Abstract
Individually tailoring education over time may help more patients, especially racial/ethnic minorities, get wait-listed and pursue deceased and living donor kidney transplant (DDKT and LDKT, respectively). We enrolled 802 patients pursuing transplant evaluation at the University of California, Los Angeles Transplant Program into a randomized education trial. We compared the effectiveness of Your Path to Transplant (YPT), an individually tailored coaching and education program delivered at four time points, with standard of care (SOC) education on improving readiness to pursue DDKT and LDKT, transplant knowledge, taking 15 small transplant-related actions, and pursuing transplant (waitlisting or LDKT rates) over 8 months. Survey outcomes were collected prior to evaluation and at 4- and 8-months. Time to waitlisting or LDKT was assessed with at least 18 months of follow-up. At 8 months, compared to SOC, the YPT group demonstrated increased LDKT readiness (47% vs 33%, p = 0.003) and transplant knowledge (effect size [ES]=0.41, p<0.001). Transplant pursuit was higher in the YPT group (HR: 1.44, 95% CI: 1.15–1.79, p = 0.002). A focused, coordinated education effort can improve transplant-seeking behaviors and wait-listing rates.
ClinicalTrials.gov registration: NCT02181114
INTRODUCTION
End-stage kidney disease (ESKD) is becoming the new epidemic of our time (1). Approximately 15% of Americans have chronic kidney disease (CKD), with more than 700,000 people in ESKD, requiring either ongoing dialysis or kidney transplant (KT)(2). Compared to transplant, dialysis is associated with a significantly shorter life expectancy and poorer health-related quality of life (3–5). Living donor kidney transplant (LDKT) is associated with better post-transplant survival rates than deceased donor kidney transplant (DDKT) (6, 7). While the overall number of KTs performed each year increases, LDKTs comprise a declining share of these transplants (7).
Black and Hispanic patients are less likely than White patients to be waitlisted for DDKT or receive LDKTs, even though Black and Hispanic patients have higher rates of ESKD (7). In 2014, while White patients had 11.4% cumulative incidence of LDKT, Black and Hispanic patients only had 2.9% and 5.9% incidence, respectively (8).
Research has identified key modifiable factors that are associated with successful waitlisting, evaluation, and receipt of LDKT. The quality and applicability of education received about transplant and LDKT has been shown in multiple studies to be critical to preparing a patient to pursue KT and LDKT (9, 10). Examining the characteristics of patients who receive LDKTs, multiple studies (11–15) have shown that patients who complete evaluation and receive a LDKT are more likely to have received better education within dialysis centers (16), greater knowledge about transplant, and greater readiness to pursue LDKT (13). Targeted education for patients of racial and ethnic minorities and low socioeconomic status (SES) has also been shown to be beneficial, particularly when the education is culturally sensitive, in their own language, subsidizes transplant costs, and addresses barriers more common to these communities including low health literacy, transportation challenges, and cultural norms (17–20). However, the impact of educational interventions varies, with some failing to show improvements in knowledge or pursuit of transplant (21, 22).
Best practices for the design of transplant education recommend honoring the patient’s stage of readiness for transplant and delivering modular, culturally sensitive, health literate education over longer time periods (10). Computer-tailored interventions (CTIs) have the ability to create tailored feedback based on an individual patient’s specific level of readiness, knowledge gaps, self-efficacy challenges, and socioeconomic derailers and detect changes over time (23). In a longitudinal, randomized controlled trial (RCT) at the University of California, Los Angeles Kidney and Pancreas Transplant Program (UCLA-KPTP), we compared the effectiveness of a new CTI for transplant, Your Path to Transplant (YPT), with standard of care (SOC) education. We assessed: (1) YPT’s effectiveness for improving patients’ transplant knowledge, attitudes toward transplant, readiness to pursue transplant, completion of 15 transplant action-steps, and successful pursuit of transplant (waitlisted or LDKT.
METHODS
Randomized Controlled Trial (RCT) Design
This study was a prospective, parallel arm RCT with two follow-up time points conducted among 802 non-Hispanic Black, Hispanic (any race), and non-Hispanic White ESKD patients presenting for transplant evaluation at UCLA-KPTP. Enrolled patients were electronically randomized, stratified by race/ethnicity, with equal allocation to two treatment arms: the YPT intervention and SOC. All patients were surveyed prior to presenting at the transplant center (baseline), and at 4- and 8-months post-baseline.
The study protocol was approved by the University of California, Los Angeles’s Institutional Review Board (#14–000382) and registered at ClinicalTrials.gov (#NCT02181114). The full details of the protocol have been published (23).
Setting and Participants
Inclusion criteria for the RCT were: 1) presentation for KT evaluation at UCLA; 2) self-identification as White, Black, or Hispanic (any race). Patients were excluded if they were: 1) under age 18; 2) unable to speak or read English; 3) previously deemed ineligible at UCLA for KT; 4) on the waitlist at another center; 5) pursuing multi-organ transplant; or 6) without a working telephone. Patients were asked to give verbal informed consent to participate and have their electronic medical records reviewed.
Standard of Care (SOC) Arm
The SOC arm consisted of UCLA-KPTP education provided during a 3-hour transplant education session for patients and their family and friends, transplant coordinator communications, and self-study afterwards. The session outlined recipient and donor evaluation, surgery, and recovery processes.
Your Path to Transplant (YPT) Arm
YPT is a computer-tailored intervention that provides patients with telephonic coaching, feedback reports, access to community resources to overcome SES barriers, and video and print KT education resources tailored uniquely to them after a computerized patient assessment. At 4 time points, patients completed a screening to determine their current level of readiness to pursue DDKT and LDKT, transplant knowledge, socioeconomic barriers to transplant, and plan to take specific actions towards pursuing transplant and LDKT. Individual feedback reports were generated by the computer based on this screening that supported a patient at each unique level of transplant readiness, answered their specific knowledge gaps, and suggested how best to begin taking small transplant actions reported to be of interest to the patient. Patients were also provided referrals to community resources that might overcome SES barriers that might derail patients from transplantation, videos and print brochures from the Explore Transplant education program (24). Coaches emphasized the content and recommendations generated within the report and brainstormed with the patient on any transplant actions of interest to them and SES barriers identified. Each new screening at different time points updated the computerized patient assessment and generated a new tailored report. YPT patients received educational resources and coaching at 4 time points: a few weeks before and during transplant evaluation, and 4 and 8 months after baseline (Figure 1). Across all these time points, YPT patients received approximately 75 additional minutes of education compared to the SOC patients over an 8-month period. The YPT-generated coaching was delivered in person during evaluation and by telephone by a diverse racial/ethnic group of trained social work and public health coaches overseen by a clinical psychologist. Coaches were not matched by race/ethnicity to the patients they were coaching.
Figure 1.
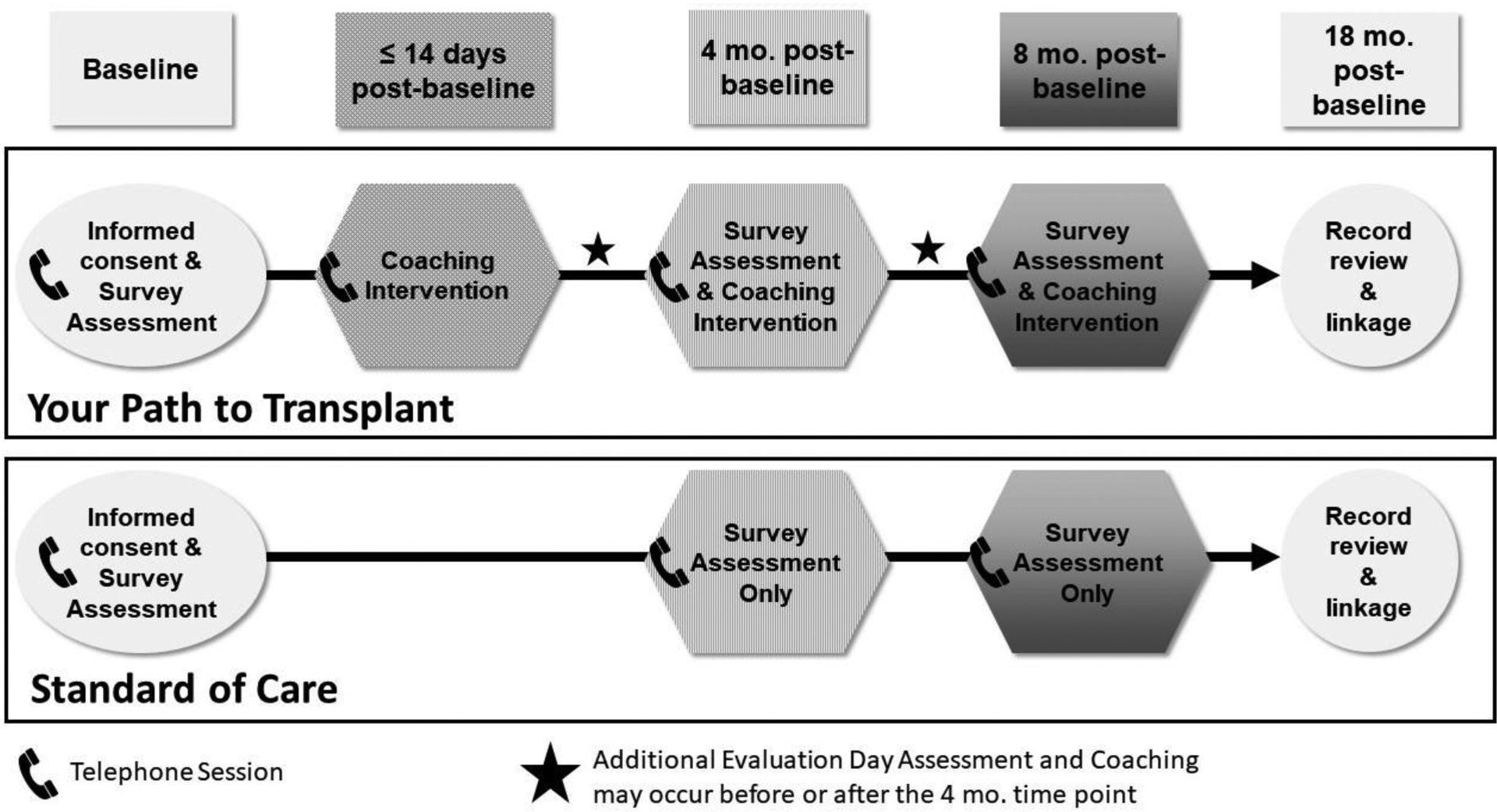
Study design
Measures
The primary study outcome was patients’ readiness to pursue LDKT and DDKT. To assess transplant readiness, patients were asked how ready they were to get a DDKT or LDKT and were scored as being in one of five stages (e.g., precontemplation, contemplation, preparation, action, maintenance) using our validated DDKT and LDKT stage of readiness measurement tools (25, 26) (Table 1). To assess transplant knowledge patients were asked 11 true/false and 8 multiple choice questions to determine their level of knowledge (14), producing a knowledge T-score (mean=50, SD=10) (15), with higher scores indicating greater knowledge. To assess ongoing progress toward transplant, patients were asked whether they had “Already done,” “Are planning to do,” or “Don’t plan to do” 15 transplant-related action-steps (25, 26). Examples of action-steps included “Share educational materials about deceased donation with people in your life” or “Ask potential donors to be tested.” Patients who said they had not “Already done” the action at baseline but had done so at a later survey time point were counted as having newly taken that step, with the total number of new steps taken calculated. Finally, pursuit of transplant (i.e., waitlisted for DDKT or received LDKT) was assessed via medical record review and linkage to the Scientific Registry for Transplant Recipients (SRTR) 18 months after enrollment of the last patient.
Table 1:
DDKT and LDKT Stages of Readiness Measurement
| DDKT Survey Question | Stage of Readiness |
|---|---|
| I am not considering getting a DDKT in the next six months | Precontemplation |
| I am considering getting a DDKT in the next six months | Contemplation |
| I am preparing to get a DDKT in the next 30 days | Preparation |
| I am undergoing evaluation to get a DDKT | Action |
| I am listed and waiting to get a DDKT | Maintenance |
| LDKT Survey Question | Stage of Readiness |
| I am not considering taking actions in the next six months to pursue LDKT | Precontemplation |
| I am considering taking actions in the next 30 days to pursue LDKT | Contemplation |
| I am preparing to take actions in the next 30 days to pursue LDKT | Preparation |
| I am taking actions to pursue LDKT | Action |
Additionally, the pre-intervention survey assessed basic patient demographic and clinical characteristics and level of SES barriers using the Kidney Transplant Derailers Index (KTDI)(27). We also asked patients whether they had previously read transplant brochures, watched transplant videos, or visited transplant websites.
Statistical Analyses
Details of the power analysis and rationale for the patient sample size recruited for this RCT have been published (23). All statistical tests employ an intent-to-treat (ITT) approach wherein subjects maintain their assignment to the study arm to which they were originally randomized regardless of whether they completed the planned interventions (28). To compare baseline characteristics between patients who dropped out of the study to those who did not, independent samples t-tests or nonparametric Kruskal-Wallis tests were used for continuous variables and chi-square or Fisher’s exact tests were used for categorical variables.
To evaluate differences between groups on the primary endpoint, DDKT and LDKT readiness levels were each first collapsed to a binary classification of Action versus all earlier stages of readiness. This binary outcome was then assessed in a mixed effect logistic regression model using R package lme4 (29). Maximum likelihood-based mixed effects models use all available data for each patient and provide valid estimates under the assumption that missing data are missing at random, conditional on the observed data. Intervention group, time, and the interaction between group and time were included in the model as fixed effects, along with random intercept and slope (time) terms at the patient level. The interaction between group and time represents the primary test of whether the changes in readiness over time differ between the two groups.
For the secondary endpoints, to test whether YPT patients showed increased knowledge scores compared to the SOC, a linear mixed effect model was fit using similar specifications of fixed and random effects as the model used for readiness. Effect sizes (ES = mean difference / baseline standard deviation) were calculated to provide a standardized, unitless measure of the magnitude of differences, which can be interpreted with the following cut-offs: 0.20 ≤ ES < 0.50 = small; 0.50 ≤ ES < 0.80 = medium; ≥ 0.80 = large. For the number of new steps taken, differences between the study arms in the count of new steps was analyzed with a Poisson model.
Pursuit of transplant was analyzed as time to event, defined as being placed on the deceased donor waiting list or receiving a LDKT. The time (in months) was calculated between the baseline survey date and date listed in SRTR, or date that patient received an LDKT. Patients who were not listed or transplanted were censored on November 30, 2018—18 months after the last patient was enrolled in the study. We also examined time to LDKT, specifically. Kaplan-Meier curves were stratified by study arm and differences assessed using the log-rank test. Cox proportional hazards models, adjusted for the randomization stratification factor – race/ethnicity, were also fit and hazards ratios estimated. The proportional hazards assumption was evaluated using statistical tests and graphical diagnostics based on the scaled Schoenfeld residuals.
Since this study was powered only to detect a main effect of intervention, interaction tests by race/ethnicity are considered exploratory. No adjustments for multiple comparisons were applied. All analyses were conducted in R version 3.5.1 (R Core Team)(30) and SAS version 9.4 (Cary, NC).
RESULTS
Participants
Study enrollment took place from May 2014 to May 2017, with follow-up for final pursuit of transplant outcomes through November 2018. Compared to those who consented (33%), those who declined participation were more likely to be Hispanic (Table S1). Of the 802 eligible patients who completed the baseline survey, 407 were allocated to the YPT group and 395 to the SOC group. Characteristics of the sample are listed in Table 2. Before joining the study, most participants read transplant brochures (62.8%), browsed websites about transplant (53.5%), or talked to doctors and other medical staff about transplant (87.4%), but few had watched videos about transplant (26.8%).
Table 2.
Baseline patient characteristics overall and by randomized group
| Overall | YPT | SOC | |
|---|---|---|---|
| (N=802) | (N= 407) | (N= 395) | |
| Age, mean (SD) | 53.0 (13.1) | 52.7 (13.0) | 53.2 (13.3) |
| Sex, n (%) | |||
| Men | 486 (60.6) | 239 (58.7) | 247 (62.5) |
| Women | 316 (39.4) | 168 (41.3) | 148 (37.5) |
| Race/ethnicity, n (%) | |||
| Non-Hispanic Black | 200 (24.9) | 108 (26.5) | 92 (23.3) |
| Hispanic | 313 (39.0) | 155 (38.0) | 158 (40.0) |
| Non-Hispanic White | 279 (34.7) | 138 (33.8) | 141 (35.7) |
| Other | 11 (1.4) | 7 (1.7) | 4 (1.0) |
| Comorbidities, n (%) | |||
| Diabetes | 350 (43.6) | 157 (38.6) | 193 (48.9) |
| Hypertension | 661 (82.4) | 337 (82.8) | 324 (82.0) |
| Polycystic kidney disease | 89 (11.1) | 44 (10.8) | 45 (11.4) |
| Insurance, n (%) | |||
| Medicare | 122 (15.3) | 56 (13.9) | 66 (16.8) |
| Medicaid | 221 (27.7) | 119 (29.5) | 102 (26.0) |
| Private Insurance (i.e. HMO, PPO) | 427 (53.6) | 221 (54.7) | 206 (52.4) |
| Don’t know | 7 (0.9) | 2 (0.5) | 5 (1.3) |
| Other insurance | 20 (2.5) | 6 (1.5) | 14 (3.6) |
| On dialysis, n (%) | 560 (69.8) | 275 (67.6) | 285 (72.2) |
| Education, n (%) | |||
| 8th grade or less | 19 (2.4) | 6 (1.5) | 13 (3.3) |
| Some high school | 56 (7.0) | 23 (5.7) | 33 (8.4) |
| High School Diploma or GED | 197 (24.6) | 101 (24.8) | 96 (24.3) |
| Some college or vocational school | 253 (31.6) | 129 (31.7) | 124 (31.4) |
| College or vocational school degree | 182 (22.7) | 100 (24.6) | 82 (20.8) |
| Some professional or graduate school | 21 (2.6) | 10 (2.5) | 11 (2.8) |
| Professional or graduate degree | 74 (9.2) | 38 (9.3) | 36 (9.1) |
| Transplant Education, n (%) | |||
| Read brochures about transplants | 504 (62.8) | 258 (63.4) | 246 (62.3) |
| Watched videos | 215 (26.8) | 111 (27.3) | 104 (26.3) |
| Browsed Internet websites | 429 (53.5) | 222 (54.5) | 207 (52.4) |
| Talked to doctors and other medical staff | 701 (87.4) | 357 (87.7) | 344 (87.1) |
A CONSORT diagram with reasons for drop-out at each time point is displayed in Figure 2. Patients who completed the 8-month survey were more likely to be in the SOC arm (p=0.009), have polycystic kidney disease as their etiology for ESKD (p = 0.016), and not yet be on dialysis (p = 0.013). There were no differences in study drop-out between race/ethnicity groups (Tables S2–S3).
Figure 2.
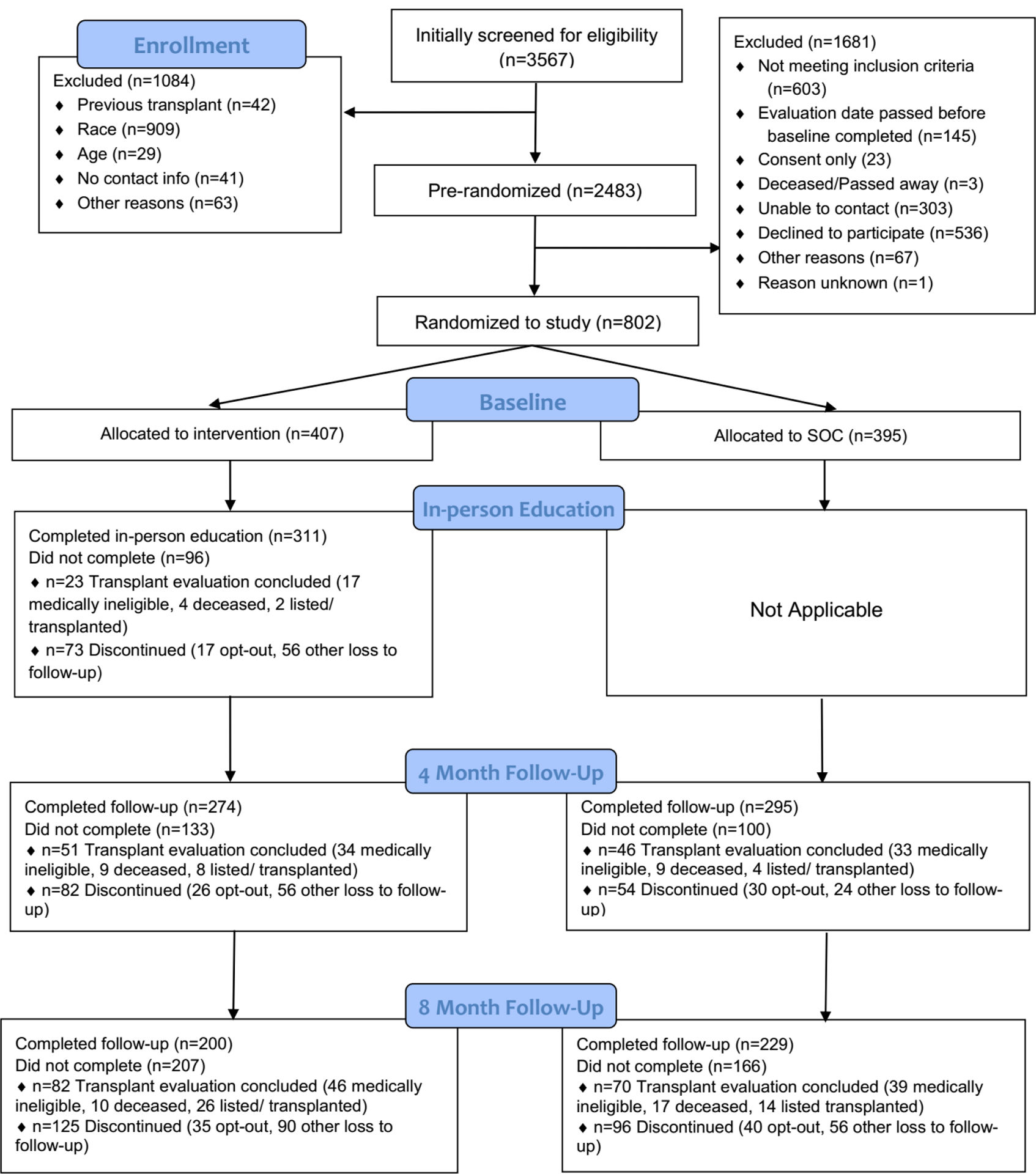
Your Path to Transplant Trial CONSORT Flowchart
Primary Outcome: Transplant Readiness
At baseline, 67.5% of patients reported being in the Action stage of readiness for DDKT and 44.5% in the Action stage for LDKT. Significantly higher proportions of YPT patients reported being in Action for DDKT compared to the SOC group at 4 months (82.8% vs. 72.5%, p = 0.004), but this difference was not as large at 8 months (84.0% vs. 76.4.0%, p = 0.066). In the mixed effects longitudinal model, the odds ratio [OR] for the comparison at 8 months was 3.16 (95% confidence interval [CI]: 0.92, 5.39; p-value = 0.019). A higher proportion of YPT patients reported being in Action for LDKT compared to SOC patients at 4 months (59.3% vs. 50.2%, p = 0.036), with a larger difference at 8 months (67.0% vs. 44.1%, p< 0.001; mixed model OR: 3.77, 95% CI: 1.04, 6.50; p = 0.005). The effect of YPT on LDKT readiness differed by race/ethnicity in the model (interaction p=0.039). However, this interaction between treatment and race/ethnicity was not observed for DDKT readiness (interaction p=0.087).
Secondary Outcome: Transplant Knowledge
At baseline, mean transplant knowledge T-score was 52.1 (SD=9.7). Compared to the SOC arm, a larger increase in transplant knowledge was observed for the YPT group over time (Figure 3; interaction p < 0.001). The difference between YPT and SOC was 1.5 points (ES = 0.15, p = 0.082) at 4 months and 4.1 points (ES = 0.42, p < 0.001) at 8 months. Race did not interact with treatment, indicating the effect of study arm on transplant knowledge after baseline did not differ substantially by race/ethnicity group (interaction p=0.70).
Figure 3.
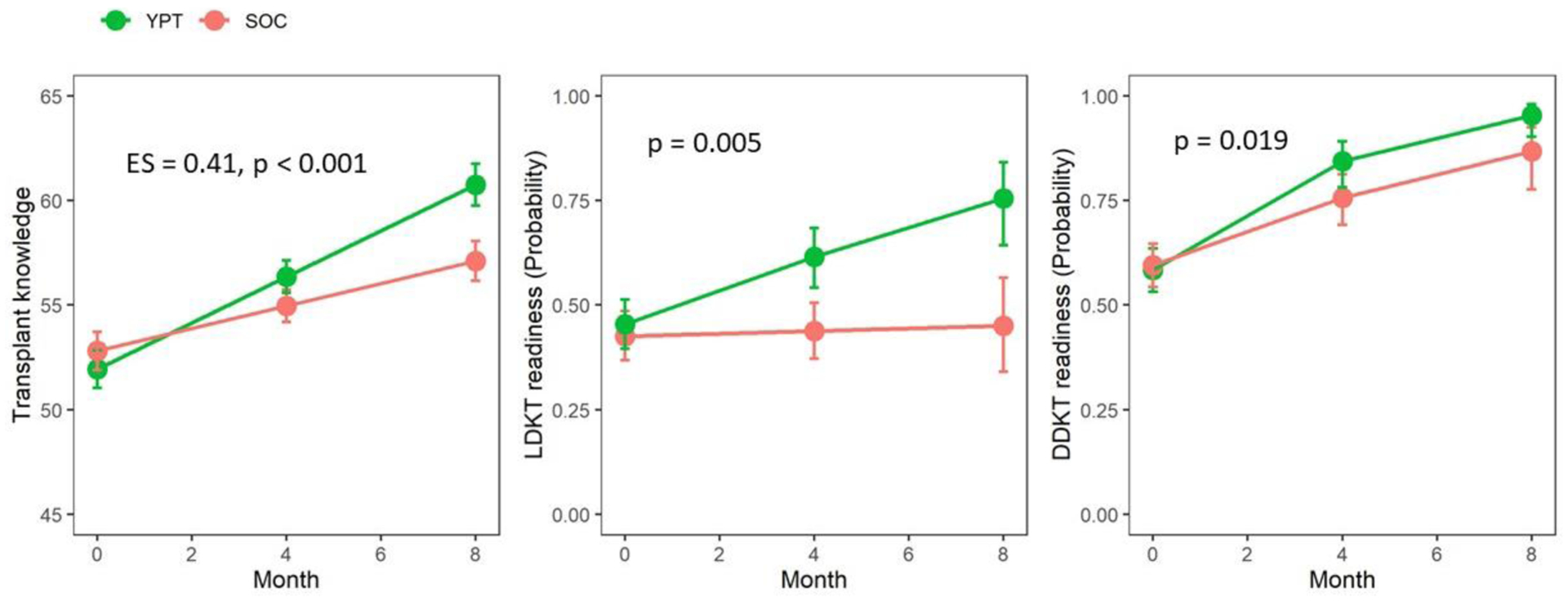
Transplant knowledge and readiness over time (mixed effect model predicted means and 95% confidence intervals)
Effect size and p-values are for comparison between YPT and SOC at month 8.
Secondary Outcome: New Steps toward LDKT and DDKT
At baseline, patients had taken a median of 1.0 steps towards LDKT (IQR = 4.0) and 2.0 steps towards DDKT (SD=3.0). Overall, the most common steps already taken at baseline were calling the transplant center to pursue evaluation, talking to people they trust about whether to get a living donor transplant, and making a list of people who might be living donors.
By the end of the study, YPT patients had taken a median of 3.0 (IQR = 3.0) new steps towards LDKT, compared to a median of 2.0 (IQR = 3.0) new steps in the SOC arm (RR: 1.12, 95% CI: 1.01 – 1.24, p=0.034). In addition to total new steps taken, YPT patients were more likely to take almost every individual new step towards LDKT and DDKT in comparison with the SOC arm (Table 3). Specifically, more YPT patients shared their need for a living donor with a large community (43.6% vs. 27.1%, p=0.001), shared educational materials about living donation with others in their life (86.0% vs. 67.0%, p<0.001), asked another person to tell others of their need for a living donor (63.8% vs. 49.3%, p=0.009), and asked potential donors to be tested (70.7% vs. 53.7%).
Table 3.
New steps towards LDKT and DDKT over the 8-month study period by randomized group
| Total N* | YPT N (%) | SOC N (%) | p-value | |
|---|---|---|---|---|
| Steps toward LDKT | ||||
| Share education materials about living donation with people in your life | 342 | 135 (86.0%) | 124 (67.0%) | <0.001 |
| Generally, talk to people you trust about whether to get a living donor transplant | 270 | 109 (86.5%) | 108 (75.0%) | 0.026 |
| Make a list of people who might be a living donor for you | 280 | 87 (70.7%) | 93 (59.2%) | 0.062 |
| Ask another person to tell others about your need for a living donor transplant | 353 | 97 (63.8%) | 99 (49.3%) | 0.009 |
| Ask potential donors to be tested | 358 | 111 (70.7%) | 108 (53.7%) | 0.002 |
| Give potential living donors the transplant center phone number | 417 | 134 (69.4%) | 129 (57.6%) | 0.017 |
| Share my need for a living donor with a large community (e.g., Facebook, Twitter, etc.)? | 397 | 78 (43.6%) | 59 (27.1%) | 0.001 |
| Steps toward DDKT | ||||
| Read information/watch videos about getting on the deceased donor waiting list | 419 | 179 (88.6%) | 157 (72.4%) | <0.001 |
| Share educational materials about deceased donation with people in your life | 387 | 160 (87.9%) | 138 (67.3%) | <0.001 |
| Generally, talk to people you trust about whether to get a deceased donor transplant | 348 | 150 (87.2%) | 119 (67.6%) | <0.001 |
| Call the transplant center to pursue evaluation | 219 | 97 (93.3%) | 101 (87.8%) | 0.256 |
| Complete and mail back the transplant center’s new patient medical forms | 451 | 208 (95.9%) | 207 (88.5%) | 0.007 |
| Invite someone to come to evaluation with you | 286 | 125 (94.7%) | 135 (87.7%) | 0.063 |
| Come to the transplant center to complete medical tests | 499 | 232 (93.5%) | 206 (82.1%) | <0.001 |
| Follow-up with transplant coordinator until transplant evaluation is complete | 462 | 178 (79.1%) | 162 (68.4%) | 0.012 |
Total sample size not already doing step at baseline.
There was also a significant difference between groups in number of new steps taken towards DDKT (RR = 1.13, 95% CI: 1.05 – 1.22, p=0.002) with a median of 5.0 (IQR = 3.0) new steps taken for the YPT arm and 4.0 (IQR = 3.0) for the SOC arm. More YPT patients shared educational materials about DDKT with people in their life (87.9% vs. 67.3%, p<0.001) and talked to people they trust about whether to get a DDKT (87.2% vs. 67.6%, p<0.001). No heterogeneity of intervention effect was observed for race (interaction p=0.67).
Final Outcome – Transplant Pursuit
After a minimum of 18 months follow-up, 323 patients total (40.2%) were either waitlisted for DDKT or received a LDKT (57.0% YPT vs 43.0% SOC), with those receiving the YPT intervention faring better (Figure 4, log-rank p = 0.003; HR: 1.39, 95% CI: 1.12 – 1.74). This benefit was unchanged after adjusting for race/ethnicity (HR: 1.44, 95% CI: 1.15 – 1.79; p = 0.002). No statistically significant interaction was observed between race/ethnicity and intervention group (p>0.2).
Figure 4.
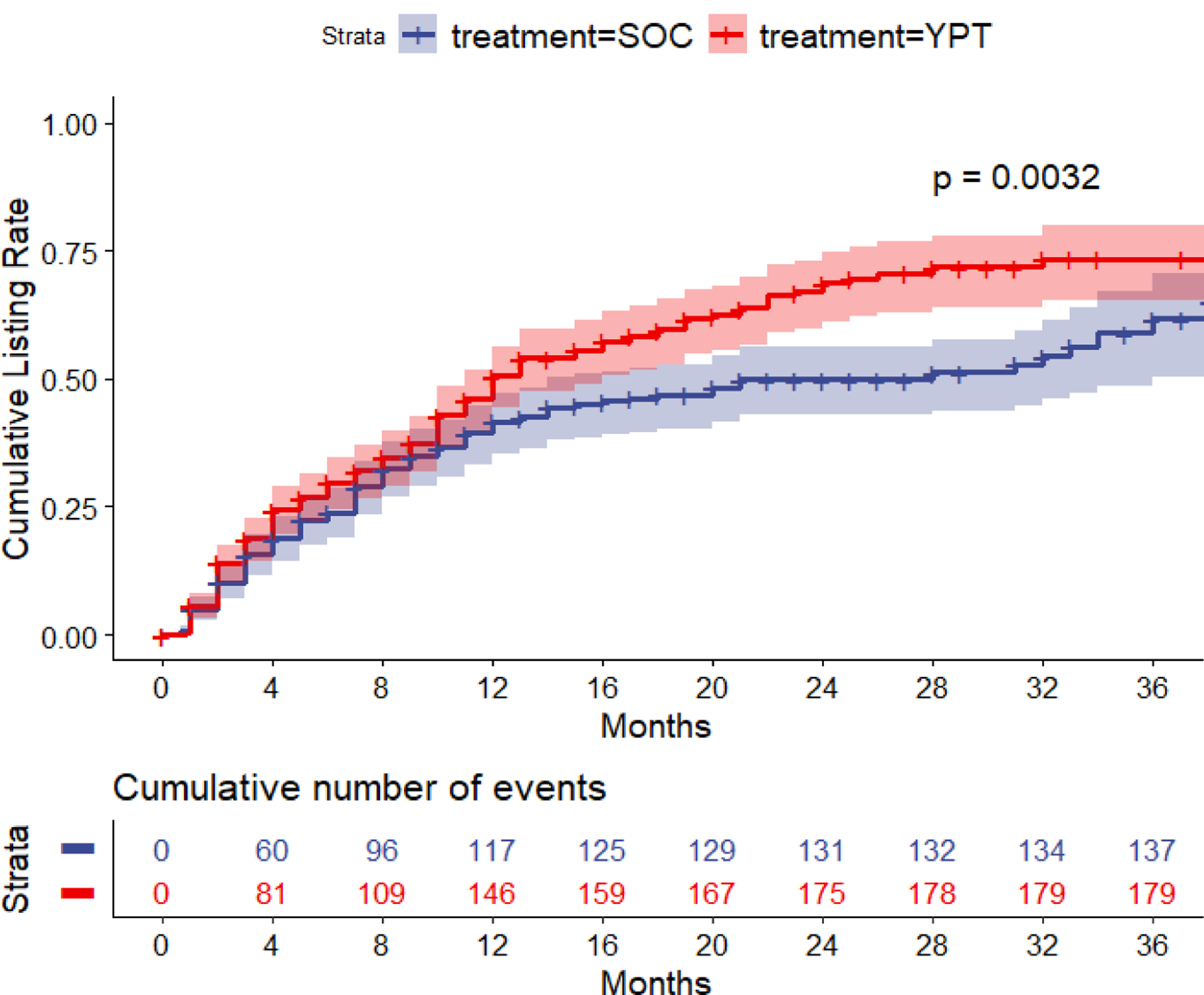
Waitlisting rate by randomized group
During the same follow-up period, 95 patients (11.8%) received an LDKT, with 53 (13.0%) in the YPT condition and 42 (10.6%) in the SOC condition (Figure 5, log-rank p = 0.42). There was no evidence that the YPT intervention had an effect on LDKT rates (HR: 1.23, 95% CI: 0.81 – 1.85; p=0.329). No interaction was observed between race/ethnicity and intervention groups in receipt of LDKT (interaction p=0.943).
Figure 5.
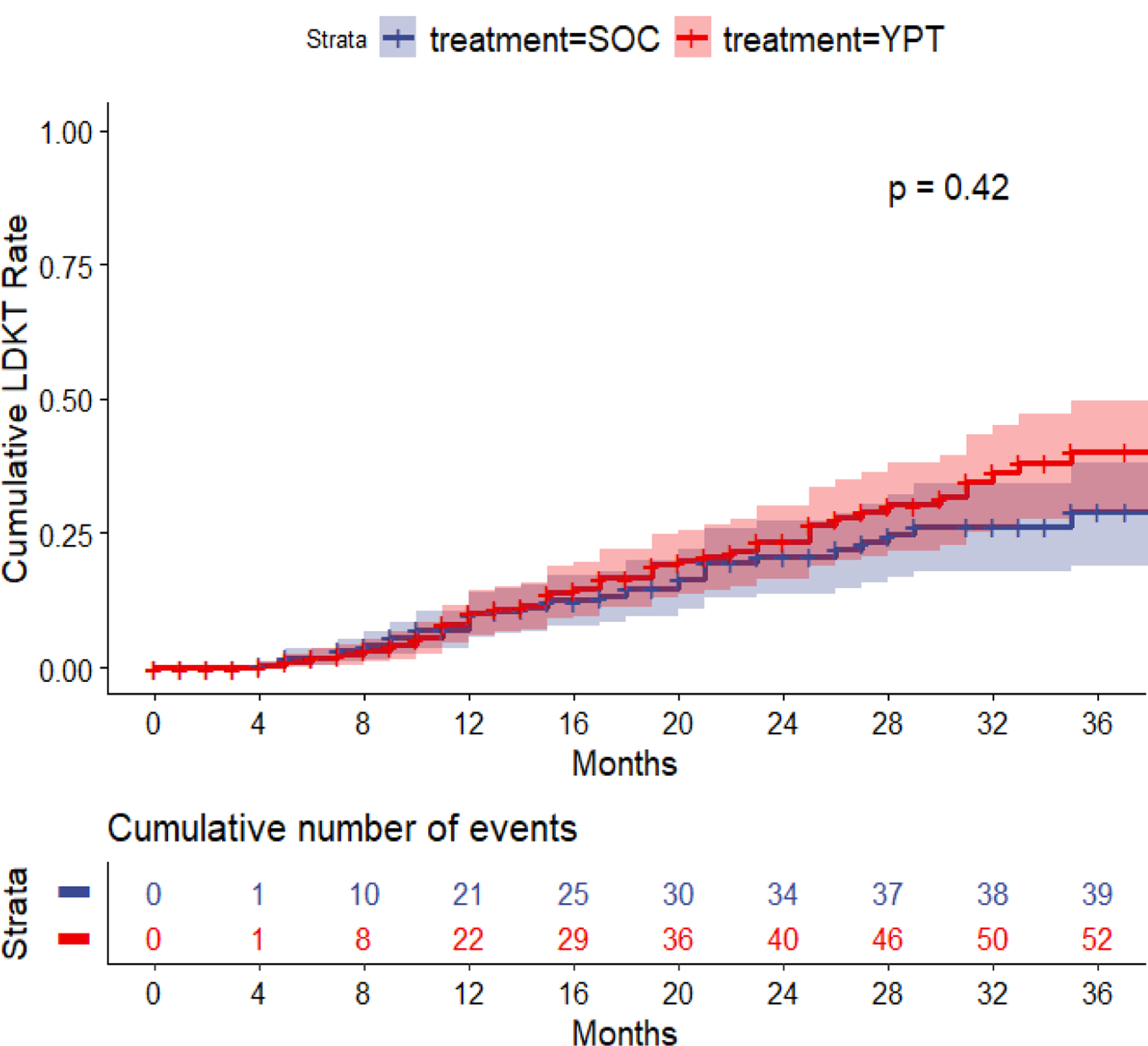
LDKT rate by randomized group
Evaluation of YPT.
Over 95% of participants found the coaches and print materials helpful and easy to understand. There was no difference between race/ethnicity groups in evaluation ratings.
DISCUSSION
For patients presenting for transplant evaluation, the road to successful kidney transplantation can be long and challenging. A recent study found that the average time to complete evaluation and get waitlisted was 226 days (31). This is the first examination of the effectiveness of an individually tailored education and coaching program, Your Path to Transplant, being delivered over 8 months during pursuit of evaluation. This study found that kidney patients who received YPT were more likely to increase their transplant knowledge, increase their readiness to pursue DDKT and LDKT, take more steps toward DDKT and LDKT, and be listed for transplant than patients who received only traditional SOC education. While YPT patients also were more likely to share their interest with people about LDKT and solicit living donors, there were no differences in actual LDKT rates by education condition after 18 months.
This is one of the longest and most comprehensive educational interventions ever to occur within a transplant center. While similar transplant educational studies vary in duration from one day to 18 months (17, 22, 24, 32–34), most commonly, they involve interventions occurring on evaluation day or during a single clinical visit with supplemental information provided afterwards for additional self-study (35, 36). Multiple studies now support expanding the length of interventions, involving living donors, and including multiple resources within interventions like videos, print materials, and coaching (17, 24, 32).
As part of their conversations, YPT coaches spent considerable time attempting to overcome commonly reported SES barriers to transplant (17–19). For example, during the coaching sessions, they provided information about low-cost or free transportation to the transplant center, dental care, and child care services, and discussed practical topics like where to park at the center and which bus route would help patients most easily get to the transplant center. Similarly, Basu et al., found that 4% of patient navigator encounters addressed transportation challenges (37).
In examining other interventions shown to increase transplant-seeking behaviors in racial/ethnic minorities, patient-level interventions using patient navigators (37, 38), home-based education with a minority health educator (17, 39), culturally targeted websites (33, 40), and culturally congruent transplant programs (41) have been found to be effective. At the patient and family level, discussions between participants and social workers (36), web-based education (33, 42), home-based educational meetings with patients (43), and meetings using technology to seek donors (44), and involving a patient’s social network, including potential living donors (45) have proven effectiveness. At the provider and system level, research has found that transplant facilities with specifically tailored toolkits to coordinate patient care (46, 47), and risk-based approaches identifying patients in need of targeted care (48, 49) were more successful. Interventions including multiple levels of the socioecological model may be needed, perhaps in combination (50–52).
Finally, this study has several limitations. First, the RCT was conducted in a single, high-volume transplant center in an urban area and, thus, may be limited in generalizability. Selection bias also potentially threatens generalizability of the study, as 21.6% (536 out of 2483) of pre-randomized patients declined to participate in the study, with a lower proportion of Hispanic patients providing consent. Over time, nearly 20% of patients could not complete all time points because they either died or became ineligible for transplant. Of the 80% that remained eligible for transplant over the entire 8- month time period, 36% were lost to follow-up by the 8-month visit, with a higher drop-out rate in the YPT group compared to SOC, potentially biasing our conclusions. If all patients still eligible for transplant but lost to follow-up were considered to be “not taking actions” towards LDKT, we find that patients in the YPT arm were still more likely to be taking actions than SOC (YPT: 130/325=40% vs SOC: 101/325=31%, p=0.017). Finally, it is possible that some of YPT’s treatment effect was diluted by patients who did not read the tailored education reports or watch the videos on their own at home. Since telephonic coaching sessions reviewed the content from these materials, even patients using the materials on their own but less often would still have some exposure to the intervention.
YPT provides an innovative option for supporting a racially and ethnically diverse ESKD patient population facing the many challenges of transplant evaluation and finding a living donor. This study revealed that it is possible to improve transplant patients’ knowledge, pursuit of transplant, and wait-listing rates if a focused, coordinated education effort honoring patients’ readiness and motivation to pursue DDKT and LDKT, addressing their unique SES barriers, and supporting them in taking critical transplant actions over time can be implemented. These individually tailored strategies could be embedded within traditional education programs at transplant centers to meet patients’ educational needs.
Supplementary Material
Acknowledgments
Funding for this study was provided by the National Institutes of Health (R01DK088711; T32DK104687).
Abbreviations
- CKD
Chronic kidney disease
- DDKT
Deceased donor kidney transplant
- ESKD
End-stage kidney disease
- KT
Kidney Transplant
- LDKT
Living donor kidney transplant
- OPTN
Organ Procurement Transplantation Network
- RCT
Randomized controlled trial
- SOC
Standard of care
- UCLA-KPTP
University of California, Los Angeles Kidney and Pancreas Transplant Program
- YPT
Your Path to Transplant
Footnotes
Disclosure
Dr. Amy D. Waterman, PhD owns the intellectual property to the transplant education product Explore Transplant and has licensed it at no-cost to a nonprofit, Health Literacy Media (HLM), who retains all revenue as to their sales. She serves as an unpaid consultant to HLM to ensure the accuracy of educational content. All other authors declare that they have no competing interests.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author, ADW.
Supporting Information
Additional supporting information may be found online in the Supporting Information section at the end of the article.
REFERENCES
- 1.Barnieh L, Collister D, Manns B, Lam NN, Shojai S, Lorenzetti D et al. A Scoping Review for Strategies to Increase Living Kidney Donation. Clin J Am Soc Nephrol 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saran R, Robinson B, Abbott KC, Bragg-Gresham J, Chen X, Gipson D et al. US Renal Data System 2019 Annual Data Report: Epidemiology of Kidney Disease in the United States. Am J Kidney Dis 2020;75(1s1):A6–a7. [DOI] [PubMed] [Google Scholar]
- 3.Neipp M, Karavul B, Jackobs S, Meyer zu Vilsendorf A, Richter N, Becker T et al. Quality of life in adult transplant recipients more than 15 years after kidney transplantation. Transplantation 2006;81(12):1640–1644. [DOI] [PubMed] [Google Scholar]
- 4.United States Renal Data System. 2018 USRDS annual data report: Epidemiology of kidney disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2018. [Google Scholar]
- 5.Kovacs AZ, Molnar MZ, Szeifert L, Ambrus C, Molnar-Varga M, Szentkiralyi A et al. Sleep disorders, depressive symptoms and health-related quality of life—a cross-sectional comparison between kidney transplant recipients and waitlisted patients on maintenance dialysis. Nephrol Dial Transplant 2011;26(3):1058–1065. [DOI] [PubMed] [Google Scholar]
- 6.de Groot IB, Veen JIE, van der Boog PJM, van Dijk S, Stiggelbout AM, Marang-van de Mheen PJ et al. Difference in quality of life, fatigue and societal participation between living and deceased donor kidney transplant recipients. Clin Transplant 2013;27(4):E415–E423. [DOI] [PubMed] [Google Scholar]
- 7.Hart A, Smith JM, Skeans MA, Gustafson SK, Wilk AR, Castro S et al. OPTN/SRTR 2017 Annual Data Report: Kidney. 2019;19(S2):19–123. [DOI] [PubMed] [Google Scholar]
- 8.Purnell TS, Luo X, Cooper LA, Massie AB, Kucirka LM, Henderson ML et al. Association of Race and Ethnicity With Live Donor Kidney Transplantation in the United States From 1995 to 2014. Jama 2018;319(1):49–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Segev DL. Innovative strategies in living donor kidney transplantation. Nature Reviews Nephrology 2012;8:332. [DOI] [PubMed] [Google Scholar]
- 10.Waterman AD, Robbins ML, Peipert JD. Educating Prospective Kidney Transplant Recipients and Living Donors about Living Donation: Practical and Theoretical Recommendations for Increasing Living Donation Rates. Curr Transplant Rep 2016;3(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Waterman AD, Hyland SS, Stanley SL, Barrett AC, Millinger R. Improving education increases dialysis patients’ pursuit of transplant: Explore Transplant RCT findings. In: American Transplant Congress; 2009 May 30-June 3; Boston, MA: American Journal of Transplantation; 2009. p. 360. [Google Scholar]
- 12.Dageforde LA, Box A, Feurer ID, Cavanaugh KL. Understanding Patient Barriers to Kidney Transplant Evaluation. Transplantation 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Waterman AD, Peipert JD, Hyland SS, McCabe MS, Schenk EA, Liu J. Modifiable patient characteristics and racial disparities in evaluation completion and living donor transplant. Clin J Am Soc Nephrol 2013;8(6):995–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patzer RE, Perryman JP, Pastan S, Amaral S, Gazmararian JA, Klein M et al. Impact of a patient education program on disparities in kidney transplant evaluation. Clin J Am Soc Nephrol 2012;7(4):648–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lockwood MB, Saunders MR, Nass R, McGivern CL, Cunningham PN, Chon WJ et al. Patient-Reported Barriers to the Prekidney Transplant Evaluation in an At-Risk Population in the United States. Prog Transplant 2017;27(2):131–138. [DOI] [PubMed] [Google Scholar]
- 16.Waterman AD, Peipert JD, Xiao H, Goalby CJ, Kawakita S, Cui Y et al. Education Strategies in Dialysis Centers Associated with Increased Transplant Wait-listing Rates. Transplantation 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rodrigue JR, Paek MJ, Egbuna O, Waterman AD, Schold JD, Pavlakis M et al. Making house calls increases living donor inquiries and evaluations for blacks on the kidney transplant waiting list. Transplantation 2014;98(9):979–986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gordon EJ, Reddy E, Gil S, Feinglass J, Rodde J, Abecassis MM et al. Culturally competent transplant program improves Hispanics’ knowledge and attitudes about live kidney donation and transplant. Progress in transplantation 2014;24:56–68. [DOI] [PubMed] [Google Scholar]
- 19.Sieverdes JC, Price M, Ruggiero KJ, Baliga PK, Chavin KD, Brunner-Jackson B et al. Design and approach of the Living Organ Video Educated Donors (LOVED) program to promote living kidney donation in African Americans. Contemp Clin Trials 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Purnell TS, Hall YN, Boulware LE. Understanding and overcoming barriers to living kidney donation among racial and ethnic minorities in the United States. Advances in chronic kidney disease 2012;19(4):244–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vilme H, Davenport CA, Pendergast J, Boulware LE. Trends in African Americans’ Attitudes and Behaviors About Living Donor Kidney Transplantation. Progress in Transplantation 2018:1526924818800036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weng FL, Peipert JD, Holland BK, Brown DR, Waterman AD. A Clustered Randomized Trial of an Educational Intervention During Transplant Evaluation to Increase Knowledge of Living Donor Kidney Transplant. Prog Transplant 2017;27(4):377–385. [DOI] [PubMed] [Google Scholar]
- 23.Waterman AD, Robbins ML, Paiva AL, Peipert JD, Kynard-Amerson CS, Goalby C et al. Your path to transplant: a randomized controlled trial of a tailored computer education intervention to increase living donor kidney transplant. BMC Nephrol 2014;15(166). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Waterman AD, Peipert JD. An Explore Transplant Group Randomized Controlled Education Trial to Increase Dialysis Patients’ Decision-Making and Pursuit of Transplantation. Progress in Transplantation 2018;28(2):174–183. [DOI] [PubMed] [Google Scholar]
- 25.Waterman A, Robbins M, Paiva A, Hyland SS. Kidney patients’ intention to receive a deceased donor transplant: Development of stage of change, decisional balance, and self-efficacy measures Journal of Health Psychology 2010;15(3):436–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Waterman AD, Robbins ML, Paiva AL, Peipert JD, Davis LA, Hyland SS et al. Measuring kidney patients’ motivation to pursue living donor kidney transplant: development of stage of change, decisional balance and self-efficacy measures. J Health Psychol 2015;20(2):210–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Peipert JD, Beaumont JL, Robbins M, Paiva A, Anderson C, Waterman A. Development and Validation of a Socioeconomic Kidney Transplant Derailers Index (KTDI). Am J Transplant 2017;17(suppl 3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Piantadosi S Clinical Trials: A Methodological Perspective. 2nd ed. Hoboken, NJ: Wiley, 2005. [Google Scholar]
- 29.Bates D, Mächler M, Bolker B, Walker S. Fitting Linear Mixed-Effects Models Using lme4. 2015 2015;67(1):48. [Google Scholar]
- 30.Team RC. R: A language and environment for statistical computing. R Foundation for Statistical Computing. 2017; Available from: https://www.R-project.org/ [Google Scholar]
- 31.Formica RN Jr., Barrantes F, Asch WS, Bia MJ, Coca S, Kalyesubula R et al. A One-Day Centralized Work-up for Kidney Transplant Recipient Candidates: A Quality Improvement Report. American Journal of Kidney Diseases 2012;60(2):288–294. [DOI] [PubMed] [Google Scholar]
- 32.Patzer RE, McPherson L, Basu M, Mohan S, Wolf M, Chiles M et al. Effect of the iChoose Kidney Decision Aid in Improving Knowledge about Treatment Options among Transplant Candidates: a Randomized Controlled Trial. Am J Transplant 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gordon EJ, Feinglass J, Carney P, Vera K, Olivero M, Black A et al. A Website Intervention to Increase Knowledge About Living Kidney Donation and Transplantation Among Hispanic/Latino Dialysis Patients. Prog Transplant 2016;26(1):82–91. [DOI] [PubMed] [Google Scholar]
- 34.Strigo TS, Ephraim PL, Pounds I, Hill-Briggs F, Darrell L, Ellis M et al. The TALKS study to improve communication, logistical, and financial barriers to live donor kidney transplantation in African Americans: protocol of a randomized clinical trial. BMC Nephrol 2015;16(1):160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Waterman AD, Peipert JD, Goalby CJ, Dinkel KM, Xiao H, Lentine KL. Assessing Transplant Education Practices in Dialysis Centers: Comparing Educator Reported and Medicare Data. Clin J Am Soc Nephrol 2015;10(9):1617–1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Boulware LE, Hill-Briggs F, Kraus ES, Melancon JK, Falcone B, Ephraim PL et al. Effectiveness of educational and social worker interventions to activate patients’ discussion and pursuit of preemptive living donor kidney transplantation: a randomized controlled trial. Am J Kidney Dis 2013;61(3):476–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Basu M, Petgrave-Nelson L, Smith KD, Perryman JP, Clark K, Pastan SO et al. Transplant Center Patient Navigator and Access to Transplantation among High-Risk Population: A Randomized, Controlled Trial. Clin J Am Soc Nephrol 2018;13(4):620–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sullivan C, Leon JB, Sayre SS, Marbury M, Ivers M, Pencak JA et al. Impact of Navigators on Completion of Steps in the Kidney Transplant Process: A Randomized, Controlled Trial. Clin J Am Soc Nephrol 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rodrigue JR, Cornell DL, Kaplan B, Howard RJ. A randomized trial of a home-based educational approach to increase live donor kidney transplantation: effects in blacks and whites. American Journal of Kidney Diseases 2008;51(4):663–670. [DOI] [PubMed] [Google Scholar]
- 40.Gordon EJ, Feinglass J, Carney P, Vera K, Olivero M, Black A et al. A Culturally Targeted Website for Hispanics/Latinos About Living Kidney Donation and Transplantation: A Randomized Controlled Trial of Increased Knowledge. Transplantation 2016;100(5):1149–1160. [DOI] [PubMed] [Google Scholar]
- 41.Gordon EJ, Lee J, Kang R, Ladner DP, Skaro AI, Holl JL et al. Hispanic/Latino Disparities in Living Donor Kidney Transplantation: Role of a Culturally Competent Transplant Program. Transplant Direct 2015;1(8):e29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gordon EJ, Sohn MW, Chang CH, McNatt G, Vera K, Beauvais N et al. Effect of a Mobile Web App on Kidney Transplant Candidates’ Knowledge About Increased Risk Donor Kidneys: A Randomized Controlled Trial. Transplantation 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Massey EK. Recommendations on how to improve medication adherence studies in the field of transplantation. Transplantation 2016;100(1):12–13. [DOI] [PubMed] [Google Scholar]
- 44.Cameron AM. Social Media and Organ Donation: The Facebook Effect. The Journal of legal medicine 2015;36(1):39–44. [DOI] [PubMed] [Google Scholar]
- 45.Ismail SY, Luchtenburg AE, Timman R, Zuidema WC, Boonstra C, Weimar W et al. Home-based family intervention increases knowledge, communication and living donation rates: a randomized controlled trial. Am J Transplant 2014;14(8):1862–1869. [DOI] [PubMed] [Google Scholar]
- 46.Taji L, Battistella M, Grill AK, Cunningham J, Hemmelgarn BL, Quinn KM et al. Medications Used Routinely in Primary Care to be Dose-Adjusted or Avoided in People With Chronic Kidney Disease: Results of a Modified Delphi Study. Ann Pharmacother 2020:1060028019897371. [DOI] [PubMed] [Google Scholar]
- 47.Haley WE, Beckrich AL, Sayre J, McNeil R, Fumo P, Rao VM et al. Improving care coordination between nephrology and primary care: a quality improvement initiative using the renal physicians association toolkit. American Journal of Kidney Diseases 2015;65(1):67–79. [DOI] [PubMed] [Google Scholar]
- 48.Smekal MD, Tam-Tham H, Finlay J, Donald M, Thomas C, Weaver RG et al. Patient and provider experience and perspectives of a risk-based approach to multidisciplinary chronic kidney disease care: a mixed methods study. BMC nephrology 2019;20(1):110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Smekal MD, Tam-Tham H, Finlay J, Donald M, Benterud E, Thomas C et al. Perceived benefits and challenges of a risk-based approach to multidisciplinary chronic kidney disease care: a qualitative descriptive study. Canadian journal of kidney health and disease 2018;5:2054358118763809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Patzer RE, McPherson L, Redmond N, DuBay D, Zayas C, Hartmann E et al. A Culturally Sensitive Web-based Intervention to Improve Living Donor Kidney Transplant Among African Americans. Kidney Int Rep 2019;4(9):1285–1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hamoda RE, Gander JC, McPherson LJ, Arriola KJ, Cobb L, Pastan SO et al. Process evaluation of the RaDIANT community study: a dialysis facility-level intervention to increase referral for kidney transplantation. BMC Nephrol 2018;19(1):13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mucsi I, Novak M, Toews D, Waterman A. Explore Transplant Ontario: Adapting the Explore Transplant Education Program to Facilitate Informed Decision Making About Kidney Transplantation. Canadian journal of kidney health and disease 2018;5:2054358118789369–2054358118789369. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


