To the Editor:
A 5‐month‐old Caucasian male child presented with 36 h of persistent fever (temperature 40.2°C). The patient was very irritable, with lip ulceration and perineal cellulitis. Complete blood counts showed nonregenerative anemia, leukopenia, and severe neutropenia (hemoglobin, 7.6 g/dL; leukocyte count, 1660/μL; neutrophil count, 150/μL; lymphocyte count, 1380/μL, platelet count, 157 × 103/μL). A bone marrow aspiration showed hyperplasia of the granulocyte lineage with notably unbalanced maturation shifted toward promyelocytic and myelocytic forms, whereas neutrophils were very poorly represented (bone marrow smear differential count:70% granulocyte lineage cells including 8% myeloblasts, 16% promyelocytes, 23% myelocytes, 15% metamyelocytes, 3% neutrophils, as illustrated in Figure 1, panel A). Granular precursors showed cytological atypia, including the regular presence of small vacuoles (panel B), persistence of basophilia in myelocytes and large metamyelocytes with banded nuclei (panel C). Also, there was relative hypoplasia of the erythroid lineage with erythroblast precursors often carrying small vacuoles (panel D). In the context of pandemic COVID‐19, the nasal swab polymerase chain reaction test routinely performed was negative but SARS‐CoV‐2 antibody IgG and IgM tests were positive, leading to the diagnosis of pediatric inflammatory multisystem syndrome temporally associated with COVID‐19 (PIMS‐TS; also known as multisystem inflammatory syndrome in children [MIS‐C]). 1
FIGURE 1.
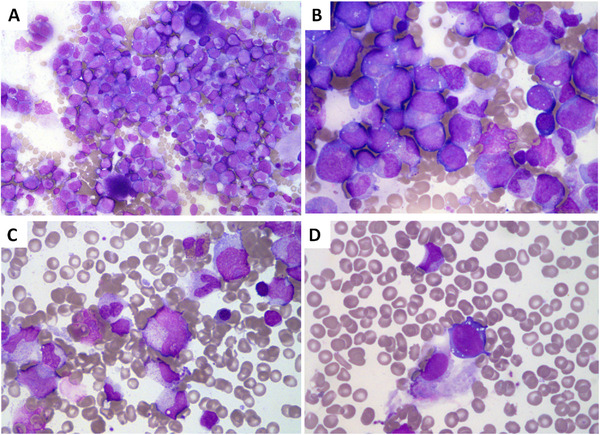
Bone marrow aspirate smear. (A) Hyperplasia of the granulocyte lineage with unbalanced maturation shifted toward promyelocytic and myelocytic forms (original magnification ×40). (B) Granular precursors with presence of small vacuoles (original magnification ×100). (C) Persistence of basophilia in myelocytes and large metamyelocytes with banded nuclei (original magnification ×100). (D) Erythroblast precursor carrying small vacuoles (original magnification ×100)
The patient was successfully treated with filgrastim (10 μg/kg/day for 4 days), empirical broad‐spectrum intravenous antibiotic therapy, and immunoglobulin. Moderate neutropenia persisted for 1 month after discontinuation of filgrastim (range, 500‐1200/μL) before complete normalization without further intervention. Study of known genes involved in congenital neutropenia using a targeted NGS panel of 28 genes 2 did not detect anypathogenic variants and tests for antibodies against neutrophil membrane antigen were negative. At the last evaluation 5 months later, the neutrophil count was normal at 2700/μL.
Neutropenia related to COVID‐19 infection is uncommon; the hematological abnormalities associated with COVID‐19 infection are lymphopenia and less frequently neutrophilia or thrombophilia. 3 , 4 Neutropenia is also not a characteristic associated with PIMS‐TS 1 and this was the only PIMS‐TS case with neutropenia reported in our institution. 5 Conversely, postviral neutropenia is frequent and associated with zero or minor consequences, which was not the case initially for this patient.
Thus, the clinico‐hematological presentation reported here with favorable outcome is atypical and requires a specific attention for clinicians and biologists while facing an emerging disease such as COVID‐19.
CONFLICT Of INTEREST
The authors declare that there is no conflict of interest.
REFERENCES
- 1. Harwood R, Allin B, Jones CE, et al. A national consensus management pathway for paediatric inflammatory multisystem syndrome temporally associated with COVID‐19 (PIMS‐TS): results of a national Delphi process. Lancet Child Adolesc Health. 2020. 10.1016/S2352-4642(20)30304-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Donadieu J, Beaupain B, Fenneteau O, Bellanné‐Chantelot C. Congenital neutropenia in the era of genomics: classification, diagnosis, and natural history. Br J Haematol. 2017;179:557‐574. [DOI] [PubMed] [Google Scholar]
- 3. Frater JL, Zini G, d'Onofrio G, Rogers HJ. COVID‐19 and the clinical hematology laboratory. Int J Lab Hematol. 2020;42(Suppl 1):11‐18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fan BE, Chong VCL, Chan SSW, et al. Hematologic parameters in patients with COVID‐19 infection. Am J Hematol. 2020;95:E131‐E134. [DOI] [PubMed] [Google Scholar]
- 5. Carbajal R, Lorrot M, Levy Y, et al. Multisystem inflammatory syndrome in children rose and fell with the first wave of the COVID‐19 pandemic in France. Acta Paediatr. 2020. 10.1111/apa.15667. [DOI] [PMC free article] [PubMed] [Google Scholar]


