Abstract
Aim
To describe diabetes nurses' perspectives on the impact of the COVID‐19 pandemic on people with diabetes and diabetes services across Europe.
Methods
An online survey developed using a rapid Delphi method. The survey was translated into 17 different languages and disseminated electronically in 27 countries via national diabetes nurse networks.
Results
Survey responses from 1829 diabetes nurses were included in the analysis. The responses indicated that 28% (n = 504) and 48% (n = 873) of diabetes nurses felt the COVID‐19 pandemic had impacted ‘a lot’ on the physical and psychological risks of people with diabetes, respectively. The following clinical problems were identified as having increased ‘a lot’: anxiety 82% (n = 1486); diabetes distress 65% (n = 1189); depression 49% (n = 893); acute hyperglycaemia 39% (n = 710) and foot complications 18% (n = 323). Forty‐seven percent (n = 771) of respondents identified that the level of care provided to people with diabetes had declined either extremely or quite severely. Self‐management support, diabetes education and psychological support were rated by diabetes nurse respondents as having declined extremely or quite severely during the COVID‐19 pandemic by 31% (n = 499), 63% (n = 1,027) and 34% (n = 551), respectively.
Conclusion
The findings show that diabetes nurses across Europe have seen significant increases in both physical and psychological problems in their patient populations during COVID‐19. The data also show that clinical diabetes services have been significantly disrupted. As the COVID‐19 situation continues, we need to adapt care systems with some urgency to minimise the impact of the pandemic on the diabetes population.
Keywords: COVID‐19, diabetes care provision, physical and psychological health
Novelty Statement.
What is known?
COVID‐19 has increased health hazards for people with diabetes.
What are the new findings?
Diabetes nurses reported increases in the physical health risks of people with diabetes, including acute hyperglycaemia, hospital admissions and foot complications.
Diabetes nurses reported large increases in the psychological health risks of people with diabetes, particularly depression, anxiety and diabetes distress.
Diabetes nurses reported severe disruption to diabetes services during the COVID‐19 pandemic.
Implications for clinical practice?
The clinical priority is to pool learning in respect of strategies for optimising care delivery during the COVID‐19 pandemic to maintain support for people with diabetes.
1. INTRODUCTION
Coronavirus disease 2019 (COVID‐19), caused by the severe acute respiratory syndrome‐coronavirus‐2 (SARS‐CoV‐2), presents a significant global health hazard. 1 People with diabetes are at increased risk of incident mortality and severe infection from COVID‐19 compared to those without diabetes. 2 , 3 , 4 While there are variations in risk related to diabetes type, age, co‐morbidities, ethnicity and glycaemic control, the relative risk is higher for most people with diabetes. 4 , 5 These risks are evident in the high proportion of people with diabetes in those hospitalised with COVID‐19. 6 COVID‐19 has also been associated with increased acute hyperglycaemic episodes and potentially with new onset diabetes. 7 , 8 In addition, there are limited data showing that the pandemic is having a negative impact on the psychological well‐being of people with diabetes. 9 Hence, we urgently need more information on how the pandemic is impacting on the diabetes population, in relation to both their physical and psychological health.
It is concerning that during this time of heightened need among the diabetes population, the COVID‐19 pandemic is also impacting on routine diabetes care delivery. Diabetes is a complex chronic condition and people living with diabetes require ongoing support from inter‐disciplinary diabetes services. The COVID‐19 pandemic has disrupted diabetes care provision in two ways: first, the social isolation measures have reduced access to routine diabetes appointments, education and screening; and second, many diabetes professionals have been redeployed to acute medical services to help with the high volume of acutely ill patients. This disruption means that people with diabetes may not be able to access the medical and self‐management support they require in reducing their risk of diabetes complications. In addition, the reduced capacity of services may also mean that many of the more acute needs of people with diabetes during the crisis are going unmet. Again, it is important that we gain insights into the extent of this disruption to services and identify strategies that may help address the current challenges and short falls in provision.
To help address these knowledge deficits, we have undertaken a pan‐European survey of diabetes nurses focussing on the impact of COVID‐19 on people with diabetes and diabetes services. The diabetes nurses workforce makes a major contribution to the care of people living with diabetes across Europe, and as such, they have significant oversight of how COVID‐19 has impacted on the diabetes population and care delivery in their clinical areas.
2. STUDY METHODS
2.1. Survey design
We undertook a cross‐sectional survey of diabetes nurses from across Europe using an electronic questionnaire, distributed through diabetes nurses' networks. The survey was designed to give a qualitative perspective on how the COVID‐19 crisis was impacting on people with diabetes and services in different countries across Europe, from the perspective of the diabetes nurses in those countries. The study received ethical approval from the King's College London ethics committee (REF. MRA‐19/20‐19221), some countries also obtained local approval.
2.2. Survey aim and objectives
The aim of the survey was to identify diabetes nurses' perspectives on the impact of the COVID‐19 pandemic on people with diabetes and diabetes services across Europe. In this initial report on the survey findings, we present data addressing the following objectives:
Generate information on how COVID‐19 has impacted on people with diabetes (acute illness presentations, diabetes emergencies, physical and mental health).
Identify how COVID‐19 has affected routine diabetes care (patient appointments, self‐management support, diabetes education and psychological support).
2.3. Questionnaire design and content
The questionnaire was designed to address the survey objectives using a rapid Delphi method to ensure content validity and that the questionnaire was meaningful to diabetes nurses from across Europe. The Delphi panel included diabetes nurses and diabetes researchers from all the participating countries. The questionnaire was concise in design (completable within 20 minutes) reflecting the busy working context of diabetes nurses during the COVID‐19 crisis. The survey was embedded in QualtricsTM survey software and used: tick box responses to provide categorical data (e.g. yes/no responses or selecting from a list); ordinal scales (e.g. not at all, minimally, moderately, quite severely, extremely) and ranking exercises. We worked with local investigators in the participating countries to translate the questionnaire from English into the host languages required. Content fidelity was maintained using translators who were involved in the Delphi processes and had advanced English language skills. The questionnaire comprised four domains, three of which are considered here: diabetes nurses characteristics and work context; impact of COVID‐19 on the population of people with diabetes with whom they work and Impact of COVID‐19 on diabetes care delivery. The survey was piloted by diabetes nurses (n = 24) prior to distribution to assess the reliability of the online system; and the ease of and time taken to complete. It was not possible to assess the test and re‐test reliability of the survey in the limited time available for distributing the questionnaire. The approach taken in developing the questionnaire was designed to enhance the content, construct and face validity of the questionnaire, as the questionnaire sort to provide descriptive data only criterion validity was not considered.
2.4. Survey setting
The survey was conducted in 27 countries with varying populations, healthcare systems and resources, as follows: Belgium; Bosnia and Herzegovina; Croatia; Cyprus; Czechia; Denmark; Estonia; Finland; France; Germany; Greece; Ireland; Italy; Latvia; Malta; Netherlands; Norway; Poland; Portugal; Romania; Spain; Sweden; Switzerland; Turkey; Ukraine; United Kingdom (UK).
2.5. Participants and sample
Participants were diabetes nurses in the countries who agreed to participate. As the definition of a diabetes nurse may vary between countries and working contexts, the following criteria were applied, respondents should be qualified nurses with training in diabetes working with adults or children living with diabetes either in specialist, community or in‐patient settings, prior to the pandemic. While we were reliant on self‐reporting of these criteria, we considered that the risk of criteria non‐compliance was small.
The sampling was opportunistic and designed to provide a qualitative assessment of the impact of COVID‐19 on diabetes care, rather than test a generalisable hypothesis. We aimed to recruit around 20% of diabetes nurses in each of the participating countries, although monitoring this was problematic in many countries where the number of diabetes nurses is unknown. We felt that such an approach would yield sufficient descriptive data to address the study objectives.
2.6. Survey distribution
Survey distribution was from early June to July 2020, the survey was initiated in the UK first with other countries following as their translations were finalised. The survey link was disseminated via email or social media platforms to known diabetes nurse networks and other diabetes groups. To expand the reach of the survey, respondents were also asked to cascade the survey to colleagues and other professional networks. To avoid multiple submissions by one individual, responses were limited to two responses from one IP address. The length of time the survey was open in each country ranged from 4 to 6 weeks, depending when translations were completed.
2.7. Data analysis
The categorical and ordinal data captured by the survey were exported into SPSS (V26) for analysis. The data were checked for response completion rates and missing data with a minimum requirement of ≥60% data completion. A limited number of data transformations were conducted to provide categorical groupings, for example to group respondent according to which population of people with diabetes they worked with (i.e. exclusively type 1, exclusively type 2, or a mixture of type 1 and type 2 patients). Descriptive statistics (frequencies with percentages and ranks) were produced to summarise the variables observed in the data. While it was not the objective of the study to analyse between country differences, country‐level data were collated for comparative purposes to consider the level of convergence in the profile of responses across countries. The descriptive data for each country were summarised in graphs detailing the proportion of responses to the main survey questions, with the median response (inter‐quartile range) for all countries presented as an overlay for reference. Some additional analyses were performed to estimate potential biases in relation to variations in country response rates. Responses from diabetes nurses who worked exclusively with either type 1 or type 2 diabetes were also made to consider any potential differences in the nurses' perspectives of impacts on people with type 1 or type 2 diabetes. These comparisons were conducted using cross‐tabulations to compare response profiles and to test for differences (Chi‐square test).
3. RESULTS
There were 2212 responses to the survey, 383 of which were excluded as they had completed <40% of the survey questions leaving 1829 responses. Country‐level responses are summarised in Chart 1.
CHART 1.
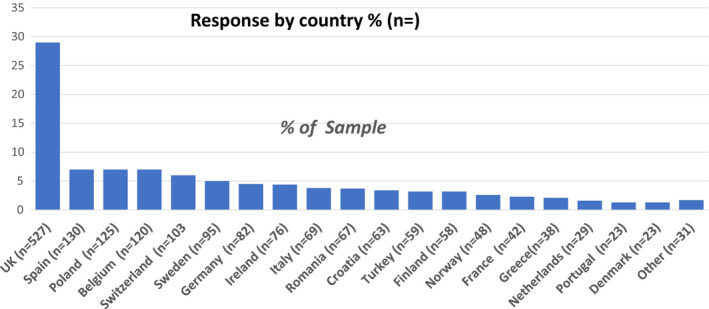
Response by country
3.1. Diabetes nurses' characteristics
All responders were registered nurses, with 27% (n = 449) and 48% (n = 779) having either a degree or post‐graduate qualification, respectively. The majority (62%, n = 1123) of respondents had worked in diabetes >8 years, and 83% (n = 1517) respondents had a diabetes qualification. In terms of patient populations worked with 54% (n = 992) indicated both type 1 and type 2 diabetes; 24% (n = 435) type 2 diabetes; 7% (n = 135) type 1 diabetes; 13% (n = 230) children and adolescents; and 2% (n = 37) were other (pregnancy and cystic fibrosis).
3.2. Survey responses
The survey responses relating to diabetes nurses perceived impact of COVID‐19 on people with diabetes are summarised in Table 1. The data show that diabetes nurses felt that the risks to the physical and psychological health of people with diabetes had increased ‘a lot’ by close to a third and a half of respondents, respectively. Psychological problems (anxiety, diabetes distress and depression) were reported to have increased the most during the COVID‐19 pandemic, although large increases in acute hyperglycaemia were reported by around a half of respondents. The data also show that diabetes nurses have seen increases in hospital admissions and new incident diabetes cases compared to their pre‐COVID‐19 experience. While the proportion of diabetes nurses reporting that foot complications had increased ‘a lot’ was comparatively small, such an increase in these high‐risk events is important.
TABLE 1.
Perceived impact of COVID‐19 on people with diabetes in the respondents clinical area
| Question topics | Responses % (n=) | ||||
|---|---|---|---|---|---|
| Level of impact of COVID‐19 on the following: | Reduced | Stayed the same | Increased | Not sure | |
| Diabetes related hospital admission | 18 (336) | 32 (584) | 29 (593) | 19 (341) | |
| Diabetic‐ketoacidosis (DKA) | 7 (121) | 46 (765) | 25 (423) | 22 (372) | |
| Hyperosmolar‐Hyperglycaemic‐state | 5 (83) | 39 (649) | 23 (377) | 33 (544) | |
| Severe‐hypoglycaemia | 10 (168) | 59 (983) | 10 (157) | 21 (352) | |
| New diabetes diagnoses | 20 (361) | 37 (674) | 31 (549) | 12 (218) | |
| Impact on patient health risks | Reduced | Stayed the same | Increased a little | Increased a lot | Not sure |
| Physical health risks | 7 (118) | 13 (237) | 47 (839) | 28 (504) | 5 (103) |
| Psychological health risks | 7 (113) | 6 (109) | 37 (667) | 48 (873) | 2 (43) |
| Clinical problems that respondents identified as having increased a lot: | Response | ||||
| Anxiety | 82 (1486) | ||||
| Diabetes distress | 65 (1189) | ||||
| Depression | 49 (893) | ||||
| Acute hyperglycaemia | 39 (710) | ||||
| Foot complications | 18 (323) | ||||
There were some variations between countries in the assessment of the level of health risks (psychological and physical) posed by the COVID‐19 pandemic to people with diabetes as shown in Chart 2. The data show that in most countries diabetes nurses perceived that the greatest increase in risk has been to the psychological health of people with diabetes, although the nurses in Croatia, Italy, Poland, Romania, Spain and Turkey reported an equivalent increase in risk for physical and psychological health.
CHART 2.
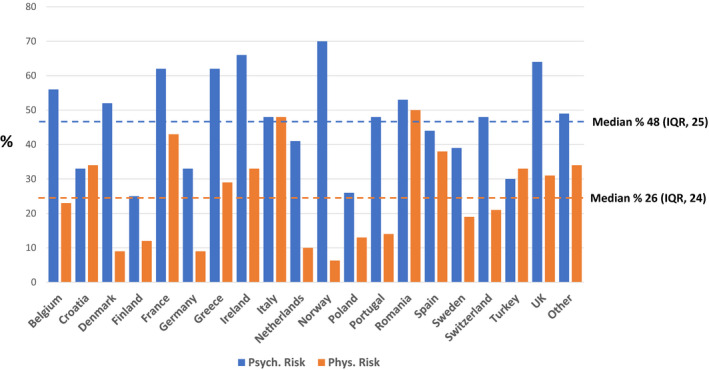
Proportion of nurses indicating increased risk to the physical and psychological health of people with diabetes* Country
The survey responses relating to the impact of COVID‐19 on diabetes services and care provision are summarised in Table 2. The diabetes nurses' responses showed that the majority have seen disruption to routine diabetes care, with 47% (n = 771) rating this as quite severe or extreme. The areas of greatest disruption where diabetes education, psychological and self‐management support with more modest disruption to diabetes technology and medicines support. Two thirds of respondents had found it necessary to prioritise care to those at highest risk of complications, the newly diagnosed, elevated glycaemia, pregnancy or diabetes events (diabetes emergencies, diabetic‐ketoacidosis [DKA], hyperosmolar hyperglycaemic State and hypoglycaemia), other prioritised groups included: older people, children, people with foot problems and those with technology issues. The data also show a change in how diabetes nurses interacted with people with diabetes with a shift towards virtual contact, this was mainly telephone although the use of video consultations had also increased. Group interactions which were the second most common method of contact pre‐COVID‐19 became the least common method.
TABLE 2.
Perceived impact of COVID‐19 on diabetes services
| Question topics | Responses % (n=) | ||||
|---|---|---|---|---|---|
| Increased a lot | Increased a little | Stayed the same | Decreased a little | Decreased a lot | |
| Level of care provided to the newly diagnosed | 4 (67) | 10 (170) | 38 (623) | 32 (532) | 15 (252) |
| Perceived level of disruption to care elements | Level of disruption | ||||
| Not at all | Minimally | Moderately | Quite severely | Extremely | |
| Overall care provision | 4 (58) | 13 (210) | 36 (588) | 34 (552) | 13 (219) |
| Self‐management support | 7 (112) | 22 (352) | 40 (647) | 24 (385) | 7 (114) |
| Diabetes education | 5 (70) | 10 (116) | 21 (352) | 35 (569) | 28 (458) |
| Technology and medicines support | 19 (315) | 29 (469) | 30 (483) | 14 (243) | 6 (100) |
| Psychological support | 11 (175) | 20 (321) | 31 (496) | 24 (394) | 10 (157) |
| Have you had to prioritise groups of patients? | Yes | No | |||
| 67 (1097) | 33 (535) | ||||
| Groups prioritised | |||||
| High‐risk patients | 22 (184) | ||||
| Newly diagnosed | 21 (180) | ||||
| Pregnancy | 20 (167) | ||||
| High glycaemic levels | 18 (150) | ||||
| Acute diabetes events | 13 (104) | ||||
| Other | 35 (295) | ||||
| Patient contact methods ranked from 1 to 5 (most to least common) | Pre‐COVID‐19 Rank | During COVID‐19 Rank | |||
| Face‐to‐face individual sessions | 1 | 3 | |||
| Group face‐to‐face sessions | 2 | 5 | |||
| Telephone contact | 3 | 1 | |||
| E‐mail | 4 | 2 | |||
| Video contact | 5 | 4 | |||
As with the nurses' assessments of the impact on people with diabetes, there were some country‐level variations in the severity of the perceived disruption to diabetes services. Chart 3 details the proposition of nurses who rated the effect of the pandemic as having an extreme or very severe negative impact on diabetes care in general and in respect of self‐management support, diabetes education, technical care and psychological care. The impact on overall care was consistent across most countries with the acceptation of Denmark where the nurses where more likely to rate impact as moderate (81%, n = 17). While overall, the level of disruption to technical care support was identified as having the lowest severity, it was higher in Romania and in the Other countries most of which were low‐income countries (Bosnia and Herzegovina, Czechia, Cyprus, Estonia, Latvia, Malta and Ukraine).
CHART 3.
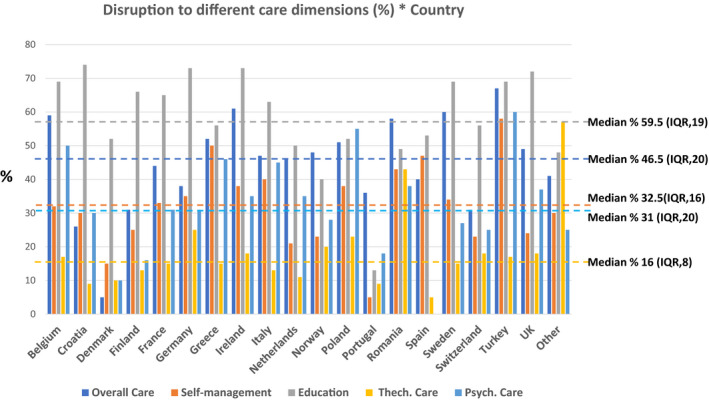
Disruption to different care dimensions (%)* Country
Additional analyses were undertaken to identify potential country biases and differences between diabetes types. In terms of countries, the largest potential for bias was the high proportion of respondents from the UK; hence, the analysis compared the UK to the responses from the other countries. While the data showed statistically significant differences (p < 0.05) in the responses from the UK and the other countries for some variables, the response profiles where generally concordant. The main differences observed where in the level of severity reported, with the UK reporting higher ratings for psychological and physical impact compared to other European countries, at 31% (n = 161) versus 27% (n = 343) for physical impact and 64% (n = 332) versus 42% (n = 541) for psychological impact in UK and European countries, respectively. In terms of impact on services, the differences were marginal, with 18% (n = 88) versus 14% (n = 164) suggesting that services had reduced ‘a lot’ during the pandemic. In analysing responses from those who worked exclusively with type 1 diabetes or type 2 diabetes, the overall rating showed that nurses working with people with type 2 diabetes felt there was more negative physical impact compared to those working with people who have type 1 diabetes, with 38% (n = 160) versus 23% (n = 30) indicating that health risks had increased a lot, respectively.
4. DISCUSSION
This survey has provided some novel and timely insights into the impact of COVID‐19 on people living with diabetes and diabetes services across Europe. Overall the data suggest that the pandemic has negatively impacted on the physical and psychological health risks of people with diabetes, with reported increases, in acute diabetes events, new diagnoses, and anxiety, diabetes distress and depression. The survey has also revealed significant disruption to routine diabetes care, particularly in relation to self‐management and psychological support. This disruption may have both short‐ and longer‐term consequences. To our knowledge, this is the first study to provide an assessment of the impact of COVID‐19 exclusively on people with diabetes in Europe, from the experiences of diabetes health professionals. There has been two previous global surveys: one undertaken in paediatrics by the International Society for Pediatric and Adolescent Diabetes (ISPAD), with responses from 215 centres 10 ; and the other was a survey of health professionals (n = 202) working in chronic disease (including diabetes). 11 The ISPAD survey concurred with our findings reporting a shift towards virtual consultation and an increased incidence of DKA. Similarly, the other survey reported a shift to virtual consultations, a disruption to care provision and increases in mental health issues.
In relation to the physical health risks and problems identified by the diabetes nurses, the data are generally concordant with patient‐level studies which show increases in hospitalisation; hyperglycaemia and ketosis; and incident diabetes cases. 4 , 6 , 7 While this study was not designed to consider differences in the impact of COVID‐19 by types of diabetes, the diabetes nurses who worked exclusively with people who have type 2 diabetes tended to rate the physical impact of the disease more highly. Although the diabetes nurses also reported increased risks in all groups of people with diabetes, reflecting the findings of recent epidemiological studies. 4 , 5 A worrying finding was that 18% of the respondents reported an increase in foot problems. While this was relatively small number of diabetes nurses compared to other problems, given the potential consequences and costs of foot complications further data are required to confirm the extent of this problem; as recent reports have emphasised the risk of foot complications increasing during the pandemic and the challenges of delivering foot care (with physical examination and intervention being an integral element of foot care). 12 , 13
The psychological health impacts reported by the survey respondents are of particular concern, as there is already a higher background level of psychological morbidity in the diabetes population. Our data indicated that across Europe the majority of diabetes nurses reported increased levels of anxiety, distress and depression in their patient populations. While data on the psychological impact of the COVID‐19 pandemic are limited, our findings reflect those reported in a large survey (n = 1396) of Danish people with diabetes showing increased levels of health anxiety in relation to the pandemic. 9 These findings are of heightened concern, as the survey responses also indicated a reduced capacity in the provision of psychological support. Hence, finding strategies for identifying and reducing the anxiety and distress caused by the pandemic in people with diabetes should be a priority for diabetes services.
Worryingly, at this time of heightened need for people with diabetes, the survey also showed that diabetes care provision has been significantly disrupted during the pandemic, most notably in relation to diabetes self‐management support. The impact on group education is a major concern, as it may mean that many newly diagnosed or those with established diabetes may experience delays in accessing structured education programmes. While the impact on technology and medicines support was rated less severely, without adequate self‐management support the potential benefits of these technologies may be compromised. Therefore, we need to learn from the experiences of teams in different care context in managing and adapting to the ongoing COVID‐19 situation to enhance the current COVID‐19 diabetes guidelines. 14 , 15 In a subsequent paper, we will report on what strategies diabetes nurses and the teams they work in, have been using to meet the challenges of this pandemic to provide further guidance on how we can adapt our working practices and services to ameliorate the impact of COVID‐10 on people with diabetes.
Finally, the survey also showed a large increase in virtual contact with people with diabetes (telephone, e‐mail and video consultations). While telemedicine approaches have been used effectively in diabetes care delivery, 16 their introduction during this crisis was born of necessity without preparation (for health professionals or people with diabetes) and it is unclear what impact this rapid transition will have on diabetes outcomes or the future adoption of telemedicine in routine diabetes care. A recent international survey of people with diabetes (n = 7477), assessing their views on telemedicine experiences was encouraging in this regard, reporting that the majority of the 28% respondents who experienced virtual consultations (telephone, 72%; video calls, 28%) found these appointments useful. 17 They also reported that three quarters plan to use virtual appointments in the future. Hence, while the COVID‐19 pandemic may lead to significant changes in care delivery, it will be important to consider this carefully and ensure good accessibility and preparation for professionals and people with diabetes in using these media. Virtual consultations should also be considered in respect of their impact on patient outcomes.
4.1. Survey limitations
This was a pragmatic qualitative survey designed to give a general description of the impact of the COVID‐18 pandemic on people with diabetes and services, across Europe based on diabetes nurses' experiences. As such, it was not designed to provide a quantifiable metric on the impact of the pandemic, rather to identify potential care deficits and health impacts in the diabetes population. Despite this limitation, we feel that the data have provide some useful insights into the problems being experienced by people with diabetes across Europe and the levels of disruption to diabetes care provision. While we emphasise that this is limited to the experiences of diabetes nurses, we are confident that as key members of diabetes teams with frequent contact with the people with diabetes in those services, the data provide a reasonable representation of the impact of the pandemic. Diabetes nurses also have the advantage of having particular insights into the provision of self‐management support, diabetes education and psychological support.
As with all surveys, there are also a number of more specific limitations to consider, and in respect of this study: challenges to the validity of the questionnaire content and translation; sampling bias; the response bias between countries and item completion (missing data). In relation to the questionnaire, the challenge was to identify questions that would enable us to assess impact on people with diabetes and services in a way that would be meaningful to countries with different healthcare context and across languages. As it was necessary to develop and disseminate the survey rapidly during the pandemic, it is possible that potentially important questions were omitted. To address this challenge, we used a wide pool of experts in the Delphi process to enhance content validity, and reduced inconsistencies in the meaning of questions across languages by using those involved in developing the questionnaire in the translations. In respect of the sampling bias, it was not possible to systematically characterise the population of diabetes nurses in all the participating countries. Indeed, such data are not available in many countries and the number of diabetes nurses are very variable in different countries. Therefore, this could have introduced a response bias in that only nurses who are linked to particular professional networks participated. A further limitation is that we could not assess the reach of the survey in each country without knowing the total population. While the overall response to survey was reasonable, we cannot say that the responses from each country were fully representative. The country‐level variations in diabetes nurse numbers reflect the size of the participating country; the prominence of the diabetes nurse role in those countries and the level of membership in the networks we targeted (although lateral cascade was also encouraged to expand the reach of the survey). However, as the objective of the survey was to provide a general picture of impact of the pandemic on people with diabetes and diabetes services, the overall convergence of country‐level perspectives suggests that at descriptive level the results achieved this objective. To address the potential response bias between countries, particularly the large UK response, we compared responses from the UK to the other countries. While this analysis indicted some differences between diabetes nurses from the UK (where the response was larger) and the other European states, descriptively the trends were again consistent. Finally, we must consider item completion and missing data. Overall item completion was extremely high with 89% (n = 1631) of respondents achieving 100% completion. The lowest level of item completion was 40%–60% of items. While this was a very small proportion of the sample <9% (n = 163), there was a discrepancy in that these respondents completed the questions on the impact on people with diabetes but not on services. Hence, there was a small discrepancy in terms of the number of respondents to each section, although any significant level of bias given the descriptive nature of survey is unlikely.
5. CONCLUSION
The survey shows that diabetes nurses across Europe report significant increases in both physical and psychological problems in their patient populations during COVID‐19. The data also show that clinical diabetes services have been highly disrupted. As the COVID‐19 situation continues, we need to adapt care systems with some urgency to minimise the impact of the pandemic on the diabetes population.
CONFLICT OF INTEREST
None.
ACKNOWLEDGEMENTS
The authors also thank the Foundation of European Nurses in Diabetes (FEND) for funding this study.
The authors would like to thank the following consortium members who contributed to this survey: Maya Allen‐Taylor, Freya Browne, Aycan Celick, Sarah Gane, Rabab Hashem, Hellena Habete‐Asres, Qinxiu Tian, Jackie Sturt, Kirsty Winkley—King's College London. Rudi Caron (Belgium), Snježana Gaćina (Croatia), Yvonne Moloney (Ireland), Ewa Kobos (Poland), Margarida Jansà (Spain) and Carmen Yoldi (Spain).
Contributor Information
Rita Forde, Email: rita.forde@kcl.ac.uk.
the FEND COVID‐19 consortium:
Maya Allen‐Taylor, Freya Brown, Aycan Celick, Sarah Gane, Rabab Hashem, Hellena Habete‐Asres, Qinxiu Tian, Jackie Sturt, Kirsty Winkley, Rudi Caron, Snježana Gaćina, Yvonne Moloney, Ewa Kobos, Margarida Jansà, and Carmen Yoldi
REFERENCES
- 1. Guan W‐J, Ni Z‐Y, Hu YU, et al. For the China Medical Treatment Expert Group for Covid‐19. Clinical characteristics of coronavirus disease 2019 in China. N Eng J Med. 2020;382(18):1708‐1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hussain A, Bhowmik B, do Vale Moreira NC. COVID‐19 and diabetes: knowledge in progress. Diabetes Res Clin Pract. 2020;162:108142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Remuzzi A, Remuzzi G. COVID‐19 and Italy: what next? Lancet. 2020;395:1225‐1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Holman N, Knighton P, Kar P, et al. Risk factors for COVID‐19‐related mortality in people with type 1 and type 2 diabetes in England: a population‐based cohort study. Lancet Diabetes Endocrinol. 2020;8(10):823‐833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Apicella M, Campopiano MC, Mantuano M, Mazoni L, Coppelli A, Del Prato S. COVID‐19 in people with diabetes: understanding the reasons for worse outcomes. Lancet Diabetes Endocrinol. 2020;8(9):782‐792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Docherty AB, Harrison EM, Green CA, et al. Features of 16,749 hospitalised UK patients with COVID‐19 using the ISARIC WHO Clinical Characterisation Protocol. medRxiv. 2020;2020.04.23.20076042. [Google Scholar]
- 7. Li J, Wang X, Chen J, Zuo X, Zhang H, Deng A. COVID‐19 infection may cause ketosis and ketoacidosis. Diabetes Obes Metab. 2020;22(10):1935‐1941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rubino F, Amiel SA, Zimmet P, et al. New‐onset diabetes in Covid‐19. New Engl J Med. 2020;383(8):789‐790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Joensen LE, Madsen KP, Holm L, et al. Diabetes and COVID‐19: psychosocial consequences of the COVID‐19 pandemic in people with diabetes in Denmark—what characterizes people with high levels ofCOVID‐19‐related worries? Diabet Med. 2020;37:1146‐1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Elbarbary NS, dos Santos TJ, de Beaufort C, Agwu JC, Calliari LE, Scaramuzza AE. COVID‐19 outbreak and pediatric diabetes: Perceptions of health care professionals worldwide. Pediatr Diabetes. 2020;21(7):1083‐1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chudasama YV, Gillies CL, Zaccardi F, et al. Impact of COVID‐19 on routine care for chronic diseases: a global survey of views from healthcare professionals. Diabetes Metab Syndr. 2020;14:965‐967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kyrou I, Robbins T, Randeva HS. COVID‐19 and diabetes: no time to drag our feet during an untimely pandemic. J Diabetes Complications. 2020;34(9):107621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Shin L, Bowling FL, Armstrong DG, Boulton AJM. Saving the diabetic foot during the COVID‐19 pandemic: a tale of two cities. Diabetes Care. 2020;43(8):1704‐1709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bornstein SR, Rubino F, Khunti K, et al. Practical recommendations for the management of diabetes in patients with COVID‐19. Lancet Diabetes Endocrinol. 2020;8(6):546‐550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rayman G, Lumb A, Kennon B, et al. Guidelines for the management of diabetes services and patients during the COVID‐19 pandemic. Diabet Med. 2020;37(7):1087‐1089. [DOI] [PubMed] [Google Scholar]
- 16. Tchero H, Kangambega P, Briatte C, Brunet‐Houdard S, Retali G‐R, Rusch E. Clinical effectiveness of telemedicine in diabetes mellitus: a meta‐analysis of 42 randomized controlled trials. Telemed J E Health. 2019;25(7):569‐583. [DOI] [PubMed] [Google Scholar]
- 17. Wu C, Wu Z, Yang L, et al. Evaluation of the clinical outcomes of telehealth for managing diabetes: a PRISMA‐compliant meta‐analysis. Medicine (Baltimore). 2018;97(43):e12962. [DOI] [PMC free article] [PubMed] [Google Scholar]


