative video information on anxiety and satisfaction in patients undergoing abdominal surgery. Comput Inform Nurs. 2019;37:430‐436. [DOI] [PubMed] [Google Scholar]
- 16. Sudore RL, Schillinger D. Interventions to improe care for patients with limited health literacy. J Clin Outcomes Manag. 2009;16:20‐29. [PMC free article] [PubMed] [Google Scholar]
- 17. Ahlander BM, Engvall J, Maret E, Ericsson E. Positive effect on patient experience of video information given prior to cardiovascular magnetic resonance imaging: a clinical trial. J Clin Nurs. 2018;27:1250‐1261. [DOI] [PubMed] [Google Scholar]
- 18. Babapour Mofrad R, Visser LNC, Fruijtier AD, et al. Cerebrospinal fluid collection: an informative animation video for patients and caregivers. Alzheimers Dement (Amst). 2019;11:435‐438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. van der Flier WM, Scheltens P. amsterdam dementia cohort: performing research to optimize care. J Alzheimers Dis. 2018;62:1091‐1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mishel MH, Braden CJ. finding meaning: antecedents of uncertainty in illness. Nursing Research. 1988;37:98‐127. [PubMed] [Google Scholar]
- 21. Marteau TM, Bekker H. The development of a six‐item short‐form of the state scale of the Spielberger State‐Trait Anxiety Inventory (STAI). Brifish Journal of Clinical Psycbholog. 1992;31:301‐306. [DOI] [PubMed] [Google Scholar]
- 22. van der Bij AK, de Weerd S, Cikot RJ, Steegers EA, Braspenning JC. Validation of the dutch short form of the state scale of the Spielberger State‐Trait Anxiety Inventory: considerations for usage in screening outcomes. Community Genet. 2003;6:84‐87. [DOI] [PubMed] [Google Scholar]
- 23. Headache classification committee of the international headache society (ihs) the international classification of headache disorders, 3rd edition. Cephalalgia. 2018;38:1‐211. [DOI] [PubMed] [Google Scholar]
- 24. Frosch DL, Legare F, Mangione CM. Using decision aids in community‐based primary care: a theory‐driven evaluation with ethnically diverse patients. Patient Educ Couns. 2008;73:490‐496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hoppe DJ, Denkers M, Hoppe FM, Wong IH. The use of video before arthroscopic shoulder surgery to enhance patient recall and satisfaction: a randomized‐controlled study. J Shoulder Elbow Surg. 2014;23:e134‐9. [DOI] [PubMed] [Google Scholar]
- 26. Kakinuma A, Nagatani H, Otake H, Mizuno J, Nakata Y. The effects of short interactive animation video information on preanesthetic anxiety, knowledge, and interview time: a randomized controlled trial. Anesth Analg. 2011;112:1314‐1318. [DOI] [PubMed] [Google Scholar]
- 27. Winter M, Kam J, Nalavenkata S, et al. The use of portable video media vs standard verbal communication in the urological consent process: a multicentre, randomised controlled, crossover trial. BJU Int. 2016;118:823‐828. [DOI] [PubMed] [Google Scholar]
- 28. Fruijtier AD, Visser LNC, van Maurik IS, et al. ABIDE Delphi study: topics to discuss in diagnostic consultations in memory clinics. Alzheimers Res Ther. 2019;11:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ahmed KJ, Pilling JD, Ahmed K, Buchan J. Effect of a patient‐information video on the preoperative anxiety levels of cataract surgery patients. J Cataract Refract Surg. 2019;45:475‐479. [DOI] [PubMed] [Google Scholar]
- 30. Dias R, Baliarsing L, Barnwal NK, Mogal S, Gujjar P. Role of pre‐operative multimedia video information in allaying anxiety related to spinal anaesthesia: a randomised controlled trial. Indian J Anaesth. 2016;60:843‐847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lin SY, Huang HA, Lin SC, Huang YT, Wang KY, Shi HY. The effect of an anaesthetic patient information video on perioperative anxiety: a randomised study. Eur J Anaesthesiol. 2016;33:134‐139. [DOI] [PubMed] [Google Scholar]
- 32. Purcell‐Jones JMA, Haasbroek M, Van der Westhuizen JL, Dyer RA, Lombard CJ, Duys RA. Overcoming language barriers using an information video on spinal anesthesia for cesarean delivery: implementation and impact on maternal anxiety. Anesth Analg. 2019;129:1137‐1143. [DOI] [PubMed] [Google Scholar]
- 33. Babapour Mofrad R, Bouwman FH, Slot RER, et al. Lumbar puncture in patients with neurologic conditions. Alzheimers Dement. 2017;8:108‐110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Sorensen K, Pelikan JM, Rothlin F, et al. Health literacy in Europe: comparative results of the European health literacy survey (HLS‐EU). Eur J Public Health. 2015;25:1053‐1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Cucinotta D, Vanelli M. WHO declares COVID‐19 a pandemic. Acta Biomed. 2020;91:157‐160. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information
Supporting Information
Supporting Information


