Abstract
Objective
To investigate the perception of self‐isolation at home in patients with cancer during the lockdown period resulting from the COVID‐19 outbreak in Italy.
Methods
A cross‐sectional descriptive study was conducted through an online survey of patients with cancer who were sheltering at home from 29th March to 3rd May 2020. Perception of self‐isolation was assessed using the ISOLA scale, after evaluation of its psychometric properties. Content analysis was used to analyse two open‐ended questions.
Results
The participants were 195 adult patients with cancer (female = 76%; mean age = 50.3 ± 11.2; haematological malignancy = 51.3%). They reported moderate isolation‐related suffering (M = 2.64 ± 0.81), problems in their relationships with others (M = 3.31 ± 1.13) and difficulties in their relationships with themselves (M = 3.14 ± 1.06). Patients who experienced significantly more social problems were older, had less education and were living without minor children. Overall, four main categories emerged from the qualitative content analysis: (1) lack of freedom and social life, (2) uncertainty and worries, (3) feeling supported and (4) dealing with isolation.
Conclusion
Living with cancer in the COVID‐19 pandemic was often perceived as an isolating experience, primarily in terms of detachment from loved ones.
Keywords: COVID‐19, delivery of health care, loneliness, neoplasms, patient isolation
1. INTRODUCTION
After China (Wang, Pan, et al., 2020), Italy was the second country to be involved in the COVID‐19 pandemic, and it had one of the highest death tolls (ISS, 2020; Remuzzi & Remuzzi, 2020). The World Health Organization (WHO) recommended preventive actions to reduce transmission of the SARS‐CoV‐2 virus, and these actions included appropriate hand hygiene and social distancing (WHO, 2020). On 9th March 2020, the Italian government implemented extraordinary measures to contain the spread of COVID‐19 (Lazzerini & Putoto, 2020). Lockdown was enforced on all citizens, except in circumstances of necessity, for work in essential services, and for health reasons (Sjödin et al., 2020). More restrictive containment measures, the so‐called ‘Phase One’ of the COVID‐19 emergency plan, were implemented from 9th March until 4th May (Italian Ministry of Health, 2020). This required people to shelter at home and led to a substantial behavioural change in terms of hygiene and social practices within the community.
Among people at higher risk, patients with cancer were indicated as more vulnerable to both the SARS‐CoV‐2 infection (Richardson et al., 2020; Yu et al., 2020) and its complications (Emami et al., 2020; Liang et al., 2020; Onder et al., 2020; Passamonti et al., 2020). Thus, the request to stay at home in self‐isolation was to be read not only as a restrictive measure but also as a protective recommendation (ESMO, 2020; NCCN, 2020). Despite the efforts made by oncology clinicians to provide cancer treatment safely in the face of uncertainty and rapid change (Cinar et al., 2020; Combs et al., 2020; Meattini et al., 2020; Russano et al., 2020; Trapani et al., 2020; Ueda et al., 2020; Valenza et al., 2020), cancer patients and survivors, especially those travelling to receive care, had to face various challenges in accessing healthcare services (ACV, 2020; Chan et al., 2020).
In the context of grave threats to their physical and mental health (Stefana et al., 2020; Vigo et al., 2020), people living with cancer had to cope with various stressors, including fear of SARS‐CoV‐2 infection, inadequate supplies, scarcity of information, financial loss, stigma and constrained freedom (Brooks et al., 2020). The psychological impact of a lockdown in the context of a pandemic, in terms of stress, anxiety, depression and poor sleep quality (Casagrande et al., 2020; Rubin & Wessely, 2020; Wang, Pan, et al., 2020; Wang, Hu, et al., 2020), as well as isolation‐related loneliness (Brooks et al., 2020; Hawryluck et al., 2004), could be even worse for patients with cancer, who need emotional support from others to alleviate their feelings of loneliness and maintain good mental health (Adams et al., 2016; Secinti et al., 2019). Although the restrictive measures were essential to reduce the spread of the virus, they may have had severe psychosocial consequences for people living with cancer.
When isolation is forced on patients with cancer to protect them from infection, it may often be experienced as a shield to create an effective defence (Biagioli, Piredda, Annibali, et al., 2017) but can still lead to psychological suffering (Biagioli et al., 2016). Similarly, stay‐at‐home ordinances have been proved to be effective at containing the spread of a novel coronavirus, but prolonged self‐isolation at home may have substantial negative implications (Brooks et al., 2020) and may jeopardise people's health (Lippi et al., 2020). Thus, describing how people living with cancer experienced self‐isolation at home during the lockdown in Italy may help health professionals to obtain a more complete picture of the cancer experience during the COVID‐19 emergency, from the patient perspective. Therefore, this study aimed to investigate the perception of self‐isolation at home in people living with cancer during the lockdown in Italy for COVID‐19.
2. METHODS
2.1. Design and participants
This is a cross‐sectional descriptive study of cancer patients’ perceptions of self‐isolation at home in the context of the COVID‐19 emergency. Data were collected through an online survey from 29th March to 3rd May 2020, which corresponds to ‘Phase One’ of the lockdown in Italy. The participants were adult patients with cancer (≥ 18 years) who were sheltering at home because of the COVID‐19 outbreak in Italy, regardless of their stage of disease and treatment phase.
2.2. Instruments
Perceived isolation was measured using the ISOLA scale (Biagioli et al., 2019a). This is a 14‐item self‐reported questionnaire to assess the perception of being in protective isolation. It was originally developed to collect the isolation experiences of patients with haematological malignancies undergoing haematopoietic stem cell transplantation (HSCT). Its construct validity has been tested through exploratory factor analysis (EFA), and three dimensions have been found: isolation‐related suffering (F1), problems in relationships with others (F2) and difficulties in one's relationship with oneself (F3) (Biagioli et al., 2019a). Participants are asked to indicate the extent to which they feel isolated, on a scale ranging from 1 (not at all) to 5 (completely). Higher scores in each of the three dimensions indicate a more negative experience. In this study, at the end of the ISOLA scale, two open‐ended questions were posed: ‘What is helping you in this isolating situation?’ and ‘What is the worst aspect of this isolating condition for you?’.
Socio‐demographic information and information on the cancer diagnosis were also collected, together with data about the characteristics of the participants’ sheltering at home. Participants were asked to describe the changes in their relationships with their family members, their beliefs about their risk of SARS‐CoV‐2 infection and potential complications, and the impact on their disease, using multiple‐choice items.
2.3. Procedure and ethical aspects
People living with cancer were invited to participate in the study while they were self‐isolating at home because of the national lockdown. The lockdown was imposed by the Italian government on 9th March in response to the growing COVID‐19 outbreak in the country, was confirmed on 17th March (with additional restrictions mandating the temporary closure of non‐essential shops and the closure of parks) and was relaxed on 4th May 2020. Potential participants were contacted via social groups like Facebook or patient associations and asked to fill in the survey by following a link. A snowball sample was generated among cancer patients.
The study's purposes, procedures and data collection were clearly explained to potential participants in the text accompanying the link to the survey. The first part of the survey informed them that participation was voluntary and that completion of the survey included consent to the use of the data for scientific purposes. The data were collected and held anonymously according to the International Ethical Guidelines and Principles for Research (CIOMS, 2016). The study was approved by the Institutional Review Board of the Italian Association of Cancer Nurses (AIIAO), which has the role of evaluating and approving scientific projects.
2.4. Data analysis
The study variables were described using descriptive statistics (frequency, percentage, range, median, mean and standard deviation [SD]). The construct validity of the ISOLA scale in the context of being isolated at home, which was hypothesised to be similar to the original version (Biagioli et al., 2019a), was tested through confirmatory factorial analysis (CFA) using a robust estimator (MLr). To evaluate the fit of the model, the following indices were considered: chi‐square (χ 2), the root mean square error of approximation (RMSEA; values ≤0.06 indicate a good fit), the comparative fit index (CFI; values ≥0.90 indicate a good fit), the Tucker and Lewis index (TLI; values ≥0.90 indicate a good fit) and the standardised root mean square residual (SRMR; values ≤0.08 indicate a good fit) (Muthén & Muthén, 1998‐2017). Reliability was tested using Cronbach's alpha (internal consistency).
The ISOLA scale scores were calculated as means (SD). Univariate analysis of variance (ANOVA) and t‐tests were used to identify any difference in the mean scores for socio‐demographic and clinical variables. Pearson correlation was employed to investigate associations between continuous variables. Statistical analyses were performed using SPSS 22.00 (IBM Corp, Chicago) and Mplus 6.1 (Muthèn & Muthèn, Los Angeles, California 2012).
To analyse the two open‐ended questions at the end of the ISOLA scale, we used a descriptive qualitative approach based on inductive qualitative content analysis (Vaismoradi et al., 2013). The coding process was systematic, and sentence responses to each question constituted the meaning units. Two researchers first read and discussed each meaning unit and then assigned units with a shared sense to preliminary sub‐categories. To generate overarching commonalities, the sub‐categories were grouped into broad categories, which were exhaustive and mutually exclusive. Consensus with two additional expert researchers was gained to ensure trustworthiness.
3. RESULTS
3.1. Participant characteristics
Overall, 195 patients with cancer completed the survey. Their socio‐demographic and clinical characteristics are reported in Table 1. They were mainly female (n = 148, 75.9%), with a mean age of 50.3 (SD = 11.2, range = 25–78) years and a high level of education (university or postgraduate = 66, 34%). The patients had been diagnosed with haematological malignancies (n = 100, 51.3%), breast cancer (n = 51, 26.2%) or another solid tumour (n = 44, 22.6%). Only 9% were living alone and 39.1% were living with children younger than 18 years (Table 2).
Table 1.
Participants’ socio‐demographic characteristics (n = 195).
| n | % | |
|---|---|---|
| Sex | ||
| Male | 47 | 24.1 |
| Female | 148 | 75.9 |
| Age (mean, SD) | 50.3 | (11.2) |
| Age | ||
| <40 years | 32 | 16.5 |
| 40–50 years | 68 | 35.1 |
| 51–60 years | 52 | 26.8 |
| >60 years | 42 | 21.6 |
| Education | ||
| ≤Secondary school | 29 | 14.9 |
| High school | 99 | 51.0 |
| University | 45 | 23.2 |
| Postgraduate | 21 | 10.8 |
| Marital status | ||
| Single | 29 | 14.9 |
| Partnered | 129 | 66.5 |
| Divorced/ Widowed | 36 | 18.6 |
| Italian region | ||
| North | 75 | 38.9 |
| Centre | 51 | 26.4 |
| South | 67 | 34.7 |
| Cancer diagnosis | ||
| Haematology | 100 | 51.3 |
| Breast cancer | 51 | 26.2 |
| Others | 44 | 22.6 |
| Religiosity | ||
| Believer | 90 | 47.1 |
| Quite a believer | 48 | 25.1 |
| Not believer/indifferent | 53 | 27.7 |
| Living with | ||
| Partner | 48 | 25.0 |
| Partner and children | 74 | 38.5 |
| Alone | 17 | 8.9 |
| Other | 53 | 27.6 |
| Living with children <18 years | ||
| Yes | 75 | 39.1 |
| No | 117 | 60.9 |
Table 2.
Participants’ opinion, behaviour and experiences during self‐isolation (n = 195).
| n | % | |
|---|---|---|
| Time in self‐isolation | ||
| <4 weeks | 57 | 29.2 |
| 4–6 week | 61 | 31.3 |
| >6 weeks | 77 | 39.5 |
| I leave my house | ||
| Every day | 15 | 7.7 |
| Sometimes (2–3 times per week) | 23 | 11.9 |
| Rarely | 115 | 59.3 |
| Never | 41 | 21.1 |
| Changes in the relationship with family members a | ||
| No kisses and hugs | 61 | 31.9 |
| Social distance | 23 | 12.0 |
| Separate rooms | 13 | 6.8 |
| Nothing changed | 107 | 56.0 |
| Other | 13 | 6.8 |
| SARS‐CoV‐2 infection | ||
| I believe I am at higher risk | 105 | 53.8 |
| I believe I am not at higher risk | 90 | 46.2 |
| I will suffer from severe consequences in case of infection due to my cancer | ||
| Very much/Completely | 99 | 50.8 |
| Quite a bit | 46 | 23.6 |
| A little/Not at all | 50 | 25.6 |
| My cancer will become less important | ||
| Very much/Completely | 47 | 24.5 |
| Quite a bit | 38 | 19.8 |
| A little/Not at all | 107 | 55.7 |
| Health status under control | ||
| No | 56 | 29.0 |
| Yes | 137 | 71.0 |
| Fear of going to the hospital | ||
| Not at all | 16 | 8.3 |
| A little | 65 | 33.7 |
| Quite a bit | 40 | 20.7 |
| Very much/Completely | 72 | 37.3 |
Multi‐response variable.
3.2. Participants’ opinion, behaviour and experiences during self‐isolation
Many of the respondents (n = 77, 39.5%) had been in self‐isolation for more than six weeks. Most participants reported never or rarely (n = 156, 80.4%) leaving their house during the lockdown (Table 2). Changes in their relationships with their family members occurred in 45.1% participants, including avoiding kisses and hugs (n = 61, 31.9%) and practising social distancing (n = 23, 12.0%). Many participants believed that they were at higher risk of SARS‐CoV‐2 infection than the general population (n = 105, 53.8%) and were extremely or very afraid of suffering from severe consequences in the case of infection, because of their cancer (n = 99, 50.8%). Some of them (n = 47, 24.5%) were also very or completely afraid that their cancer care would become less important and that this would have a negative impact on their prognosis (n = 26, 19.1%). About 29% (n = 56) of the participants reported that their health status was not under control, mainly because their cancer condition was not being monitored through clinical examinations (n = 17, 8.7%) and/or at outpatient visits (n = 41, 21%). Besides, many of them (n = 72, 37.3%) were very or extremely afraid of going to hospital because of the COVID‐19 outbreak.
3.3. ISOLA scale
The mean scores of each item of the ISOLA scale show that the participants considered not being able to stay close to their loved ones to be a relevant problem and that they felt quite detached from their loved ones, while missing contact with the outside world (Table 3). The three original dimensions (F1 ‘Isolation‐related suffering’, F2 ‘Relationship with others’ and F3 ‘Relationship with oneself’) were confirmed by the CFA, except for item 12 which loaded on F1 rather than on F3 (Figure 1). The covariance between the residuals for item 9 ‘I feel cut off from the world’ and item 11 ‘I feel imprisoned’ was specified in the model because of the similarity in meaning and modification indices. The fit indices were satisfactory: χ 2 (df: 73) = 144.69, p < 0.001; RMSEA = 0.071 (90% CI = 0.054–0.088); CFI = 0.926; TLI = 0.908; and SRMR = 0.057. The factor loadings were all significant and at least │0.3│. Cronbach's alpha for F1 was 0.88, for F2 it was 0.83, and for F3 it was 0.70. The mean scores were 2.64 (SD = 0.81) for isolation‐related suffering, 3.31 (SD = 1.13) for problems in relationships with others and 3.14 (SD = 1.06) for difficulties in one's relationship with oneself.
Table 3.
Mean scores of the 14 items about perceived isolation related to COVID‐19 (n = 195).
| Item | Mean | SD | Skew | Kurt |
|---|---|---|---|---|
| 1. I get bored because time passes slowly. | 2.06 | 1.00 | 1.07 | 1.04 |
| 2. I miss the contact with the outside world. | 3.18 | 1.14 | 0.06 | −0.91 |
| 3. I can stay in isolation with serenity. | 2.79 | 0.92 | −0.10 | 0.07 |
| 4. Being shut inside my home is hard. | 2.66 | 1.09 | 0.44 | −0.46 |
| 5. It is a problem for me not being able to stay close to my loved ones. | 3.35 | 1.17 | −0.09 | −0.97 |
| 6. I lack space to move around. | 2.23 | 1.28 | 0.86 | −0.33 |
| 7. Staying in isolation helps me to look at life from a new perspective. | 2.80 | 1.23 | 0.09 | −1.00 |
| 8. I need someone close to me to talk with. | 2.53 | 1.22 | 0.65 | −0.44 |
| 9. I feel cut off from the world. | 2.28 | 1.31 | 0.92 | −0.24 |
| 10. Staying here on my own allows me to think more about myself. | 2.91 | 1.19 | 0.13 | −0.83 |
| 11. I feel imprisoned. | 2.30 | 1.30 | 0.79 | −0.46 |
| 12. Staying in isolation makes me feel safe. | 2.90 | 1.24 | 0.04 | −0.92 |
| 13. I feel detached from my loved ones. | 3.27 | 1.27 | −0.07 | −1.13 |
| 14. I feel I want to leave my house. | 2.87 | 1.21 | 0.40 | −0.87 |
Kurt, kurtosis; SD, standard deviation; Skew, skewness.
Figure 1.
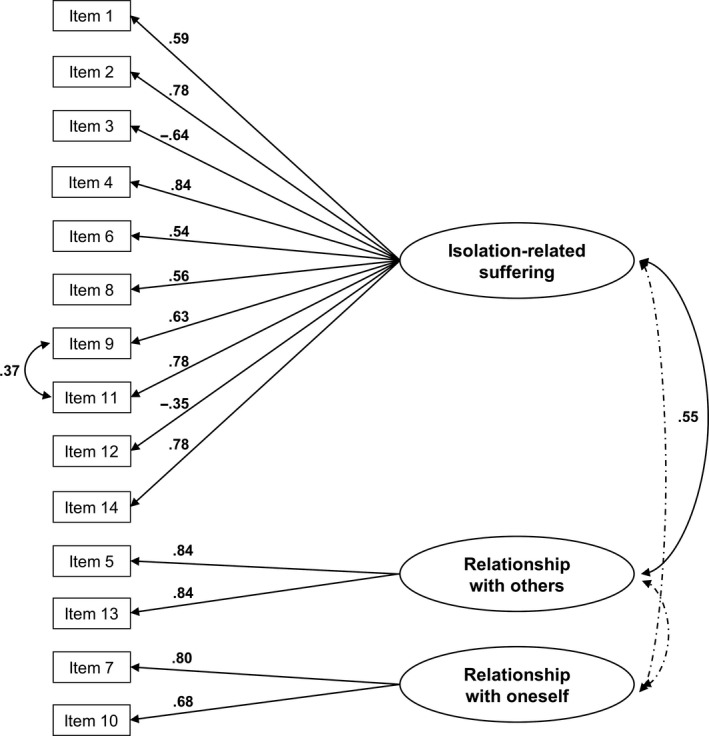
CFA model of the ISOLA scale (n = 195).
3.4. Associations
F2 was significantly negatively correlated with the level of education (r = −0.249, p < 0.001): the less education the participants had received, the more they experienced problems in their relationship with others. Also, older participants reported more problems in their relationship with others, as F2 was positively correlated with age (r = 0.249, p < 0.001). Using the ANOVA, participants living with children younger than 18 years reported fewer problems in their relationship with others than the rest of the sample (M = 3.09 ± 1.04 vs M = 3.44 ± 1.17, p = 0.04).
3.5. Qualitative data
Overall, four main categories emerged from the qualitative content analysis (Table 4). Two of these refer to the worst aspects of isolation: (1) lack of freedom and social life and (2) uncertainty and worries. The other two refer to what was helpful: (3) feeling supported and (4) dealing with isolation.
Table 4.
Categories, sub‐categories and quotes of qualitative data from the two open‐ended questions.
| Question | Main category | Sub‐category | Quotes |
|---|---|---|---|
| What is the worst aspect of this isolating condition for you? | Lack of freedom and social life | The deprivation of freedom and mobility |
I miss the freedom to move around (P86) Feeling in prison (P141) The lack of freedom (P155) |
| Detachment from family members |
I miss the rest of my family (P13) I miss the physical contact, especially with my son. His hugs are my strength, my oxygen (P16) Not being allowed to meet my parents, siblings, nephews, and friends (P176) |
||
| Lack of social interaction |
Not being allowed to hug anyone and give them my smiles and take energy from their looks (P1) Not having interpersonal relationships (P60) Not having a social life anymore (P104) |
||
| Missing everyday life |
I miss my job (P69) I miss my usual life, already partially compromised by the disease last year (P116) Having suddenly interrupted my life (P183) |
||
| Uncertainty and worries | Unknown future |
How and when it will end (P34) The feeling of being in an endless tunnel and having very few alternatives available (P50) Uncertainty (P167) |
|
| The fear of infection for oneself and loved ones |
The fear of infection because of my health condition (P39) Fear of getting COVID‐19 and infect my children (P109) Fear of contagion (P159) |
||
| Economic difficulties |
The economic aspect (P45) The perplexity about the economic solution of the problem (P54) The job uncertainty (P189) |
||
| Concerns on the health system |
Anxiety about not being able to go to the hospital (P18) Not having treatment and check‐ups (P47) Understanding that we can't trust anyone, from those who govern us to doctors (P70) |
||
| What is helping you in this isolating situation? | Feeling supported | Closeness of family |
My children (P17) My little girl and my husband (P19) My partner, as we comfort each other (P69) |
| Being close to my pets |
Having a cat (P12) Except for my puppies and my cat, nothing and nobody (P108) The fact of not being alone, because I have my husband, two teenage children, and a dog (P142) |
||
| Self‐help/mutual support |
Talking to other patients and trying to comfort them. I get so many requests for help; I am touched by their ‘thank you’ (P1) Following other patients’ stories helps me, as they are ill like me. Then I take heart (P91) |
||
| Hope and spirituality |
Prayer (P52) Meditation and yoga (P97) Faith and hope (P130) |
||
| Dealing with isolation | Use of technology |
Reading, calling friends, keeping in touch with the world on TV (P11) After so many days, the only thing that helps me is exercising and watching videos (P90) Seeing my children and grandchildren via the Internet (P34) |
|
| Engaging in daily activities |
A little workout (P27) The smart working, as it keeps my mind busy, and video calls (P44) Books, music, and TV series (P92) |
||
| Open private spaces |
Living in an isolated house with a garden, so that I can be outside to take care of my flowers and prepare the vegetable garden (P12) Having a house with a garden helps me a lot (P41) Going out into the home garden and thereby having the possibility not to be staring at four walls all day (P134) |
3.5.1. Lack of freedom and social life
The lack of freedom and social life was described in terms of deprivation of freedom and mobility, detachment from family members, lack of social interaction and missing everyday life. One of the worst aspects of self‐isolation was expressed by patients in terms of missing freedom and the possibility of moving around, so that they felt ‘in prison’ (P141). It was not only the absence of other family members who were not living with them that was particularly distressing, but also the impossibility of having physical contact with those close to them, such as their children, and this was expressed as depleting: ‘His hugs are my strength, my oxygen’ (P16). Moreover, participants reported that their social interactions had vanished: ‘Not having a social life anymore’ (P104). They also missed their everyday life and their routines, including their jobs, which contributed to their conception of normality. This was expressed as complicating a delicate situation: ‘I miss my usual life, already partially compromised by the disease last year’ (P116).
3.5.2. Uncertainty and worries
Uncertainty about an unknown future and worries about infection, economic difficulties, and the health system were predominantly expressed by the participants. The uncertainty was described as an endless tunnel and was commonly manifested about the future situation: ‘how and when it will end’ (P34). One of the participants’ biggest concerns was the fear of getting COVID‐19, which was enhanced by their cancer diagnosis: ‘the fear of infection because of my health condition’ (P39). Worries also emerged in relation to ‘the economic aspect’ (P45) and, more importantly, to the continuation of cancer care: ‘anxiety about not being able to go the hospital’ (P18).
3.5.3. Feeling supported
Feeling supported came from the closeness of family and pets, self‐help/mutual support, and hope and spirituality. In particular, participants acknowledged the value of having their family members, especially their children, close to them during self‐isolation, and finding support in their partners: ‘My partner, as we comfort each other’ (P69). Furthermore, being close to their pets had a unique buffering effect against feeling lonely during self‐isolation: ‘Except for my puppies and my cat, nothing and nobody’ (P108). Participants also reported self‐help/mutual support from other patients as a key strategy to receive and provide helpful virtual/actual support: ‘It helps me following other patients’ stories, as they are sick like me. Then I take heart’ (P91). Lastly, patients showed a deep sense of hope and spirituality, which through ‘prayer’ (P52) and ‘meditation and yoga’ (P97), became a real help.
3.5.4. Dealing with isolation
To deal with isolation, patients adopted several strategies, including the use of technology, engaging in daily activities and spending time in open private spaces. To cope with self‐isolation, it was important for the participants to keep themselves busy by ‘reading, calling friends, keeping in touch with the world on TV’ (P11). The Internet helped them a lot with this, as it allowed virtual contact: ‘Seeing my children and grandchildren via the Internet’ (P34). Patients tried to continue their daily activities, such as ‘a little workout’ (P27) and ‘the smart working, as it keeps my mind busy, and video calls’ (P44). Open private spaces, such as gardens, also helped participants spend time in self‐isolation with more serenity: ‘Living in an isolated house with a garden, so that I can be outside to take care of my flowers and prepare the vegetable garden’ (P12).
4. DISCUSSION
This study highlights how patients with cancer perceived self‐isolation at home during the Italian lockdown for COVID‐19. Their perception was assessed through the ISOLA scale, which had previously been developed for patients with cancer in protective isolation (Biagioli et al., 2019a) and was found to be valid and reliable in the context of self‐isolation at home. In particular, the CFA confirmed the three original dimensions and the items loading on them, except for item 12 (staying in isolation makes me feel safe), which loaded on F1 (isolation‐related suffering) rather than on F3 (difficulties in one's relationship with oneself). It is possible that, in the context of staying at home during a pandemic, perceived safety in isolation (item 12) becomes a measure of the extent to which people accept self‐isolation, as they give it a protective meaning that can lessen their suffering (Biagioli, Piredda, Annibali, et al., 2017). In addition, the ability to give meaning to isolation during a pandemic might not only be part of the patient's inner resources but also be reinforced by the stay‐at‐home campaigns. In fact, the participants felt moderately safe at home and rarely left their houses over a period of more than six weeks. On the one hand, their perceived safety might merely be bound up with their self‐isolation status, as a considerable number of the participants expressed a fear of going to hospital and a loss of control with regard to their cancer. On the other hand, their perceived risk of getting the SARS‐CoV‐2 infection and its complications was lower than expected (Paterson et al., 2020; Vaughan, 2011), as only half of the participants believed they were at higher risk than the general population.
Staying at home may sound easier than being isolated in a hospital room (Biagioli et al., 2017). This was confirmed in relation to several aspects such as the difficulty of being shut inside, the lack of space to move around, and boredom. One simple explanation is that a person's own house was considered to be larger and more comfortable than a hospital room. Moreover, most of the participants were not alone at home and could relate to their family members, without substantially changing their affective behaviour even when precautions were adopted. This may indicate that family relationships and affectivity remained essential despite the risk of SARS‐CoV‐2 (Stefana, Youngstrom, Jun, et al., 2020), given the tendency of cancer patients to seek emotional support from their families (Tay et al., 2011).
Nevertheless, our results revealed that prolonged self‐isolation can have a psychosocial negative impact on people living with cancer, in line with studies emphasising the dangerous implications for mental health of being sheltered in place (Brooks et al., 2020; Stefana, Youngstrom, Hopwood, et al., 2020). Participants reported substantial problems in relating to significant others, as shelter at home prevented them from being close to non‐cohabitant loved ones, and increased their feelings of detachment, in the same way as does protective isolation (Biagioli et al., 2019a). Compared to the latter situation, the participants felt more cut off from the world and more imprisoned, and they experienced less serenity and less of an advantage in looking at life from a new perspective (Biagioli et al., 2019a). The patients who experienced greater problems in their relationship with others were those with a lower level of education, in line with previous studies underlining the buffering role of education in fostering social cognitive activities while isolated (Biagioli et al., 2019b). In addition, being older and not living with minor children were factors associated with greater problems in one's relationship with others. Older adults were not only at higher risk of fatal SARS‐CoV‐2 infection (Onder et al., 2020) but were also disproportionately affected by social isolation during the lockdown period (Armitage & Nellums, 2020). Although the stress of a lockdown can be experienced at both individual and dyadic levels (Spinelli et al., 2020), the parent–child relationship may have contributed to increasing participants’ engagement in social activities, given the closure of schools and the need for parents to manage online classes for their children.
The qualitative data confirmed that self‐isolation at home during the lockdown was particularly challenging for the participants, who found it difficult to deal with the lack of freedom and social interaction, in line with studies underlining the unfavourable psychological consequences of social isolation (Brooks et al., 2020; Lippi et al., 2020). In the context of having ‘little time left to live’ in the cancer trajectory, the importance of maintaining a social life gains more relevance, given the need for patients with cancer to safeguard social relations, the activities of daily life, the perception of social support and their networks (Roij et al., 2019). Engaging in daily activities, spending time in open private spaces and using technology helped the participants to deal with isolation, while the closeness of family members and pets, self‐help/mutual support, hope and spirituality became the main drivers of the patients’ quality of life. However, the perception of being imprisoned at home might reflect the urgent need to maintain social relationships and re‐establish everyday life. This need also implies regular treatments and check‐ups, and if these are withdrawn, this can increase patients’ uncertainty, fear for the future and depression (Biagioli et al., 2020; Zheng et al., 2020). In addition, several of the participants were afraid that their cancer care would become less important because of the COVID‐19 emergency and that this would have a negative impact on their prognosis. This seems reasonable in the light of their urgent need for scans, blood monitoring, chemotherapy, surgery and transplants, which, if delayed indefinitely, could mean a loss of the window to treat. Health professionals should do their best to ensure continuity of care for these patients (ACV, 2020; Chan et al., 2020), while taking a proactive approach to reduce their challenges in accessing healthcare services (Paterson et al., 2020), in order to avoid cancer patients paying the price for this pandemic.
4.1. Limitations
Although this study represents a meaningful insight into cancer patients’ perception of staying at home during the COVID‐19 outbreak in Italy, some limitations could be addressed. First, the small sample size may significantly limit the generalisability of the results, as the participants could not be considered representative of the whole cancer population in Italy. A second limitation concerns the use of a snowball sampling technique, resulting in a non‐probabilistic sample estimation, self‐selection and an oversampling of female compared to male participants as well as other sample characteristics, such as level of education and type of cancer. Although the variables included in this study are meaningful, other variables not considered here, such as the stage of disease and treatment, could have affected the perception of isolation. Moreover, the ISOLA scale showed robust construct validity in this study, but it was developed for assessing perceived isolation in patients undergoing HSCT in protective isolation, which can be considered to be quite different from sheltering at home. Finally, another limitation is the cross‐sectional data collection, which may have prevented information being gathered about changes over time.
5. CONCLUSIONS
This study sheds light on the perceptions of self‐isolation at home in people living with cancer during the Italian lockdown. The COVID‐19 pandemic had a significant impact on their lives in terms of loneliness, detachment from loved ones, access to healthcare services and feeling safe in a critical situation. Patients who experienced more social problems were older, with less education, and lived without minor children. Although most of the participants felt safe at home, it seems that their perception of the risk of getting the SARS‐CoV‐2 infection was somehow mitigated, and they were scared both of going to hospital and of losing control of their cancer. Perceived safety in the context of a pandemic may be affected by social dynamics, preventive behaviour and personal beliefs. However, patients with cancer should be protected not only from SARS‐CoV‐2 infections but also from the severe psychosocial implications of the pandemic and treatment delays.
CONFLICT OF INTEREST
The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
AUTHOR CONTRIBUTION
V.B., B.A. and R.C. conceived and planned the survey. V.B., B.A. and S.B. disseminated the survey. A.P. was involved in planning and supervised the work. V.B. performed statistical analyses. S.B. and B.A. analysed qualitative data. V.B. and R.C. verified the qualitative content analysis. V.B. wrote the manuscript with input from all authors. All authors discussed the results and contributed to the final manuscript.
ACKNOWLEDGEMENTS
We would like to thank the patient participants. In particular, Antonella Barone, Sandro Muscolino, Giacomo Giurato and Donatella Giagnori provided precious suggestions for the development of the survey. We also acknowledge the support of Serafina Biagioli, PsyD, in the revision of the survey and the qualitative data.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Adams, R. N. , Mosher, C. E. , Abonour, R. , Robertson, M. J. , Champion, V. L. , & Kroenke, K. (2016). Cognitive and situational precipitants of loneliness among patients with cancer: A qualitative analysis. Oncology Nursing Forum, 43(2), 156–163. 10.1188/16.ONF.156-163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armitage, R. , & Nellums, L. B. (2020). COVID‐19 and the consequences of isolating the elderly. The Lancet Public Health, 5(5), e256. 10.1016/S2468-2667(20)30061-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Association ‘Codice Viola’ (ACV) (2020). Diluvia sul bagnato: Risultati questionario Coronavirus [When it rains, it pours: Coronavirus questionnaire results]. Retrieved 14th April 2020, from Tumore pancreas website: https://tumorepancreas.codiceviola.org/pazienti‐cancro‐risultati‐questionario‐coronavirus/ [Google Scholar]
- Biagioli, V. , Belloni, S. , Albanesi, B. , Piredda, A. , & Caruso, R. (2020). Comment on “The experience on coronavirus disease 2019 and cancer from an oncology hub institution in Milan, Lombardy Region” and reflections from the Italian Association of Oncology Nurses. European Journal of Cancer, 135, 8–10. 10.1016/j.ejca.2020.05.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biagioli, V. , Piredda, M. , Alvaro, R. , & de Marinis, M. G. (2017). The experiences of protective isolation in patients undergoing bone marrow or haematopoietic stem cell transplantation: Systematic review and metasynthesis. European Journal of Cancer Care, 26(5), e12461. 10.1111/ecc.12461 [DOI] [PubMed] [Google Scholar]
- Biagioli, V. , Piredda, M. , Annibali, O. , Iacorossi, L. , D'Angelo, D. , Matarese, M. , Alvaro, R. , & De Marinis, M. G. (2017). Being in protective isolation following autologous haematopoietic stem cell transplantation: A phenomenological study. Journal of Clinical Nursing, 26(23–24), 4467–4478. 10.1111/jocn.13777 [DOI] [PubMed] [Google Scholar]
- Biagioli, V. , Piredda, M. , Annibali, O. , Tirindelli, M. C. , Pignatelli, A. , Marchesi, F. , Mauroni, M. R. , Soave, S. , Del Giudice, E. , Ponticelli, E. , Clari, M. , Cavallero, S. , Monni, P. , Ottani, L. , Sica, S. , Cioce, M. , Cappucciati, L. , Bonifazi, F. , Alvaro, R. , … Gargiulo, G. (2019a). Development and initial validation of a questionnaire to assess patients’ perception of protective isolation following haematopoietic stem cell transplantation. European Journal of Cancer Care, 28(2), e12955. 10.1111/ecc.12955 [DOI] [PubMed] [Google Scholar]
- Biagioli, V. , Piredda, M. , Annibali, O. , Tirindelli, M. C. , Pignatelli, A. , Marchesi, F. , Mauroni, M. R. , Soave, S. , Del Giudice, E. , Ponticelli, E. , Clari, M. , Cavallero, S. , Monni, P. , Ottani, L. , Sica, S. , Cioce, M. , Cappucciati, L. , Bonifazi, F. , Alvaro, R. , … Gargiulo, G. (2019b). Factors influencing the perception of protective isolation in patients undergoing haematopoietic stem cell transplantation: A multicentre prospective study. European Journal of Cancer Care, 28(6), e13148. 10.1111/ecc.13148 [DOI] [PubMed] [Google Scholar]
- Biagioli, V. , Piredda, M. , Mauroni, M. R. , Alvaro, R. , & De Marinis, M. G. (2016). The lived experience of patients in protective isolation during their hospital stay for allogeneic haematopoietic stem cell transplantation. European Journal of Oncology Nursing, 24, 79–86. 10.1016/j.ejon.2016.09.001 [DOI] [PubMed] [Google Scholar]
- Brooks, S. K. , Webster, R. K. , Smith, L. E. , Woodland, L. , Wessely, S. , Greenberg, N. , & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet, 395(10227), 912–920. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casagrande, M. , Favieri, F. , Tambelli, R. , & Forte, G. (2020). The enemy who sealed the world: Effects quarantine due to the COVID‐19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Medicine, 75, 12–20. 10.1016/j.sleep.2020.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan, A. , Ashbury, F. , Fitch, M. I. , Koczwara, B. , & Chan, R. J. , & MASCC Survivorship Study Group (2020). Cancer survivorship care during COVID‐19‐perspectives and recommendations from the MASCC survivorship study group. Supportive Care in Cancer, 28, 3485–3488. 10.1007/s00520-020-05544-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cinar, P. , Kubal, T. , Freifeld, A. , Mishra, A. , Shulman, L. , Bachman, J. , Fonseca, R. , Uronis, H. , Klemanski, D. , Slusser, K. , & Lunning, M. (2020). Safety at the time of the COVID‐19 pandemic: How to keep our oncology patients and healthcare workers safe. Journal of the National Comprehensive Cancer Network, 1–6, 10.6004/jnccn.2020.7572 [DOI] [PubMed] [Google Scholar]
- Combs, S. E. , Belka, C. , Niyazi, M. , Corradini, S. , Pigorsch, S. , Wilkens, J. , Grosu, A. L. , Guckenberger, M. , Ganswindt, U. , & Bernhardt, D. (2020). First statement on preparation for the COVID‐19 pandemic in large German Speaking University‐based radiation oncology departments. Radiation Oncology, 15(1), 1–12. 10.1186/s13014-020-01527-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Council for International Organizations of Medical Sciences (CIOMS) (2016). International ethical guidelines for health‐related research involving humans, 4th ed. Council for International Organizations of Medical Sciences. [Google Scholar]
- Emami, A. , Javanmardi, F. , Pirbonyeh, N. , & Akbari, A. (2020). Prevalence of underlying diseases in hospitalized patients with COVID‐19: A systematic review and meta‐analysis. Archives of Academic Emergency Medicine, 8(1), e35. [PMC free article] [PubMed] [Google Scholar]
- European Society for Medical Oncology (ESMO) (2020). Cancer care during the COVID‐19 pandemic: An ESMO guide for patients. Retrieved April 2020, from https://www.esmo.org/for‐patients/patient‐guides/cancer‐care‐during‐the‐covid‐19‐pandemic [Google Scholar]
- Hawryluck, L. , Gold, W. L. , Robinson, S. , Pogorski, S. , Galea, S. , & Styra, R. (2004). SARS control and psychological effects of quarantine, Toronto. Canada. Emerging Infectious Diseases, 10(7), 1206–1212. 10.3201/eid1007.030703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Istituto Superiore di Sanità (ISS) (2020). Characteristics of COVID‐19 patients dying in Italy: Report based on available data on April 6th, 2020. Retrieved May 2020, from https://www.epicentro.iss.it/en/coronavirus/bollettino/Report‐COVID‐2019_6_april_2020.pdf [Google Scholar]
- Italian Ministry of Health (2020). FAQ ‐ Covid‐19, questions and answers. Retrieved May 2020, from http://www.salute.gov.it/portale/nuovocoronavirus/dettaglioFaqNuovoCoronavirus.jsp?lingua=english&id=230#11 [Google Scholar]
- Lazzerini, M. , & Putoto, G. (2020). COVID‐19 in Italy: Momentous decisions and many uncertainties. The Lancet Global Health, 8(5), e641–e642. 10.1016/S2214-109X(20)30110-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang, W. , Guan, W. , Chen, R. , Wang, W. , Li, J. , Xu, K. E. , Li, C. , Ai, Q. , Lu, W. , Liang, H. , Li, S. , & He, J. (2020). Cancer patients in SARS‐CoV‐2 infection: A nationwide analysis in China. The Lancet Oncology, 21(3), 335–337. 10.1016/S1470-2045(20)30096-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lippi, G. , Henry, B. M. , Bovo, C. , & Sanchis‐Gomar, F. (2020). Health risks and potential remedies during prolonged lockdowns for coronavirus disease 2019 (COVID‐19). Diagnosis, 7(2), 85–90. 10.1515/dx-2020-0041 [DOI] [PubMed] [Google Scholar]
- Meattini, I. , Franco, P. , Belgioia, L. , Boldrini, L. , Botticella, A. , De Santis, M. C. , Marvaso, G. , Montesi, G. , Parisi, S. , Triggiani, L. , Lambertini, M. , & Livi, L. (2020). Radiation therapy during the coronavirus disease 2019 (covid‐19) pandemic in Italy: A view of the nation’s young oncologists. ESMO Open, 5(2), e000779. 10.1136/esmoopen-2020-000779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén, L. & Muthén, B. (1998–2017). Mplus user's guide (8th ed.). Muthén & Muthén. [Google Scholar]
- National Comprehensive Cancer Network (NCCN) (2020). Coronavirus disease 2019 (COVID‐19): Resources for the cancer care community. Retrieved April 2020, from https://www.nccn.org/covid‐19/ [Google Scholar]
- Onder, G. , Rezza, G. , & Brusaferro, S. (2020). Case‐fatality rate and characteristics of patients dying in relation to COVID‐19 in Italy. Journal of American Medical Association, 323(18), 1775–1776. 10.1001/jama.2020.4683 [DOI] [PubMed] [Google Scholar]
- Passamonti, F. , Cattaneo, C. , Arcaini, L. , Bruna, R. , Cavo, M. , Merli, F. , Angelucci, E. , Krampera, M. , Cairoli, R. , Della Porta, M. G. , Fracchiolla, N. , Ladetto, M. , Gambacorti Passerini, C. , Salvini, M. , Marchetti, M. , Lemoli, R. , Molteni, A. , Busca, A. , Cuneo, A. , … Corradini, P. (2020). Clinical characteristics and risk factors associated with COVID‐19 severity in patients with haematological malignancies in Italy: A retrospective, multicentre, cohort study. The Lancet Haematology, 7(10), e737–e745. 10.1016/S2352-3026(20)30251-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paterson, C. , Gobel, B. , Gosselin, T. , Haylock, P. J. , Papadopoulou, C. , Slusser, K. , Rodriguez, A. , & Pituskin, E. (2020). Oncology nursing during a pandemic: Critical reflections in the context of COVID‐19. Seminars in Oncology Nursing, 36(3), . 10.1016/j.soncn.2020.151028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Remuzzi, A. , & Remuzzi, G. (2020). COVID‐19 and Italy: What next? Lancet, 395(10231), 1225–1228. 10.1016/S0140-6736(20)30627-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson, S. , Hirsch, J. S. , Narasimhan, M. , Crawford, J. M. , McGinn, T. , Davidson, K. W. , Barnaby, D. P. , Becker, L. B. , Chelico, J. D. , Cohen, S. L. , Cookingham, J. , Coppa, K. , Diefenbach, M. A. , Dominello, A. J. , Duer‐Hefele, J. , Falzon, L. , Gitlin, J. , Hajizadeh, N. , Harvin, T. G. , … Zanos, T. P. (2020). Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID‐19 in the New York city area. Journal of American Medical Association, 323(20), 2052–2059. 10.1001/jama.2020.6775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin, G. J. , & Wessely, S. (2020). The psychological effects of quarantining a city. British Medical Journal, 368, . 10.1136/bmj.m313 [DOI] [PubMed] [Google Scholar]
- Russano, M. , Citarella, F. , Vincenzi, B. , Tonini, G. , & Santini, D. (2020). COVID‐19 or lung cancer: What should we treat? Journal of Thoracic Oncology, 15(7), e105–e106. 10.1016/j.jtho.2020.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Secinti, E. , Rand, K. L. , Johns, S. A. , O’Neil, B. H. , Helft, P. R. , Shahda, S. , Jalal, S. I. , & Mosher, C. E. (2019). Social correlates of mental health in gastrointestinal cancer patients and their family caregivers: Exploring the role of loneliness. Supportive Care in Cancer, 27(6), 2077–2086. 10.1007/s00520-018-4467-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sjödin, H. , Wilder‐Smith, A. , Osman, S. , Farooq, Z. , & Rocklöv, J. (2020). Only strict quarantine measures can curb the coronavirus disease (COVID‐19) outbreak in Italy, 2020. Euro Surveillance, 25(13). 10.2807/1560-7917.ES.2020.25.13.2000280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spinelli, M. , Lionetti, F. , Pastore, M. , & Fasolo, M. (2020). Parents' stress and children's psychological problems in families facing the COVID‐19 outbreak in Italy. Frontiers in Psychology, 11, 1713. 10.3389/fpsyg.2020.01713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stefana, A. , Youngstrom, E. A. , Hopwood, C. J. , & Dakanalis, A. (2020). The COVID‐19 pandemic brings a second wave of social isolation and disrupted services. European Archives of Psychiatry and Clinical Neuroscience, 270, 785–786. 10.1007/s00406-020-01137-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stefana, A. , Youngstrom, E. A. , Jun, C. , Hinshaw, S. , Maxwell, V. , Michalak, E. , & Vieta, E. (2020). The COVID‐19 pandemic is a crisis and opportunity for bipolar disorder. Bipolar Disorders, 22(6), 641–643. 10.1111/bdi.12949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tay, L. H. , Hegney, D. , & Ang, E. (2011). Factors affecting effective communication between registered nurses and adult cancer patients in an inpatient setting: A systematic review. International Journal of Evidence‐Based Healthcare, 9(2), 151–164. 10.1111/j.1744-1609.2011.00212.x [DOI] [PubMed] [Google Scholar]
- Trapani, D. , Marra, A. , & Curigliano, G. (2020). The experience on coronavirus disease 2019 and cancer from an oncology hub institution in Milan, Lombardy Region. European Journal of Cancer, 132, 199–206. 10.1016/j.ejca.2020.04.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ueda, M. , Martins, R. , Hendrie, P. C. , McDonnell, T. , Crews, J. R. , Wong, T. L. , McCreery, B. , Jagels, B. , Crane, A. , Byrd, D. R. , Pergam, S. A. , Davidson, N. E. , Liu, C. , & Stewart, F. M. (2020). Managing cancer care during the COVID‐19 pandemic: Agility and collaboration toward a common goal. Journal of the National Comprehensive Cancer Network, 1–4, 366–369. 10.6004/jnccn.2020.7560 [DOI] [PubMed] [Google Scholar]
- Vaismoradi, M. , Turunen, H. , & Bondas, T. (2013). Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nursing and Health Sciences, 15(3), 398–405. 10.1111/nhs.12048 [DOI] [PubMed] [Google Scholar]
- Valenza, F. , Papagni, G. , Marchianò, A. , Daidone, M. G. , De’Braud, F. , Colombo, M. P. , Frignani, A. , Galmozzi, G. , Ladisa, V. , Pruneri, G. , Salvioni, R. , Spada, P. , Torresani, M. , Rinaldi, O. , Manfredi, S. , Votta, M. , & Apolone, G. (2020). Response of a comprehensive cancer center to the COVID‐19 pandemic: The experience of the Fondazione IRCCS‐Istituto Nazionale dei Tumori di Milano. Tumori, 106(3), 193–202. 10.1177/0300891620923790 [DOI] [PubMed] [Google Scholar]
- van Roij, J. , Brom, L. , Youssef‐El Soud, M. , van de Poll‐Franse, L. , & Raijmakers, N. J. H. (2019). Social consequences of advanced cancer in patients and their informal caregivers: A qualitative study. Supportive Care in Cancer, 27(4), 1187–1195. 10.1007/s00520-018-4437-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaughan, E. (2011). Contemporary perspectives on risk perceptions, health‐protective behaviors, and control of emerging infectious diseases. International Journal of Behavioral Medicine, 18(2), 83–87. 10.1007/s12529-011-9160-y [DOI] [PubMed] [Google Scholar]
- Vigo, D. , Patten, S. , Pajer, K. , Krausz, M. , Taylor, S. , Rush, B. , Raviola, G. , Saxena, S. , Thornicroft, G. , & Yatham, L. N. (2020). Mental health of communities during the COVID‐19 pandemic. Canadian Journal of Psychiatry, 65(10), 681–687. 10.1177/0706743720926676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, C. , Pan, R. , Wan, X. , Tan, Y. , Xu, L. , Ho, C. S. , & Ho, R. C. (2020). Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID‐19) epidemic among the general population in China. International Journal of Environmental Research and Public Health, 17(5), 1729. 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, D. , Hu, B. O. , Hu, C. , Zhu, F. , Liu, X. , Zhang, J. , Wang, B. , Xiang, H. , Cheng, Z. , Xiong, Y. , Zhao, Y. , Li, Y. , Wang, X. , & Peng, Z. (2020). Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus‐infected pneumonia in Wuhan, China. Journal of American Medical Association, 323(11), 1061–1069. 10.1001/jama.2020.1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO) (2020). Responding to community spread of COVID‐19: Interim guidance, 7 March 2020. Retrieved April 2020, from https://www.who.int/publications‐detail/responding‐to‐community‐spread‐of‐covid‐19 [Google Scholar]
- Yu, J. , Ouyang, W. , Chua, M. L. K. , & Xie, C. (2020). SARS‐CoV‐2 transmission in patients with cancer at a tertiary care hospital in Wuhan, China. Journal of American Medical Association Oncology, 6(7), 1108–1110. 10.1001/jamaoncol.2020.0980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng, X. , Tao, G. , Huang, P. , He, F. , Shao, X. , Xu, Y. , Yang, G. (2020). Self‐reported depression of cancer patients under 2019 novel coronavirus pandemic. SSRN Electronic Journal. 10.2139/ssrn.3555252 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


