Abstract
Study Design:
Retrospective cohort study.
Objective:
We intend to evaluate the accuracy and safety of cervical pedicle screw (CPS) insertion under O-arm-based 3-dimensional (3D) navigation guidance.
Methods:
This is a retrospective study of patients who underwent CPS insertion under intraoperative O-arm-based 3D navigation during the years 2009 to 2018. The radiological accuracy of CPS placement was evaluated using their intraoperative scans.
Results:
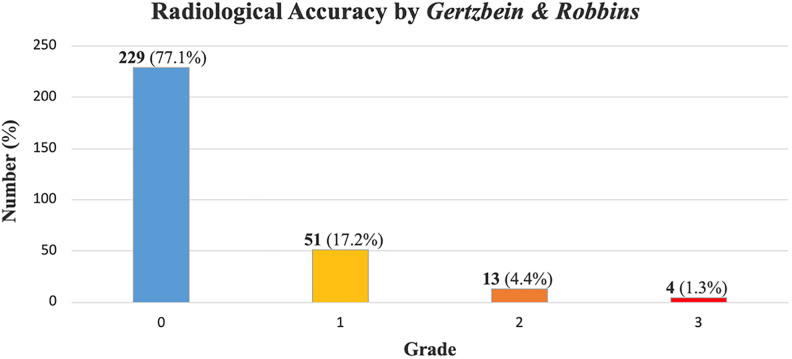
A total of 297 CPSs were inserted under navigation. According to Gertzbein classification, 229 screws (77.1%) were placed without any pedicle breach (grade 0). Of the screws that did breach the pedicle, 51 screws (17.2%) had a minor breach of less than 2 mm (grade 1), 13 screws (4.4%) had a breach of between 2 and 4 mm (grade 2), and 4 screws (1.3%) had a complete breach of 4 mm or more (grade 3). Six screws were revised intraoperatively. There was no incidence of neurovascular injury in this series of patients. 59 of the 68 breaches (86.8%) were found to perforate laterally, and the remaining 9 (13.2%) medially. It was noted that the C5 cervical level had the highest breach rate of 33.3%.
Conclusions:
O-arm-based 3D navigation can improve the accuracy and safety of CPS insertion. The overall breach rate in this study was 22.9%. Despite these breaches, there was no incidence of neurovascular injury or need for revision surgery for screw malposition.
Keywords: computer-assisted surgery, equipment safety, intraoperative complications, neuronavigation, pedicle screws
Introduction
The cervical pedicle screw (CPS) was first reported in the literature for its use in the traumatic cervical spine in 1994.1 Since its advent, its indications have gradually extended to include other nontraumatic pathologies, such as congenital, infective, inflammatory, malignant, and degenerative pathology.2,3
Biomechanical studies have time and time again proven that CPS fixation is superior.4 It has been demonstrated that it has a significantly lower rate of loosening at the bone-screw interface, as well as higher strength after fatigue testing.5 It allows for better bone purchase, creates robust and reliable fixation, and allows for shorter constructs.6
However, the CPS is also known to be technically challenging in its insertion. The anatomy of the cervical spine is complex which may limit the use of the pedicle screw.7 Moreover, this could further be compounded by pathology. The pedicle itself is small and narrow and lies in close proximity to neurovascular structures. If the screw were to breach the pedicle’s wall, it may result in catastrophic consequences.8
In the recent past, 3-dimensional (3D) navigation has evolved to be an excellent tool and has shown promising results in overcoming the challenges associated with pedicle screw insertion.9-17 However, the existing literature on the use of intraoperative O-arm-based 3D navigation, specifically for CPS insertion, is still sparse with small sample sizes.
Therefore, we intend to evaluate the accuracy and safety of CPS insertion under O-arm-based 3D navigation by assessing intraoperative pedicle breach rates in a predominantly Asian population. We believe that our observations and results will add to the current understanding of the importance of O-arm-based 3D navigation for CPS, particularly in preventing potential pedicle breaches that could lead to irreversible neurological compromise.
Materials and Methods
This is a retrospective study that was conducted on all patients who underwent CPS insertion under intraoperative O-arm-based 3D navigation. These surgeries were performed by spine surgeons from the orthopedic surgery and neurosurgery departments at a tertiary institution between January 2009 and July 2018 inclusive. The inclusion criteria were independent of the patient’s pathology. The exclusion criteria were for those who were undergoing revision surgery or whereby their intraoperative O-arm images were not available. Institutional review board approval was obtained prior to conducting this study (National Healthcare Group Domain Specific Review Board Reference No. 2018/00 889).
Patients were identified using the institution’s electronic patient database. Patient demographics, pathology, and surgical data was retrieved from their electronic records. Their intraoperative scans were reviewed, and postoperative recovery and complications were recorded as well. This study’s main outcome measures were the accuracy and safety of CPS insertion.
The accuracy of CPS insertion was evaluated using the intraoperative post-insertion scan and was classified according to Gertzbein and Robbins.18 Grade 0 is for screws that did not breach. For those that did breach, grade 1 is for minor breaches of less than 2 mm, grade 2 for breaches between 2 and 4 mm, and grade 3 for breaches more than 4 mm.
The intraoperative O-arm scanner (O-arm Medtronic plc Surgical Technologies, Louisville, KY, USA) is a mobile imaging system that has a computed tomography (CT) scanner in a 3D scan acquisition mode that can produce near CT quality imaging. Our institution acquired this system in January 2009.
Surgical Technique
The patient is positioned prone on the Jackson table (Modular Table System, Mizuho OSI, Union City, CA, USA). The patient’s head is then secured with a horseshoe or a head clamp. After which, the O-arm scanner is brought in perpendicular to the table length and centered using fluoroscopic images. Once centered, the O-arm scanner is carefully shifted to the foot of the table for the patient to be cleaned and draped.
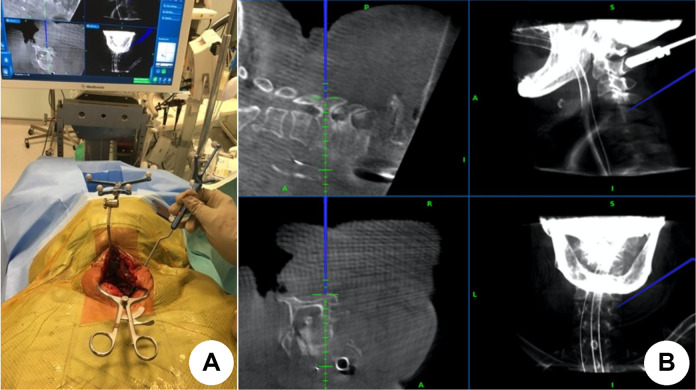
The surgical exposure is made via a posterior approach. With adequate bony exposure of the spinous processes and the lateral masses of the relevant cervical levels, the reference frame is attached securely to one of the spinous processes. Often, this will be the C2 spinous process. The sterile-draped O-arm scanner is then shifted back into position for the pre-insertion scan. The images are then processed by the 3D Navigation System (Stealth Station S7 Navigation System; Medtronic, Minneapolis, MN, USA), with the surgeon verifying the registration of the navigated surgical instruments (Figure 1).
Figure 1.
Verification process for the registration of navigated instruments.
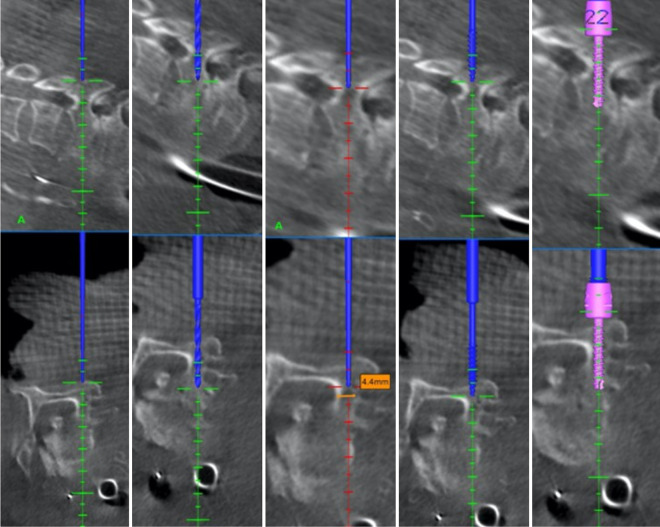
The CPS is then inserted under 3D navigation in a stepwise manner (Figure 2). The entry point and intended screw trajectory are identified. A divot is first made through the hard posterior cortex with a burr, to allow for the drill to anchor onto before drilling to its desired depth. The dimensions of the pedicle width and desired depth are then measured, which will inform the operating surgeon of the ideal CPS dimension. The screw hole is then tapped before the insertion of the CPS.
Figure 2.
Sequence of cervical pedicle screw (CPS) insertion under O-arm-based 3-dimensional navigation.
After the CPS screws have been inserted, the O-arm scanner is brought back into position for the post-insertion scan. The images are then reviewed intraoperatively, for the operating surgeon to assess the screw placement and if there is a need for any intraoperative screw revision.
Microsoft Excel 2013 was used for the generation of descriptive statistics. The simple ratio method was used for breach rates according to grade, level, and direction. Ninety-five percent confidence intervals were calculated for the overall breach rates. Linear regression analysis was used to identify if the study sample’s patient demographics (age, ethnicity, gender and pathology) can predict for pedicle breach.
Results
A total of 82 patients were included in this study. The mean age of these patients was 58.9 (range 12-82) years, with a male preponderance of 60 males to 22 females. It has a multiethnic makeup of 63 Chinese: 9 Malay, 5 Indian, and 5 others. These patient characteristics are presented in Table 1.
Table 1.
Patient Characteristics.
| Sample size | 82 |
| Age, y, mean (range) | 58.9 (12-82) |
| Gender, male:female | 60:22 |
| Ethnicity, n | |
| Chinese | 63 |
| Malay | 9 |
| Indian | 5 |
| Others | 5 |
| Pathology, n | |
| Congenital | 1 |
| Trauma | 20 |
| Infective | 5 |
| Inflammatory | 3 |
| Malignancy | 13 |
| Degenerative | 40 |
A total of 297 were CPSs analyzed in this study. Forty-two (14.1%) screws were inserted into the C2 level, and the remaining 255 (85.9%) of the screws were inserted into the subaxial (C3-7) levels. The spread of the CPS’s radiological accuracy is illustrated in Figure 3. There is an inverse relationship between the number of screws inserted to the grade of screw accuracy. 68 out of the 297 CPSs were found to have breached the pedicle, giving an overall breach rate of 22.9%. According to the Gertzbein classification, 51 (17.2%) were minor grade 1 breaches, 13 (4.4%) were grade 2 breaches, and 4 (1.3%) were grade 3 breaches.
Figure 3.
Radiological accuracy of cervical pedicle screw (CPS) insertion under O-arm-based 3-dimensional navigation according to Gertzbein and Robbins classification.
The breach rates were further analyzed according to their corresponding cervical level and their direction and are presented in Table 2. It is found that the C5 level had the highest breach rate of 33.3%, followed by the C6 level at 32.7%. It is further noted that C5 also had the highest breach rates in the significant grade 2 and 3 breaches, at 10.4% and 4.2% respectively. Of the screws that did breach, 86.8% of them breached laterally, while the remaining 13.2% breached medially. There were 6 (2.02%) screws that were revised intraoperatively. Despite these breaches, there was no incidence of sequelae of neurovascular injury. There was also no need for revision surgery a result of screw malposition.
Table 2.
Distribution of Cervical Pedicle Screws and Pedicle Breaches.
| Cervical Level | Total No. of Pedicle Screws | Total No. of Pedicle Breaches | 95% Confidence Interval | Pedicle Breaches | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Grade 0 | Grade 1 | Grade 2 | Grade 3 | Medial | Lateral | ||||||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | ||
| C2 | 42 | 14.1 | 7 | 16.7 | 0.070-0.314 | 35 | 83.3 | 6 | 14.3 | 0 | 0.0 | 1 | 2.4 | 1 | 14.3 | 6 | 85.7 |
| C3 | 28 | 9.4 | 6 | 21.4 | 0.083-0.410 | 22 | 78.6 | 6 | 21.4 | 0 | 0.0 | 0 | 0.0 | 2 | 33.3 | 4 | 66.7 |
| C4 | 30 | 10.1 | 5 | 16.7 | 0.056-0.347 | 25 | 83.3 | 4 | 13.3 | 1 | 3.3 | 0 | 0.0 | 0 | 0.0 | 5 | 100.0 |
| C5 | 48 | 16.2 | 16 | 33.3 | 0.204-0.484 | 32 | 66.7 | 9 | 18.8 | 5 | 10.4 | 2 | 4.2 | 2 | 12.5 | 14 | 87.5 |
| C6 | 52 | 17.5 | 17 | 32.7 | 0.203-0.471 | 35 | 67.3 | 12 | 23.1 | 4 | 7.7 | 1 | 1.9 | 1 | 5.9 | 16 | 94.1 |
| C7 | 97 | 32.7 | 17 | 17.5 | 0.106-0.266 | 80 | 82.5 | 14 | 14.4 | 3 | 3.1 | 0 | 0.0 | 3 | 17.6 | 14 | 82.4 |
| Total | 297 | 100.0 | 68 | 22.9 | 0.182-0.281 | 229 | 77.1 | 51 | 17.2 | 13 | 4.4 | 4 | 1.3 | 9 | 13.2 | 59 | 86.8 |
Patient demographics (age, ethnicity, gender, and pathology) were not found to be statistically significant predictors for pedicle breach, with P values of .053, .644, .058, and .179, respectively.
Discussion
Pedicle screws are routinely used in the thoracic and lumbar spine, although its adoption in the cervical spine has been cautious. The insertion of CPS is challenging, as the pedicles are smaller, narrower, and more variable in this region, and lie in close proximity to vital neurovascular structures. Thus, there is a drive to employ newer technologies that may improve the accuracy and safety of CPS insertion.
There have been a few studies over the past decade to evaluate the utility of intraoperative O-arm-based 3D navigation for the insertion of CPS. These studies have shown promising results, with an overall breach rate range of between 2.9% and 11.1%.13,19,20 This series of studies was first led by Ishikawa et al,19 who reviewed 108 CPS inserted by a group of well-experienced surgeons. It had an overall breach rate of 11.1%.19 The recent study by Chachan et al20 reviewed 241 CPS inserted by a single experienced surgeon, with an overall breach rate of 7.1%. Our study had a higher overall breach rate of 22.9%, which may be confounded by surgeon experience and anatomical characteristics of the selected population. The data collected for analysis started from when the institution first acquired the O-arm scanner and included surgeons from both orthopedic and neurosurgical departments with varying experience in the insertion of CPS, less so with the navigation system. There is a learning curve for screw insertion, that is likely factored into the breach rate.21 It is also noteworthy that there is a certain error in evaluating screw breach using CT, which may misrepresent a higher breach rate.22
Shimokawa et al13 and Chachan et al20 identified the C7 level to have the highest breach rate of 10.2% and 16.7%, respectively. This was attributed to the conflict with the paraspinal muscles in achieving the screw trajectory. Our study found that it was the C5 level that had the highest breach rate of 33.3%, followed by the C6 level with 32.7%. This may be explained by the pedicle’s anatomy. Morphometric studies have described cervical pedicles to have a mean pedicle width of 5.4 to 6.6 mm, reaching a nadir at C3 before increasing in size caudally. It was also noted that 3.8% of C5 pedicles did not have a medullary canal.23 The mean pedicle transverse angle was approximately 45° from C3 to C6 and 33° at C7, and the projected length of the pedicle axis was greatest at C5.24,25 These anatomical factors predispose the pedicle to breach. Furthermore, the relative mobility of the C5-C6 and C6-7 motion segments may inadvertently change the cervical alignment during instrumentation.26 This is especially so with navigation when the discrepancy may not be reflected and go unnoticed by the operating surgeon.
In terms of the direction of pedicle breaches, the current literature has consistently found them to be through the lateral cortex.13,20 This finding was again confirmed in our study, with a lateral breach rate of 86.8%. This is likely as a result of the far lateral entry point and the high medial angulation required to achieve the desired screw trajectory. In order to achieve this, the operating surgeon will have to overcome the forces from the paraspinal muscles without disturbing the cervical alignment. The cervical pedicle lateral wall has also been shown to be thinnest on cadaveric studies, making the wall prone to breach.7,23,26
The post-insertion scan allows for intraoperative evaluation and remedial CPS re-insertion if deemed necessary. There were 6 (2.02%) screws that were revised intraoperatively in this study. Despite the breaches in our study, there was no incidence of sequelae of neurovascular injury. It has been recognized in the literature that the breach rates may not translate to these injuries.8,27 This may be explained by how the occupancy of the vertebral artery in the transverse foramen is only 32.1% to 37.1%, and that the safe zone between the vertebral artery and the lateral wall increases caudally from 1.1 to 1.7 mm. For the less frequent medial breaches, the pedicle wall is at its thickest, and the dural sac is 2.4 to 3.1 mm away from the medial wall.28
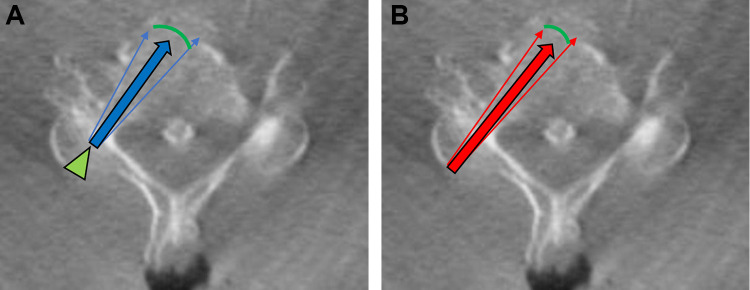
There are a couple of surgical pearls and pitfalls to limit pedicle breach that the authors have accrued over the years inserting CPS under O-arm-based 3D navigation. The first is to achieve adequate surgical exposure (Figure 4), which is dependent on a number of requisites. The exposure has to allow the operating surgeon to visualize the desired far lateral entry point, and to position the navigated instruments along the intended high medial angulation trajectory. This has to be done under minimal soft tissue interference, which may necessitate additional soft tissue releases to overcome the medializing forces of the paraspinal muscles. Underestimating the exposure required and placing the entry point more medial than intended narrows the window of safety to pedicle breach. With the medializing forces of the paraspinal muscles, it will predispose to the lateral breach.
Figure 4.
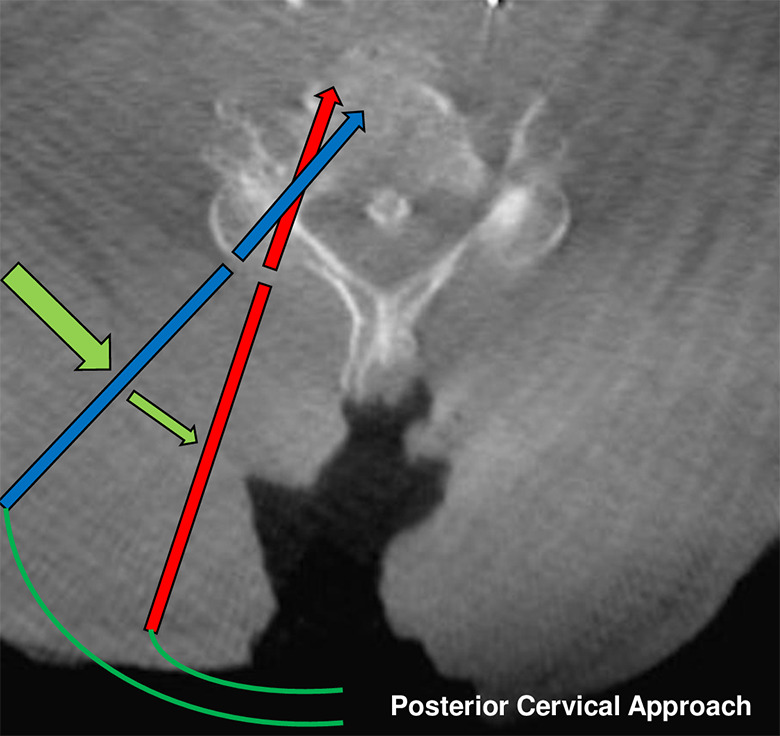
The surgical exposure required for screw insertion represented by curved lines.(Red line) Medial-most entry point and corresponding trajectory to clear the pedicle without breach. (Blue line) Desired entry point and trajectory. Notice the relative lateral entry point and the high medial angulation trajectory. (Green line) Relative medializing forces of the paraspinal muscles.
The second is to employ the modified funnel technique (Figure 5).29 This technique involves using a surgical burr to open up the hard posterior cortex at the intended screw entry point. The resulting ‘funnel’ allows for navigated instruments to anchor onto the cervical vertebrae, preventing them from deviating off the desired entry point. This reduces the excessive forces routinely applied via the instruments to hold it stable over the entry point, against soft tissue interference, which may alter the cervical alignment in the mobile cervical spine. Also, this technique shortens the pedicle axis length, bringing the starting point closer to the pedicle entrance. This widens the angle of safety by which the instruments and screw can take to traverse the pedicle length without breach.
Figure 5.
The modified funnel technique; the difference in pedicle axis length and window of safety is illustrated (A) with the technique employed and (B) without the technique employed. There is a relatively shorter pedicle axis length the screw will have to traverse, with an increase in the angle of safety from breaching.
The limitations of this study are that it is a retrospective study and there were no direct comparisons made with another navigation technique. This study achieves a moderate sample size with a predominantly Asian population and includes a number of operating surgeons with varying experience in the use of the O-arm-based 3D navigation. These factors may influence our results and interpretation.
Conclusion
O-arm-based 3D navigation can improve the accuracy and safety of CPS insertion. The overall breach rate in this study was 22.9%. Despite these breaches, there was no incidence of neurovascular injury or need for revision surgery for screw malposition. Although there is a learning curve with the adoption of this navigation system, with experience, the challenges associated with CPS insertion can be overcome.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Arun-Kumar Kaliya-Perumal, MS  https://orcid.org/0000-0002-2747-4500
https://orcid.org/0000-0002-2747-4500
Jacob Yoong-Leong Oh, FRCS  https://orcid.org/0000-0002-2832-8433
https://orcid.org/0000-0002-2832-8433
References
- 1. Abumi K, Itoh H, Taneichi H, Kaneda K. Transpedicular screw fixation for traumatic lesions of the middle and lower cervical spine: description of the techniques and preliminary report. J Spinal Disord. 1994;7:19–28. [DOI] [PubMed] [Google Scholar]
- 2. Abumi K, Ito M, Kaneda K. Surgical treatment of cervical destructive spondyloarthropathy (DSA). Spine (Phila Pa 1976). 2000;25:2899–2905. [DOI] [PubMed] [Google Scholar]
- 3. Oda I, Abumi K, Ito M, et al. Palliative spinal reconstruction using cervical pedicle screws for metastatic lesions of the spine: a retrospective analysis of 32 cases. Spine (Phila Pa 1976). 2006;31:1439–1444. [DOI] [PubMed] [Google Scholar]
- 4. Jones EL, Heller JG, Silcox DH, Hutton WC. Cervical pedicle screws versus lateral mass screws. Anatomic feasibility and biomechanical comparison. Spine (Phila Pa 1976). 1997;22:977–982. [DOI] [PubMed] [Google Scholar]
- 5. Johnston TL, Karaikovic EE, Lautenschlager EP, Marcu D. Cervical pedicle screws vs. lateral mass screws: uniplanar fatigue analysis and residual pullout strengths. Spine J. 2006;6:667–672. [DOI] [PubMed] [Google Scholar]
- 6. Kothe R, Ruther W, Schneider E, Linke B. Biomechanical analysis of transpedicular screw fixation in the subaxial cervical spine. Spine (Phila Pa 1976). 2004;29:1869–1875. [DOI] [PubMed] [Google Scholar]
- 7. Panjabi MM, Duranceau J, Goel V, Oxland T, Takata K. Cervical human vertebrae. Quantitative three-dimensional anatomy of the middle and lower regions. Spine (Phila Pa 1976). 1991;16:861–869. [DOI] [PubMed] [Google Scholar]
- 8. Abumi K, Shono Y, Ito M, Taneichi H, Kotani Y, Kaneda K. Complications of pedicle screw fixation in reconstructive surgery of the cervical spine. Spine (Phila Pa 1976). 2000;25:962–969. [DOI] [PubMed] [Google Scholar]
- 9. Kotani Y, Abumi K, Ito M, Minami A. Improved accuracy of computer-assisted cervical pedicle screw insertion. J Neurosurg. 2003;99(3 suppl):257–263. [DOI] [PubMed] [Google Scholar]
- 10. Ishikawa Y, Kanemura T, Yoshida G, Ito Z, Muramoto A, Ohno S. Clinical accuracy of three-dimensional fluoroscopy-based computer-assisted cervical pedicle screw placement: a retrospective comparative study of conventional versus computer-assisted cervical pedicle screw placement. J Neurosurg Spine. 2010;13:606–611. [DOI] [PubMed] [Google Scholar]
- 11. Rajasekaran S, Kanna PR, Shetty TA. Intra-operative computer navigation guided cervical pedicle screw insertion in thirty-three complex cervical spine deformities. J Craniovertebr Junction Spine. 2010;1:38–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Tauchi R, Imagama S, Sakai Y, et al. The correlation between cervical range of motion and misplacement of cervical pedicle screws during cervical posterior spinal fixation surgery using a CT-based navigation system. Eur Spine J. 2013;22:1504–1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Shimokawa N, Takami T. Surgical safety of cervical pedicle screw placement with computer navigation system. Neurosurg Rev. 2017;40:251–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chen YH, Feng SW, Yang YJ, Li CZ, Lin MC, Chung TT. Accuracy of spinal screw fixation using intraoperative O-arm navigation: consecutive series of 118 screws. J Med Sci. 2016;36:6–13. [Google Scholar]
- 15. Hur JW, Kim JS, Ryu KS, Shin MH. Accuracy and safety in screw placement in the high cervical spine: retrospective analysis of O-arm-based navigation-assisted C1 lateral mass and C2 pedicle screws. Clin Spine Surg. 2019;32:E193–E199. [DOI] [PubMed] [Google Scholar]
- 16. Du JP, Fan Y, Wu QN, Wang DH, Zhang J, Hao DJ. Accuracy of pedicle screw insertion among 3 image-guided navigation systems: systematic review and meta-analysis. World Neurosurg. 2018;109:24–30. [DOI] [PubMed] [Google Scholar]
- 17. Staartjes VE, Klukowska AM, Schroder ML. Pedicle screw revision in robot-guided, navigated, and freehand thoracolumbar instrumentation: a systematic review and meta-analysis. World Neurosurg. 2018;116:433–443. [DOI] [PubMed] [Google Scholar]
- 18. Gertzbein SD, Robbins SE. Accuracy of pedicular screw placement in vivo. Spine (Phila Pa 1976). 1990;15:11–14. [DOI] [PubMed] [Google Scholar]
- 19. Ishikawa Y, Kanemura T, Yoshida G, et al. Intraoperative, full-rotation, three-dimensional image (O-arm)-based navigation system for cervical pedicle screw insertion. J Neurosurg Spine. 2011;15:472–478. [DOI] [PubMed] [Google Scholar]
- 20. Chachan S, Bin Abd Razak HR, Loo WL, Allen JC, Kumar DS. Cervical pedicle screw instrumentation is more reliable with O-arm-based 3D navigation: analysis of cervical pedicle screw placement accuracy with O-arm-based 3D navigation. Eur Spine J. 2018;27:2729–2736. [DOI] [PubMed] [Google Scholar]
- 21. Yoshimoto H, Sato S, Hyakumachi T, Yanagibashi Y, Masuda T. Spinal reconstruction using a cervical pedicle screw system. Clin Orthop Relat Res. 2005;(431):111–119. [DOI] [PubMed] [Google Scholar]
- 22. Kim HS, Heller JG, Hudgins PA, Fountain JA. The accuracy of computed tomography in assessing cervical pedicle screw placement. Spine (Phila Pa 1976). 2003;28:2441–2446. [DOI] [PubMed] [Google Scholar]
- 23. Karaikovic EE, Daubs MD, Madsen RW, Gaines RW., Jr Morphologic characteristics of human cervical pedicles. Spine (Phila Pa 1976). 1997;22:493–500. [DOI] [PubMed] [Google Scholar]
- 24. Chazono M, Soshi S, Inoue T, Kida Y, Ushiku C. Anatomical considerations for cervical pedicle screw insertion: the use of multiplanar computerized tomography reconstruction measurements. J Neurosurg Spine. 2006;4:472–477. [DOI] [PubMed] [Google Scholar]
- 25. Sakamoto T, Neo M, Nakamura T. Transpedicular screw placement evaluated by axial computed tomography of the cervical pedicle. Spine (Phila Pa 1976). 2004;29:2510–2515. [DOI] [PubMed] [Google Scholar]
- 26. Bogduk N, Mercer S. Biomechanics of the cervical spine. I: Normal kinematics. Clin Biomech (Bristol, Avon). 2000;15:633–648. [DOI] [PubMed] [Google Scholar]
- 27. Neo M, Sakamoto T, Fujibayashi S, Nakamura T. The clinical risk of vertebral artery injury from cervical pedicle screws inserted in degenerative vertebrae. Spine (Phila Pa 1976). 2005;30:2800–2805. [DOI] [PubMed] [Google Scholar]
- 28. Tomasino A, Parikh K, Koller H, et al. The vertebral artery and the cervical pedicle: morphometric analysis of a critical neighborhood. J Neurosurg Spine. 2010;13:52–60. [DOI] [PubMed] [Google Scholar]
- 29. Karaikovic EE, Yingsakmongkol W, Gaines RW., Jr Accuracy of cervical pedicle screw placement using the funnel technique. Spine (Phila Pa 1976). 2001;26:2456–2462. [DOI] [PubMed] [Google Scholar]