Abstract
Study Design:
Descriptive study.
Objective:
Assessing the applicability of blended learning to specific domains of spine surgery.
Methods:
After the needs assessment, a blended pediatric spine deformity course program was designed. A total of 33 participants, including orthopedic and neurosurgeons, registered for the course and all of them completed an online entrance quiz. Thus, they were eligible to have online part of course, which included the theoretical part of the course and also a discussion forum where the discussions about the topics facilitated by faculty. Thirteen of 33 subjects participated second part of the blended pediatric spine deformity course. This face-to-face (F2F) part consisted of case discussions for each topic and discussions facilitated by faculty members. The same quiz was also taken before and after the F2F part. All quiz results were compared statistically.
Results:
There were 11 lectures within the online part and 6 case discussions in the F2F part. The quiz scores were improved significantly by having a complete blended pediatric deformity course (P < .05).
Conclusions:
The current study has demonstrated that blended learning format, including online and F2F, is feasible and effective in training for a domain of spine surgery, pediatric deformity in this specific context.
Keywords: blended learning, e-learning, spine surgery, postgraduate education
Introduction
The widespread availability of information and communication technologies has created radical changes in the learning needs of individuals, especially in medicine. While new information in forms of new studies and techniques flow in, utilization of time effectively to reach, absorb, and internalize them becomes of utmost importance. As traditional teaching strategies may be insufficient to meet these changing needs. Blended learning approaches, as alternatives based on communication and information technologies, are increasing in popularity.1 Blended learning not only translates theory into practice2 but also enables adaptive and collaborative learning, and transforms the teacher’s role from transmitting knowledge (instructing) to facilitating learning. Moreover, through the integration of technology into education, it enables flexible, learner-centered learning, as well as asynchronous communication and collaboration, using adult learning principles3 and potentially eliminates problems of crowded classrooms with little real teacher-learner interaction.4
On the other hand, blended learning is highly content- and context-sensitive and interdisciplinary transitions are unpredictable. There is no guarantee that a successful blended learning application in one field will be equally successful in another one. In order to ensure a successful transition, educator(s) should first determine how best to teach the subject and then decide how to integrate technology into this teaching.5
Medicine has been reported as one of the very suitable disciplines for blended learning.3 Reports indicate that medical students reported that they were satisfied with e-learning4,5 but did not think of it as a strategy to replace traditional teacher-cantered education. Another advantage of the use in clinical medical disciplines is that training can be done at any time and be tailored to the individual’s learning needs.6 Blended learning is also on the rise in subspecialty medical education.5,7-11 For example, it was demonstrated that blended learning was used in training in maxillofacial surgery, participants preferred online learning over the traditional alternative and were very satisfied12; blended learning was shown to be effective in reducing obstetric anal sphincter injuries in a program attended by doctors and midwives13; and blended learning resulted in the highest gains in acquiring information compared with online learning alone in family planning education.14 For our purposes, Gunzburg and coworkers,14 analyzing the benefits of blended learning in spinal surgery training, concluded that it was very valuable in terms of cost for spine surgeons with limited time due to intensive work.
Based on these, the research question that originated the present study was whether blended learning may apply to specific domains of spinal surgery (such as deformity) and whether its efficacy is assessable.
Materials and Method
The study participants consist of orthopedic surgeons and neurosurgeons who are members of the Turkish Spine Society. An open invitation was placed on the email groups of Spine Society, orthopedic and neurosurgeons inviting participants to register for the course, which included the mandatory needs assessment (NA) and a quiz to be taken for completion. Thirty-three participants who took the quiz and filled the NA form were admitted to the course and constitute the population of this study.
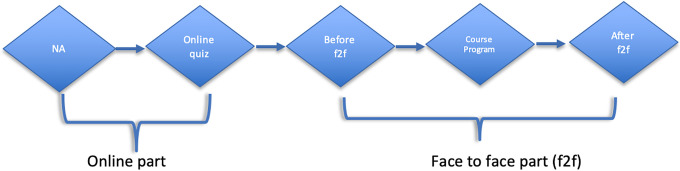
A blended pediatric spine deformity course program (Figure 1) was designed according to the NA survey of participants.
Figure 1.
Demonstrative flow chart of study design. NA, needs assessment; F2F, face-to-face.
First, the topics to be covered and faculty members were decided (by EA and AS). Then, 2 or 3 learning outcomes (LOs) were generated for each topic under the assistance and supervision of the medical educator members of the team (IB and OC). This step was followed by the development of a modified NA questionnaire and a quiz. The difference between how the health care problem is currently being addressed, in general, and how it should be addressed is called a general NA.15 The LOs were shared with the participants and the questions were asked for each outcome 2 weeks before the beginning of the actual course. The NA was based on the LO and 3 questions to be marked by the participants on an analogue scale basis from 0 to 10 (from none to perfect), with 0.5 increments, were asked
How do you rate your current level on this LO? (Current status)
How do you rate your desired level on this LO? (Expectation)
How do you rate the likelihood of using your learning on this LO in your practice? (Activity)
The course program and content were revised according to the responses received from the candidates. The difference between questions 2 and 1 was accepted as “Learning Gap” (Table 1).
Table 1.
Distribution of Learning Gap Scores.
| Questions (n = 33) | Median (Min-Max) |
|---|---|
| 1 | 5.0 (−1 to 9) |
| 2 | 4 (−1 to 8) |
| 3 | 4 (0-8) |
| 4 | 4 (0-9) |
| 5 | 5 (0-8) |
| 6 | 4 (−1 to 8) |
Following this assessment, participants (n = 33) were exposed to the online part covering the theoretical curriculum of the course at the first stage. This part includes lectures on fundamental knowledge, links to important open access papers on these topics, and videos for basic surgical techniques. The course was then complemented by face-to-face (F2F) part at the end. This part mainly focused on case-based discussions for every single topic.
For the quiz, faculty members assigned to specific topics were instructed to prepare 2 questions (multiple-choice or card opening) per the LO relevant to that topic. These questions were then pooled and entered into a blueprint table based on the LO and difficulty (assessed by the faculty members). Based on this blueprint, a quiz consisting of 10 questions (2 for 4 topics, 1 for 2 topics), 6 of which were classified as difficult was constructed. Of the 10 questions, 8 were multiple choice whereas 2 were card opening questions.
A learning management system (LMS) developed by the authors (EA, AS, BS) based on a Moodle (Modular Object-Oriented Dynamic Learning Environment; HQ, version 3.0) was used as the educational framework for the online part of the course.
Online Part
The online section of this course took 3 weeks. Within this period, participants had access to the course content online, which included PowerPoint presentations with or without voice-over records, video lectures, operation videos, supplementary text, and scientific articles related to the topics presented. Moreover, participants were also encouraged to participate in a discussion forum, which was specifically created for this course and facilitated by the faculty. Practically, after allowing for some time to the participants to study the learning objects for the specified week and topics, faculty members provoked the participants on this forum by open-ended questions or small practical assignments (such as classifying scoliosis cases and sharing with the group). Every topic of the course is designed in such a way that on completion, a set of LO is satisfied. These LO were listed at the beginning of each topic so that a participant can know what to expect from that section. Participants, as well as the faculty, were monitored for their active participation in this part of the course by 2 mechanisms. First, faculty members were presented with information on the login times of the participants (and other faculty members) so that they were aware of the amount of participation by individuals; and second, by a discussion forum facilitated by faculty that encouraged and promoted peer discussion in the learner group. One week after completion of the online part of the course, participants were asked to fill in the quiz and the NA again before proceeding with the F2F part.
Face-to-Face Part
Attending to the online part of the course was a prerequisite for the F2F part. Among those eligible, 13 attended this part and were divided into 3 groups, each of which was supervised by a faculty member, who was there to facilitate and maintain the discussions. The F2F part consisted only of case discussions, 1 case per topic, 1 hour per case. This hour was divided into parts of:
Presentation of the case (by faculty) and questions: 10 minutes
Discussion of the case within groups: 15 minutes
Discussion of the case and solutions of the groups by all participants/faculty: 20 minutes
Case solution (by faculty) and discussion of the solution: 10 minutes
Reflection: 5 minutes
During the discussions, participants were able to exchange their ideas regarding the cases with each other and learn about the experiences of their peers and faculty to arrive at a conclusion(s) as to what to do regarding each particular case. After the discussions, each group nominated a spokesman to communicate the decisions of that particular group to other groups, which later did the same. After these discussions were over, the faculty member who had presented the case presented his/her solution, which was also was discussed by the participants. In the end, participants were asked to prepare a question or 2 to 3 tweets on what they have learned during the case as a means of reflection. At the end of the day, after all the cases were presented and discussed, participants were asked to take the same quiz and NA before the course was adjourned.
Participants were also asked to complete the quiz and NA at the end of the third month after the course as objective and self-assessed measures of retention of knowledge but as only 3 of them had responded to that invitation, the results at that time point were not included in the analysis. Results of quiz questions at other time points (ie, enrollment, end of online, end of F2F) were analyzed using Student’s t test for variations between time points.
Statistical Analyses
Statistical analyses were performed using the SPSS software version 20. The variables were investigated whether or not they were normally distributed by using Kolmogorov-Smirnov/Shapiro-Wilk test. Descriptive analyses were presented using means and standard deviations. When investigating the changes in quiz scores, repeated-measures analysis of variance was used. A P value <.05 was accepted as statistically significant.
Results
The first week of the online part included four lectures with voice-overs and a technique video on fundamental topics about pediatric spine deformity. The second and third weeks contained 7 lectures about different topics of pediatric spine deformity. The F2F part involved 6 case discussions related to online topics.
Although the learning analytics data on login times was too scattered to provide concrete conclusions, in general, it was the active participant who had spent more time on the online learning part and engaged in the discussion forum who had participated in the F2F part. Discussion forum was used by the faculty and participants for 18 separate discussion chains (12 by participants and 6 by faculty), which generated 34 replies. Faculty members were active in these forums, the last entry to 16/18 chains were by faculty members.
For the analysis of efficacy in learning, quiz scores of the participants were compared. The scores of the quizzes are presented in Table 2.
Table 2.
Comparison of Quiz Scores.
| Online (n = 33) | Before Face-to-Face (n = 13) | After Face-to-Face (n = 12) | P a | |
|---|---|---|---|---|
| Quiz scores, mean +SD (min-max) | 5.9 ± 2.3 (1.6-9.2) | 6.8 ± 1.6 (4.2-9.6) | 7.9 ± 0.8 (6.8-8.9) | .004 |
a Repeated-measures analysis of variance.
The quiz score after F2F is significantly higher than the other scores (P = .004).
Discussion
This study demonstrated that a blended learning model may be applicable to improve learning in a domain of spinal surgery, pediatric deformity. Based on our results, it was also seen that the F2F part of the model made a significant change in quiz scores. On the other hand, our study failed to demonstrate the sustainability of this improved learning due to a lack of participation by the trainees in the follow-up assessment.
Although blended learning is a fairly widely used methodology in most fields of medicine and specifically surgery, this usage is not supported by empirical data on its feasibility and efficacy. There are very few reports available in this context.5,7-15 Our results are in line with the available literature in that blended learning (and potentially other forms of online learning) is an effective means of achieving and to some extent assessing (albeit summative in our study) learning by participants. Education literature proposes several mechanisms/reasons behind this favorable result. First, blended learning allows for the use of time dedicated to education more effectively. This is a problem especially in departments of surgery because of the clinical and surgical workload expected from learners, leaving limited time for education during hospital time. Therefore, transferring a substantial portion of learning to outside hospital time makes more sense. Second, blended learning (or flipped classroom) model has the potential of achieving better results by reducing failure rates,16 probably due to the spaced delivery of content (read or watch first and discuss shortly after) which affords more effective reflection17 and/or increased teacher and learner enthusiasm and active participation.
In this regard, it needs to be noted that the blended learning model presented in this article is a step ahead of what is understood by a flipped classroom. A flipped classroom usually refers to a model in which the learners are presented with the learning materials before they even enter the classroom. Therefore, theoretically, much of the theoretical knowledge is acquired beforehand, allowing more time for teacher-learner interaction in the classroom (or F2F part of a course). Even though this is a model with many advantages, it also possesses 2 major interrelated weaknesses: (a) as the learners are not supervised during their studies away from the classroom, the ability of the teachers to assess learning at this stage is limited and (b) for the same reason, the ability of teachers to provide guidance and support to the learners is also limited. Therefore, the online studies part of this model becomes its weakest link. The model used and described in this study is an adaptation of the methodology and the LMS used by the Open University UK (Milton Keynes, UK) which enables the teachers (faculty) to intervene with the learners during their studies away from the classroom so that learners are encouraged to study more, to discuss more and to reflect more.
In addition, blended learning affords the teachers with the capability of learning analytics to varying extents. Learning analytics was used in our study retrospectively (ie, not as a means of immediate feedback on the studies of learners) but still provided some insight into the learning by participants. Learning analytics may be used differently and more effectively in future courses, especially when a certification of learning is at stake, for the prediction of under-achieving students.18
Another advantage of blended learning is that the online content may be presented in any form, such as blogs, journal articles, podcasts, videos, and from any source, not limited to the faculty pool of the existing unit. Thereby, our learners were exposed to different formats as well as views, establishing a broader knowledge base. F2F sessions were then utilized for case discussions and reflection on learning. In this way, we have supplemented the transfer of know-how and know-what by know-where, in accordance with Siemens.19
This study has several shortcomings. First, the number of learners decreased considerably from the time of enrollment to F2F part to follow-up in the third month. This needs to be acknowledged as a major problem but nevertheless, is not unique to our course and study. This is one of the major problems associated with online learning in general.20 In this regard, our dropout rate is not significantly different from the general rate of online courses (except for the follow-up rate). The second major shortcoming is the lack of follow-up information on how much of the learning achieved during the educational activity had been retained. This is closely interlinked with the dropout rate discussed above, and at the present time, the authors of this study are not aware of any solutions to this problem. Finally, another shortcoming would be the methodology used for assessment, that is, it’s being confined to summative assessment by way of a quiz. Although the methodology used for the preparation of the quiz was meticulous, we need to acknowledge that this is a shortcoming but at the time this study was conducted, it was the only measure available with us to perform a standardized assessment of learning. In this context, studies on standardized assessment rubrics are needed.
In conclusion, the current study has demonstrated that an interactive blended learning format is feasible and effective in training for a surgical domain, pediatric deformity in this specific context. Blended learning provided many advantages along with several disadvantages. Future work to overcome the disadvantages, especially the dropout rates may render this format even more effective.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by a restricted research grant from REA Distance and Online Education Co Ltd.
ORCID iD: Berkay Senkoylu, BSc  https://orcid.org/0000-0001-5125-2329
https://orcid.org/0000-0001-5125-2329
Emre Acaroglu, MD  https://orcid.org/0000-0002-8163-2944
https://orcid.org/0000-0002-8163-2944
References
- 1. Herbert C, Velan GM, Pryor WM, Kumar RK. A model for the use of blended learning in large group teaching sessions. BMC Med Educ. 2017;17:197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Keifenheim KE, Velten-Schurian K, Fahse B, et al. “A change would do you good”: training medical students in Motivational Interviewing using a blended-learning approach—a pilot evaluation. Patient Educ Couns. 2019;102:663–669. [DOI] [PubMed] [Google Scholar]
- 3. Gray K, Tobin J. Introducing an online community into a clinical education setting: A pilot study of student and staff engagement and outcomes using blended learning. BMC Med Educ. 2010;10:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rowe M, Frantz J, Bozalek V. The role of blended learning in the clinical education of healthcare students: a systematic review. Med Teach. 2012;34:e216–e221. [DOI] [PubMed] [Google Scholar]
- 5. Kassab SE, Al-Shafei AI, Salem AH, Otoom S. Relationships between the quality of blended learning experience, self-regulated learning, and academic achievement of medical students: a path analysis. Adv Med Educ Pract. 2015;6:27–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Makhdoom N, Khoshhal KI, Algaidi S, Heissam K, Zolaly MA. “Blended learning” as an effective teaching and learning strategy in clinical medicine: a comparative cross-sectional university-based study. J Taibah Univ Med Sci. 2013;8:12–17. doi:10.1016/j.jtumed.2013.01.002 [Google Scholar]
- 7. Lewin LO, Singh M, Bateman BL, Glover PB. Improving education in primary care: development of an online curriculum using the blended learning model. BMC Med Educ. 2009;9:33 doi:10.1186/1472-6920-9-33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Duque G, Demontiero O, Whereat S, et al. Evaluation of a blended learning model in geriatric medicine: a successful learning experience for medical students. Australas J Ageing. 2013;32:103–109. [DOI] [PubMed] [Google Scholar]
- 9. Protsiv M, Rosales-Klintz S, Bwanga F, Zwarenstein M, Atkins S. Blended learning across universities in a South–North–South collaboration: a case study. Health Res Policy Syst. 2016;14:67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Karamizadeh Z, Zarifsanayei N, Faghihi AA, Mohammadi H, Habibi M. The study of effectiveness of blended learning approach for medical training courses. Iran Red Crescent Med J. 2012;14:41–44. [PMC free article] [PubMed] [Google Scholar]
- 11. Bock A, Modabber A, Kniha K, Lemos M, Rafai N, Hölzle F. Blended learning modules for lectures on oral and maxillofacial surgery. Br J Oral Maxillofac Surg. 2018;56956–961. [DOI] [PubMed] [Google Scholar]
- 12. Ali-Masri H, Hassan S, Fosse E, et al. Impact of electronic and blended learning programs for manual perineal support on incidence of obstetric anal sphincter injuries: a prospective interventional study. BMC Med Educ. 2018;18:258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Munro V, Morello A, Oster C, et al. E-learning for self-management support: introducing blended learning for graduate students—a cohort study. BMC Med Educ. 2018;18:219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gunzburg R, Szpalski M, Lamartina C. Postgraduate education in spine surgery: the blended online learning concept. Eur Spine J. 2018;27:2059–2061. [DOI] [PubMed] [Google Scholar]
- 15. Thomas PA, Kern DE, Hughes MT, Chen BY. Curriculum Development for Medical Education: A Six-Step Approach. 2nd ed Baltimore, MD: Johns Hopkins University Press; 2016:12. [Google Scholar]
- 16. Sharples M, Adams A, Ferguson R, et al. Innovating Pedagogy 2014: Open University Innovation Report 3. Milton Keynes, England: Open University; 2014. [Google Scholar]
- 17. Ferguson R, Barzilai S, Ben-Zvi D, et al. Innovating Pedagogy 2017: Open University Innovation Report 6. Milton Keynes, England: Open University; 2017. [Google Scholar]
- 18. Saqr M, Fors U, Tedre M. How learning analytics can early predict under-achieving students in a blended medical education course. Med Teach. 2017;39:757–767. [DOI] [PubMed] [Google Scholar]
- 19. Siemens G. Connectivism: a learning theory for the digital age. http://er.dut.ac.za/bitstream/handle/123456789/69/Siemens_2005_Connectivism_A_learning_theory_for_the_digital_age.pdf. Published January 2005. Accessed February 22, 2018.
- 20. Bawa P. Retention in online courses: exploring issues and solutions—a literature review. SAGE Open. 2016;6 doi:10.1177/2158244015621777 [Google Scholar]